CA0012192 Prov enews 12-19-06.indd
advertisement

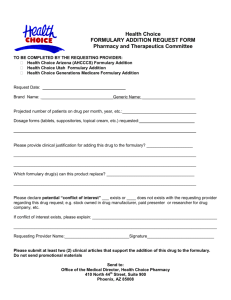
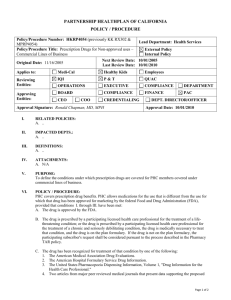
Volume 2 2006 Table of Contents To view a specific article, click on the article title, and it will take you directly to the story. Priority Policy and Benefit Updates In this redesigned issue of STAT, the Blue Cross of California (Blue Cross) Provider e-News, you will find important policy updates and new programs or services to help you care for our members in these plans: • Medi-Cal • L.A. Care Health Plan • Healthy Families Program • Access for Infants and Mothers • Managed Risk Medical Insurance Program • County Medical Services Program Provider Tools Now Online Your time is valuable. To make it easier and faster for you to do your work, we have added some important information to our provider website. Prior Authorization Forms You now can find our prior authorization forms for the top 10 most popular provider authorization requests − right at your fingertips! Click here to go to the forms now. To use these forms in the future go to www.bluecrossca.com. Click on Providers. Then click on State Sponsored Plans (Medi-Cal, Healthy Families Program, MRMIP, AIM, CMSP). Click on Prior Authorization Toolkit. Then click on the plan type of the member and select the form. You can download and complete the forms or follow the instructions on where to call for prior authorization. Utilization Management (UM) Guidelines Our corporate clinical UM guidelines now are available online for your review. Members also have access to these guidelines. To view these guidelines, visit www.bluecrossca.com. On the home page, click on Medical Policies and Clinical UM Guidelines. This link is the first bullet under the Learn More heading at the bottom left of the page. We have adopted these clinical guidelines that apply to our plans. Hard copies of these UM guidelines are available upon request. 1 Provider Tools Now Online 2 Quality Improvement Program Ensures Accessible Quality Care 4 Medical Record Audit Compliance Rate Takes a Dip Spotlight 4 Apply for NPI Now! 6 Blue Cross Receives Prestigious EPA Award 7 Awarded NCQA Excellent Status Operations Updates 7 Change in Address? 7 After-Hours Care Health Improvement 8 Initial Health Assessment Reminder 8 Educate Members About the Flu 9 New Surgeon General’s Report on Secondhand Smoke Rx Updates 10 Formulary Available Online 10 New Formulary Updates – Second Quarter, Third Quarter, Third Quarter Supplement, and Fourth Quarter 2006 14 Consider Generics 14 What You Need to Know About Prior Authorization of Benefits (PAB) 15 PAB Results Review and Notification 15 Nonformulary Medications Access 15 Quantity and Dosing STAT Physician & Provider e-News is published by Blue Cross of California to serve our State Sponsored Business providers. Blue Cross of California is an affiliate of L.A. Care Health Plan, providing Medi-Cal Managed Care services in Los Angeles County. Blue Cross of California and Blue Cross of California Partnership Plan are independent licensees of the Blue Cross Association. 1106 CA0012192 12/06 Provider e-News Vol 2 2006 1 Priority Policy and Benefit Updates Quality Improvement Program Ensures Accessible Quality Care An overview of processes, goals, and outcomes Blue Cross State Sponsored Business’ Quality Improvement (QI) Program seeks to continually improve the quality of the clinical care and services that its members receive through a systematic approach. To achieve this goal, we monitor and evaluate all aspects of the health care delivery system. We also develop and offer quality improvement initiatives directed at members, practitioners, and other health care professionals. We design our processes and procedures to ensure all covered services are available and accessible to all members, regardless of race, color, national origin, creed, ancestry, religion, language, age, gender, marital status, sexual orientation, health status, or disability, and that all covered services are provided in a culturally and linguistically appropriate manner. • Protect member-identifiable health information by ensuring that protected health information (PHI) is released in accordance with federal, state, and all other pertinent regulatory requirements • Promote collaborative activities among other Medicaid and state-funded health care plans and providers, including behavioral health providers and practitioners To thoroughly assess the system and prioritize initiatives, we select critical monitors from the following QI Program components that promote quality clinical care and service. Taking Care of Chronic Illnesses We measure public health issues and chronic conditions affecting our Medi-Cal member QI Program Goals population. We do this through the Health Plan Blue Cross has established the following goals for our Employer Data and Information Set (HEDIS), the QI Program: set of standardized performance measures designed to ensure that consumers have information to compare • Develop and maintain a well-integrated system the performance of health plans. The performance to continuously identify, measure, assess, and measures in HEDIS include cancer, heart disease, improve quality outcomes smoking, asthma, and diabetes and well as access to • Respond to the needs and expectations of the care, and customer service. Here are results of provider program’s internal and external customers by and plan performance in some key categories for evaluating performance relative to meeting those our Medi-Cal members, as well as other awards and needs and expectations achievements. It is due to our collaboration with you, • Maintain compliance with regulatory our providers, that these results are possible. requirements and accreditation standards • Promote high quality of care and service and effective utilization of service to all members, including those with a limited proficiency in English • Identify the educational needs of members, practitioners, and other health care professionals, including behavioral health care providers and practitioners as determined by product • Promote processes that reduce medical errors and improve patient safety Asthma What we track: The number of asthmatic Medi-Cal members who take the appropriate medications for asthma What we do: Help members try to keep their asthma under control • We schedule appointments for our asthmatics to see their primary care physician (PCP) if they have not been in for a visit within the last 12 months. Provider e-News Vol 2 2006 2 Priority Policy and Benefit Updates • In 2005, almost 90 percent of all asthmatic members who required medication were prescribed the correct medication. • Our asthma program was honored by the state’s External Quality Review Organization as a best practice. • We were the only health plan to receive the U.S. Environmental Protection Agency’s 2006 National Leadership Award in Asthma Management based on a series of statewide asthma projects. Read more in “Blue Cross Receives Prestigious EPA Award.” Diabetes What we track: The number of Medi-Cal diabetic members who get the required Diabetic Retinal Eye exams, Hgb A1C tests, Nephropathy screening, and Cholesterol screening annually. What we do: Provide educational materials to members, and schedule appointments for our members to see their PCP and/or ophthalmologist for their recommended screenings. Inform physicians when diabetic members are not coming in for routine exams. How we’re doing: In 2005, 56 percent of our diabetic members had a Diabetic Retinal Eye exam; an increase from 2004. Preventive Health Childhood Immunizations What we track: The number of Medi-Cal members 2 years of age and younger who get all required immunizations What we do: Send a yearly reminder to members to let them know the vaccines doctors recommend for children 2 years of age and younger How we’re doing: Blue Cross beat the Medicaid average and most health plans! In 2005, 75 percent of our members 2 years of age and younger got the immunizations they needed, including shots for mumps, measles, and hepatitis. Breast Cancer Prevention What we track: The number of female Medi-Cal members, ages 52 to 69, who have had a mammogram in the current or prior year What we do: Send a yearly reminder to our female members identified as requiring a mammogram How we’re doing: In 2005, more than 52 percent of our female members, ages 52 to 69, had mammograms Cervical Cancer Prevention What we track: The number of female Medi-Cal members, ages 21 to 64, who have had a cervical cancer screening What we do: Send a reminder to our female members identified as requiring this test How we’re doing: In 2005, more than 67 percent of our female members, ages 21 to 64, had a cervical cancer screening. Blue Cross scored better than most health plans in this category. We Ask Our Members We survey member opinions on the health care they receive. Here are a few key results from our most recent survey: • To the question regarding how easy it is to see the doctor when you need to, the response “getting care quickly” was rated 3 percent higher than last year. • Members who had a good opinion of Blue Cross as a health plan increased by 6.4 percent from last year to 75.3 percent. • Members rated more than 90 percent of the office staff in our provider offices as courteous and respectful. • Members believed 85 percent of physicians showed respect for what the member had to say and 86 percent listened carefully to what the member said. Thank you for working hard to care for our members. The survey responses show how much your efforts are paying off and making a difference to our members. Provider e-News Vol 2 2006 3 Priority Policy and Benefit Updates Medical Record Audit Compliance Rate Takes a Dip Make process improvement a priority We want to call your attention to Blue Cross’ 2006 Medical Record Audit results. The report, presented at the December meeting of the Blue Cross Physician Quality Improvement Committee (QIC), focused on the Continuity and Coordination of Care Criteria that declined from 88.7 percent in 2005 to 83 percent in 2006. This 6 percent decline revealed the lack of practitioner compliance in signing the review of lab reports, specialty consults, emergency room reports, and hospital discharge summaries. As many as 2,198 charts representing 791 primary care physicians were reviewed for the audit. Continually improving our processes and services is one of our most important goals. By bringing this finding to your attention, we would like to remind you to review your office practices related to this important documentation of member chart information prior to filing reports in your medical records. Spotlight Apply for NPI Now! Contact CMS The Health Insurance Portability and Accountability Act (HIPAA) requires the adoption of a standard 10-position unique identifier for health care providers, effective May 23, 2007. The unique identifier is the National Provider Identifier (NPI) which will replace health care provider identifiers used in HIPAA-covered entities. HIPAA-covered entities need to obtain NPIs to identify themselves in HIPAA standard transactions by May 23, 2007. Small health plans are allowed an additional 12 months to comply. Please note: As a participating Blue Cross provider, your practice is a HIPAA-covered entity. How to Get Started With only a few months before the new NPI requirements become effective, we encourage you to obtain your new NPI now from the Centers for Medicare and Medicaid Services (CMS). Visit the CMS website at www.cms.hhs.gov/NationalProvIdentStand or call (800) 465-3203 to get started. To apply for an NPI online, go to the National Plan and Provider Enumeration System website at https://nppes.cms.hhs.gov. Please apply right away. Otherwise, you may not be able to complete the full NPI transition with your health plans and electronic vendors. Not having your NPI by the scheduled effective date may disrupt services and payments. Register Your NPI with Us Once you receive your NPI, you need to complete our online submission form to register your NPI at https://npi.wellpoint.com. Registration ensures our internal systems accurately reflect your NPI information. If you are registering more than one NPI, please complete one form for each NPI. If you have a large quantity of NPIs to submit, we will implement a “bulk” submission process soon. Please be sure to check https://npi.wellpoint.com regularly for additional information regarding this process. Provider e-News Vol 2 2006 4 Spotlight Assess System Capabilities Early It will take time to incorporate NPI changes. You can help by assessing any NPI impact to your practice management systems. Consider the impact to the following technological systems you have to help gauge your NPI readiness: • Applications systems such as accounting and patient records management • Files and databases with provider numbers • Functions outsourced to other companies, such as lab work or accounting • Telephone and interactive voice response systems Consider Your Vendors If you use vendors such as medical supply companies, third-party billing agencies, and laboratory services, check and see if they are working toward becoming NPI-compliant. Their noncompliance may impact your operations and hamper your ability to transition to NPI. In addition, testing is a key component of the NPI preparation process. You may be able to minimize problems by testing early with electronic vendors and Blue Cross. By preparing in advance, you can help ensure a seamless conversion to NPI, minimizing any potential payment disruptions in your operations with us. Act now! Let’s work together to ensure that when the May 23, 2007, NPI implementation date arrives, we will be able to continue business as usual. Provider e-News Vol 2 2006 5 Spotlight Blue Cross Receives Prestigious EPA Award Addressing asthma management in a Medicaid population Blue Cross recently received the 2006 National Environmental Leadership Award in Asthma Management from the U.S. Environmental Protection Agency (EPA). This important award acknowledged our Medicaid plan and providers for offering comprehensive resources to help people with asthma lead normal, active lives. Our application, titled “Asthma, Air Quality, and Community Health: A Health Plan’s Contribution,” emphasized the exceptional importance and value of community partnerships in addressing the significant health challenges posed by asthma. “The award honored our unique accomplishments in addressing both indoor and outdoor environmental asthma triggers through the Asthma Management Program statewide, the Plan/Practice Improvement Project Asthma Collaborative in San Francisco, and the Valley Air Quality Project in Fresno,” says Blue Cross State Sponsored Business Vice President and Medical Director Dawn Wood, MD. care, and streamline daily clinical activities, so that evidence-based interactions between informed patients and prepared practice teams become the norm. By creating planned disease-management visits, maximizing patient self-management, and teaching patients to reduce exposure to environmental asthma triggers, patients and physicians are better prepared to focus on chronic illness management, and to use critical information to make the best use of their visits. (More to come on this innovative project in an upcoming e-Newsletter.) Valley Air Quality Project Through this effort, we use community partnerships and collaborative research with public health, local health care leaders, community agencies, and academic researchers to help improve community responses to environmental air pollution affecting the respiratory health of Fresno County residents. Fresno County is an area where asthma prevalence is high. (More to come on this ground-breaking project as well.) Asthma Management Program Working with the EPA You may be familiar with our Asthma Management Program. It provides a wide range of educational resources, tools, and information to members, physicians, and pharmacists to help improve member outcomes. Asthma education emphasizes minimizing exposure to asthma triggers and improving patient self-management skills. The EPA award jumpstarted a collaboration with the EPA. The coordinator for the EPA’s Pacific Southwest Region Indoor Air Program, Barbara Spark, served as a guest speaker at our Field Business Meeting, an annual event for our field staff to share best practices. Spark’s presentation, in turn, prompted our health promotion consultants at Community Resource Centers throughout California and in several other states to organize a focused project on environmental asthma management this year in collaboration with local schools. This effort will augment ongoing asthma interventions, and should help identify additional best practices in community collaboration for improved asthma outcomes. Plan/Practice Improvement Project Asthma Collaborative Facilitated by the Center for Health Care Strategies, the National Initiative for Children’s Health Care Quality, and the California Health Care Foundation, this asthma collaborative is a pilot project which involves five practices in San Francisco. The collaborative encourages physicians to apply the chronic care model to asthma To learn more about our award, visit the EPA’s site at www.epa.gov/asthma/leadership_award_winners.html. Provider e-News Vol 2 2006 6 Spotlight Awarded NCQA Excellent Status Thank you to our providers For the fourth year in a row, we have been awarded an “Excellent” accreditation status for our California Medicaid program. If you’d like to review our NCQA report card, visit www.ncqa.org. In the Hot Links! Report Cards menu on the right, click on Health Plans. The National Committee for Quality Assurance (NCQA) is a nonprofit organization created to improve patient care quality and health plan performance in partnership with managed care plans, purchasers, consumers, and the public sector. NCQA ratings were calculated using results from the Health Plan Employer Data and Information Set (HEDIS) and Consumer Assessment of Healthcare Providers and Systems surveys (CAHPS). We’d like to extend our congratulations to you, our plan providers. Without your dedication, hard work, and commitment to our members, we could not have received this accreditation. Thank you for your excellent care. Operations Updates Change in Address? After-Hours Care Contact us right away What’s expected of you If you change your office address, telephone numbers, capacity, or other important demographic information, please contact us right away. Our online Provider Change Request Form allows you to change your tax identification number, clinic hours, address, phone number, fax number, or hospital privilege information. Click here to view the form. Instructions on how to submit the form are included on the form itself. If you’re a primary care physician, you need to have an after-hours system in place and give members a telephone number to call after business hours to reach you, the on-call physician (if not you), or a provider in your physician group. You are responsible for being available to determine the need for emergency and after-hours services and to authorize care for our members who are your patients. Providers who receive calls after business hours need to contact the member back within 30 minutes of receiving the call. Refer to your Blue Cross Provider Operations Manual (POM) for a more detailed explanation of our after-hours procedures. Provider e-News Vol 2 2006 7 Health Improvement Initial Health Assessment Reminder Meeting the requirement is an important step If you’re a primary care physican, please be aware that you’re responsible for getting a complete history, physical examination, and assessment of health behaviors for all new members. This is an “initial health assessment,” or IHA. This critical procedure for treating patients is mandatory. The IHA is an important part of the audit process and providers who do not complete this assessment are out of compliance. Just as importantly, the IHA is one of the key ways to identify health problems early on and to build a relationship with your patient. You need to provide these assessments within the following mandated time frames: • Within 60 calendar days following enrollment for children under the age of 18 months, or within periodicity timelines of the American Academy of Pediatrics (AAP) for ages 2 years and younger, whichever is less • Within 120 calendar days of enrollment for children 18 months of age and older (The IHA needs to include, or you must arrange for the provision of, all necessary immunizations and an appropriate health education behavioral assessment.) • Within 120 calendar days of enrollment for adults older than 21 years of age (The assessments should include a complete history and physical exam as well as a health education behavioral risk assessment.) For more information on IHAs, refer to your POM. Helpful hint: Administer the Staying Healthy Assessment Tool along with the IHA so you have a complete medical record on each patient. Educate Members About the Flu What you can do Flu season is in full swing. Some of your patients may head to the emergency room unnecessarily and wait hours for care. A new survey by the Oakland, California-based California HealthCare Foundation indicates that publicly insured Medi-Cal patients were more than twice as likely as those with private insurance to have used emergency department services in the past year. The report shows Medi-Cal patients were less likely to have a regular doctor and more likely to use a clinic or emergency room for care. We Need Your Help You can teach our members how to get the right care for the flu. • Encourage your high-risk members to get a flu shot. • Be sure members know antibiotics will not cure the flu. • Remind your Blue Cross members that they can call the MedCall® 24-hour nurse help line at (800) 224-0336 to help them figure out what to do when they have a cold or the flu. MedCall is staffed by registered nurses who can answer questions, give self-care tips, and help members schedule an appointment when they need it. However, your members must see you for medical advice. Flu Resources • The Centers for Disease Control Flu Website www.cdc.gov/flu - Preventing the Flu www.cdc.gov/flu/protect/preventing.htm - What to Do if You Get Sick www.cdc.gov/flu/symptoms.htm - Key Facts About Influenza and the Influenza Vaccine www.cdc.gov/flu/keyfacts.htm • National Institute of Allergy and Infectious Diseases’ Focus on Flu Website www3.niaid.nih.gov/news/focuson/flu/default.htm - Is It a Cold or the Flu? www.niaid.nih.gov/Publications/cold/sick.pdf Provider e-News Vol 2 2006 8 Health Improvement New Surgeon General’s Report on Secondhand Smoke Talk to your patients who smoke U.S. Surgeon General Richard H. Carmona has issued a comprehensive scientific report that concludes no level of exposure to secondhand smoke is risk-free. This is one more reason to ask your patients if they smoke and to counsel them to quit smoking. The study indicates nonsmokers exposed to secondhand smoke at home or work increase their risk of developing heart disease by 25 to 30 percent and lung cancer by 20 to 30 percent. The finding is a major public health concern because statistics show nearly half of all nonsmoking Americans are regularly exposed to secondhand smoke. “The report is a crucial warning sign to nonsmokers and smokers alike,” says U.S. Health and Human Services Secretary Michael Leavitt. “Smoking can sicken and kill, and even people who do not smoke can be harmed by smoke from those who do.” Secondhand smoke exposure also is a known cause of sudden infant death syndrome (SIDS), respiratory problems, ear infections, and asthma attacks in infants and children, the report finds. “The good news is that, unlike some public health hazards, secondhand smoke exposure is easily prevented,” Carmona says. “Smoke-free indoor environments are proven, simple approaches that prevent exposure and harm.” You can get copies of “The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General” and related materials on the Surgeon General’s website. For details, go to: www.surgeongeneral.gov/library/secondhandsmoke. Provider e-News Vol 2 2006 9 Rx Updates Formulary Available Online Blue Cross formulary is available on our website at www.bluecrossca.com under the Learn More section. Select Pharmacy. Select the Formulary – PDF Format link on the left navigation bar if you want to print a full copy of the formulary. Other information available online includes: • Searchable drug formulary which can be obtained by selecting Formulary on the left navigation bar • Lists of preferred pharmaceuticals or formularies for various Blue Cross benefits New Formulary Updates Second Quarter 2006 The following table lists the outcomes of the second quarter 2006 WellPoint Pharmacy and Therapeutics Committee meeting held on May 31, 2006. Drug Name Active Ingredient Formulary Status Generic Available Abilify aripiprazole Add No Aerobid/M flunisolide Add No Aerospan HFA flunisolide Add No Asmanex mometasone Add No Eligard leuprolide acetate Self-Injectable Benefit* Yes Fazaclo ODT clozapine Add No Geodon ziprasidone Add No Leukine sargramostim Self-Injectable Benefit* No Generic Lupron leuprolide acetate Self-Injectable Benefit* Yes Neulasta pegfilgrastim Self-Injectable Benefit* No Neupogen filgrastim Self-Injectable Benefit* No Synarel narfarelin Delete No Twinject epinephrine Self-Injectable Benefit* No *Self-Injectable Benefit: Members should refer to our Member Handbook for benefit details regarding applicable copayments or coinsurance. Please Note These pharmacy updates are not applicable to County Medical Services Program (CMSP) members. CMSP members have pharmacy benefits through MedImpact. See www.cmspcounties.org for more information. Provider e-News Vol 2 2006 10 Rx Updates Third Quarter 2006 This table lists the outcomes of the third quarter 2006 WellPoint Pharmacy and Therapeutics Committee meeting held on Aug. 31, 2006. Drug Name Active Ingredient Formulary Status Generic Available Akne-Mycin erythromycin Nonformulary No Ala-Scalp lotion 2% hydrocortisone Nonformulary No Ancobon flucytosine Nonformulary No Apidra insulin glulisine Nonformulary No Benzaclin gel benzoyl peroxide/clindamycin Nonformulary No Capex shampoo fluocinolone acetonide Nonformulary No Cloderm clocortolone pivalate Nonformulary No Colazal balsalazide Formulary No Dermatop prednicarbate Nonformulary No Diprolene lotion augmented betamethasone dipropionate Nonformulary No Elidel 1% cream pimecrolimus Formulary No Entocort EC budesonide Formulary No Exubera insulin Nonformulary No Finacea gel 15% azelaic acid Nonformulary No Grifulvin V griseofulvin microsize Nonformulary No Gris-PEG griseofulvin ultra microsize Nonformulary No Infergen interferon alfacon-1 Self-Injectable Benefit* No Locoid lipocream hydrocortisone butyrate Nonformulary No Loprox gel ciclopirox Formulary No Oxistat cream oxiconazole Nonformulary No Oxistat lotion oxiconazole Nonformulary No Pandel hydrocortisone probutate Nonformulary No Pegasys peginterferon alfa-2a Self-Injectable Benefit* No Peg-Intron peginterferon alfa-2b Self-Injectable Benefit* No * Self-Injectable Benefit: Members should refer to our Member Handbook for benefit details regarding applicable copayments or coinsurance. Provider e-News Vol 2 2006 11 Rx Updates Drug Name Active Ingredient Formulary Status Generic Available Protopic 0.03% & 0.1% ointment tacrolimus Formulary No Rebetol solution ribavirin Nonformulary Yes Relenza zanamivir Nonformulary No Roferon-A interferon alfa-2a Self-Injectable Benefit* No Sporanox oral solution itraconazole Nonformulary No Tamiflu oseltamivir Nonformulary No Tazorac cream 0.05%, 0.1%; gel 0.05%, 0.1% tazarotene Nonformulary No Vfend voriconazole Nonformulary No Zocor simvastatin Nonformulary Yes * Self-Injectable Benefit: Members should refer to our Member Handbook for benefit details regarding applicable copayments or coinsurance. Third Quarter Supplement 2006 The following table lists the outcomes from the third quarter 2006 Supplemental WellPoint Pharmacy and Therapeutics Committee meeting held on Sept. 6, 2006. Drug Name Active Ingredient Formulary Status Generic Available Cleocin 75 mg clindamycin HCl Nonformulary No Cleocin Pediatric clindamycin palmitate Nonformulary No Miacalcin Injectable salmon-calcitonin Self-Injectable Benefit* No Neumega oprelvekin Self-Injectable Benefit* No Pulmozyme dornase alfa Nonformulary No Sumycin tetracycline oral suspension and tablets Nonformulary No Suprax cefixime oral suspension Nonformulary No Zyvox linezolid Nonformulary No Zavesca miglustat Formulary No * Self-Injectable Benefit: Members should refer to our Member Handbook for benefit details regarding applicable copayments or coinsurance. Provider e-News Vol 2 2006 12 Rx Updates Fourth Quarter 2006 The following table lists the outcomes of the fourth quarter 2006 WellPoint Pharmacy and Therapeutics Committee meeting held on Nov. 2, 2006. Drug Name Active Ingredient Formulary Status Generic Available Acular PF ketorolac tromethamine Nonformulary No Androgel testosterone gel 1% Formulary No Anadrol-50 oxymetholone Nonformulary No Avodart dutasteride Nonformulary No Cyclomydril cyclopentolate/phenylephrine Nonformulary No Emend aprepitant Nonformulary No Estrostep FE norethindrone 1 mg/esthinyl estradiol 20 mcg, 30 mcg, or 35 mcg Nonformulary No Flarex fluorometholone Nonformulary No Forteo teriparatide Self-Injectable Benefit* No Inspra eplerenone Nonformulary No Isopto Carbachol carbachol Nonformulary No Isopto Hyoscine scopolamine Nonformulary No Kytril Solution granisetron Formulary No Oxandrin oxandrolone Nonformulary No NuvaRing etonogestrel 0.12 mg/ethinyl estradiol 0.015 mg Nonformulary No Patanol olopatadine Nonformulary No Phospholine Iodide phospholine iodide Nonformulary No Pilopine HS Nonformulary No Nonformulary No Razadyne/ER pilocarpine HCL micronized progesterone vaginal gel galantamine Nonformulary No Sensipar cinacalcet Nonformulary No Seasonique levonorgestrel 0.15 mg/estradiol 0.03 mg/ethinyl estradiol 0.01 mg Nonformulary No Testim testosterone gel 1% Formulary No Tracleer bosentan Nonformulary No Prochieve * Self-Injectable Benefit: Members should refer to our Member Handbook for benefit details regarding applicable copayments or coinsurance. Provider e-News Vol 2 2006 13 Consider Generics Rx Updates An affordable alternative With today’s rising health care costs, substituting generic products approved by the Food and Drug Administration (FDA) helps reduce medication costs. Generic drugs provide a safe, effective, and less expensive alternative for patients, when medically appropriate. With an FDA-approved generic drug, the strength, dosage form, route of administration, and intended usage are identical to the brand-name counterpart. Both brand-name and generic drugs must complete a rigorous approval process successfully. Patients and providers should expect that the generic product will produce the same clinical effect and safety profile as the brand-name drug. For a copy of the Blue Cross formulary, please go to our website at www.bluecrossca.com and select Pharmacy, or contact WellPoint NextRx at (800) 227-3032. What You Need to Know About Prior Authorization of Benefits (PAB) How it works The PAB process for Blue Cross prescription drug benefits alerts prescribers about safe and less costly alternatives on the formulary, as well as prescribed drugs that may not be clinically recommended for the condition for which they are prescribed. Keep in mind that certain medications on the formulary and all nonformulary medications require written PABs. Here are clarifications about our PAB requirements: • Blue Cross covers medications that are medically necessary. We defer to the prescribing physician’s decision so long as the physician supplies medical evidence that the drug is appropriate for a patient’s condition. • We cover medication that requires PAB and is prescribed for off-label use in the treatment of an illness if there is supporting medical evidence. Supporting medical evidence validates a drug when it has been recognized for treatment of that condition by one of the following: • The American Medical Association drug evaluations • The American Hospital Formulary Service drug information • The United States Pharmacopoeia Dispensing Information, Volume 1, “Drug Information for the Health Care Professional” • Two articles from major peer-reviewed medical journals that present data supporting the proposed off-label use or uses as generally safe and effective unless clear and convincing contradictory evidence is presented in a major peer-reviewed journal If we receive a request without the information necessary to make a decision, we will ask the prescribing physician to provide us with additional medical information in order to proceed with the review. Provider e-News Vol 2 2006 14 PAB Results Review and Notification Rx Updates Standards for turnaround time We review and make determinations on nonurgent PAB requests within 24 hours. In emergency cases or life-threatening situations, the pharmacy may proceed with dispensing a 72-hour supply of a medication by calling WellPoint NextRx. We notify prescribing physicians within one working day of the determination. If the determination results in a denial, we will notify both the member and the physician in writing within two working days and give them information on the Blue Cross grievance and appeals process. We will send a letter to the prescribing physician explaining the medical reasons for the denial, along with the name of the Blue Cross physician who issued the denial. We monitor the PAB process regularly to ensure timely outcomes. To Reach the PAB Center When you need help with PAB, call the WellPoint NextRx PAB Center at (866) 302-7166. We can help you: • Submit a PAB request • Obtain the status of a PAB request • Get a PAB Request Form Please fax completed PAB Request Forms to (866) 302-7167. Nonformulary Medications Access Medi-Cal PAB Healthy Families Program DUR The Blue Cross Medi-Cal program has implemented a PAB program for nonformulary medications. The “dispense as written” (DAW-1) or “do not substitute” (DNS) override has been replaced with this PAB program for all nonformulary medications. The Drug Utilization Review (DUR) exception process provides access to most nonformulary medications, therapeutic interchanges, and step therapy procedures. It is still available for our Healthy Families Program. Consequently, when the prescribing physician denotes “do not substitute” or “dispense as written” on the prescription for a Healthy Families Program member, the pharmacist transmits the claim using the appropriate DUR code to allow claim adjudication. Quantity and Dosing 30-Day Quantity Supply Limits Dose Optimization Program The pharmacy benefit program allows up to a 30-day supply of most medications with the new exception of select maintenance medications on the 90-day supply list. This program defines a quantity limit based on FDA dosing recommendations. If a medical condition warrants a greater supply than what has been recommended, then PAB is required in order to ensure access to a medically appropriate quantity. Medications in this program require an internal review by Blue Cross prior to dispensing. The Dose Optimization Program helps increase patient adherence to drug therapies. This program works with the member, the member’s physician or health care provider, and the pharmacist to replace multiple doses of lower-strength medications where clinically appropriate with a single dose of a higher-strength medication (only with the prescribing physician’s approval). If you have questions, please contact WellPoint NextRx at (800) 227-3032. Provider e-News Vol 2 2006 15