VIEW PDF - Practical Dermatology
advertisement

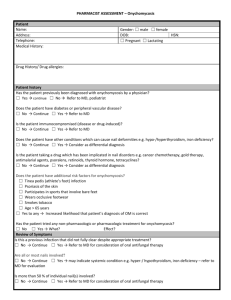
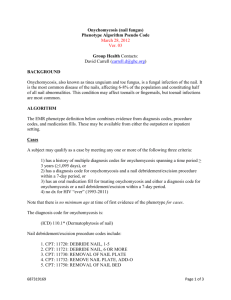
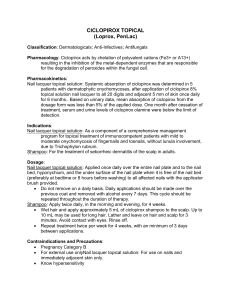
cover focus Update on Management of Dermatophytoses Reviewing principles of diagnosis and management and understanding the latest therapeutic developments can lead to improved outcomes. By Joseph Bikowski, MD, FAAD T inea corporis and tinea pedis are reportedly the most common dermatophytoses in the US and are each estimated to affect approximately 20 percent of the population, however true incidence may be understimated.1 Some dermatophyte infections are more common in certain populations. For example, tinea pedis, tinea cruris or “jock itch,” and tinea corporis are more common complaints among athletes than is onychomycosis. In contrast, onychomycosis affects an estimated 12 percent of the US population; Incidence increases with age and is highest among those over age 65.2 Both tinea pedis and onychomycosis are more common in those with diabetes.3 Diagnosis of tineas tends to be straightforward for specialists, and the diagnosis can be confirmed with KOH preparation. Note that contact dermatitis of the feet or hands may mimic tinea pedis or manuum, respectively, and must be considered in the final diagnosis. Of note, a dermatitis that develops on both hands and both feet is more likely to have a systemic cause rather than to be a contact dermatitis.4 Conversely, involvement of two feet and one hand suggests a primary fungal infection of the foot that has been transferred to one hand only.5 It is unknown why the other hand is not involved. Other similar presentations include one foot/two hands, and even one foot/one hand. Diagnostic Pearl: If the webspace between the fourth and fifth toe is spared, consider a diagnosis other than tinea. Interdigital type tinea pedis is one of three primary presentations of tinea pedis. The others are vesiculobullous type tinea pedis and plantar moccasin type. Superficial cutaneous yeast infections may be predominantly caused by Candida. Among immunocompetent individuals, candidiasis may be especially common in the inframammary folds or genital crease region (more so for women than men). Culture can be used to distinguish Candidiasis from dermatophytosis. Topical antimycotics are standard treatment for candidiasis, particularly clotrimazole or ketoconazole. Oral fluconazole is the primary systemic agent with anti-Candida activity. February 2014 PRACTICAL DERMATOLOGY 23 cover focus Topical AntiFUNGALS Drug Brand Name(s) Example Vehicle Butenafine 1% Mentax, Sinphar Cream Econazole nitrate 1% Cream, lotion Luliconazole 1% Luzu, Valeant Cream Ketoconazole 2% Xolegel, Aqua Pharmaceuticals Cream, gel Naftifine 1% Naftitine 2% Naftin, Merz Cream (Tube and 1% Pump), Gel (Tube) Oxiconazole nitrate 1% Oxistat, PharmaDerm Cream, lotion Sertaconazole nitrate 2% Ertaczo, Ortho Dermatologics Cream Sulconazole nitrate Exelderm, Ranbaxy Laboratories Cream, solution Diagnostic Pearl: Tinea Cruris is rarely if ever seen in women. Most tineas can be managed with topical antifungals (Table 1). Treatment must be selected that is expected to address the causative organism and in a vehicle formulation that the patient can easily apply to the treatment site. A broad-spectrum antifungal is preferred.6 Oral antifungals typically are reserved for extensive or chronic involvement or when application of a topical agent is physically challenging for the patient.7 New to the market is a novel azole called luliconazole, available in a 1% cream (Luzu, Valeant) for the management of interdigital tinea pedis or tinea corporis. The key feature of this formulation is its dosing schedule. For the treatment of tinea pedis, luliconazole cream is applied once-daily for two weeks. For the treatment of tinea cruris, it is applied once-daily for one week. Also new to the market are new 2% cream and gel formulations of naftifine (Naftin, Merz) for the treatment of interdigital tinea pedis, tinea cruris, or tinea corporis. It is indicated for once-daily application for two weeks in all three indications. Prophylactic topical antifungal therapy applied at intervals may be indicated for those at high risk for or with a history of recurrence of dermatophytosis, although this is an off-label use. Treatment of tineas is important for reasons beyond symptom control. Tinea pedis or manuum may provide a reservoir of dermatophytes leading to onychomycosis, though in some cases nail involvement is a primary presentation. Update on Onychomycosis In contrast to tineas of the skin, most cases of onychomycosis require oral therapy. Development of topical therapies for 24 PRACTICAL DERMATOLOGY February 2014 onychomycosis has proven challenging, due to the difficulty of penetrating the nail plate to deliver drugs to the nail bed, the site of infection. The lengthy period the nail takes to grow, the hardness of the nail plate, and location of the infection between the nail bed and plate are major contributing factors. Poor nail penetration is the main factor limiting the use of topical antifungal agents in the treatment of onychomycosis, and directly relates to the nail plate’s unique properties: its thickness and relatively compact cellular structure.8,9,10 Currently, systemic antifungal therapy with terbinafine or itraconazole is the mainstay of treatment. FDA last year issued a warning about potential risks associated with ketoconazole, including potentially fatal liver injury and risk of drug interactions and adrenal gland problems, and indicated that the agent should not be used as a first-line treatment option for fungal infections. Systemic terbinafine and itraconazole are shown to be effective and generally safe for the management of onychomycosis, but there are potential risks associated with therapy.11 Mycologic cure (i.e., the eradication of the causative organism proven by negative culture) is widely accepted as the main treatment goal, with complete clinical clearing occurring after this stage has been achieved.12 Reported PRACTICAL POINTER Treatment of tineas is important for reasons beyond symptom control. Tinea pedis or manuum may provide a reservoir of dermatophytes leading to onychomycosis, though in some cases nail involvement is a primary presentation. • In contrast to tineas of the skin, most cases of onychomycosis require oral therapy. Development of topical therapies for onychomycosis has proven challenging, due to the difficulty of penetrating the nail plate to deliver drugs to the nail bed, the site of infection. cover focus mycologic cure rates in the phase III studies for oral itraconazole and terbinafine were 54 percent and 70 percent, respectively.13,14 Relapse may occur in up to one fifth of those treated with terbinafine, and one-quarter of those treated with itraconazole. Relapse has been attributed to chronic or recurrent tinea pedis, genetic predisposition, and re-exposure to pathologic organisms.15 Diagnostic Pearl: Onychomycosis of the fingernails in the absence of toenail involvement is virtually non-existent. Common side effects of terbinafine include gastrointestinal upset, headache, and minor rashes. Serious side effects are reported in less than one percent of patients,16 but include serious or even fatal liver toxicity one in 54,000. Thus, systemic therapy is not recommended in patients with chronic or active liver disease, and liver-function testing is advisable. Monitoring liver function at four to six weeks is recommended by several experts.17 The side effects of itraconazole are similar to those of terbinafine but also include congestive heart failure, which represents a contraindication. Relatively new to the market is Onmel (Merz), a new oncedaily 200mg single tablet formulation of itraconazole indicated for the oral treatment of onychomycosis of the toenail caused by Trichophyton rubrum or T. Mentagrophytes in non-immunocompromised patients. The tablets are manufactured with what is described as a “melt extrusion” or Meltrex Technology that enables the single tablet formulation. Ciclopirox 8% nail lacquer is the only topical treatment currently approved by the FDA for the treatment of onychomycosis. Currently under FDA review, efinaconazole 10% solution is the first triazole antifungal specifically developed for the topical treatment of mild to moderate distal subungal onychomycosis. It is believed that low surface tension of the alcohol-based formulation helps efinaconazole to first penetrate through the nail plate, then access the nail bed by wicking into the air gap and spreading over the site of infection.18 In two large pivotal trials involving 1,655 patients, mycologic cure was 56 percent, and significantly greater than vehicle (Figure 1, P<.001). Clinical treatment success (0 percent to ≤10 percent area disease involvement of the affected toenail) was achieved in 43 percent of patients. Given that the majority of patients had ≥40 percent affected area involvement of the great toenail at baseline, this represents a meaningful improvement for the onychomycosis patients in the studies. Mild, transient irritation at the site of application was the most common adverse event in two percent of study patients. 26 PRACTICAL DERMATOLOGY February 2014 Diagnostic Pearl: An off-label topical treatment option for distal subungual onychomycosis is a topically applied, low-viscosity, alcohol-based antifungal solution (sulconazole nitrate 1%, Exelderm, Ranbaxy Laboratories). Therapeutic success requires that the patient deliver the solution directly into the nail bed by placing the toe or fingernail in an upright position then instilling one to two drops subungually between the nail plate and nail bed. The patient should hold the toe or finger in an upright position for 30 seconds, to allow gravity to pull the active agent into the nail bed. Treatment should be applied twice daily. Coexistent tinea pedis or manuum must be managed to minimize the risk of re-infection of the nail. Despite successful elimination of fungus from the nails, patients undertaking treatments for toenail onychomycosis should be advised that successful eradication of fungus from the nail may not necessarily restore a toenail to a normal appearance, as it may have been damaged and dystrophic before the infection occurred. Checking the foot for early signs of re-infection is key so that topical treatment can be instigated at an early stage. Maintenance therapy at proper intervals may also be indicated, though not formally studied. n Dr. Bikowski has served as an advisory board member/consultant to Promius Pharma. Joseph Bikowski, MD, FAAD is Director of Bikowski Skin Care Center in Sewickley, PA. 1. Gupta AK, Tu LQ. Therapies for onychomycosis: a review. Dermatologic Clinics 2006;24:375–379. 2. Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013 Jun;32(2 Suppl 1):S2-4. 3. Papini M, Cicoletti M, Fabrizi V, Landucci P. Skin and nail mycoses in patients with diabetic foot. G Ital Dermatol Venereol. 2013 Dec;148(6):603-8. 4. Nedorost S. Clinical patterns of hand and foot dermatitis: emphasis on rubber and chromate allergens. Dermatol Clin. 2009 Jul;27(3):281-7. 5. Daniel CR 3rd, Gupta AK, Daniel MP, Daniel CM. Two feet-one hand syndrome: a retrospective multicenter survey. Int J Dermatol. 1997 Sep;36(9):658-60. 6. Aly R. Tinea Pedis: Epidemiology, Clinical Manifestations, PAthophysiology, and Therapy. in Cutaneous Infection and Therapy. Aly R, Beutner KR, Maibach H, eds. 1997. Marcel Decker, Inc. New York, NY. 7. Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008 NovDec;166(5-6):353-67. 8. Baran R, Kaoukhov A. Topical antifungal drugs for the treatment of onychomycosis: an overview of current strategies for monotherapy and combination therapy J Eur Acad Dermatol Venereol 2005;19(1): 21–29. 9. Lecha M, Effendy I, Feuilhade de Chauvin M, et al. Treatment options—development of consensus guidelines. J Eur Acad Dermatol Venereol 2005;19 suppl 1:25–33. 10. Murdan S. Drug delivery to the nail following topical application. Int J Pharm 2002;236:1-26. 11. Gupta AK, Paquet M, Simpson FC. Therapies for the treatment of onychomycosis. Clin Dermatol. 2013 Sep-Oct;31(5):544-54. 12. Gupta AK. Treatment of dermatophyte toenail onychomycosis in the United States: a pharmacoeconomic analysis. J Am Podiatr Med Assoc 2002;92:272-286. 13. Sporanox (itraconazole) [package insert]. Janssen Pharmaceuticals Inc, Titusville, NJ; 2012. 14. Lamisil (terbinafine HCl) [package insert]. Novartis Pharmaceuticals Corporation, East Hanover, NJ; 2012 15. Tosti A, Piraccini BM, Stinchi C, et al. Relapses of onychomycosis after successful treatment with systemic antifungals: a 3-year follow-up. Dermatology 1998;197:162–166. 16. O’Sullivan DP, Needham CA, Bangs A, et al. Postmarketing surveillance of oral terbinafine in the UK: report of a large cohort study. Br J Clin Pharmacol 1996;42:559-65. 17. Chambers WM, Millar A, Jain S, et al. Terbinafine-induced hepatic dysfunction. Eur J Gastroenterol Hepatol 2001;13:1115-8. 18. Data on file. Valeant Pharmaceuticals.