Ongoing Assessment Nursing Diagnosis
advertisement

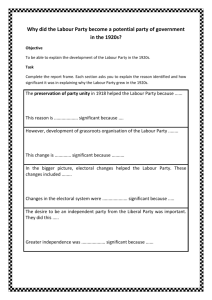
Registered Nurse Initiated Activities Decision Support Tool No. 5: Discomfort and Pain in Labour Decision support tools are evidenced-based documents used to guide the assessment, diagnosis and treatment of client-specific clinical problems. When practice support tools are used to direct practice, they are used in conjunction with clinical judgment, available evidence, and following discussion with colleagues. Nurses also consider client needs and preferences when using decision support tools to make clinical decisions. The Nurses (Registered) and Nurse Practitioners Regulation: Regulation: (6)(1)(h.1) authorizes registered nurses to “manage labour in an institutional setting if the primary maternal care provider is absent.” Indications: For the assessment and management of discomfort and pain in labour For RNs to supervise the self-administration of Nitrous Oxide in labouring women (see DST No. 5A) Related Resources, Policies, and Standards: BCPHP (2007) Obstetric Guideline 4 – Pain Management Options During Labour Neonatal Resuscitation Program Adult CPR Ongoing Assessment • Review initial assessment of discomfort and pain in labour (See Assessment of normal labour and • • • • • • birth in Core Competency Document) Woman’s strategies and confidence in managing pain Presence and support of support person Observation of a woman’s normal response to labour Pain is normal in labour and may be expressed in many ways: ■ Physical cues – intense contraction pain, backache, nausea, vomiting, flushing, perspiration, increases in pulse, respiratory rate, and blood pressure, numbness in extremities ■ Behavioural cues (body language) - e.g. anxiety, panicked activity, guarding, facial expression, eye contact, rubbing a particular area of her body, crying, tremulous voice, thrashing in bed, ability to respond to supportive measures, ability to follow directions, responses to touch, maintaining sense of control ■ Verbal cues- response to questions, expression of needs, interactions with support person(s)/ nurse, making statements about characteristics of the pain and discomfort Assess the woman’s perception of pain intensity using a scale of 1 to 10, 1 being the least and 10 being the most pain Woman’s ongoing response to supportive activities, comfort measures and to changes in environment (e.g. lighting, voice,) (Baker, Ferguson, Roach, & Dawson, 2001; Mattson, 2004) Nursing Diagnosis • Woman’s response to pain indicates need for comfort measures Perinatal Services BC Copyright © 2011 - PSBC Managing Labour Decision Support Tool No. 5: Discomfort and Pain in Labour 48 Special Considerations and Precautions • Impact of provider information/bias about labour interventions • “Women who receive continuous labour support are less likely to experience analgesia or anesthe• • • • • sia (including epidurals and opioids), instrumental delivery; caesarean birth and are less likely to report dissatisfaction or a negative rating of their birth experience” (Simkin & Bolding, 2004) The effectiveness of comfort measures and relaxation techniques varies among women (Simkin, 1995; BCPHP, 2007) The severity and tolerance of pain is unique to each woman and cannot be predicted prior to its occurrence (SOGC, 2007) The nonpharmacologic approach to pain includes a wide variety of techniques to address not only the physical sensations of pain but also to prevent suffering by enhancing the emotional and spiritual components of care (Simkin & Bolding, 2004) When pharmacologic agents are used, guidelines that include method of action, average and maximum dose, possible maternal and fetal side effects, precautions, and resuscitation measures should be available for all staff (SOGC, MOREOB, 2007) Meperidine (Demerol®) is not recommended for use as obstetrical analgesia – only used in the case of morphine allergy Interventions • Engage the woman and her support persons in providing non-pharmacologic comfort measures • • • • (see Appendix 1) Ask the woman if she has a Birth Plan and had access to Baby’s Best Chance (M.O.H., 2010) Determine the need for and instruct the woman on Nitrous Oxide use if applicable (see DST #5A) Consult and refer to PCP if woman requests pharmacological pain relief options besides Nitrous Oxide Provide woman-centred care – reassure, guide, encourage, and accept woman’s style and choices of comfort measures for managing labour Intended Clinical Outcomes • The woman understands the benefits and risks of non pharmacological and pharmacological pain relief options offered/chosen • The woman’s pain is manageable and appropriate comfort measures are provided • The woman experience no or minimal adverse effects from the use of non-pharmacologic and/or pharmacologic comfort measures Education • Provide information on the benefits, risks and limitations of each nonpharmacological or pharmacological comfort measure chosen by the woman Documentation Document as appropriate on Labour Partogram (PSBC 1583), Labour and Birth Summary Record (PSBC 1588), Anesthesia Record, Fluid Balance Sheet, Interprofessional Notes: • Woman’s description of level of pain • Woman’s response to pain including request for comfort measure(s) • Time of assessment prior to providing comfort measures • Type of comfort measures provided • Maternal BP, pulse, temperature, respirations and emotional status Perinatal Services BC Copyright © 2011 - PSBC Managing Labour Decision Support Tool No. 5: Discomfort and Pain in Labour 49 • Maternal responses to comfort measure(s) • Fetal response to comfort measure(s) • Communication to PCP for orders for pharmacological comfort measures and to inform of variances in maternal and fetal responses to labour ■ Time of call to PCP ■ Time of PCP response/orders ■ Orders/response received References Baker, A., Ferguson, S.A., Roach, G.D., & Dawson, D. (2001). Perceptions of labour pain by mothers and their attending midwives. J Adv Nurs, 35(2), 171-179. British Columbia Perinatal Health Program. (BCPHP). (2007). Obstetric Guideline 4. Pain Management Options during Labour. BCPHP. British Columbia Women’s Hospital (BCW). (2005). CE0100-Epidural Analgesia. Fetal Maternal Newborn and Family Health Policy & Procedure Manual. Children’s & Women’s Health Centre of British Columbia. British Columbia Women’s Hospital (BCW). (2006). CMO700 Appendix A, Fentanyl:Intravenous Protocol for Labour. Fetal Maternal Newborn and Family Health Policy & Procedure Manual. Children’s & Women’s Health Centre of British Columbia. British Columbia Women’s Hospital (BCW). (2006). CMO700 Appendix B, Morphine: Protocol for Labour- Intravenous and Intramuscular. Fetal Maternal Newborn and Family Health Policy & Procedure Manual. Children’s & Women’s Health Centre of British Columbia. Geissbuehler, V.; Eberhard, J.; Lebrecht, A. (2002). Waterbirth: water temperature and bathing time-mother knows best. Journal of Perinatal Medicine, 30, 371-378. Mattson, S.a.S., J.E. eds. (2004). Core Curriculum for Maternal-Newborn Nursing. St. Louis, MO: Elsevier Saunders. Ministry of Health. (2010). Baby’s Best Chance. (6th ed). Victoria, BC: Open School BC. www.publications.gov.bc.ca Ministry of Health, EMA Licensing. (2007). Pain Management with the use of Entonox. Remote Nursing Certified practice. Adult Decision Support Tools. Ministry of Health. Gilbert, S. (2007). High Risk Pregnancy & Delivery. (4th ed.) St. Louis, MO: Mosby. Health Canada. (2000). Family-Centred Maternity and Newborn Care: National Guidelines, Minister of Public Works and Government Services, Ottawa. http://www.phac-aspc.gc.ca/dca-dea/publications/fcmc05_e.html Lowdermilk, D.L., Perry, S.E., Cashion, K., & Alden, K.R. (2012). Maternity & women’s health care. (10th ed.). St. Louis, MO: Mosby Elsevier. National Collaborating Centre for Women’s and Children’s Health. (2007). Intrapartum care: Care of healthy women and their babies during childbirth. Royal College of Obstetricians and Gynaecologists (RCOG) Press. London. England. http://www.nice.org.uk/nicemedia/pdf/IntrapartumCareSeptember2007mainguideline.pdf Simkin, P. (Reducing Pain and Enhancing Progress in Labor: A Guide to Nonpharmacologic Methods for Maternity Caregivers. BIRTH 22(3) 161-170. Simkin, P; Bolding, A. (2004). Update on Nonpharmacologic Approaches to Relieve Labor Pain and Prevent Suffering. Journal of Midwifery & Women’s Health. 49(6) 489-504. Society of Gynecologists and Obstetricians (SOGC). (2010). Advances in Labour and Risk Management (ALARM) Course Syllabus. Postpartum Hemorrhage. SOGC. Ottawa, Ontario. SOGC. (2010). MOREOB. Management of Labour. Salus Global Corporation. Mattson, S.a.S., J.E. eds. (2004). Core Curriculum for Maternal-Newborn Nursing. St. Louis, MO: Elsevier Saunders. SOGC. (2007). Fetal health surveillance: antepartum and intrapartum consensus guideline. J Obstet Gynaecol Can, 29(9 Suppl 4), S3-56. Perinatal Services BC Copyright © 2011 - PSBC Managing Labour Decision Support Tool No. 5: Discomfort and Pain in Labour 50 Appendix 1 Non-Pharmacological Comfort Measures Measures Communication Interventions Welcome and encourage support person(s) (partner, doula) Encourage woman to verbalize her needs/concerns and be available to answer questions from woman and/or support person(s) Discuss woman’s expectations, worries and concerns Ensure aspects of birth plan are observed – review with nursing colleagues, PCP and other medical staff as needed Explain to the woman and support person(s) the use of the chosen comfort measure (provide education/information pamphlet if available) Labour Support Stay in the room with the woman to provide 1:1 nursing care Continuous supportive presence of a trained person (e.g. doula) Attend to physical & emotional needs Breathing Various types of focused breathing techniques assist with relaxation and focusing First Stage – Slow and light breathing Second Stage – Encourage spontaneous pushing efforts, panting to assist with delivery of head Positioning Staying upright, relaxed and moving and changing positions as often as possibleWalking Standing-rocking or swaying, leaning forward and resting on something Squatting or support squat Sitting – Leaning against partner, on toilet Kneeling – Doing pelvic tilt, using chair/bed for hand support Hands and knees – Good for back pain and rotating to anterior position Semi-reclining or side-lying – Comfortable for birth Pelvic Rocking USE of: Birthing ball Birthing stool Birthing rope/sheet pull Squatting bar – 2nd stage Encourage non supine position in 2nd stage for pushing Massage Firm sacral counter pressure – Steady firm pressure applied with heel of hand at the sacral iliac joint, rolled towel or tennis ball-helps relieve back pain Effleurage – Light stroking of the abdomen in rhythm with breathing Massage – Smooth, rhythmic stroking or rubbing of shoulder, back, foot , face, hand Application of heat – Warm blankets, compresses, heated rice bags Application of cold – Cool cloths, ice packs to chest face, back or area of pain Perinatal Services BC Copyright © 2011 - PSBC Managing Labour Decision Support Tool No. 5: Discomfort and Pain in Labour Measures Hydrotherapy 51 Interventions Deep water immersion in tub Woman can maintain water temperature and bathing time (Geissbuehler, Eberhard, Lebrecht, 2002) Assess maternal temperature q 1h, to prevent hyperthermia. If maternal temperature exceeds 37.5°C, decrease water temperature or have the woman leave the tub for short periods and re-evaluate. There are no known contraindications to using the tub in the presence of ruptured membranes (BCPHP, 2007) Standing or sitting in the shower – Directing water to specific areas for comfort Spray bottles Ensure adequate oral intake Psychoprophylaxis & Complementary Therapies Examples include: Acupressure – Best applied over skin without lubricants-points, neck, shoulders, wrists, lower back, hips, below kneecaps, ankles, nails on small toes, soles of feet Focal Point Concentration – Focusing on something other than pain Visualization – Picturing safe and a special thing, place that assists in relaxation Biofeedback – Needs prior education; uses thinking and mental processes (focusing) on how to relax; use of verbal and touch feedback Music – Chant, song or prayer Patterned breathing Environmental Ensure the room is comfortable Provide privacy Allow space for freedom of movement Provide safety for the woman to be free to be herself Ask the woman’s preference for: Lighting, noise level Perinatal Services BC Copyright © 2011 - PSBC