(GENDER MANAGEMENT SERVICE), A NEW CLINIC FOR DSD
advertisement
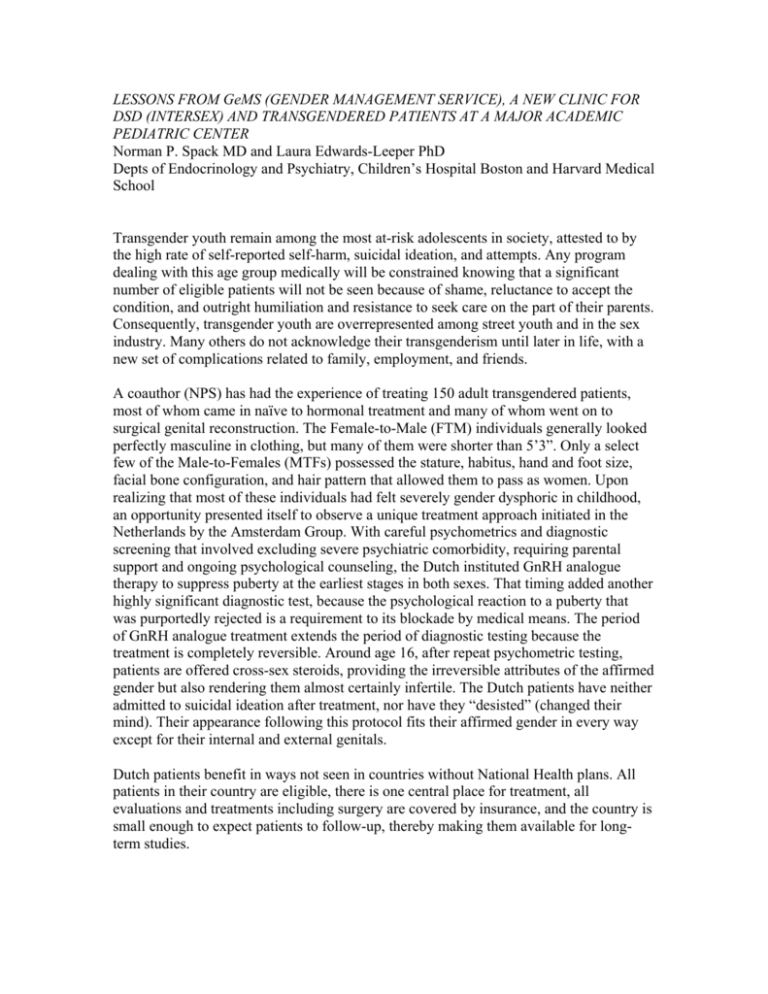
LESSONS FROM GeMS (GENDER MANAGEMENT SERVICE), A NEW CLINIC FOR DSD (INTERSEX) AND TRANSGENDERED PATIENTS AT A MAJOR ACADEMIC PEDIATRIC CENTER Norman P. Spack MD and Laura Edwards-Leeper PhD Depts of Endocrinology and Psychiatry, Children’s Hospital Boston and Harvard Medical School Transgender youth remain among the most at-risk adolescents in society, attested to by the high rate of self-reported self-harm, suicidal ideation, and attempts. Any program dealing with this age group medically will be constrained knowing that a significant number of eligible patients will not be seen because of shame, reluctance to accept the condition, and outright humiliation and resistance to seek care on the part of their parents. Consequently, transgender youth are overrepresented among street youth and in the sex industry. Many others do not acknowledge their transgenderism until later in life, with a new set of complications related to family, employment, and friends. A coauthor (NPS) has had the experience of treating 150 adult transgendered patients, most of whom came in naïve to hormonal treatment and many of whom went on to surgical genital reconstruction. The Female-to-Male (FTM) individuals generally looked perfectly masculine in clothing, but many of them were shorter than 5’3”. Only a select few of the Male-to-Females (MTFs) possessed the stature, habitus, hand and foot size, facial bone configuration, and hair pattern that allowed them to pass as women. Upon realizing that most of these individuals had felt severely gender dysphoric in childhood, an opportunity presented itself to observe a unique treatment approach initiated in the Netherlands by the Amsterdam Group. With careful psychometrics and diagnostic screening that involved excluding severe psychiatric comorbidity, requiring parental support and ongoing psychological counseling, the Dutch instituted GnRH analogue therapy to suppress puberty at the earliest stages in both sexes. That timing added another highly significant diagnostic test, because the psychological reaction to a puberty that was purportedly rejected is a requirement to its blockade by medical means. The period of GnRH analogue treatment extends the period of diagnostic testing because the treatment is completely reversible. Around age 16, after repeat psychometric testing, patients are offered cross-sex steroids, providing the irreversible attributes of the affirmed gender but also rendering them almost certainly infertile. The Dutch patients have neither admitted to suicidal ideation after treatment, nor have they “desisted” (changed their mind). Their appearance following this protocol fits their affirmed gender in every way except for their internal and external genitals. Dutch patients benefit in ways not seen in countries without National Health plans. All patients in their country are eligible, there is one central place for treatment, all evaluations and treatments including surgery are covered by insurance, and the country is small enough to expect patients to follow-up, thereby making them available for longterm studies. While several other Western European countries are following similar protocols, the United Kingdom, which has only one National Health Service center for evaluation and treatment of children and adolescents with GID, has taken the position not to provide any medical interventions until age 16, by which time most adolescents have completed the pubertal process, rendering them at their genotypic heights, etc. Their long-standing policy is being challenged by an active group of parents of transgendered teens, some of whom have sought treatment outside the UK. These parents are feeling validated by the June ’09 release of the International Task Force appointed by the Endocrine Society to create Guidelines for the Endocrine Treatment of Transsexual Persons. The guidelines recommend pubertal suppression using GnRH analogue in the early stages of puberty in appropriately screened adolescents. The barriers to implementation of these guidelines in the USA are economic, attitudinal, and subjected to the classification of transgenderism as a psychiatric condition in the DSM-IV. The GnRH analogues may cost as little as 200 dollars per month in Western Europe, being able for purchase in bulk, and having more effective bargaining power with pharmaceutical companies. The same medications may cost 1,000 to 1,500 dollars per month if purchased in the USA, and the diagnosis “Gender Identity Disorder” provides insurance coverage only for psychiatric counseling and psychological testing, not for medical or surgical treatments. Thus, many patients go untreated for lack of ability to afford it. Secondly, although pediatric endocrinologists are familiar with both pubertal blockade, as is provided for patients with precocious puberty, and with hormonal reconstitution, using estrogen and testosterone in hypogonadal patients, many pediatric endocrinologists in North America are extremely uncomfortable treating Gender Identity Disorder for several reasons: unfamiliarity, a history that it has been traditionally regarded as a psychiatric condition, fear of negative publicity similar to that which characterized some cases of gender assignment in complicated Disorders of Sex Development, or plain antipathy towards these patients. Since 2007, we have accumulated 96 children, adolescents, and young adults between the ages of 6 and 21 who, by the best criteria we can apply, including the Dutch psychometric testing, appear to be transgendered. Fifty percent of the patients are postpubertal, and 16 have been started on GnRH analogue in the early phase of puberty. Four are “refugees” from the British clinic, which only offered them counseling. One of our greatest challenges comes when a patient has been labeled with a comorbid psychiatric condition when we have reason to believe that that condition is secondary to his or her gender dysphoria. Another group for whom initiation of treatment is extremely challenging are those patients who are not brought in by both parents, but who have a noncustodial parent, usually in the context of a divorce, who retains joint custody and who strongly opposes any medical intervention before the child reaches the age of legal consent at age 18. The stress on the treatment team in these cases is considerable because in some cases there is relatively little time between the patient’s presentation in our clinic and the expected rapid progression into puberty. In every city, there are transgendered children who are rejected by their parents and often take to the streets. Some of them qualify for treatment in clinics serving street youth as “emancipated minors.” Some are in the custody of state institutions where legal proceedings may be necessary for them to receive hormonal treatment prior to age 18. Complicating the issue, some state insurances will not cover medical treatment for transgenderism. The past year has been a momentous one for the transgender community. Increasingly, the “T” in the GLBT movement has been more than a caboose, but part of the engine. These individuals are gaining a higher level or respect, resulting in more coming forward at younger ages, with colleges increasingly providing services to trans students, and greater acceptance by employers. That an august organization such as the Endocrine Society would take on the management of transgenderism as a topic to disseminate to its world-wide membership is a stunning development. Furthermore, most of the leading Endocrine Societies around the world, including the European Endocrine Society, the European Society for Pediatric Endocrinology, the Lawson-Wilkins Pediatric Society of North America, and the WPATH (World Professional Association for Transgender Health) are all cosigners of the document. What remains? A major debate concerning the retention of Gender Identity Disorder in the next edition of DSM, which is scheduled for publication in 2012. It may not matter to the countries with national health services, but as long as the psychiatric community labels transgenderism in its diagnostic manual, and as long as the United States continues to have hundreds, if not thousands, of individual health insurers striving to reduce their costs, transgendered people in the US should not expect insurance coverage for their condition. Those who recall the societal attitudes towards gays and lesbians in the 1970’s can well remember what a difference occurred when homosexuality was removed from the DSM in 1973. The combination of Endocrine Society mandates and the removal of Gender Identity Disorder from the DSM will likely put transgenderism into the realm of a medical condition, where it belongs. REFERENCES Cohen-Kettenis PT, Owen A, Kaijser VG, Bradley SJ, Zucker KJ 2003 Demographic characteristics, social competence, and behavior problems in children with gender identity disorder, a cross-national, cross-clinic comparative analysis. J Abnorm Child Psychol 31:41-53 Cohen-Kettenis PT, van Goozen SH 1997 Sex reassignemnt of adolescent transsexuals: a follow-up study. J Am Acad Adolesc Psychiatry 36:263-71 Cohen-Kettenis PT, Delmarre-van de Waal HA, Gooren LJ 2008 treatment of adolescent transsexuals: changing insights: J Sex Med 5:1892-7 Delmarre-Van de Waal HA, Cohen-Kettenis PT 2006 Clinical managemet of gender identity disorder in adolesecents: a protocol on psychological and paediatric endocrinology aspects. Eur J Endocrinol 155 Suppl 1:S131-S137 De Sutter P 2007 Reproduction and fertility issues for transpeople. In: Ettner R, Monstrey S, Eyler AE (eds) PRicniples of transgender medicine and surgery. Haworth Press, New York; pp 209-221 Gooren L 1990 The endocrinology of transsexualism: a review and commentary. Psychoneuroendocrinology 15:3-14. Gooren LJ, Giltay EJ, Bunck MC 2008 Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J Clin Endocrinol Metb 93:19-25 Gooren LJ, Giltay EJ 2008 Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of adrogens to females. J Sex Med 5:76776 Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal H, Gooren LJ, Meyer WJ, Spack NP, Tangpricha V, Montori VM 2009 Endocrine Treatment of Transsexual Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab doi:10.1210/jc.2009-0345 Manasco PK, Prescovits OH, Feuillan PP, Hench KD, Barnes KM, Jones J, Hill SC, Loriaux DL, Cutler GB, Jr. 1988 Resumption of puberty after long term luteinizing hormone-releasing hormone agonist treatment of central precocious puberty. J Clin Enocrinol Metab 67:368-72 Meyer 3rd WJ, Bockting W, Cohen-Kettenis P, Coleman E, DiCeglie D, Devor H, Gooren L, Hage JJ, Kirk S, Kuiper B, Laub D, Lawrence A, Menard Y, Monstrey S, Patton J, Schaefer L, Webb A, Wheeler CC 2001 Harry Benjamin Internation Gender Dysphoria Association’s The Standards of Care for Gender Identity Disorders, 6th version. Int J Transgenderism 5(1) Moore E Wisniewski A, Dobs A 2003 Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab 88:3467-73 Tugnet N, Goddard JC, Vickery RM, Khoosal D, Terry TR 2007 Current management of male-to-female gender identity disorder in the UK. Postgrad Med J 83:638-42 Tuvemo T 2006 Treatment of central precocious puberty. Expert Opin Investig Drugs 15:495-505 Wallien MS, Swaab H, Cohen-Kettenis PT 2007 Psychiatric comorbidity among children with gender identity disorder. J Am Acad Child Adolesc Psychiatry 46:1307-14 Wallien MS, Cohen-Kettenis PT 2008 Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry 47:1413-23 Zucker, KJ, Bradley SJ 1995 Gender identity disorder and psychosexual problems in children and adolescents. Guilford Press, New York Zucker, KJ 2004 Gender identity development and issues. Child Adolesc Psychiatr Clin N Am 13:551-68, vii