Aseptic Technique v3:2 - Plymouth Community Healthcare
advertisement

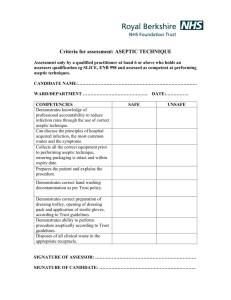
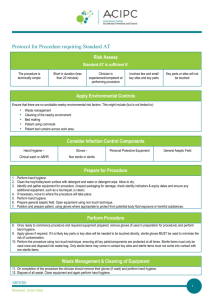
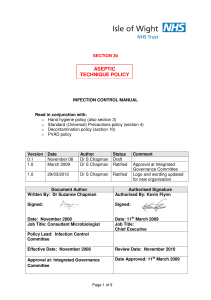
Plymouth Community Healthcare CIC Aseptic Technique Policy Version No 3.2 Notice to staff using a paper copy of this guidance The policies and procedures page of Intranet holds the most recent version of this guidance. Staff must ensure they are using the most recent guidance. Author: Professional Lead Asset Number: 589 Page 1 of 22 Aseptic Technique Policy. V.3.2 Reader Information and Asset Registration Title Information Asset Register Number Rights of Access Type of Formal Paper Category Format Language Subject Document Purpose and Description Aseptic Technique Policy. V.3.2 589 Author Ratification Date and Group Publication Date Review Date and Frequency of Review Disposal Date Professional Lead 15th January 2014. Policy Ratification Group. Public Policy Clinical Microsoft Word 2003 and PDF English Aseptic technique To ensure health care staff understand the principles of asepsis and so reduce the risk of Health Care Associated Infections Job Title of Person Responsible for Review 24/01/2014 2 years after publication, or earlier if there is a change in evidence. The policy ratification group will retain an e signed copy for the database in accordance with the Retention and Disposal Schedule, all previous copies will be destroyed. Clinical Specialist Tissue Viability Nurse/ Nurse Consultant Infection Prevention and Control Target Audience Circulation List All staff Electronic: Plymouth Intranet and PCH website Written: Upon request to the Policy Ratification Secretary on 01752 435104. Consultation Process Please note if this document is needed in other formats or languages please ask the document author to arrange this. Infection Prevention and Control Team Inpatient Registered Nurse Forum District Nurse Forum Continence Advisor Impact Assessment Yes References/Source AfPP Standards and Recommendations for Safe Perioperative Practice. Association for Perioperative Practice, Harrogate 2007 Department of Health (2003), Winning Ways: Working together to reduce Healthcare Associate Infection in Page 2 of 22 Aseptic Technique Policy. V. 3.2 England; Department of Health: London Department of Health, (2005), Saving Lives: a delivery programme to reduce Healthcare associated infection including MRSA; Department of Health: London Hart. S, (2007) Using an aseptic technique to reduce the risk of infection. Nursing Standard 21.47 p43-48 Pratt RJ, Pellowe CM, Loveday HP, Robinson N, Smith GW et al (2001). The EPIC project: developing national evidence-based guidelines for preventing healthcare associated infections. Phase 1 guidelines for preventing hospital-acquired infections. Journal of Hospital Infection, 47:S3-S82 Preston RM, (2006) Aseptic Technique: Evidenced-based approach for patient safety. British Journal of Nursing 14(10), pp.540-546 Wilson, J (2006), Infection Control in Clinical Practice, 3rd Edition, Baillière Tindall: London World Health Organisation (2009) Guidelines on hand care, Geneva, Switzerland: World Health Organisation Associated Documentation The Hygiene Code Supersedes Document Author Contact Details V.3 Publisher (for externally produced information): 1. Hand Hygiene Guidelines. 2. Safe Disposal of Sharps Guidelines. 3. Guidelines on the Management of Urinary Catheters. 4. Guidelines for the Management of Peripheral Intravenous Devices. 5. Guidelines for the Management of Central Venous Catheters. By post: Local Care Centre Mount Gould Hospital 200 Mount Gould Road Plymouth Devon PL4 7PY Tel: Fax: 0845 155 8085 01752 272522 (LCC Reception) N/A Page 3 of 22 Aseptic Technique Policy. V. 3.2 Document Version Control Version Number Type of change e.g. Updated or full review 1 Date Author of Change Feb. 2007 Description of Changes and reason for change New policy. 2 Updated Feb 2009 2.1 Updated Sept 2011 Nurse Consultant Infection Prevention & Control. 3 Ratified Sept 2011 Policy Ratification Group 3.1 Extended PRG Secretary Extended no changes. 3.2 Formal review November 2013 December 2013 Professional Lead Page 4 of 22 Aseptic Technique Policy. V. 3.2 Contents of Aseptic Technique Policy. V.3.2 Page 1 Introduction 6 2 Purpose 6 3 Duties 6 4 Principles of Aseptic Technique 7 5 Aseptic Non-Touch Technique 7 6 Indications for Aseptic Technique 8 7 Principles of asepsis 8 8 Aseptic Technique Guidelines 8 9 Hand Decontamination 9 10 Procedure 9 11 Post-Procedure 10 12 Documentation 10 13 Competence 10 Appendix A Appendix B Appendix C Appendix D Aseptic Technique procedure and competencies Ten-stage Hand Decontamination Technique Aseptic Technique Guidelines 18 20 Application of Sterile Gloves 22 Page 5 of 22 Aseptic Technique Policy. V. 3.2 12 Aseptic Technique Policy 1. Introduction 1.1. Aseptic non-touch technique prevents the introduction of micro-organisms that could cause infection to susceptible sites and hence is important in reducing the risk of Healthcare Associated Infection. 1.2. Clinical procedures involving aseptic technique should only be performed by staff who have been assessed to be competent in the technique. 1.3. The guidelines outlined in this document should be followed when performing clinical procedures that require aseptic technique. 2. Purpose These guidelines aim to: 2.1. Ensure clinical procedures are performed in an appropriate manner to maintain asepsis 2.2. Minimise the risk of acquisition of Healthcare Associated Infection (HCAI) during clinical procedures. 3. Duties 3.1 The Chief Executive is ultimately responsible for infection prevention and control and the content of all Policies and their implementation. The Chief Executive delegates the day to day responsibility of implementation of the policies to the Deputy Director of Professional Practice and the Infection Prevention and Control team (IPCT). 3.2 Directors are responsible for identifying, producing and implementing policies in relevant to their area. 3.3 The Locality Managers and Deputy Locality Managers will support and enable operational Clinical Leads and Managers to fulfil their responsibilities and ensure the effective implementation of this Policy within their speciality. 3.4 Ward Managers/Team Leaders are responsible for ensuring that good Practice is embedded into their clinical areas. 3.5 All staff, both clinical and non clinical have a responsibility for ensuring they have read, understood and adhere to local Protocols and Policies. Guidance and competencies will be included within clinical training sessions. Page 6 of 22 Aseptic Technique Policy. V. 3.2 3.6 Clinical procedures involving aseptic technique should only be performed by staff who have been assessed as competent in the technique. Education, training and assessment in the aseptic technique will be provided to all staff undertaking such procedures. These competencies can be found within specific procedures e.g. urinary catheterisation, pleurx drain. 4. Principles of Aseptic Technique The principles of aseptic technique are as follows: 4.1. Aseptic technique aims to prevent micro-organisms on hands, surfaces or equipment from being introduced to susceptible sites. 4.2. The susceptible site should not come into contact with any item that is not sterile. 4.3. A non-touch technique should be maintained throughout the procedure. 4.4. If there are any breaches during the procedure, the operator must stop the procedure and continue only when asepsis can be resumed. 4.5. Where possible, ‘clean’ procedures should be carried out prior to ‘infective’ or ‘contaminated’ procedures. 4.6. All open wounds should only be exposed for a minimum amount of time. 5. Aseptic Non-Touch Technique 5.1 The Aseptic Non-Touch Technique (ANTT) is a framework to both ‘standardise and raise clinical standards whilst undertaking aseptic clinical procedures’ (Hart 2007). 5.2 It is essential to ensure that hands, even though they have been washed, do not contaminate the sterile equipment or the patient. The aim is for asepsis not sterility. The individual healthcare professionals need to decide between sterile or non sterile field/gloves and simply ask themselves ‘can I do this procedure without touching key-parts?’ If the answer is NO – they use a sterile dressing pack and sterile gloves. If YES – they wear non-sterile gloves. 5.3 The principle is that you cannot infect a key part if it is not touched. Any key part must only come into contact with other key parts (i.e. syringe tip and needle hub);. Page 7 of 22 Aseptic Technique Policy. V. 3.2 ● Always wash hands effectively ● Never contaminate key parts ● Touch non key - parts with confidence ● Take appropriate standard infection control precautions 6. Indications for Aseptic Technique Procedures that require the full use of aseptic technique (as outlined in Section 6) include: 6.1. Any medical invasive procedure that breaches the skin or mucous membranes, including tracheostomy care. 6.2. Dressing of wounds healing by primary intention (e.g. surgical wounds). 6.3. Urinary catheterisation. 6.4. Central venous lines insertion and access/manipulation. 6.5. Intravenous feeding lines insertion and access. 6.6. Suturing. 6.7. Vaginal examination during labour. 6.8. Removal of surgical drains. 7. Principles of asepsis: The principles of asepsis including clean procedures also apply to other procedures including: 7.1. Tracheal suctioning. 7.2. Central venous lines access and manipulation. 7.3. Peripheral intravenous cannulae insertion and access. 7.4. Taking blood cultures. 7.5. Enteral feeding care. 7.6. Urinary catheter care (changing and emptying catheter bags, and obtaining urine samples. 8. Aseptic Technique Guidelines Page 8 of 22 Aseptic Technique Policy. V. 3.2 8.1 Preparation 8.2 Explain and discuss the procedure with the patient and gain their consent. If English is not the patient’s first language, ensure there are suitable arrangements for an interpreter. In the case of children, ensure they and a legal guardian are involved in the consent process. 8.3 Planning is an essential part of the process. Obtain all the equipment needed for the procedure. 8.4 Prepare the patient and environment to allow any organisms to settle before the sterile field is exposed. Ideally, all activities that can disperse micro-organisms into the air, for example bed-making or cleaning, should cease 30 minutes before a dressing is undertaken. Air movement should be kept to a minimum during the procedure. Ideally, aseptic procedures should be undertaken in a designated clean area, for example a clinical room. 9. Hand Decontamination 9.1 Decontaminate hands using the ten-stage hand decontamination technique (Appendix B; please see Hand Hygiene Policy). 9.2 There must be a dedicated dressing trolley available. This should be cleaned with a detergent wipe prior to use. For venepuncture or cannulation, use the sharps tray provided. For community settings, ensure there is a clean and dry surface to put your sterile field on. Refer to the Decontamination guidelines and procedures (cleaning and disinfection) for correct decontamination of equipment. 9.3 Place all equipment required for the procedure on the bottom of the trolley. This is your non-sterile field. Check all equipment is in date and sterile. 9.4 Put on a single-use, disposable plastic apron. Assess the need for other personal protective equipment. 9.5 In Inpatient ward areas take the trolley or tray to the patient, disturbing the screens as little as possible. 10. Procedure 10.1 If carrying out a wound dressing, loosen the outer dressing tape, taking care not to expose wound. 10.2 Decontaminate hands using alcohol hand rub. Page 9 of 22 Aseptic Technique Policy. V. 3.2 10.3 Open the outer cover of the sterile pack and turn out the sterile pack on to the top shelf of the trolley (Appendix C). 10.4 Open the sterile field using only the corners of the paper, taking care not to lean over the sterile field. 10.5 Open any other equipment and drop on to the centre of the sterile field. Ensure that this is performed without touching the equipment itself. 10.6 Place hand in the sterile disposable clinical waste bag and arrange the contents on the sterile field. 10.7 If carrying out a wound dressing, remove loosened dressing with hand covered with the clinical waste bag, invert the bag and secure the bag with the adhesive tape to the side of the trolley, ensuring it falls below the sterile field. 10.8 Where appropriate, swab along the ‘tear line’ of sachets of saline using swab impregnated with 70% isopropyl alcohol or Chlorhexidine in 70% alcohol (or Chloraprep if available).Tear open sachets of saline and pour contents into a sterile gallipot. 10.9 Decontaminate hands using alcohol rub. 10.10Put on sterile gloves (Appendix D). 10.11Carry out procedure as per Trust policy or local protocol ensuring you maintain asepsis and use a non-touch technique throughout application. 11. Post-Procedure 11.1 Ensure correct disposal of sharps (see Safe Disposal of Sharps Policy). 11.2 Place all used disposable items, including the apron and gloves, in an clinical waste bag for incineration. Ensure correct disposal of waste. In the community this is the refuse collection. For infected waste refer to the Safe Handling and Disposal of Healthcare Waste Policy and Procedures v2:4. 11.3 The trolley/sharps tray should be cleaned with a detergent wipe. Spillages of blood or high-risk body fluids should be dealt with according to the Decontamination guidelines and procedures (cleaning and disinfection) 11.4 Decontaminate hands using the ten`-stage hand decontamination technique (Appendix B; please see Hand Hygiene Policy). 12. Documentation Page 10 of 22 Aseptic Technique Policy. V. 3.2 Document fully the procedure in nursing and/or medical notes. 13. Competence Clinical procedures involving aseptic technique should only be performed by staff who have been assessed as competent in the technique using the competency framework. Control T All policies are required to be electronically signed by the Lead Director. Proof of the e-signature is stored in the policies database. The Lead Director approves this document and any attached appendices. For operational policies this will be the Locality Manager. Signed: Director of Operations Date: 15th January 2014 Page 11 of 22 Aseptic Technique Policy. V. 3.2 Appendix A Aseptic Technique procedure and competencies Essential Equipment • • Appropriate hand hygiene preparation as per Plymouth Community Healthcare Policy • Identified clean dry surface • Appropriate sterile dressing pack*, Frontier Medical Supplies • Warm clean tap water or sterile saline for cleaning and/or irrigation or specific specified solution for procedure. • A sterile/clean container to hold solution (if not included in sterile pack) • Appropriate wound management materials and/or dressings • Any other material will be determined by the nature of the dressing • Special features of a dressing should be referred to in the patient’s care plan. • Any extra equipment that may be needed during procedure e.g. sterile scissors. (Patient single use scissors/dedicated patient use scissors) Page 12 of 22 Aseptic Technique Policy. V. 3.2 Final assessment by assessor : Name O Awareness through observation A Performing with assistance S Performing under supervision C Competent, performing independently Date O Action Rationale 1 Explain and discuss the procedure with the patient and obtain verbal consent and document To ensure that the patient understands the procedure and gives his/her valid consent 2 Wash hands using protocol for Plymouth Community Healthcare. Washing hands is the single most important contribution to minimising infection. Hands must be washed before and after every patient contact and cleansed before commencing the preparations for aseptic technique, to minimise risk of introducing potential infection. 3 Identify a clean work surface such as a stool, table or tray. In a clinical setting staff should use a dressing trolley, cleaned with a detergent wipe and dried with a paper towel. To provide a clean working surface. In a home situation, the surface should be rendered as clean as possible and protect the environment from any damage 4 Place all the equipment required for the procedure on the surface or on the bottom of the trolley To establish an identified working field A Page 13 of 22 Aseptic Technique Policy. V. 3.2 S C ACTION Reassure patient and position them comfortably so that the area to be dealt with is easily accessible without exposing the patient unduly. Use screens / curtains as appropriate RATIONALE To ensure access to the patient whilst maintaining the patient’s dignity and comfort. Put on a disposable plastic apron and unsterile gloves To reduce the risk of cross infection and protect uniform or clothing from possible contaminants Loosen the product and/or dressing tape. The patient may prefer to do this themselves. Remove and dispose of gloves and apron and wash hands To reduce traumatic removal of adhesive materials and ensure wound is not exposed for a prolonged time. This reduces the risk of infection and a drop in temperature of the wound, which will delay wound healing (Lock 1980;Naylor et al 2001) 8 Check dressing pack is sterile (undamaged, intact and dry) Open the sterile dressing pack and slide on to the trolley/work surface Gel hands To minimize airborne contamination. 9. So that areas of potential Open the sterile field using contamination are kept to a only the corners of the paper for areas where dressing must minimum be kept and laid out within the confines of their packaging 10 Check any other packs (dressings etc) for sterility, open and tip contents onto the centre of the sterile field 5 6 7 O A To prepare the equipment to reduce the amount of time the wound is kept uncovered once the procedure is in progress Page 14 of 22 Aseptic Technique Policy. V. 3.2 S C ACTION Cleanse hands with alcohol hand rub RATIONALE 12 Place hand in disposable bag, and arrange contents of dressing pack To maintain sterility of pack 13 Remove loosened dressing with hand (still covered with the disposable bag), invert bag and stick to trolley (or appropriate surface) Observe what has come away with the dressing – exudates, blood etc. To minimise risk of contamination by keeping dressing in the bag) and ongoing assessment of the wound bed. 14 Pour lotion into gallipots or other sterile receptacle and wash hands. 15 Put on sterile gloves, touching only the inside wrist To reduce the risk of infection. Gloves provide greater sensitivity than forceps and are less likely to cause trauma to the patient (David 1991) 16 Carry out procedure according to plan of care. Any changes must be reflected in a new plan of care 17 Keep one hand for contact with the trolley and its contents (clean) and one hand for contact with the wound or site of procedure (dirty). Maintain asepsis and reduce risk of contaminating sterile materials on the trolley. 11 O A Page 15 of 22 Aseptic Technique Policy. V. 3.2 S C ACTION RATIONALE This section (18,19,20,21) applies to wound care only O 18 Using ‘clean’ hand, dip gauze into cleaning solution, transfer to ‘dirty hand and clean surrounding skin of wound from top-to-bottom or away from the body (inside-tooutside) with single stroke of each swab. Observe surface of swab. Discard into disposal bag. Repeat as necessary using each swab once only. Not every wound needs to be cleansed at dressing change. Cleansing to the wound bed should be with warmed irrigation To remove debris and cleanse wound surface where necessary. 19 Dry surrounding area with clean gauze top-to-bottom or away from the site. To prevent cross infection and facilitate adherence of wound management dressing. 20 Apply chosen dressing according to Wound Management Protocol Formulary or Plan of Care. Following Manufacturers guidelines and instructions To continue to promote wound healing and prevent complications 21 Secure dressing to provide comfort and security. To prevent dressing becoming detached A For all procedures 22 Inform patient that procedure is complete and leave them comfortably .It allows patients to ask questions and confirms prescribed care plan 23 Dispose of Clinical Waste as per PCH Policy Remove and dispose of Safe disposal of waste prevents cross contamination Page 16 of 22 Aseptic Technique Policy. V. 3.2 S C gloves and apron and wash hands 24 ACTION Dispose of any opened but unused dressings RATIONALE O To avoid inadvertent use of non-sterile dressings at a future date 25 Wash and dry work surface/ trolley To reduce the risk of spreading infection (Ayliffe et al 2000) 26 Document procedure and observations as per PCH Policy Ensure any adhesive labels (e.g. on catheters)are placed in the patient record as evidence Documentation ensures continuity of care, provides communication between patients and disciplines. It ensures safe practice as dictated by Nursing and Midwifery Council regulations. A Statement of competency I certify that I am aware of my professional responsibility for continuing professional development and that I am accountable for my actions. With this in mind I make the following statement: I am competent to undertake an aseptic technique training. Signature of practitioner: Date: Assessors signature: Date: Page 17 of 22 Aseptic Technique Policy. V. 3.2 S C Appendix B Ten-stage Hand Decontamination Technique Effective hand washing technique involves three stages: preparation, washing, rinsing and drying. Preparation requires wetting hands under tepid running water before applying liquid soap or an antimicrobial preparation. The hand wash solution must come into contact with all surfaces of the hand. The hands must be rubbed together vigorously for a minimum of 10-15 seconds paying particular attention to the tips of the fingers, the thumbs and the areas between the fingers. Hands should be rinsed thoroughly prior to drying with good quality paper towels. When decontaminating using alcohol hand rub, hands should be free of dirt and organic material. The hand rub must come into contact with all surfaces of the hand. The hands must be rubbed together vigorously, paying particular attention to the tips of the fingers, the thumbs and the areas between the fingers until the solution has evaporated and dried. 1. Wet hands with water 6. Rub the backs of fingers to opposing palms with fingers interlocked 2. Apply enough soap to cover all hand surfaces 7. Rotational rubbing of left thumb clasped in right palm and vice versa move to rotational rubbing of both wrists 3. Rub hands palm to palm 8. Rotational rubbing, backwards and forwards with tops of fingers of right hand in left palm and vice versa 4. Rub the palm of one hand over the back of the other with interlaced fingers and vice versa 9. Rinse hands with water Page 18 of 22 Aseptic Technique Policy. V. 3.2 5. Rub palm to palm with fingers interlaced 10. Dry thoroughly with a towel Hand Drying Wet surfaces transfer micro-organisms more effectively than dry ones. Consequently, the method of hand drying is also important. Skin Care/Staff Issues Staff are encouraged to apply an emollient hand cream regularly to protect skin from the drying effects of regular hand decontamination. Staff should only use the products available in the clinical areas as these have been specifically designed not to interact with soaps and alcohol hand rub. If a particular soap, antimicrobial hand wash or alcohol product causes skin irritation, seek advice from the Staff Health and Wellbeing Department. Page 19 of 22 Aseptic Technique Policy. V. 3.2 Appendix C Aseptic Technique Guidelines 1. Explain and discuss the procedure with the patient. Assess and identify all equipment needed. Prepare environment 2. Clean the trolley with a detergent wipe and place all equipment required onto the bottom shelf of the trolley. 4. Open dressing pack and empty contents onto the top shelf of the trolley. 3. Wash hands with soap and water using the ten-stage hand washing technique. Put on a single–use, disposable plastic apron. Take the trolley to the patient. 5. Decontaminate hands using the alcohol hand rub. If carrying out a wound dressing, loosen the dressing tape taking care not to expose wound, and decontaminate hands. 6. Open the sterile field. 7. Empty the contents of any additional packs/equipment required onto the sterile field. 8. Decontaminate hands using alcohol hand rub. 10. Keeping the bag on your hand remove the dressing and invert the bag to enclose the soiled dressing. Aseptic Technique Policy. V. 3.2 11. Secure the bag to the side of the trolley below the sterile field. 9. Place hand in yellow bag and arrange sterile field as required. 12. Decontaminate hands using alcohol hand rub. Page 20 of 22 13. Put on sterile gloves – see Appendix D. 14. Once procedure completed, fold up remaining items of the dressing field and place in disposal bag. Remove gloves and apron and place in disposal bag. 15. Seal the disposal bag and dispose of according to Trust policy. 16. Wash hands with soap and water using the six-stage hand washing technique. 17. Document procedure in nursing and/or medical notes. Page 21 of 22 Aseptic Technique Policy. V. 3.2 Appendix D Application of Sterile Gloves Fig. 1 Fig. 3 Fig. 2 Fig. 4 Fig. 5 Page 22 of 22 Aseptic Technique Policy. V. 3.2