Breath Analysis Offers Non-invasive Method to Detect Early Lung
advertisement

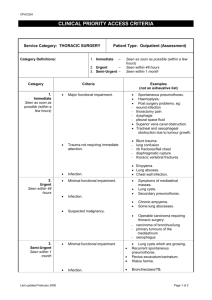
NEWS RELEASE UNDER EMBARGO UNTIL APRIL 29, 2014, 5:15 PM ET For more information contact: Nicole Baritot Managing Editor, AATS Scientific Publications American Association for Thoracic Surgery 500 Cummings Center, Suite 4550 Beverly, MA 01915 USA +1 978-299-4520 press@aats.org www.aats.org Breath Analysis Offers Non-invasive Method to Detect Early Lung Cancer Specificity Double that of PET Scans, According to Presentation at 94th AATS Annual Meeting Toronto, ON, Canada, April 29, 2014 – Researchers at the University of Louisville School of Medicine are using breath analysis to detect the presence of lung cancer. Preliminary data indicate that this promising noninvasive tool offers the sensitivity of PET scanning, and has almost twice the specificity of PET for distinguishing patients with benign lung disease from those with early stage cancer. Michael Bousamra II, MD, Associate Professor, Department of Cardiovascular and Thoracic Surgery, is presenting the results of the study at the AATS 2014 Conference on April 29, 2014. A reliable, noninvasive diagnostic method imposes less physical and financial burden on patients who actually have no significant disease, while rapid and accurate diagnosis expedites treatment for patients who truly have lung cancer. The team believes that while the breath test would not replace CT as a primary screening tool, it would be particularly helpful in conjunction with a positive CT scan result. “This breath analysis method presents the potential for a cheaper and more reliable diagnostic option for patients found to have bulky disease on a CT scan. If the breath analysis is negative, the patient may, in some instances, be followed with repeated exams without necessitating a biopsy. But a positive breath analysis would indicate that the patient may proceed to definitive biopsy, thus expediting treatment,” says Dr. Bousamra. Investigators used specially coated silicon microchips to collect breath samples from 88 healthy controls, 107 patients with lung cancer, 40 individuals with benign pulmonary disease, and 7 with metastatic lung cancer. Previous work had pinpointed four specific substances, known as carbonyl compounds, in breath samples as “elevated cancer markers” (ECMs) that distinguish patients with lung cancer from those with benign disease. The carbonyl compounds found in the breath are thought to reflect chemical reactions occurring in malignant lung tumors. In this study, the authors compared the findings from the breath analyses to the results from PET scans. The investigators found that the sensitivity and specificity of breath analysis depended upon how many of the ECMs were elevated. For example, having 3 or 4 ECMs was diagnostic of lung cancer in 95% of those with this result. The majority of patients with benign pulmonary disease had either 0 or 1 ECM, while those with Stage IV cancer were most likely to have 3 or 4. The number of ECMs could be used to differentiate benign disease from both early and advanced stage lung cancer. Interestingly, 3 of the 4 elevated markers returned to normal levels after cancer resection. When it comes to differentiating early stage lung cancer from benign pulmonary disease, breath analysis and PET scanning had similar sensitivities (82.8% and 90.3%, respectively). However, breath analysis had a much higher specificity than PET (75% vs. 38.7%, respectively) for distinguishing benign disease, which means that it was much more accurate at identifying those who did not have cancer. This would be an important feature for patients with benign disease, since having a breath analysis rather than PET scan could mean avoiding an unnecessary invasive biopsy procedure later on. # # # NOTES FOR EDITORS “Quantitative analysis of exhaled carbonyl compounds distinguishes benign from malignant pulmonary disease,” by Michael Bousamra II, MD, Erin Schumer, MS, MD, Mingxiao Li, PhD, Ralph J. Knipp, MS, Michael H. Nantz, PhD, Victor van Berkel, MD, PhD, and Xiao-An Fu, PhD. Presentation at the 94th AATS Annual Meeting. April 26-30, 2014. Toronto, ON, Canada, during the General Thoracic Surgery Session on April 29, 5:15 PM ET. http://aats.org/annualmeeting/ For more information contact Nicole Baritot, Managing Editor, AATS Scientific Publications, at +1 978299-4520 or press@aats.org. Journalists wishing to interview Dr. Bousamra may contact him at mbousamra@louisvilleheartsurgery.com. ABOUT THE AUTHORS Michael Bousamra II, MD, Department of Cardiovascular and Thoracic Surgery, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Erin Schumer, MS, MD, Department of Cardiovascular and Thoracic Surgery, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Mingxiao Li, PhD, Department of Chemical Engineering, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Ralph J. Knipp, MS, Department of Chemistry, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Michael H. Nantz, PhD, Department of Chemistry, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Victor van Berkel, MD, PhD, Department of Cardiovascular and Thoracic Surgery, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA Xiao-An Fu, PhD, Department of Chemical Engineering, University of Louisville School of Medicine, Abell Administration Center, Louisville, Kentucky USA ABOUT THE AMERICAN ASSOCIATION FOR THORACIC SURGERY (AATS) The American Association for Thoracic Surgery (AATS) is an international organization of over 1,300 of the world’s foremost thoracic and cardiothoracic surgeons, representing 35 countries. AATS encourages and stimulates education and investigation into the areas of intrathoracic physiology, pathology and therapy. Founded in 1917 by a respected group of the last century’s earliest pioneers in the field of thoracic surgery, the AATS’ original mission was to “foster the evolution of an interest in surgery of the Thorax.” One hundred years later, the AATS continues to be the premiere association among cardiothoracic surgeons. The purpose of the Association is the continual enhancement of the ability of cardiothoracic surgeons to provide the highest level of quality patient care. To this end, the AATS encourages, promotes, and stimulates the scientific investigation and study of cardiothoracic surgery. Visit www.aats.org.