EFFECTIVE 60 DAYS FROM DATE ABOVE Meridian Health Plan
advertisement

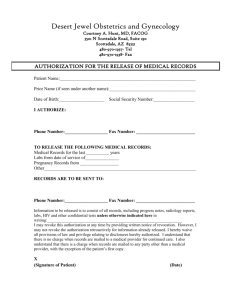
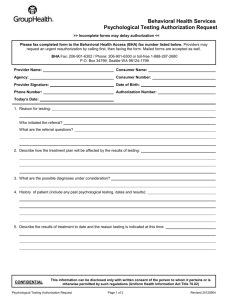
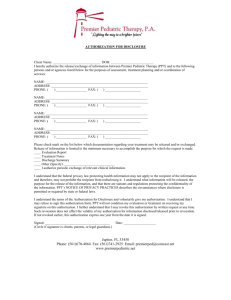
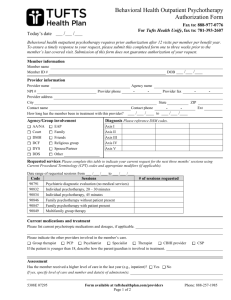
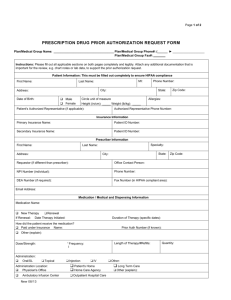
To: Behavioral Health Providers From: Meridian Health Plan Behavioral Health Department State: New Hampshire Line of Business: Medicaid Date: February 26, 2014 Re: Updated Behavioral Health Prior Authorization Form Now Available EFFECTIVE 60 DAYS FROM DATE ABOVE Meridian Health Plan has updated a Behavioral Health Prior Authorization Form to help streamline and expedite prior authorization requests. The form is available online at www.mhplan.com/nh under Documents & Forms. Please contact the Behavioral Health department if you have any questions regarding this form or Meridian’s authorization process at 855-291-5218. Providers may always verify member eligibility by using the following resources: NH MMIS Health Enterprise Portal: You can verify your patients’ eligibility information online at: https://nhmmis.nh.gov/portals/wps/portal/enterprisehome Meridian Health Plan Provider Portal: If you have already registered for our provider portal or would like to sign up, you can check eligibility 24/7 at http://www.mhplan.com/nh/mcs If you have any additional questions or concerns, please contact your local Provider Network Development Representative or: For general questions, call the Provider Services department at 877-480-8250 For Member Services, call 855-291-5221 or fax 603-263-3901 For urgent behavioral health questions, call 855-291-5218 or fax 603-263-3447 Confidentiality Note: This fax contains information from Meridian Health Plan, which may be confidential, legally privileged, or otherwise protected from disclosure. This information is intended for the use of the addressee only. If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution, printing or any other use of, or any action in reliance on, the contents of this fax is strictly prohibited. If you have received this communication in error, please notify us by phone at 313-324-3700. www.mhplan.com New Hampshire Behavioral Health Prior Authorization Form Date: / Fax all authorizations and supporting clinical information to: 603-263-3447 / NPI #: TID #: Last Name : Phone: ( ) Member ID#: Address: PATIENT INFORMATION First Name: DOB: / / Last Name : Phone: ( ) Address: Specialty: PROVIDER INFORMATION First Name: Fax: ( ) Office Contact: SPECIALIST/FACILITY REFERRED TO Specialist Name (Last, First): Fax: ( ) End: / / Specialty: Facility Name: Phone: ( ) Start: / / Address: SERVICES THAT DO NOT REQUIRE PRIOR AUTHORIZATION Individual Psychotherapy, Group Psychotherapy and Family Therapy provided by a psychiatrist. Psychotherapy services provided by psychotherapy providers other than psychiatrists are limited to 18 visits per year for members 21 and older, and 24 visits for members under 21 years of age. SERVICES THAT REQUIRE NOTIFICATION TO MERIDIAN Involuntary emergency admissions to NH Hospital/DRF Intensive Outpatient Program for members under 22 SERVICES THAT REQUIRE PRIOR AUTHORIZATION Bilateral Electroconvulsive Therapy (ECT) Psychological Testing (>6 hours in a 6 month period) Unilateral Electroconvulsive Therapy (ECT) Neuropsychological Testing (>6 hours testing in a 6 month period) Psychological Testing (1st 6 hours in a 6 month period) Developmental Testing (1st 6 hours in a 6 month period) Neuropsychological Testing (1st 6 hours in a 6 month period) SERVICES THAT REQUIRE PRIOR AUTHORIZATION FOR NON-BBH ELIGIBLE MEMBERS Additional Outpatient visits beyond service limits SERVICES THAT REQUIRE PRIOR AUTHORIZATION FOR BBH ELIGIBLE MEMBERS Additional Outpatient visits beyond service limits for low utilizers CMHC Service Providers: Refer to your provider agreement and to the Meridian Provider Manual for a complete list of prior authorized services, Billable Provider Types and codes. SERVICES REQUESTED CPT Code CPT Code ICD 9/ICD 10 Code: # of Visits Requested: CPT Code CPT Code CPT Code CPT Code Comments: _______________________________________________________________________________________________ _________________________________________________________________________________________________________ The following services are not covered benefits under Medicaid, but are not limited to: Psychological or Neuropsych testing ordered for—Forensic Evaluation, Custody Determination or Placement, Academic or Educational Determinations Services or items free to the public Services provided by halfway houses Detoxification services provided outside an acute care facility or medical service clinic Please see the Meridian Provider Manual for a complete service list of non-covered services FORM45 NH—Rev. 20140224 All Voluntary Inpatient Admissions require authorization from Meridian Health Plan. Please refer to the Meridian Provider Manual for details. PAGE 1 of 2 New Hampshire Behavioral Health Prior Authorization Form Fax all authorizations and clinical information to: 603-263-3447 Phone: 855-291-5218 Please summarize briefly and attach supportive clinical documentation: RECIPIENT HISTORY: __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ LEVEL OF FUNCTIONAL IMPAIRMENT: __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ WHY ARE THE SERVICES MEDICALLY NECESSARY?: __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ TREATMENT PLAN (Include time frames and progress information): __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ ARE THERE EXTENUATING CIRCUMSTANCES? IF YES, PLEASE ADVISE: __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ __________________________________________________________________________________________________________ Signature: Name/Title (Print): By requesting prior authorization, the provider is representing that the services to be provided are medically necessary. As a condition of authorization for services, the servicing provider agrees to accept no more than 100% of New Hampshire Medicaid rates. At no time will Meridian Health Plan pay more than 100% of NH Medicaid rates for any service. In the event that these services are deemed not to be medically necessary, Meridian will not reimburse the provider for those services. FORM45 NH—Rev. 20140224 PAGE 2 of 2