Journal Of Endurance July 2004
advertisement

JOURNAL OF ENDURANCE
JULY 2004 #6
Omnia Mutantur Nos Et Mutamur In Illis...
(ALL things change, including us...)
=============================================================
Greetings, the following questions are reviewed in this issue:
#1 How many calories
calories does basal metabolic rate (BMR) require and
what happens to BMR during training?
#2 What specific hormone genetically activates mitochondria cell
energyenergy-producing rate for endurance?
#3 How is dietary protein best manipulated for optimal lean muscle
mass
mass growth and recovery following intense endurance training?
#4 What causes exerciseexercise-associated muscle cramps?
#5 How many calories are actually burned during exercise?
#6 What guidelines preserve lean muscle mass, enhance health with
longevity implications?
implications?
#7 What overover-thethe-counter NSAIDS, which remarkably reduces the risk
of breast cancer?
#8 Why is folate so important a companion to vitamin BB-12 for optimal
lean muscle mass synthesis, cardiovascular markers, and red blood cell
volume?
#9 What foods block the progression of colorectal cancer and why
should endurance athletes be so concerned about reducing this risk?
#10 What's wrong with drinking alcohol after a workout?
=============================================================
#1 How many calories does
does basal metabolic rate (BMR) require and
what happens to BMR during training?
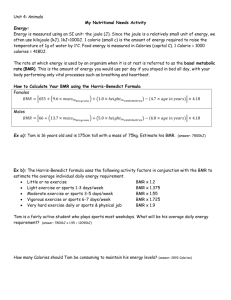
If you know your body fat and lean body mass (body muscle) percentage, you can
obtain a fairly precise estimate of your BMR. For example, the formula from Katch
& McArdle (1) takes into account lean mass and therefore is more accurate than a
formula based on total body weight. The Katch-McArdle formula applies equally to
men and women As Follows:
BASAL METABOLISM RATE = 370 + (21.6 X lean mass in kg)
To determine your total daily calorie needs, now multiply your BMR by the
appropriate activity factor, as follows:
•
If you are Sedentary - little or no exercise
Calorie-Calculation = BMR X 1.2
•
If you are Lightly Active (light exercise/sports 1-3 days/week)
Calorie-Calculation = BMR X 1.375
•
If you are Moderately Active (moderate exercise/sports 3-5 days/week)
Calorie-Calculation = BMR X 1.55
•
If you are Very Active = BMR X 1.725 (hard exercise/sports 6-7 days/week)
Calorie-Calculation = BMR X 1.725
•
If you are Extra Active (very hard daily exercise/sports & physical job or 2X day
training)
Calorie-Calculation = BMR X 1.9
THE EFFECTS ON BMR FROM EXERCISE TRAINING (2)
Researchers measured basal metabolic rate (BMR) during training on 3 different
phases of training prior to competition:
(1) TRANSITION (TP)
(2) PRE-COMPETITION (PP)
(3) COMPETITION (CP)
Twelve national level male athletes, aged between 18 and 20 years were recruited.
Anthropometry, body composition and BMR were measured. The quantification of
training was done by time allocation pattern combined with measurements of oxygen
consumption, heart rate and mechanical power output relationships in all three phases.
The results showed an increase of 1.2 folds in training intensity and 2 folds in training
duration from transition to competition phase of training.
These training changes resulted as:
(1) Increased 1.5 kg weight gain
(2) Increased 1.6 kg Lean Body Mass gain
(3) Increased 9% BMR in 24-hours
(4) Increased in 1.5 Kcal/kg body weight (2.8 Kcal/M2 and 1.7 Kcal/kg LBM when
expressed in terms of BMR)
(5) Increased 12 L/min in MVE Max from TP to CP of training
This study concludes that the BMR varies with the quantum of training was made to
provide phase wise phase wise prediction equations of BMR for athletes and hence it
must be measured periodically to identify energy needs. It is well established that
measurement of Basal Metabolic Rate (BMR) provides an important energy baseline for
the formulation of a sound diet, as it contributes about 50-70% of the total daily energy
expenditure. In addition to BMR, the additional variables than combine to influence the
quality of an athlete’s diet and training are age, sex, climate and body composition.
The FAO/WHO/UNU (1985) study on energy and protein requirements of humans,
suggested that various components of energy expenditure be expressed as multiples of
BMR. Even though many prediction equations are available for BMR, the validity of
their application to athletes can be questioned due to the limited involvement of athletes
ins the subjects used to formulate these equations. For the BMR equations that have been
developed with athletes, NONE provide an assessment of the change in BMR with
changes in training. Therefore, the present study was carried out to measure BMRs of
athletes during different phases of training. It was theorized identification of changes in
BMR would detect needed changes in caloric intake, which in turn would support the
maintenance of desirable weight, body composition and peak performance.
RESULTS
The results of the physical characteristics including anthropometry and body composition
are given in Table 1. The mean height of these athletes was increased by 0.5 cm with a
considerable increase in weight by 1.5 kg from TP to CP, without any significant
variation between first two phases (TP to PP). The BMI was increased from TP to CP by
about 2%. The body surface area was also significantly increased from TP to CP.
However, no significant difference between first two phases was found in all these
parameters. It can be understood from the results that the body composition was altered
by an increase in LBM by 1.6 kg (2.6%) with a 0.1 kg reduction (not significant) in fat
mass. However, no significant alteration was found in LBM in first two phases of
training.
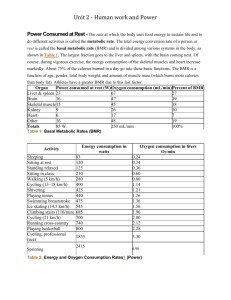
TABLE 1: PHYSICAL CHARACTERISTICS OF THE ATHLETES (n=12)
Training
Height
Weight
BMI
BSA
Phase
(cm)
(Kg)
(Kg/m2)
(m2)
TP
172.8a ± 2.83 61.4a ± 5.36 20.6a ± 1.69 1.73a± 0.07
PP
CP
F-Ratio
P-Value
LBM
Fat%
(Kg)
55.2a± 4.22 9.9a ±
2.69
172.8a ± 2.87 61.1a ± 4.99 20.4a ± 1.71 1.73a ± 0.06 55.0 a ± 4.00 9.8a ±
3.07
173.3b ± 2.69 62.9b ± 5.19 21.0b ± 1.71 1.75b ± 0.07 56.8b ± 4.27 9.6a ±
2.12
7.90
16.85
9.70
23.79
45.90
0.36
**
***
***
***
***
NS
Values are expressed as mean SD; variation in superscript indicates significance of difference between
mean values of phases. **P<0.01, ***P<0.001, NS=Not Significant.
The basal metabolic rates (BMR) data are presented in Table 2. The 24-hour BMR was
significantly increased from TP to CP, without any significant rise between first two
phases of training. On the other hand, the BMR was found to increase from TP to PP with
no further rise to CP when expressed in terms of unit mass of body weight. Similar
observations were made when BMR was expressed per unit LBM. However, the BMR
when expressed in terms of unit BSA increased from TP to PP and then to CP.
TABLE 2: BASAL METABOLIC RATE OF THE ATHLETES (N=12)
Training Kcal/min
Kcal/day
Kcal/
Kcal/ m2
Kcal/
Phase
Kg body wt
Kg.LBM
TP
1.008a ± 0.10 1451.8a ± 145.16 23.7a ± 1.84 34.9a ± 2.61 26.3a ± 1.52
1.041a ± 0.09
1499.8a ± 138.15 24.6b ± 1.51 36.2b ± 0.06
27.9b ± 2.45
1.100b ± 2.69
F-Ratio
16.35
1584.4b ± 151.19 25.2b ± 1.71 37.7c ± 0.07
16.35
9.26
12.38
28.0b ± 4.27
5.63
PP
CP
P-Value
***
***
***
***
*
Values are expressed as mean ± SD; variation in superscript indicates significance of difference between
mean values of phases. *P<0.05, ***P<0.001, NS=Not Significant.
During the exercise test, the energy expended in terms of BMR (BMR multiple factor) at
maximal workload was almost similar in all the 3 phases of training (Table 3), but the
athletes could perform more work (WR) in CP than the other two phases.
TABLE 3: PHYSIOLOGICAL CHARACTERISTICS OF ATHLETES AT
MAXIMAL LOAD OF GRADED EXERCISE TEST (N=12)
Training
O2
MVE
HR
BMR
O2
WR
Phase
ml/min
L/min
bpm
Factor
Pulse
Kpm/min
TP
2909.6 a
71.9a
191a
14.6a
15.3a
2012.8a
± 382.4
± 7.72
± 10.7
± 2.72
± 2.19
± 78.29
PP
3015.4 a
71.6a
188a
14.6a
16.1ab
2099.3a
± 541.6
± 4.99
± 10.3
± 3.16
± 2.79
± 171.66
CP
3254.8 a 83.94b
188a
15.0a
17.3 b
2319.3b
± 258.8
± 10.64 ± 11.2
± 1.75
± 1.07
± 206.63
F-Ratio
3.17
20.78
0.62
0.16
4.85
11.27
P-Value
NS
***
NS
NS
*
***
Values are expressed as mean±SD; variation in superscript indicates significance of difference between
mean values of phases. *P<0.05, ***P<0.001, NS=Not Significant.
Quantification of training (Table 4) showed that the duration of training was significantly
increased by 1.8 fold and 2.0 fold from TP to PP, and TP to CP, respectively. The energy
expenditure (Kcals/min) minute was comparable in first two phases and significantly
increased in CP. The intensity of training expressed in terms of work rate (kpm/min)
increased significantly by 1.20 fold (20.5%) from TP to CP (Table 4).
The percent contribution of 24 hr BMR in total daily energy expenditure along with
the BMR multiple factor of athletes in different phases of training are given in Table
5. The percent contribution of BMR was about 50.2% in both TP and PP, while it
was reduced to 46.5% in CP. The BMR multiple factor (the ratio between TDEE
and 24 hr BMR) was found to be 1.81,1.98 and 2.15 during TP, PP and CP of
training respectively. Based on the results of the present study, the 24-hour BMR
prediction equations were developed and presented for each phase using subject height
and weight as independent variables (Table 6).
TABLE 4: ENERGY COST QUANTIFICATION OF TRAINING IN ATHLETES
(N=12)
Training
Phase
TP
PP
CP
F-Ratio
P-Value
Duration
Kcal/min
(min)
88.0a ± 3.85
7.987a ± 1.47
158.0b ± 14.73 7.330a ± 0.44
171.0c ± 16.24 8.987b ± 5.19
403.27
11.99
***
***
Training Intensity
(kpm/min)
825.6a ± 120.73
883.8a ± 1.51
994.7b ± 1.71
11.92
***
Values are expressed as mean±SD; variation in superscript indicates significance of difference between mean values
of phases. ***P<0.001.
TABLE 5: PERCENT CONTRIBUTION OF BMR IN TDEE AND BMR
MULTIPLE FACTOR OF ATHLETES IN DIFFERENT PHASES OF TRAINING
(N=12)
Training
BMR
TDEE
% Contribution
BMR Multiple
Phase
Kcal/day
Kcal
Factor
TP
55.21
1.81
1451.8a ± 145.6 2629.3 a ± 214.67
PP
50.32
1.98
1499.8a ± 138.15 2980.6b ± 324.12
CP
46.5
2.15
1584.4b ± 144.07 3409.8c ± 148.18
Values are expressed as mean±SD; variation in superscript indicates significance of difference between
mean values of phases. +
TABLE 6: PREDICTION EQUATIONS FOR 24-HR BMR OF ATHLETES
USING HEIGHT AND WEIGHT DURING DIFFERENT PHASES OF TRAINING
Training Phase
Equation
R2
F-Ratio
TP
(Ht X 9.629) + (Wt. X 14.968) - - 1140.2 64.18 28.67
PP
(Ht X 0.584) + (Wt. X 19.257) + + 211.01 78.68 59.03
CP
(Ht X 7.529) + (Wt. X 14.305) - - 628.27 62.59 26.76
Ht = Height in cm, Wt = Weight in Kg.
DISCUSSION
BMR plays a crucial role in human energy metabolism by providing a strong basis for the
understanding and formulation of a sound nutrition. In the present study, the 24-hour
BMR of athletes significantly increased from TP to CP by +9% without any
significant variation between first two phases of training. The increase in BMR might
be due to an over-all increase in body surface area and/or body weight, resulting in an
increase in metabolically active tissue. There were also some close evidences to show
that BMR increases with an increase in body weight and lean body mass. Similar
observations were found in the present study in that there was a significant increase in 24
hour BMR with an increase in body weight and lean body mass from TP to CP as a
consequence to incremental training load. This association is also evident from the high
positive correlation between 24-hourbasal metabolic rates (BMR) and body weights as
well as between BMR and LBM. It is difficult to make comparison of BMR of these
athletes with other athletes since there is scant literature available from India and other
parts of the world. In a study carried out by Poelhman BMR was measured in male
athletes, resulting in a 24 hour BMR of 1712 Kcal/day. On the other hand, the studies
carried out by Ramana et al showed the BMR of Indian athletes ranged between 13001450 Kcal/day. Interestingly, the 24-hour BMR of normal healthy untrained males (1830 years, 60 kg) was found to be 1430 Kcal/day, as reported by ICMR in the
recommended energy allowances for Indians. However, to compare the BMR of trained
and untrained individuals a suitable approach might be to normalize BMR for LBM.
Another study reported no difference in BMR between long-distance runners and
untrained men. On the other hand, many studies reported 5-19% higher BMR values
when expressed as percent LBM (BMR/LBM) in trained individuals when compared to
untrained individuals. It is also important to note that such comparative studies must be
analyzed carefully by considering various other factors like nutritional status, physical
activity pattern and degrees of adaptation to training. A limited number of studies were
available in healthy human subjects about the assessment of changes in BMR with
training.
Some studies show a decrease in BMR among men at different stages of training from
which it appears that longer and more strenuous training correlates with decreases in
BMR. Another study during training associated with average decreases in BMR
approximating 7% (range 3-14%) in athletes participating either in football, swimming or
basketball, while it did not change in swimmers and increased 12% in cross country
runners. Apart from this, in three non-athletes who were trained for 6 weeks, the impact
was variable. One had shown a fall below control over the first 28-35 days and then
increased to 9% higher than control by 42nd day. When assessing the results of the
present study, the percent contribution of BMR in the 24 hour daily energy expenditure
of these athletes during different phases it can be understood that it was slowly
decreasing from 55.2% to 50.3% to 46.5% during TP, PP & CP respectively. The
conserved energy from BMR might be diverted to cope with the increased intensity of
training load from TP to CP. In addition to this, when BMR is expressed in terms of unit
lean body mass, it was significantly increased during PP and reached a near plateau
during CP. Further increases in training volume or intensity may then decrease BMR. As
shown by Parizkova, when the athletes receive overload training, the 24-hour BMR or
per unit LBM reduced, presumably to conserve energy to support adaptation processes.
Based on the extensive review of literature available on the influence of various factors
on BMR, the FAO/WHO/UNU (1985) expert committee reiterated age, sex and body
composition are the main influential variables to BMR. They worked out an equation to
predict BMR based on the body weight (Kg) for different age and sex groups for normal
healthy population that did not include athletic population. The BMR prediction equation
for 18-30 years males was 13.3 X Body Wt (Kg) + 679. Based on this equation, and
considering the body weight of the study group, the predicted value of BMR was derived.
It was observed that these predicted values were estimated higher by 11%, 8% and 4%
during TP, PP and CP, respectively when compared to the measured values. Hence, these
equations may not be applicable to the athletic population. Therefore, an effort was
made to derive phase wise 24-hour BMR prediction equations using simple
anthropometric indices such as heights and weights based on the data of the study
subjects using multiple regression analysis and the same were given. It can be concluded
from this study that the BMR should be evaluated periodically for athletes to determine
variations in energy allowances so as to maintain desirable body weight and
composition. The phase-dependent BMR prediction equations can be of greater use for
the sport nutritionists in recommending energy allowances for the athletes (2).
References
(1) Katch F, Katch V, McArdle W. EXERCISE PHYSIOLOGY: ENERGY,
NUTRITION, AND HUMAN PERFORMANCE, 4th edition. Williams & Wilkins,
1996.
(2) Excerpts from: Variations in basal metabolic rate with incremental training load
in athletes. Venkata Ramana Y, Surya Kumari Mvl, Sudhakar Rao S, Balakrishna
N. JEP 2004;7(1):26-33. by permission courtesy of Dr. Venkata Ramana Y1,
Dept. Of Physiology, Biophysics Division, National Institute of Nutrition, Indian
Council Of Medical Research, Hyderabad – 500 007 (A.P.), India; Phone: 91-4027008921 ext. 333; FAX: 91-40-27019074; Email: vryagnam@yahoo.com
COMMENT: The differences reported between decreased and increased BMR during
training may reflect the body’s adaptation as a survival preservation reaction to change.
This may reflect why weight loss intervention often plateau or cease weight loss.
________________________________________________________________________
#2 What specific hormone genetically activates mitochondria cell
energyenergy-producing rate for endurance?
The influence of Thyroid Hormone (T3) on respiration is partly mediated via its
effect on the cytochrome c oxidase (COX) enzyme,
enzyme a multi-subunit complex
within the mitochondrial respiratory chain. Researchers compared the expression
of COX subunits I, III, Vb, and VIc and thyroid receptors (TR)1 and TR1 with
functional changes in COX activity in tissues that possess high oxidative
capacities. In response to 5 days of T3 treatment, TR1 increased 1.6-fold in liver,
whereas TR1 remained unchanged. T3 also induced concomitant increases in
the protein and mRNA expression of nuclear-encoded subunit COX Vb in liver,
matched by a 1.3-fold increase in binding to a putative thyroid response element
(TRE) within the COX Vb promoter in liver, suggesting transcriptional regulation.
1
Special gratitude to Dr. Venkata Ramana et al. (2), for granting permission to share their important
research.
In contrast, T3 had no effect on COX Vb expression in heart. T3 produced a
significant increase in COX III mRNA in liver but decreased COX III mRNA in
heart. These changes were matched by parallel alterations in mitochondrial
transcription factor A expression in both tissues. In contrast, COX I protein
increased in both liver and heart 1.7- and 1.5-fold (P < 0.05), respectively. These
changes in COX I closely paralleled the T3-induced increases in COX activity
observed in both of these tissues. In liver, T3 induced a coordinated increase in
the expression of the nuclear (COX Vb) and mitochondrial (COX I) genomes at
the protein level. However, in heart, the main effect of T3 was restricted to the
expression of mitochondrial DNA subunits. Thus our data suggest that T3
regulates the expression of COX subunits by both transcriptional and
posttranscriptional mechanisms. The nature of this regulation differs between
tissues possessing a high mitochondrial content, like liver and heart [1].
COMMENT:
COMMENT Tissue-specific regeneration effecting both quality and quantity
regeneration in high energy mitochondria synthesis suggests a relationship
associated with thyroid hormone. Thyroid hormones are known to regulate the
rate of metabolism effecting how fast, how slow, and how efficiently the body
uses fuel substrates to produce energy. Low thyroid production is diagnosed by
high levels of TSH (thyroid stimulating hormone). Borderline thyroid levels may
be accompanied by low body temperature, which may be associated with low
normal thyroid, low progesterone (prior to ovulation in females), or even in some
males.If morning AM body temperature upon awakening is 97.5 degrees F, a
thyroid panel may be ordered to determine if thyroid is low. As metabolic rate
decreases, performance decreases, and until now, the association between
lower rate of metabolism and energy production have been not understood.
Since it is often most difficult to control the dose effects of thyroid medication
accurately, some researchers suggest modest dose of 2 oral supplements,
Coleus Forskolin and 7-keto DHEA have been shown to resolve hypothyroid
disorders for some subjects. Hyperthyroid patients, pregnant or lactating females
or anyone being treated by reducing androgens should NOT take either
supplement. The mitochondria's most potent electron carriers for reproducing
ATP from within mitochondria cells are Coenzyme Q-10 and several
Cytochromes, especially Cytochrome c Oxidase. Whatever increases volume of
both, from exogenous or endogenous presence, will increase the efficiency/rate
by which the body produces energy.
Reference
[1] Tissue-specific regulation of cytochrome c oxidase subunit expression by
thyroid hormone Treacey E. Sheehan, Ponni A. Kumar, and David A. Hood Am J
Physiol Endocrinol Metab 2004;286 968-974.
Animation of Electron Transport Cycle in Mitochondria
© Thomas M. Terry, The University of Connecticut.2
2
By Permission, courtesy of Professor Thomas Terry, Ph.D. University of Connecticut @
http://www.biologie.uni-hamburg.de/b-online/library/bio201/bio201.html
Click for animation
Go to Animation of ATP synthesis in Mitochondria
The schematic diagram above illustrates a mitochondrion. In the animation, watch as
NADH transfers H+ ions and electrons into the electron transport system. Note the
importance of Cytochrome c’s carrier function completing the link between Complex 2-3.
Key points:
•
•
•
•
Protons are translocated across the membrane, from the matrix to the intermembrane space
Electrons are transported along the membrane, through a series of protein carriers
Oxygen is the terminal electron acceptor, combining with electrons and H+ ions produces water
As NADH delivers more H+ and electrons into the ETS, the proton gradient increases, with H+
building up outside the inner mitochondrial membrane, and OH- inside the membrane.
Go to Dr. Terry's Home Page3
Go to Science Educators Links from NSTA
________________________________________________________________________
#3 How is dietary protein best manipulated for optimal lean muscle
mass growth and recovery following intense endurance training?
training?
Ultra filtration and all low temperature processing yields undenatured, very high
nitrogen-boosting protein. Exercising athletes tend to increase the need for
quality protein to restore their body back into a state of positive nitrogen balance
(PNB). Stable "undenatured", low heat, ultra filtered, predigested, peptidebonded Whey Protein is suggested for providing the best bioactive source of
nitrogen-balance that translates to optimal muscle growth, recuperation, and
repair. The more denatured a protein is the less your body absorbs, for expected
muscle synthesis [regrowth + growth]. Heat may damage some proteins, and
especially whey protein. Heat processing that ruptures and reforms protein
molecules is called "denaturing", which makes digestion and absorption difficult,
reducing the protein's bioavailability for anabolic growth potential. Cheap
processing methods denatures proteins robbing the athlete of what a protein
supplement should replenish.
Scientific studies clearly show that when heat is used to dry protein, it burns
thousands of cross-linked bonds into the original amino acid structure. When this
denatured protein is ingested the enzymes in your intestines work overtime,
struggling to break it down. It takes awhile, and an may be gastrically
uncomfortable. When all is finally said and done, little protein is actually absorbed
and any resulting nitrogen retention is negligible. The worst
thing about drying whey in this manner is that it destroys highly valuable
immunoglobulin fractions.
The results of low-heat processed peptide-bonding, predigested high ionechange whey protein isolates are:
1.
2.
3.
4.
5.
6.
7.
More insulin-like growth factor (IGF-1) release
Improved overall endocrine hormone response
A highly increased state of nitrogen utilization and retention
More intracellular anti-aging antioxidants present
An increased state of immune function
Improved gastrointestinal health
Increased muscle growth rates
Recent research argues favorably for"Dietary Manipulation" of 1 part protein with
3 parts carbohydrate as an adjunct for improving lean muscle mass post-exercise
recovery.
To optimize the postexercise insulin response and to increase plasma amino acid
availability, van Loon et al., [1] studied postexercise insulin levels after the
ingestion of carbohydrate and wheat protein hydrolysate with and without free
leucine and phenylalanine. After an overnight fast, eight male cyclists visited our
laboratory on five occasions, during which a control drink and two different
beverage compositions in two different doses were tested. After they performed a
glycogen-depletion protocol, subjects received a beverage (3.5 mL · kg-1) every
30 min to ensure an intake of 1.2 g · kg-1 · h-1 carbohydrate and 0, 0.2 or 0.4 g ·
kg-1 · h-1 protein hydrolysate (and amino acid) mixture. After the insulin
response was expressed as the area under the curve, only the ingestion of the
beverages containing wheat protein hydrolysate, leucine and phenylalanine
resulted in a marked increase in insulin response (+52 and + 107% for the 0.2
and 0.4 g · kg-1 · h-1 mixtures, respectively; compared w
ith the carbohydrate-only trial). A dose-related effect existed because doubling
the dose (0.2–0.4 g · kg-1 · h-1) led to an additional rise in insulin response.
Plasma leucine, phenylalanine and tyrosine concentrations showed strong
correlations with the insulin response. This study provides a practical tool to
markedly elevate insulin levels and plasma amino acid availability through dietary
manipulation, which may be of great value in clinical nutrition, (recovery) sports
drinks and metabolic research.
WHAT IS A PROTEIN?i
Amino Acids adjoined make proteins. Each amino acid consists of an amino
functional group, and a carboxyl acid group, and differs from other amino
acids by the composition of an R group:
Following digestion and breakdown of protein into an assortment of amino acids the
enormously complex process of rebuilding (synthesis) tissues begins:
Crick's central dogma. Information flow (with the exception of reverse
transcription) is from DNA to RNA via the process of transcription, and thence to
protein via translation. Transcription is the making of an RNA molecule off a DNA
template. Translation is the construction of an amino acid sequence (polypeptide)
from an RNA molecule. Although originally called dogma, this idea has been tested
repeatedly with almost no exceptions to the rule being found (save retroviruses).
The central dogma. Image from Purves et al., Life: The Science of Biology, 4th
Edition, by Sinauer Associates (www.sinauer.com) and WH Freeman
(www.whfreeman.com), used with permission.
The blue-background graphics throughout this chapter are from the University of
Illinois' DNA and Protein Synthesis site.
Messenger RNA (mRNA) is the blueprint for construction of a protein. Ribosomal
RNA (rRNA) is the construction site where the protein is made. Transfer RNA
(tRNA) is the truck delivering the proper amino acid to the site at the right time.
RNA has ribose sugar instead of deoxyribose sugar. The base uracil (U) replaces
thymine (T) in RNA. Most RNA is single stranded, although tRNA will form a
"cloverleaf" structure due to complementary base pairing.
Transcription:
Transcription: making an RNA copy of a DNA sequence
RNA polymerase opens the part of the DNA to be transcribed. Only one strand of
DNA (the template strand) is transcribed. RNA nucleotides are available in the
region of the chromatin (this process only occurs during Interphase) and are linked
together similar to the DNA process.
Transcription of a segment of DNA to form a molecule of RNA. The above images
are from http://www.biosci.uga.edu/almanac/bio_103/notes/may_23.html.
A summary picture is included below:
SUMMARY PICTURE
The illustration below is from Genentech's Access Excellence site, which may be
accessed @: http://www.gene.com
COMMENT: In response to publication of this article, I asked these researchers if
Whey Protein Isolates were considered a bioacative "protein hydrolysate" like the
one in their study. I was doubtlessly informed that undenatured Whey Protein
Isolates are highly bioactive protein donors similar to their concluded application
using wheat protein hydrolysates.
REFERENCE
[1] Ingestion of Protein Hydrolysate and Amino Acid-Carbohydrate Mixtures
Increases Postexercise Plasma Insulin Responses in Men Luc J. C. van Loon,
Margriet Kruijshoop, Hans Verhagen, Wim H. M. Saris, Anton J. M.
Wagenmakers, J. Nutr. 2000;130 2508-2513.
________________________________________________________________________
______________
#4 What causes exerciseexercise-associated muscle cramps?
Endurance Athletes often ask, What causes of muscle cramping during exercise?
I am hesitant to comment on the cause of muscle cramps, since the etiology is
very difficult to define due to EAMC cramps being very specific to the individual
athlete. The first part of this reply report the observations of researchers while the
last part of the reply share what athletes did to resolve their individual cramping
problems during intense endurance exercise. These resolutions at the end of this
XP are taken from reports we have collected since 1996.
Noakes et al., reviewed the exercise-induced muscle cramps origin: "The
aetiology of Exercise-associated Muscle Cramps (EAMC), defined as 'painful,
spasmodic, involuntary contractions of skeletal muscle during or immediately
after physical exercise', has not been well investigated and is therefore not well
understood. Their review focused on the physiological basis for skeletal muscle
relaxation, a historical perspective and analysis of the commonly postulated
causes of EAMC, and known facts about EAMC from recent clinical studies.
Historically, the causes of EAMC have been proposed are 4 theories:
(1) Abnormalities (Inherited) SUBSTRATE METABOLISM
('metabolic theory')
(2) Abnormalities of FLUID BALANCE ('dehydration theory')
(3) EXTREME ENVIRONMENT CONDITIONS H
HEAT
EAT OR COLD
('environmental theory')
(4) Abnormalities of SERUM ELECTROLYTE CONCENTRATIONS
('electrolyte theory') However, Miles & Clarkson argue: "It is
commonly assumed that cramps during exercise are the result of
fluid electrolyte imbalance induced by sweating, two studies have
not supported this. Moreover, participants in occupations that
require chronic use of a muscle but do not elicit profuse sweating,
such as musicians, often experience cramps. Fluid electrolyte
imbalance may cause cramps IF there is profuse prolonged
sweating such as that found in working in a hot environment [2]."
Detailed analyses of the available scientific literature including data from recent
studies do not support these hypothesis for the causes of EAMC.
Electromyographic (EMG) data obtained from runners during EAMC revealed
that baseline activity is increased (between spasms of cramping) and that a
reduction in the baseline EMG activity correlates well with clinical recovery.
Furthermore, during acute EAMC the EMG activity is high, and passive stretching
is effective in reducing EMG activity. This relieves the cramp probably by
invoking the inverse stretch reflex. In two animal studies, abnormal reflex activity
of the muscle spindle (increased activity) and the Golgi tendon organ (decreased
activity) has been observed in fatigued muscle. They hypothesize that EAMC is
caused by sustained abnormal spinal reflex activity which appears to be
secondary to muscle fatigue. Local muscle fatigue is therefore responsible for
increased muscle spindle afferent and decreased Golgi tendon organ afferent
activity. Muscles which cross two joints can more easily be placed in shortened
positions during exercise and would therefore decrease the Golgi tendon organ
afferent activity. In addition, sustained abnormal reflex activity would explain
increased baseline EMG activity between acute bouts of cramping. Finally,
passive stretching invokes afferent activity from the Golgi tendon organ, thereby
relieving the cramp and decreasing EMG activity [1].
Bentley's paper reviews the literature and neurophysiology of muscle cramp
occurring during exercise with no mention of gender-specificity:
Many Athletes are regularly frustrated by exercise-induced muscle cramp yet the
pathogenesis remains speculative with little scientific research on the subject.
This has resulted in a perpetuation of MYTHS as to the cause and treatment of it.
There is a need for scientifically based protocols for the management of athletes
who suffer exercise-related muscle cramp. Disturbances at various levels of the
central and peripheral nervous system and skeletal muscle are likely to be
involved in the mechanism of cramp and may explain the diverse range of
conditions in which cramp occurs.
The activity of the motor neuron is subject to a multitude of influences including:
1 Peripheral receptor sensory input
2 Spinal reflexes
3 Inhibitory interneurons in the spinal cord
(synaptic/neurotransmitter modulation)
4 Descending CNS input (synaptic/neurotransmitter modulation)
The muscle spindle and golgi tendon organ proprioceptors are fundamental to
the control of muscle length and tone and the maintenance of posture.
Disturbance in the activity of these receptors may occur through:
1 Faulty Posture
2 Shortened Muscle Length
3 Intense Exercise
4 Exercise To Fatigue
These disturbances cause increased motor neuron activity and motor unit
recruitment. The relaxation phase of muscle contraction is prolonged in a
fatigued muscle, raising the likelihood of fused summation of action potentials if
motor neuron activity delivers a sustained high firing frequency.
Treatment of cramp is directed at reducing muscle spindle and motor neuron
activity by reflex inhibition and afferent stimulation. There are no proven
strategies for the prevention of exercise-induced muscle cramp but regular
muscle stretching using post-isometric relaxation techniques, correction of
muscle balance and posture, adequate conditioning for the activity, mental
preparation for competition and avoiding provocative drugs may be beneficial.
Other strategies such as incorporating plyometrics or eccentric muscle
strengthening into training programs, maintaining adequate carbohydrate
reserves during competition or treating myofascial trigger points are speculative
and require investigation [3].
One of the more specific papers was reported that "A positive feedback loop
between peripheral afferents and alpha motor neurons, mediated by changes in
presynaptic input, is a possible mechanism underlying muscle cramp. A muscle
cramp was induced in the medial head of the gastrocnemius muscle in four of
seven subjects using unloaded maximal voluntary contraction of the triceps surae
in the shortened position. Surface electromyography over the medial and lateral
heads of gastrocnemius and the soleus muscles demonstrated that the muscle
activity during cramp was localized to part or all of the medial head of the
gastrocnemii. In the same muscle, a tungsten electrode was used to record from
200 motor units during 16 episodes of cramp and 871 units during 26 voluntary
contractions. For the first 30 seconds, significantly higher motor unit firing rates
were recorded during cramp compared with unloaded voluntary contractions.
Motor unit firing rates were also more variable during cramp. When the cramped
muscle was stretched forcibly to break the cramp, motor unit activity increased in
all the triceps surae muscles. In some experiments, the Achilles tendon of five
subjects was vibrated for 50 seconds before and after voluntary contraction or
cramp. The tonic vibration reflex (TVR) was depressed or absent after four
episodes of cramp but it was unchanged after voluntary contraction. These data
are interpreted to indicate that motor units are involved in ordinary muscle cramp.
A positive feedback loop between peripheral afferents and alpha motor neurons,
mediated by changes in presynaptic input, is a possible mechanism underlying
muscle cramp [4]."
ANECDOTAL ENDURANCE ATHLETES' CRAMPCRAMP-RELATED RESOLUTIONS
The origins of muscle cramping are multiple and poorly understood. In review of
the electrolyte, fluid, and fuel -related disturbances from athletes who resolved
cramping problems the following individual resolutions were reported to us from
1996-2004:
1 Fluid intake under 30 fluid ounces per hour
2 Endurolyte intake range 3-6 per hour
3 Fuel/calorie intake under 300 k/cal/hour
4 Acclimatization training in heat 14-21 days
5 Interval training sessions 2-3 X week
6 Glycerol hyperhydration loading protocol (Liquid Endurance)
7 Elimination of supplemental ginseng, fructose, caffeine, simple
sugar, creatine
8 Increase endurance duration training distance
9 Reduced pace to suite individual fitness state
10 Change in prescription medications
11 Unknown resolutions: "They just went away..."
COMMENT: You have probably seen some of the information in this article in the
past. With the heat and humidity of early and mid season training present, the
article needs to be repeated. Oddly when athletes properly acclimatize and
achieve fitness in the heat, with application of the above principles, the cramps
are resolved in 99.9% of the athletes. In addition to these resolutions and
research, I am unaware of reliable research specifically concluding that gender,
age, or BMI are associated with differences or similarities. Potentially, individual
athletes should test, experiment with resolution #'s 1-11 in order to reduce the
frequency of their cramping incidence. Sometimes the muscle will cramp in order
to balance our physiology downstream in anticipation of survival, because the
owner is driving the vehicle faster than it was trained to go.
References
1 Schwellnus MP, Derman EW, Noakes TD. Aetiology of skeletal muscle
'cramps' during exercise: a novel hypothesis. J Sports Sci. 1997 Jun;15(3):27785. Review.
2 Miles MP, Clarkson PM. Exercise-induced muscle pain, soreness, and cramps.
J Sports Med Phys Fitness. 1994 Sep;34(3):203-16. Review.
3 Bentley S. Exercise-induced muscle cramp. Proposed mechanisms and
management. Sports Med. 1996 Jun;21(6):409-20. Review.
4 Ross BH, Thomas CK. Human motor unit activity during induced muscle
cramp. Brain. 1995 Aug;118 ( Pt 4):983-93
________________________________________________________________________
______________
#5 How many calories are actually burned during exercise?
One calorie burning rate differs per athlete, gender, age, and size; hence the loss
of one calorie "does not fit all." Caloric expense rate is based on how much of the
calorie is cleaved in order to metabolize itself for use inside is called "Thermic
Calorie Deterioration." Then next the torque-transfer-efficiency by which an
individual's form and volume oxygen efficiency trade a calorie for torque transfer
to motion and how much of the calorie is lost to inefficiency motion factors such
as gravity, friction, air resistance, gear choice, lactate buildup, age, gender,
genetics, body type/BMI, etc.
To know exactly at what rate calories were burned an individual would require a
completely furnished human performance lab with the latest equipment and staff.
For methodological reasons, the method of indirect calorimetry is the most
suitable and accurate to evaluate caloric expenditure during exercise. Do not be
concerned with the amount of energy available from a given amount of energy
substrate, but with how much energy is available relative to oxygen consumption.
For carbohydrate and fat catabolism (breakdown), caloric expenses are actually
5.05 and 4.73 Kcal/Liter O2. Therefore, the difference in caloric expenditure
between pure carbohydrate and fat catabolism, of an average healthy person
exercising for 30 min at a VO2 (oxygen consumption) of 1.5 L/min, would amount
to 14.4 Kcals (227.25 Kcals carbohydrates to 212.85 Kcals fat). This is a small
difference, but indicates that for accurate calculations of caloric expenditure
during exercise, there is a need to know how much carbohydrate and fat are
being used as energy substrates. The contribution of carbohydrate and fat to
energy metabolism (the process of chemical changes to provide energy) can be
determined from the ratio between carbon dioxide production and oxygen
consumption. This is referred to as the RER, or respiratory exchange ratio of
carbon dioxide to oxygen consumption. The metabolic basis for this relationship
lies in that there is greater carbon dioxide production from carbohydrate
catabolism compared to fat catabolism. Thus, the lower the carbon dioxide
production relative to oxygen consumption, the greater the contribution of fat
catabolism to caloric expenditure.
The THERMIC EFFECT OF EACH CALORIE consumed permits 97% of each fat
calorie (8.73 calories of the original 9.0 calories/gm) to be stored or burned, 73%
of each protein calorie (2.92 calories of the original 4.0 calories/gm) to be stored
or burned, 77-92% of each carbohydrate (3.08-3.68 calories/gm) to be stored or
burned during exercise. Not all activity efficiently transfers the remaining
fractionally available CALORIE UNITS to generate torque-toward the activity. For
example you may review a complete report on energy efficiency cycling @: John
Bump's Homepage @: http://users.frii.com/katana/biketext.html
ADVANCED CALORIE CALCULATION (2)
Runner's Log for Windows and Cyclist's Log for Windows can also use a more
advanced method of estimating calories for certain activities. These formulas
also take into account your speed (pace) as a measure of your effort level. The
three activities that can use the advanced calorie estimation method are:
WEIGHT (kg) X DURATION (minutes) X SPEED(km/hour)
ACTIVITY
K/CAL RATE
LOSS
Running
0.01713324
Cycling
0.00653064
Walking
0.01330104
To determine the actual rate of your calorie expense, multiply activity calories per
kilogram bodyweight (2.2 lbs) times minutes times speed in km/hour. An example
of how the advanced estimation coefficients effect the result, imagine you make
an entry for running with the following data:
Distance: 5 miles converts to 8.047 km
Duration: 42 minutes
Weight: 150 lbs converts to 68.04 kg
Using the advanced estimation coefficient above, the program would calculate
calories as:
Pace = 5 miles X 42 minutes X 11.5 km/hour
M = 0.01713324 * (11.5 km/hour) = 0.197 calories X minute X kg
Calories = M * kg * minutes = 0.197 * 42 * 68.04 = 563 calories
Note that this is about the same number of calories that you would get with the
simpler estimation, using a fixed M value:
M (running) = 0.2 calories X minute X kg
Calories = 0.2 * 42 * 68.04 = 572 calories
ACTIVITY
SPEED
CALORIE EXPENSE FACTOR
Cycling
10-11.9 mph
0.100
Cycling
12-13.9 mph
0.133
Cycling BMX/MTB
Moderate
0.141
Cycling
14-15.9 mph
0.167
Cycling
16-19 mph
0.200
Cycling
20 mph
0.266
Running
5 mph (12 min
mile)
0.133
Running
5.2 mph (11.5
min mile)
0.150
Running
6 mph (10 min
mile)
0.167
Running
6.7 mph (9 min
0.183
mile)
Running
7 mph (8.5 min
0.191
mile)
Running
7.5mph (8 min
mile)
Running
8 mph (7.5 min
0.225
mile)
Running
8.6 mph (7 min
0.233
mile)
Running
9 mph (6.5 min
0.250
mile)
Running
10 mph (6 min
0.266
mile)
Running
10.9 mph (5.5
min mile)
0.300
Slow Pace
0.133
Aerobic Pace
0.167
0.208
Swimming Freestyle
CALORIE EXPENSE COMPARISONS
Swimming Freestyle Aerobic Pace
0.167
Cycling
0.167
14-15.9 mph
Running
6 mph (10 min 0.167
mile)
References
(1) John Bump's Homepage
http://users.frii.com/katana/biketext.html
[2] FitnessLog.Com
http://www.fitnesslogs.com/index.htm
________________________________________________________________________
_____________
#6 What guidelines preserve lean muscle mass, enhance health with
longevity implications?
1. Attaining and maintaining lean body mass is a lifetime
commitment to permanent, lifestyle strategies.
2. Ease on Down the Diet Road: Making gradual adjustments in
food, exercise and supplementation works better for long-term
weight-loss than drastic measures you cannot maintain.
3. Eat small frequent meals, well chewed, slowly eaten. Give
thanks before meals. Put your fork, spoon, or food down between
each bite.
4. Start eating early and try to get most of your calories in by 3-5
PM.
5. When hungry between meals, try 8 to 16 oz of water first.
Perhaps add fiber to the water to "fill you up".
6. Eat vegetable-based clear soups and fish frequently.
7. Create "reward meals". The key to a long-term strategy of eating
well is not having to be being perfect. Have some "planned
cheating" or a "cheat allowance" built into your strategy.
8. Always start with a sensible, balanced nutrient dense nutrition
strategy combined with exercise and supplements. Move to the
more extreme and restricted strategies only as proved necessary.
Then "cycle" or "sandwich" these more extreme strategies with a
balanced nutrient dense wide variety strategy. This way you will not
get "bored" with the more restrictive strategies, which are very
difficult to maintain for long periods of time for most of us. Don't
play the "all or nothing'" Yo-Yo diet game.
9. If obese, high sodium intake significantly increases death risk,
regardless of blood pressure. So if you are obese be moderate in
sodium from salt and additives.
10. Look in the mirror every day, preferably before or after
showering, and tell the person in the mirror you love him/her.
Regardless of your physical appearance, fatten up with self-love
the real person inside!
Reference
[1] By permission, courtesy of the author, from: 10 Success Strategies Every
Dieter Needs to Know Dr. J.H. Maher, ABAAHP, Editor, "Longevity News"
subscribe@rxforwellness.com
'Your FREE Anti-Aging Home Study Course On-Line'
More Details at: http://www.RxforWellness.com
________________________________________________________________________
______________
#7 What overover-thethe-counter
counter NSAIDS, which remarkably reduces the risk
of breast cancer?
Taking aspirin seven or more times a week reduces the risk of breast cancer by
28%, a study has found (JAMA 2004;291:2433). The drug reduced the risk of
hormone receptor positive tumors but not hormone receptor negative tumors. In
an accompanying editorial, Dr Raymond DuBois of Vanderbilt University,
Nashville, Tennessee, described the biochemical mechanism by which inhibition
of cyclooxygenase by aspirin could result in lower concentrations of estrogen
(JAMA 2004;291:2488-9).
The retrospective, case controlled study looked at women who had new
diagnoses of invasive breast cancer or breast cancer in situ from 1 August 1996
to 31 July 1997 in the Long Island breast cancer study project. The study
examined the high rate of breast cancer in this mostly middle class area within
125 miles of New York city. Research had already identified local risk factors as
lower parity, late age at first birth, little or no breast feeding, and a family history
of breast cancer. A total of 1508 women with breast cancer and 1556 control
patients were interviewed. Most women were white. The women were asked if
they had taken aspirin once a week for more than six months. If so, they were
asked how often and how many tablets a week they took in the two to five years
up to one year before their diagnosis of breast cancer. Women in the control
group were asked about use up to one year before their interview. Both groups
were asked about use of ibuprofen and also of paracetamol, an analgesic and
antipyretic rather than a non-steroidal anti-inflammatory drug. The study did not
look at dosages or whether the women used coated or uncoated aspirin.
The lead author, Mary Beth Terry, assistant professor of epidemiology at the
Mailman School of Public Health at Columbia University, New York, said the
group looked at recent aspirin use. “In studies of ‘former users’—women who
used it five or more years ago—it didn’t seem to have any protective effect,” she
said. Laboratory studies indicate that aspirin inhibits synthesis of prostaglandin,
which in turn inhibits estrogen production in the breast. She said that women who
used aspirin regularly—seven or more times a week—had a 28% reduction in
risk (odds ratio 0.72 (95% confidence interval 0.58 to 0.90)). Less frequent users
had only a 5% reduction, which was not statistically significant. Women who took
ibuprofen also had a lower risk of breast cancer than control patients, but the
reduction was less than in women taking aspirin. Paracetamol had no effect.
Aspirin reduced the risk of breast cancer in premenopausal women and
postmenopausal women, but the effect was more pronounced in
postmenopausal women because there were more of them in the study. If further
studies confirm that aspirin reduces breast cancer risk, women would need to
continue taking it regularly. “Frequent use would be predicted to lead to a steadystate reduction in intramammary estrogen and thereby reduce the risk of breast
cancer,” the authors write. “Aspirin has side effects, and so do other drugs such
as tamoxifen for breast cancer prevention. If we figure out the mechanism of
action, we might develop a combination that gets maximum benefits and minimal
side effects,” Dr Terry said [1].
COMMENT: When are we going to establish standard-of-care practices to
measure pre-menopausal female hormone levels as a preventative-screening
device to confirm or treat imbalances in circulatory estrogen, testosterone,
progesterone, cortisol, and DHEA? Do we not yet know that too much, too little,
or imbalances in the hormone profile are likely to increase the risk of disease? A
number of aromatizing compounds are available PO, SC, I.M., S/L, or Buc to
reduce or neutralize hormone disorders. And now, alas, female patients outside
access to the cutting edge of medical science are unknowingly successfully
medicating with regular aspirin dose and reducing intramammary estrogen and
thereby reducing their risk of breast cancer. Is this an oversimplified message we
are not hearing? May I repeat the question, When are we going to institute
routine screening of blood labs in order to treat symptomatic or out-of-balance
pre- and post- menopausal hormone profiles [2]?
STEROID HORMONE
BIOSYNTHESIS REACTIONS4
The particular steroid hormone class synthesized by a given cell type
depends upon its complement of peptide hormone receptors, its response to
peptide hormone stimulation and its genetically expressed complement of
enzymes. The following indicates which peptide hormone is responsible for
stimulating the synthesis of a steroid hormone:
Luteinizing Hormone (LH):
!!!!!
progesterone - testosterone
FOLLICLE STIMULATING HORMONE (FSH):
!!!!!
ESTRADIOL
Angiotensin II/III:
!!!!!
Aldosterone
Adrenocorticotropic Hormone (ACTH):
!!!!!
Cortisol
Testosterone is also produced by Sertoli cells but in these cells it is regulated by FSH,
again acting through a cAMP- and PKA-regulatory pathway. In addition, FSH stimulates
Sertoli cells to secrete androgen-binding protein (ABP), which transports testosterone
and DHT from Leydig cells to sites of spermatogenesis. There, testosterone acts to
stimulate protein synthesis and sperm development.
In females, LH binds to thecal cells of the ovary, where it stimulates the synthesis of
androstenedione and testosterone by the usual cAMP- and PKA-regulated pathway. An
additional enzyme complex known as aromatase is responsible for the final
conversion of the latter 2 molecules into the estrogens. Aromatase is a complex
endoplasmic reticulum enzyme found in the ovary and in numerous other tissues in both
4
By permission, courtesy of Professor Michael W. King, Ph.D., Indiana University School of
Medicine @: http://web.indstate.edu/thcme/mwking/steroid-hormones.html
males and females. Its action involves hydroxylations and dehydrations that culminate in
aromatization of the A ring of the androgens.
Synthesis of the major female sex hormones in the ovary. Synthesis of testosterone and
androstenedione from cholesterol occurs by the same pathways as indicated for synthesis of the male
sex hormones.
AROMATASE ACTIVITY is also found in granulosa cells, but in these cells the
activity is stimulated by FSH. Normally, thecal cell androgens produced in response to
LH diffuse to granulosa cells, where granulosa cell aromatase converts these androgens
to ESTROGENS. As granulosa cells mature they develop competent large numbers of
LH receptors in the plasma membrane and become increasingly responsive to LH,
increasing the quantity of estrogen produced from these cells. Granulosa cell estrogens
are largely, if not all, secreted into follicular fluid. Thecal cell estrogens are secreted
largely into the circulation, where they are delivered to target tissue by the same globulin
(GBG) used to transport testosterone.
HORMONE LEVELS DURING FEMALE MENSTRUAL
CYCLE5
MALE HORMONE PROFILE AGE CHANGE
30
25
20
Testosterone
Estrogen
15
10
5
0
20-39 40-49 50-59 60-69 70-79
80+
Male Hormone Change By Decade: Testosterone ! & Estrogen "
5
By permission, courtesy of Professor Robert Huskey, Professor Emeritus Biology, University of Virginia,
http://www.biologie.uni-hamburg.de/b-online/library/bio201/bio201.html
Is estrogen a PROBLEM HORMONE operant in male prostate and female breast
cancer?6
Estrogen Linked to Breast Cancer
Estrogen Linked to Breast Cancer. Weight-Related Increases in Breast Cancer Risk Linked to
Estrogen Levels @ http://my.webmd.com/content/article/72/81799.htm
National Cancer Institute - What You Need To Know About Breast ...
High levels of estrogen may be the reason that obese women have an increased risk of breast
cancer @: http://www.nci.nih.gov/cancerinfo/wyntk/breast
Q & A on Hormone Replacement Therapy and Breast Cancer Risk
These studies indicate a slightly higher risk for breast cancer in some subgroups of women on
combined estrogen/progestin therapy than women on unopposed .
http://www.amwa-doc.org/healthtopics/hrt_breastcancer_qa.htm
Estrogen Dominance Linked to Cancer
Dr Lee published two studies in the American Journal of Pathology in 1999 that SHOW ESTROGEN
INCREASES BREAST AND PROSTATE CANCER
http://www.natural-progesterone-advisory-network.com/ estrogen-dominance-linked-to-cancer.htm
References
[1] Daily aspirin reduces risk of breast cancer, study finds, Janice Hopkins Tanne
@ BMJ 2004;328:1336 (5 June), doi:10.1136/bmj.328.7452.1336-c
[2] Breast Cancer Hormone Profile: Is there a simple answer in plain view?
Bill D. Misner Ph.D. (4 June 2004)
http://bmj.bmjjournals.com/cgi/eletters/328/7452/1336-c
________________________________________________________________________
______________
#8 Why
Why is folate so important a companion to vitamin BB-12 for optimal
lean muscle mass synthesis, cardiovascular markers, and red blood cell
volume?
Lucy Wills once described how yeast extract could be effective in preventing
tropical macrocytic anaemia of late pregnancy. Folate was later shown to be the
crucial factor. Then in 1995 came a meta-analysis that established that high
homocysteine concentrations were a risk factor for atherosclerosis. Dietary folate
reduces homocysteine, raising the possibility that a vitamin might prevent
vascular disease. In the 1980's, a series of studies showed how periconceptional
6
Estrogen may be a problem for both males and females if it is out of balance with other hormones,
may interrupt healthy breast and prostate cell health, resulting in cancer.
folate could prevent spina bifida. Next, several nucleotide polymorphisms were
found to be related to folate, meaning that folate levels might influence the
chance of developing cancer.
These discoveries are not surprising as folate metabolism is involved in many of
the fundamental processes of life. Nucleotide Biosynthesis is directly dependant
upon Thymidylate synthase, an enzyme that helps synthesize DNA, which is a
derivative of folate. Low levels of folate may thus lead to breaks in DNA,
predisposing the hypo-folate athlete to performance inhibition, fatigue,
impoverished RBC markers, elevated homocycsteine, cardiovascular disease
and cancer. There are many other ways in which folate can affect gene function;
folate is is absolutely central to nutrigenomics—the study of the links between
nutrition and gene function [1].
DIETARY FOLATE
THYMIDYLATE SYNTHASE
SYNTHESIS
DNA
COMMENT: I enthusiastically recommend Folate + Vitamin B-12 as a
methylating substrates for not only cardiovascular anti-homocysteine health and
for the downstream DNA activities in recovering over-exercised muscle fibers.
Without folate's donor potential promoting Thymidylate Synthase activity,
downstream DNA strands vulnerable to error ...Every 180 days the body's
complex RNA
DNA sequence deliver 98% of all soft tissue cells anew. This
assumes that all the required substances are available, in place on a daily basis.
Reference
BMJ Editorial, Richard Smith, Editor's choice: "Let food be thy medicine..." BMJ
2004;328 (24 January), doi:10.1136/bmj.328.7433.0-g</x-rich>
________________________________________________________________________
______________
#9 What foods block the progression of colorectal cancer and why
should endurance athletes be so concerned about reducing this risk?
Epidemiological evidence indicates that Brassica vegetables protect against
colorectal cancer. Brassicas contain glucosinolates, the breakdown products of
which exert antiproliferative effects against cancer cells. Researchers [1]
examined the effects of allyl isothiocyanate, a major breakdown product of the
glucosinolate sinigrin, on proliferation and death of colorectal cancer cells. HT-29
colorectal cells were exposed to allyl isothiocyanate for 24 hours and the number
of adherent and detached cells determined. Both populations were analyzed for
cell cycle characteristics and examined by light and electron microscopy for
features of apoptosis and mitosis. Evidence of apoptosis was also determined by
flow cytometric analysis of Annexin V staining in the detached population of cells.
Allyl isothiocyanate-treated cells were also stained for alpha tubulin. Treatment
caused cells to round up after 7 hours of exposure and subsequently detach. At
24 hours these cells were blocked in mitosis. Detached AITC treated cells
showed no signs of apoptosis as assessed by morphological features or by
Annexin V staining but they did show evidence of disrupted tubulin. Allyl
isothiocyanate inhibits proliferation of cancer cells by causing mitotic block
associated with disruption of alpha-tubulin in a manner analogous to a number of
chemotherapeutic agents.
COMMENT: Endurance athletics generates a high turnover of food fuels through
the gut, the liver, then on to the muscles where energy is released. If a food fuel
contains a single harmful cancer-inducing substance, having this preventative
substrate present immediately neutralizes the potential outcome of cancer in the
gut, prostate, breasts, lymph, liver, brain, bone or even in bloodstream. What
foods are rich in allyl isothiocyanate (AI)? Cruciferous brassica vegetables
broccoli, cabbage, brussels sprouts, and cauliflower contain plenty of cancerblocking AI! I also recommend 2 supplements, IndoleIndole-3-Carbinal and
Diindolymethane for reducing the risk of cancer.
IndoleIndole-3-Carbinol may help to prevent Prostate Cancer (by modulating the effects
of Estrogens in Aryl Hydrocarbon Receptors in Prostate cells).
IndoleIndole-3-Carbinol helps to prevent Breast Cancer by stimulating the conversion
of Estrone (the Estrogen which is known to cause Breast Cancer in excess)
excess) to its
inactive form, 2-Hydroxyestrone.
Diindolylmethane inhibits the conversion of Estrone to its carcinogenic metabolite
- 16-Hydroxyestrone; and redirects Estrone to be converted to its safe inactive
metabolite - 2-Hydroxyestrone. Like Indole-3-Carbinol, Diindolymethane's
antiestrogen effect helps to prevent both breast cancer and prostate cancers
caused by excess 16-Hyroxyestrone levels in females or aging males.
[1] Allyl isothiocyanate causes mitotic block, loss of cell adhesion and disrupted
cytoskeletal structure in HT29 cells. Smith, T. K., Lund, E. K., Parker, M. L.,
Clarke, R. G., Johnson, I. T., Carcinogenesis 2004 Mar 19.
________________________________________________________________________
______________
#10 What's wrong with drinking alcohol
alcohol after a workout?
I blame the media for supporting of alcohol consumption by touting partial
research reporting favorable consequences. The whole picture from the sciencemethod view is both unclear and inconclusive. Some may drink moderately with
no observed harm to health reporting beneficial aspects, while we do not know
what would have resulted if they had not consumed alcohol from a
cardiovascular health perspectus. I conclude that consumption of alcohol does
not contribute to cardiovascular health based on what substances benefit human
striated or non-striated muscle synthesis benefit cardiovascular health. Clearly,
alcohol detracts from optimal training-induced muscle synthesis in endurance
athletes, hence it should be questioned as to its benefit for cardiovascular health
outcome. Only the food groups vegetables, fruits, and fish have been associated
with cardiovascular health.In Milk and Other Dietary Influences on Coronary
Heart Disease by William B. Grant, Ph.D. Alt Med Review - Volume 3, Number 4,
August 1998, @: http://www.thorne.com/altmedrev/fulltext/milk3-4.html
RATIONALE AGAINST CONSUMING ALCOHOL
Heavy drinking appears to increase the risk of hemorrhagic stroke, in part due to
hypertension, and to increase the risk of sudden death, which was probably due
to drinking per se. Light or moderate alcohol consumption seemed to protect
against nonhemorrhagic stroke and coronary heart disease [1]. Light-to-moderate
alcohol consumption reduces the overall risk of stroke and the risk of ischemic
stroke in men. The benefit is apparent with as little as one drink per week.
Greater consumption, up to one drink per day, does not increase the observed
benefit [2].
An elevated risk of ischemic stroke was found for men who drank infrequently,
that is, a few times a year or less often (RR, 2.0; 95% confidence interval [CI],
1.3 to 3.2), for those who were intoxicated now and then (RR, 1.8; 95% CI, 1.1 to
2.8), and for those who reported "binge" drinking a few times in the year or less
often (RR, 1.6; 95% CI, 1.1 to 2.5). Among women only ex-drinkers had an
elevated risk of dying of ischemic stroke (RR, 3.3; 95% CI, 1.5 to 7.2). The risk
was reduced for women who had an estimated average consumption of 0 to 5 g
pure alcohol per day (RR, 0.6; 95% CI, 0.5 to 0.8); for those who did not drink
every day (RR, 0.7; 95% CI, 0.5 to 0.9); and for those who never "went on a
binge" (RR, 0.6; 95% CI, 0.5 to 0.8) or became intoxicated (RR, 0.7; 95% CI, 0.5
to 0.9). Drinking habits were associated only with deaths from ischemic stroke,
and the risk patterns were different for men and women. In analyses, ex-drinkers
should not be included with lifelong
abstainers, since the former tend to run high health risk [3].
ALCOHOL INHIBITS POSTPOST-EXERCISE MUSCLE GROWTH
Even moderate short-term alcohol inhibits muscle protein synthesis [4]. This
effect is particularly pronounced in fast muscle fibers. Alcohol is detrimental,
dose-dependant for any athlete trying to gain muscle mass and strength. The
goal of training is to increase the rate of muscle protein synthesis. Seeing what
happens to those who abuse alcohol should influence endurance athletes during
training to abstain from alcohol. It is well established that many patients with
ethanol alcohol-induced cirrhosis, suffer muscle wasting syndrome from reduced
rate of protein synthesis. Alcoholic myopathy, or weakness secondary to
breakdown of muscle tissue, is known as alcoholic rhabdomyolysis or alcoholic
myoglobinuria. Males are affected by acute (sudden onset) alcoholic myopathy 4
times more often than females. Breakdown of muscle tissue (myonecrosis), can
come on suddenly during binge drinking or in the first days of alcohol withdrawal.
In its mildest form, muscle breakdown creates no noticeable symptoms, but may
be detected by a temporary elevation in blood levels of an enzyme (MM fraction
of creatine kinase) found predominantly in muscle. Proportionate to alcohol dose
and frequency consumed may calculate in terms of a consequent loss in strength
gain. Decreased strength loss stimulates increased fatigue rate originating from
the histological reduced type II fibers [fast twitch] in skeletal muscle, typical of an
alcoholic myopathy. Human Growth Hormone (otherwise released during
exercise) is neutralized by blood alcohol. Alcohol dehydrates muscle cell tissue
further reducing anabolic activity. Dehydrated cells cannot build muscles as fast
as hydrated muscle cells. Alcohol severely reduces the absorption of many
important nutrients key for both muscle growth and contractile torque output.
Studies indicate that alcoholic patients suffering from alcohol myopathy present
inhibited protein synthesis profile. By definition, these patients present wasting
syndrome from loss of muscle mass proportionate to alcohol consumption dose
and duration.
The high calorie content of alcohol imposes a negative effect on total calorie
intake, causing metabolism to slow down by disrupting the efficiency of the
Kreb's cycle. Since the Kreb's cycle isn't working correctly, fats are not efficiently
broken down. The body becomes so concerned with digesting and metabolizing
alcohol, that fat-burning and protein synthesis are lowered by as much as 20%.
This does not suggest an endurance athlete will waste away like an alcoholic, but
it is observed that impaired muscle mass gains will be diminished proportionate
to frequency and dose.
ALCOHOL IS AN ERGOGENIC PERFORMANCE INHIBITOR
Hormonal research concludes that optimal performance is reduced hence alcohol
is not an ergogenic [5]. It was concluded that consumption of ethanol [alcohol]
adversely influences treadmill exercise performance eliciting a hypoglycemic
effect between 30 minutes and termination of exercise [6]. Another paper
reported that acute alcohol administration affects the hypothalamic-pituitary axis
by reducing serum LH levels, an effect representative of alcohol's influence on
the hypothalamic-pituitary-gonadatropin [HPG]. Researchers indicate that alcohol
depresses serum testosterone levels and, thereby, produces clinical symptoms
associated with hypoandrogenization [7, 8]. The bottom line in optimizing
performance from a nutritional prospectus is avoid alcohol consumption during
peak training efforts for big dividends at the finish line.
Ethanol Metabolism7
Ethanol (EtOH) + NAD+ → acetaldehyde + NADH + H+ catalyzed by ADH
Metabolism of EtOH increases cytosolic load of NADH this drives the
LDH and MDH reaction in the direction of lactate and malate
production, respectively. Both of these results severely impairs the capacity
of the liver to carry out gluconeogenesis. Acetaldehyde enters the
mitochondria where it is oxidized to acetate, which also produces
NADH. The net effect in the mitochondrion is an inhibition of the TCA
cycle, this leads to reduced oxidation of fatty acids, which are then
diverted to TRIACYLGLYCEROL production - hyperlipidemia results as
well as fatty liver. At very high intake levels, EtOH is also oxidized by
the MEOS of the ER. This pathway results in NADPH and O2
consumption without being coupled to energy production.
Animal cells (primarily hepatocytes) contain the cytosolic enzyme alcohol
dehydrogenase (ADH), which oxidizes ethanol to acetaldehyde. Acetaldehyde then
enters the mitochondria where it is oxidized to acetate by acetaldehyde dehydrogenase
(AcDH).
7
By permission, courtesy of Professor Michael W. King, Ph.D., Indiana University School of
Medicine @: http://web.indstate.edu/thcme/mwking/glycolysis.html#ethanol
Acetaldehyde forms adducts with proteins, nucleic acids and other compounds, the
results of which are the toxic side effects (the hangover) that are associated with
alcohol consumption. The ADH and AcDH catalyzed reactions also leads to the
reduction of NAD+ to NADH. The metabolic effects of ethanol intoxication stem
from the actions of ADH and AcDH and the resultant cellular imbalance in the
NADH/NAD+. The NADH produced in the cytosol by ADH must be reduced back to
NAD+ via either the malate-aspartate shuttle or the glycerol-phosphate shuttle.
Thus, the ability of an individual to metabolize ethanol is dependent upon the
capacity of hepatocytes to carry out eother of these 2 shuttles, which in turn is
affected by the rate of the TCA cycle in the mitochondria whose rate of function is
being impacted by the NADH produced by the AcDH reaction. The reduction in
NAD+ impairs the flux of glucose through glycolysis at the glyceraldehyde-3phosphate dehydrogenase reaction, thereby limiting energy production. Additionally,
there is an increased rate of hepatic lactate production due to the effect of increased
NADH on direction of the hepatic lactate dehydrogenase (LDH) reaction. This
reverseral of the LDH reaction in hepatocytes diverts pyruvate from
gluconeogenesis leading to a reduction in the capacity of the liver to deliver glucose
to the blood.
In addition to the negative effects of the altered NADH/NAD+ ratio on hepatic
gluconeogenesis, fatty acid oxidation is also reduced, as this process requires NAD+
as a cofactor. In fact the opposite is true, fatty acid synthesis is increased and there
is an increase in triacylglyceride production by the liver. In the mitocondria, the
production of acetate from acetaldehyde leads to increased levels of acetyl-CoA.
Since the increased generation of NADH also reduces the activity of the TCA cycle,
the acetyl-CoA is diverted to fatty acid synthesis. The reduction in cytosolic NAD+
leads to reduced activity of glycerol-3-phosphate dehydrogenase (in the glcerol 3phosphate to DHAP direction) resulting in increased levels of glycerol 3-phosphate,
which is the backbone for the synthesis of the triacylglycerides. Both of these two
events lead to fatty acid deposition in the liver leading to fatty liver syndrome.
COMMENTS: In my opinion the effects from a 7-calorie sugar alcohol solution in
human metabolism is not healthy because it is an unpredictable unnatural calorie
source. The initial reaction of the human body to alcohol should tell the consumer
that such a substance, which creates an unnatural blood sugar response,
metabolic depression, dehydration, and dramatic changes in systemic waste
removal that the substance is being rejected as a survival mechanism. Any and
all systemic rejected substances need to be considered as a challenge to optimal
health.As implied, I see no need to include the alcohol calorie in the human food
chain especially when concern for optimal cardiovascular health is discussed
based on the facts.
REFERENCES
[1] Stroke. 1995 May;26(5):767-73.
[2] N Engl J Med. 1999 Nov 18;341(21):1557-64.
[3] Stroke. 1995 Oct;26(10):1768-73.
[1] Med Sci Sports Exerc 1996 Aug;28(8):1063-70.
[2] Br J Sports Med 1986 Jun;20(2):56-9.
[3] Int J Clin Pharmacol Ther 1994 Oct;32(10):536-41.
[4] Alcohol Clin Exp Res 1978 Jul;2(3):249-54.
[5] Pharmacol Exp Ther 1977 May;201(2):427-33.
=============================================================
================
industry
ry grant from EThe Journal of Endurance is funded by a private indust
E-CAPS &
HAMMER NUTRITION, whose product applications are referenced in articles #
(listed above):
#3 Hammer Whey Pro and a new post-exercise recovery formula for endurance
athletes, Recoverite (coming soon)
#4 Endurolytes (2-6 each) combined with 20-28 fluid ounces water and 240-280
calories each hour in divided dose. The caloric requirement is well-supported by
using one of the following:
HAMMER GEL
SUSTAINED ENERGY
PERPETUEM
HEED
i
By permission, courtesy of Professor Farrabee, Online Biology Book hosted by Estrella Mountain
Community College @ http://www.emc.maricopa.edu/faculty/farabee/BIOBK/BioBookTOC.html
All issues of J.O.E. are the property of E-Caps/Hammer Nutrition and may only be reprinted if they are
unaltered and proper credit is given, including web site url. However, please feel free to forward this or any
other issue to your friends. An explanation or rationale for each question is presented, though this is largely
a personal interpretation.