acsm's certified - ACSM Certification
advertisement

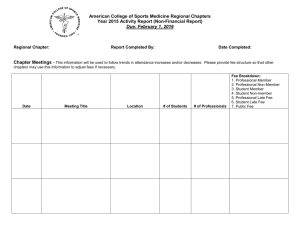
ACSM’S CERTIFIED NEWS S E C O N D Q U A R T E R 2 0 1 4 • V O L U M E 2 4 : I S S U E 2 The Exercise is Medicine Professional Credential: A Trusted Community-based Resource for Health Care ® Page 2 Issues for Clinical Exercise Physiologists Part I: Resistive Exercise Testing in Pulmonary Rehabilitation Page 3 Part 2: Suggested Lifestyle Interventions for Sarcopenic Obesity Page 4 Circuit Strength Training Page 6 Coaching News The Gallon Jug Shelf Test: An Assessment of Moderately Heavy Object Transfer Page 9 Online Tips and Tools for Exercise Professionals Page 10 Thinkstock Images/Stockbyte/Thinkstock Page 8 ACSM’S CERTIFIED NEWS Second Quarter 2014 • Volume 24, Issue 2 In This Issue The Exercise is Medicine® Professional Credential A Trusted Community-based Resource for Health Care........2 Issues for Clinical Exercise Physiologists Part I: Resistive Exercise Testing in Pulmonary Rehabilitation......................3 Part 2: Suggested Lifestyle Interventions for Sarcopenic Obesity.....................................................4 Circuit Strength Training..................................................6 Coaching News...........................................................8 The Gallon Jug Shelf Test: An Assessment of Moderately Heavy Object Transfer..................................9 The Exercise is Medicine Professional Credential ® A trusted communitybased resource for health care Online Tips and Tools for Exercise Professionals.................10 Co-Editors Peter Magyari, Ph.D. Peter Ronai, M.S., FACSM Committee on Certification and Registry Boards Chair William Simpson, Ph.D., FACSM CCRB Publications Subcommittee Chair Gregory Dwyer, Ph.D., FACSM ACSM National Center Certified News Staff National Director of Certification and Registry Programs Richard Cotton Assistant Director of Certification Traci Sue Rush Certification Coordinator Kela Webster Publications Manager David Brewer Editorial Services Lori Tish Barbara Bennett Editorial Board Chris Berger, Ph.D., CSCS Clinton Brawner, M.S., FACSM James Churilla, Ph.D., MPH, FACSM Ted Dreisinger, Ph.D., FACSM Avery Faigenbaum, Ed.D., FACSM Riggs Klika, Ph.D., FACSM Tom LaFontaine, Ed.D., FACSM Thomas Mahady, M.S. Maria Urso, Ph.D. David Verrill, M.S. Stella Volpe, Ph.D., FACSM Jan Wallace, Ph.D. For More Certification Resources Contact the ACSM Certification Resource Center 1-800-486-5643 Information for Subscribers Correspondence Regarding Editorial Content Should be Addressed to: Certification & Registry Department E-mail: certification@acsm.org Tel.: (317) 637-9200, ext. 115. For Back Issues and Author Guidelines Visit: certification.acsm.org/certified-news ACSM’s Certified News (ISSN# 1056-9677) is published quarterly by the American College of Sports Medicine Committee on Certification and Registry Boards (CCRB). All issues are published electronically and in print. The articles published in ACSM’s Certified News have been carefully reviewed, but have not been submitted for consideration as, and therefore are not, official pronouncements, policies, statements, or opinions of ACSM. Information published in ACSM’s Certified News is not necessarily the position of the American College of Sports Medicine or the Committee on Certification and Registry Boards. The purpose of the publication is to provide continuing education materials to the certified exercise and health professional and to inform these individuals about activities of ACSM and their profession. Information presented here is not intended to be information supplemental to ACSM’s Guidelines for Exercise Testing and Prescription or the established positions of ACSM. ACSM’s Certified News is copyrighted by the American College of Sports Medicine. No portion(s) of the work(s) may be reproduced without written consent from the publisher. Permission to reproduce copies of articles for noncommercial use may be obtained from the Certification Department. E xercise is Medicine® (EIM) is a global health initiative to establish physical activity as a standard in health care. Launched in 2007 as a joint effort by ACSM and the American Medical Association, EIM has evolved to a boots-on-the-ground initiative. Leading the way are fitness professionals who seek to elevate their careers by positively impacting the health of those who lack physical activity and require chronic disease prevention and management. These professionals are the credentialed EIM professionals. More at-risk individuals are entering the health care system who are sedentary, obese, and suffer with chronic diseases. In response, health care is adopting the Population Health Management (PHM) care model to identify at-risk individuals into population groups. PHM is a proactive application of strategies and interventions to defined at-risk population groups in an effort to improve the health of the individuals within the group. EIM professionals fill the role of applying engagement strategies for participation in physical activity (PA) intervention programs. The credentialing process includes EIM study materials on the EIM solution for health care, behavioral modification strategies, and chronic condition management. The study materials are available online and also are accessible through onsite workshops. The exam for credentialing is available through PearsonVUE testing centers and can be proctored at convenient locations across the country. After credentialing, EIM professionals working within the EIM Solution will be trained to receive health care referrals, maintain engagement, and deliver PA intervention programs. Structured physical activity, health education, and lifestyle behavioral change strategies are delivered as “move and learn” sessions designed to address population-specific barriers with credible engagement strategies for retention. EIM professionals are building a bridge of trust between clinical health care and nonclinical health care resources in the community. This trust building provides referrals to EIM professionals from health care potentially at every level: providers, payers, and community outreach. This means that patients, employees, eligibles, beneficiaries, and underserved community residents can be referred to EIM professionals. For more information about the prerequisites and procedures to become a trusted community-based resource for health care as a credentialed EIM professional, go to: acsmcertification.org/exercise-is-medicine-credential Phil Trotter, Exercise is Medicine® Community Solution Development Email: ptrotter@acsm.org ACSM National Center 401 West Michigan St., Indianapolis, IN 46202-3233 Tel.: (317) 637-9200 • Fax: (317) 634-7817 ©2014 American College of Sports Medicine. ISSN # 1056-9677 2 ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 Clinical Article ISSUES FOR CLINICAL EXERCISE PHYSIOLOGISTS PART I: RESISTIVE EXERCISE TESTING IN PULMONARY REHABILITATION By Dave Verrill, MS, RCEP, PD, CES, FAACVPR (This is the first in a two-part series of resistive exercise testing and training in pulmonary rehabilitation). Introduction C hronic obstructive pulmonary disease (COPD) is currently the fourth leading cause of death in the United States and projected to be the third leading cause of death by 20201. Participation in pulmonary rehabilitation (PR) is essential for patients with chronic lung disease to help them perform their activities of daily living (ADLs) most effectively and improve their overall quality of life (QOL)1-4. Developing and maintaining overall body muscular strength and endurance is critical for the pulmonary patient due to the muscle atrophy and weakness that often accompany both COPD and restrictive lung disease. The Joint ACCP/AACVPR Evidence Based Clinical Guidelines4 state that the addition of a strength training component in PR increases both muscular strength and muscle mass with a strength of evidence rating of 1A (high). The ever-increasing pool of research in this area shows multiple benefits for the pulmonary patient following resistive exercise training (RET). Studies now show that even heavier or more vigorous resistive exercise is safe and produces positive outcomes in pulmonary patients up to 80 years of age5. Thus, every PR program should incorporate some form of formal resistive exercise training for its patients with chronic lung disease. The clinical exercise physiologist (CEP) in PR must be able to design, develop, and supervise the resistive exercise component with documentation of individual strength improvements over time for exercise prescription modifications and patient outcomes6. While studies have shown that RET is highly beneficial for the pulmonary patient, many PR programs do not offer a structured resistive training period devoted solely to this modality. This is often due to the time limitations of PR sessions (typically 50 to 70 minutes) or the lack of funds for purchase of resistive exercise equipment. Practitioners in PR also may be concerned about potential medical complications that could occur with RET. The major focus of PR has traditionally been aerobic exercise training, breathing retraining, patient education, and relaxation training. Thus, with all of these necessary pulmonary interventions, RET often gets put on the “back burner” in the PR session. Nevertheless, with the advent of recent RET studies that show this form of exercise to be both safe and highly beneficial for the pulmonary patient, it is now more important than ever for the CEP to develop and incorporate structured RET protocols into their PR policies and procedures for daily program operation. Musculoskeletal Changes Associated With Lung Disease Chronic lung disease causes dramatic and detrimental deterioration to human skeletal muscle tissue. Muscle atrophy and weakness resulting from prolonged hypoxia and/or hypercapnia may decrease myofibrillar mass, mitochondrial density, and muscle fiber capillarization. The end-result of this disease-induced myopathy often includes the following adverse side-effects: 1,4,5,7 • impaired exercise tolerance • peripheral muscular atrophy • weakened thoracic muscles that impair breathing ability • a decrease in Type I (fatigue resistant) muscle fibers • altered muscle enzyme levels • muscle tendon rupture • muscle tears and strains Steroid-induced myopathy and bone degeneration are also common in the pulmonary patient, as the patient is often prescribed steroidal medications to help reduce lung inflammation for extended periods of time. This type of therapy may further exacerbate any of the above conditions, as well as decrease the patient’s overall energy expenditure, basal metabolic rate, muscular strength, bone density, breathing abilities, and daily activity levels. Risk of falls and becoming injured from these adverse changes often leads to sedentary living and further disability for the pulmonary patient. Thus, it is up to the CEP to incorporate specific strength training regimens that are individualized for their patients, based upon individual needs, to help alleviate this chronic vicious cycle of muscle and bone degeneration and disability. Research Findings on the Effects of Resistive Exercise Training in COPD While many recent investigations have conducted whole-body resistive training protocols in patients with COPD, much more research needs to be conducted in both men and women with varying types of chronic lung diseases. Current findings show that resistive training protocols using both free and machine weights can increase the pulmonary patient’s upper and lower body strength from 8% to 140%7-13, ADLs4,11, and QOL7. A mild improvement in cardiovascular endurance also has been observed with research protocols that combine resistive exercise with lower body aerobic training10,12,13. The aforementioned resistive training studies (and similar investigations) have not presented or discussed any significant cardiopulmonary or orthopedic complications within experimental study groups, thus providing further evidence that resistive exercise training is indeed a very safe modality in PR programs if performed correctly under the Resistive Exercise Testing (continued on page 11) ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 3 Clinical Feature Part 2: Suggested Lifestyle Interventions for Sarcopenic Obesity By Elizabeth O’Neill and Richard Wood I. Introduction A s exercise science professionals, it is important that we are familiar with the challenges associated with aging. As presented in Sarcopenic Obesity Part 1: Definitions and Consequences, sarcopenic obesity was identified as a complex condition involving the age-related changes in body composition: increases in fat mass with a concomitant loss of muscle mass26. Evidence and concern are mounting regarding sarcopenic obesity and its associated complications: decreased muscle quality, functional limitations, and increased inflammation. Thus, as sarcopenic obesity threatens the health and functional ability of older adults, there is a need for evidence-based interventions and recommendations for treatment. This second and final article is designed to examine the challenges in treating sarcopenic obesity and the potential lifestyle interventions that can address the consequences of sarcopenic obesity. II. Challenges Associated with Treatment Approximately 32% of people age 65 and older are classified as obese, utilizing Body Mass Index (BMI) criterion2. The typical course of action for treating obesity involves weight-loss therapy. However, traditional methods of inducing weight loss in older adults also may increase the loss of muscle mass and increase frailty. This approach is counterproductive when trying to avoid exacerbating sarcopenia. Therefore, treating sarcopenic obesity becomes more complex than trying to treat each condition independent of the other. Suggested lifestyle interventions must not only address weight loss, but also must function to maintain or even increase muscle mass in order to reduce sarcopenic processes. The following section contains three sub-sections: nutritional recommendations, diet and exercise interventions, and exercise considerations. III. Lifestyle Interventions Nutritional Recommendations The loss of muscle mass associated with aging (sarcopenia) is of concern due to the subsequent consequences to functional ability and poor muscle quality. While many factors are thought to contribute to sarcopenia, insufficient protein intake is frequently recognized as an important variable4,8. The Institute of Medicine’s Food and Nutrition Board established the recommended dietary allowances (RDA) for protein (0.8g/kg/day) based on nitrogen balance studies utilizing younger populations14-15. Some researchers suggest that the nitrogen balance studies and subsequent RDA for protein may not accurately reflect the need for muscle preservation with aging and, therefore, may be inadequate for older adults4,8,18. Some of the most convincing findings regarding protein requirements for older adults have been documented in longitudinal studies. These studies have consistently found significant asso- 4 ciations between protein consumption and maintenance of lean mass. The Health ABC study examined the protein intakes of community-dwelling older adults (n = 2066; ages 70-79)8. Subjects in the higher quintile of protein intake (1.1g/kg/day) lost 43% less total lean mass and 39% less appendicular lean mass (aLM) compared to subjects in the lowest quintile for protein intake (0.7g/kg/day) over the period of 3 years. Meng et al.11 and Scott et al.18 found similar results to The Health ABC study. Meng et al. determined whole body lean mass, aLM, and upper arm muscle mass area were maintained better by subjects (n = 862 females; 75 + 3 yoa) in the highest tertile of protein intake over a 5-year period. Additionally, protein was found to have the strongest relationship to whole body lean mass compared to other macronutrients (fat or carbohydrate). Scott also reported a positive association between protein intake and aLM in older adults (n = 740; 62 + 7 yoa). Subjects failing to meet the recommended dietary intake for protein at baseline (12%) and at the follow-up (14%) had significantly lower aLM. Scott concluded that protein intake was a positive predictor of aLM changes over the course of the 2.6-year study and suggested that age-associated loss of muscle may be reduced with higher protein intake. These and other studies have led researchers to suggest that higher protein RDA ranging between 1.0 and 1.5 g/kg may be more appropriate to address sarcopenia13. Additional guidelines have been proposed regarding the amount of protein per meal to optimize anabolic efficiency. Symons et al.19 examined the protein synthesis when manipulating the amount of protein consumed (30g versus 90g) in a single serving. The 30g serving was found to be as effective for protein synthesis as was the 90g serving. Thus, Paddon-Jones and Rasmussen suggest that consumption of high-quality protein equaling 25g to 30g per meal should be utilized to optimize protein synthesis15. Diet and Exercise Several weight-loss studies have been conducted utilizing an older adult population, which has helped provide practitioners insight regarding the most effective interventions for addressing sarcopenic obesity. Most of these studies incorporate caloric restriction, exercise, or caloric restriction combined with exercise in an effort to induce weight loss. These studies and others have helped characterize the complex nature of sarcopenic obesity treatment. In an attempt to examine body composition and functional changes in obese older adults, Villareal et al.20 randomized subjects into two groups: control group (n = 10) or treatment group (n = 17). The treatment group was directed to follow a balanced diet (30% fat, 50% carbohydrate, 20% protein) with an energy deficiency of 750 kcal/d and completed a 90 min exercise program (15 min warm-up, 30 min endurance exercise, 30 min strength training, 15 min balance exercises) three times per week for 26 ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 weeks. While the control group maintained their body weight, the treatment group lost on average 8.2 kg, with significant losses occurring in fat mass. Fat-free mass, however, was maintained at a similar level to the control group. Frimel et al.5 utilized a similar study design as Villareal20; however, comparisons were made between a dietary-only group (n = 15) and a diet-plus-exercise group (n = 15) after a 6-month intervention with older adults (70 + 5 years old). Similar losses were seen in both groups for body weight and fat mass; however, the diet-plus-exercise group did not lose as much fat-free mass as the diet-only group. Subsequent to these two studies, Villareal et al.21 added an exercise-only condition, utilizing a very similar design as the previous two studies and creating four comparisons: control (n = 27), diet (n = 26), diet plus exercise (n = 28), and exercise (n = 26). The intervention length for this study, however, was 12 months. Both the diet and diet-plus-exercise groups had significant losses of body weight and fat mass. However, the diet group had greater decreases in lean body mass as compared to the diet-plus-exercise group. The exercise group was the only group to see increases in lean body mass. Wood et al.24 compared changes in fat-free mass for a low-fat diet (LFD; < 30% of energy from fat; energy intake goal of 1800kcal/ day) versus a carbohydrate-restricted diet (CRD; < 50g of carbohydrates per day; energy consumption ad libitum) with and without progressive resistance training. The study was conducted over a 12-week period with a supervised whole-body resistance training program being completed three times per week by those subjects randomized into one of the two diet (LFD or CRD) and resistance training groups. Subjects in the LFD group without exercise had the greatest loss of fat-free mass compared to all groups. The outcomes of this study are similar to those of Layman et al.10 and provide some evidence that diets based on carbohydrate restriction should be further examined as an alternative to traditionally used diets based on fat restriction. Miller et al.12 conducted a systematic review examining randomized, controlled trials designed to measure body composition changes during weight loss. All studies examined contained both diet-only and diet-and-exercise groups. Notable to the current article, participants in the studies were not always older adults and what percentage of them were sarcopenic is unknown. It appears that adding exercise to energy restriction will likely not enhance overall weight loss, but will play a critical role in maintaining fatfree mass. Both aerobic and resistance exercise programs appear to preserve fat-free mass similarly, but future research is needed to examine resistance training programs with a higher intensity and a higher volume. The outcomes demonstrated by these studies and similar studies point to the conclusion that we must be mindful of the impact caloric restriction alone can have on body composition changes in older adults. In order to address both the need for reducing body weight and fat mass, as well as preserving or increasing muscle mass, a combined approach of diet and exercise may be most prudent. Additionally, the type of dietary manipulation may be a critical factor for optimizing the impact of a diet and exercise intervention to preserve lean mass. Exercise Considerations Exercise modalities should be selected to counter the physiologi- cal effect of sarcopenic obesity on skeletal muscle and to optimize functional ability. Optimally, exercise should assist in reducing body fat while maintaining or improving lean mass, help prevent reductions in strength and power, and reduce inflammation. For combating sarcopenic obesity, the literature points to combining both aerobic training and resistance training modalities to target the condition in a multifaceted approach. While resistance training has shown the potential to reduce fat mass, the ACSM Position Stand “Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults” concluded that resistance training is not likely to cause weight loss1. Willis et al.23 argue that most studies that found resistance training to alter fat mass compared resistance training to control populations. In the recent “Studies of Targeted Risk Reduction Intervention through Defined Exercise-Aerobic and Resistance Training” (STRRIDE-AT/RT) study, Willis and colleagues attempted to determine which mode of training was most beneficial to reducing fat mass and positively impacting lean mass, utilizing overweight or obese adults. Subjects were randomized into one of three training groups: resistance training (RT; n = 44), aerobic training (AT; n = 38), and aerobic + resistance training (AT/RT; n = 37). The AT and AT/RT groups had significant losses in fat mass, body weight, and waist circumference. The RT group did not see any significant changes in body fat, weight loss, or waist circumference. However, the RT group and the AT/RT group had significant improvements in lean body mass and thigh muscle area, while the AT group did not. Willis indicated aerobic exercise, not resistance exercise, was the critical factor for generating body fat and weight loss. However, combining aerobic and resistance training may provide the most appropriate means by which to induce reductions in body weight and fat mass to address obesity, while still improving lean mass that is so critical for sarcopenia. The loss of skeletal muscle mass with age is associated with a decline in muscle strength and power. Progressive resistance training has been found to be effective at improving strength in older adults. However, in a systematic review by Latham et al.9, interventions incorporating standard progressive resistance training (PRT) protocols found less consistent improvements in functional assessment scores. Activities of daily living (ADL) and functional assessments are thought to rely more heavily on muscular power7. With sarcopenia, power appears to decline more rapidly than strength, due to the greater loss of fast-twitch fibers22. Therefore, power or high velocity training may be a modality that warrants consideration with older adults. Researchers have compared the benefits of high-velocity (power) training versus traditional resistance training for improving power and functional ability. Bottaro et al.3 examined the difference in strength, power, and functional fitness (Rikli and Jones Functional Fitness Test) in older adults (60 to 76 years old) who completed either a 10-week strength (TST) or power (PT) based training program 2 days per week. The resistance exercises and work output were kept consistent between groups, with three sets of 8 to 10 repetitions at increasing intensity (40% 1 RM week 1 and 2; 50% 1 RM week 3 and 4; 60% 1 RM weeks 5-10). However, the power training (PT) group was to complete the concentric portion of the movements as fast as possible with a 2 Suggested Lifestyle Interventions (continued on page 7) ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 5 Health & Fitness Column Circuit Strength Training By Wayne L. Westcott, Ph. D. diovascular adaptations (aerobic conditioning). Research clearly indicates that circuit strength training provides effective exercise protocols for improving both muscular strength and cardiovascular endurance. Beginning in the late 1970s, Larry Gettman and his colleagues conducted considerable research on circuit strength training. One of their first studies compared a circuit strength training program with a standard strength training program2. In this study, the standard strength training program produced greater strength gains than the circuit strength training program (+30% vs. +20%). However, both training protocols produced equal increases in lean weight (+2%) and equal decreases in fat weight (-2%). Additionally, the circuit strength training participants experienced a 10% improvement in aerobic capacity ( ) compared to no significant change for the standard strength training participants. C Wavebreak Media Ltd/ Wavebreak Media/Thinkstock ircuit strength training provides productive resistance exercise protocols for experiencing time-efficient workouts that enhance muscular strength and cardiovascular endurance. Both circuit strength training and standard strength training typically involve about 10 to 15 exercises that cumulatively address the major muscle groups. The American College of Sports Medicine recommendations call for 2 to 4 sets of resistance exercise for each major muscle group in a standard strength training program (page 182)1. Training in this manner is highly effective, but requires varying amounts of recovery time (generally 2 to 3 minutes – page 182)1 between successive exercises or sets for the same muscle groups. On the other hand, circuit strength training requires a single set of each exercise, with the exercises sequenced to work different muscle groups. For example, in the sample circuit training program presented in Table 1, successive exercises address different (fresh) muscle groups and therefore can be performed with minimal transition time between work stations. Consistent with this protocol, circuit strength training has been defined as “a conditioning program in which you perform one set of exercise for a given muscle group (e.g., quadriceps) followed closely by one set of exercise for a different muscle group (e.g., hamstrings), and so on for all of the major muscle groups, typically 10 to 15 different exercises in close succession”11. While one circuit of 10 to 15 resistance exercises provides a relatively comprehensive strength training session, a higher volume workout may be attained by repeating the circuit a second or third time. In this manner, two or three sets of each exercise can be completed without the rest periods required for doing successive sets of the same exercise. Although each set of resistance exercise is completed within 30 to 60 seconds to stimulate muscular development (anaerobic conditioning), performing 15 to 30 minutes of relatively continuous circuit strength training activity also may elicit beneficial car- 6 Table 1: Sample Circuit Strength Training Program Work Station Exercise Major Muscle Groups Leg Extension Leg Curl Chest Press Seated Row Hip Adduction Hip Abduction Shoulder Press Lat Pulldown Low Back Extension Abdominal Curl Quadriceps Hamstrings Pectoralis Major, Triceps Latissimus Dorsi, Biceps Hip Adductors Hip Abductors Deltoids, Triceps Latissimus Dorsi, Biceps Erector Spinae Rectus Abdominis 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. A follow-up study by Gettman and his associates compared a circuit strength training program (3 circuits of 10 exercises at 30 seconds each) with a combined circuit strength training and running program (3 circuits of 10 exercises at 30 seconds each alternated with 30 seconds of running on an adjacent indoor track)3. The circuit strength training group exercised for 22.5 minutes per session and attained a 17% increase in muscle strength, a 3% decrease in percent body fat, and a 12% improvement in aerobic capacity ( ). The circuit strength training and running group exercised for 30 minutes per session and attained a 22.5% increase in muscle strength, a 3.6% decrease in percent body fat, and a 17% improvement in aerobic capacity. Statistically, both of these circuit strength training programs produced similar results. A 1987 study by Harris and Holly6 showed that circuit strength training (3 circuits of 9 exercises at 45 seconds each) produced significant increases in muscle strength (+32.5%), lean weight (+2.2%), and aerobic capacity (+7.8%). This program, conducted with borderline hypertensive subjects, also resulted in a significant reduction in resting diastolic blood pressure (-4.7%). Research by Messier and Dill10 compared a running program (30 minutes, 3 days/week), a standard strength training program (50 minutes, 3 days/week), and a circuit strength training program (20 minutes, 3 days/week). After 10 weeks of training, the mean ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 increase in exercise resistance was 23% for the standard strength training group and 38% for the circuit strength training group. With respect to aerobic capacity, both the running group, and the circuit strength training group had similar and significant improvements in (11.7% and 10.8%, respectively). The authors concluded that circuit strength training was as effective as standard strength training for increasing muscle strength, and as effective as running for increasing aerobic capacity. More recently, Westcott and associates12 conducted a comparison study between the standard Air Force conditioning program, (60 minutes of aerobic activity) and a combined circuit strength training and cycling program (1 circuit of 10 exercises at 60 seconds each, alternated with 60 seconds of stationary cycling) for improving fitness test scores in poorly conditioned Air Force personnel. Participants in the combined circuit strength training and cycling program achieved significantly greater improvements in all of the Air Force fitness assessment measures (1.5 mile run time, push-ups, abdominal crunches, waist girth, and total fitness score) than participants in the standard conditioning program. Based on these and other studies, 3 to 4 months of circuit strength training has been shown to concurrently increase muscular strength and cardiovascular endurance2, 3, 6, 9,10, reduce resting blood pressure6, lower total cholesterol8, improve body composition2, 3, 6, 9, 10, and increase post-exercise oxygen consumption4. Circuit strength training also has elicited beneficial physiological adaptations in patients with metabolic syndrome7 and heart disease5, 9. Therefore, it appears that circuit strength training (alone or in combination with aerobic activity) offers effective and timeefficient exercise protocols for improving muscular strength, cardiovascular endurance, body composition, and other health/ fitness parameters such as resting blood pressure and total blood cholesterol. There are no specific requirements for designing circuit strength training programs, but the protocols should generally include 10 to 15 exercises that address the major muscle groups, with relatively brief transition times between exercise stations. Training durations are typically between 30 and 60 seconds per exercise, and 15 to 30 minutes per session. About the Author Wayne L. Westcott, Ph.D., teaches exercise science and conducts fitness research at Quincy College in Quincy, Massachusetts. He is an active member of the New England Chapter of the American College of Sports Medicine. References References available at acsmcertification.org/cn-Q2-2014 Suggested Lifestyle Interventions (continued from page 5) to 3 sec. eccentric phase. The traditional strength training (TST) group had matching concentric and eccentric phases of 2 to 3 sec. Significantly greater improvements were seen in functional performance. Arm curl improved 50% versus 3%, 8-Ft up-and-go improved 15% versus 0.8%, and 30-s chair stand improved 43% versus 6% for the PT and TST groups respectively. Although muscular strength gains were similar between these groups, muscular power improved significantly more in the PT group than in the TST group. While this and other studies demonstrate the potential benefits of power/high-velocity training with older adults, researchers need to provide practitioners with more information regarding safety and effective implementation to reduce the risk of injury. ronutrient distribution to aid in the preservation of lean mass. Additionally, there is evidence to suggest that a variety of modes of exercise are necessary to target the diverse health challenges associated with sarcopenic obesity. Although additional research is still needed, a balanced exercise program incorporating aerobic, strength, and potentially power training may be most prudent to generate weight and fat-mass losses while also helping to maintain or reduce inflammatory markers, and minimize declines in muscle mass, strength, power, and functional ability. Thus, an appropriate diet, as well as balanced exercise prescription, has the potential to reduce sarcopenic obesity and its associated health issues. Inflammation has been recognized as a potential factor mediating the loss of skeletal muscle, which subsequently can impact strength and power. Both aerobic and resistance exercise have been found to have a positive impact on reducing inflammatory markers in older adults6,25. Additionally, as caloric expenditure increases, inflammatory markers have been found to decline6,17. Reducing the loss of skeletal muscle through exercise-induced regulation of inflammatory markers can potentially help prevent strength and power losses observed with sarcopenic obesity. Elizabeth O’Neill, DPE, M.S., is an associate professor of Exercise Science and the program director for the undergraduate Applied Exercise Science program at Springfield College in Springfield, MA. She has served as the Massachusetts state representative for the New England Chapter of the American College of Sports Medicine for the past year. Conclusion With the increasing demographic of the older adult population, sarcopenic obesity has become an important health concern. Practitioners must consider the complexity of sarcopenic obesity when trying to develop treatment plans. According to the literature, it appears that the older adult can benefit from higher protein intake and, potentially, from modification of the traditional mac- About the Authors Richard J. Wood, Ph.D., M.S., is an associate professor of Exercise Science at Springfield College in Springfield, Massachusetts. He also serves as director of the Center for Wellness Education and Research at Springfield College, which promotes physical activity and good nutrition for school-aged children and their families. References References available at acsmcertification.org/cn-Q2-2014 ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 7 Coaching News By Margaret Moore (Coach Meg), MBA Clients Response to Health Coaching: Health coaching has received high marks from our clients in engaging employees and improving health outcomes. These ingredients make for success within CHS. We have placed health coaches at various clinics and are showing positive return on investment for clients offering health coaching services. Coaching is Catching Other Clinicians’ Interest: Our clinic staffs have noticed the benefits of adding health coaching to the mix of services provided by our onsite clinics. One PA in particular mentioned that health coaching changes the atmosphere of the clinics to the point that she wondered why she wasn’t taught coaching as a part of her curriculum at medical school. She is now talking to her physician about it because she sees daily how coaching engages both patients and clinicians alike. BlueMoon Stock/BlueMoon Stock/Thinkstock This article shares two stories of health and wellness coaches making a difference in a variety of settings and demonstrates the growing career opportunities for well-trained health and wellness coaches. CHS Health Services: Putting Wellness Coaches to Work Debra Reid CWC Who We Are: CHS Health Services, Inc. (CHS) is a health and wellness organization with employer-dedicated onsite health centers designed to provide meaningful, effective, and higher quality health care to employees and their dependents across the country. We build and staff health clinics on large company campuses based on the staffing model the client desires. We might place nurse practitioners, registered nurses, registered dietitians, physician assistants, physicians, and health coaches at their site. Our health coaches are any one of these experts and can also be fitness specialists. For the last five years, we have worked with a partner to provide health and wellness coach training for our coaching staff. When we hire new coaches, we let them know that they will be required to go through our preferred training and certification program in order to maintain their employment with us. We use the organization’s model as the foundation for training and blend that together with our CHS Health Services, Inc. methodology, protocol, and philosophy to provide the most comprehensive training program possible. 8 Utilizing Coaching to Reach Beyond the Episodic Visit: Through our health management and wellness coaching programs, we provide health management education, personalized health coaching, and coordinate patients’ medical care and referrals, all from one location. Even if someone comes into our clinic for an episodic visit, we provide coaching and information to ensure he or she gets the best possible care, and we address any other health concerns he or she has. Improving a patient’s health means changing behavior, and we know that health coaching is the catalyst to that change. The Value of Wellness Coaching at Hilton Head Health Jeffrey Ford Who We Are: Hilton Head Health was founded in 1976 as a 4-week weight-loss spa retreat center. Over the past 30 years, the center has evolved so guests are able to stay and participate in our Healthy Lifestyle™ program for up to 3 months. They can be submerged in the triad of health — fitness, nutrition, and SELF (Stress management, Empowerment, Longevity, Fulfillment). We offer a 1,200 to 1,500 calorie per day meal plan in which guests eat six meals throughout the day. We provide daily educational lectures on fitness, nutrition, emotional eating, and personal responsibility. Throughout the day we offer a variety of fitness classes; we offer six to seven chances to participate in flexibility, strength training, and cardio classes. We also offer a variety of recreational activities, such as kayaking, biking, paddle boarding, and more. Finally, cooking demonstrations and handson classes teach our guests how to cook quick, healthy meals to prepare them for their return home. Our schedule is designed for guests to experience an entire week engulfed in making balanced, healthy changes in their lives, while still having a good time. Coaching News (continued on page 13) ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 Health & Fitness Feature THE GALLON JUG SHELF TEST: AN ASSESSMENT OF MODERATELY HEAVY OBJECT TRANSFER By Joseph F. Signorile, Ph.D. Through needs assessments (or diagnoses, as they may be termed, using the medical model), the recent American College of Sports Medicine’s Exercise is Medicine® initiative has increased the awareness that true exercise prescription should be preceded by a testing battery that allows training to be provided in a targeted and structured, pattern to most effectively address individuals’ specific needs. Unfortunately, all diagnostic methods have shortcomings associated with their administration and interpretation. In the case of object transfer tasks, two confluent problems confound the process. The first is the confusion that persists between measures of physical performance and measures of daily activities, the lines of which are admittedly somewhat blurred. The second is the failure to apply the theory of biomechanical specificity to the assessment methods8. Table 1: Basic and Instrumental Activities of Daily Living Instrumental Basic Activities Instrumental Activities Activities of Daily of Daily Living10 of Daily Living5 Living (AOTA)7 Figure 1. The Gallon Jug Shelf Test. Reprinted from Bending the Aging Curve. Champaign: Human Kinetics Publishers, 20118 with permission. I n their 1989 position statement, “Measuring the Activities of Daily Living among the Elderly: A Guide to National Surveys,” the U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy stated that the prevalence of disability is associated with reduced ability to perform basic (ADL) and instrumental activities of daily living (IADL)10. This is evidenced by the inclusion in ADL and IADL questionnaires5 and testing batteries1 activities such as shopping, food preparation, housework, and doing laundry, which by necessity require the transfer of moderately heavy objects as part of most assessment batteries. While it may be tempting to attribute successful performance levels during moderately heavy object transfers to upper body strength and range of motion, in reality, the majority of these tasks actually incorporate the sequential firing of lower, core, and upper body muscles in a “kinetic chain” to produce a viable performance. Bathing and Ability to use a showering telephone or other form of communication Dressing Shopping for groceries or clothing Eating Food preparation TransferringHousekeeping Personal hygiene Laundry Toileting Transportation within the community Ability to handle finances Responsibility for one’s own medications Care of others (including selecting and supervising caregivers) Care of pets Child rearing Communication management Community mobility Financial management Health management and maintenance Home establishment and maintenance Meal preparation and cleanup Religious observances Safety procedures and emergency responses Shopping Two tests which are each well-established measures of upper limb strength, handgrip strength dynamometry3,4 and the 30s arm curl test6, can be used to illustrate the problems of performance versus ADL measurement and biomechanical specificity. First of all, neither handgrip dynamometry nor the 30s arm curl test is an assessment of object transfer as a component of IADL ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 The Gallon Jug Shelf Test (continued on page 14) 9 Wellness Column Online Tips and Tools for Exercise Professionals By Peter Ronai, M.S. ACSM RCEP, CES, PD, CSCS-D, FACSM E Milenko Bokan/iStock/Thinkstock xercise practitioners interested in selecting clinically oriented tests to assess physical function in their elderly clients and clients with chronic diseases and disabilities can find them in the Rehabilitation Measures Database web site, Rehabmeasures.org. The Rehabilitation Measures Database web site is described as “the rehabilitation clinician’s place to find the best instruments to screen patients and monitor their progress ”¹. The content of this web site and database is developed under a grant from the Department of Education and was developed by the Rehabilitation Institute of Chicago, Center for Rehabilitation Outcomes Research, Northwestern University Feinberg School of Medical Social Sciences Informatics Group¹. This database is made available through a National Institute of Disability Rehabilitation Research grant number H133B090024. The Principle Investigator is Allen Heinemann, Ph.D. Exercise and rehabilitation practitioners can search for measurement tools by: • assessment area–construct(s) or variable(s) measured • diagnosis–disease(s) or condition(s) for which the assessment is most appropriate and valid • length of test–approximate time to complete a specific assessment cost Section tabs on this website include: • “home” • “complete list of instruments”–a comprehensive list of all tools within the database/ directory • “statistics review”–definition of research terms and statistics and their significance/relevance • “ links”–links to organizations and specific assessment tools • “take a tour”–a preview of all features of the website • “about us”–additional information about the Rehabilitation Institute of Chicago services • “contributors”–other institutions assisting through either research and/or funding The “complete list of instruments” tab is a comprehensive index of population-specific evaluation tools. Tools range from practitioner supervised performance test batteries and physical examination tools to disease-specific quality of life and health 10 risk assessments. Assessments can serve as a means to measure program outcomes. The “complete list of measurements” provides users with the name of specific tests, test acronym(s), organization’s links to the assessment(s), assessment duration (time to administer the test), diagnostic groups or populations in which the test(s) can accurately and reliably be used, area of assessment (functional mobility, strength, flexibility, pain, spasticity, balance, aerobic capacity, ability to perform activities of daily living (ADLs), upper extremity function, cognition, depression, quality of life, and others). Users are able to access the evaluation and learn how the test was developed and how to administer and score the assessment. Peer-reviewed research articles describing the development, administration, scoring, and interpretation of many of the assessments in this database are available in this section. An explanation of test reliability, validity, amount of training, and resources necessary to conduct specific tests are included in this section. Viewers can access information regarding: • minimal detectable change (MDC) (the smallest amount of change that can be detected by a measure that corresponds to a noticeable change in the ability)1, • minimal clinically important difference (MCID) (represents the smallest amount of change in an outcome that might be considered important by the patient/client or clinician/ practitioner)1, • predictive validity (indicates that the outcomes of an instrument predict a future state or outcome, like a fall) as well as a number of other clinically relevant statistics1 Some organizations in this directory provide links to instructional videos of specific assessment procedures, like manual muscle testing, and musculoskeletal injury screening. The “statistics review” section provides viewers with a comprehensive explanation of common yet important research/statistical terms, definitions, and measurements. Examples of ideal numeric ranges for a number of statistical variables are provided to help viewers understand the strengths and/or limitations of specific tests as assessment tools for different populations. Some terms reviewed in this section include: • predictive validity (ability of the outcomes of an assessment to predict future events, like a myocardial infarction or a fall)1 • concurrent validity (ability of a test to obtain similar results as a “Gold Standard” test/assessment)1 • cut-off scores (designates a positive or negative test score. Scores below this value typically indicate a client/patient being at a greater risk of acquiring a specific condition or encountering a specific event like a fall)1 Online Tips and Tools (continued on page 13) ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 Resistive Exercise Testing (continued from page 3) guidance of an ACSM certified Clinical Exercise SpecialistSM or Registered Clinical Exercise Physiologist®. Program Requirements for Resistive Exercise Testing in Pulmonary Rehabilitation Incorporation of resistive exercise testing for the PR patient is also important from an overall program perspective. Presented below are just a few requirements for optimal PR program operation with regard to resistive exercise outcomes documentation, patient education, and exercise prescription: • Pre- and post-rehabilitation strength testing measures for outcomes documentation of upper and lower body muscular improvements are necessary. Muscular strength and endurance testing should be performed under the same testing conditions at 3, 6, 12, 18, and/or up to 24 months or at program-specific standardized intervals. • Outcomes documentation is required for AACVPR PR program certification1, as well as for the upcoming AACVPR Pulmonary Rehabilitation Outcomes Registry. • I t is important to let the PR participant know how they “stand up” compared to those in their particular age and gender group with periodic strength testing. • The PR participant needs to be kept abreast as to how much they are improving (or regressing) over time throughout their PR participation with regard to strength gains or loss. • The CEP should thoroughly address the muscular strength, muscular endurance, and neuromotor needs of the patient to assist with the resistive exercise prescription and evaluation of vocational responsibilities and performance of home ADLs (e.g., walking, dressing, picking up items, housework, squatting). •R esistive testing (and training) should be performed to measure and compare individual success with validated population-specific norms. If normative data is unavailable for specific pulmonary populations, the CEP may choose to compare the patient’s testing results to data from geriatric or frail populations until such pulmonary normative strength testing data becomes available. •C hronic resistive exercise training may help to boost the PR participant’s confidence level, self-efficacy, and self-image. •P osture and balance issues for the PR participant may be assessed through resistive testing to assist in the prescription of posture and balance exercises. •F inally, resistive exercise testing should be performed to help assess and determine the individual needs of the patient with respect to their unique overall muscular weaknesses. Muscular Strength and Endurance Testing Traditionally, it has been difficult to design resistive exercise training protocols for the PR participant, as there is a lack of validated testing protocols designed specifically for those with chronic lung disease in the literature. Thus, many CEPs have successfully used (or adapted) many common muscular strength and endurance testing protocols designed for geriatric patients, cardiac rehabilitation participants, and the elderly. With regard to oxygen supplementation and pulse oximeter monitoring, the CEP typically need do nothing different than would normally be performed in a regular exercise session. Oftentimes, resistive exercise testing and training does not produce the same meta- bolic demand and oxygen requirement as does aerobic exercise. Thus, the patient may or may not need to use their supplemental oxygen during resistive testing, depending upon their fitness level and disease profile. It is important that each selected testing protocol be able to be performed by the PR participant safely and be previously tested for validity and reliability. Ideally, normative values also should be available for the test. Resistive exercise testing in PR does not require expensive equipment and can often be successfully performed with items that are commonly used in PR programs, such as dumbbells and chairs. Other testing items can often be built out of wood by patients or patient family members who have carpentry skills. Commonly used muscular strength and endurance testing protocols taken from the Senior Fitness Test Manual (and associated research)14-16 and others17-19 meet the above criteria and are summarized as follows: 1. The 30-second Arm or Biceps Curl Test: The subject performs as many arm curls as possible on both the right and left arms with a dumbbell (8 lbs. men, 5 lbs. women) for 30 seconds in a seated position. 2. The 30-second Chair Stand Test: The subject completes as many full stands as possible in 30 seconds from a seated position in a chair that is placed against a wall or ceiling support beam. 3. The 8-Foot Up and Go Test: As a test of lower body muscular strength/endurance, motor performance, and dynamic balance, the subject stands from a chair and quickly walks around a cone placed 8 feet in front of the chair for the best of two trials, timed to the nearest 1/10 of a second. 4. The Signorile Gallon Jug Shelf Test17: As a measure of upper body power and strength, five (5) one-gallon jugs are filled with water and are moved from the bottom shelf of a bookcase to the top shelf. The subject is timed to the nearest 1/10 of a second, and percentile rankings are available by age group and gender. 5. T he 6-Minute Peg Board and Ring Test18: As a test of unsupported upper body muscular endurance, the subject moves a series of 10 lightweight wooden rings from an upper level of 10 wooden pegs to a lower level of pegs as many times as possible in 6 minutes. This test has shown excellent test-retest reliability in pulmonary patients. 6. T he Seated Medicine Ball Throw Test19: From a seated position, the patient performs a basketball chest pass with medicine balls that weigh 1.5 kg and 3 kg each for 3 trials, with a 3-minute rest between trials. The distance is measured from the spot where the patient drops the ball in front of them initially on a piece of masking tape to the furthest point where the ball lands on a taped line with a typical chest pass. The CEP may be able to accurately calculate measures of work rate and power in watts and kilogram-meters/minute from some of the tests described above. These types of calculations may aid in the development of the resistive exercise prescription and outcomes documentation over time for the patient. While other muscular strength and endurance tests have been presented in the literature, few are designed or validated specifically for patients with chronic lung disease. ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 Resistive Exercise Testing (continued on page 12) 11 Resistive Exercise Testing (continued from page 11) Using Machines and Free Weights for Resistive Exercise Testing Free weights and machine weights also may be used as resistive testing modalities in PR programs. Unfortunately, as stated there has been little research on the development of resistive testing protocols using these modalities in pulmonary populations, resulting in a lack of normative strength testing data for patients with chronic lung disease. This lack of normative data makes it difficult for the CEP to determine what is an optimal level of resistance to be lifted in order for a patient with COPD to be classified as “normal.” The AACVPR1 and ACSM20 have provided general recommendations for resistive exercise training in pulmonary populations, but little if any information on resistive exercise testing. This is due to the lack of evidenced-based research in this area. ACSM recommends using exercise training protocols for resistive training as those prescribed for healthy adults and/or older patients (discussed further in Part II of this article in the next issue of ACSM’s Certified News). Therefore, the CEP in PR has to rely on previously published research as well as his or her own intuition and knowledge of each individual patient to select the best resistive testing modality and protocol suitable for that particular patient or group of patients. One-repetition maximum (1 RM) testing and variations thereof have been shown to be safe and effective in pulmonary populations. Kaelin et al.21 examined older male and female PR participants with 1 RM testing consisting of parallel squat and incline bench press exercises. These investigators concluded that a properly supervised and screened PR population can perform 1 RM testing without significant muscle soreness, injury, or abnormal cardiopulmonary responses. While this is one of very few investigations that have studied 1 RM testing in pulmonary patients, this is an encouraging study that hopefully promotes on further strength testing research in pulmonary populations. Many variations of machine and free weight initial strength testing have been used in geriatric, cardiac, and pulmonary populations over recent years. These variations include the following protocols and adaptations: 1. An initial weight load is determined that allows 5-10 reps at ~ 30% to 40% of 1 RM for upper body and 50% to 60% for the lower body20,22. 2. Using a rating of perceived exertion (RPE) assessment, the patient starts with a light weight and performs 12 to 15 repetitions to an RPE of light to somewhat hard (12 to 13) on the Borg Category Scale23. 3. For novice and intermediate clients, it is recommended that moderate loading be used at 70% to 85% of 1 RM for 8 to 12 repetitions24. 4. Using a titration technique, where the patient begins at a level of 10 reps with lighter machine weights and progresses to 15 reps/session. At this time, the resistance is increased 2 to 5 pounds, and the patient falls back to 10 reps/machine. 5. The patient performs a traditional 1 RM assessment, the resistance is progressively increased to see how much can be lifted once with proper warm-up and technique25. 6. The patient performs a 3-repetition maximum (3 RM) test, which has been shown to be safer and more reliable than a traditional 1 RM test26. Regardless of the initial strength testing assessment modality or protocol utilized, the CEP has to always put patient safety at the forefront of all testing. Hopefully with further research in this area, strength testing protocols will be designed specifically for patients with chronic lung disease who participate in PR programs. Handgrip Dynamometer Testing The handgrip dynamometer has been used to test grip strength as an indicator of overall body strength and physical function status in older populations27-30 and in cardiac patients31. While this device may have practical applicability for strength assessment in these populations, the ability of this device to assess overall body strength in cardiac patients has been questioned32. Nevertheless, the handgrip dynamometer would appear to be an excellent modality for assessment of grip strength in most PR participants as this modality requires little training, is lightweight and portable, and provides a low-risk assessment of grip strength with only a brief isometric component. Research has shown that handgrip muscle strength decreases as FVC and FEV1.0 decreases33 and BODE Index (a rating scale used to stage disease severity in persons with COPD) values increase34 in patients with COPD. While there is a lack of normative handgrip data for pulmonary patients, these have been published for older populations35,36. Proper techniques to perform the handgrip dynamometer test have been presented elsewhere36. Summary Resistive exercise testing is an important component in PR. This form of testing should be performed routinely on all patients at periodic time intervals for patient outcomes documentation of strength improvements, as well as for the development of the resistive exercise prescription. While there is a current lack of research that presents optimal resistive exercise testing protocols for the PR participant, the CEP can rely on validated muscular strength and endurance testing techniques that have been previously performed in older and frail populations. Obviously, not all PR participants are elderly or frail, but patient safety is paramount and testing with validated low risk protocols for older patients is prudent. With the ever-expanding exercise and pulmonary disease research base, it is hoped that the CEP will soon be able to refer to standardized pulmonary strength testing protocols with associated normative data to assist in long-term patient outcomes documentation and the development of the ideal individualized resistive exercise prescription. About the Author Dave Verrill, MS, FAACVPR, is a clinical exercise physiologist, laboratory director, and lecturer in the Department of Kinesiology at the University of North Carolina at Charlotte (UNCC). He is certified as an ACSM Exercise SpecialistSM, ACSM Program DirectorSM, and ACSM Registered Clinical Exercise Physiologist®. Dave is currently chair of the committee for state licensure for CEPs in North Carolina and is past-president of the Clinical Exercise Physiology Association (CEPA) and North Carolina Cardiopulmonary Rehabilitation Association (NCCRA). He has co-written chapters for ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription, ACSM’s Resources for the Clinical Exercise Physiologist, and ACSM’s Certification Review. He also has published a number of journal articles, abstracts, and book chapters in the field of cardiopulmonary rehabilitation and resistive exercise training and has presented at many regional and national ACSM and AACVPR meetings. References References available at acsmcertification.org/cn-Q2-2014 12 ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 Coaching News (continued from page 8) What Was Missing From Our Program: I have been with Hilton Head Health for just over two years and was hired to create a continued support program for our guests. H3@Home Wellness coaching offers a component that was missing from our program before. Upon returning home, guests now have the option for continued, structured support from one of our trained wellness coaches to ensure the tools and knowledge gained during their stay are not just being put into practice, but are actually sticking. We were all very excited when H3 fitness director Adam Martin started throwing around the idea of at-home coaching and came across the highly recommended and leading-edge coach training program. Adam and I shared the same vision for our guests, and he trusted me to bring that vision to life. We are so excited that we are sitting here today with the program successfully put into action. How We Began: We made the decision that we were not going to start a coaching program at Hilton Head Health until we had a viable certification. We found that the coach training program we selected was a perfect fit and the focus went hand-in-hand with what we wanted to do here. We began the training with our entire program staff in June 2011 and we went through the training classes together and studied together. Learning about motivational interviewing and non-violent communication were particularly impactful to me. The format for structuring the coaching calls that the program uses has been huge for getting our program off the ground. I was the first coach to become certified, and right away we launched our H3@Home Wellness Coaching program. Implementing Coaching: We now offer a few different types of coaching programs, all of which are based on what we learned in coach training. These are follow-up programs, and our goal is for our guests to sustain success in living the healthy habits they learned here. All of our programs offer an initial 90-min- ute coaching session to get started. Then to create a group feel, we send weekly group e-mail messages, weekly text messages, and challenges that we give our guests at home. Guests have 30-minute calls with their coach once a week for 3 months. At the end of the 3 months, they either continue with the coaching or feel ready to move on. Coaching’s Impact: The biggest impact of coaching for our guests has been accountability! We felt the need to implement a coaching program to become certified because although many of our guests are successful at home, we find several guests come back to our facility and need continued education and assistance. The difference today with the implementation of coaching is that these guests are coming back 50 to 60 lbs. lighter, with new sustainable habits, such as reducing work hours, exercising regularly, improved nutrition, planning, and journaling. Coaching has been a great way for guests to use the motivation that they get from staying a week with us and really focus on those habits as they go home. We have definitely seen more successful outcomes with our guests because of coaching. A little bit of accountability goes a long way! About the Author Margaret Moore (Coach Meg), MBA, is the founder and CEO of Wellcoaches Corporation, a strategic partner of the ACSM, widely recognized as setting a gold standard for professional coaches in health care and wellness. Wellcoaches has trained 8,000 health professionals as coaches in 47 countries. Moore is co-director of the Institute of Coaching at McLean Hospital, an affiliate of Harvard Medical School, and co-directs the annual Coaching in Leadership & Healthcare Conference offered by Harvard Medical School. She co-authored the ACSM-endorsed Lippincott, Williams & Wilkins Coaching Psychology Manual, the first coaching textbook in health care and, the Harvard Health Book, published by Harlequin: Organize Your Mind, Organize Your Life. Online Tips and Tools (continued from page 10) This section of the rehabmeasures.org website and database provide viewers with a better understanding of how to use specific measurements. And it enables them to select the best measurement instruments for each patient or client on an individual basis. Viewers can access the Rehabmeasures.org database at http://www.rehabmeasures.org/default.aspx Exercise practitioners can search for and access physical assessment tools that best meet the individual needs of each of their patients and clients on the Rehabilitation Measures Database. Resources The Rehabilitation Measures Database Website [Internet]. Chicago, (IL): Rehabilitation Institute of Chicago: [cited 2013 Sept. 1]. Available from http://www.rehabmeasures.org/default.aspc. About the Author Peter Ronai, MS, RCEP, CSCS-D, FACSM, is a clinical associate professor in the department of physical therapy and human movement science at Sacred Heart University in Fairfield Connecticut. He is a Fellow of the American College of Sports Medicine. Ronai is past-president of the New England Chapter of the American College of Sports Medicine (NEACSM), past member of the ACSM Registered Clinical Exercise Physiologist (RCEP) Practice Board, Continuing Professional Education Committee and current member of the ACSM Publications sub-committee. Ronai is co-editor of ACSM’s Certified News and also the Special Populations column editor for the National Strength and Conditioning Association’s (NSCA) The Journal of Strength and Conditioning Research (SCJ). He is also ACSM Program Director Certified. ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 13 The Gallon Jug Shelf Test (continued from page 9) performance. Rather, both are measures of a neuromuscular performance measure — strength. Second, these measures assess strength production by the flexor muscles of the hand and forearm (grip strength) or the elbow flexors (30s arm curl). While the strength of these muscles is important to performance of the overall task, these measures cannot be considered complete assessments of this complex task which incorporates the sequential operations of multiple joints in a skilled movement pattern. In contrast, the Gallon Jug Shelf Test (GJST) has been shown to be a valid, reliable, inexpensive, safe, and easily administered clinical test of moderately heavy object transfer. Briefly described, the test requires the participant to sequentially transfer five one-gallon jugs (weight app 3.9 kg) as quickly as possible from a shelf set at the level of the participant’s patella to a shelf aligned with the top of the participant’s shoulder (see Figure 1)9. Three Table 2: The Gallon Jug Test Methodology Equipment • Bookshelf 84” H x 42” W x 12” D with adjustable shelves • 5 one-gallon water-filled milk jugs • 1 Stopwatch Set-up • Align the lower shelf with the participant’s patella. • Align the upper shelf with the top of the participant’s shoulder. • Place the 5 one-gallon jugs on the bottom shelf. • Provide detailed instructions prior to testing. • Demonstrate the test. Test Procedure 1. H ave the participant stand comfortably in front of the bookcase. 2. I nstruct the participant to keep the back as straight as possible, keep the head up, not lean forward, use the legs as the primary source of power for the lift, and abort the task if there is any feeling of stress or discomfort. 3. P rovide a test trial, evaluate form, correct form, and provide another practice if necessary. 4. R emind the participant to move only one jug at a time, not to alternate hands, and begin the test standing straight up. 5. B egin the trial with a “ready” command to prepare the participant, followed by a “go” command. 6. B egin the timing with the “go” command and stop when the fifth jug is placed on the top shelf. 7. I f multiple trials are used, allow a 1-minute recovery between attempts. explicit directions provided in preparation for the test are to keep the back as straight as possible, to not alternate hands, and to use the legs to help with the task. Obviously these instructions are designed to put limits on performance strategies and to increase safety during test performance. But more germane to the current discussion, the last direction, to use the legs to help with the task, reflects the developers’ recognition of the importance of force transfer from the lower body through the core and to the upper body in the performance of transfer skills involving moderate to moderately heavy objects (see Figure 2). In agreement with current arguments favoring the use of task-specific exercises to maximize improvements in daily activities2, the GJST provides the researcher and clinician with an assessment that evaluates a skill critical to independence — the controlled transfer of moderately heavy objects. Figure 2. Kinetic Chain Utilization during the Gallon Jug Shelf Test. Reprinted from Bending the Aging Curve. Champaign: Human Kinetics Publishers, 2011 with permission8. About the Author Dr. Signorile is a Professor of Exercise Physiology at the University of Miami with a joint appointment at the University of Miami Center on Aging. He have been involved in research using exercise to address independence and fall prevention for over 20 years, has over 65 refereed manuscripts and 200 national and international scientific presentations. He have been a pioneer in applying the diagnosis/prescription model for tailored exercise to improve function and reduce falls in older persons and continues to work on new technologies for improving independence. Within the context of prescriptive exercise he has organized and led a series of studies that produced and published refereed articles detailing novel tools to assess and improve independence. He has chaired over 20 doctoral dissertations and served as a committee member on countless more. Dr. Signorile is the coauthor of SouthBeach Diet Supercharged and recently released his definitive book on aging exercise prescription entitled Bending the Aging Curve recently translated into Cantonese. References References available at acsmcertification.org/cn-Q2-2014 14 ACSM’S CERTIFIED NEWS • SECOND QUARTER 2014 • VOLUME 24: ISSUE 2 www.onlinelearning-acsm.org Your Resource for Online Continuing Education! ACSM ceOnline Benefits: Affordable 4 ACSM CECs for as little as $20! Flexible Completely accessible Online: 24/7/365 Self-paced: Start and stop per your schedule Convenient Track CECs earned from outside agencies Instant Instant notifications Immediate access to content including course materials, tests, certificates, and receipts. ACSM members: find the member discount code in the Membership Resources section of ACSM’s website after you log in or email the membership department at membership@acsm.org Don’t wait until the last minute… log on today to gain access to these and other great CEC opportunities www.onlinelearning-acsm.org! For additional CEC questions, email onlinelearning@acsm.org ACSM’s 2014 Health & Fitness Summit Videos are now available! Was there a session you missed? Or, maybe you attended a session that you’d like to repeat? Several Summit sessions were filmed and are currently available on ACSM’s ceOnline website. Sessions recorded include several ACSM gold standard presenters: · Great Instructors and Trainers: Born or Made? Presented by Fred Hoffman · The Physiology of TABATA – Is 4-Minutes Enough? Presented by Michelle Olson · 10,000 Workouts in 10 Minutes: Movement Based Programming Presented by Dixie Stanforth & Matt King · Can Broccoli Make You Beautiful? Presented by Leslie Bonci · And many more…. ACSM’s Certified News ISSN # 1056-9677 401 West Michigan Street Indianapolis, IN 46202-3233 USA