PDF - Faculty Of Pharmacy
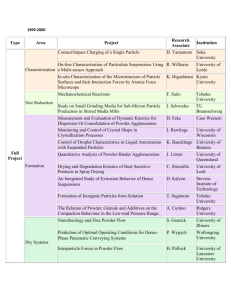
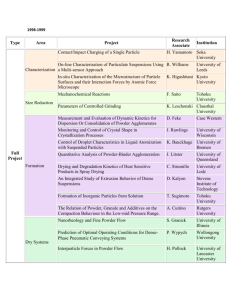
advertisement

DEPARTMENT OF PHARMACEUTICS AND PHARMACEUTICAL TECHNOLOGY FACULTY OF PHARMACY UNIVERSITY OF BENIN BENIN CITY PRACTICAL MANUAL FOR THE PHARM. D DEGREE (Revised 2012/2013) Revised & Edited By Prof. R.S. Okor Prof. M.A. Iwuagwu Dr (Mrs) F.E. Eichie Dr. M.I. Arhewoh Pharm. J.E. Isessele Dr. E.Q. Osazuwa Prof. A.O. Okhamafe Prof. A.O. Onyekweli Dr. M.U. Uhumwangho Pharm. S.O. Eraga Pharm. J.O. Erebor 200 LEVEL 2 LABORATORY RULES 1. Dressing: A clean well ironed overall laboratory coat must be worn at all times during the practical class. Male students should be dressed in shirt, tie and leather shoes while females should be dressed in skirt, blouse and low-heeled or flat sole cover shoes (No sandals, slip-on, or easy ware). Wearing make-up, false eye lashes, jewelries and hair styles with loose strands or locks of hair should be avoided. 2. Cleanliness: Cleanliness is indispensable to good dispensing and every exercise must receive the same meticulous care as if it were a doctor’s prescription. 3. Accuracy: Most errors in the compounding operation are the result of carelessness or the use of improper equipment when translating one system of weights and measures to another. 4. Replacing Stock Bottles: Bottles of chemicals must be returned immediately after use and never kept on the bench as the habit of accumulating bottles hinders smooth working. Excess chemicals must never be returned to the stock bottles. 5. Practical Notebook A practical well-indexed thick back notebook is of great value in revising and for future reference. 6. Equipment and Techniques used in Weighing: Balances: It is the personal responsibility of each student to keep the dispensing balance and weights scrupulously clean. 3 WEIGHING TECHNIQUES 1. Place suitable weighing papers on each balance pan. 2. Release the pan arrest gently and make the necessary adjustment using the leveling screws so that the pointer shows a rest point of zero as indicated by equal swings to the right and left of the zero index mark and then arrest the balance. 3. Place the appropriate weights on the left hand stainless steel pan. 4. Place the approximate weight of the material to be weighed on the right hand watch glass and release the pan arrest gently to determine whether too much or too little was added. 5. Remove or add the material using a spatula arresting the pan mechanism after each transfer is made. 6. The weighing process is completed when a release of the pan arrest shows a zero rest point. SENSITIVITY OF BALANCE Limits of error of about 5 per cent are allowed in most weighing and measuring processes. The error inevitably results because the operator cannot estimate the equilibrium point closer than about one index scale division. The pharmacist must ascertain the “sensitivity of the balance”. The sensitivity of a prescription balance is defined as the weight usually expressed in milligrams, required to produce a pointer deflection of one scale division. The minimum permissible weight is at least 20 times the sensitivity of the balance to avoid error greater than 5 per cent. EQUIPMENT AND TECHNIQUE USED IN MEASURING 1. Select the appropriate graduate i.e. with a capacity equal to or exceeding the volume to be measured. 2. Hold the graduate by the base with your left hand. Elevate the graduate so that the desired mark is at eye level. Then pour the liquid decreasing the rate of flow as the surface of liquid approaches the desired mark. 4 GENERAL PROCEDURE FOR DISPENSING A PREPARATION 1. Each student is expected to work on his/her own. If advice is needed, it should be obtained only from the lecturer. 2. A glass cloth is for polishing containers; it will not be suitable for this purpose if it used for wiping the bench – this is the function of a duster (a small hand towel or cloth). Dispensable paper towels are provided at the end of each bench for mopping up wet spillage. You will require a pair of scissors, a pair of forceps, a black/blue and red pen (fine point), a ruler and a calculator. 3. All work should be done in a clean and tidy manner. This minimizes contamination of the products and is conducive to precision and accuracy. 4. Read the prescription carefully and, if necessary, look up and copy out the formula from the B.N.F. (British National Formulary), B.P. (British Pharmacopoeia). Always use the most recent editions of these books. 5. Check the doses of internal preparations (including suppositories and enemas) and take into account the directions for use. Report any over dosages to a member of staff. 6. If any ingredient is a poison (check this in the Poisons and T.S.A. Guide) the weight or volume dispensed must be checked by a registered pharmacist. 7. Use the B.P.C. Extra Pharmacopoeia or B.P. to confirm that there are no pharmaceutical or pharmacological incompatibilities in the preparation. 8. If you are unsure about the method of preparation to use, refer to your previous dispensing schedules, which should be well indexed, or to DISPENSING FOR PHARMAEUTICAL STUDENTS. 9. Look up the storage requirements for the preparation (if the formula is in the B.N.C., B.P.C., or B.P) or the medicaments (if the preparation is a special formulation not in one of these books). Protection from light, storage in a cool place, etc. may also be necessary. 10. From the formula, work out the amounts to be used and write them in ink, at the side of the prescribed amounts, to facilitate checking. 5 11. Check your calculations in two ways if possible. 12. Collect the correct container. 13. If necessary, cut the label to fit the container but do not trim off the name of the supplier (the faculty in this case). In general, just the largest possible label should be used. 14. Write the main label and collect any special labels that are necessary. Leave them in a conspicuous place. 15. Start making the preparation. 16. If for any reason a preparation is left unfinished, even for a few minutes, a label must be attached giving details of the materials added. The preparation must be protected from accidental contamination. ADDITIONAL SAFETY PRECAUTIONS 1. If a wrong figure or unit is written cross it out and write the correct one above or at the side. Do not attempt to alter the wrong one. 2. Always protect the decimal point with a ‘0’ i.e. 0.1 not .1; since if the decimal point is not written distinctly, there is a risk of giving a times ten (×10) overdose. 3. Always write down details of every weighing and measurement. 4. Carefully check the labels of the stock bottles you use and watch particularly for such words as: (a) Compound; e.g. Compound Tragacanth Powder is different from Tragacanth Powder. (b) Concentration; e.g. Concentrated Compound Infusion of Gentian is different from Compound Infusion of Gentian. (c) Strong (Fort); e.g. Strong Coal Tar Solution is different from Coal Tar Solution. Also, watch out for medicaments that have similar names: e.g. Eucalyptol and Eucalyptus Oil. Terebone and Turpentine Oil (Oil Terebinth). APPROXIMATIONS 1. In general, approximations should not be made and, certainly, never when the amount can be weighed or measured with the weights. When they are unavoidable, approximations should be minimal and in no circumstances greater than 5 per cent. 6 2. Always write the correct amount first and show the approximation in brackets at the side – e.g. 18.478g (18.48g). USE OF STOCK BOTTLES 1. Check the label against the prescription before and after using the bottle. 2. Hold the bottle with the label uppermost so that it can be seen during use. As a result, an error may be detected. Also, liquid from the rim will not run down the label. 3. Always use a spatula for weighing solids. This avoids fouling the neck of the bottle. To keep out dust, hold the bottle as near to horizontal as possible with one hand and remove the stopper with the little finger and palm of the other. Unless the stopper is too large, keep it in the hand; you will find that you can easily use the spatula with the same hand. If it is essential to put the stopper down, place it the right way up on a clean sheet of white paper. PRESENTATION 1. Glass and plastic containers must be polished before issue. Polishing should be done after, as well as before labeling, to remove gum and finger- marks. 2. Acacia-gum labels will not adhere to plastics or metal containers; selfadhesive labels must be used. NOTES ON WRITING-UP DISPENSING SHEETS 1. Prescription: Make an exact copy of the prescription as written. Record the date. 2. Formula and Calculation of Doses: (a) Where the prescription consists of a formula showing all the ingredients to be used, record the quantity of each substance used opposite the name of the drug to which it refers. (b) Where the prescription refers to a B.P., B.P.C., or B.N.F. preparation, record the official formula together with the official quantities, and record as in the quantities used. 7 (c) Record details of all calculations and formula used including those for dilutions and trituration. For all oral and injectable preparations, record the maximum B.P. or B.P.C. dose of each active ingredient. 3. Specimen Label: Affix a duplicate of the label applied to the product. Include also any auxiliary labels used; e.g. shake the bottle. 4. Container: Record details of the size and type of container used together with any special container specification for the product. E.g. test for t he limit of alkalinity of glass (L.A.G.). 5. Storage Requirements: Record the shelf life of the product and details of any special requirements for storage, e.g. protect from light. 6. Main Pharmaceutical Actions of the Active Drug(s): Make brief notes on the main pharmaceutical actions of the active ingredients in the preparation, in the context of the dosage form supplied. 7. Clinical Conditions and Dose Regimen of Product: Note that this action refers to the final dispensed product only, and not to other dosage forms of the same drugs. 8. Methods of Preparation: Describe in note form, but in detail the methods used. 9. Clarification: Where applicable, specify medium used. 10. Sterilization: Where applicable, record methods, time and temperature. 11. Formulation Notes: Record details of additives, excipients, colouring, and aids to formulation. Mention also any incompatibilities encountered. If you have formulated the product, give the reasons for your choice of formulation. PACKAGING AND LABELLING OF DISPENSED MEDICINES See Cooper and Gunns’ Dispensing for Pharmaceutical Students (12th Edn. Pp.13 – 30). 8 A. Packaging: The type of container used for dispensed medicines are only general suggestions and the choice of packaging for individual preparations is made solely on technical grounds. Official recommendations on colours and changes of container for each type of medication should be adhered to so as to help reduce the accidental misuse of medicines. The following points are to be noted in the packaging of dispensed products. 1. All mixtures intended for oral use must be packed in plain bottles and covered with plastic screw-caps. 2. All preparations intended for external use only (e.g. applications, gargles, lotions, etc.) must be packed in fluted or ribbed glass bottles. 3. All preparations containing photo-labile (i.e. light sensitive) ingredients are packed in amber coloured bottles. 4. Any thick liquid preparations such as emulsion, liniments etc are packed in wide-mouthed bottles to allow for easy pouring out of contents from the bottle. B. Labeling: The primary function of a label is that of accurately directing the patient how and when the medicine should be taken or used. The label is an important factor in the appearance of the final medicine and a high standard in label presentation will do much to maintain confidence of the patient. Therefore, every effort should be made to be competent on this point. A number of important requirements are listed below: 1. Label instructions should be LEGIBLE, NEAT AND WELL BALANCED. 2. Choose the correct size of container for the product and match the label size to the container. 3. Polish bottles before labeling. 4. Affix labels symmetrically on the container. 9 5. Never have more than one unlabelled product on the bench at the same time. Never place a fresh label over an old label. This is seriously and potentially dangerous. In general, labels for “Internal Medicines” adopt Black Prints and those for “External Medicines” adopt Red Prints. The main label should clearly state: 1. The quantity of the product. 2. The type of preparation e.g. “The Mixture” The Tablets”, etc. or where so directed the actual name of the preparation. For example, if any official (B.P.C., B.N.F. or B.P.) product is dispensed, it is not necessary to declare on the label, the concentration of the active ingredients. It is for instance sufficient to label the product as; “AMMONIUM CHLORIDE AND MORPHINE MIXTURE BP 188. Vol.I.” 3. Precise instructions for use by the patient. 4. The date of dispensing. 5. A reference number (if it is a private prescription) 6. The name of the patient. 7. The name and address of the pharmacy. NOTE. The word “POISON” should not appear on the label of a dispensed medicine unless specifically requested. C. Auxiliary Labels: For some preparations, instructions which are specifically detailed on the prescription must be given on the container. Such instructions serve to amplify how the medicine is to be used or to guide the patient regarding the best storage conditions. Auxiliary labels should be sensibly positioned relative to the main label and should not be fixed on the main label. Here are some examples of such auxiliary labels. 10 AUXILIARY LABEL “SHAKE THE BOTTLE” “FOR EXTERNAL USE ONLY” “NOT TO BE TAKEN” (A possible Alternative Label for these products is) “NOT TO BE TAKEN BY MOUTH” CIRCUMSTANCES IN WHICH LABEL IS USED (a) Liquid preparations which are disperse systems. (b) Liquid preparations where precipitations or separation is considered possible. (a) All liquid preparations for external application. EXAMPLES OF PREPARATIONS FOR WHICH THE LABEL IS APPROPRIATE Emulsions, Suspensions Applications, Lotions, Liniments, Skin Paints. (b) Solid and semi-solid preparations for external application. Creams, Dusting Powders, Ointments. (a) Liquid preparation which are not administered orally and which are not applied to a skin surface. Ear Drops, Eye Lotions, Eye Drops, Inhalations, Nasal Drops, Enemas. (b) Solid dosage forms which might inadvertently be administered by oral route. Inhalation, Pessaries, Some Solutions, Tablet, Suppositories. D. Other Labeling Instructions. A number of B.P. and B.N.F. recommendations form the basis of additional labels. 11 INSTRUCTIONS EXPLAINING USE AND ADMINISTRATION ‘Immerse in water for a few seconds, place upon the tongue and swallow with a draught of water’ – Cachets ‘To be added to hot, but not boiling water and the vapour inhaled for 5 to 10 minutes’ – Inhalations (unless otherwise directed). ‘Not to be swallowed in large volumes’ – Gargles (unless other-wise directed). ‘Not to be applied to open wounds or to raw wounds’ – Dusting Powders (surfaces of large area) ‘Warm to body temperature before use’ – Enema (large volumes) ‘Sip and swallow slowly without the addition of water’ – Linctuses. INSTRUCTIONS EMPHASIZING CORRECT STORAGE CONDITIONS ‘Store in a cool place’ - Capsules, creams, ointments, pessaries, suppositories, and all liquid preparations. For certain preparations such as diluted elixirs, diluted creams, eye drops, eye lotions, eye ointments, and freshly prepared mixtures, specific periods are indicated beyond which the preparations should not be used. In such cases, an indication of the expiry date is more helpful than reference to a period of time. A general guide to the packaging and labeling of dispensed medicines follows. Our own practice does not completely fit the official recommendations. In particular, most of our bottles for liquid preparations are quite few and obsolete and are all colourless. It is hoped that more bottles and labels will be obtained in the near future to facilitate correct dispensing practice. 12 Applications: Coloured fluted glass bottles fitted with plastic screw-cape with plastic or other impervious liners. Labeling: “For External Use Only” in red. Cachets: Airtight containers which give adequate physical protection. Containers made of glass, rigid plastics, or extruded aluminum are generally suitable. Use cardboard boxes, which are suitable for short storage periods. Labeling – See Section D above. Capsules: Airtight containers which give adequate physical protection. Containers made of glass rigid plastics, or extruded aluminum is generally suitable. A suitable internal wadding may be required. Labeling: Colour of label black. Creams: Wide-mouthed, squat glass jars fitted with plastic screw caps and suitable liners. Certain plastic containers may also be suitable, provided they prevent evaporation of water vapour; plastic containers are unsuitable for those preparations containing plasticizers such as methylsalicylate or phthalate esters. Labeling: “For External Use Only”. Draughts: White glass bottles fitted with plastic screw caps with plastic or other impervious liners. Such dose should be packed separately or the exact dosage made plain on the label. Dusting Powders: Cylindrical paperboard boxes or plain white glass jars with sprinkler holes on the closure. Labeling: “For External Use Only” Red or black label depending on the nature of the product. 13 Eardrops: Coloured fluted glass bottles fitted with suitable droppers. Plastic dropper bottles are also suitable provided that the plastic is compatible with the content. Labeling: “For External Use Only” Red. Elixirs: Plain white glass bottles fitted with plastic screw-caps with plastic or other impervious liners. Labeling: Black. Enemas: Coloured fluted glass bottles with plastic screw-caps with plastic or other impervious liners. Disposable flexible plastic containers are suitable for some enemas provided that the plastic is compatible with the content. Labeling: See Sections C and D above. Red label. Eye-Drops: Coloured, fluted glass dropper bottles which are capable of being sterilized by autoclaving. Plastic containers are suitable for some eye-drops provided that the plastic is compatible with the content. Note: The glass must be neutral or soda treated screw-capped dropper bottles and must comply with British Standard 1679; Part 5: 1965. Labeling: “Not to be taken” Red label. Eye Lotion: Coloured, fluted glass bottles fitted with plastic screw caps with plastic or other impervious liners. Unprotected bulk closures should not be used for eye lotions. Labeling: “For External Use Only” Red label. Eye Ointment: Sterile collapsible tubes. 14 Gargles: White fluted glass bottles fitted with plastic screw-caps with plastic or other impervious liners. Labeling: “Not to be taken” Red. Directions for dilution may be required. For those gargles directed to be swallowed after gargling plain white bottles should be used. Granules: Airtight containers which give adequate; physical protection containers made of glass, rigid plastics, or extruded aluminum; are generally suitable. Labeling: Depends on the purpose for which the granules are to be used. Inhalations: White fluted glass bottles fitted with plastic screw caps with plastic or impervious liners. Labeling: “Not to be taken”. “Warm to body temperature before use”. Linctuses: Plain white glass bottles fitted with plastic screw caps with plastic or other impervious liners. Labeling: Black “To be sipped swallowed slowly”. Liniments: Coloured fluted glass bottles fitted with plastic screw caps with plastic or other impervious liners. Lotions: Coloured fluted glass bottles fitted with plastic screw caps with plastic or other impervious liners. Labeling: Red. “For External Use Only”. Lozenges: Airtight containers which give adequate physical protection. Containers made of glass, rigid plastics, or extruded aluminum, are generally suitable. Labeling: Black. 15 Mixtures: Plain white non-graduated glass bottles fitted with plastic or other impervious liners. Labeling: Black “Shake the bottle” for those mixtures containing insoluble materials. Mouthwashes: White fluted glass bottles fitted with plastic screw caps with plastic or other impervious liners. Labeling: Red. “Not to be taken”. Direction for dilution may be required. Nasal Drops: Coloured fluted glass bottles with a dropper. Plastic dropper bottles are also suitable, provided that the plastic is compatible with the content. Labeling: Red and “For External Use Only”. Ointments: Wide-mouthed, screw-capped, plain squat glass jars or plastic jars metal or plastic flexible tubes with screw caps. Certain plastic containers containing plasticizers such as methyl salicylate ester are not suitable for some ointments. Labeling: Red and “For External Use Only”. Paints: Coloured fluted glass bottles fitted with plastic screw caps with plastic or other impervious liners. Labeling: “For External Use Only”. Red label for skin paints. Red label “Not to be taken” for throat and gum paints. Pastes: Wide-mouthed, screw-capped, plain squat glass or plastic jar metal or; plastic flexible tubes with screw caps. Labeling: Red and “For External Use Only”. 16 Pastilles: Airtight containers, which give adequate physical protection, containers made of glass, rigid plastics, or extruded aluminum, are generally suitable. Labeling: Black. Pessaries: They should be wrapped individually in waxed paper, in metal foil, or in some suitable form of strip packing. They should be dispensed in partitioned boxes or in suitable plastics containers (for 4g pessaries use 120g ointment jars). Labeling: Red. “Not to be taken”. Powders: Bulk powders should be dispensed in airtight containers, which give adequate physical protection. Containers made of glass, rigid plastics, or extruded aluminum, are generally suitable. Individually wrapped powders should be dispensed in stout paperboard boxes with bonded plastic membrane plastic boxes with bonded plastic membrane, plastic boxes or folding paperboard cartons, which give adequate physical protection. Powders containing deliquescent or volatile materials should be double wrapped in greaseproof paper. Labeling: Black. Instructions for administration should be included. Solution – Tablets: Airtight containers, which give adequate physical protection. Containers made of glass, rigid plastics, or extruded aluminum, are generally suitable. Labeling: Red. “Not to be taken” for tablets used to prepare external solutions. Spray Solutions: White fluted glass bottles fitted with plastic screw-caps with plastic or other impervious liners. Labeling: Red. “Not to be taken”. 17 Suppositories: As for pessaries. Tablets: Airtight containers which give adequate physical protection. Containers made of glass, rigid plastics, or extruded aluminum, are generally suitable. Foil or strip packed tablets should be packed in suitable paperboard boxes or folding paperboard cartons which give adequate physical protection. Internal wadding may be necessary. Labeling: Black. 18 SCHEDULE 1 HOUSEHOLD MEASURES AND WEIGHING OF SMALL AMOUNTS OF MATERIALS. Although medicines are prepared in the pharmacy with professional accuracy, they are administered in the home with available measures, called the household measures. Studies have shown that these household measures may vary in capacity. (a) Measure the Capacities of the Following Household Measures: 1 – Teaspoonful 5ml. 2 – Dessertspoonful 10ml. 3 – Tablespoonful 15ml. (b) Measurement of Drop Volume. Measure the volume of drops obtained from different liquids, e.g. water, alcohol and glycerin, using various droppers. Comment on the result. Equipment for Weighing: Under the weighing and measures regulations (1963), weighing instruments for certain retail transactions are graded, according to design, construction, and performance, into two categories, viz: Balances Beam scales marked “Class B” and Beam scales marked “Class C”. For dispensing purposes, beam scales marked “class B” are generally used and are the types we have in the laboratory. They satisfy the requirements stipulated in the regulations for weighing instruments used for transactions, by retail in drugs and other pharmaceutical products. 19 Class B dispensing balance has a capacity of 50g, a sensitivity of 20mg and a maximum error of 20mg. NB/Sensitivity – is the minimum weight to which the instrument responds. Error: is the possible inaccuracy at full load. Minimum Weighable Quantity: Since it is generally accepted that the error in the amount of any ingredients in a dispensed preparation should not be more than 5%, the minimum weighable amount is 100mg. Smaller amounts than 100mg (or 300mg for potent substances) should be weighed on a high quality analytical balance or obtained by trituration. (c) Weighing of Small Quantities of Powders by Trituration: This is the method employed in pharmaceutical formulations, and a trituration is a term applied to a mixture or dilution of a substance with an inert one. Small quantities of finely powdered solids are mixed on a sheet of white paper by means of a powder knife or spatula. The rule is to add a little of the substance present in lesser amount (usually the more potent substance), and mix intimately. The remainder of the substance present in greater amount is then introduced into the mixture in very small quantities at first but gradually increasing the quantities; until the whole substance is used up (It is impossible to ensure intimate dispersion of one powder in another by mixing the two substances all at once). For powders weighing less than 100mg a trituration must be made using lactose or other inert diluent and an aliquot portion is taken. The trituration may be obtained by making all in 10 or 1 in 100 dilution. PRACTICAL Weigh 15mg of Atropine sulphate. 20 SCHEDULE 2 AROMATIC WATERS Synonym: Aromatic Water These are aqueous solutions, usually saturated, of volatile oils or other aromatic substances in water. Some of them have a mild therapeutic action, but they are mainly used for their flavouring properties as vehicles for the internal administration of medicaments. Preparation of Aromatic Waters: Aromatic waters are prepared by one of the following general methods: 1. Dilution from concentrated waters. The concentrated water diluted with 39 times its volume of water. 2. Solution (There are two methods): (a) The essential oil is shaken with 500 times its volume of water; the shaking is done at intervals during about 15 minutes, and allowed to stand for 12 hours and filtered. (b) The volatile oil is triturated with a sufficient quantity of purified talc or kieselguhr or pulped filter paper and 500 times its volume of water is gradually added while stirring, and filtered. 3. Distillation: The drug or essential oil is distilled with water until the specific volume of distillate has been collected. The distillate is shaken thoroughly, allowed to stand for not less than 12 hours and any excess oil removed. 21 PRACTICAL 1. Prepare 100ml of Chloroform Water BP (Double Strength) Synonym: Chloroform Water. Note: You will have to check the B.P. 1973 for the formula and prepare 100ml ONLY of the formula. 2. Prepare 100ml of Concentrated Peppermint Water BP Synonym: Concentrated Peppermint Water. Note: Check BP 1973 for the formula and prepare 100ml only of the formula. 3. Prepare 100ml of Peppermint Water BP by diluting conc. Peppermint Water BP you prepared in No. 2 above, with 39 times its volume of water. Comment on your practical note books: The storage conditions, action and uses of the preparations. BP Preparation of Normal Saline: Normal saline (0.9% w/v sodium chloride) is isotonic with blood serum, lachrymal secretions (tears) and nasal secretions. It is therefore used as the vehicle for preparations that require adjustment to iso-osmoticity such as parenteral solutions, ophthalmic solutions and some nasal drops. (See Dispensing for Pharm. Students – 324). 4. Prepare 0.9% w/v sodium chloride in purified water; Send 200ml. 22 SCHEDULE 3 SIMPLE MIXTURES CONTAINING READILY SOLUBLE LIQUIDS Synonyms. Mixtures, Oral Liquids, Oral Solutions. Mixtures are liquid preparations intended for administration by mouth and consist of one or more medicaments dissolved or suspended usually in an aqueous vehicle but occasionally in a suitable non-aqueous vehicle. They are normally dispensed in a container, which holds several doses. Classification of Mixtures: 1. Simple mixtures containing soluble substance 2. Mixtures containing diffusible solids 3. Mixtures containing indiffusible solids 4. Mixtures containing precipitate – forming liquids 5. Mixtures containing slightly soluble liquids. SIMPLE MIXTURE CONTAINING SOLUBLE SUBSTANCES ONLY General Method of Preparation: These are prepared by dissolving the weighed solids to about three quarters of t he vehicles, without previous powdering, in a suitable container. The liquid ingredients are added and after measuring each of the liquid, the vessel used is rinsed with a little of the vehicle and the contents are added to the mixture. The mixture is transferred to the dispensing bottle in which it is made up to volume with more of the vehicle and the label is attached. Containers for Mixtures: Plain white glass should be used. The bottle should be fitted with a plastic screw-cap with plastic or other impervious liners. 23 PRACTICAL Dispense the following: 1. Drugs Readily Soluble in the Vehicle ℞ Ammonium Chloride and Morphine Mixture BP 1988 Synonym: Ammonium Chloride and Morphine Mixtures Ammonium Chloride Ammonium Bicarbonate Liquorice Liquid Extract Chloroform and Morphine Tincture Water to Send 50ml Let a mixture be made Label: Three time daily. 30g 20g 50ml 30ml 1000ml Follow the General Dispensing Procedure: (a) Copy the prescription into the LHP of your practical book (b) Check the principles underlying the product (c) Calculate the quantities of materials required and enter these values into the appropriate column of your practical book (d) Write the method of preparation on the top of the LHP of the practical book, and (e) Dispense the prescription. Method of Preparation: (i) Weigh the ammonium salts and transfer to a beaker. Add some vehicle and stir to dissolve the salts. (ii) Measure the liquorices liquid extract in a pipette (check) and transfer to the measure. (iii) Measure the chloroform and morphine tincture, but shake it well first because it separates on standing. Add more vehicle and transfer the 24 mixture into a dispensing bottle. Shake the bottle and make up to volume. (f) Label the product – check label, calculations and critically examine the mixture for faults. (g) Complete the practical book description of the preparation. 2. Solution of Drugs not Readily Soluble in the Vehicle. These may often be more quickly prepared by grinding the solid in a glass mortar before weighing and heating with water to a beaker. This does not apply if the vehicle contains volatile ingredients. ℞ Paediatric Ferrous Sulphate Oral Solution BP 1988 Synonym: Paediatric Ferrous Sulphate Mixture. Ferrous Sulphate 12g Ascorbic Acid 2g Orange Syrup 100ml. Chloroform Water D/S 500ml. Water to 1000ml. Send 50ml. Label – One desert spoonful to be taken after food daily. Cochleire mediumegter in die dost cibos sumendum. Method: Dissolve the ascorbic acid in the double strength chloroform water and use this solution to dissolve the ferrous sulphate. Add the orange syrup and sufficient water to produce 100ml and shake the bottle thoroughly. Note: 1. The ferrous ion could undergo oxidation to ferric, an anti-oxidant, ascorbic acid is therefore included in the formula. The product is meant for children’s use. It is therefore flavoured with orange syrup. The preservative and sweetening agent in chloroform water. 25 2. Paediatric mixtures are usually given undiluted but some contain ingredients that irritate the stomach or intestine and may cause vomiting and diarrhoea unless the preparation is well diluted with water before administration. Paediatric ferrous sulphate solution is an example of such mixtures. The omission of a direction to dilute well with water is a serous error. ℞ Potassium Citrate Mixture BP 1988 Synonym: Potassium Citrate Oral Solution Potassium Citrate 300g Citric Acid Monohydrate 50g Lemon Spirit 5ml Quillaia Tincture 10ml Syrup 250ml Chloroform Water D/S 300ml Water to 1000ml Send 50ml. Label. Three teaspoonfuls to be taken at night. Follow the general dispensing procedure as above. State the following under each preparation in your practical book. 1. Storage conditions 2. Action and uses. 26 SCHEDULE 4 MIXTURES CONTAINING DIFFUSIBLE SOLIDS Diffusible solids are insoluble powders that are light and easily wettable. They readily mix with water and on shaking; they diffuse evenly throughout the liquid for long enough to ensure uniform distribution in each dose (such substances are also known as dispersible solids). Examples of such substances are: Bismuth Carbonate Light Kaolin Light Magnesium Carbonate Magnesium Oxide Magnesium Trisilicate Rhubarb Powder. General Method of Preparation: 1. Finely powder the substance using a mortar (if necessary). Mix the insoluble powders in the mortar. Measure about three quarters of the vehicle, pour a little portion of it into the mortar containing the powders and triturate to form a smooth paste, then gradually add the remainder of the measured vehicle. 2. Add any liquid ingredients; and rinse the measure and mix well after each addition. 3. Rinse the mortar and pestle with successive volumes of the vehicle, transferring the rinsing into the dispensing bottle. 4. Add more of the vehicle to produce the prescribed volume and shake the bottle. 5. Attach the label. NOTE: A direction to “Shake the bottle” should be given on the label. 27 PRACTICAL Dispense the following: 1. ℞ Magnesium Sulphate Mixture BP 1988. Synonym: Magnesium Sulphate Oral Suspension. Magnesium sulphate 400g Light magnesium carbonate 50g Concentrated peppermint emulsion 25ml. Double strength chloroform water 300ml. Water to 1000ml. Let the mixture be made. Label one tablespoonful to be taken two and half hour before breakfast. Send 50ml. Note: Follow the general dispensing procedure as stated in your practical schedule of last week. Follow the method of preparation given above. Comment on the role of each ingredient in this preparation. 2. ℞ Magnesium Trisilicate and Belladonna Mixture PC. Magnesium Trisilicate 500mg. Light Magnesium Carbonate 500mg. Sodium Bicarbonate 500mg. Balladonna Tincture 0.5mlo. Peppermint Water to 10ml. Make the mixture. Label one tablespoonful to be taken three times daily after food. Send 50ml. Follow the general dispensing procedure. A suitable method of dispensing the mixture is as follows: (a) Dissolve the sodium bicarbonate in the vehicle. 28 (b) Rub the magnesium trisilicate and light magnesium carbonate powders down to a smooth paste in a mortar with the sodium bicarbonate solution. (c) Add the belladonna tincture and more vehicle. (d) Transfer the suspension quantitatively to the dispensing bottle and make up to volume. Comment on the role of each ingredient, in this preparation. 3. ℞ Kaolin and Morphine Mixture BP 1988 Synonym: Kaolin and Morphine Oral Suspension. Light Kaolin Sodium Bicarbonate Chloroform and Morphine Tincture Water to Send 50ml. 2.0g. 0.5g. 0.4ml. 10ml. 29 SCHEDLE 5 MIXTURES CONTAINING INDIFFUSIBLE SOLIDS A solid is regarded as indiffusible when it will NOT remain evenly distributed in the vehicle long enough to ensure uniformity of the measured dose. Examples of some common indiffusible substances are as follows: Acetylsalicylic Acid Barbiturates e.g. Phenobarbitone Bismuth Salicylate Phenacetin Podophyllum Resin Prepared Chalk and Aromatic Chalk Salicylic Acid Sulphonamides e.g. Succinyl Sulphethiazole, Sulphadimidine. The viscosity of the medium should be increased to obtain a stable suspension. Therefore, a suitable suspending agent is added. The amount of the suspending agent depends upon the volume of the mixture. The two best suspending agents for general use are: (a) Compound Tragacanth Powder BP. The quantity used is 2g per 100ml. of mixture (i.e. 2% w/v of the preparation). (b) Tragacanth Mucilage B.P. The volume used is 1¼ of the volume of the mixture (i.e. 25 v/v of the preparation) Method of Preparation using Compound Tragacanth Powder BP 1. Finely powder the indiffusible substance, add any soluble or diffusible solids and the compound tragacanth powder and mix intimately. 2. Dissolve any soluble powders in some of the vehicle. Triturate the insoluble powder in the mortar with the solution. 3. Proceed, following the different stage given under the preparation of mixtures containing diffusible solids. 30 PRACTICAL 1. ℞ MIXTURE I Acetylsalicylic Acid Chloroform Water ad. 300mg 15ml. Make the mixture. Send 50ml. Label: t.d.s. 2. ℞ MIXTURE II Acetylsalicylic Acid 450mg Compd. Tragacanth Powder 300mg Chloroform Spirit 0.4ml. Water to 20ml. Make the mixture. Send five doses. Label: t.d.s. Answer the following questions: (1) (2) Comment on the differences in quality between Mixture I & Mixture II. State the role of each ingredient in the three formulations. 31 SCHEDULE 6 PREPARATION OF SYRUPS Synonyms: Syrup; Oral Liquids; or Oral Solutions. Syrups are concentrated aqueous solutions of sucrose or other sugars to which medicaments or flavourings may be added. Glycerin, sorbitol or other polyhydric alcohols are sometimes added in small amounts to medicated syrups to retard crystallization of sucrose or to increase the solubility of other ingredients. PRACTICAL. Dispense the following: ℞ Syrup BP Sucrose Purified Water sufficient to produce 667g. 1000g. Make the syrup Send 50ml. Method of Preparation (Gravimetric) 1. Weigh the appropriate quantity of sucrose, place it in a porcelain dish, and add purified water. 2. Next, counter-balance the dish and its content on the scales and note the total weight. 3. Dissolve the sucrose by heating on a water bath stirring continuously. 4. When the solution is complete allow the dish to cool somewhat return to the scales and add sufficient boiling purified water to make up for that lost by evaporation. 5. Finally, if impurities are present, strain the syrup, while still warm, through fine muslin supported in a funnel into a bottle and shake occasionally until the contents are quite cold. 32 Answer the following questions: (1) What will be the effect on the syrup prepared above? (a) When it is packed in a wet bottle and stored? (b) When stored either in a warm or a cold place? Suggest the best storage conditions for syrup BP. (2) Name the different types of syrups used in pharmacy. (3) State the different methods of preparing syrups. Orange Syrup BP 1. ℞ Orange Syrup BP OrangeTtincture Syrup, sufficient to produce Send: 50ml. 2. 60ml. 1000ml. ℞ Ferrous Phosphate Syrup Compound BP Synonyms: Ferrish’s Food, Farrish’s Syrup; Chemical Food. Sucrose Calcium Carbonate Iron Cochineal Potassium Bicarbonate Sodium Phosphate Orange-Flower Water of commerce, undiluted Phosphoric Acid Water to 700.0g 3.6g. 4.3g. 3.5g. 1.0g. 1.0g. 50.0ml. 48.0ml 1000.0ml. Make the syrup. Send 50ml. Label: One desert spoonful to be taken three times daily. 33 Method of Preparation (Volumetric) 1. Dilute 20ml of the phosphoric acid with 25ml of water, add the iron and heat gently on a water-bath until the iron has dissolved. 2. Add the solution to the calcium carbonate, the potassium bicarbonate and the sodium phosphate, previously triturated with the remainder of the phosphoric acid and 80ml of water. 3. Boil the cochineal with 375ml of water for 15 minutes, cool, strain, and pass sufficient water through the strainer to produce 800ml. 4. Filter the iron solution into the syrup thus obtained add the orange flower water, pass sufficient water through the filter to produce the required volume, mix, allow to stand for at least 8 hours, and filter if necessary. 5. Pack and label the preparation. Answer the following questions: (1) What are the active ingredients of this preparation? (2) Explain why ferrous (iron) and the phosphoric acid was heated separately. (3) What is cochineal and how is the colouring agent sufficiently extracted according to the BP procedure? 34 SCHEDULE 7 PREPARATION OF ELIXIRS AND LINCTUSES Synonyms: Elixirs; Elix., Oral Liquids, Oral Solutions. Elixirs are clear, pleasantly flavoured liquid preparations of potent or nauseous medicaments. The vehicle may contain a high proportion of alcohol or other solvent such as glycerin or propylene glycol, sugars, or other sweetening agents may be present. 1. Streptomycin Elixir, Paediatric BP 1988 Synonym: Streptomycin Mixture, Paediatric ℞ Sucrose 750.0g. Streptomycin Sulphate 31.4g. Sodium Citrate 9.0g,. Methyl Hydroxybenzoate 1.3g. Citric Acid 1.0g. Amaranth Solution 2.0ml. Purified Water to 1000.0ml. Send 50ml. Label: One desert spoonful t.d.s. Dissolve the methyl hydroxybenzoate in 100ml of water with the aid of gentle heat, dissolve the sodium citrate, the citric acid add sucrose in the hot solution and cool. Dissolve the streptomycin sulphate in 100ml of cold water, and mix the two solutions. Add the amaranth solution and sufficient water to produce the required volume and mix. 2. Paracetamol Elixir Paediatric BP Synonym: Elix. Paracetamol Oral Solutions. ℞ Paracetamol Alcohol 120mg 0.5ml. 35 Chloroform Spirit Propylene Glycol Conc. Raspberry Juice Amaranth Solution Invert Syrup Glycerin to Send 50ml. Label: One teaspoonful t.d.s 0.1ml. 0.5ml. 0.125ml. 0.01ml. 1.375ml. 5ml. Dissolve the paracetamol by shaking with the alcohol, chloroform spirit and propylene glycol and add the other ingredients. LINCTUSES: Synonym: Linct. Linctuses are viscous liquid preparations usually containing sucrose and medicinal substances and possessing demulcent, expectorant or sedative properties. They are usually used for the relief of cough. They are administered in doses of small volume and should be sipped and swallowed slowly without the addition of water. 3. Codeine Linctus BP 1988 ℞ Codeine Phosphate 3g. Lemon Syrup 200ml. Benzoic Acid Solution 20ml. Chloroform Spirit 20ml. Water 20ml Tartrazine Solution Compound 10ml. Syrup to 1000ml. Send 50ml. Label: One dessertspoonful t.d.s. Dissolve the codeine in the water and add the other ingredients. 36 SCHEDULE 8 LIQUID PREPARATIONS FOR EXTERNAL USE PREPARATION OF LOTIONS. Synonyms: Lotions, Lt. Lotions are liquid preparations intended for application to the skin for the treatment of skin diseases or as antiseptics, anti-pruritic or protective. They are applied without friction on lint or other soft material or dabbed on the skin. The inclusion of alcohol in a lotion hastens its drying and accentuates its cooling effect, whilst the inclusion of glycerin keeps the skin moist for a considerable time; and also promotes adherence of the residue powder on the skin surface. Lotions may be classified into: (a) Simple solutions (watery lotions). (b) Emulsion type lotions; and (c) Suspensions (shake lotions) i.e. lotions containing insoluble substance. Containers for Lotions Lotions should be dispensed in coloured fluted bottles in order that they may be distinguished from preparations intended for internal use. Labeling: The container should be labeled, “For external use only” and “shake the bottle”. The label on a diluted lotion should also state that the lotion should not be used later than one month after issue for use. 37 1. ℞ Lead Lotion, Evaporating (BP 1988) Alcohol (95%) Strong Lead Sub Acetate Solution Purified Water freshly boiled and cooled to Send 50ml Label: Apply to the affected part. 2. ℞ Calamine Lotion, Oily (BP 1988) Calamine 50g. Wool Fat 10g. Arachis Oil 500ml. Oleic Acid 5ml. Calcium Hydroxide Solution to 1000ml. Prepare 50ml Label: To be used as directed. 125ml. 25ml. 1000ml. Method of Preparation: Triturate the calamine with the wool fat, the arachis oil and the oleic acid previously melted together, transfer to a suitable container, add the calcium hydroxide solution and shake vigorously. Make up to volume with more calcium hydroxide solution and shake again. 3. ℞ Sulphur Lotion, Compound (BP 1988) Precipitated Sulphur 40g. Alcohol (95%) 60ml. Glycerin 20ml Quillaia Tincture 5ml. Calcium Hydroxide Solution to 1000ml. Send 50ml Label: Apply to affected part every night. Method of Preparation. Dispense the precipitated sulphr in the alcohol and the glycerin previously mixed, add the quillain tincture and sufficient of the calcium hydroxide solution to produce the required volume, and mix. 38 SCHEDULE 9 PREPARATION OF LINIMENTS Synonyms: Liniments; Lin. Liniments are liquid or semi-liquid preparation which are intended for external application and may contain substances possessing analgesic, rubefacient, soothing or stimulating properties. Methods of Application Analgesic and soothing liniments may be applied to the skin on a warmed flannel or other suitable material, or by means of camel-hair brush. Stimulating liniments should be applied to the skin with considerable friction by massaging with the hand. Liniments should not be applied to broken skin. Types of Liniments They may be solutions or emulsions, the method of preparation depending on the class to which they belong. The B. P. monograph on liniments and the general recommendations for containers and labeling in the hand-note should be read carefully. N/B Liniments are always packed in coloured fluted glass bottles and labeled “for external use only”. The emulsions are also labeled “Shake the bottle”. A. SIMPLE SOLUTIONS The preparation of this type requires no further explanation. Vehicle: 1. Alcohol 2. Oil. 39 PRACTICAL 1. ℞ Methyl Salicylate Liniment BP (Linimentum Methylis Calicylatis; Lin Methyl. Sal.) Methyl Salicylate 250ml Arachis Oil to 1000ml Make the liniment and send 50ml. Label: To be applied as directed. Dispense the preparation, pack and label. Note the storage condition. B. EMULSIONS Emulsifying Agents Soaps: Soft Soap (Potassium Oleate) In certain cases, soap is formed during preparation of the liniment from alkali and fatty acid (e.g. soap liniment B.P.). Acacia gives a “sticky” preparation unsuitable for external use and is not suitable as an emulsifying agent. PRACTICAL 2. ℞ Soap Liniment, (BP. 1988) Camphor 40g Oleic Acid 40g Alcohol (90%) 700ml Potassium Hydroxide Solution 140ml Rosemary Oil 15ml Purified Water to 1000ml. Make the liniment and send 25ml Label: To be applied to the affected parts. Dissolve the oleic acid in 500ml of the alcohol, and add, with stirring, the potassium hydroxide solution. Dissolve the camphor and the rosemary oil in the remainder of the alcohol, mix the two solutions add sufficient of the water to produce the required volume; mix, allow to stand for not less than seven days and filter. 40 3. ℞ White Liniment (BP. 1988) (Linimentum Album; Lin. Alb.) Synonym: White Embrocation Ammonium Chloride 12.5g Water 625.0ml Turpentine Oil 250.0ml Oleic Acid 80.0ml Dilute Ammonia Solution 45.0ml Make the liniment. Send 50ml. Label: To be applied as directed. NOTE: The B.P. quantities above, allow for just over 1000mls, therefore for 100mls, prepare 1/10 of those quantities. Mix the oleic acid with the turpentine oil, add the dilute ammonia solution mixed with an equal volume of the water, previously warmed, and shake. Dissolve the ammonium chloride in the reminder of the water, add to the emulsion, and mix. Pack 50mls and label. 41 SCHEDULE 10 PREPARATION OF COLLODIONS AND PAINTS 1. PAINTS Synonyms: Pigents, Pig. Paints are liquid preparations intended for application to the skin or mucus surfaces. They are usually medicated with substances possessing antiseptic, astringent, caustic or analgesic properties. Resinous substances such as benzoin, prepared storex or tolu balsam in ethereal solution are employed as bases of medicated varnishes. ℞ Magenta Paint (B.P. 1968) (Pigmentum Magentae, Pig, Magent) Synonyms: Castellani’s Paint, Pigmentum Tuchsinae Resorcinol 80g Phenol 40g Boric Acid 8g Magenta 4g Alcohol (90%) 85ml Acetone 40ml Water to 1000ml Send 25ml. Label: To be used as directed. Dissolve the magenta in the alcohol and the acetone previously mixed. Dissolve the boric acid in a portion of water; dissolve the alcohol and the resorcinol in this solution, add the alcoholic magenta solution and sufficient water to produce the required volume and mix. Label – “For external use only”. 42 2. COLLODIONS These are preparations applied to the skin for the protection of small cuts and abrasions. Collodions are also used as vehicles for the application of drugs when prolonged local action is required. ℞ Salicylic Acid Collodion (B.P. 1988). Salicylic Acid 120g. Flexible Collodion to 1000ml. Prepare 25ml ℞ Flexible Collodion (BP 1988) Pyroxylin Colophony Castor Oil Alcohol (90%) Solvent Ether, sufficient to produce Send 25ml. Label: To be used as directed. 16g 30g 20g 240ml 1000ml. Immerse the pyroxylin in the alcohol and add the colophony and castor oil, and finally sufficient solvent either to produce 1000ml. Shake occasionally until dissolved; allow any deposit of unreacted cotton or of high nitrates of cellulose to settle; decant the clear solution. Preparation of Pyroxylin Pyroxylin is nitrated cellulose obtained by the actions of a mixture of nitric and sulphuric acids on cotton linters, which have been freed from fatty matter. Procedure. 1. Mix 5ml of conc. Nitric acid with 5ml of conc. Sulphuric acid and cool the mixture at room temperature. 2. Immerse 0.40 of absorbent cotton wool in the mixture, keeping the latter cool by standing the vessel in cold water. 43 3. Stir well the wool in the mixture for 10 minutes. In order to ensure even distribution of the acids. Allow to stand for 50 mins. Remove the nitrated wool, press and wash to remove the acids completely and weigh the amount required to prepare the flexible collodion. Storage: Collodions are stored in small light-resistant, well-closed containers and labeled: “For external use only” Store in a cool place Highly inflammable “Keep away from naked flames” Throat Paints Throat paints are used for mouth and throat infection; e.g. Compound Iodine Paint (Mandl’s Paint) for pharyngitis and follicular tonsillitis. ℞ Crystal Violet Paint Compound (BP 1988) (Pigmentum Iodine Compositum; Pig. Ind. Gp.) Synonym: Mandl’s Paint. Potassium Iodide 25.9g Iodine 12.5g Alcohol (90%) 40.0ml. Water 25.0ml. Peppermint Oil 4.0ml. Glycerin to 1000.0ml. Send: 25ml. Label: The Throat Paint. NOTES: (a) Because of the high viscosity of the vehicle this preparation is best made entirely in a measure. For the same reason, excess should be prepared since it is impossible to transfer the entire content of the measure to a bottle. In this instance, 40ml should be made to 44 avoid approximation, the excess is rather large but the remainder is usually kept for future use. (b) (c) A glass can or a counter-balanced watch glass and a vulcanite spatula must be used for weighing the iodine and they should be washed immediately afterwards. Care must be taken to avoid spillage during weighing preparation of the solution. This is because the bench surface can be badly stained by the dye, iodine. Method of Preparation: (a) Put the water into a 50ml conical measure; (b) Dissolve the Kl, add the iodine and stir until completely dissolved (c) In a 10ml conical measure, dissolve 0.2ml of peppermint oil in 2ml of alcohol (90%). Using a pipette transfer 1.76ml to the iodine solution and mix well. (d) Make up to volume with glycerol and mix thoroughly; (e) By difference, transfer 25ml. to the container. Container and storage – see the BP under paints. Labels “Store in a cool place” – because iodine is volatile “Shake the bottle” – because some of the oil separates on storage. “Not to be swallowed in large amounts” – alternatively this advice can be given verbally to the patient, with an explanation. 45 SCHEDULE 11 PREPARATION OF GARGLES, MOUTHWASHES AND EAR DROPS A. GARGLES Synonym: Gargarismaye, Garg. A gargle is an aqueous solution, usually in a concentrated form, intended for use, after dilution, as a prophylactic or in the treatment of an infection of the throat. The particular method of using a gargle intended in brings it into intimate contact with the membranous lining throat. It is not intended to act as a protective covering to the membrane, and therefore oily substances requiring suspending agents, and drugs of a mucilaginous nature should not be used. 1. Potassium Chlorate and Phenol Gargle (BP 1988) (Gargarisms Potassium Chloratis at Phenolis) Potassium Chlorate 30.0g Sulphon Blue (Blue BPS food Grade of commerce) 0.009g Liquefied Phenol 15.0ml. Purified Water to 1000ml. Send 50mls. Label: One tablespoonful to be added to half a tumbler-full of warm water before use. “Not to be swallowed in large amounts”. A stock solution of the dye containing 50mg/100ml. should be prepared. 2ml of this stock solution contains approximately 1mg of sulphon blue required in the preparation. Method: (a) Dissolve the potassium chlorate in about 75ml of warm water. 46 (b) Cool before adding the liquefied phenol. Note: Liquefied phenol is very caustic and measurement in a pipette by mouth must not be attempted. (c) Add the dye solution, filter if necessary, and make up to volume. Containers A white fluted bottle is recommended for gargles unless they are to be swallowed hut since this gargle is to be protected from light, a light resistant bottle is used. Label: Label in red. Add “Not to be taken” (and “shake the bottle” if appropriate). B. MOUTH-WASHES Synonym – Collutaria: Collut. Mouth – washes are usually aqueous solutions, in a concentrated form, of substances with antiseptic, local analgesic or astringent properties. 2. Zinc Sulphate and Zinc Chloride Mouth-Wash (BP 1988) (Collutoruim Zinc Sulphatis et Zinc Chloridi) Collut. Zinc Sulph. Et Zinc Chlori Zincl Sulphate 20.0g Zinc Chloride 10.0g Dilute Hydrochloric Acid 10.0ml Compound Tartrazine Solution 10.0ml Chloroform Water to 1000ml Send 50ml. Label: To be diluted with two time its volume of warm water before use. Does this direction for use correspond with that of the BP? If not, what do you do? 47 Method: (a) Zinc chloride is very deliquescent. Crush a stick quickly in a mortar weigh the required amount and immediately return the excess to the bottle and close tightly. (b) Proceed as for gargles. Container White fluted screw-capped bottle. Label: The print on the label should be in red. Add “Not to be taken” (“Shake the bottle” if required) so that the product is clearly distinguishable from a preparation. Intended for internal use. C. EAR DROPS Synonyms – Auristillae, Aurist. Ear-drops are solutions, or suspensions, or suspensions of medicaments in water, glycerin, diluted alcohol, propylene glycol, or other suitable vehicle, which are intended for instillation into the ear. 3. Sodium Bicarbonate Ear-Drops (B.P. 1988) Sodium Bicarbonate Glycerin Purified Water, freshly boiled and cooled to Label: Three or four drops to be put into the affected day. 5.0g 30.0ml 100.0ml ear three times a Method: Dissolve the sodium bicarbonate in about 6.0ml of the water, add the glycerin and sufficient of the water to produce the required volume and mix. Note: The ear-drops should be recently prepared. Containers and Labeling See the B.P. and the general recommendation in the manual. 48 SCHEDULE 12 PREPARATION OF INHALATIONS AND NASAL DROPS Inhalations are liquid preparations containing volatile ingredients for the medication of the respiratory tract. The ingredients may be volatile at room temperature in which case they may be inhaled from an absorbent pad on which the inhalation has been placed, or they may require volatilization by adding the inhalation to hot (not boiling) water and the vapour inhaled for five to ten minutes. Volatile oils and terpene derivatives are commonly prescribed ingredients and they must NOT be emulsified with gums or suspended with compound powder of tragacanth. Container – A white flutted bottle. Label: (1) “Shake the bottle” if insoluble ingredients are ;present (2) “Not to be taken” (3) The B.N.F. directs that unless otherwise required the wards “Add one teaspoonful to a pint of hot, not boiling water and inhale the vapour” shall be written on the label. PRACTICAL ℞ Menthol 2% Thymol 1.5% Compound Tincture of Benzoin to 25ml. Send 25ml. Make the inhalation Label: To be used as directed. Note: No dispersion agent is necessary in this product. 1. 49 Method: (1) Measure about 20mls of compound tincture of benzoin (2) Weigh the menthol, add to the inhalation and stir until dissolved (3) Repeat with the thymol. (4) Add sufficient compound tincture of benzoin to adjust the final volume to 25mls. Pack into a ribbed bottle, label and polish. ℞ Menthol and Eucalyptus Inhalation (B.P. 1988) Menthol 2% Eucalyptus Oil 10% Light Magnesium Carbonate 7% Water to 50ml. Send 50ml. Label: Add one teaspoonful to a pint of hot, not boiling water and inhale the vapour. Note: As menthol and eucalyptus oil are immiscible with water. Light magnesium carbonate must be added. Method: (a) Measure the oil of eucalyptus and transfer it to a glass mortar. (b) Weigh the menthol, add to the oil and stir with a glass pestle until dissolved. (c) Weigh the light magnesium carbonate and carefully “float” it on to the surface of the oil. Triturate gently with the glass pestle until a smooth cream is obtained. (d) Gradually incorporate water, adding initially about the same volume of ingredients in the mortar. (e) Transfer to a measure, wash the mortar with further quantities of water adding the washings to the measure until 25mls is obtained. Questions: (1) Which is the alcoholic ingredient in preparation No.1 and what is its function in the product? (2) What is the function of light magnesium carbonate in product No.2 and is there any alcoholic ingredient in the preparation? 50 NASAL DROPS These are solutions of drugs possessing antiseptic, local analgesic or vasoconstrictor properties. They are usually simple solutions of medicaments in water, diluted alcohol or glycerin and are intended for instillation into the nostrils for their local effect. Oily liquids (e.g. light liquid paraffin) should not be used as vehicles for nasal drops. Container – Nasal drops should be dispensed in coloured fluted bottles with dropper. Label: The label should include the instructions “NOT TO BE TAKEN” or “FOR USE ONLY IN THE NOSE” and “STORE IN A COOL PLACE”. PRACTICAL 3. ℞ Ephedrine Nasal Drops (BP 1988) Ephedrine Hydrochloride 0.5% Chlorbutol 0.5% Sodium Chloride 0.5% Water to 20ml. Send 20ml. Label: Two drops to be placed in each nostril as directed. Method (1) Heat about 15mls of water in a conical flask to about 60oC. (2) Weigh and add the chlorbutol to this warm water in the conical flask, close by inserting a stopper and shake vigorously until it has completely dissolved. (3) Dissolve the ephedrine hydrochloride and sodium chloride in the warm solution. (4) Cool, filter and make up to volume through the filter. Questions: 1. Why are oily liquids not used as vehicles for nasal drops? 2. Why is ephedrine nasal drops not recommended to be used repeatedly? 51 SCHEDULE 13 PREPARATION OF ENEMAS AND IRRIGATIONS ENEMAS Enemas are solutions, suspensions or oil-in-water “emulsions” of medicaments intended for rectal administration. Enemas are given for their anthelmintic, anti-inflammatory, nutritive, purgative or sedative effects or for X-ray, examination of the lower bowel. There are two types: (a) Retention enemas and (b) Evacuant enemas The volume given varies according to the type of enema. Retention enemas do not normally exceed 100ml in volume while evacuant enemas may be as much as 2 litres. Such large volume enemas should be warmed to body temperature before administration in order to avoid discomfort to the patient. This is achieved by standing the container in warm water before use. PRACTICAL 1. ℞ Paraldehyde Solution Sodium Chloride Solution (0.9% w/v) to Send 50ml. Label: To be administered rectally as directed. 10ml. 100ml. Method: (1) Weigh the sodium chloride and dissolve it in a suitable volume of water to obtain a 0.9% solution. (2) Filter the normal saline solution using either a filter paper or cotton wool. 52 NOTE: Usually, a clarify grade sintered glass or membrane filter is used, paraldehyde is more soluble in cold than warm water therefore to aid its solution cool the sodium chloride solution under a running tap. (3) Put the paraldehyde in the bottle, adjust to volume with the vehicle and shake vigorously until solution is complete. Container: Coloured, fluted, screw-capped, glass bottles. Label: Red label. “Not to be taken” or for rectal use only” “Store in a cool place in complete darkness” Expiry Date: Discard after two days”. 2. ℞ Castor Oil 20% Starch 2.5% Water to 100ml. Make the enema. Label: The enema. To be used at bed time as directed Note: (The dose of this enema is usually 300ml.) METHOD: 1. Triturate the starch is a mortar with about 20ml. of water to make a thin smooth paste. Transfer to a measure and add sufficient water to produce 80mls. 2. Transfer to a beaker and heat over a Bunsen with frequent agitation until the contents of the flask boil, when the starch will gelatinize and form a mucilage. 3. Remove from the heat and cool the contents of the beaker under a stream of cold water, rotating constantly. (This prevents formation of a “skin”). 4. Adjust the volume to 80mls. with water, add the castor oil mix by vigorous stirring and transfer to a bottle and label. Container: - Coloured, fluted, glass bottles. Label: “Warm to body temperature before use” 53 Red label “Not to be taken” Note: The description “emulsion” is frequently applied to suspension of oil in starch mucilage. Starch mucilage is not a true emulsifying agentproducts made with it are really suspensions of large oil globules which are prevented from coalescing by the high viscosity of the starch by the high viscosity of the starch mucilage. Questions: 1. What type of enema is preparation No.1, and why is it not essential to warm this solution before administration? 2. What type of enema is preparation No.2? IRRIGATIONS Irrigations are aqueous solutions used as venial or urethral douches. They may have soothing, antiseptic or astringent action on the mucous membranes. They are generally required to be dissolved or diluted before use at body temperature. Container: White, fluted screw-capped bottle. Label: Printing in red. “Not to be taken” To be warmed to body temperature before use. PRACTICAL 3. ℞ Send 100mls of a 1.0% solution of zinc sulphate. Label with directions for preparing half of a pint of a vaginal douche containing 1% of zinc sulphate. 54 LATIN TERMS USED IN PRESCRIPTIONS (Cooper and Guns Dispensing for Pharmaceutical Students 19th Edition) (pp.720-723). Traditionally prescriptions are written in Latin and consist of the following parts. A heading which is the sign Rx, a formula, directions to the dispenser, labeling instructions, the patients name and the prescriber’s name. Prescriptions are usually dated. In recent years physicians have tended to write their prescriptions in English or with very abbreviated Latin instructions. Understanding of the terms used is best obtained by practice on prescriptions, referring where necessary of the book listed above or other sources. A brief list is given below: LATIN TERM Ante cibum Ante jentaculum ana adde amplus (a, um) ante application aqua aquae adauris auristillae bis bis in die calidus (a. um) capiat capsule cibus cochleare cochleare amplum “ “ “ medium) “ modicum) “ parvum) ABBREVIATION a.c. a.j. a.a. add amp. applic. aq. aq. ad. aur. aorist b. b.i.d. calin. cap cap. cib. cock. amp mag. med. min. parv. TRANSLATION before food before breakfast of each add full large before an application water water up to the ear ear-drops twice twice a day warm or hot let him take a capsule food Spoonful a tablespoonful a dessertspoonful a teaspoonful 55 collutarium collyrium comperais cremor de die diebus alternaia dolere urgente duplex emeticum emplastrium enema ex aqua fiat (fiant) fiat mistura fist secundum artem flavus gargarisma gultae hera somni haustus inter nibos infusum infricetur injectio insufflatio irrigation liquor lotio mane more dicto more dicto utendus misture mitte molls. nocte nocte maneque nomen proprium naristillae nebular collut. a mouth wash collyr. an eye lotion conspers. a dusting powder crem. a cream d.d. daily diab altern. every other day dol. urg. when the pain is severe dup. Double emet. an emetic emp. a plaster enem. an enema ax. aq. in water f.f.; ft. let it (then) be made f.m. or ft. mist. let a mixture be made f.a.a. let it be made according to art. flav. yellow garg. a gargle ftt. drops h.s at bed time haust. a draught i.c. between meals inf. an infusion infric. let it be rubbed in inj. an injection insuff. an insufflation irrig. an irrigation liq. a solution lot. a lotion m. in the morning m.d. as directed m.d.u. to be used as directed mist. a mixture mitt. send moll. soft n. at night n.et m. night and morning n.n. (NP) the proper name narist nasal drops neb. a spray 56 omni mane omni nocte oculentum oleum parti affecta applicandus(a.um) post cibum pro re nata pas ta pessus pigmentum pulvis quarter die quartum sufficiat quarta quaque hora recipe sumendus si opus sit signa solvella statim o.m. every morning o.n. every night oculent an eye ointment ol. oil n.a.a. to be applied to the affected part. p.c. after food p.r.n. occasionally, when required past. a paste pess. a possary pig. a paint pulv. a powder q.d. four times a day q.s. sufficient q.q.h. every fourth hour Rx. take s. to be taken s.n.s. if necessary sin. label solv. solution-tables stat. immediately. A more comprehensive list of Latin terms phrases that you may find in prescriptions or dispensing practice. S/N. 1. 2.` 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. LATIN NAME, TERM OR PHRASE Quantum sufficiat ad ana auristillae collutorium collyrium quttae liquor lotio mistura naristillae nebula oculentum pigmentum pulvis ABREVIATIONS q.a. ad a.a. auristill collut. collyr. qtt. liq. lot. m., mist. narist neb. oculent. pigm. pulv. ENGLISH NAME OR MEANING as much as sufficient up to, sufficient to produce of each ear drops a mouth wash an eye lotion drops a solution a lotion a mixture nasal drops a spray solution an eye ointment a paint a powder 57 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. solvellas trochiscus unguentum fiat misce fiat mistura mitte signa semel in die bis in die or bis die ter in die or ter die quarter in die or quarter die bis tar ve in die prima mane mane omni mane vespere nocte hora decubitus, hora somni nocte maneque mane sequenti jentaculum prandium omni hora or quaque hora ante cibos ante cibum post cibos, post cibum more dicto, modo dicto. pro re nata si. opus sit statim ex aqua dexter parti arfectae applicandus sinister unus duo decem undecim duo decim viginti unus et viginti more dicto utendus solv. solution tablets troch a lozenge uno. an ointment ft. let(it) be made or let (them) be made. m.ft.m. mix to make a mixture mitt. send sig. Label sem. In die once a day b.i.d., b.d. twice a day t.i.d., t.d. three times a day q.i.d. or q.d. four times a day b.t.i.d. two or three times a day prim. m. early in the morning m. in the morning o.m. every morning vesp in the evening n. at night n.d., h.s. at bed time n.m. night and morning m.seq. the following morning jentac. Breakfast prand. Dinner o.h. or q.q.h. every hour a.c. before meals a.c. before food p.c. after food m.d. as directed p.r.n. occasionally s.o.s when required or when necessary stat. immediately or at once ex. aq. with water dext. Right p.a.a to be applied to the affected part sinist. Left 1 one II two x ten xi eleven xii twelve xx twenty xxi twenty-one m.d.u. to be used as directed 58 300 LEVEL 59 LIQUID EMULSIONS An emulsion consists of two liquid phases, one of which is finely subdivided and dispersed in the other, the system being stabilized by the presence of an emulsifying agent. Emulsions intended for oral administration should be of o/w (oil-in-water) type. For container labeling and storage requirements consult, B.P. 1988, pages 10 (or 616) and 717, and P.C. (11th ed.) pp. 630 – 632. EXERCISES ON O/W TYPE EMUSLIONS (A) O/W Emulsions – Based on Acacia and Methyl Cellulose. Oil-in-water emulsions which are prepared in bulk must always be preserved using a suitable, non-toxic preservative, methyl paraben and/or propyl paraben are suitable for most emulsions, but care must be taken to ensure that the preservation is compatible with the ingredients of the emulsion. Emusions which are intended to be used within a fortnight of preparation need not be preserved, but the use of chloroform water B.P. is to be recommended for these small quantities. The amounts of the parabens to be used in large scale manufacture will be found in your lecture notes. Exercise 1: ℞ Cod Liver Oil 50ml. Water to 100ml. Make an Emulsion. Send 50ml. 10ml. to be taken twice a day. Notes: 1. For preparing an emulsion using gum acacia powder as the emulsifying agent, it is necessary to make a concentrated primary emulsion first which is then diluted to the required volume. 2. Cod liver oil is a fixed oil. The ratio of the oil, water, emulgent (gum acacia powder) for the primary emulsion of any fixed oil is 4:2:1 (in exceptional cases, e.g., castor oil and liquid paraffin, a more stable emulsion is formed if 3:2:1 ratio is used). 3. Calibrate the bottle first and make up the volume in the bottle. 60 Dry Gum Method: 1. Weigh the required quantity of gum acacia powder in a dry mortar. 2. Measure the oil in a dry measure, transfer into the mortar and triturate with the gum lightly. 3. Measure the calculated quantity of water in a clean measure and add all at a time to the content of the mortar and triturate until a thick, white “clicking” primary emulsion is formed. 4. Dilute with some more quantity of water and transfer into the bottle. Add sufficient water to make up the volume. Wet Gum Method: This method may be used when a large quantity of emulsion is prepared. 1. Some as dry gum method. 2. Measure the water, transfer into the mortar and triturate with the gum to form a mucilage. 3. Measure the oil and add small quantity at a time to the content of the mortar, and triturate. This is repeated until the whole quantity of the oil is mixed. 4. Same as dry gum method. Exercise 2: I. (Tincture of Quillaia (Mucilage of Acacia (2% Mucilage of Methyl Cellulose II. 0.5ml. 6ml. 30ml. Cod Liver Oil 50ml. Water, purified to 100ml. Prepare an emulsion. Send 50ml. Label for a hospital ward. METHOD: Mix I in a calibrated bottle. Add II in 3 to 4 portions. Shake vigorously after each addition for about 30 seconds. Make up the volume with water and shake well. 61 Note: Quillaia root contain saponin, a surfactant, which facilitates emulsification. Compare the stability of the two emulsions prepared in exercises 1 and 2. Exercise 3: Liquid Paraffin 50ml. Orange Syrup 20ml. Water to 100ml. Prepare an emulsion. Send 50ml. 5ml. b.i.d. Note: Use 3:2:1 ratio for the primary emulsion. Exercise 4: I. (Tincture of Quillaia (Mucilage of Acacia (2% Mucilage of Methyl Cellulose II. III. 0.5ml. 6ml. 30ml. Liquid Paraffin 50ml. Cinnamon Water to 100ml. Make an emulsion. Send 50ml. Label for a ward. METHOD: (See Exercise 2). 1. Pass half of the emulsion through a hand homogenizer and compare the globule sizes of the dispersed phase with those of the other half. Exercise 5: Repeat exercise 3 using 30% oil ricine (castor oil) in place of liquid paraffin. Exercise 6: Repeat exercise 4 using castor oil in place of liquid paraffin, label for a hospital ward, find the type of the above two emulsions by dilution and staining taste. 62 Exercise 7: Arachis Oil 3ml Phenolphthalein 50mg. Sodium Citrate 200mg. Water to 10ml. Make an emulsion. Label as such. Send 50ml. (B) O/W Emulsions Based on Monovalent Soaps: Exercise 8: ℞ I. (Triethanolamine (Oleic Acid II. III. 0.5g. 2.0g. Benzyl Benzoate 25.0ml. Water 25.0ml. Water to 100ml. Make an emulsion. Send 50ml. To be used as directed. METHOD: Mix I, add II and shake. Add III and shake intensively. Mix more water by shaking to make up to volume. Find the type of the above emulsion by dilution and staining tests. Exercise 9: ℞ I. (Oleic Acid (Arachis Oil II. 1 74 Liquid Ammonia (10%) 25 Make an emulsion. Send 50ml. To be used as directed. METHOD: Mix I and II and shake vigorously. 63 Arachis oil may not contain the required quantity of free fatty acids hence the addition of an extra quantity of oleic acids. However, if the oil is of good quality emulsion will form without the addition of oleic acid. (C) Emulsions Based on Multivalent Soaps and Cholesterol Compounds: Exercise 10: ℞ Oleic Acid 1% Arachis Oil 50% Lime Water to 100% Send 50ml. METHOD: Mix all the three ingredients in a bottle by shaking vigorously. Exercise 11: ℞ Wool Fat 6 parts Liquid Paraffin 50 parts Water 44 parts Make an emulsion. Label as such. Send 50ml. METHOD: Melt the wool fat over a water bath; add liquid paraffin and transfer into a dry bottle. Add water of same temperature as the water bath in three to four portions, with intensive shaking. Note: 1. Wool fat can emulsify about half its own weight of water; when mixed with fats, e.g. liquid paraffin, it can emulsify several times its own weight of an aqueous liquid. The resultant emulsions are of the water-in-oil type. 2. Wool fat consists mainly of fatty acid esters of cholesterol, lanesterol and fatty alcohols, which exert emulsifying property. 64 Exercise 12: Wool Alcohols 3% Liquid Paraffin 52% Water 45% Send 50ml. Follow the same method as described under exercise 11. Wool alcohols contain about 30 – 35 percent of cholesterol and 10 – 13 percent of isocholesterol. A portion of this emulsions will be passed through a hand homogenizer and both the non-homogenized and the homogenized emulsion, place on glass slides, will be mounted on microscope. Students are required to see the sizes of the disperse phase globules on these and comment. Exercise 13: Cholesterol 1% Liquid Paraffin 54% Water 45% Send 50ml. of the emulsion. METHOD: Dissolve cholesterol in liquid paraffin in a flask placed over a water bath and cool. Transfer to a bottle and add water of same temperature and the bath in portions with intensive shaking. Find the type of the above three emulsions by dilution and staining tests. 65 SEMI-SOLID PREPARATIONS (OINTMENTS, CREAMS AND PASTES) Most of these products are intended for external application to the skin. Ointments are semi-solid preparations usually containing a medicament dissolved or dispersed in fatty bases. Water-soluble ointments may be prepared using a base consisting of mixtures of polyethylene glycols (Macrogols). Emulsifying agents are incorporated in some anhydrous fatty bases to make them miscible with exudates and more easily removable from the skin by washing. Creams are semi-solid emulsions which may be of an oil-in-water (o/w, aqueous creams) or water-in-oil type (w/o, oily creams); o/w emulsifying agents used in creams include sulphated alcohols, quaternary ammonium compounds, monovalent soaps and non-ionic surface active agents, often in combination with fatty alcohols or fatty acids. Oily creams are prepared with wool alcohols beeswax, calcium soaps, certain sorbitan esters and other emulsifying agents. Preservation of creams is often a problem, particularly the aqueous type, as they are often attacked by moulds and other microorganisms. For this reason, a preservative is usually included in o/w creams. Certain medicaments are also incompatible with some emulsifying systems. Pastes are similar to ointments but often contain a very high proportion of powdered medicaments. Note: For a complete description of these products and the relevant container, storage and labeling requirements, students are advised to read the general monographs on pages 232 and 614 of P.C. 1979 and pages 10 (or 616), 650 and 704 of B.P. 1988. Note also the remarks on ointments used in tropical countries on page 8138 of the B.P. 1973. One method of classifying ointments has been given to you in your course work. In your laboratory notebook, at the end of each write-up, state to which class the ointment or cream belongs. It is necessary to make a reasonable allowance for unavoidable losses by preparing a slight excess. For example, if you are required to send 25g, a 66 reasonable amount to prepare would be 30g out of which 25g is transferred to the jar. (A) Ointment Bases of Lipoid Character (Fatty or Hydrocarbon Bases): Send 25g each of the following ointment bases: Ex. 1 Simple Ointment B.P. Ex. 2 Paraffin Ointment P.C. Ex. 3 Wool Alcohols Ointment P.C. (B) Medicated Ointments of Lipoid Character: Send 25g each of the following: Ex. 4 Zinc Ointment B.P. Ex. 5 Calamine Ointment P.C. Ex. 6 Calamine and Coal Tar Ointment P.C. Ex. 7 Methyl Salicylate Ointment P.C. (C) Ointment with Polyethylene Glycol (Macrogol) Bases: Send 25g of each of the following: Ex. 8 Macrogol Ointment P.C. Ex. 9 Sulphur, finely sifted Macrogol Ointment P.C. to Label as appropriate. 1.0g. 30.0g. Note: The high degree of solubility of macrogol bases in water preclude the addition of aqueous solutions much in excess of 5% of the total formula. The following base composition is recommended when larger amounts of aqueous solution are to be incorporated; Macrogol 4000 47.5 Macrogol 400 47.5 Cetyl Alcohol 5.0 67 (D) O/W Cream Bases: Send 25g of the following: Ex. 10 Emulsifying Ointment B.P. Emulsifying Wax 300g. White Soft Paraffin 500g. Liquid Paraffin 200g. Label as such. METHOD: Melt together and stir until cold. Note: This ointment is ANIONIC in character due to the presence of emulsifying wax which contains sodium lauryl sulphate as one of its ingredients. As such, this is lipoid in character but on addition of water it forms an o/w cream base (see following exercise). Ex. 11: Aqueous Cream B.P. Emulsifying Ointment Chlorocresol Purified Water Label as such. Send 25g. (Hydrous Emulsifying Ointment) 300g. 1g. 699g. This is an o/w emulsion of paraffins and it is used as a water-miscible cream base. It is preserved with chlorocresol. The emulsion is prepared by melting the fatty ingredients at about 60oC, adding the requisite amount of aqueous phase heated to the same temperature and stirring the mixture until it is cold. The quality of the emulsion depends largely on the degree of shearing applied at a critical temperature when the emulsion begins to solidify. The chlorocresol cannot be directly weighed and must be obtained by trituration. The emulsifying ointment required should be obtained by trituration. The emulsifying ointment required should be obtained from the preparation made in Ex.10 above. 68 METHOD: (i) Dissolve the chlorocresol in an appropriate volume of purified water over a hot water at 60oC. (ii) Weigh and melt the emulsifying ointment in a tarred porcelain dish over the same water bath. (iii) Mix the chlorocresol solution with the molten fatty materials at the same temperature. Add more purified water, warmed to 60oC, to make the product up to the final weight. (iv) Stir until cold (over a cold water bath, if necessary) using a glass rod or a glass pestle as stirrer. Note: As the cream is ANIONIC in character, this base is incompatible with cationic drugs, e.g. cetrimide, antihistamines, acridines etc. Ex. 12: Cetrimide Emulsifying Ointment B.P. White Soft Paraffin 500g. Cetostearyl Alcohol 270g. Liquid Paraffin 200g. Cetrimide 30g. NOTE: This ointment is CATIONIC in character due to the presence of cetrimide. This is also lipoid in character. Ex. 13: Cetrimide Cream B.P. Cetrimide Cetostearyl Alcohol Liquid Paraffin Purified Water freshly boiled and cooled to Send 25g. Label as appropriate. 5g. 50g. 500g. 1000g. METHOD: Melt the cetostearyl alcohol over a heated water bath, add the liquid paraffin, and warm; dissolve the cetrimide in the water at the same temperature and add to the melted oily mixture, stirring gently (over a cold water bath, if necessary) until cold. 69 NOTE: This cream can also be prepared by mixing 30% Cetrimide Emulsifying Wax P.C. with 70% purified water. Ex. 14: Cetomacroscol Emulsifying Ointment B.P. White Soft Paraffin 500g. Cetemacrogol Emulsifying Wax 300g. Liquid Paraffin 200g. Send 25g. Label as such. Melt together and stir until cold. NOTE: This is non-ionic in character. Like those prepared in Ex.10 and 12, this can also be converted to an o/w cream base on the addition of water. Ex. 15: Cetomacrogol Cream B.P. (using formula A of the B.P.) Cetomacrogol Emulsifying Ointment 300g. Chlorocresol 1g. Purified water freshly boiled and cooled to 1000g. Send 25g. Label appropriately. METHOD: Same as in Ex. 11 and the Cetomacrogol Emulsifying Ointment is obtained from Ex. 14 above. NOTE: To help to prevent production of a granular preparation, the temperature of the melted ingredients should not exceed 65oC and the Chlorocresol should be dissolved in not less than 50ml of warm water before adding to the melted emulsifying bases. NOTE: This base is non-ionic in character and compatible with most ionic drugs. QUESTION: Explain why a preservative (chlorocresol) is included in the aqueous cream and Cetomacrogol Cream but not in Cetrimide Cream. 70 Ex. 16: Send 25g of the following cream base. Stearic Acid 10 Cetyl Alcohol 5 Glycerin 10 Light Mineral Oil 20 Triethanolamine 2 Water to 100 To be used as directed. Ex. 17: Vanishing Cream Base. Stearic Acid 15.0 White Beeswax 2.0 Triethanolamine 8.0 Propylene Glycol 1.5 Water 65.5 Send 25g. To be used as directed. (E) Medicated O/W Creams Ex. 18: Send 25g of Calamine Cream, Aqueous P.C. Label appropriately. Ex. 19: ℞ Sulphur 2.0 Phenol 0.5 Cetyl Alcohol 8.0 White Beeswax 0.5 Propylene Glycol 5.0 Sodium Lauryl Sulphate 1.0 Water to 80.0 Label. Apply to scalp as directed. Dispense 25g. 71 1. SHAVING PREPARATIONS A. LATHER TYPE A shaving product is a preparation, which softens the beard sufficiently and provides lubricity so that the razor can glide and cut easily along the face. A shaving product should not be irritant to the face and should retain its moisture during application. Coconut oil possesses short-chain irritant free fatty acids. In some formulations therefore, olive oil is included to reduce the irritant effect of coconut oil. The hydroxides react with the stearic acid and free fatty acids to form soap. Sodium hydroxide form hard soap while potassium hydroxide forms soft soap. This helps to give the final cream consistency. 1. ℞ Stearic Acid Coconut Oil Glycerol Potassium Hydroxide Sodium Hydroxide Water ad Send 25g. 35g. 10g 10g 6.8g 1.6g 100g. METHOD OF PREPARATIONS: 1. Melt ¼ of the stearic acid together with the coconut oil on a water bath. 2. Dissolve the required quantities of KOH and NaOH in a mixture of water and glycerol. Heat the solution and add to the molten oils. 3. After complete saponification add the remaining amount of stearic acid in melted form, to the formed soap and triturate in a mortar. 4. Dispense 25g of the product in a cream jar. B. BRUSHLESS TYPE SHAVING CREAM At the time of their introduction, brushless shaving creams were thought to be quite revolutionary. They undoubtedly suit some dry skins and those that are abnormally sensitive to soap. In general brushless creams have a more pronounced lubrication action than lather creams, and can be distinguished from ordinary vanishing creams, which they otherwise 72 resemble, by their higher oil content. The addition of wetting agents to these creams is a source of skin irritation and is not to be recommended. The following formula provides a useful starting point for individual experimentation in that it contains a humectant and lubricant in a relative non-greasy, self-emulsifying base. 1. ℞ Glyceryl Monostearate Spermaceti Olive Oil Glycerin Water Preservative Perfume Make 25g. 12% 4.5% 2.5% 7.0% 73.5% 0.1% 0.1% METHOD OF PREPARATION: Melt the glyceryl monostearate with the spermaceti and olive oil at 75oC. Heat the glycerin, water and preservative together at the same temperature, mix and stir until a homogenous product is obtained. The perfume is added 45oC whilst the product is still soft. 2. AFTER-SHAVE PREPARATIONS After-shave preparations are intended to relieve the felling of discomfort caused by shaving. They should refresh and cool the skin, sooth minor irritation and give a feel of well-being. After shave lotions also act as mild astringent and neutralizing agent to the soap left on the skin. 1. ℞ AFTER-SHAVE LOTION Stearic Acid 3g. Cetyl Alcohol 0.5g. Glycerin 2g. Potassium Hydroxide 0.2g. Ethyl Alcohol 5ml Water to 100ml. Send 50ml. 73 METHOD OF PREPARATION: 1. Melt the required quantities of stearic acid and cetyl alcohol on a water bath. 2. Dissolve the potassium hydroxide in about 6ml of water; add the glycerin and heat gently to the same temperature of the melted oils. 3. Mix the above two liquid preparations with gentle stirring until saponification is achieved. 4. Add to the mixture, the required amount of the 20% mucilage of tragacanth and the remaining portion of water with continuous stirring. 5. Allow the preparation to cool and add the required volume of ethyl alcohol. Unfortunately, it has recently been shown that after-shave lotions are not all soothing, or even act to leave behind a refreshing odour. A consumer organization known as ‘which’ carried out a survey in U.K. in 1961 and found that of 45 products tested, the pH varied between 3.7 and 8.8 and the alcohol content was between 40 – 75%. In general, after-shave lotions resemble the skin tonics used by women. A typical formula is the following: 2 3. (Not to be made) Glycerin Menthol Alcohol Witchazel Extract Water Preservative Perfume (water soluble) 5% 0.05% 40% 18.5% 35% 0.05% 1.4% PRE-SHAVE LOTIONS (not to be made) For electric razors, the shaving conditions are totally different. The beard must be dry, the hairs stiffened and raised so that each individual hair can be caught in the razor combs and clearly removed by the cutting edge. 74 Pre-shave lotions must “set up” the beard, make a coating on the skin on which the razor glides and act as a lubricant for the cutting head of the shaver itself. A basic formula to which small amounts of astringents, menthol, etc. can be added is: Isopropyl Myristate 10% Alcohol 90% The high proportion of alcohol in this type of preparation is less objectionable than it would be in an ordinary after-shave lotion. DEPILATORIES The term “depilatory” refers to preparations intended for the chemical breakdown of superfluous hair without injury to the skin. The desirable requirements of a depilatory may be defined as follows: 1. Non-toxic and non-irritant to the skin. 2. Reacts preferentially with the hair and will be sufficiently rapid to cause disintegration to the hair before causing any damage of the underlying and surrounding skin. 3. Preferably odourless 4. Harmless to clothing 5. Cosmetically elegant. Depilatories usually contain as one of their active ingredients, an alkaline reducing agent which will cause the hair fibers to swell and produce a preliminary step to the complete degradation of the hair. Sulphides and stannites have been used for a long time. The majority of depilatories available today are substituted mercantans, for example, calcium thioglycollate in conjunction with calcium hydroxide. Depilatories based on the enzyme keratinase have also been developed which do not have the unpleasant odour of sulphide or even thioglycollate depilatories and are non irritant. 75 Thioglycollate depilatories are non-toxic and possess less odour than the sulphide type but take longer to act. At the concentration in 5 – 15 minutes depending on the pH of the preparation. This should be about pH 12.5. A convenient formula of the calcium thioglycollate type is as follows: Calcium Thioglycollate Calcium Hydroxide Calcium Carbonate, Precipitated Cetyl Alcohol Sodium Lauryl Sulphate Sodium Silicate Water Perfume to Send 25g. 7.0% 7.0% 20.0% 5.0% 1.0% 2.5% 100.0% Procedure: The sodium lauryl sulphate, sodium silicate and cetyl alcohol are made into a paste with the rest of the water. The two phases are then mixed and passed through a triple roll mill to remove lumps and gritty particles. NB. 1. The pH is maintained by a slight excess of calcium hydroxide, which acts as a reserving of alkalinity. 2. Chalk or other fillers may be added together with thickening agent to produce thioglycollate depilatories in a paste form. 3. Substances tending to accelerate the depilatory action may be added. (F) W/O Cream Bases Ex. 20: Send 25g of Oily Cream P.C. Label appropriately. Ex. 21: Cold Cream Base. ℞ Liquid Paraffin Beeswax Borax 51.0 15.0 15.0 76 Water 36.0 Send 25g. To be used as directed. METHOD: Oily and oil-miscible or oil-soluble ingredients are mixed and melted together over a heated water bath. The water and water-miscible or soluble ingredients are also heated together to form a solution. The two phases are mixed together at the same temperature and stirred (over a cold water bath, if necessary) until cold. (G) Pastes Ex. 22: Send 25g of Zinc and Salicylic Acid Paste B.P. Label as such. Ex, 23: ℞ Coal Tar 2.0 Zinc Oxide 5.0 Polysorbate 80 0.5 Yellow Soft Paraffin 60.0 Send 25g. Label: Apply to the affected part twice daily. METHOD: Mix the coal tar with polysorbate 80. Levigate the zinc oxide with a small proportion of the soft paraffin and incorporate the coal tar/polysorbate 80 mixture in the remaining soft paraffin. Triturate the two portions together. NOTE: The polysorbate 80 serves a dual purpose. It functions as a dispersing agent and also in the removal of the ointment from the skin. 77 (H) OTHER COSMETIC PRODUCTS (1) DEODORANTS AND ANTIPERSPIRANTS The perspiration mal-odour is due to apocrine sweat, which contains an appreciable amount of potentially odour-producing lipid and proteinaceous matter. When the latter reaches the skin surface it becomes subject to bacterial attack resulting in its decomposition. The decomposition product formed usually gives rise to the distinctive axillary or body mal-odour. These products include low molecular weight fatty acids mercaptans, ammonia, aromatic amines, indoles and hydrogen sulphide. It has been shown that perspiration odours do not develop in sterile mixtures of insoluble sediments of perspiration. For the control of body odour, two approaches have been suggested. 1. The topical application of suitable antiseptics to prevent bacterial decomposition, i.e., the use of deodorants. 2. The topical application of suitable astringent substances to reduce the flow of perspiration i.e. the use of antiperspirants. The modern trend is to formulate preparations combining deodorant as well as antiperspirant properties. The most widely accepted antibacterial compound for use in deodorants are hexachlorophene (gas), bithionol, quaternary ammonium compounds, neomycin, ion-exchange resins and metal chelates of 1,3 diketones. Commercially available antiperspirants are largely based on astringent aluminium compounds such as aluminium chlorhydrate, aluminium sulphate and aluminium chloride. Various theories were put forward in respect of the mode of action of antiperspirants and the conclusion reached was that aluminium compounds reduce sweating by obstructing sweet glands rather than by exerting a direct effect upon them. Moreover, aluminium compounds possess deodorant effect due to inhibition of bacterial activity by virtue of the relatively low pH of their preparations and by neutralization of the mal-odour by the chemical combination with the odoriferous substance. 78 A simple basic formula for a liquid deodorant antiperspirant is as follows: Aluminium Chlorhydrate 20.0% Propylene Gglycol 5.0% Alcohol 10.0% Germicide 0.2% Perfume 9.5% Water to 100.0 Send 25ml. Cream Antiperspirant: Aluminium Chlorhydrate Glyceryl Monostearate (soap free) Spermaceti Perfume Glycerin Water to Send 25g. 20.0% 20.0% 5.0% 9.5% 3.0% 100.0% (2) SKIN CLEANERS The use of soap and water in reasonable amounts will clean satisfactorily most normal skins and also those in chronic phase of many diseases. There is, however, a well-established place in cosmetic practice for nonsaponaceous detergents. Women whose facial skin are excessively dry or are irritated by soap and water are advised to use a cleansing cream or lotion. A satisfactory cleansing cream should be mild on the skin, with a near neutral pH and should readily wet to the touch not too greasy and not excessive in quantity. Suitable cleansing creams could be based on the following formula: - 79 1. O/W Emulsion Type: ℞ Beeswax 8.0 Mineral Oil 49.6 Hard Paraffin 5.0 Soft Alcohol 8.4 Cetyl Alcohol 3.0 Sodium Lauryl Sulphate 3.0 Water to 100.0 Send 25g. METHOD OF PREPARATION: Melt the solid substances in an evaporating dish over a water bath (i.e. cetyl alcohol, beeswax and hard paraffin). Then add the mineral oil and soft paraffin. Dissolve the sodium lauryl sulphate in the warm purified water which had been freshly boiled and cooled to about 50oC and mix this solution with the melted ointments. Stir constantly until cold using a pestle, and not a glass rod. 2. W/O Emulsion Type (Not to be made) (a) ℞ Beeswax Mineral Oil Span 80 Anhydrous Lanoline Water to Send 25g. 100 25g 10 3.1g. 100g. Beeswax Borax Type (b) ℞ Beeswax 14% Almond Oil 50% Borax 1% Water 31% Send 25g. 80 NOTE: Spermaceti is usually added as a thickener. A preservative and perfume are also included. METHOD OF PREPARATION: Dissolve the beeswax to the almond oil at 60oC. Add the borax dissolved in the water at the same temperature. Mix and stir constantly until cold. The above beeswax-borax cream is still one of the most popular types of cleansing cream and is the familiar COLD CREAM. It is emulsified insitu by beeswax and borax. 3. Cleansing Lotion Triethanolamine3g. Stearic acid Beeswax Liquid paraffin Water Send 25g. 5g. 2g. 35g. 55g. METHOD: Dissolve the triethanolamine in water and heat to 60oC. Melt the stearic acid, beeswax and liquid paraffin together and add the aqueous solution to the oil at the same temperature with continuous trituration. (3) SHAMPOOS AND HAIR CREAM Shampoos These are products possessing cleansing and foaming properties, and are characterized by leaving the hair soft, lustrous and manageable. Shampoos may be classified according to their physical appearance into 1. Liquid shampoos 2. Cream shampoos 3. Powder shampoos. 81 By careful formulation, excellent shampoos could be obtained either from soaps or synthetic detergents. 1. Liquid Shampoos ℞ Coconut Oil Olive Oil Sodium Hydroxide/Potassium Hydroxide Alcohol Water to Send 25ml. 21g. 3g. 1:2 15ml. 100ml. Procedure: The weighed amounts of sodium hydroxide and potassium hydroxide are dissolved in the least amount of water (about 2ml) and solution is heated. The solution of alkali is added to the melted oils mixture on a water bath until complete saponification. The soap is dissolved in hot water. After cooling, alcohol is added and the volume is finally adjusted with water. 2. Cream Shampoos ℞ Sodium Lauryl Sulphate Sodium Stearate Lanolin Water Send 25g. 50g. 8g. 1g. 100ml. Procedure: Stearic acid is melted on a water bath, sodium hydroxide is dissolved in a small volume of water the solution is heated and added to the molten stearic acid. After complete saponification, lanolin is added. A paste of sodium lauryl sulphate in the remaining amount of water is prepared and mixed with the soap formed. 82 Hair Cream The ideal aid to hair grooming would probably be non-oily, non-gummy, non-resinous and likely to form an invisible stable, resilient, adequately controlling yet readily removable film on the hair. Successful brilliantine cream of the water-in-oil type are usually based on relatively simple formulae. In spite of this, they are not easy to imitate. Strict attention to the reliability and uniformity of raw materials is as essential as effective control of all processes and temperatures. Comparative analysis of several different commercial products gives an oil content of 35 – 50% an aqueous phase of 50 – 60% and an emulsifying agent of under 4%. ℞ Light Liquid Paraffin White Soft Paraffin White Beeswax Oleic Acid Lime Water Perfume Make 25g. 40% 6% 3% 0.5% 50% 0.5% Procedure: Slowly add the lime water (freshly prepared) to the light liquid paraffin, beeswax and oleic acid held at 70oC. Continue to stir until cold. Add the perfume at about 45oC. NOTE: Creams of the above type have the advantage of reasonably good stability on storage provided that they are passed through an homogeniser and carefully processed in other aspects. They break down readily when mechanically disturbed by rubbing on the hair and they act more like brilliantine oil then a cold cream. 83 400 LEVEL 84 POWDER TECHNOLOGY & DOSAGE FORM DESIGN POWDERS Oral powders are mixtures of powder substances intended for administration by mouth. They are usually mixed with water before administration. But some oral powders for veterinary use are administered by mixing with animal ration. Furthermore, most raw materials required in the preparation of tablets and capsules are available as powders, which are compressed into the tablet dosage form after granulation process. Classification: They can be classified according to their size: (i.e. ability to pass through a mesh aperture): 1. Coarse Powder 2. Moderately Coarse Powder 3. Moderately Fine Powder 4. Fine Powder 5. Very Fine Powder 6. Ultra-Fine Powder PREPARATION OF INSUFFLATION AND DUSTING POWDERS INSUFFLATIONS Synonym: Insufflations. These are powders, which are intended to be blown by means of an insufflator onto or into the affected part, e.g. Ear, Nose and Throat. The preparation of insufflations is similar to the preparation of dusting powders. 85 Frequently, insufflations contain substances, which liquefy when mixed. Most often encountered are camphor, menthol, phenol, ephedrine and thymol. To avoid the production of a down mass, disperse each of the liquefying substances in part of the base, sieve, and then mix the parts lightly together, with a spatula, on a place of paper, patients should be warned to store in a dry place. Packing: Glass jar with screw cap. Labeling: “Not to be taken”. PRACTICAL ℞ Menthol Camphor Send 20g. Make the insufflation. Label: To be used as directed. 5 5 METHOD 1. Powder the menthol in a glass mortar and add approximately half the Heavy Magnesium Carbonate, using the “doubling up” techniques, and pass through a No.60 sieve. 2. Separately powder the camphor in a glass mortar and add the remaining heavy magnesium carbonate and sift. 3. Mix the two portions from (1) and (2) lightly together on a piece of paper, using a spatula. 4. Pack and label. DUSTING POWDERS Synonyms: Pulvis Consperous. These are usually admixtures of two or more substances in fine powder, and are intended for application to the skin. Mineral ingredients such as Talc and Light kaolin are often used, and since they may be contaminated 86 with pathogenic organism, should be heat-treated before use (B.P. maintain at 160oC for 1 hour). The ingredients are mixed in ascending order of weight and are passed through a No.60 sieve before packing. Containers: Cylindrical paper – board boxes with sprinkler holes on closure. For economy, powder jars are used. Labeling: “For external use only” and “store in a dry place”. “Not to be applied to open wounds or areas of broken skin”. PRACTICAL ℞ Zinc Oxide 20.0 Salicylic Acid 2.0 Starch Powder 78.0 Send 30g. Label: The dusting powder. To be applied as directed. METHOD: 1. Weigh out the salicylic acid and powder finely in a glass mortar. 2. Weigh out the zinc oxide and place in the glass mortar a quantity roughly equal to the bulk of salicylic acid therein. Mix thoroughly, then add a further quantity of zinc oxide, equal in bulk to the contents of the mortar, and continue in this manner until all the zinc oxide has been added. Note below:- This process is known as “doubling up” and is used to ensure even dispersion of small quantities in a large bulk of material. 3. Weigh out the starch and mix with the powder in the mortar. 4. Pass the dusting powder through a No. 60 sieve onto a large piece of paper. 5. Mix the powder together lightly on the paper, using a spatula since some separation may have occurred on sieving. 6. Pack in a suitable container and label. 87 PREPARATION OF BULK AND INDIVIDUALLY WRAPPED ORAL POWDERS Synonym: Pulverse; Pulv; Pdr: Powders are usually mixtures of two of more medicaments intended for internal use. Each does may be wrapped individually or the powder may be supplied in bulk with, for example, a teaspoonful does. The general B.P. monographs on powders should be read. General Principles of Dispensing Powder. All medicaments plus any added “bulking” agent is reduced to a fine powder in a glass mortar before mixing. Mixing is carried out using the “doubling-up” process in order to ensure uniformity of the final product, and even dosage when the powder is divided into proportions. Bulk powders are prepared according to the general rules and packed in wide mouthed screw-capped jars. Single-dose, individually wrapped powders are prepared in bulk and each dose is then weighed separately and placed on a powder paper. This paper is then folded to enclose the powder and prevent any leakage on subsequent handling. All the powders of a particular batch must be uniformly wrapped and the individual powders held together with an elastic hand or dispensing thread before packing them into a powder box. Note: When a small quantity of a potent medicament is ordered by itself as a powder, it should be diluted by trituration with an amount of an inert diluent such as lactose so that the weight of the triturate to be taken as a dose is 120mg. The triturate should then be suitably wrapped as single doses. 88 PRACTICAL 1. Bulk Oral Powder: ℞ Compound Magnesium Carbonate Powder (BP 1988). Synonym: Pulbis Magnesii, carbonates compositus; Pulv. Mag. Carb. Co. Calcium Carbonate Heavy Magnesium Carbonate Sodium Bicarbonate Light Kaolin Send 30g. Label: Two teaspoonfuls to be after meals. 400g 400g 300g 100g. taken in water, three times a day METHOD: 1. Weigh out the ingredients 2. Mix in a mortar in order of ascending weight 3. Pass through a No. 60 sieve 4. Mix lightly with a spatula and pack in a screw-caped jar. 2. Single Dose Powders: ℞ Hyoscine Hydrobromide 0.6mg. Make the powder Label: One dose to be taken after food. METHOD: 1. Weigh out 100mg of hyoscine hydrobromide and triturate with 2.4g of lactose in a glass mortar. 2. Weigh 120mg of this triturate and mix with 0.84g of lactose in a glass mortar. 89 3. Prepare five powder papers and pack 120mg. of the powder in each. 4. Check the weight of powder left. 5. Label and pack the product. 3. ℞ Sod. Bicarb. 700mg Phein Pulv. 100mg Peppermint Oil 0.03ml. Make the powder. Label: One dose to be taken with water after food. Notice that the exact weight of each powder is unknown. It will be about 800mg. It is necessary therefore, to make the total weight the bulk powder up to a suitable figure by adding a suitable inert substance. METHOD: 1. Weigh and mix the solid ingredients (for 10 powders) 2. Add the peppermint oil and mix thoroughly. 3. Transfer the whole of the powder to a balance pan and add sufficient lactose to give a total weight of 10g. (Each powder will then weigh 10). 4. Mix the lactose into the other ingredients. Weigh out the individual powders into double powder papers, the inner paper being cut from a waxed or greaseproof paper is smaller than the outer paper all the way round. Wrap each powder as it is weighed to avoid excessive lose of peppermint oil. 90 DENTIFRICES These are preparations intended for use with a tooth brush for the process of cleansing the surface of the tooth. They could be classified according to their physical appearance, into: 1. 2. 3. 4. Powder Dentifrices Paste Dentifrices Gel Dentifrices Liquid Dentifrices Functions of Dentifrices The normal oral cavity supports a very large and varied population of bacteria, fungi and protozoa. In spite of what advertisers claim or imply, dentifrices are intended primarily to aid in cleansing the tooth and are of value just for that purpose. Some pastes, of course, go beyond the requirements of simple detergency and brushing the teeth with a dentifrice to include the aesthetic objective of removing food particles from around the teeth, polishing the teeth and freshen up the mouth by importing a cool and pleasant flavour. Therefore, the functions of dentifrices are: a. Polishing of the tooth; b. Reduction of the incidence of tooth decay; c. The maintenance of a healthy gum; d. Reduction of mouth odour. Ingredients of tooth preparations include: (a) Abrasives (b) Surface active agents or detergents (c) Flavouring agents and (d) Sweetening agents. Tooth pastes contain, in addition to the above ingredients, water, humectants, binders and preservatives. They may also contain: 91 1. Fluorides to strengthen the teeth and to decrease their susceptibility to decay. 2. Anti-enzymes to prevent putrefaction resulting from enzymatic decomposition of sugars. They should be non-toxic and free from unpleasant taste. 3. Colouring matter e.g. chlorophyll. 1. ABRASIVES An abrasive is an ingredient with rough surfaces i.e. a mechanical cleansing agent whose functions are: (a) Removal of debris and residual stains from the teeth. (b) Polishing of the tooth surface. Examples of common abrasives are: Calcium Carbonate and Calcium Phosphate. 2. SURFACE ACTIVE AGENTS Soaps are rarely used due to their irritant effect and their incompatibility with certain ingredients of dentifrices. Synthetic detergents, such as sodium lauryl sulphate are more commonly employed in modern dentifrices. 3. BINDERS Simple mixing of the solid and liquid phases of tooth paste is inadequate to prevent the separation of the liquid phase particularly during storage: a binder must be added. Examples are: Glycerin of Starch Gum Arabic Gum Tragacanth and Methyl Cellulose. 92 ANALYSIS OF POWDER PARTICLES The particle size of drugs have significant effect on the physical, chemical and biological properties of solid dosage forms such as degree of mixing, chemical stability, rate of dissolution and drug blood level. It is therefore an important particulate property of characterizing a material and understanding its behavior. The size of a particle is the dimension which best states the size subdivision. For a sphere this is unambiguously the diameter, for cuboids, it is the length of one edge. Derived diameters are determined by measuring a size dependent property of the particle and relating it to a linear dimension. For irregular particles, the assigned size usually depends on the method of measurement. Therefore the technique of particle size analysis should reflect the process under control, e.g. for tableting, particle volume is important; for catalysts, surface area is important and measurements are referred to an equivalent spherical diameter. A. Particle Size Analysis Methods: Microscopy: 1. Collect a sample of the powder with a spatula and spread lightly on a slide and view under a light microscope.(a) Describe the shape. 2. Insert an eyepiece graticle and calibrate it using a stage micrometer. Determine the size of particles and count the number of the different particles under view at various locations on the slide. Create a table of distribution of the particles using the Normal Distribution Method namely, Size Range, Mean Size Range, Number of Particles in each size range, etc. (b) Plot the Size-Frequency distribution both as a Histogram and a Curve. (c) Calculate: Arithmetic Mean Diameter, (∑nd/∑n), and Mean Surface Diameter √(∑nd2/∑n). Sieve Method: 1. Weigh 100 g of a given powder (vegetable drug or pure chemical such as ASA). Arrange the sieves in order of decreasing sieve number or aperture size in a sieve shaker. Operate the sieve shaker until no further change in the weight of the primary sample is observed. (a) Determine the 93 weight of the samples collected from the different sieves. (b) Name the class(es) of powder you have produced. (c) Plot the distribution obtained as Cumulative % Weight Frequency Undersize. B. Mixing of Powders Content uniformity is largely dependent upon the quality of the initial powder mixture and particle size distribution. Factors affecting mixing include particle size distribution, density, shape and attraction, mixing time and types of mixer. Further discussions on the different types of mixers, forces that are relevant for mixing to occur and mechanism of mixing are found in your lecture notes or relevant textbooks of pharmaceutical technology. Degree of Mixing: This is the qualitative expression, which defines the state of a mix. Such expression also allows the course of mixing to be followed and the performance of different mixers to be compared. PRACTICAL Incorporate a dye (Methylene Blue), 10 mg, into a given 1 kg base. Collect samples from different parts of the mix at 5 minutes intervals and assay for the dye Method of Assay: Dissolve the sample in a specific volume of water and read the absorbance using UV/Visible Spectrophotometer. NB: The smallest amount of sample collected for analysis is call the scale of scrutiny (the dose unit for such medicament is recommended) The Mixing Index is calculated by: M= ࡿD ࡿ Where; M = Index of Mixing SD = Standard Deviation S = SD of samples drawn from the mixture under examination M approaches unity as mixing is completed. 94 C. Flow Properties of Powder: Based on their flow properties, powders can further be classified as: 1. Free flowing powders 2. Cohesive powders Free flowing powders are usually of coarse dimension while the cohesive types are of fine particle size. (a) Bulk Density: Bulk density is defined as the weight per unit volume of material. The bulk density of a powder is the ratio of the mass of an untapped powder sample and its volume including the contribution of the interparticulate void volume. Hence, the bulk density depends on both the density of powder particles and the spatial arrangement of particles in the powder bed. The bulk density is expressed in grams per mL (g/mL) (b) Tapped Density: If the granules in the measuring cylinder are tapped, a volume less than the bulk volume is obtained. This is the tapped volume. The ratio of the weight of the granules over its tapped volume is known as the tapped density. (c) Carr’s Index: An alternative test to characterize the flow of particulate solids is the determination of the Carr’s index. This parameter relates the bulk (or “fluff”) density of the material (the volume occupied by a certain mass of powder when gently poured into a measure) to the tapped density (the volume occupied by that same mass of powder after a standard tapping of the measure to consolidate the powder). This can be mathematically expressed as: Carr’s index = 100(V0 - VF)/V0 V0 = unsettled apparent volume VF = final tapped volume Values below 15% would indicate excellent flow. Powders with values over 20% would have poor flow. 95 (d) Hausner Ratio: The Hausner ratio is similar to the Carr’s index. It is computed simply by dividing the tapped density by the bulk density. =V0/VF (e) Angle of Repose: This is the maximum angle possible between the surface of a pile of a powder and the horizontal at which the powdered particles starts to slide down. (This assay is useful for free flowing powders). PRACTICAL Methods: 1. Funnel Method: Allow the powder to pour out from a funnel. (a) Measure the angle it forms with the base. The Funnel and Rotating Drum Methods are characterized by high human error and therefore results are not reproducible. 2. Hollow Tube: Fill a hollow tube sitting on a base with the same diameter as the tube with the powder. Remove the tube to allow excess powder to fall off. (b) Measure the angle of the slope of the heap with the base using a semicircle rule. 3. Drained Cylinder: Fill a wide cylinder with the powder and then remove the plug at the base in order to drain off the powder. (c) Measure the angle of the drained cone formed within the cylinder. (f) Flow Through an Orifice: This is used to determine whether a powder is free flowing or not. It is usually expressed as weight collected per unit time. i.e. U(g.s1) = W(gm)/t(sec) 96 PRACTICAL Methods: Drained Cylinder Method: Fill the cylinder with the powder, remove the plug at the base of the cylinder and collect the powder flowing out through the orifice into a beaker. (a) Determine the time it takes the powder to completely flow out. (b) Determine the weight of powder that flowed out. (c) Plot the effects of the following factors, particle/granule size and orifice size, on the flow rate of the powders used. (g) Tensile Strength Measurement: Tensile strength is a measure of the force/unit area required to split the powder bed under tension. This measurement applies only to cohesive powders. PRACTICAL Methods: Tideswell & Todyfield Method (Split Plate Method) Assemble the apparatus, clamp the cells, pack the powder to be determined into it and adjust the plunger to the required stress (pressure) until a depth of 1cm is covered. Tilt the cell at a rate of 100/min until the bed fractures. (a) Measure the angle, , of the plane to the horizontal at which the bed fractures. Calculate the cohesion using the formula: Cohesion = ࢃࢍࡿࣂ dynes/cm2 Where: W = Total Weight (i.e. sliding half of cell, its content and the rollers) g = Acceleration due to gravity A = Surface Area = Angle of the plane to the horizontal 97 Other Methods Includes; Warren Spring tensile testing, a motorized method employed in fracturing the packed bed on a horizontal plane. The tensile strength is calculated as: T= ࡼ ࡰ࢚࣊ Where P = Applied Force D = Diameter of the compact T = Thickness of the compact π = Constant (3.143). 98 DOSAGE FORM DESIGN A. TABLETS The lecturer takes the students through the tablets manufacturing laboratory and introduce them to the different aspects of tablets manufacture and machines. The technologist describes how the machines are operated and maintained GRANULATION, DRYING PROCESSES & TABLET COMPRESSION Granulation Techniques: A. Wet Granulation Wet granulation is a process of using a liquid binder to lightly agglomerate the powder mixture. The amount of liquid has to be properly controlled, as over-wetting will cause the granules to be too hard and under-wetting will cause them to be too soft and friable. Aqueous solutions have the advantage of being safer to deal with than solvent-based systems but may not be suitable for drugs which are degraded by hydrolysis. Procedure 1. The active ingredient and excipients are weighed and mixed. 2. The wet granulate is prepared by adding the liquid binder–adhesive to the powder blend and mixing thoroughly. Examples of binders/adhesives include aqueous preparations of cornstarch, natural gums such as acacia, cellulose derivatives such as methyl cellulose, gelatin, and povidone. 3. Screening the damp mass through a mesh to form pellets or granules. 4. Drying the granulation. A conventional tray-dryer or fluid-bed dryer are most commonly used. 5. After the granules are dried, they are passed through a screen of smaller size than the one used for the wet mass to create granules of uniform size. 99 B. Dry Granulation (Slugging) Dry granulation processes create granules by light compaction of the powder blend under low pressures. The compacts so-formed are broken up gently to produce granules (agglomerates). This process is often used when the product to be granulated is sensitive to moisture and heat. Dry granulation can be conducted on a tablet press using slugging tooling or on a roll press called a roller compactor. Dry granulation equipment offers a wide range of pressures to attain proper densification and granule formation. Dry granulation is simpler than wet granulation, therefore the cost is reduced. However, dry granulation often produces a higher percentage of fine granules, which can compromise the quality or create yield problems for the tablet. Dry granulation requires drugs or excipients with cohesive properties, and a 'dry binder' may need to be added to the formulation to facilitate the formation of granules. C. Melt Granulation Melt granulation is a process by which pharmaceutical powders are efficiently agglomerated by the use of a binder which melts during the process. Examples of binders traditionally used includes; Poloxamers, Polyethylene Glycols, Carnauba Wax, Beeswax, Paraffin Wax, Stearic Acid and Hydrogenated Castor Oil PRACTICAL ℞ 20 Tablets of Paracetamol 500mg Paracetamol 500mg Lactose 50mg 15% Maize Starch Mucilage q.s Maize Starch Powder 25mg Talc 5mg Magnesium Stearate 5mg 100 Procedure 1. Weight the required amount of Paracetamol powder into a mortar, mix with sufficient quantity of 15% starch mucilage; make a mould using your hand and press between your thumb and fore-finger. How does it feel? Record your observation. 2. Press through a large pore sieve to produce beads of extruded wet granular sized particles. 3. Dry in an oven at about 50-60oC for about 30 min, mill the dry mass to granular size. What other process of granulation and drying do you know? 4. Determine the flow properties of the granules by calculating the a. Bulk Density, b. Tapped Density, c. Carr’s Index, d. Hausner Ratio and e. Angle of Repose. 5. Carry out the compression of these granules and the powders from which they were formed using the manually operated single punch machine. IN-PROCESS CONTROLS IN TABLETING In-process controls (IPC) are checks that are carried out before the manufacturing process is completed. The function of in-process controls is monitoring and – if necessary – adaptation of the manufacturing process in order to comply with the specifications. This may include control of equipment and environment. In-process controls may be performed in regular intervals during a process step (e.g. tabletting) or at the end of a process step (e.g. granulation, blending). The objectives of in-process control are both quality control and process control. • Tablet weight variation, • Disintegration time, • Content uniformity and homogeneity, • Dissolution time and rate, 101 PRACTICAL From the previous practical, determine the following; (a) Weight of tablets produced (b) Tablet dimensions (diameter & thickness) (c) Friability (d) Crushing Strength (hardness/tensile strength) using the formula T= ۾ ۲ૈܜ (e) Disintegration time (f) Content of active drug and (g) Dissolution according to the official books 102 B. CAPSULES DEFINITION OF CAPSULES Capsules are solid dosage forms in which the drug substance is enclosed in either a hard or soft soluble container or shell of a suitable form of gelatin. The word capsule is derived from the Latin word ‘capsula’, meaning a small box. In current English usage, it is applied to many different objects ranging from flowers to spacecraft. TYPES OF CAPSULES There are two types of capsules, 1. Hard gelatin capsules 2. Soft gelatin capsules The hard gelatin capsule which could be said to be two-piece consist of two hard pieces in the form of cylinders closed at one end, the shorter piece which is called the ‘cap’ fits the open end of the longer piece which is called the ‘body’. The soft capsule on the other hand is said to be the one-piece and is a soft globular gelatin shell. Although the standard capsules have the conventional oblong shape, exceptions are capsule products by Lilly and Smith Kline & French (SK&F), which are of a distinctive shape. For Lilly products, capsules are used in which the end of the base is tapered to give the capsule a bullet-like shape; products encapsulated in this form are called ‘pulvules’. The SK&F Spansule capsule differ in that both the ends of the cap and the body are angular rather than round. Examples of materials that are preferably formulated into capsule dosage forms of hard gelatin types include dried powdered plant parts and some antibiotics Students should obtain more information from the official books and product brochures on the formulation, packaging and storage of capsules 103 CAPSULE CAPACITIES Size Volume (ml) 000 00 0 1 2 3 4 5 1.37 0.95 0.68 0.50 0.37 0.30 0.21 0.13 Fill weight at powder density of 0.8g/cm3(g) 1.096 0.760 0.544 0.400 0.296 0.240 0.168 0.104 SOME REASONS FOR FORMULATION OF CAPSULES AS DOSAGE FORM 1. Some drugs have poor binding and compressibility property and hence are better formulated as capsules 2. Capsules are used to mask bitter and unpleasant taste of drugs 3. To improve bioavailability. This is because of the fast dissolution of the shell and absence of compaction. 4. Hard gelatin capsules allow for a degree of flexibility of formulation that is not obtainable with tablets. It is often easier to formulate hard gelatin capsules than tablets because there is no requirement that the powders must be formed into a coherent compact. 5. Hard gelatin capsules allow for flexibility in clinical testing and are widely used in preliminary studies of drugs. PRACTICAL Send 8 hard capsules of 150mg capacity, each containing 550 micrograms of Hyoscine hydrobromide. A suitable filler should be selected 104 PRACTICAL Send 15 capsules each containing 250 mg Ampicillin trihydrate equivalent to 150 mg Ampicillin base. 1. Use a suitable filler, lubricant and glidant. 2. Make a capsule weight of 400 mg. 3. Label to be used as prescribed PRACTICAL Send 500 mg capsule of the formula Occimum gratissimum 100 mg Venonia amigdalina 150 mg Andrographis paniculata 100 mg Garcenia kola 100 mg Lubricant (Talc) qs Disintegrant qs Label: To be swallowed twice daily after food Analysis Analysis of capsules is similar to that of tablets with the exception of hardness and friability tests 105 C. MICROENCAPSULATION DEFINITION OF MICROENCAPSULES These are systems consisting of fine solid particles, solutions, or emulsion droplets coated reproducibly with extremely thin polymeric films or shells. The coated particles or droplets are generally referred to as microcapsules. The term “microcapsule” has been defined as a spherical particle with a size varying between 1m and 1000m containing drug in the core Microsphere is a term often used synonymously with microcapsule. In strict sense Microcapsules are spherical particles made up of a continuous phase of one or more miscible polymers in which particulate drug is dispersed, at either the macroscopic (particulate) or molecular (dissolved) levels. Microsphere is different from microcapsule by having no welldefined wall or envelope. Different methods of encapsulation result in most cases, in either a microcapsule or a microsphere. In addition, some related terms are used as well. For example “microbeads” and “beads” are used alternately. “Spheres and “spherical” particles are also employed for large size and rigid morphology. Liposomes, otherwise known as multilamellar vesicles (MLV), consist of one or more phospholipid bilayers alternating with aqueous drug compartments (Okhamafe, 1990). Nanoparticles differ from conventional microcapsules only in being much smaller. They are of colloidal dimensions with particle diameter in the range 10-1000 nm. Microencapsulation has found application in a number of fields: pharmaceutical, biomedical, agricultural and cosmetics, to mention but a few. 106 Reasons for Formulating Drugs as Microcapsules Microencapsulation technology was first applied in engineering industrial production. This technology is now being applied in almost every aspect of science including pharmacy, biotechnology, agriculture, cosmetics and also many scientific disciplines: chemistry, biology and physics. 1. To improve formulation of incompatible drug components. 2. In Pharmacy, other reasons include achieving ccontrol of drug release, masking of unpleasant taste, Protection of labile drugs, minimize gastric irritations, separation of incompatible drugs, change liquid drugs to solid, entrapment of carcinogens, drug targeting, bioartificial organs and production of biopharmaceuticals. Materials for Producing Microcapsules Some of the materials that are currently being used or studied for controlled drug delivery include Poly-2-hydroxy ethyl methacrylate Poly-n-vinyl pyrrolidone Polymethyl methacrylate Polyvinyl alcohol Polyacrylic acid Polyacrylamide. Polyethylene-co-vinyl acetate Polyethylene glycol Polymethacrylic acid In recent years additional polymers designed primarily for medicinal applications have entered the arena of controlled release. Many of these materials are designed to degrade within the body. Among them are: o Polylactides o Polyglycolides o Polylactide-co-glycolides o Polyanhydrides o Polyorthoesters 107 The greatest advantage of these degradable polymers is that they are broken down into biologically acceptable molecules that are metabolized and removed from the body via normal metabolic pathways. Biodegradable materials produce degradation by-products that must be tolerated with little or no adverse reactions within the biological environment Methods of Producing Microcapsules A wide range of microencapsulation techniques has been developed. Two major classes of encapsulation methods have evolved; chemical and physical. Chemical methods involve polymerization during the process of preparing the microcapsules. Examples of methods in this class are interfacial or in situ polymerisation, simple and complex coacervation, solvent extraction, phase separation, counterion coacervation, emulsion/interfacial polymerisation, internal gelation and solvent evaporation. Physical methods involve the controlled precipitation of a polymeric solution wherein physical changes usually occure e.g. spray drying, spray chilling, rotary disk atomisation, fluidized bed coating, stationary nozzle coextrusion, centrifugal head coextrusion, submerged nozzle coextrusion and pan coating. The classification of the various methods of microencapsulation is not easy due to the huge and increasing number of processes involved in encapsulation. Also specific techniques can be hybrid of two or more methods or can use different mechanism simultaneously. Moreover, many names have changed throughout the years. Many new patents evolve solely on the basis of novel ways to produce microspheres. Thus, many scientists try to develop a systemic nomenclature for encapsulation depending on the nature of the polymer and the drug to be incorporated. Students should look up some published literature for other new methods of microencapsulation. 108 Gelation This method can be used for alginates due to their ability to form gels by reacting with calcium salt. It has been used as a method of enclosing viable cells, tissues and other labile biological substances within a semi permeable membrane. Other materials that have been successfully encapsulated by this method include, cloths dyes, proteins, DNA and recently, plant extracts. The method involves the extrusion of a suspension of the cell or tissue through a microdroplet-forming device producing microbeads, which fall into CaCl2 solution and form, gelled microbeads with the cells or tissues entrapped. These cell-containing, gel microbeads are then treated with a solution of polylysine, which displaces the surface layer of calcium ion, and form a permanent polysalt shell or membrane. Finally the interior calcium alginate gel is “liquefied” either to stay or to come out (depending on molecular weight and size of the starting alginate) of the capsule with calcium sequestrate such as buffered citrate solution PRACTICAL Formulate insulin microcapsules for oral administration such that 100 mg of microcapsules will contain 200 IU of insulin PRACTICAL Formulate Calcium alginate microbeads for the entrapment of Vit A for incorporation into table salt as “Vitamin A fortified table salt” such that 200 mg microcapsules will contain an equivalence of 20 mg Vit. A Preparation of Coating Material (0.1% Chitosan Solution) Dissolve the calculated amount of chitosan in distilled water, containing 1% glacial acetic acid with the aid of a magnetic stirrer. Adjust the viscosity of the chitosan solution by digesting overnight with 2.14 ml of 1%w/v Sodium Nitrite Solution. Add the calculated amount of Calcium chloride dehydrate. Add Polysorbate 80 (2 drops) a non-ionic surfactant to reduce surface tension of the coating solution. 109 Adjust the pH of the solution to 5.5 using NaOH pellets and solution. Filter the solution and adjust its volume to 1000 ml. Preparation of Core Materials Dissolve Sodium alginate (1%) in distilled water Add the active drug and stir using a magnetic stirrer until it dissolves. Adjust the volume to 100 ml. Method of Microencapsulation The electrostatic droplet generator system can be used for microcapsule preparation. Spherical droplets are formed with a syringe pump (ColeParmer Instrument Company, Illinois, USA) on which is fitted a different sizes of 90o blunt tip needle depending on the microcapsule size range desired. In the laboratory, students are to use hypodermic syringes to which different sizes of needles are mounted Load the core material into the syringe and extruded the syringe content into the coating material in a vertical position. Describe your result Filter and air-dry the particles. Analysis of Microcapsules Carry out the following analysis on the microcapsules you have produced. 1. Characterization of weight, size and shape of microcapsules 2. Morphology 3. Entrapment efficiency 4. Drug release profile 110 DETERMINATION OF VISCOSITY OF NEWTONIAN FLUIDS. Introduction and Theory. The viscosity of a liquid is that property which is responsible for the internal resistance offered to the relative motion of different parts of the liquid. This internal resistance is closely connected with the interaction between separate molecules of the liquid and the structure of the liquid phase. When a liquid flows through a tube, the “layer” of liquid in contact with the wall of the tube is stationary, whereas the liquid in the center has the highest velocity. Newton assumed the shearing forces (F) between two parallel planes in a liquid in relative motion to be proportional to the area of the planes and to the velocity gradient between them; he wrote his law for infinitely near planes in the form: dv F n A d Where dv = velocity gradient perpendicular to the planes, d A = area of the planes H = coefficient of dynamic viscosity. The absolute c.g.s. Unit of the coefficient of viscosity is the POISE (g.cm-1 sec-1). A liquid has a viscosity of 1 poise if a steady tangential force of 1 dyne produces a relative viscosity of 1cm per second between two parallel planes of area 1cm2 separated by 1cm and immersed in the fluid. The new S.I. unit of dynamic viscosity is Newton second per square meter. The poise is one of the units still allowed in conjunction with S.I. units and is 10-1s-1. 111 For most pure liquids and many solutions, Newton’s law has been confirmed for streamline or laminar flow, i.e. it is independent of the velocity gradient and such liquids are said to exhibit Newtonian viscosity. At a certain high critical liquid velocity (Vc) orderly steaming fluid motion is replaced by disorderly turbulent flow involving dissipation of energy in dry formation and the Newtonian Law is not applicable. Reynolds showed that the critical velocity could be expressed by: Vc = Rc h PD Where Rc is constant (Reynoldn a number) and it is approximately 2000 for long tubes. D = diameter of tube P = density of fluid Capillary Flow Method for Measuring Viscosity. Under conditions of streamline flow, Poiseuille showed that for narrow tubes of radius R the volume of liquid V flowing through the tube in time, t, under a given pressure, p, was related to the resistance to flow as a function of the area of the tube well the viscosity of the liquid and the velocity gradient. V = πR4 Pt 8hl Where l is the length of the tube, or H = πR4 Pt 8 Iv Thus, h = CPt if πR4 Constant C 8Iv 112 and C = h Pt Providing that the viscometer is vertical, the ;pressure P = heg, but for any given viscometer h and g are both constant, so that p is proportional to C. Denoting the properties of a standard liquid by subscript 1 and of the test liquid by subscript 2, H2 = P2 t2 P1 t1 h1 h2 = h1 = CP2 t2 P1 t1 Where C = h1 P1 t1 And provided P2 is known, measuring t2 enables h2 to be calculated. The constant C is determined by calibrating the instrument with a liquid of known viscosity. For the highest accuracy a correction may have to be made for the pressure used in imparting kinetic energy to the liquid. The calculation of dynamic viscosity can be tedious since it involves the determination of density. For this reason the kinematic viscosity is often used. Kinematic viscosity = h e The unit of kinematic viscosity is the stokes. Kinematic viscosity of a fluid is thus directly proportional to the time of flow through a capillary tube (N.B. when liquid flows under its own head of pressure). This is another unit which may be used in conjunction with S.I. units where kinematic viscosity is defined as square meter per second. The stoke is thus defined as 10-4m2s-1. 113 EXPERIMENTAL Measurement of Viscosity using an Ostwald Viscometer. Using purified water as the standard liquid and taking the viscosity as 0.01 poise and density as 1 gm cm-1 at room temperature determine the following: 1. Calculate the constant (C ) of the Ostwald viscometer provided according to the POISEUILLE’S equation. 2. Determine the dynamic and kinematic viscosities of the 3 unknown liquids provided. and Liquid A has a density of 0.790 gm. cm-1 Liquid B has a density of 0.880 gm. cm-1 Liquid C has a density of 1.324 gm. cm-1 3. Determine the unknown concentration of glycerin provided. Procedure: (a) Determine the relative viscosity of different concentrations of glycerin (suggested concentrations of glycerin/water mixtures to be prepared are 0%, 10%, 25%, 75%, 90% and 100%). (b) Plot a graph of hrel against concentration; (c) Determine the relative viscosity of the unknown samples of glycerin; (d) From the above graph determine the corresponding concentration of glycerin. 4. Determine the unknown concentration of ethanol/water mixture provided. Procedure: Follow the same method as in No. 2 above (suggested concentrations of ethanol/water mixture to be prepared are 0%, 20%, 50%, 60%, 80% and 100%). 114