Abbott Northwestern Hospital, Allina Hospitals
advertisement

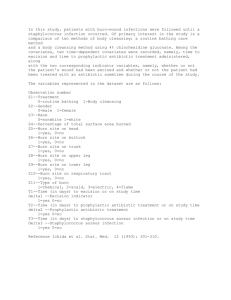
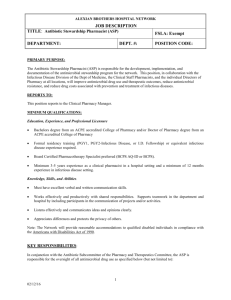
Description of the Program Prior to Implementation: • Policies and order sets reviewed and revised • Antibiotic usage guidelines developed • Antibiotic stewardship workbench report developed Pharmacist-Led Antibiotic Stewardship Program Reduces Inappropriate Antibiotic Use and Hospital-acquired Clostridium difficile Example: Anti-­‐infective Usage Guidelines Caspofungin: • Restricted for Infectious Disease Service use only for the parenteral treatment of invasive aspergillosis and other susceptible fungal infections. Cefepime: parenteral • An alternative to broad spectrum penicillins, carbapenems, and ceftazidime for the treatment of nosocomial infections including pseudomonas and extended spectrum beta lactamase producing organisms. Ceftazidime: parenteral • Empiric therapy in febrile, neutropenic patients with a documented ANC < 1000 and patients with suspected nosocomial meningitis. • Treatment of documented infections caused by susceptible strains of Pseudomonas aeruginosa or other gram negative bacilli which are resistant to penicillins. Ceftriaxone: doses > 2 • Reserved for the treatment of meningitis (recommended dose is 2 a gm i.v. daily grams i.v. every 12 hours in combination with vancomycin until culture results are finalized). • Treatment of brain abscess. Cefuroxime: parenteral • Reserved for pediatric patients only for the following indications: (reserved for pediatric pneumonia, epiglottitis, cellulitis, and septic arthritis. Cefuroxime patients only) should not be used for the treatment of meningitis. Introduction Health-Care Facility • Abbott Northwestern Hospital is part of Allina Hospitals & Clinics • Provides care to patients in Minnesota and Western Wisconsin • 639-bed general medical-surgical teaching hospital • Largest not-for-profit hospital in Minneapolis/St. Paul area a intravenous • Approximately 50-60 patients reviewed per day in 5-6 hours; average rate of 6.33 minutes per patient • 1419 pharmacist recommendations with 90% acceptance rate • 61 antibiotic-related Joint Commission Core Measure “misses” prevented ASP-Graph1 2010 Pharmacist Recommendations Number of a Recommendation Number Accepted Recommendations Dose adjustment 63 57 Route change 128 116 Add a new medication 58 56 Change/modify medication 303 250 Consult specialist 24 23 Discontinue/assess duration 650 615 76 68 1 Document indication for use 11/8/11 8:53 PM Lab or non-­‐medication orders 10 8 Order/note clarification 26 25 Pneumonia Core Measure 12 11 b SCIP Core Measure 69 50 Total 1419 1279 a Interventions completed per hospital approved protocol(s) are not included b Surgical Care Improvement Project Abbott Northwestern Hospital, Allina Hospitals & Clinics • 4.6% decrease in total antibiotic days of therapy (DOT)/1000 patient days 600.00 Minneapolis, Minnesota Authors of this presentation have the following to disclose concerning possible financial or personal relationships with commercial entities that may have direct or indirect interest in the subject matter of this presentation: Authors have nothing to disclose. 590.00 580.00 Days of Therapy 570.00 560.00 jpGraph 2 Pharmacist-Led ASP 1 550.00 11/8/11 8:57 PM 540.00 530.00 DOT/1000 PD 2006 2007 2008 2009 2010 583.99 594.05 584.03 588.91 557.06- • 25.5% decrease in total fluoroquinolone DOT/1000 patient days Total Fluoroquinolone Days of Therapy per 1000 Patient Days 120.00 Purpose • To determine the impact of a pharmacist-led ASP on: › Reducing inappropriate antibiotic use and costs › Increasing compliance with Joint Commission Core Measures › Reducing hospital-acquired Clostridium difficile-associated disease (CDAD) Percent Accepted 91% 91% 97% 83% 96% 95% 90% 80% 96% 92% 73% 90% Total Antibiotic Days of Therapy per 1000 Patient Days • Antibiotic stewardship programs (ASPs) improve patient care by reducing: › Inappropriate antimicrobial use › Antimicrobial resistance › Hospital-acquired infections • Hospitals struggle to obtain resources for infectious diseases (ID) physicians or ID-trained pharmacists • Limited studies describe pharmacist-led ASPs without daily physician involvement • ASP team determined that an ID-trained pharmacist would lead daily operations to provide consistency and prevent perception of ASP physician-driven consults Implementation: • Implemented hospital-wide July 2009 • Pharmacist reviewed antibiotic orders daily for adult patients with no ID consult • Recommendations based on: › Current published guidelines › Hospital usage guidelines › Hospital medication policies • ID physicians available for curbside consults • 15.8% decrease in antibiotic cost per patient day, equating to approximately $370,000 over 2 years Pharmacist-Led Antibiotic Stewardship Program Reduces Inappropriate Antibiotic Use and Hospital-acquired Clostridium difficile Background Jessica Holt, Pharm.D., BCPS-ID Kristine Gullickson, Pharm.D. Daniel Anderson, M.D. Elliot Francke, M.D. Jessica Nerby, M.P.H. Jason Sanchez, M.D. Experience with the Program (continued) Experience with the Program 100.00 80.00 Days of Therapy 60.00 40.00 20.00 0.00 DOT/1000 PD 2006 2007 2008 2009 2010 81.35 110.82 106.50 92.38 79.39 • 26% reduction in hospital-acquired CDAD rates Conclusion • The pharmacist-led ASP at our institution is innovative in that it does not involve a physician in its daily operations and was successful in reducing inappropriate antibiotic use and costs, increasing Joint Commission Core Measure compliance, and reducing hospital-acquired Clostridium difficile-associated disease. • To sustain the program, we developed and implemented a PGY2 Pharmacy Residency in Infectious Diseases in which the resident works closely with the ID pharmacist to review patients and track program outcomes. • Hospitals with limited resources can successfully utilize an ID-trained pharmacist to conduct the daily operations of the ASP. ID training can be achieved through a formal residency or available training programs.