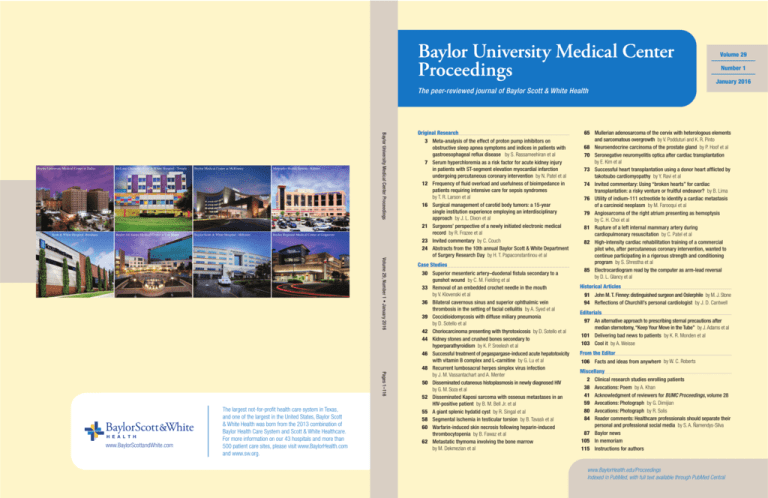
Volume 29
Number 1
January 2016
The peer-reviewed journal of Baylor Scott & White Health
Scott & White Hospital -Brenham
McLane Children’s Scott & White Hospital - Temple
Baylor Medical Center at McKinney
Metroplex Health System - Killeen
Baylor All Saints Medical Center at Fort Worth
Baylor Scott & White Hospital - Hillcrest
Baylor Regional Medical Center at Grapevine
Baylor University Medical Center Proceedings
Baylor University Medical Center at Dallas
Volume 29, Number 1 • January 2016
Pages 1–116
www.BaylorScottandWhite.com
The largest not-for-profit health care system in Texas,
and one of the largest in the United States, Baylor Scott
& White Health was born from the 2013 combination of
Baylor Health Care System and Scott & White Healthcare.
For more information on our 43 hospitals and more than
500 patient care sites, please visit www.BaylorHealth.com
and www.sw.org.
Original Research
3 Meta-analysis of the effect of proton pump inhibitors on
obstructive sleep apnea symptoms and indices in patients with
gastroesophageal reflux disease by S. Rassameehiran et al
7 Serum hyperchloremia as a risk factor for acute kidney injury
in patients with ST-segment elevation myocardial infarction
undergoing percutaneous coronary intervention by N. Patel et al
12 Frequency of fluid overload and usefulness of bioimpedance in
patients requiring intensive care for sepsis syndromes
by T. R. Larson et al
16 Surgical management of carotid body tumors: a 15-year
single institution experience employing an interdisciplinary
approach by J. L. Dixon et al
21 Surgeons’ perspective of a newly initiated electronic medical
record by R. Frazee et al
23 Invited commentary by C. Couch
24 Abstracts from the 10th annual Baylor Scott & White Department
of Surgery Research Day by H. T. Papaconstantinou et al
Case Studies
30 Superior mesenteric artery–duodenal fistula secondary to a
gunshot wound by C. M. Fielding et al
33 Removal of an embedded crochet needle in the mouth
by V. Klovenski et al
36 Bilateral cavernous sinus and superior ophthalmic vein
thrombosis in the setting of facial cellulitis by A. Syed et al
39 Coccidioidomycosis with diffuse miliary pneumonia
by D. Sotello et al
42 Choriocarcinoma presenting with thyrotoxicosis by D. Sotello et al
44 Kidney stones and crushed bones secondary to
hyperparathyroidism by K. P. Sreelesh et al
46 Successful treatment of pegaspargase-induced acute hepatotoxicity
with vitamin B complex and L-carnitine by G. Lu et al
48 Recurrent lumbosacral herpes simplex virus infection
by J. M. Vassantachart and A. Menter
50 Disseminated cutaneous histoplasmosis in newly diagnosed HIV
by G. M. Soza et al
52 Disseminated Kaposi sarcoma with osseous metastases in an
HIV-positive patient by B. M. Bell Jr. et al
55 A giant splenic hydatid cyst by R. Singal et al
58 Segmental ischemia in testicular torsion by B. Tavaslı et al
60 Warfarin-induced skin necrosis following heparin-induced
thrombocytopenia by B. Fawaz et al
62 Metastatic thymoma involving the bone marrow
by M. Dekmezian et al
65 Mullerian adenosarcoma of the cervix with heterologous elements
and sarcomatous overgrowth by V. Podduturi and K. R. Pinto
68 Neuroendocrine carcinoma of the prostate gland by P. Hoof et al
70 Seronegative neuromyelitis optica after cardiac transplantation
by E. Kim et al
73 Successful heart transplantation using a donor heart afflicted by
takotsubo cardiomyopathy by Y. Ravi et al
74 Invited commentary: Using “broken hearts” for cardiac
transplantation: a risky venture or fruitful endeavor? by B. Lima
76 Utility of indium-111 octreotide to identify a cardiac metastasis
of a carcinoid neoplasm by M. Farooqui et al
79 Angiosarcoma of the right atrium presenting as hemoptysis
by C. H. Choi et al
81 Rupture of a left internal mammary artery during
cardiopulmonary resuscitation by C. Patel et al
82 High-intensity cardiac rehabilitation training of a commercial
pilot who, after percutaneous coronary intervention, wanted to
continue participating in a rigorous strength and conditioning
program by S. Shrestha et al
85 Electrocardiogram read by the computer as arm-lead reversal
by D. L. Glancy et al
Historical Articles
91 John M. T. Finney: distinguished surgeon and Oslerphile by M. J. Stone
94 Reflections of Churchill’s personal cardiologist by J. D. Cantwell
Editorials
97 An alternative approach to prescribing sternal precautions after
median sternotomy, “Keep Your Move in the Tube” by J. Adams et al
101 Delivering bad news to patients by K. R. Monden et al
103 Cool it by A. Weisse
From the Editor
106 Facts and ideas from anywhere by W. C. Roberts
Miscellany
Clinical research studies enrolling patients
Avocations: Poem by A. Khan
Acknowledgment of reviewers for BUMC Proceedings, volume 28
Avocations: Photograph by G. Dimijian
Avocations: Photograph by R. Solis
Reader comments: Healthcare professionals should separate their
personal and professional social media by S. A. Ñamendys-Silva
87 Baylor news
105 In memoriam
115 Instructions for authors
2
38
41
59
80
84
www.BaylorHealth.edu/Proceedings
Indexed in PubMed, with full text available through PubMed Central
Baylor University Medical Center
Proceedings
The peer-reviewed journal of Baylor Scott & White Health
Volume 29, Number 1 • January 2016
Editor in Chief
William C. Roberts, MD
Associate Editor
Michael A. E. Ramsay, MD
Founding Editor
George J. Race, MD, PhD
Steven M. Frost, MD
Dennis R. Gable, MD
D. Luke Glancy, MD
Paul A. Grayburn, MD
Bradley R. Grimsley, MD
Joseph M. Guileyardo, MD
Carson Harrod, PhD
H. A. Tillmann Hein, MD
Daragh Heitzman, MD
Priscilla A. Hollander, MD, PhD
Roger S. Khetan, MD
Göran B. Klintmalm, MD, PhD
Sally M. Knox, MD
John R. Krause, MD
Bradley T. Lembcke, MD
Jay D. Mabrey, MD
Michael J. Mack, MD
David P. Mason, MD
Peter A. McCullough, MD, MPH
Gavin M. Melmed, JD, MBA, MD
Robert G. Mennel, MD
Michael Opatowsky, MD
Joyce A. O’Shaughnessy, MD
Dighton C. Packard, MD
Harry T. Papaconstantinou, MD
Gregory J. Pearl, MD
Robert P. Perrillo, MD
Daniel E. Polter, MD
Irving D. Prengler, MD
Chet R. Rees, MD
Erin D. Roe, MD
Randall L. Rosenblatt, MD
Lawrence R. Schiller, MD
W. Greg Schucany, MD
wc.roberts@BaylorHealth.edu
Editorial Board
Jenny Adams, PhD
W. Mark Armstrong, MD
Raul Benavides Jr., MD
Mezgebe G. Berhe, MD
Joanne L. Blum, MD, PhD
C. Richard Boland Jr., MD
Jennifer Clay Cather, MD
James W. Choi, MD
Cristie Columbus, MD
Barry Cooper, MD
Gregory J. Dehmer, MD
R. D. Dignan, MD
Gregory G. Dimijian, MD
Michael Emmett, MD
Andrew Z. Fenves, MD
Giovanni Filardo, PhD
James W. Fleshman, MD
Editorial Staff
Managing Editor
Cynthia D. Orticio, MA, ELS
Administrative Liaison
Bradley T. Lembcke, MD
Jeffrey M. Schussler, MD
S. Michelle Shiller, DO
Michael J. Smerud, MD
Marvin J. Stone, MD
C. Allen Stringer Jr., MD
Tanya Sudia, RN, PhD
William L. Sutker, MD
Marc A. Tribble, MD
James F. Trotter, MD
Gary L. Tunell, MD
Lawrence S. Weprin, MD
F. David Winter Jr., MD
Larry M. Wolford, DMD
Scott W. Yates, MD, MBA, MS
Residents/Fellows
Aasim Afzal, MD
Timothy Ball, MD
Philip M. Edmundson, MD
Design and Production
Aptara, Inc.
Cynthia.Orticio@BaylorHealth.edu
Baylor University Medical Center Proceedings (ISSN 0899-8280), a peer-reviewed journal, is published quarterly (January, April, July, and October).
Proceedings is indexed in PubMed and CINAHL; the full text of articles is
available both at www.BaylorHealth.edu/Proceedings and www.pubmedcentral.nih.gov. The journal’s mission is to communicate information about the
research and clinical activities, continuing education, philosophy, and history
of Baylor Scott & White Health.
Funding for the journal is provided by the Baylor Health Care System
Foundation. Funding is also provided by donations made by the medical staff and subscribers. These donations are acknowledged each year in a
journal issue. For more information on supporting Proceedings and Baylor
Scott & White Health with charitable gifts and bequests, please call the
Foundation at 214-820-3136. Donations can also be made online at http://
give.baylorhealth.com/.
Statements and opinions expressed in Proceedings are those of the authors and
not necessarily those of Baylor Scott & White Health or its board of trustees.
Guidelines for authors are available at http://www.baylorhealth.edu/Research/
Proceedings/SubmitaManuscript/Pages/default.aspx.
January 2016
Subscriptions are offered free to libraries, physicians affiliated with Baylor,
and other interested physicians and health care professionals; donations are
suggested for print subscriptions. To add or remove your name from the mailing list, call 214-820-9996 or e-mail Cynthia.Orticio@BaylorHealth.edu.
POSTMASTER: Send address changes to Baylor Scientific Publications Office,
3500 Gaston Avenue, Dallas, Texas 75246.
Advertising is accepted. Acceptance of advertising does not imply endorsement
by Baylor Scott & White Health. For information, contact Cindy Orticio at
Cynthia.Orticio@BaylorHealth.edu.
Permission is granted to students and teachers to copy material herein for
educational purposes. Authors also have permission to reproduce their own
articles. Written permission is required for other uses and can be obtained
through Copyright.com.
Copyright © 2016, Baylor University Medical Center. All rights reserved. Printed
in the United States of America on acid-free paper. Press date: December 8, 2015.
To access Baylor’s physicians, clinical services, or educational programs, contact the Baylor Physician ConsultLine: 1-800-9BAYLOR (1-800-922-9567).
1
Clinical research studies enrolling patients through
Baylor Research Institute
Currently, Baylor Research Institute is conducting more than 800 research projects. Studies open to enrollment are listed in
the Table. To learn more about a study or to enroll patients, please call or e-mail the contact person listed.
Research area
Specific disease/condition
Contact information (name, phone number, and e-mail address)
Asthma and
pulmonary disease
Chronic obstructive pulmonary disease, asthma (adult)
Jana Holloway, RRT, CRC
Courtney Patenaude, BS
Horacio Martinez
214-818-9495
214-818-7899
214-820-0338
janahol@baylorhealth.edu
courtney.patenaude@baylorhealth.edu
horacio.martinez@baylorhealth.edu
Cancer
Breast, ovarian, endometrial, prostate, brain, lung, bladder, colorectal,
pancreatic, and head and neck cancer; hematological malignancies,
leukemia, multiple myeloma, non-Hodgkin’s lymphoma; melanoma
vaccine; bone marrow transplant
Grace Townsend
214-818-8472
cancer.trials@BaylorHealth.edu
Type 1 and type 2 diabetes, cardiovascular events
Lorie Estrada
214-820-3416
Lorie.estrada@baylorhealth.edu
Pancreatic islet cell transplantation for type I diabetics, who either have
or have not had a kidney transplant
Kerri Purcell, RN
817-922-4640
kerri.purcell@baylorhealth.edu
Type 2; cardiac events
Trista Bachand, RN
817-922-2587
trista.bachand@baylorhealth.edu
Pancreatic islet cell transplantation for type I diabetics, who either have or
have not had a kidney transplant; high cholesterol
Kerri Purcell, RN
817-922-4640
kerri.purcell@baylorhealth.edu
Diabetes (Dallas)
Diabetes (Fort Worth)
Gastroenterology
Heart and vascular
disease (Dallas)
Inflammatory bowel disease
Dr. Themistocles Dassopoulos
469-800-7180
T.Dassopoulos@baylorhealth.edu
Aortic aneurysms, coronary artery disease, hypertension, poor leg
circulation, heart attack, heart disease, congestive heart failure, angina,
carotid artery disease, familial hypercholesterolemia, renal denervation
for hypertension, diabetes in heart disease, cholesterol disorders, heart
valves, thoracotomy pain, stem cells, critical limb ischemia, cardiac
surgery associated with kidney injury, pulmonary hypertension
Merielle Boatman
214-820-2273
MeriellH@BaylorHealth.edu
Heart and lung transplant, mechanical assist device such as LVAD
Elizabeth Owens, BA, CCRP
214-820-4015
Liz.Owens@baylorhealth.edu
Heart and vascular disease
(Fort Worth)
Atrial fibrillation, atrial fibrillation post PCI
Meagan King
817-922-2583
Meagan.king@baylorhealth.edu
Heart and vascular disease
(Legacy Heart)
At risk for heart attack/stroke; previous heart attack/stroke/PAD; cholesterol
disorders; atrial fibrillation; overweight/obese; other heart-related conditions
Angela Germany
469-800-6409
lhcresearch@baylorhealth.edu
Heart and vascular
disease (Plano)
Aortic aneurysm; coronary artery disease; renal stent for uncontrolled
hypertension; poor leg circulation; heart attack; heart disease; heart valve
repair and replacement; critical limb ischemia; repair of aortic dissections
with endografts; surgical leak repair; atrial fibrillation; heart rhythm
disorders; carotid artery disease; congestive heart failure; gene profiling
Tina Worley
469-814-4712
christina.worley1@baylorhealth.edu
Hepatology
Infectious disease
Nephrology
Neurology
Liver disease
Jonnie Edwards
214-820-6243
jonnie.edwards@baylorhealth.edu
HIV/AIDS
Bryan King, LVN
214-823-2533
bryan.king@ntidc.org
Hepatitis C, hepatitis B
Jonnie Edwards
214-820-6243
Jonnie.edwards@baylorhealth.edu
Type 2 diabetes with chronic kidney disease
Lisa Mamo, RN
Dr. Harold Szerlip
214-818-2526
214-358-2300
Lisa.Mamo@BaylorHealth.edu
Harold.Szerlip@baylorhealth.edu
Stroke, migraine
Quynh Lan Doan
214-818-2522
quynh.doan@BaylorHealth.edu
Multiple sclerosis, stroke
Portland Pleasant, RN
214-820-7903
portland.pleasant@baylorhealth.edu
Cerebral aneurysms
Kennith Layton, MD
214-827-1600
KennithL@BaylorHealth.edu
Interventional stroke therapy
Tomica Harrison
214-820-2615
tomica.harrison@baylorhealth.edu
Rheumatology (9900 N.
Central Expressway)
Rheumatoid arthritis, psoriatic arthritis, lupus, gout,
ankylosing spondylitis
Giselle Huet
214-987-1253
ruth.huet@baylorhealth.edu
Surgery
Chronic limb ischemia, pain management with chest tubes, colon polyps,
diaphragm stimulators, and surgery as it pertains to GERD, breast cancer,
esophagus, colon, colon cancer, pancreas, lung, hernias, dialysis access,
per-oral endoscopic myology (POEM), thoracic outlet syndrome
Tammy Fisher
214-820-7221
tammyfi@BaylorHealth.edu
Bone marrow, blood stem cells
Grace Townsend
Gabrielle Ethington
214-818-8472
214-818-8326
Grace.Townsend@BaylorHealth.edu
gabriele@baylorhealth.edu
Solid organs
Jonnie Edwards
214-820-6243
jonnie.edwards@baylorhealth.edu
Obesity
Lorie Estrada
214-820-3416
Lorie.estrada@baylorhealth.edu
Neurosurgery
Transplantation
Weight management
Baylor Research Institute is dedicated to providing the support and tools needed for successful clinical research. To learn
more about Baylor Research Institute, please contact Kristine Hughes at 214-820-7556 or Kristine.Hughes@BaylorHealth.edu.
2
Proc (Bayl Univ Med Cent) 2016;29(1):2
Meta-analysis of the effect of proton pump inhibitors on
obstructive sleep apnea symptoms and indices in patients
with gastroesophageal reflux disease
Supannee Rassameehiran, MD, Saranapoom Klomjit, MD, Nattamol Hosiriluck, MD, and Kenneth Nugent, MD
This study was designed to assess evidence for an association between
the treatment of gastroesophageal reflux disease (GERD) with proton
pump inhibitors (PPIs) and improvement in obstructive sleep apnea (OSA).
We conducted a systematic review and meta-analysis of randomized
controlled trials and prospective cohort studies to evaluate the treatment
effect of PPIs on OSA symptoms and indices in patients with GERD.
EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials,
the Cochrane Database of Systematic Reviews, and ClinicalTrials.gov
were reviewed up to October 2014. From 238 articles, two randomized
trials and four prospective cohort studies were selected. In four cohort
studies there were no differences in the apnea-hypopnea indices before
and after treatment with PPIs (standard mean difference, 0.21; 95%
confidence interval, –0.11 to 0.54). There was moderate heterogeneity
among these studies. Two cohort studies revealed significantly decreased
apnea indices after treatment (percent change, 31% and 35%), but
one showed no significant difference. A significant improvement in the
Epworth Sleepiness Scale was observed in three cohort studies and one
trial. The frequency of apnea attacks recorded in diaries was decreased
by 73% in one trial. In conclusion, available studies do not provide enough
evidence to make firm conclusions about the effects of PPI treatment on
OSA symptoms and indices in patients with concomitant GERD. Controlled
clinical trials with larger sample sizes are needed to evaluate these associations. We recommend PPIs in OSA patients with concomitant GERD
to treat reflux symptoms. This treatment may improve the quality of sleep
without any effect on apnea-hypopnea indices.
T
he prevalence of gastroesophageal reflux disease (GERD)
is significantly higher in patients with obstructive sleep
apnea (OSA) (1–6), and 54% to 76% of patients with
OSA have GERD (2, 3). These two conditions share
one common risk factor, namely obesity, which increases the
risk for both apnea and reflux (7). This association may be explained by lower esophageal sphincter pressures and prolonged
esophageal relaxation following swallowing (8). These changes
could increase the frequency and severity of reflux. Nocturnal
reflux could cause sleep arousals and sleep fragmentation in
OSA patients, and acid exposure could cause edema and inflammation in the upper airway, which increase the frequency of
airway occlusions during inspiration (6). Studies supporting this
hypothesis have shown that continuous positive airway pressure
Proc (Bayl Univ Med Cent) 2016;29(1):3–6
(CPAP) has antireflux effects in OSA patients (9, 10). However,
other studies have reported that the severity of OSA does not
correlate with the occurrence of reflux symptoms (11). Given
the significant morbidity and mortality of OSA, including left
ventricular dysfunction, arrhythmias, myocardial infarction,
stroke, systemic hypertension, and risk of motor vehicle accidents, it is important to evaluate all factors associated with OSA
and to consider the potential benefit of treatment of factors not
directly related to upper airway anatomy (12–15). Several studies have suggested that proton pump inhibitors (PPIs) improve
OSA symptoms and reduce some complications. We conducted
a systematic review and meta-analysis of the published reports
to better understand the treatment effect of GERD on the
OSA-hypopnea syndrome.
METHODS
We searched EMBASE, MEDLINE, the Cochrane Central
Register of Controlled Trials, the Cochrane Database of Systematic Reviews, and ClinicalTrials.gov from database inception to
October 2014. We used the following text words as search terms:
“sleep apnea syndrome” and “proton pump inhibitor.” Our
search included articles published in English and non-English
languages. We also scanned the bibliographies of all retrieved
articles for additional relevant articles.
Two independent reviewers (S.R. and S.K.) performed
article selection, data extraction, and assessment of the risk of
bias. Disagreements were resolved through consensus. Studies were included if they met the following criteria: 1) were
controlled clinical trials or observational studies that assessed
the effect of PPIs on OSA, including symptoms of daytime
somnolence, nocturnal symptoms, Epworth Sleepiness Score
(ESS), apnea-hypopnea index (AHI), apnea index, hypopnea
index, and respiratory disturbance index; 2) reported concomitant GERD in patients with OSA; and 3) provided adequate
data to extract the outcomes. We excluded studies that reported
From the Department of Internal Medicine, Texas Tech University Health Sciences
Center, Lubbock, Texas.
Corresponding author: Supannee Rassameehiran, MD, Department of Internal
Medicine, Texas Tech University Health Science Center, 3601 4th Street, Lubbock,
TX 79430 (e-mail: Supannee.Rassameehiran@ttuhsc.edu).
3
only the prevalence of GERD in OSA patients, patients who
were treated with CPAP and PPIs, and OSA patients without
underlying GERD who were treated with PPIs. If multiple
updates of the same data were found, we used the most recent
version for analysis. From each study, we abstracted the study
design, setting, population characteristics (including sex, age,
race or ethnicity, baseline body mass index [BMI], and baseline AHI), patient eligibility and exclusion criteria, number of
patients, type of PPIs used, treatment duration, and method of
outcome determination.
Two reviewers (S.R. and S.K.) independently assessed the
quality of each trial by using a tool developed by the Cochrane
Collaboration (16). Each trial was given an overall summary
assessment of low, unclear, or high risk of bias. We adapted
existing tools to assess the quality of observational studies. The
strength of evidence for outcomes was graded as high, moderate, low, or very low according to the approach of the GRADE
working group (17).
AHIs in patients before treatment versus after treatment
were evaluated. Statistical analysis was conducted with Review
Manager (RevMan Version 5.3, The Cochrane Collaboration,
The Nordic Cochrane Centre, Copenhagen, Denmark). The
chi-square test and I2 statistic were used to address heterogeneity
among studies. The results of the studies were pooled, and an
overall standard mean difference with 95% confidence intervals
(CIs) was obtained using generic inverse variance weighting and
a random effects method.
RESULTS
The electronic and manual searches yielded 238 total citations (Figure 1). We identified 20 potentially relevant full-text
articles and analyzed six published articles, published as full
papers, which met our inclusion criteria. No additional abstracts
were identified by hand searches of conference proceedings.
Figure 1. Literature search strategy.
4
Two controlled clinical trials compared the effects of PPIs
and placebos on OSA (18, 19). The first trial was a double-blind,
randomized, placebo-controlled crossover trial (18). This trial
recruited 57 patients with ESS > 8 (mean ESS ± SD: 14 ± 3.5),
mild to moderate OSA (mean AHI ± SD: 10 ± 8.4), and typical
symptoms and finding of GERD between February 2004 and
August 2006 and treated them with either placebo or pantoprazole 40 mg once daily followed by a 2-week washout period
and then a 2-week crossover treatment period. ESS decreased
with pantoprazole (–1.8, 95% CI: –3.0 to –0.5) compared with
placebo (–1.5, 95% CI: –2.1 to –0.4, P = 0.04). There were
no significant changes in sleep-related quality of life using the
Functional Outcomes Sleep Questionnaire or reaction times,
tested by having subjects push a button as fast as they could
whenever they saw a clock begin counting up from 0000 (18).
The trial had a low risk of bias.
The second trial included 20 patients with confirmed OSA
(mean AHI: 30.9) by overnight polysomnography and confirmed GERD by 24 h esophageal pH electrode (19). The patients were randomly divided into two groups and treated with
omeprazole 20 mg or placebo 30 minutes before breakfast and
before dinner (n = 10 each group) for 6 weeks. The number of
apnea attacks, which were defined as a symptom of nocturnal
choking, gasping, or snoring that awakened the patients, was
recorded by patients in diaries. The frequency of apnea attacks
decreased 73% in the treatment group compared to their basal
period and in the treatment group compared with the placebo
group in the sixth week (P < 0.001). This trial had an unclear
risk of bias due to unclear reporting of randomization and allocation concealment techniques.
The four prospective cohort studies analyzed in this review
included 91 patients who had OSA and GERD. The main
characteristics of these studies are summarized in Table 1. Four
studies (20–23) reported data on AHI; three studies (20, 21,
23) provided data on apnea index, and three
studies (20, 22) reported data on ESS. These
trials had methodological limitations that
led to an unclear risk of bias since all studies
were single-center prospective cohort studies conducted in the United States, used
patients’ baseline parameters as the control,
and had small sample sizes.
Four observational studies compared the
effects of PPI use on AHI in patients before
treatment versus after treatment (20–23).
There was no statistically significant difference between the two groups. The standard
mean difference was 0.21 (95% CI: –0.11 to
0.54) (Table 2). Heterogeneity was minimal
in the studies (P for heterogeneity = 0.31,
I 2 = 17%).
Three observational studies (20, 21, 23)
compared the effects of PPI use on the apnea
index in patients before treatment versus after treatment. Two studies reported a statistically significant improvement in the apnea
Baylor University Medical Center Proceedings
Volume 29, Number 1
Table 1. Characteristics of obstructive sleep apnea patients using proton pump inhibitors
First author
Treated Control Mean
age Women
BMI
cases cases
Mean Mean
(years)
(n)
(kg/m2) ESS
(n)
(n)
AHI
Proton pump
inhibitor
(40 mg/day)
Randomized controlled trials
Suurna
28*
29
51
33
31
14
10
Pantoprazole
Bortolotti
10
10
55
3
30
NR
30.9
Omeprazole
statistically significant mean change in ESS
(21). Two studies reported decreased snoring as assessed by bed partners (20, 21),
and one reported decreased upper airway
inflammation based on fiberoptic nasopharyngoscopy examinations before and after
treatment (22).
DISCUSSION
The articles used in this systematic reFriedman
29
–
45
17
33
14.2
38
Esomeprazole
view and meta-analysis studied the effects
of PPIs on OSA indices, daytime sleepiness,
Steward
27
–
49
9
33
12.9 15.4 Pantoprazole
and other nocturnal symptoms. This analysis
Orr
25
–
43
7
31
12
9.3
Rabeprazole
included two randomized controlled trials
Senior
10
–
18–59
0
NR
NR
62
Omeprazole
and four observational prospective studies.
*Crossover design.
The studies identified a modest benefit of
AHI indicates apnea-hypopnea index; ESS, Epworth Sleepiness Scale; NR, not reported; –, not applicable.
PPI therapy on daytime somnolence but
did not identify any significant difference
in apnea or hypopnea indices. The effect on
Table 2. Effect of proton pump inhibitors on apnea and hypopnea indices*
the ESS was modest and not associated with
any change in sleep-related quality of life or
Before treatment
After treatment
Study or
Std. mean difference IV,
reaction times. The other trial reported a
subgroup
Mean SD Total Mean SD Total Weight
random, 95% CI
reduction in nocturnal symptoms based on
Friedman (2007) 37.9 19.1 29
28.8 11.5 29
30.3%
0.57 (0.04, 1.10)
diary records. The symptoms are not necesOrr (2009)
9.3
4.7 25
9.1
8.7 25
27.8%
0.03 (–0.53, 0.58)
sarily unique to OSA and could have other
Steward (2004)
15.4 11.7 27
16.2
8.0 27
29.6%
–0.08 (–0.61, 0.45)
causes during the night. The results with
Senior (2001)
62.0 30.5 10
46.0 37.0 10
12.2%
0.45 (–0.44, 1.34)
AHI comparisons should be interpreted
with caution, due to the clinical heterogeTotal (95% CI)
91
91 100.0%
0.21 (–0.11, 0.54)
neity among studies and unclear risk of bias.
*Heterogeneity: Tau2 = 0.02; Chi2 = 3.62; df = 3 (P = 0.31); F = 17%. Test for overall effect: Z = 1.28 (P = 0.20).
These limitations are discussed more below.
There are several potential explanations
for the lack of benefit with PPI therapy in patients with OSA.
index (mean 5.9 ± 7.2 to 3.8 ± 4.7, P = 0.04 in the study by
GERD and OSA are relatively common problems; they could
Friedman [20]; mean 45 [range: 10–108] to 31 [range: 1–78],
occur coincidentally in some patients and have no causal reP = 0.04 in the study by Senior [23]). However, the study
lationships. Shepherd and coworkers reported detailed studies
reported by Steward revealed no statistically significant differin eight patients with OSA undergoing polysomnography with
ence between the two groups (mean change 1.4, 95% CI: –0.1
esophageal manometry and pH monitoring (8). During the
to 2.9, P = 0.07) (21). No baseline mean apnea index in this
recording phase without CPAP, the patients had 70 ± 39 respirastudy was available.
tory events per hour and 2.7 ± 1.8 reflux events per hour. The
Three observational studies (20–22) compared the effects
number of obstructive events in this study appeared to have little
of PPI use on ESS in patients before treatment versus after
or no effect on reflux events. In addition, overlapping symptoms
treatment. Two studies reported statistically significant imcould confuse this situation and an y conclusions about cause
provement of ESS and provided numerical scores for the ESS
and effect relationships. However, very frequent reflux events
before and after treatment (Figure 2). One study reported a
could influence OSA and sleep quality through central nervous
system arousals, chronic lower esophageal inflammation with
vagal stimulation, and laryngeal inflammation with changes in
the upper airway dynamics.
There might be a threshold in the number of reflux events
required before any effect occurs, and the duration of these
two syndromes could influence any interaction. The treatment
of GERD with PPIs may require more time than most studies
have used in their study design. An adequate treatment period
for PPIs to completely resolve anatomic changes caused by acid
reflux–related injury can take up to 6 months; however, only
one study in this review reached that period of time (20, 24,
25). Another possibility is that PPI treatment may truly improve
Figure 2. Effect of proton pump inhibitors on Epworth Sleepiness Scale.
Prospective trials
January 2016
Effect of proton pump inhibitors on obstructive sleep apnea symptoms and indices in patients with GERD
5
OSA symptoms, but this effect would be important only in
patients with very frequent reflux events.
In addition, treatment with CPAP could have several possible effects on GERD which might influence results in studies
on GERD in patients with OSA. First, CPAP may have no
effect, or CPAP could change intrathoracic pressure dynamics
and reduce reflux. This effect most likely would occur at the
gastroesophageal junction. CPAP could also change esophageal
motility and improve esophageal clearance. Shepherd reported
that CPAP increased the nadir pressure in the lower esophagus
and reduced the duration of the lower esophageal sphincter
relaxation time (8). Again, these effects are important only in
patients with frequent reflux events.
Our meta-analysis has several limitations. First, our analysis included only six studies with small numbers of patients.
Second, there was heterogeneity across the studies in the analysis of AHI reduction. This can be partly explained by different study designs, types of PPIs, and duration of treatment.
Most studies had design limitations, including small sample
size and single-center cohort studies, which resulted in a low
strength of evidence. Observational studies that used patients’
baseline parameters as controls may be compromised by placebo effects in addition to other design limitations. The ESS is
a self-assessment scale that represents only a predilection to fall
asleep and is not a specific outcome in OSA patients. Other
symptoms reported in sleep diaries may not be specific for OSA
and may introduce another source of variability in study results.
Patients with GERD have reduced health-related quality of life,
and this is associated with nocturnal reflux symptoms (26, 27).
We used a random effects method for analysis to account for
heterogeneity among studies, and we attempted to minimize the
risk of missing relevant studies by searching multiple databases,
bibliographies, and trial registries.
1.
2.
3.
4.
5.
6.
7.
6
Ing AJ, Ngu MC, Breslin AB. Obstructive sleep apnea and gastroesophageal reflux. Am J Med 2000;108(Suppl 4a):120S–125S.
Green BT, Broughton WA, O’Connor JB. Marked improvement in
nocturnal gastroesophageal reflux in a large cohort of patients with obstructive sleep apnea treated with continuous positive airway pressure.
Arch Intern Med 2003;163(1):41–45.
Valipour A, Makker HK, Hardy R, Emegbo S, Toma T, Spiro SG. Symptomatic gastroesophageal reflux in subjects with a breathing sleep disorder.
Chest 2002;121(6):1748–1753.
Guda N, Partington S, Vakil N. Symptomatic gastro-oesophageal reflux, arousals and sleep quality in patients undergoing polysomnography
for possible obstructive sleep apnoea. Alimentary Pharm Therapeutics
2004;20(10):1153–1159.
Graf KI, Karaus M, Heinemann S, Körber S, Dorow P, Hampel KE.
Gastroesophageal reflux in patients with sleep apnea syndrome. Z
Gastroenterol 1995;33(12):689–693.
Penzel T, Becker HF, Brandenburg U, Labunski T, Pankow W, Peter JH.
Arousal in patients with gastro-oesophageal reflux and sleep apnoea. Eur
Respir J 1999;14(6):1266–1270.
Janson C, Gislason T, De Backer W, Plaschke P, Björnsson E, Hetta J,
Kristbjarnason H, Vermeire P, Boman G. Daytime sleepiness, snoring
and gastro-oesophageal reflux amongst young adults in three European
countries. J Intern Med 1995;237(3):277–285.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
Shepherd K, Hillman D, Holloway R, Eastwood P. Mechanisms of
nocturnal gastroesophageal reflux events in obstructive sleep apnea.
Sleep Breath 2011;15(3):561–570.
Kerr P, Shoenut JP, Millar T, Buckle P, Kryger MH. Nasal CPAP reduces
gastroesophageal reflux in obstructive sleep apnea syndrome. Chest
1992;101(6):1539–1544.
Zanation AM, Senior BA. The relationship between extraesophageal reflux
(EER) and obstructive sleep apnea (OSA). Sleep Med Rev 2005;9(6):453–458.
Kim HN, Vorona RD, Winn MP, Doviak M, Johnson DA, Ware JC.
Symptoms of gastro-oesophageal reflux disease and the severity of
obstructive sleep apnoea syndrome are not related in sleep disorders center
patients. Aliment Pharmacol Ther 2005;21(9):1127–1133.
Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J; Cooperative
Group Burgos-Santander. The association between sleep apnea and the
risk of traffic accidents. N Engl J Med 1999;340(11):847–851.
Hla KM, Young TB, Bidwell T, Palta M, Skatrud JB, Dempsey J. Sleep
apnea and hypertension. A population-based study. Ann Intern Med
1994;120(5):382–388.
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino
RB, Newman AB, Lebowitz MD, Pickering TG. Association of sleepdisordered breathing, sleep apnea, and hypertension in a large communitybased study. Sleep Heart Health Study. JAMA 2000;283(14):1829–1836.
Caples SM, Somers VK. Sleep-disordered breathing and atrial fibrillation.
Prog Cardiovasc Dis 2009;51(5):411–415.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD,
Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group;
Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool
for assessing risk of bias in randomised trials. BMJ 2011;343:d5928.
Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A.
GRADE guidelines: a new series of articles in the Journal of Clinical
Epidemiology. J Clin Epidemiol 2011;64(4):380–382.
Suurna MV, Welge J, Surdulescu V, Kushner J, Steward DL. Randomized
placebo-controlled trial of pantoprazole for daytime sleepiness in GERD
and obstructive sleep disordered breathing. Otolaryngol Head Neck Surg
2008;139(2):286–290.
Bortolotti M, Gentilini L, Morselli C, Giovannini M. Obstructive sleep
apnoea is improved by a prolonged treatment of gastrooesophageal reflux
with omeprazole. Dig Liver Dis 2006;38(2):78–81.
Friedman M, Gurpinar B, Lin HC, Schalch P, Joseph NJ. Impact of
treatment of gastroesophageal reflux on obstructive sleep apnea-hypopnea
syndrome. Ann Otol Rhinol Laryngol 2007;116(11):805–811.
Steward DL. Pantoprazole for sleepiness associated with acid reflux and obstructive sleep disordered breathing. Laryngoscope 2004;114(9):1525–1528.
Orr WC, Robert JJ, Houck JR, Giddens CL, Tawk MM. The effect of
acid suppression on upper airway anatomy and obstruction in patients
with sleep apnea and gastroesophageal reflux disease. J Clin Sleep Med
2009;5(4):330–334.
Senior BA, Khan M, Schwimmer C, Rosenthal L, Benninger M.
Gastroesophageal reflux and obstructive sleep apnea. Laryngoscope
2001;111(12):2144–2146.
Belafsky PC, Postma GN, Koufman JA. Laryngopharyngeal reflux
symptoms improve before changes in physical findings. Laryngoscope
2001;111(6):979–981.
Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux:
position statement of the Committee on Speech, Voice, and Swallowing
Disorders of the American Academy of Otolaryngology–Head and Neck
Surgery. Otolaryngol Head Neck Surg 2002;127(1):32–35.
Farup C, Kleinman L, Sloan S, Ganoczy D, Chee E, Lee C, Revicki D. The
impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med 2001;161(1):45–52.
Revicki DA, Wood M, Maton PN, Sorensen S. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med
1998;104(3):252–258.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Serum hyperchloremia as a risk factor for acute kidney
injury in patients with ST-segment elevation myocardial
infarction undergoing percutaneous coronary intervention
Nachiket Patel, MD, Sarah M. Baker, BSN, RN, Ryan W. Walters, MS, Ajay Kaja, MBBS, Vimalkumar Kandasamy, MBBS,
Ahmed Abuzaid, MBChB, and Ariel M. Modrykamien, MD
A high serum chloride concentration has been associated with the development of acute kidney injury in critically ill patients. However, the
association between hyperchloremia and acute kidney injury (AKI) in patients admitted with ST-segment elevation myocardial infarction (STEMI)
treated with percutaneous coronary intervention (PCI) is unknown. A
retrospective analysis of consecutive patients admitted with the diagnosis
of STEMI and treated with PCI was performed. Subjects were classified
as having hyper- or normochloremia based upon their admission serum
chloride level. Multivariable logistic regression analyses were employed
for the primary and secondary outcomes. The primary analysis evaluated whether high serum chloride on admission was associated with the
development of AKI after adjusting for age, diabetes mellitus, admission
systolic blood pressure, contrast volume used during angiography, Killip
class, and need for vasopressor therapy or intraaortic balloon pump. The
secondary analyses evaluated whether high serum chloride was associated with sustained ventricular tachycardia or fibrillation. Of 291 patients
(26.1% female, mean age of 59.9 ± 12.6 years, and mean body mass
index of 29.3 ± 6.1 kg/m2), 25 (8.6%) developed AKI. High serum chloride
on admission did not contribute significantly to the development of AKI
(odds ratio, 95%; confidence interval, 0.90 to 1.24). In addition, serum
chloride on admission was not significantly associated with sustained
ventricular tachycardia or fibrillation after adjusting for demographic and
clinical covariates. In conclusion, our study demonstrated no association
between baseline serum hyperchloremia and an increased risk of AKI in
patients admitted with STEMI treated with PCI.
C
oronary angiography is the third leading cause of acute
kidney injury (AKI) among hospitalized patients (1,
2). Several risk factors for the development of radiocontrast-induced kidney injury have been identified,
including diabetes mellitus, chronic kidney disease, and heart
failure (3–5). Since AKI after angiography has been associated
with a variety of adverse clinical outcomes, such as increased
mortality, cardiovascular events, and prolonged hospitalization,
several lines of investigation have focused on finding risk factors
to predict its occurrence (6, 7). Particularly, the relation between
serum chloride concentration and the development of AKI has
been gaining increasing attention. Among critically ill patients,
the presence of a high chloride concentration prior to intensive care unit (ICU) admission has been associated with AKI.
Proc (Bayl Univ Med Cent) 2016;29(1):7–11
Furthermore, a positive correlation between chloride levels and
severity of AKI has also been described (8). Recent investigations have shown that baseline hyperchloremia >110 mEq/L is
associated with higher hospital mortality in critically ill septic
patients (9). Other recently published articles have revealed
that the administration of chloride-enriched fluids is associated with renal vasoconstriction and the subsequent decline of
glomerular filtration rate (10, 11). Consequently, strategies of
fluid resuscitation using chloride-restrictive solutions have been
studied, demonstrating a lower incidence of AKI compared with
chloride-liberal fluid strategies (12). Despite the aforementioned
data, many gaps in our understanding of the relation between
serum chloride levels and consequent AKI still remain. Specifically, whether high chloride concentration is a risk factor for the
development of AKI in patients undergoing coronary angiography is currently unknown. This study addressed this question
by analyzing data from a consecutive series of patients who
underwent emergent cardiac catheterization due to ST-segment
elevation myocardial infarction (STEMI) at our institution.
METHODS
We conducted a single-center retrospective study to assess the
association between serum hyperchloremia at hospital admission
and AKI in patients admitted with STEMI treated with emergent percutaneous coronary intervention (PCI). After approval
by the institutional review board of the Creighton University
School of Medicine, we collected data from patients admitted with STEMI who underwent emergent PCI from January
2003 to June 2010. Patients whose admission serum sodium
was outside the physiological range, <135 and >145 mEq/L,
were excluded. Hyperchloremia was defined as a serum chloride
From the Division of Cardiology University of Florida College of Medicine,
Jacksonville (Patel); the Division of Clinical Research and Evaluative Sciences
(Walters) and Division of General Internal Medicine (Kaja, Kandasamy, Abuzaid),
Creighton University School of Medicine, Omaha, Nebraska; Intensive Care Unit,
Alegent-Creighton Health, Creighton University Medical Center, Omaha, Nebraska
(Baker); and Division of Pulmonary and Critical Care Medicine, Baylor University
Medical Center at Dallas, Dallas, Texas (Modrykamien).
Corresponding author: Ariel Modrykamien, MD, Medical Director, Respiratory
Care Services, Division of Pulmonary and Critical Care Medicine, Baylor University
Medical Center at Dallas, 3600 Gaston Avenue, Suite 960, Dallas, TX 75246
(e-mail: ariel.modrykamien@baylorhealth.edu).
7
as discriminative ability via C-statistic. Perfect discrimination
concentration >75% of the serum sodium concentration on the
yields a C-statistic of 1.0, whereas a C-statistic of 0.50 indicates
electrolyte panel obtained at the time of admission. Normochlorthat discrimination was no better than chance. For analysis,
emia was defined as a serum chloride concentration ≤75% of
continuous variables were centered near their mean. All analyses
the serum sodium concentration (13). Electrolyte measurements
were performed using SAS v. 9.3 (SAS Institute, Inc); P < .05
were performed using the Dimension Vista® 500 (Siemens, Newwas considered statistically significant for all analyses.
ark, DE). Demographic, clinical, procedural, and outcome data
were collected. Importantly, patients with end-stage renal disease
RESULTS
undergoing intermittent hemodialysis or peritoneal dialysis, as
Of the 401 patients admitted with STEMI and treated with
well as pregnant women, were excluded from this study.
PCI between January 2003 and June 2010, 105 had abnormal
The primary outcome of interest was the development of
serum sodium on admission (104 patients <135 mEq/L and 1
AKI during the hospitalization, within 7 days after PCI. AKI
patient >145 mEq/L); these patients were excluded from analywas defined based on changes in creatinine concentration, acsis. Of the remaining 296 patients, 5 did not have complete
cording to criteria of the Acute Kidney Injury Network (14).
data. Thus, analyses included 291 patients, with 26.1% female,
This classification and staging system of AKI states that the
a mean age of 59.9 ± 12.6 years, and a mean body mass index
elevation of baseline creatinine by 1.5 to 1.9 times, or an absoof 29.3 ± 6.1 kg/m2.
lute increase of 0.3 mg/dL from the baseline (both within 48
hours of a known baseline), constitute the first stage of AKI.
Descriptive statistics for demographic and clinical variThe secondary endpoint was the development of either susables are presented in Table 1. Of the 291 patients, 25 (8.6%)
tained ventricular tachycardia or ventricular fibrillation durdeveloped AKI and had significantly greater corrected anion
ing the hospitalization. Sustained ventricular tachycardia was
gap, as well as higher rates of intraaortic balloon pump use
defined as lasting >30 seconds or requiring termination due to
and cardiogenic shock, and were more likely to have higher
hemodynamic instability in <30 seconds (15).
Killip class compared with patients who did not develop AKI.
Continuous demographic and clinical variables are presented as mean ±
Table 1. Univariate analyses of demographic and clinical covariates
standard deviation, whereas categorical
variables are presented as frequency and
Acute kidney injury
percentage. Differences in these variables
No (n = 266)
Yes (n = 25)
P
between patients who developed AKI and
Age (years)
0.08
patients who did not were evaluated using
59.5 ± 12.5
64.1 ± 13.7
independent-samples t tests for continu2
0.30
Body mass index (kg/m )
29.2 ± 6.0
30.5 ± 6.2
ous variables and Pearson’s χ2 or Fisher’s
Admit systolic blood pressure (mm Hg)
0.7
122.4 ± 19.6
120.7 ± 22.1
exact tests for categorical variables.
Admit sodium (mEq/L)
0.99
137.9 ± 2.0
137.9 ± 1.9
Multivariable logistic regression analyses were employed for the primary and
Admit chloride (mEq/L)
0.65
104.0 ± 3.4
104.2 ± 3.0
secondary analyses. The primary analysis
Admit glomerular filtration rate (mL/min)
1.0
83.3 ± 26.1
83.3 ± 41.6
evaluated whether serum chloride on adContrast volume (mL)
0.89
171.2 ± 72.2
173.3 ± 91.8
mission was associated with the developCorrected
anion
gap
(mEq/L)
<0.05
10.3 ± 2.8
12.5 ± 3.4
ment of AKI in patients admitted with
STEMI after adjusting for age, diabetes
Female
68 (26%)
8 (32%)
0.45
mellitus, contrast volume (iopamidol 755
Smoker
142 (53%)
12 (48%)
0.86
mg/mL, Bracco Diagnostics, NJ) adminHypertension
144 (54%)
17 (68%)
0.41
istered, Killip class, use of pressor medicaDiabetes mellitus
4 1 (15%)
7 (28%)
0.05
tions or intraaortic balloon pump, whether
the patient suffered cardiogenic shock durHyperlipidemia
127 (48%)
14 (56%)
1.00
ing hospitalization, corrected anion gap, as
Use of pressors
9 (3%)
3 (12%)
<0.05
well as systolic blood pressure, glomerular
Intraaortic balloon pump (used)
12 (5%)
7 (28%)
<0.05
filtration rate, and systolic blood pressure
Killip class
<0.05
on admission. Two secondary analyses evaluated whether serum chloride on admission
I
227 (84%)
13 (52%)
was associated with sustained ventricular
II
24 (9%)
4 (16%)
tachycardia or ventricular fibrillation after
III
11 (4%)
3 (12%)
adjusting for the same demographic and
IV
7 (4%)
5 (20%)
clinical covariates listed above.
The accuracy of the logistic regresShock
16 (6%)
8 (32%)
<0.05
sion models was assessed by Hosmer
Data presented as mean ± standard deviation or as n (%).
and Lemeshow goodness of fit as well
8
Baylor University Medical Center Proceedings
Volume 29, Number 1
subgroup analyses aimed at studying particular ICU patients, such as those with
trauma, abdominal surgery, and cardio95% CI for OR
vascular diseases, revealed similar results.
Lower
Upper
Variable
Coefficient
SE
OR
AKI in the context of hyperchloremia
Intercept
–2.76
1.17
0.06
0.11
10.60
could be explained by several physiologic
mechanisms. Wilcox et al (10) used an
Age (0 = 60)
0.03
0.02
1.03
0.99
1.07
animal model to demonstrate the speDiabetes mellitus
0.50
0.57
1.64
0.54
4.99
cific vasoconstrictive effect of chloride
Use of pressors
0.00
0.94
1.00
0.16
6.36
in renal vessels, with subsequent reduction of cortical perfusion and increase of
Intraaortic balloon pump
1.22
0.77
3.38
0.75
15.29
inflammatory mediators. Furthermore,
Killip class (reference = IV)
Wu et al (16) specifically assessed the efI
–0.65
1.04
0.52
0.07
4.00
fect of chloride in the inflammatory casII
0.03
1.04
1.03
0.13
7.88
cade. Strikingly, patients randomized to
receive saline 0.9% had higher C-reactive
III
0.54
1.13
1.72
0.19
15.78
protein levels and higher rates of systemic
Shock
0.96
0.84
2.60
0.50
13.62
inflammatory response syndrome comAdmit sodium (0 = 135)
0.01
0.12
1.01
0.79
1.28
pared with subjects treated with Ringer’s
Admit glomerular filtration rate (0 = 85)
0.00
0.01
1.00
0.99
1.02
solutions.
Based on the aforementioned data, reAdmit systolic blood pressure (0 = 121)
0.01
0.01
1.01
0.99
1.03
cent
investigations attempted to compare
Control volume (0 = 172)
0.00
0.00
1.00
0.99
1.01
different fluid resuscitation strategies in
Corrected anion gap (0 = 10)
0.25
0.09
1.28*
1.08
1.52
critically ill patients. Particularly, Yunos
Admit chloride (0 = 105)
0.05
0.08
1.06
0.90
1.24
et al (12) compared a chloride-restrictive
vs a chloride-liberal fluid strategy in
*P < 0.05.
a before-and-after study. As expected,
CI indicates confidence interval; OR, odds ratio; SE, standard error.
patients in the chloride-restrictive arm
received less chloride (496 vs 694 mmol
per patient) and had lower rates of AKI. Nevertheless, this study
Nonsignificant clinical covariates were included in the multidid not report serum chloride levels in each arm, limiting the
variable analysis due to theoretical considerations.
interpretation of whether the presented outcome was directly
Final model results from the multivariable logistic regression
associated with chloride concentrations.
analysis for AKI are presented in Table 2. The logistic model fit
2
Despite the studies demonstrating adverse renal outthe data well (χ 8 = 6.90, P = .55) with good discrimination
comes associated with hyperchloremia and administration of
(C = 0.81; 95% confidence interval [CI] = 0.70 to 0.91). After
chloride-liberal fluids, our study did not show an association
adjustment, serum chloride on admission did not contribute
between hyperchloremia and the development of post-PCI AKI.
significantly to the development of AKI (odds ratio, 95%;
However, these results seem to be in line with prior studies
CI = 0.90 to 1.24). In addition, serum chloride on admisexamining the effect of the type of fluid administration on
sion was not significantly associated with sustained ventricular
the development of AKI in patients undergoing coronary antachycardia or fibrillation after adjusting for demographic and
giography, none of which demonstrated any relation between
clinical covariates.
the concentration of chloride administered in the intravenous
fluid and the development of AKI. Specifically, Mueller et al
DISCUSSION
(17) found that hydration with 0.9% saline before and after
This study shows the following results: 1) hyperchloremia
exposure to contrast media significantly reduced the incidence
upon hospital admission is not associated with the developof contrast-induced nephropathy compared with 0.45% saline
ment of AKI post-PCI, and 2) hyperchloremia is not associated
with dextrose in patients undergoing coronary angiography. In
with severe arrhythmias post-PCI, such as sustained ventricular
addition, two prospective studies comparing 0.9% saline and
tachycardia or ventricular fibrillation.
isotonic bicarbonate in patients who received contrast media for
Several studies suggest adverse outcomes associated with the
coronary angiography found no difference in the development
presence of serum hyperchloremia. Specifically, Zhang et al (8)
of contrast-induced nephropathy (18, 19). The role of chloride
retrospectively evaluated a consecutive series of patients admitin the development of AKI in patients undergoing coronary
ted in a mixed ICU for the presence of hyperchloremia and
angiography and PCI remains to be clarified.
its association with AKI. Interestingly, patients with higher
We focused our study on patients with STEMI treated
chloride concentrations had a statistically significant associawith PCI. This particular group has an increased incidence
tion with the development of AKI (chloride concentrations
of AKI postprocedure, mostly due to contrast nephrotoxicity.
of 118.8 ± 8.1 vs 107.9 ± 5.4 mmol/L; P < 0.001). Notably,
Table 2. Multivariable logistic regression results for development of acute kidney injury
January 2016
Serum hyperchloremia as a risk factor for acute kidney injury in patients with STEMI undergoing PCI
9
As a matter of fact, the rate of kidney injury in this patient
population ranges from 2% to 30%, being higher in individuals with baseline creatinine >2 mg/dL prior to the procedure
(3, 20). Previous studies revealed a higher incidence of AKI
postangiography in specific populations, such as those with
preexisting renal disease, diabetes, congestive heart failure, and
those receiving large intraprocedural volumes of hyperosmolar contrast (21–25). However, we were unable to find these
associations after adjustment for some of those variables. It
is possible that our sample was not large enough to find the
aforementioned results.
We attempted to assess whether the presence of hyperchloremia was associated with severe cardiac arrhythmias, namely sustained ventricular tachycardia or fibrillation. Studies in animal
models and humans showed associations between electrolyte
disturbances and cardiac arrhythmias. The cardiac implications
of potassium, calcium, magnesium, and sodium alterations have
been extensively described (26–32). Nevertheless, no prior reports have focused on the eventual arrhythmogenic effects of
abnormal chloride concentrations. Our study revealed no significant differences in the incidence of ventricular arrhythmias
associated with chloride levels.
The present study has many strengths. First, this is the first
report that aimed to assess the relationship between baseline
chloride concentrations and kidney function post-PCI. Second,
this is the first study to address the impact of hyperchloremia
in cardiac arrhythmias. Although we did not find any association between serum chloride levels and arrhythmias, our study
may be hypothesis generating for further research in this area.
Third, variables included in our statistical analysis were obtained from prior validated models, which showed association
between each of them and the development of contrast-induced
nephropathy (33).
Despite its strengths, our study also presents several limitations. First, being a retrospective study, it is likely that we
incurred a selection bias. The lack of relevant information on
nine patients affected the completeness of our dataset. Therefore, it is possible that our results may have changed had these
subjects been included. Second, the small number of patients
could have led to underestimation of important differences in
clinical outcomes, such as incidence of cardiac arrhythmias.
Last, a number of relevant factors, such as hemoglobin A1c
levels, ventricular ejection fraction, and use of prior nephrotoxic
medications, were not included in our dataset. These meaningful factors could have altered the incidence of AKI without our
knowledge.
1.
2.
3.
4.
10
Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced
by contrast medium. N Engl J Med 2006;354(4):379–386.
Finn WF. The clinical and renal consequences of contrast-induced
nephropathy. Nephrol Dial Transplant 2006;21(6):i2–i10.
McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute
renal failure after coronary intervention: incidence, risk factors, and
relationship to mortality. Am J Med 1997;103(5):368–375.
Bartholomew BA, Harjai KJ, Dukkipati S, Boura JA, Yerkey MW, Glazier
S, Grines CL, O’Neill WW. Impact of nephropathy after percutaneous
coronary intervention and a method for risk stratification. Am J Cardiol
2004;93(12):1515–1519.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
McCullough PA, Stacul F, Becker CR, Adam A, Lameire N, Tumlin
JA, Davidson CJ; CIN Consensus Working Panel. Contrast-Induced
Nephropathy (CIN) Consensus Working Panel: executive summary.
Rev Cardiovasc Med 2006;7(4):177–197.
Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, Palevsky
PM. Associations of increases in serum creatinine with mortality and
length of hospital stay after coronary angiography. J Am Soc Nephrol
2006;17(10):2871–2877.
James MT, Samuel SM, Manning MA, Tonelli M, Ghali WA, Faris P,
Knudtson ML, Pannu N, Hemmelgarn BR. Contrast-induced acute
kidney injury and risk of adverse clinical outcomes after coronary
angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv
2013;6(1):37–43.
Zhang Z, Xu X, Fan H, Li D, Deng H. Higher serum chloride concentrations are associated with acute kidney injury in unselected critically ill
patients. BMC Nephrol 2013;14:235.
Neyra JA, Canepa-Escaro F, Li X, Manllo J, Adams-Huet B, Yee J, Yessayan
L; Acute Kidney Injury in Critical Illness Study Group. Association of
hyperchloremia with hospital mortality in critically ill septic patients. Crit
Care Med 2015;43(9):1938–1944.
Wilcox CS. Regulation of renal blood flow by plasma chloride. J Clin
Invest 1983;71(3):726–735.
Wilcox CS. Renal haemodynamics during hyperchloraemia in the
anaesthetized dog: effects of captopril. J Physiol 1988;406:27–34.
Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid
administration strategy and kidney injury in critically ill adults. JAMA
2012;308(15):1566–1572.
Durward A, Skellett S, Mayer A, Taylor D, Tibby SM, Murdoch IA.
The value of the chloride:sodium ratio in differentiating the aetiology of
metabolic acidosis. Intensive Care Med 2001;27(5):828–835.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG,
Levin A. Acute Kidney Injury Network: report of an initiative to improve
outcomes in acute kidney injury. Crit Care 2007;11(2):R31.
Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer
M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones
MA, Roden DM, Silka MJ, Tracy C, Smith SC Jr, Jacobs AK, Adams CD,
Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato
JP, Page RL, Riegel B, Blanc JJ, Budaj A, Dean V, Deckers JW, Despres
C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey
A, Tamargo JL, Zamorano JL. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of
sudden cardiac death. Circulation 2006;114(10):e385–e484.
Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, Smith B,
Banks PA, Conwell DL. Lactated Ringer’s solution reduces systemic
inflammation compared with saline in patients with acute pancreatitis.
Clin Gastroenterol Hepatol 2011;9(8):710–717.e1.
Mueller C, Buerkle G, Buettner HJ, Petersen J, Perruchoud AP, Eriksson
U, Marsch S, Roskamm H. Prevention of contrast media–associated
nephropathy: randomized comparison of 2 hydration regimens in
1620 patients undergoing coronary angioplasty. Arch Intern Med
2002;162(3):329–336.
Maioli M, Toso A, Leoncini M, Gallopin M, Tedeschi D, Micheletti
C, Bellandi F. Sodium bicarbonate versus saline for the prevention
of contrast-induced nephropathy in patients with renal dysfunction
undergoing coronary angiography or intervention. J Am Coll Cardiol
2008;52(8):599–604.
Adolph E, Holdt-Lehmann B, Chatterjee T, Paschka S, Prott A, Schneider
H, Koerber T, Ince H, Steiner M, Schuff-Werner P, Nienaber CA. Renal
Insufficiency Following Radiocontrast Exposure Trial (REINFORCE): a
randomized comparison of sodium bicarbonate versus sodium chloride
hydration for the prevention of contrast-induced nephropathy. Coron
Artery Dis 2008;19(6):413–419.
Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, Singh M,
Bell MR, Barsness GW, Mathew V, Garratt KN, Holmes DR Jr. Incidence and prognostic importance of acute renal failure after percutaneous
coronary intervention. Circulation 2002;105(19):2259–2264.
Baylor University Medical Center Proceedings
Volume 29, Number 1
21. Stacul F, van der Molen AJ, Reimer P, Webb JA, Thomsen HS, Morcos
SK, Almén T, Aspelin P, Bellin MF, Clement O, Heinz-Peer G; Contrast
Media Safety Committee of European Society of Urogenital Radiology
(ESUR). Contrast induced nephropathy: updated ESUR Contrast Media
Safety Committee guidelines. Eur Radiol 2011;21(12):2527–2541.
22. Parfrey PS, Griffiths SM, Barrett BJ, Paul MD, Genge M, Withers J,
Farid N, McManamon PJ. Contrast material–induced renal failure in
patients with diabetes mellitus, renal insufficiency, or both. A prospective
controlled study. N Engl J Med 1989;320(3):143–149.
23. Seeliger E, Sendeski M, Rihal CS, Persson PB. Contrast-induced
kidney injury: mechanisms, risk factors, and prevention. Eur Heart J
2012;33(16):2007–2015.
24. Heinrich MC, Kuhlmann MK, Grgic A, Heckmann M, Kramann B, Uder
M. Cytotoxic effects of ionic high-osmolar, nonionic monomeric, and
nonionic iso-osmolar dimeric iodinated contrast media on renal tubular
cells in vitro. Radiology 2005;235(3):843–849.
25. Tehrani S, Laing C, Yellon DM, Hausenloy DJ. Contrast-induced acute
kidney injury following PCI. Eur J Clin Invest 2013;43(5):483–490.
26. Schulman M, Narins RG. Hypokalemia and cardiovascular disease. Am
J Cardiol 1990;65(10):4E–9E.
January 2016
27. Gettes L, Surawicz B. Effects of low and high concentrations of potassium
on the simultaneously recorded Purkinje and ventricular action potentials
of the perfused pig moderator band. Circ Res 1968;23(6):717–729.
28. Hohnloser SH, Verrier RL, Lown B, Raeder EA. Effect of hypokalemia
on susceptibility to ventricular fibrillation in the normal and ischemic
canine heart. Am Heart J 1986;112(1):32–35.
29. Ettinger PO, Regan TJ, Oldewurtel HA. Hyperkalemia, cardiac conduction, and the electrocardiogram: a review. Am Heart J 1974;88(3):360–371.
30. Leitch SP, Brown HF. Effect of raised extracellular calcium on characteristics of the guinea-pig ventricular action potential. J Mol Cell Cardiol
1996;28(3):541–551.
31. Keller PK, Aronson RS. The role of magnesium in cardiac arrhythmias.
Prog Cardiovasc Dis 1990;32(6):433–448.
32. El-Sherif N, Turitto G. Electrolyte disorders and arrhythmogenesis.
Cardiol J 2011;18(3):233–245.
33. Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz
GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G. A simple
risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll
Cardiol 2004;44(7):1393–1399.
Serum hyperchloremia as a risk factor for acute kidney injury in patients with STEMI undergoing PCI
11
Frequency of fluid overload and usefulness of bioimpedance
in patients requiring intensive care for sepsis syndromes
Timothy R. Larsen, DO, Gurbir Singh, MD, Victor Velocci, MD, Mohamed Nasser, MD, and Peter A. McCullough, MD, MPH
Guideline-directed therapy for sepsis calls for early fluid resuscitation.
Often patients receive large volumes of intravenous fluids. Bioimpedance
vector analysis (BIVA) is a noninvasive technique useful for measuring
total body water. In this prospective observational study, we enrolled
18 patients admitted to the intensive care unit for the treatment of
sepsis syndromes. Laboratory data, clinical parameters, and BIVA were
recorded daily. All but one patient experienced volume overload during
the course of treatment. Two patients had >20 L of excess volume.
Volume overload is clinically represented by tissue edema. Edema is
not a benign condition, as it impairs tissue oxygenation, obstructs capillary blood flow, disrupts metabolite clearance, and alters cell-to-cell
interactions. Specifically, volume overload has been shown to impair
pulmonary, cardiac, and renal function. A positive fluid balance is a
predictor of hospital mortality. As septic patients recover, volume excess
should be aggressively treated with the use of targeted diuretics and
renal replacement therapies if necessary.
T
he mainstay of treatment for sepsis is the early initiation of both antibiotic therapy and fl uid resuscitation (1). Recommendations based on the early
goal-directed therapy algorithm call for continued
administration of intravenous fluid until the central venous
pressure is at least 8 mm Hg (2) with the goal of maintaining
perfusion of vital organs. The underlying pathophysiologic
mechanism responsible for hypotension and hypoperfusion is
a combination of vasodilatation (leading to peripheral blood
pooling) and increased vascular permeability, which allows
fluid transfer from the vascular space to the interstitial fluid
compartment. The latter can result in large intravascular fluid
deficits. Bioimpedance vector analysis (BIVA) is a noninvasive technique that utilizes the principle that the body acts
as an electrical circuit with a measureable resistance and reactance. BIVA can be used to accurately quantify total body
water and is comparable to the gold standard of deuterium
dilution (r > 0.99) (3). BIVA has been used to identify volume overload in heart failure (4), liver disease (5), and renal
failure (6). We examined the incidence and degree of volume
overload in patients admitted to the intensive care unit (ICU)
for sepsis syndromes.
12
METHODS
In this prospective observational study, BIVA was used to
measure total body water in patients admitted to the ICU for
the treatment of sepsis syndromes. Bioimpedance was measured
using an EFG Diagnostics CardioEFG machine. This device was
approved by TriMedx clinical engineering. The first measurement had to be obtained within 24 hours of ICU admission.
Serial measurements of total body water were taken until ICU
discharge or day 8, whichever occurred first.
We enrolled patients >18 years old who were admitted to
the ICU with the diagnosis of sepsis, severe sepsis, or septic
shock. Patients were classified as having sepsis, severe sepsis, or
septic shock based on the definitions set forth by the American
College of Chest Physicians/Society of Critical Care Medicine
(7). We excluded patients with end-stage liver or kidney disease
(requiring dialysis). Data on demographic and clinical characteristics were collected prospectively. Excess total body water
(in L) was calculated by subtracting 74.3 (the upper limit of
normal) from the measured percent total body volume and
multiplying the difference by patient weight in kg. Written
informed consent was obtained from all participants prior to
enrollment. The study protocol was approved by the St. John
Providence Institutional Review Board.
RESULTS
A total of 18 patients were enrolled; 11 (61%) were men and
7 (39%) were women, and the mean age was 71 years (range,
43–93). Diabetes mellitus was present in 10 (56%) patients; hypertension, 14 (78%); heart failure, 4 (22%); liver disease, 1 (6%);
From the Department of Internal Medicine, Section of Cardiology, Virginia Tech
Carilion School of Medicine, Roanoke, Virginia (Larsen); Department of Internal
Medicine, Providence Hospital and Medical Center, Southfield, Michigan (Singh,
Velocci, Nasser); and Baylor Heart and Vascular Institute, Baylor Jack and Jane
Hamilton Heart and Vascular Hospital and Baylor University Medical Center, Dallas,
Texas, and The Heart Hospital, Plano, Texas (McCullough).
Funding for this project was provided by the Providence Hospital and Medical
Center Research Committee.
Corresponding author: Timothy R. Larsen, DO, Department of Internal Medicine,
Section of Cardiology, Virginia Tech Carilion School of Medicine, 2001 Crystal
Spring Avenue, Suite 203, Roanoke, VA 24014 (e-mail: tlarsen17@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):12–15
Table 1. Patient characteristics
Age
(yrs)
1
Peak %
TBW
Mean daily
excess vol
(L)
Peak
excess
vol (L)
RH
84.9
6.5
8.0
Shock
RH
90.7
5.7
9.0
Shock
RF
96.9
9.1
11.4
31
Shock
RH
92.0
12.6
15.1
49
Shock
RH
92.9
17.7
26.2
4
37
Severe sepsis
RF
91.3
14.5
17.2
M
2
19
Shock
RH
91.8
10.9
11.1
M
4
30
Sepsis
Overdose
90.2
9.4
15.9
Gender
ICU LOS
(days)
BMI
(kg/m2)
Diagnosis
43
F
2
29
Severe sepsis
2
47
M
4
21
3
47
M
8
41
4
61
F
4
5
61
F
4
6
63
F
7
68
8
69
Patient
Reason for
ICU admit
9
69
F
5
26
Severe sepsis
RF
93.2
15.3
15.9
10
74
F
3
21
Severe sepsis
RF
91.4
7.5
8.2
11
75
M
1
22
Sepsis
Acidosis
81.2
5.0
5.0
12
81
M
3
25
Sepsis
RF
89.2
6.2
10.0
13
82
M
5
21
Severe sepsis
RH
82.5
1.4
5.6
14
82
F
2
19
Severe sepsis
RH
73.9
0
0
15
85
M
5
20
Shock
RH
93.1
10.1
11.3
16
85
M
6
19
Shock
RH
92.2
10.1
11.5
17
87
M
5
37
Shock
RF
94.0
21.3
23.4
18
93
M
3
21
Severe sepsis
RH
89.0
7.4
14.9
BMI indicates body mass index; ICU, intensive care unit; LOS, length of stay; RF, respiratory failure; RH, refractory hypotension; TBW, total body water; VOL, volume overload.
(r = 0.70, P = 0.001). On day 1, 10 (56%) had clinically evident
edema, and by day 3, all patients remaining in the ICU had
clinically evident edema. Twelve (67%) developed radiographic
evidence of pulmonary edema. Mean ICU stay was 3.8 days
(range, 1–6 days). Mean excess volume peaked on day 5 at
13.5 L. Individual patients’ peak volume excess ranged from
none (1 patient) to 26.2 L (Figure 4).
DISCUSSION
Patients with sepsis syndromes require large quantities of
intravenous fluids. There has been much debate over the use
of colloid versus crystalloid solutions for resuscitation. Several
studies have failed to identify an advantage in using colloids over
crystalloids, with emerging evidence demonstrating increased
Excess volume (L)
current tobacco use, 8 (44%); and former tobacco use, 3 (17%).
The mean length of ICU stay was 3.9 days (SD 1.68). At the time
of admission, 8 (44%) met diagnostic criteria for septic shock, 7
for severe sepsis (39%), and 3 for sepsis (17%) (Table 1).
Mean total body water percentage was 84.5% on day 1,
87.6% on day 2, 87.0% on day 3, 94.9% on day 4, and 90.1%
on day 5 (Figure 1). Mean excess total body water by day is
shown in Figure 2. The normal total body water percentage is
between 72.7% and 74.3% of lean body weight. Values between
74.3% and 81% indicate slight volume excess, and values between 81% and 87% indicate moderate volume excess. Values
exceeding 87% indicate severe volume overload. Figure 3 displays peak excess fluid volume by peak percent water content
15
10
5
0
1
2
3
4
5
6
Day
Figure 1. Mean percent body water by day in the intensive care unit for 18 patients
with sepsis syndromes.
January 2016
Figure 2. Mean excess fluid volume by day in the intensive care unit for 18 patients
with sepsis syndromes.
Frequency of fluid overload and usefulness of bioimpedance in patients requiring intensive care for sepsis syndromes
13
Peak hydration (%)
100
0.00
90
0.00
80
0.00
70
0.00
0
5
10
15
2
20
25
30
ess volume (L)
Peak exce
Figure 3. Peak excess volume (L) by percent hydration in 18 patients requiring
intensive care for sepsis syndromes (normal range, 72.7%–74.3%, r = 0.70,
P = 0.001).
adverse events including mortality with the use of colloids,
particularly hydroxyethyl starch (8, 9). Therefore, isotonic
crystalloids, such as 0.9% normal saline, are often the first-line
resuscitation fluids. Importantly, each liter of normal saline
contains 9 g of sodium chloride; therefore, critically ill patients
who receive multiple liters of this crystalloid also receive a large
salt load. Additionally, this supraphysiological concentration of
chloride can induce hyperchloremic metabolic acidosis (10),
which in turn causes renal vasoconstriction, decreased glomerular filtration rate, and renal dysfunction (11, 12).
Edema is commonly observed in the critically ill ICU population, as these patients frequently develop extensive volume
overload (13). Volume will accumulate in interstitial tissues when
the rate of fluid entering the extracellular space exceeds reuptake
into the capillaries, i.e., the plasma refill rate. The plasma refill
rate is proportional to the transcapillary pressure gradient and
the permeability of the capillary membrane (14). In patients
treated for sepsis, the combination of increased capillary permeability and increased intravascular hydrostatic pressure from fluid
loading both favor the accumulation of extracellular fluid. Tissue
edema is not a benign condition, as it can result in impaired tissue oxygenation, obstruction of capillary blood flow, disruption
in metabolite clearance, and altered cell-cell interactions (15).
Excess volume disturbs the function of multiple organ systems. Volume overload adversely affects pulmonary function
resulting in impaired gas exchange, increased pulmonary restrictive defects, and reduced pulmonary compliance (16, 17). Once
hypovolemia is resolved, further volume loading has been shown
to be detrimental to renal function (18). FACTT (Fluid and
Catheter Treatment Trial) identified an increased need for renal
replacement therapies in patients randomized to a liberal versus
conservative fluid management strategy (14 vs 10%; P = 0.06)
(19). Additionally, excess volume can promote or exacerbate
congestive heart failure. A positive fluid balance has been shown
to be an independent predictor of hospital mortality (20–22).
The importance of avoiding persistent fluid overload after
the acute resuscitative phase of treatment (after hemostasis is
achieved) was emphasized by Cerda et al (23). They recommended administration of diuretics (short term and only if
effective) while avoiding nephrotoxins (such as aminoglycosides)
with early initiation of continuous renal replacement therapies
for patients who do not respond to diuretics. In the SOAP
study, early initiation of renal replacement therapy (<2 days after
14
Figure 4. Peak excess fluid volume (L) by patient for 18 patients requiring
intensive care for sepsis syndromes.
ICU admission) resulted in a lower 60-day mortality (44.8%
vs 64.6%; P < 0.01) despite greater severity of illness, which
further supports early treatment of volume excess (24).
All but one of our patients became volume overloaded, with
a mean peak excess volume of 12.2 L. The degree of volume
excess was variable, with several patients reaching a peak volume
excess of >20 L. Additionally, many of our patients (13, 72%)
were already significantly volume overloaded at the time of first
measurement, presumably from resuscitative efforts prior to or
concurrent with ICU admission.
The kidney is the primary organ responsible for regulating
salt and water homeostasis. As patients recover from critical
illness (such as sepsis), the kidneys must excrete the massive
load of salt (and concomitant water) received during volume
resuscitation. Acute kidney injury (AKI) is very common in
critically ill patients. Hoste et al reported a 67.4% incidence of
renal injury in intensive care unit admissions (25). Patients with
AKI due to sepsis suffer a higher mortality rate than patients
with AKI from other causes, and this relationship is maintained
for all degrees of AKI (by RIFLE category) (26).
In conclusion, volume overload is commonly observed in
patients requiring ICU-level care for the treatment of sepsis syndromes. Some patients develop massive volume excess (>20 L).
Volume overload manifests clinically as tissue edema and weight
gain. Edema impairs multiple physiologic processes (particularly
pulmonary, cardiovascular, and renal function). As patients recover, persistent volume overload should be avoided with the use
of targeted diuretics and renal replacement therapies if necessary.
1.
2.
3.
4.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R,
Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut
JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G,
Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL,
Vincent JL. Surviving Sepsis Campaign: international guidelines for
management of severe sepsis and septic shock: 2008. Intensive Care Med
2008;34(1):17–60.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson
E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group.
Early goal-directed therapy in the treatment of severe sepsis and septic
shock. N Engl J Med 2001;345(19):1368–1377.
Kushner RF, Schoeller DA, Fjeld CR, Danford L. Is the impedance index (ht2/R) significant in predicting total body water? Am J Clin Nutr
1992;56(5):835–839.
Uszko-Lencer NH, Bothmer F, van Pol PE, Schols AM. Measuring body
composition in chronic heart failure: a comparison of methods. Eur J
Heart Fail 2006;8(2):208–214.
Baylor University Medical Center Proceedings
Volume 29, Number 1
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
Panella C, Guglielmi FW, Mastronuzzi T, Francavilla A. Whole-body and
segmental bioelectrical parameters in chronic liver disease: effect of gender
and disease stages. Hepatology 1995;21(2):352–358.
Piccoli A, Rossi B, Pillon L, Bucciante G. A new method for monitoring
body fluid variation by bioimpedance analysis: the RXc graph. Kidney Int
1994;46(2):534–539.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein
RM, Sibbald WJ; ACCP/SCCM Consensus Conference Committee.
Definitions for sepsis and organ failure and guidelines for the use of
innovative therapies in sepsis. Chest 1992;101(6):1644–1655.
Schierhout G, Roberts I. Fluid resuscitation with colloid or crystalloid
solutions in critically ill patients: a systematic review of randomised trials.
BMJ 1998;316(7136):961–964.
McDermid RC, Raghunathan K, Romanovsky A, Shaw AD, Bagshaw
SM. Controversies in fluid therapy: type, dose and toxicity. World J Crit
Care Med 2014;3(1):24–33.
Yunos NM, Kim IB, Bellomo R, Bailey M, Ho L, Story D, Gutteridge
GA, Hart GK. The biochemical effects of restricting chloride-rich fluids
in intensive care. Crit Care Med 2011;39(11):2419–2424.
Yunos NM, Bellomo R, Story D, Kellum J. Bench-to-bedside review:
chloride in critical illness. Crit Care 2010;14(4):226–236.
Wilcox CS. Regulation of renal blood flow by plasma chloride. J Clin
Invest 1983;71(3):726–735.
Fishel RS, Are C, Barbul A. Vessel injury and capillary leak. Crit Care
Med 2003;31(8 Suppl):S502–S511.
Boyle A, Sobotka PA. Redefining the therapeutic objective in decompensated heart failure: hemoconcentration as a surrogate for plasma refill rate.
J Card Fail 2006;12(4):247–249.
Prowle JR, Echeverri JE, Ligabo EV, Ronco C, Bellomo R. Fluid balance
and acute kidney injury. Nat Rev Nephrol 2010;6(2):107–115.
Murphy CV, Schramm GE, Doherty JA, Reichley RM, Gajic O, Afessa
B, Micek ST, Kollef MH. The importance of fluid management in
acute lung injury secondary to septic shock. Chest 2009;136(1):102–
109.
January 2016
17. Arikan AA, Zappitelli M, Goldstein SL, Naipaul A, Jefferson LS, Loftis
LL. Fluid overload is associated with impaired oxygenation and morbidity
in critically ill children. Pediatr Crit Care Med 2012;13(3):253–258.
18. Van Biesen W, Yegenaga I, Vanholder R, Verbeke F, Hoste E, Colardyn
F, Lameire N. Relationship between fluid status and its management on
acute renal failure (ARF) in intensive care unit (ICU) patients with sepsis:
a prospective analysis. J Nephrol 2005;18(1):54–60.
19. National Heart, Lung, and Blood Institute Acute Respiratory Distress
Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP,
Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr,
Hite RD, Harabin AL. Comparison of two fluid-management strategies
in acute lung injury. N Engl J Med 2006;354(24):2564–2575.
20. Bagshaw SM, Bellomo R, Kellum JA. Oliguria, volume overload, and
loop diuretics. Crit Care Med 2008;36(4 Suppl):S172–S178.
21. Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini
EP, Mehta RL; Program to Improve Care in Acute Renal Disease (PICARD)
Study Group. Fluid accumulation, survival and recovery of kidney function in
critically ill patients with acute kidney injury. Kidney Int 2009;76(4):422–427.
22. Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous
CA. Negative fluid balance predicts survival in patients with septic shock:
a retrospective pilot study. Chest 2000;117(6):1749–1754.
23. Cerda J, Sheinfeld G, Ronco C. Fluid overload in critically ill patients
with acute kidney injury. Blood Purif 2010;29(4):331–338.
24. Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL; Sepsis
Occurrence in Acutely Ill Patients (SOAP) Investigators. A positive fluid
balance is associated with a worse outcome in patients with acute renal
failure. Crit Care 2008;12(3):R74.
25. Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De
Bacquer D, Kellum JA. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit
Care 2006;10(3):R73.
26. Bagshaw SM, George C, Bellomo R; ANZICS Database Management
Committee. Early acute kidney injury and sepsis: a multicentre evaluation.
Crit Care 2008;12(2):R47.
Frequency of fluid overload and usefulness of bioimpedance in patients requiring intensive care for sepsis syndromes
15
Surgical management of carotid body tumors: a 15-year
single institution experience employing an interdisciplinary
approach
Jennifer L. Dixon, MD, Marvin D. Atkins, MD, William T. Bohannon, MD, Clifford J. Buckley, MD, and Terry C. Lairmore, MD
Cervical paragangliomas are rare neoplasms that arise from extraadrenal
paraganglia in close association with the cranial nerves and extracranial
arterial system of the head and neck, and therefore surgical extirpation
can be challenging. A retrospective study was conducted of all patients
undergoing surgical excision of a cervical paraganglioma between 2000
and 2015. The demographic characteristics, clinical features, surgical
approach, and outcomes were reviewed. A total of 20 cervical paragangliomas were excised in 17 patients. There were 14 female and 3
male patients with a mean age of 56.6 ± 17.0 at the time of operation.
Twelve patients had unilateral tumors and 5 patients had bilateral tumors.
Familial involvement was confirmed by history or direct genetic analysis
in 8 (47%) of the 17 patients. There were no malignant paragangliomas,
and only 3 patients had tumors that were determined to be functional.
Tumor size ranged from 1.3 to 6.0 cm. Two patients required combined
arterial resection as part of complete excision of the tumor. There were
no permanent operative cranial nerve injuries, no recurrences, minimal
morbidity, and no mortality. In conclusion, optimal management of cervical paragangliomas should include a thorough preoperative evaluation,
accurate definition of the surgical anatomy, and exclusion of synchronous
paragangliomas. A combined therapeutic approach by a multidisciplinary
team including surgeons and interventional radiologists provides safe and
effective management of cervical paragangliomas with very low morbidity
and excellent outcomes.
C
arotid body tumors (CBTs) are rare neoplasms that arise
near the carotid bifurcation within glomus cells derived
from the embryonic neural crest. CBTs comprise approximately 65% of head and neck paragangliomas.
Most paragangliomas (75%) are sporadic, but a subset (25%)
are associated with hereditary paraganglioma syndrome. Cervical paragangliomas arise from the sympathetic ganglia in the
head and neck, and similar tumors may arise from the vagus
nerve ganglia (glomus vagale) (1–3). The majority of sporadic
tumors are asymptomatic and initially found by palpation during physical exam, or more commonly as incidental findings on
imaging studies (4, 5). Symptomatic patients present with pain,
dysphagia, or autonomic dysfunction (1, 4, 6).
Cervical paragangliomas are usually benign and biochemically silent, but functional and malignant tumors can occur
in a small subset of patients. Sporadic benign tumors typi-
16
cally present between the ages of 40 and 70 years, whereas
malignant tumors present at younger ages (20–40 years) (7).
Hereditary paragangliomas result from mutations in the genes
for succinate dehydrogenase (SDHD, SDHA, SDHC, SDHB).
Patients with hereditary paraganglioma syndrome often undergo routine surveillance and, therefore, tumors can be detected at an earlier stage. Most cervical paragangliomas are
slow growing, but left untreated they will eventually result in
a progressive enlarging cervical mass with direct involvement
and dysfunction of cranial nerves. Complete surgical removal
is the treatment of choice for these tumors whenever technically achievable. Excision of CBTs can be technically challenging owing to their proximity to the cranial nerves and the
extracranial arterial system, as well as the associated complex
anatomy in the head and neck (Figure 1). In 1971, Shamblin
introduced a classification system for these tumors based on
size and extent of local involvement (8). This study reviews
the outcomes of a standardized multidisciplinary approach to
the treatment of patients with cervical paraganglioma at our
institution, in conjunction with a review of previous publications on this topic.
METHODS
After approval by the institutional review board, all patients
undergoing treatment for cervical paraganglioma from 2000 to
2015 were identified using a search for the associated ICD-9
diagnosis and CPT procedure codes. Demographic, biochemical, radiographic, and clinicopathologic information was collected by retrospective chart review; this information included
age, gender, family history, functionality of the tumor, genetic
studies, surgical details (case duration, blood loss), preoperative angioembolization, postoperative outcomes, and operative
complications. The Shamblin classification was assigned retrospectively according to data from the operative and pathology reports (8). The results were compiled and analyzed using
descriptive statistics.
From Baylor Scott & White Healthcare and Texas A&M University Health Science
Center College of Medicine, Temple, Texas.
Corresponding author: Terry C. Lairmore, MD, Department of Surgery, Baylor
Scott & White Health, MS-01-730C, 2401 South 31st Street, Temple, TX 76508
(e-mail: tlairmore@sw.org).
Proc (Bayl Univ Med Cent) 2016;29(1):16–20
a
b
Figure 1. Exposure of carotid body tumor.
All patients underwent a complete history and physical
evaluation by the primary surgical team. A complete family
history was obtained, and (in the current era) where appropriate, formal genetic counseling and direct genetic testing
for mutations in the succinate dehydrogenase (SDH) subunit
genes was performed. Patients with a preoperative diagnosis of paraganglioma underwent biochemical screening to
evaluate for a functional tumor, including measurement of
fractionated plasma metanephrines and/or excretion of urine
catecholamines and metabolites. Although CBTs are infrequently associated with catecholamine hypersecretion, it is
our practice to perform biochemical testing for all patients
with this diagnosis. Routine screening identifies those patients
with secretory tumors and allows for preoperative alpha blockade to minimize perioperative complications from episodic
catecholamine excess. Patients with functional tumors were
begun on phenoxybenzamine 10 mg orally in divided doses 7
to 10 days preoperatively to allow for normalization of blood
pressure and volume expansion.
The preoperative evaluation, diagnostic imaging tests, and
invasive procedures for preoperative preparation were performed
with a multidisciplinary team approach by members of the interventional radiology, vascular surgery, and endocrine surgery/
surgical oncology services. Appropriate preoperative imaging
was performed to assess the size, extent, and anatomic relationships of the tumor. These studies included cross-sectional
imaging with contrast-enhanced computed tomography (CT),
magnetic resonance imaging (MRI), and/or angiography. Preoperative angioembolization was performed selectively in patients with a tumor that was large, close to critical vessels, or
was believed to benefit from reduced size/vascular supply prior
to resection (Figure 2). The selection of patients for preoperative transarterial catheter embolization was therefore based on
surgical judgment, as well as the experience and expertise of the
interventional radiologist.
After appropriate preoperative evaluation and informed
consent, patients were taken to the operating room for primary excision under general anesthesia. The surgical technique
included precise anatomic dissection and vascular control prior
to attempted tumor excision. The dissection to remove the CBT
was carried out along the arterial subadventitial plane to allow
for complete local tumor excision, as well as preservation of
critical vascular structures. In one patient the internal carotid
artery required transection. Postoperative care included close
January 2016
pharmacologic control of systolic
blood pressure and postoperative
clinical neurologic evaluation.
In patients requiring arterial reconstruction following CBT resection, we prefer an autogenous venous
conduit if an end-to-end arterial
anastomosis is not feasible. Medical therapy following end-to-end
reconstruction or venous interposition grafting is typically antiplatelet
therapy with aspirin alone for at
least a year, depending on the patient’s other comorbidities. In
the single patient who required arterial reconstruction with a
polytetrafluoroethylene graft/hybrid stent, we elected to keep
the patient on dual antiplatelet therapy indefinitely given the
limited data on such reconstructions.
Patients with a known diagnosis of hereditary paraganglioma should undergo lifelong annual biochemical and clinical
screening. Annual biochemical testing for plasma and/or urinary
catecholamines should begin at age 10 or 10 years before the
earliest age of tumor development in the family. Periodic imaging with CT/MRI or 123I-metaiodobenzylguanidine is indicated
for surveillance in patients with a known SDH mutation and in
patients with the development of symptoms or if the fractionated metanephrines and/or catecholamines become elevated.
After resection of a CBT, patients should continue to have lifelong biochemical and clinical surveillance. Although no clear
consensus has been developed regarding when, how, and how
often biochemical studies and imaging should be performed,
testing should be individualized to the patient.
RESULTS
Seventeen patients were identified with either single or bilateral cervical paragangliomas, and a total of 20 tumors were
excised. The female to male ratio was 4.7:1, with ages of 22
to 79 years (mean 56.6 ± 17.0) at the time of operation. The
follow-up period for the study patients was 1 to 126 months
(mean 56 ± 34 months). Twelve patients had unilateral tumors
and 5 patients had bilateral tumors. Some patients with bilateral involvement underwent removal of the larger tumor first,
a
b
Figure 2. Angiography of carotid body tumor.
Surgical management of carotid body tumors: a 15-year single institution experience employing an interdisciplinary approach
17
Table 1. Consecutive patients
Patient
Age
Gender
Follow-up
(months)
Arterial
resection
Size Shamblin Familial Functional
Preop
(cm)
class
history
tumor
embolized
1
62
M
126
0
2.6
II
+
+
0
Stroke
2
75
F
115
+
5.0
III
+
0
+
Cerebral salt wasting
3
77
F
106
0
2.0
I
0
0
0
0
4
63
F
85
0
2.5
II
0
0
0
0
5
40
M
62
0
2.5
II
0
0
+
0
5*
40
M
57
0
1.7
I
0
0
+
0
6
59
F
71
0
3.7
II
0
0
+
0
6*
60
F
67
0
2.7
II
0
0
+
0
7
74
F
52
0
1.3
I
0
0
0
0
8
79
F
70
0
1.3
I
0
0
0
0
9
68
F
63
0
2.8
I
0
0
+
Preoperative vocal cord paralysis
10
67
F
57
0
2.3
II
0
0
0
Temporary dysphagia
11
54
F
49
0
3.0
I
0
0
0
0
12
66
F
49
0
3.0
II
+
0
+
0
13
42
M
42
0
1.6
I
+
0
0
0
14
29
F
15
0
2.4
I
+
0
0
0
14*
29
F
11
0
1.5
I
+
0
0
0
15
22
F
11
0
3.8
II
0
+
+
Temporary dysphagia
16
73
F
5
+
6.0
III
+
0
+
Vagus sacrificed due to tumor involvement
17
52
F
1
0
3.5
I
0
+
+
0
Complication/nerve injury
*Duplicate numbers indicate bilateral resections in the same patient.
with a smaller asymptomatic contralateral lesion either followed
expectantly or with a planned staged resection depending on
individual patient and physician preference. A cervical mass was
present preoperatively in 8 (47%) patients. Familial involvement
was confirmed by history or direct genetic analysis in 8 (47%) of
the 17 patients. There were no malignant paragangliomas in this
series, and only three tumors were determined to be functional
by preoperative biochemical testing. The excised tumors ranged
from 1.3 to 6.0 cm (mean 2.76 ± 1.17 cm) in size. Most of the
tumors were Shamblin class I and II, as depicted in Table 1
(4, 5, 9–12).
Two patients had recognized preoperative vocal cord paralysis due to tumor involvement of the vagus nerve. There were
no permanent operative nerve injuries. One nonfunctioning
preoperative nerve was sacrificed at the time of tumor resection. Two patients had postoperative difficulty swallowing that
was transient and resolved by the first clinical follow-up visit.
Preoperative angiographic embolization was performed for
10 of 20 (50%) of the excised tumors. Two patients required
a combined arterial resection as part of complete excision
of the tumor. For one patient, an arterial resection was performed and a primary end-to-end anastomosis was achieved
for reconstruction. A second patient had reconstruction with
a polytetrafluoroethylene hybrid vascular graft. No patients
had tumor recurrence during the follow-up period, and there
was no perioperative mortality.
18
DISCUSSION
A complete preoperative evaluation should be performed
in patients with a known or suspected cervical paraganglioma,
including a directed family history and genetic testing when
appropriate. Hereditary paraganglioma syndromes occur in
approximately 25% of cases, and the SDH enzyme complex
gene mutation has been identified as the cause of familial types
(13–15). Patients with hereditary paraganglioma syndrome have
a greater incidence of bilateral tumors and develop tumors at
a younger age than those with sporadic tumors. Functional
tumors are detected by preoperative biochemical screening,
including measurement of plasma metanephrines and urine
catecholamines. Patients with functional tumors should be prepared preoperatively with alpha-adrenergic receptor blockade
to prevent dangerous blood pressure elevations intraoperatively.
Hormonally active cervical paragangliomas are reported to be
very infrequent (1%–3%) (16). Only three patients had functional tumors in our series, and most patients were asymptomatic, presenting with either a painless neck mass or the detection
of a cervical tumor on imaging obtained for other reasons. Six
patients in the current series had familial involvement based on
genetic testing or history.
Early excision of cervical paragangliomas is recommended to
prevent the development of larger, more locally advanced tumors
(Shamblin class III), which are associated with a higher incidence of operative nerve injury as well as poorer outcomes (17).
Baylor University Medical Center Proceedings
Volume 29, Number 1
Published nerve injury rates range
from 11% to 50% (1, 4, 5, 18, 19) and
increase with higher Shamblin class
(1, 7). Operative injuries (transient
Year
Authors (ref)
or permanent) of the vagus nerve, hy2005 Luna-Ortiz et al (5)
poglossal nerve, sympathetic chain,
2006 Antonitsis et al (9)
or marginal mandibular branch of
2008 Makeieff et al (10)
the facial nerve have been associated
2009 Grotemeyer et al (11)
with operative treatment of CBTs (5,
2010
Kruger et al (12)
18), especially in larger tumors with
close proximity to critical structures
2011 O’Neill et al (4)
requiring a more complex procedure
for removal. All but two patients in
2015 Dixon et al
our series had Shamblin class I or II
*Transient injuries.
tumors, and the incidence of transient
or permanent cranial nerve injuries in
our series is low. Patients with bilateral tumors should undergo
staged resections with surgical removal of one side at a time to
obviate the risk of synchronous bilateral cranial nerve injury
with attendant significant morbidity. Unfortunately, vascular
and especially cranial nerve injuries occur relatively frequently
in patients requiring excision of large or bilateral CBTs. The
baroreflex failure syndrome can occur after the bilateral excision of CBTs (20).
Preoperative embolization of large, vascular tumors can
facilitate surgical treatment. This typically includes embolization of the ascending pharyngeal branch of the external
carotid, allowing for up to 75% reduction in tumor blood
flow. The optimal timing is generally 1 to 2 days prior to
surgical excision (4, 21). At our institution, embolization
is performed by neurointerventional radiologists. They also
assess the internal carotid artery if there is potential need
for ligation. Prior to embolization, a pretest is performed by
means of a soft balloon in the internal carotid artery on that
side. The patient is assessed for any neurologic changes, and
the balloon is deflated if necessary. If no changes are detected,
the blood pressure is dropped to simulate mild hypotension
(systolic blood pressure 90–100) and verify that the patient
still has no symptoms. If the patient passes the test, then the
patient will tolerate internal carotid artery ligation without
reconstruction.
Most modern series of CBTs reserve preoperative embolization for Shamblin III tumors. In the present series, all Shamblin III and some of the Shamblin I and II tumors underwent
preoperative embolization. More liberal use of preoperative
embolization during CBT resection for Shamblin I and II tumors has resulted in decreased operative blood loss in individual
surgeon experience within our group. Although there is a risk
of stroke or other complications with preoperative angiography
and embolization, we did not experience that in our small series.
That risk, albeit small, has limited preoperative embolization
for Shamblin I and II tumors at other institutions.
In addition to perioperative complications of nerve injury
and bleeding, excision of CBTs is associated with a risk of perioperative stroke. Table 2 shows complication rates in many
historical series. Arterial manipulation results in a very small
January 2016
Table 2. Historical series
Patients F:M
(n)
ratio Malignant Bilateral Functional
Family
history
Nerve
injury
53
31:1
0
3 (5%)
–
0
23 (49%)
13
1.6:1
0
1 (8%)
0
–
7 (54%)
52
2.1:1
1 (2%)
3 (6%)
3 (6%)
4 (8%)
24 (42%)
36
1.8:1
0
6 (17%)
–
–
23 (64%)
39
2:1
7 (18%)
–
–
11
(28%)
13 (27%)
29
1:1
1 (3%)
6 (21%)
–
17
4.7:1
0
5 (29%)
3 (18%)
4 (14%) *8 (25%)
8 (47%)
*1 (7%)
associated stroke risk, which approaches 0% in many experienced hands but can be as high as 11% in some reports (5). In
our series, one patient had a perioperative stroke (5.9%). This
patient (patient 1) did not require carotid occlusion during the
operation. He was initially neurologically intact postoperatively
and was discharged home on postoperative day 1. However, he
returned on postoperative day 3 with complaints of weakness
and slurred speech. He was found to have an infarct of the ipsilateral brainstem on MRI. He subsequently required physical
therapy and rehabilitation for convalescence.
Paragangliomas may be initially detected during ultrasound
or Doppler ultrasound of the neck; however CT and MRI are
more sensitive for accurate tumor measurement (22). The typical
radiologic findings include a hypervascular, hypoechoic tumor
with splaying of the carotid bifurcation. 123I-metaiodobenzylguanidine scintigraphy images paraganglioma tumor tissue
based on the selective uptake of precursors for catecholamine
synthesis, but is most useful in detecting occult paragangliomas
or extraadrenal tumors in unusual anatomic sites and is therefore
infrequently utilized (16).
More widespread and frequent use of sensitive imaging
modalities enhances early tumor detection. This may explain
the decreasing rates of radical carotid artery resection and the
declining rate of nerve injury (3). Higher Shamblin class tumors are associated with greater blood loss, longer operative
times, higher incidence of nerve injury, and the need for vascular
sacrifice and reconstruction (14, 23). Complete operative excision remains the treatment of choice for CBTs when it can be
performed safely. This requires a surgical team with extensive
experience and expertise in the management of these complex
tumors. Some patients have been treated with radiation therapy
for these tumors; however, the current recommendation is for
surgical excision alone, unless significant structural involvement
prohibits safe surgical exploration (2, 18).
1.
2.
Del Guercio L, Narese D, Ferrara D, Butrico L, Padricelli A, Porcellini M.
Carotid and vagal body paragangliomas. Transl Med UniSa 2013;6(6):11–
15.
Kataria T, Bisht SS, Mitra S, Abhishek A, Ptharaju S, Chakarvarty D. Synchronous malignant vagal paraganglioma with contralateral carotid body
paraganglioma treated by radiation therapy. Rare Tumors 2010;2(2):e21.
Surgical management of carotid body tumors: a 15-year single institution experience employing an interdisciplinary approach
19
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
20
Kollert M, Minovi AA, Draf W, Bockmuhl U. Cervical paragangliomas—
tumor control and long-term functional results after surgery. Skull Base
2006;16(4):185–191.
O’Neill S, O’Donnell M, Harkin D, Loughrey M, Lee B, Blair P. A
22-year northern Irish experience of carotid body tumours. Ulster Med J
2011;80(3):133–140.
Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, GranadosGarcia M, Herrera-Gomez A. Carotid body tumors: review of a 20-year
experience. Oral Oncol 2005;41(1):56–61.
Beigi AA, Ashtari F, Salari M, Norouzi R. Convulsive syncope as presenting symptom of carotid body tumors: case series. J Res Med Sci
2013;18(2):164–166.
Obholzer RJ, Hornigold R, Connor S, Gleeson MJ. Classification
and management of cervical paragangliomas. Ann R Coll Surg Engl
2011;93(8):596–602.
Shamblin WR, Remine WH, Sheps SG, Harrison EG. Carotid body
tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am
J Surg 1971;122(6):732–739.
Antonitsis P, Saratzis N, Velissaris I, Lazaridis I, Melas N, Ginis G,
Giavroglou C, Kiskinis D. Management of cervical paragangliomas:
review of a 15-year experience. Langenbecks Arch Surg 2006;391(4):
396–402.
Makeieff M, Raingeard I, Alric P, Bonafe A, Guerrier B, Marty-Ane
Ch. Surgical management of carotid body tumors. Ann Surg Oncol
2008;15(8):2180–2186.
Grotemeyer D, Loghmanieh SM, Pourhassan S, Sagban TA, Iskandar F,
Reinecke P, Sandmann W. Dignity of carotid body tumors. Review of the
literature and clinical experiences. Chirurg 2009;80(9):854–863.
Kruger AJ, Walker PJ, Foster WJ, Jenkins JS, Boyne NS, Jenkins J. Important observations made managing carotid body tumors during a 25-year
experience. J Vasc Surg 2010;52(6):1518–1523.
Schiavi F, Dematte S, Cecchini ME, Taschin E, Bobisse S, Del Piano A,
Donner D, Barbareschi M, Manera V, Zovato S, Erlic Z, Savvoukidis T,
Barollo S, Grego F, Trabalzini F, Amista P, Grandi C, Branz F, Marroni
F, Neumann HP, Opocher G. The endemic paraganglioma syndrome
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
type I: origin, spread, and clinical expression. J Clin Endocrinol Metab
2012;97(4):E637–E641.
Burnichon N, Briere JJ, Libe R, Vescovo L, Riviere J, Tissier F, Jouanno
E, Jeunemaitre X, Benit P, Tzagoloff A, Rustin P, Bertherat J, Favier J,
Gimenez-Roqueplo AP. SDHA is a tumor suppressor gene causing paraganglioma. Hum Mol Genet 2010;19(15):3011–3020.
Niemann S, Muller U. Mutations in SDHC cause autosomal dominant
paraganglioma, type 3. Nat Genet 2000;26(3):268–270.
Offergeld C, Brase C, Yaremchuk S, Mader I, Rische HC, Glasker S,
Schmid KW, Wiech T, Preuss SF, Suarez C, Kopec T, Patocs A, Wohllk
N, Malekpour M, Boedeker CC, Neumann HP. Head and neck paragangliomas: clinical and molecular genetic classification. Clinics (Sao Paulo)
2012;67(Supp 1):19–28.
Lim JY, Kim J, Kim SH, Lee S, Lim YC, Kim JW, Choi EC. Surgical treatment of carotid body paragangliomas: outcomes and complications according to Shamblin classification. Clin Exp Otorhinolaryg
2010;3(2):91–95.
Neskey DM, Hatoum G, Modh R, Civantos F, Telischi FF, Angeli SI,
Weed D, Sargi Z. Outcomes after surgical resection of head and neck
paragangliomas: a review of 61 patients. Skull Base 2011;21(3):171–176.
Davidovic LB, Djukic VB, Vasic DM, Sindjelic RP, Duvnjak SN. Diagnosis and treatment of carotid body paraganglioma: 21 year experience
at a clinical center of Serbia. World J Surg Oncol 2005;3(1):10.
DeToma G, Nicolanti V, Plocco M, Cavallaro G, Letizia C, Piccirillo G,
Cavallaro A. Baroreflex failure syndrome after bilateral excision of carotid
body tumors: an underestimated problem. J Vasc Surg 2000;31:806–810.
White JB, Link MJ, Cloft HJ. Endovascular embolization of paragangliomas: a safe adjuvant to treatment. J Vac Interv Neurol 2008;1(2):37–41.
Dematte S, DiSarra D, Schiavi F, Casadei A, Opocher G. Role of ultrasound and color Doppler imaging in detection of carotid paragangliomas.
J Ultrasound 2012;15(3):158–163.
Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Herrera-Gomez
A. Does Shamblin’s classification predict postoperative morbidity in carotid body tumors? A proposal to modify Shamblin’s classification. Eur
Arch Otorhinolaryngol 2006;263(2):171–175.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Surgeons’ perspective of a newly initiated electronic medical
record
Richard Frazee, MD, Laura Harmon, MD, and Harry T. Papaconstantinou, MD
The American Recovery and Reinvestment Act mandates “meaningful
use” of an electronic health record (EHR) to receive current financial
incentives and to avoid future financial penalties. Surgeons’ ongoing
adoption of an EHR nationally will be influenced by the early experiences
of institutions that have made the transition from paper to electronic
records. We conducted a survey to query surgeons at our institution
regarding their perception of the EHR 3 months after institutional implementation. A total of 59 surveys were obtained from 24 senior staff
and 35 residents. Results showed that surgeons believed the EHR was
more effective as a billing tool than as a form of clinical documentation
and believed the billing was more complete and accurate with the EHR.
Surgeons also expressed concern that the EHR would negatively impact
patient satisfaction, but in spite of this, they indicated that their personal
quality of life was not negatively impacted.
T
he Health Information Technology for Economic and
Clinical Health (HITECH) Act in the American Recovery and Reinvestment Act of 2009 directed the adoption
of an electronic health record (EHR) by hospitals and
health care providers. It outlined three components that represent “meaningful use” of an EHR: 1) use of a certified EHR; 2)
electronic exchange of health information to improve quality; and
3) submission of quality and other measures (1). The reported
advantages of an EHR include reduction of errors, increased ability to communicate between providers, and facilitation of quality
improvement projects (2–4). In spite of the potential advantages
of an EHR, there has been slow adoption in the US. To encourage use of the EHR, the 2009 legislation included provisions for
incentive payments to physicians and hospitals for participation
in maintaining qualified electronic records. In 2006, 13% of
office-based physicians reported use of a basic EHR, and this
increased to 48% by 2013. Based upon application to Medicare
and Medicaid incentive programs, an estimated 69% of physicians plan to participate in a qualified EHR in 2014 (5).
Successful implementation of the EHR is strongly affected by
physician perception. In a cross-section survey of 133 specialist
physicians at three teaching hospitals, Lakbala and Dindarloo
found that more than 80% of respondents had both resistance to implementation and a positive attitude toward EHR
implementation (6). The failure to adopt the EHR is felt to
Proc (Bayl Univ Med Cent) 2016;29(1):21–23
be multifactorial (7). System expense, patient confidentiality,
and difficulty with data entry have all been cited as concerns
with electronic record use (7). Few studies have evaluated multispecialty surgical practices’ perception of the EHR. We sought
to analyze both resident and senior staff surgeons’ perceptions
3 months after adoption of an EHR.
METHODS
Prior to adoption of the EHR, our institution initiated a
6-month educational program on use of the EHR. This consisted of video modules, lectures from industry representatives,
lectures from physicians who had prior use of the EHR, and
practice sessions using mock patients. The adoption of the EHR
occurred overnight for all areas of the hospital and outpatient
clinics. Three months after adoption of the EHR, a survey of
members of the Department of Surgery, including residents and
senior staff, was performed. The survey was designed on a Likert
scale of 1 (strongly disagree) to 5 (strongly agree). Responses
were anonymous, but included demographic data including age
and level of training/years of practice. Three areas of questions
were included: 1) quality of documentation with the EHR,
2) billing questions, and 3) physician/patient satisfaction related
to the EHR.
RESULTS
The Department of Surgery at Baylor Scott & White
Temple consists of 37 senior staff in seven separate divisions
and 36 residents and fellows in general surgery, urology, ear
nose and throat, plastic surgery, and endocrine surgery. A total
of 59 survey results were received, for a response rate of 81%;
35 responses were from surgical residents (97%) and 24 were
from senior staff (65%). Three questions reflected ease and
quality of documentation. Responses indicated greater ease of
documentation but less accuracy and completeness of notes, as
well as increased difficulty with conveying the clinician’s thought
processes. Two questions addressed billing issues. Surgeons felt
the EHR was more effective as a billing tool than for clinical
documentation and believed the billing was more complete and
From the Department of Surgery, Baylor Scott & White Health, Temple, Texas.
Corresponding author: Richard Frazee, MD, Baylor Scott & White Healthcare,
2401 South 31st Street, Temple, TX 76508 (e-mail: rfrazee@sw.org).
21
Table 1. Survey results
Statement
Average
score
EHR documentation takes less time than my former documentation
3.2
EHR notes are more accurate and complete
2.6
EHR notes better convey my thoughts regarding patient care
2.5
EHR is better for billing documentation than clinical documentation
3.9
Billing is more accurate and complete since initiation of EHR
3.5
I am satisfied with our choice of EHR
3.8
My quality of life was negatively impacted by the EHR
2.8
The EHR has improved my patient satisfaction scores
2.5
accurate with the EHR. Finally, surgeons expressed concern that
the EHR would negatively impact patient satisfaction, but in
spite of this, disagreed that their personal quality of life was
negatively impacted and overall felt satisfied with the selection
of EPIC as the commercial electronic system (Table 1).
DISCUSSION
There are significant differences in the EHR experience between specialties (8). Commercial EHR systems generally have
separate “modules” for different areas of care. Many primary
care practices are office based and require only a single module,
whereas surgical practices include additional modules for hospital floor and intensive care unit inpatient care, the hospital
surgical suite, freestanding outpatient surgery centers, and the
emergency department. Our study therefore sought to analyze
surgeons’ perception of the EHR within a large multispecialty
Department of Surgery.
Survey questions addressed three specific areas. The first pertained to quality of documentation. Responses indicated greater
ease of documentation, but surgeons felt the documentation
was less complete and did not convey their thought processes
as thoroughly. Studies in the literature have indicated improved
documentation through use of the EHR with regard to inclusion of key elements of the history and physical (9). One
study showed improved documentation, clinical processes, and
revenue capture with the EHR (10). Perception of quality of
documentation could be specialty specific. Specialties that see a
high volume of finite diagnoses can benefit from the templates
offered in the EHR. Many surgical specialties see a more disparate cross-section of patients who require more individualized
documentation, and templates do not always convey the clinical
decision-making process.
Our surgeons felt that compliance with billing requirements
and the capture of charges were improved with EHR use. The
EHR can be set up to incorporate all of the key elements of documentation for billing purposes. Many of the key elements can
be autopopulated and reviewed by the physician for accuracy.
There is also a link to electronic charge entry with Centers for
Medicare and Medicaid Services term-specific diagnoses. Weiss
described a 37% decrease in insurance denials with improved
22
documentation from an electronic system (11). All of these
features can contribute to more effective billing and collections.
The final area we investigated was perception of physician user
and patient satisfaction with EHR use. While our surgeons were
satisfied with the choice of EHR and did not feel that it negatively
impacted them personally, they indicated concern regarding the effect on patient satisfaction. In a cross-sectional retrospective analysis
of hospitals under the Medicare Hospital Value-Based Purchasing
Program, use of “advanced” EHRs did not detrimentally impact
the patient experience (12). A separate multistudy review showed
a positive or neutral assessment of patient experience with EHR
use (13). Certain aspects of the EHR can enhance patients’ experience, including access to their health records via a patient portal
and easy-to-read and language-specific patient instructions that are
available for physicians to use in patient education.
In spite of the advantages of an EHR and electronic order
entry (14, 15) and a focused effort from federal agencies to
encourage EHR use, there has been reluctance to adopt EHR
systems in the United States. With the initiation of new programs and the lack of widespread experience, perception can
drive behavior as much as reality. Holden stated, “Behavioral
theory asserts that decisions to accept and use technology are
based on internal psychological variables, i.e., beliefs” (16). He
analyzed physicians’ perceptions about the electronic record
system to determine potential barriers to EHR implementation
and found that beliefs could be grouped into broad categories
including “performance outcome effects,” “entities that approve
or encourage use,” and “facilitators or barriers.” He concluded
that the details of these behavior-shaping beliefs could provide
guidance to both practitioners and researchers.
Other studies have outlined the importance of differentiating
between true system problems and resistance behaviors. The true
system problems require cooperation between users and implementers to address inefficiencies in the system. These interactions
are productive and increase utilization. Resistance behaviors, on
the other hand, are counterproductive and lead to diminished
productivity (17). Chen found several factors that were significant in physician acceptance of the EHR. These included top
management support, project team competency, system quality,
and physicians’ perceptions of the usefulness and ease of use (18).
In conclusion, surgeons’ early perception of the EHR is that it
is more effective in providing billing documentation than clinical
documentation. There is concern regarding the impact of the EHR
on patient satisfaction. In spite of these drawbacks, the surgeons
were satisfied with the choice of EHR. Although we believe our
study captured surgeons’ perspective of EHR, there were limitations. Future investigation into the subject could include a more
detailed breakdown of the participants. Our study detailed the
reactions of senior staff and residents, but we did not review changes
of opinion between divisions or levels of seniority. This information
would be helpful in further understanding surgeons’ perspective, as
opinions may change with the level of training or specialty.
Acknowledgments
The authors would like to thank Gina Du Par for her
editorial support.
Baylor University Medical Center Proceedings
Volume 29, Number 1
9.
1.
2.
3.
4.
5.
6.
7.
8.
Goveia J, Van Stiphout F, Cheung Z, Kamta B, Keijsers C, Valk G, Ter
Braak E. Educational interventions to improve the meaningful use of
electronic health records: a review of the literature: BEME Guide No.
29. Med Teach 2013;35(11):e1551–e1560.
Yoo SK, Kim DK, Kim JC, Park YJ, Chang BC. Implementation of a
large-scale hospital information infrastructure for multi-unit health-care
services. J Telemed Telecare 2008;14(3):164–166.
Wang SJ, Middleton B, Prosser LA, Bardon CG, Spurr CD, Carchidi PH,
Kittler AF, Goldszer RC, Fairchild DG, Sussman AJ, Kuperman GJ, Bates
DW. A cost-benefit analysis of electronic medical records in primary care.
Am J Med 2003;114(5):397–403.
Miller RH, Sim I. Physicians’ use of electronic medical records: barriers
and solutions. Health Aff (Millwood) 2004;23(2):116–126.
Hsiao CJ, Hing E. Use and Characteristics of Electronic Health Record
Systems among Office-Based Physician Practices: United States, 2001–2012
[NCHS Data Brief No. 111]. Hyattsville, MD: National Center for
Health Statistics, 2012.
Lakbala P, Dindarloo K. Physicians’ perception and attitude toward
electronic medical record. Springerplus 2014;3:63.
Loomis GA, Ries JS, Saywell RM Jr, Thakker NR. If electronic medical
records are so great, why aren’t family physicians using them? J Fam Pract
2002;51(7):636–641.
O’Connell RT, Cho C, Shah N, Brown K, Shiffman RN. Take note(s):
differential EHR satisfaction with two implementations under one roof.
J Am Med Inform Assoc 2004;11(1):43–49.
10.
11.
12.
13.
14.
15.
16.
17.
18.
Saleem JJ, Adams S, Frankel RM, Doebbeling BN, Patterson ES. Efficiency strategies for facilitating computerized clinical documentation
in ambulatory care. Stud Health Technol Inform 2013;192:13–17.
Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the
electronic health record on an academic pediatric primary care center.
J Ambul Care Manage 2009;32(3):180–187.
Weiss AM, Jain A. Using computerized physician order entry to decrease
insurance denials. AMIA Annu Symp Proc 2005:1152.
Jarvis B, Johnson T, Butler P, O’Shaughnessy K, Fullam F, Tran L, Gupta R.
Assessing the impact of electronic health records as an enabler of hospital
quality and patient satisfaction. Acad Med 2013;88(10):1471–1477.
Irani JS, Middleton JL, Marfatia R, Omana ET, D’Amico F. The use of
electronic health records in the exam room and patient satisfaction: a
systematic review. J Am Board Fam Med 2009;22(5):553–562.
Blumenthal D, Glaser JP. Information technology comes to medicine.
N Engl J Med 2007;356(24):2527–2534.
Glaser J, Foley T. The future of healthcare IT: what can we expect to see?
Healthc Financ Manage 2008;62(11):82–88.
Holden RJ. Physician’s beliefs about using EMR and CPOE: in pursuit
of a contextualized understanding of health IT use behavior. Int J Med
Inform 2010;79(2):71–80.
Lapointe L, Rivard S. Getting physicians to accept new information
technology: insights from case studies. CMAJ 2006;174(11):1573–1578.
Chen RF, Hsiao JL. An investigation on physicians’ acceptance of hospital
information systems: a case study. Int J Med Inform 2012;81(12):810–
820.
Invited Commentary
D
rs. Frazee and Papaconstantinou have well documented
the perspective of surgical specialists in a tertiary academic health center regarding electronic health record
(EHR) use. In the data presented regarding those opinions, the physicians reflect back two facts: 1) EHRs are a good
vehicle for properly documenting care to achieve proper billing
(a fact that is a direct corollary of the growth and development
of the EHR industry as a whole), and 2) EHRs are at best just
above neutral in terms of physicians’ workflow.
The article chronicles the evolution of EHRs nicely, including barriers and incentives for EHR adoption. Other surveys (1)
have indicated acceptance in general positive directions, with
Morton et al concluding that “the overall attitude about EHR
use was computed to be 3.74 on the five-point scale.” Similar
scores have been reported in the HealthTexas Provider network.
In spite of continuing evolution of EHRs, problems remain.
Physicians often push back at the 20% to 30% of their time
with patients being devoted to entering data. Many have not
mastered typing. Slow-typing physicians complain of significant
after-hours effort just to keep up with their required documentation. Some have difficulty simultaneously entering data
and maintaining eye contact with attentive interaction with the
patients. Most EHR systems were designed by technology pro-
January 2016
fessionals and do not support the workflow of physicians. In the
“best” EHRs (ranking changes every year in KLAS surveys [2]),
it seems that all EHRs today are still in Generation 1, having not
ideally solved the data entry interface or created ideal support
of physician workflow. Who will invent a Generation 2 EHR?
In an idealized world, documentation of the patient encounter might become a passive byproduct of the encounter. Physicians could focus entirely on patient interaction, the history,
the physical examination, and diagnostic and treatment plans.
Data would be immediately retrievable both to physicians and
patients. And the essential documentation and coding to justify
accurate billing would be automated. An enjoyable futuristic
view of such an encounter is portrayed in an online video available at http://youtu.be/VHMJaV7zJxE.
—Carl Couch, MD
Vice President, Baylor Scott & White Innovation Center
E-mail: carlc@baylorhealth.edu
1.
2.
Morton ME, Wiedenbeck S. EHR acceptance factors in ambulatory care:
a survey of physician perceptions. Perspect Health Inf Manag 2010 Jan
1;7:1c.
Klas Enterprises. KLAS announces top-performing vendors in 2015 midterm
performance review: software & services report [Press release]. Retrieved from
http://www.klasresearch.com/midterm-performance-report-pr
Surgeons’ perspective of a newly initiated electronic medical record
23
Abstracts from the 10th annual Baylor Scott & White
Department of Surgery Research Day
Harry T. Papaconstantinou, MD, James Fleshman, MD, J. Scott Thomas, MD, Marcin Czerwinski, MD, and M. Karen
Newell-Rogers, PhD, editors
T
his year marks the 10th anniversary of the Department
of Surgery Research Day. We want to begin by expressing
gratitude to all who made this Research Day a success.
This included a dedicated staff, including Dee Ann Gillam, Lynn Botts, and Kathleen McKee, the organizers of the
2015 Research Day, the founders and visionaries that established
and maintained the tradition of having a yearly Department of
Surgery Research Day, and the young physicians and physicianscientists whose scholarly activity and efforts were shared at our
May 1, 2015, event. This year also marked our second year in
existence as Baylor Scott & White Healthcare, and as such, we
celebrate the collaborative effort of the Departments of Surgery
at Scott & White Memorial Hospital and Baylor University
Medical Center to make this a systemwide integrated event.
Research Day started as a grassroots initiative to showcase
the efforts of medical students, residents, and fellows in the areas
of basic, translational, and clinical research. Each year for the
last 10 years, surgical trainees within the Department of Surgery
have worked to integrate the clinical problems they encounter
into research projects aimed at offering new insights and knowledge with the potential of advancing medical knowledge and
improving patient outcomes.
The robust participation and quality of research presented at
the Baylor Scott & White Department of Surgery Research Day
highlight the importance of research to the residents, faculty,
department, institution, and system. Many of the studies and
presentations have been submitted and accepted for presentation at regional, national, and international specialty meetings.
It is this level of participation that increases the awareness of
quality education, research, and clinical/surgical care provided
in our organizations. Many of these presentations will be submitted as manuscripts to peer-reviewed journals, such as Baylor
Proceedings, and upon successful publication will be the basis for
future patient care and the foundation for future research. This
concept is powerful, as our surgical trainees and departments
of surgery are shaping the standard of surgical patient care and
developing innovative techniques to improve quality of care
and patient outcomes.
This year we had the opportunity to host two keynote
speakers. Dr. Paul Kuo, chairman of surgery and director of
the Oncology Research Institute at Loyola University Medical
24
Center, gave a talk entitled “Not knowing is part of the fun.”
Dr. Lisa Poritz, an associate professor in the Department of Surgery and Section of Colon and Rectal Surgery from Pennsylvania
State University Medical School, spoke about “Alteration of the
tight junction complex in intestinal inflammation.” Presentations from these highly regarded surgeon scientists demonstrate
how a lifetime of dedicated inquiry and research can lead to a
productive and successful academic career. We are appreciative
of their willingness to participate and be a critical participant
in this important day.
Together with Dr. Carl Tong, director of the Baylor Scott
& White Heart Transplant Team, our invited guest speakers
not only presented their inspiring work, but also reviewed the
presentations and acted as judges for the awardees of the event.
After strict review and careful deliberation, the judges distributed awards to the following recipients:
• Trung Ho (Baylor Scott & White Central), Best Presentation, “The incidence of ocular injuries in isolated orbital
fractures”
• Anson Nguyen (Baylor Scott & White Central), Best Poster,
“Safety of outpatient orbital fracture repair”
• Philip Edmundson (Baylor Scott & White North), Second
Place (tie), “Sarcopenia as a marker of frailty: PSOAS muscle
size predicts functional outcome in mild to moderately injured
trauma patients”
• Mark Draoua (Baylor Scott & White North), Second
Place (tie), “Signifi cance of measured intraoperative
portal vein flows after thrombendvenectomy in deceased donor liver transplant recipients with portal vein
thrombosis”
Collectively, we are proud of our residents, faculty, and this
important event. We look forward to continuing this tradition
and expanding participation among surgical trainees within the
Baylor Scott & White Healthcare System.
From the Department of Surgery, Baylor Scott & White Health, Temple, Texas
(Papaconstantinou, Thomas, Czerwinski, Newell-Rogers) and the Department of
Surgery, Baylor University Medical Center at Dallas (Fleshman).
Corresponding author: Harry T. Papaconstantinou, MD, Department of
Surgery, Baylor Scott & White Health, 2401 South 31st Street, Temple, TX
76508 (e-mail: hpapaconstantinou@sw.org).
Proc (Bayl Univ Med Cent) 2016;29(1):24–29
The incidence of ocular injuries in isolated orbital fractures
Trung Ho,* Jonathan Tsai, and Marcin Czerwinski (e-mail: tho@sw.org)
Orbital fractures are common and have the potential for an associated ocular globe injury. Prompt identification of significant
ocular injuries is important to prevent any potential long-term
visual sequelae; however, their true incidence in this patient
population has not been determined due to the suboptimal
design of previously conducted studies. As a consequence, most
surgeons choose to have all such patients formally evaluated
by an ophthalmologist. The objective of this study was to conclusively identify the incidence of significant ocular injuries in
patients with isolated orbital fractures and to determine their
predictors in order to guide more efficient patient care. A prospective cohort study, powered to detect a 15% incidence of
ocular injuries, was designed. All patients presenting to our
regional Level I trauma center with computed tomography findings of an isolated orbital fracture were included and followed a
strict evaluation protocol. Plastic surgery examination included
visual acuity, pupillary reactivity, ocular range of motion, and
presence of visible injuries. Ophthalmology evaluation also included intraocular pressure and formal anterior chamber and
posterior chamber exams. Significant ocular injury was defined
as that requiring ophthalmologic intervention in an attempt
to preserve or restore vision. Patients were followed for a minimum of 1 week to identify any delayed injuries. Eighty patients
were enrolled from 2012 to 2014. There were 46 males and 34
females with a mean age of 42.8 years. Assault was the most
common mechanism of injury. There were eight ocular injuries (10%): ruptured globe (1), uveal prolapse (1), retrobulbar
hemorrhage (2), hyphema (3), and scleral tear (1). Four of the
injuries were considered significant. Predictors for significant
ocular injuries were grossly abnormal visual acuity and obvious
lack of pupillary reactivity of the affected eye. The incidence of
significant ocular injuries in isolated orbital fractures is much
lower than previously reported. Therefore, not all patients with
isolated orbital fractures require formal ophthalmologic evaluation. However, patients presenting with grossly abnormal visual
acuity or abnormal pupillary reactivity are at high risk and likely
require urgent ocular intervention.
Significance of measured intraoperative portal vein flows
after thrombendvenectomy in deceased donor liver transplant
recipients with portal vein thrombosis
Mark Draoua,* Nicole Titze, Amara Gupta, Hoylan Fernandez, Giovanna Saracino,
Michael Ramsay, Giuliano Testa, Goran Klintmalm, and Peter Kim (e-mail: mark.
draoua@baylorhealth.edu)
Adequate portal vein (PV) flow, an important factor in liver
transplantation, may still be compromised after thrombendvenectomy in patients with portal vein thrombosis (PVT). This
study evaluated the impact on patient outcomes of measured intraoperative PV flow after PV thrombendvenectomy during deceased donor liver transplantation (DDLT). Eighty patients who
underwent PV thrombendvenectomy during DDLT with available flow data over a 16-year period were included in the study.
Patients were classified into two groups: high PV flow (>1300
mL/min, n = 57) and low PV flow (<1300 mL/min, n = 23).
January 2016
From a prospectively maintained database, postoperative complications and graft survival were analyzed. Both groups had
similar demographics. High PV flow was associated with lower
rates of biliary strictures (9% vs 38%, P = 0.005) and higher
1-, 2-, and 5-year graft survival rates (88%, 84%, and 69% vs
61%, 57% and 42%; P = 0.002). The difference in the incidence of postoperative PVT was not significant (2% vs 9%, P =
0.20). No biliary leaks or hepatic artery thromboses were reported in either group. By multivariate analyses, age >60 years
(hazard ratio [HR] 3.03 [1.08–8.54], P = 0.04), male sex (HR
4.4 [1.45–13.3], P = 0.009), and PV flow <1300 mL (HR
12.9 [2.26–74], P = 0.004) were associated with worse survival.
PV flow >1300 mL/min after PV thrombendvenectomy for
PVT during DDLT was associated with lower rates of biliary
strictures and better long-term survival. Consideration should
be given to identifying reasons for low flow and maneuvers
to increase PV flow when PV is <1300 mL/min during liver
transplantation.
Congestive heart failure is associated with increased risk of
pneumonia, reintubation, and death following laparoscopic
cholecystectomy: a National Surgical Quality Improvement
Program database review
Chad Hall,* Justin Regner, and Daniel Jupiter (e-mail: cmhall@sw.org)
Laparoscopic cholecystectomy (LC) is the gold standard operation for gallbladder disease in patients of all ages with a variety
of medical conditions. Elective LC has been performed as an
outpatient operation for nearly 15 years. Few studies have examined the impact of specific comorbidities on outcomes after
LC and determined if certain comorbidities may benefit from
postoperative admission. Congestive heart failure (CHF) is a
common comorbidity that necessitates appropriate perioperative management. This study aimed to quantify adverse events
after LC and determine if patients with CHF should be admitted following LC. A retrospective review was conducted of all
adult cases of laparoscopic cholecystectomy recorded in the National Surgical Quality Improvement Program database between
2005 and 2012. Exclusion criteria were pregnancy, disseminated
cancer, recent chemotherapy or radiation, and liver disease.
Included patients were categorized into elective and emergent
populations. Bivariate and multivariate analyses determined the
impact of CHF on postoperative complications. Laparoscopic
cholecystectomies were performed electively in 131,081 patients
and emergently in 12,680 patients. CHF was more common in
older patients and accounted for 0.38% of elective and 0.62%
of emergent operations. Pneumonia, reintubation, and death
occurred in 9% of elective and 17% of emergent operations in
CHF patients. Bivariate analysis revealed a relative risk for pulmonary complications of 16.6 in the elective and 12.98 in the
emergent populations. The multivariate analysis demonstrated
that patients with CHF were nearly four times more likely to
suffer from these outcomes. Other comorbidities contributing
to respiratory complications included age, body mass index,
chronic obstructive pulmonary disease, and dyspnea. Thus, LC
is a safe operation, but patient comorbidities affect surgical
outcomes. Patients with CHF need appropriate preoperative
Abstracts from the 10th annual Baylor Scott & White Department of Surgery Research Day
25
counseling and management to improve outcomes after LC
and may benefit from postoperative admission following LC
for prevention of pulmonary complications.
Mild traumatic brain injury increases risk for the development
of posttraumatic stress disorder
Rebecca Weddle,* Ann Marie Warren, Michael Foreman, Evan Rainey, Stephanie
Agtarap, and Grace Viere (e-mail: Rebecca.Weddle@baylorhealth.edu)
Debate remains regarding whether posttraumatic stress disorder
(PTSD) requires conscious exposure to a trauma, the extent to
which PTSD and traumatic brain injury (TBI) etiology are related, and the causal relationship between mild TBI (mTBI) and
PTSD. This prospective cohort study included patients ≥18 years
admitted to a level I trauma center for ≥24 hours. Demographic
and injury-related data were gathered from the trauma registry.
PTSD assessments were administered during hospitalization and
3 and 6 months afterwards. Positive PTSD was determined using
the Primary Care PTSD Screen with a cutoff ≥3 and a score ≥50
on the PTSD Checklist–Civilian Version. mTBI was determined
through ICD-9 coding. This analysis included 494 patients at
baseline, 311 at 3 months, and 231 at 6 months. Preinjury PTSD
was reported by 7% of participants. Chi-square analysis was performed. At 3 months, patients with mTBI evidenced a probable
PTSD rate of 18%, compared with 9% for patients with no
mTBI (P < 0.05). At 6 months, patients with mTBI evidenced
a probable PTSD rate of 26%, compared with 15% for patients
with no mTBI (P < 0.05). Preinjury TBI did not predict PTSD,
but incidence of TBI at the time of injury did predict PTSD. TBI
at the time of injury predicted higher rates of PTSD at both 3
and 6 months postinjury, suggesting that sustaining a TBI at the
time of injury places one at risk for later PTSD. This important
finding may help clinicians identify patients at high risk for PTSD
after injury and target these patients for screening, intervention,
and referral for treatment.
Pharmacological modulation of PTEN ameliorates the
progression of pulmonary hypertension in heart failure
Yazhini Ravi,* Karuppaiyah Selvendiran, Shan K. Naidu, Sarath Medura, Lucas
Citro, Mahmood Khan, Brian K. Rivera, Periannan Kuppusamy, and Chittoor B.
Sai-Sudhakar (e-mail: yravi@sw.org)
Pulmonary hypertension (PH) that occurs secondary to congestive heart failure leads to vascular remodeling, including
neointima formation and vascular occlusion. Currently there
is a significant gap in the understanding of the mechanisms
involved in vascular remodeling, which, if identified, could provide key therapeutic targets. Phosphatase and tensin homolog
on chromosome 10 (PTEN) has been implicated in arterial
remodeling. However, the involvement of PTEN in PH-mediated vascular remodeling remains unclear. The objective of the
present study was to determine the role of PTEN in PH and
to develop a therapeutic strategy. PH was induced in rats by
ligating the left anterior descending coronary artery. The onset
of PH was monitored by echocardiography and confirmed by
hemodynamic measurements. Rats were continuously treated
with 100 ppm HO-3867, a promoter of PTEN expression, in
the feed for 4 weeks. Control groups did not receive HO-3867.
26
The vascular smooth muscle cells in the lung were collected
using laser capture microdissection. The cells and whole lung
tissues were analyzed by Western blot, reverse transcription polymerase chain reaction, and quantitative reverse transcription
polymerase chain reaction. The HO-3867 treatment group had
a significantly higher ejection fraction compared with the control. Pulmonary arterial and right ventricular systolic pressure
data showed the development of PH at 4 weeks after ligation
of the left anterior descending artery. Phosphorylated PTEN
(Ser380/Thr382/383) was markedly depressed in the PH lungs
(43.8% compared to non-PH). Rats treated with HO-3867
showed a significant recovery of PTEN (57.61%). Focal adhesion kinase expression was higher in the PH group than in the
HO-3867–treated group. Similar results were obtained at the
mRNA levels of the key proteins in the vascular smooth muscle
cells collected from the lung. In conclusion, deregulation of
PTEN is involved in PH-mediated vascular remodeling. The
vascular remodeling can be inhibited by targeting the PTEN
pathway using PTEN-promoting agents such as HO-3867.
Variables associated with weaning from mechanical
ventilation in patients admitted to a long-term acute
care hospital
Frans van Wagenberg,* Jennifer Dixon, Michael Martinez, Ying Fang-Hollingsworth,
Cecilia Benz, Alejandro Arroliga, Shekhar Ghamande, and David Ciceri (e-mail:
fvanwagenberg@sw.org)
Historically, 33% to 50% of patients requiring long-term ventilation are eventually liberated from invasive mechanical ventilation (MV). Prognostication is crucial in this population. We
retrospectively examined data on 184 consecutive patients on
MV admitted to our long-term acute care hospital for ventilator
management from 2011 to 2012 to determine variables associated with failure to wean from MV. A standardized protocol for
ventilator weaning, nutrition, and mobilization was used for all
patients. Successful weaning from the ventilator was defined
as being free from any MV assistance for 5 days. Two-sample
t tests and Wilcoxon two-sample tests were used to compare
continuous variables. A chi-square test or Fisher’s exact test was
used for categorical variables. Overall, 75.4% of patients were
liberated from MV. The mortality in this group was 14.7% (27
of 184). Variables associated with failure to wean were older age
(67.8 [±14.6] vs 61.9 [±16.0] years; P = 0.01), a primary medical diagnosis (57.2% vs 42.8%; P = 0.02), a history of chronic
obstructive pulmonary disease (51.1% vs 25.4%; P = 0.001),
acute renal failure (>stage II) (55.6% vs 26.8%; P = 0.004), and
myocardial infarction during hospitalization (20% vs 8.7%; P =
0.039). Among weaned patients, 18.8% were discharged home,
39.9% to a skilled nursing facility, 29.7% to an inpatient rehabilitation facility, 3.6% to hospice, and 2.2% to the intensive
care unit. Failure to wean imparted a 14-fold increased mortality
at 1 month (odds ratio, 14.23 [6.39–31.71]; P < 0.001). We
report a higher weaning rate than in prior studies. Increased
age, chronic obstructive pulmonary disease, renal failure, and
myocardial infarction impact liberation from MV. Incorporating these variables can facilitate meaningful family discussions
regarding weaning expectations.
Baylor University Medical Center Proceedings
Volume 29, Number 1
The benefits to pediatric trauma patients offered by freestanding pediatric hospitals with trauma centers
Laura Harmon,* Matthew Davis, and Justin Regner (e-mail: laharmon@sw.org)
Differences in the care of pediatric trauma patients at combined
adult and pediatric trauma centers versus stand-alone pediatric
trauma centers remains unclear with regard to complications
and outcomes. While pediatric trauma centers are becoming
more common, only 36% of states have designated pediatric
trauma centers, and <24% are level I status. The goal of this
study was to compare the treatment of pediatric trauma patients at a tertiary level I trauma center before and after the
institution of a freestanding pediatric trauma center with level
2 status. Local data from the National Trauma Data Bank were
retrospectively reviewed. Descriptive statistics were calculated
for all variables of interest. A total of 2823 patients were evaluated between 2008 and 2014, with 1630 at the level I center
and 1193 patients at the level 2 center. Median Injury Severity
Score was higher at the adult trauma center hospital, with a
median score of 9 vs 4 (P = 0.002). Eighty-nine percent of
patients evaluated had a Glasgow Coma Scale score of 15, with
no significant difference noted between the two institutions.
The length of emergency room stay was significantly shorter at
the pediatric hospital (P = 0.002); however, total length of stay
was longer at the pediatric hospital (P = 0.01). The pediatric
trauma center volume was made up of more transfers (72% vs
60%; P = 0.002). Complication rates were similar between the
two institutions: 2.02% at the adult trauma center vs 3.64% at
the pediatric trauma center (P = 0.05). In summary, pediatric
trauma patients presenting to a freestanding pediatric trauma
center had a shorter length of stay in the emergency room and
a lower average Injury Severity Score, but a longer overall length
of stay. Complication rates were similar between the adult and
pediatric trauma centers. Based on our data, pediatric trauma
centers may have some advantage in terms of process, but outcomes do not appear to be different.
Urban blunt carotid and vertebral artery injury: a 12-year
comparison
Mark Lytle,* James West, Jason Burkes, Tammy Fisher, Yahya Doaud, and William
Shutze (e-mail: mark.lytle@baylorhealth.edu)
Blunt cerebrovascular injury (BCVI) is more common than
we used to think and carries a substantial stroke and mortality
risk. The purpose of our study was to review our experience
with extracranial BCVI and evaluate a modified injury grading scale relating stroke and death to blunt carotid artery (CA)
and vertebral artery (VA) injury. We retrospectively reviewed
the records of patients who were treated for BCVI over the
12-year span from January 2003 to July 2014. Demographic,
injury-related, imaging, and outcomes data were obtained
and analyzed. A new BCVI grading scale, with a luminal
narrowing grade, was utilized to grade both blunt CA and
VA injuries, and stroke and mortality outcomes were evaluated. A total of 103 patients, with BCVI in 114 vessels, were
identified and treated at a single, urban level I trauma center
from January 2003 to July 2014. The average Injury Severity
Score (ISS) was 22 (range, 4–75). Cervical spine fractures
January 2016
occurred in 64 patients (80% of VA injuries). CA injuries
were associated with more traumatic brain injury (TBI) (61%
vs 46%) and stroke (24% vs 3%) and a higher ISS (27 vs
18) compared with the VA group. The mortality rates in the
CA and VA groups were 30% and 3%, respectively. Stroke
occurred more frequently in injuries with >70% stenosis or
occlusion (75%). Mortality also occurred more frequently in
injuries with >50% stenosis or occlusion (71%). For BCVI,
the ISS, incidence of TBI, incidence of stroke, and mortality were higher for CA than VA injuries. Cervical fractures
were much more common with VA injuries. Stroke occurred
only in injuries with >70% luminal stenosis/occlusion or
with persistent sciatic artery, and mortality occurred 6 times
more frequently in injuries with >50% luminal stenosis/occlusion or with PSA. Due to this, the new Dallas modified
BCVI grading scale gives better prognostic outcomes than
the original grading scale.
S100β induces blood-brain barrier endothelial cell hyperpermeability via caspase-3–mediated disruption of the tight
junctions
Chen Chen,* Himakarnika Alluri, Anasooya Shaji, Katie Wiggins-Dohlvik, Matthew
Davis, and Binu Tharakan (e-mail: chchen@sw.org)
Traumatic brain injury (TBI) is a leading cause of death and
disability in the younger population. Microvascular permeability that occurs due to breakdown of the blood-brain barrier
(BBB) is one of the major contributors of the vasogenic brain
edema and elevated intracranial pressure that occur following
TBI. The BBB consists of endothelial cells linked together by
tight junction proteins that are intracellularly linked to the
actin cytoskeleton of the cell mainly by zonula occludens-I
(ZO-I). S100β, a glial-specific protein expressed by astrocytes,
is released during TBI and is a biomarker for it. However, it has
not been determined whether the protein contributes to BBB
breakdown. Our objective was to determine if S100β causes
BBB breakdown and hyperpermeability and to determine if it
occurs through tight junction protein disruption via caspase-3.
TBI was induced in mice with a controlled cortical impactor, and serum S100β was measured using an antibody array
technique. Rat brain microvascular endothelial cell (RBMEC)
monolayers were exposed to S100β in the presence or absence
of the caspase-3 inhibitor Z-DEVD-fmk. Monolayer permeability was measured fluorometrically. Changes in tight junction integrity and cytoskeletal assembly were studied using
ZO-1 immunofluorescence and rhodamine phalloidin staining
for F-actin, respectively. Serum S100β levels were increased
following TBI injury in animals. Treatment of S100β caused
a significant increase in RBMEC monolayer permeability at
1 ug/mL and 10 ug/mL concentrations (P < 0.05), while ZDEVD-fmk (10 uM; 1 hour) pretreatment attenuated S100β
(1 ug/mL; 4 hours)–induced hyperpermeability significantly
(P < 0.05). Z-DEVD-fmk prevented S100β-induced disruption of the tight junctions and resulted in cytoskeletal
reorganization. S100β-induced BBB endothelial cell hyperpermeability may be mediated via caspase-3 disruption of tight
junction proteins.
Abstracts from the 10th annual Baylor Scott & White Department of Surgery Research Day
27
What risk factors within the first 24 hours of admission are
associated with mortality after traumatic injury?
Stephanie Joyce,* Geoffrey Funk, Stephanie Agrarap, Megan Reynolds, and
Michael Foreman (e-mail: Stephanie.joyce@baylorhealth.edu)
The Trauma Quality Improvement Program (TQIP) was
created to provide risk-adjusted benchmarking in trauma
centers. Currently, 9 variables in TQIP are used in risk adjustment. There are risk factors not yet validated by TQIP that are
direct contributors to mortality. Looking specifically at variables
within the first 24 hours of admission, we hoped to identify
novel contributors predictive of overall mortality within trauma
patients at our institution. A retrospective review of concurrently collected trauma registry data included all trauma patients
admitted to the institution in the year 2013. Multiple variables
were reviewed, including diagnostic and procedural processes
during the first 24 hours following hospital arrival (i.e., age,
Injury Severity Score [ISS], motor component of the Glasgow
Coma Scale [GCS], initial systolic blood pressure and pulse rate,
mechanism of injury, head injury severity, abdominal injury severity, and patient transfer status). Additional variables included
time of arrival, operative vs minimally invasive interventions,
volume of crystalloid and/or blood transfused, acidosis/base
deficit, race, as well as scene time and vitals. For continuous variables (e.g., age and ISS), independent t tests were run; for categorical variables (e.g., sex, race, and trauma type), chi-squared
tests were used to determine initial differences between those
who survived and died. There were significant differences in
initial pulse, systolic and diastolic blood pressure, GCS, and
ISS (all P < 0.001). Additionally, there were significant differences for race (P = 0.003), sex (P = 0.01), hospital transfer (P =
0.002), and disposition from the emergency department, cause
of injury, trauma type, comorbidities, and use of paralytics in
the emergency department (all P < 0.001). These initial findings identify distinctive differences among variables of patients
who survived traumatic injury and those who did not. This
suggests that multiple factors within the first 24 hours, beyond
the standard risk factors, are predictive of eventual mortality.
Melatonin inhibits hemorrhagic shock-induced microvascular
endothelial cell derangements
Katie Wiggins-Dohlvik,* Himakarnika Alluir, Chinchusha Anasooya Shaji, Vivayak
Govande, Madhava Beeram, Amin Mohammad, Matthew Davis, and Binu
Tharakan (e-mail: kwigginsdohlvik@sw.org)
Hemorrhagic shock (HS) induces global ischemia and reperfusion injuries, resulting in vascular hyperpermeability. The mechanisms that regulate this process are unclear. We hypothesized
that matrix metalloproteinase-9 (MMP-9) is pivotal therein
and that such damage can be attenuated with melatonin. Rats
were divided into sham, HS, and HS plus melatonin groups
(shock for 1 hour, n = 5). Laparotomy was performed and
mesenteric postcapillary venules were examined with intravital
microscopy. Fluorescent intensities were measured intravascularly and extravascularly to assess vessel permeability, vital
signs and fluid requirements were recorded, and serum and
tissue were collected. MMP activity was assayed in lung tissue homogenates (n = 8). In parallel, rat lung microvascular
28
endothelial cells (RLMEC) were grown and divided into the
following groups: sham serum, HS serum, sham serum plus
melatonin, and HS serum plus melatonin. Albumin flux across
the monolayers was obtained as a marker of permeability (n =
6). RLMEC grown on chamber slides (n = 4) were stained for
adherens junction protein β-catenin and the cytoskeletal protein
F-actin, and protein degradation was examined with confocal
microscopy. Statistical analysis was conducted using Student’s
t test and analysis of variance. Intravital microscopy revealed
an increase in vascular hyperpermeability following HS, which
was attenuated with melatonin (P < 0.05). HS animals required
more fluid to maintain normotension, and this was mitigated
with melatonin (P < 0.05). MMP-9 activity was elevated in
lung homogenates from HS animals, and levels were lower with
melatonin treatment (P < 0.05). Monolayer permeability was
increased with exposure to HS serum, and melatonin attenuated
this (P < 0.05). Chamber slides showed that HS serum induced
disruption of adherens junction proteins and incited formation of F-actin stress fibers; melatonin preserved the baseline
configuration of both. In conclusion, HS induces microvascular
hyperpermeability and clinical fluid derangements and causes
alterations in endothelial cell structure; melatonin attenuates
these changes.
The effect of multidisciplinary teams for rectal cancer on
delivery of care and patient outcome
Bradford Richardson,* James Fleshman, John Preskitt, and Stephanie Peschka
(e-mail: Bradford.richardson@baylorhealth.edu)
Baylor University Medical Center at Dallas initiated biweekly
colorectal tumor multidisciplinary team (MDT) conferences
in January 2013. All cases of colorectal cancer are presented to
a team of specialists across disciplines. The complex treatment
of rectal cancer requires an MDT approach. It is hypothesized
that these MDTs will allow for 1) standardization of care and
improved utilization of available resources to meet this standard; 2) improvements in the technical aspects of treatment;
and 3) improvements in patient outcome. A retrospective chart
review and review of prospectively collected MDT data was
conducted for all patients treated for primary rectal adenocarcinoma at the institution in the past 5 years. The 130 patients
were grouped by those discussed by the MDT in 2014 (n =
47) and 2013 (n = 41) and those treated before the initiation
of MDT conferences (n = 42). Data on demographics, clinical stage, process evaluation, quality of surgery, and outcomes
were collected. The National Comprehensive Cancer Network
guidelines and College of American Pathologists protocol were
used as standards. Clinical stage III was higher in 2013. Steady
improvements were seen in 13 of the 15 preoperative process
variables, 7 significantly. Improvement in an important technical aspect of surgery, the completeness of total mesorectal excision, was significant. The time to recurrence in the pre-MDT
group was 27 months. The mean time since resection in the
MDT groups was 6.5 and 14.5 months. It is too early to determine if recurrence rates and survival rates have improved. Since
adopting the MDT approach, steady improvements have been
made in preoperative clinical staging, multimodality treatment,
Baylor University Medical Center Proceedings
Volume 29, Number 1
pathologic staging, and technical aspects of surgery. There is still
considerable room for improvement in some areas, especially the
use of the rigid proctoscope and chest imaging for metastasis.
Close follow-up of the 88 post-MDT patients will show whether
these improvements in delivery of care result in improvements
in patient outcomes.
Tailoring surgical approach for elective ventral hernia repairs
based on obesity and outcomes
in ventral hernia repairs. National data demonstrate that the
laparoscopic approach is increasingly preferred as BMI increases
when repairing elective reducible hernias. Early postoperative
complications are more common as BMI increases in both open
and laparoscopic repairs. The laparoscopic approach is associated with lower superficial and deep SSI complications for all
BMI categories, in addition to lower organ space infections,
reoperation, and wound dehiscence complications for higher
obesity classes.
Mary Mrdutt* and Justin Regner (e-mail: mmrdutt@sw.org)
Currently, a third of the US population is obese, and that percentage is projected to exceed 40% by 2030, involving approximately 140 million people. Obesity’s influence on postoperative
complications in laparoscopic ventral hernia repairs (LVHR)
versus open ventral hernia repairs (OVHR) has yet to be defined.
While 30-day postoperative complications in both LVHR and
OVHR are more frequent as body mass index (BMI) increases,
we propose that the laparoscopic approach minimizes infectious
complications for given BMI categories. A retrospective review
was conducted of the American College of Surgeons National
Surgical Quality Improvement Program database (2009–2012)
for all patients ≥18 years undergoing elective repair of reducible
ventral hernia. Exclusion criteria included immunosuppression,
disseminated malignancy, advanced liver disease, or pregnancy.
Patients were stratified by World Health Organization BMI
categories of normal weight, overweight, and obesity classes I,
II, and III (BMI 20–25, 25–30, 30–35, 35–40, and ≥40 respectively). Thirty-day postoperative complications were evaluated
across BMI groups for LVHR vs OVHR using chi-squared test.
Linear regression was adjusted for diabetes, smoking, gender,
and age. A total of 75,168 patients met inclusion criteria, with
nearly 55% of patients obese. The rate of LVHR increased with
BMI (normal weight, 17.8%; BMI ≥40, 28.3%). Superficial
and deep surgical site infections (SSIs) increased with increasing
BMI for both techniques. However, LVHR minimized superficial and deep SSIs across all BMIs (odds ratio, open versus
laparoscopic, specifically for BMI ≥40, superficial SSI, 5.34;
deep infections, 4.76). Organ space infections, reoperation,
and wound dehiscence increased with increasing BMI only in
OVHR (P < 0.05). For organ space infections, reoperation, and
wound dehiscence, only higher classes of obesity had a statistically significant difference (odds ratio, open versus laparoscopic
at BMI 35–40: organ space, 1.98; reoperation, 1.86; wound
dehiscence, 4.79; P < 0.05). Obese patients are overrepresented
January 2016
Do donor lifestyle choices and polysubstance abuse affect
long-term survival in heart transplant recipients?
Yazhini Ravi, Shelly Bansal, Kim Jeong, Sitaramesh Emani, Bryan A. Whitson, Carl
Tong, and Chittoor B. Sai-Sudhakar (e-mail: yravi@sw.org)
High-risk behavior negatively impacts donor acceptance. We
sought to evaluate the impact of donors’ negative lifestyle
choices and substance abuse on long-term outcomes in heart
transplant recipients. The registry of the United Network for
Organ Sharing was queried for adult heart transplant recipients
from 2000 to 2013. Donors were categorized into non–high
risk and high-risk based upon the factors listed by the Centers
for Disease Control and Prevention: a history of intravenous
drug use, prostitution, high-risk sexual activity, HIV exposure,
and hemophilia. We also sought to evaluate the impact of alcohol, tobacco, or cocaine abuse. A t test was used to analyze
continuous variables, and a chi-square test was used to analyze
categorical variables. Kaplan-Meier survival curves were created to analyze the impact of substance abuse on transplant
recipient survival. A total of 17,546 heart transplant recipients
were identified. In the high-risk donor group, 43% had type
O blood, 78% were males, and 69% were Caucasians. In the
non–high-risk donor group, 54% had type O blood, the mean
donor age was 29.9 ± 9.5 years, body mass index was 26.2 ±
4.8 kg/m2, and 69% were Caucasians. There were no significant differences in age and body mass index between the two
groups, but donor age and BMI were significantly lower in
transplant recipients. Equivalent waiting times were seen in
both groups. Rejection and graft failure secondary to acute or
chronic rejection at 1 year were not statistically significantly
different between groups. Posttransplant survival at 5 years was
similar in both groups. In conclusion, high-risk donor behaviors and polysubstance abuse do not adversely affect outcomes
in heart transplantation. Negative lifestyle choices should not
deter organ acceptance.
Abstracts from the 10th annual Baylor Scott & White Department of Surgery Research Day
29
Superior mesenteric artery–duodenal fistula secondary to a
gunshot wound
Cory M. Fielding, MD, Wesam Frandah, MD, Steven Krohmer, MD, and Deborah Flomenhoft, MD
Arterioenteric fistulas are a rare cause of massive gastrointestinal hemorrhage. We present a patient who developed a fistula between a middle
colic artery pseudoaneurysm, a proximal branch of the superior mesenteric artery (SMA), and the third part of the duodenum 2 weeks after a
self-inflicted gunshot wound to the abdomen. The patient’s presentation,
evaluation, treatment, and prognosis are discussed. All prior published
cases of SMA-duodenal fistulas are reviewed.
A
neurysms of mesenteric arteries are rare, and most
are asymptomatic when detected on cross-sectional
imaging. Otherwise, patients may present with gastrointestinal bleeding and abdominal pain if an aneurysm
forms a fistula upon rupture. Historically a “herald bleed”
often precedes massive exsanguination, thus giving a clinician the opportunity to diagnose an often fatal presentation.
Although an arterioenteric fistula is rare, this case highlights
the importance of quickly diagnosing and intervening in a
highly lethal diagnosis.
CASE REPORT
A 59-year-old white woman experienced two large episodes
of bright red emesis associated with dizziness and near syncope.
She was admitted 2 weeks prior for a self-inflected gunshot
wound to the anterior abdomen and underwent exploratory
laparotomy, which showed perforation in the fourth part of the
duodenum and a mesenteric defect around the transverse colon.
She underwent successful primary repair. Her hospital course
was complicated by atrial fibrillation with rapid ventricular response. On physical examination, her heart rate varied from
130 to 140 beats per minute, with a mean systemic arterial
pressure of 60 mm Hg. Bowel sounds were normal, and no localized tenderness was noted. She had a hemoglobin of 5.2 g/dL,
platelet count of 176,000/uL, international normalized ratio
of 1.3, blood urea nitrogen of 16 mg/dL, and creatinine of
0.55 mg/dL.
The patient received four units of packed red blood cells,
2 L of lactated Ringer’s solution, intravenous proton pump
inhibitors, and 250 mg of erythromycin prior to endoscopy.
Esophagogastroduodenoscopy revealed blood in the stomach
and duodenum. After the area was cleaned using a water-jet
30
Figure 1. Pulsating clot in the third part of the duodenum.
pump, a pulsating clot was seen in the third part of the duodenum (Figure 1) attached to the wall with the underlying cavity.
No intervention was attempted. Computed tomographic angiography showed attenuation in the diameter of the proximal
superior mesenteric artery (SMA) adjacent to an air-fluid collection. There was a blush of contrast adjacent to the third portion of the duodenum and the air-fluid collection (Figure 2).
A mesenteric angiogram revealed a pseudoaneurysm of the
proximal middle colic artery, a proximal branch of the SMA,
with a diseased segment of the middle colic artery proximal
to the pseudoaneurysm and contrast extravasation (Figure 3).
This area was successfully coiled angiographically without any
further gastrointestinal bleeding (Figure 4). Later in the hospitalization, lysis of adhesions was performed during repeat
exploratory laparotomy, and a drain was placed into a fluid
collection near the duodenal perforation. Due to its location
From the Division of Digestive Diseases and Nutrition in the Department of Internal
Medicine (Fielding, Frandah, Flomenhoft) and the Department of Radiology
(Krohmer), University of Kentucky, Lexington, Kentucky,
Corresponding author: Wesam Frandah, MD, Department of Internal Medicine,
University of Kentucky, 800 Rose Street, Lexington, KY 40536-0298 (e-mail:
wfrandah@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):30–32
Figure 4. Successful endovascular coiling of the bleeding vessel.
Figure 2. Contrast blush on computed tomographic angiogram in the superior
mesenteric artery–duodenum area.
near numerous vascular structures and adhesions, no surgical repair was performed on the duodenum. The patient was
discharged home 10 days later in stable condition with a hemoglobin of 9.3 g/dL.
Figure 3. Pseudoaneurysm of the middle colic branch (black arrow) of the superior mesenteric artery (white arrow) on mesenteric angiography.
January 2016
DISCUSSION
Arterioenteric fistulization is a rare, and often feared, presentation of massive gastrointestinal hemorrhage with a high
mortality rate. The two types of fistula are primary (from atherosclerosis, an aortic aneurysm, aortitis, penetrating ulcer,
radiation, or trauma) or secondary after surgical vascular reconstruction (1, 2). Often, these fistulas develop in the aorta
and erode into the duodenum, causing massive hematemesis
due to their anatomic proximity (3). In patients with penetrating trauma to the abdominal aorta, 98% have injured viscera
as well (4). Patients with arterioenteric fistulas can present with
a “herald bleed,” or small episode of bleeding, before massive
hemorrhage leading to exsanguination, as described in the first
case report by Sir Astley Cooper in 1825 (3).
The diagnosis of this presentation can elude the unsuspecting clinician if a thorough history (including any prior vascular
repairs) is not obtained. Prompt evaluation, usually with upper
endoscopy, should be performed and vascular imaging obtained
if a vascular injury is suspected (5). Endoscopic therapy of an
adherent clot in the management of gastrointestinal bleeding is
controversial. Randomized controlled trials are inconclusive (6,
7). Consensus guidelines state that endoscopic removal can be
considered in the management of an adherent clot after injecting
the underlying ulcer, or intensive proton pump therapy can be
used alone with a similar outcome (8). In our case, because of
the clot location, there was significant concern of major vessel
communication; the endoscopist thought clot removal would
likely lead to massive bleeding and a significant adverse outcome. Because these fistulas are very uncommon, no evidencebased management guidelines are available.
Table 1 summarizes all cases of fistulization of the SMA (or
its branches) and the duodenum published in the English medical literature (10–18). Most of these reported cases were treated
either angiographically or by surgical intervention. Our patient
had higher surgical risk and, therefore, we picked the less morbid approach. Exsanguination was the most common cause of
death (in 82% of patients) in a series of 28 autopsies of patients
Superior mesenteric artery–duodenal fistula secondary to a gunshot wound
31
Table 1. Published cases of SMA-duodenal fistulas
Intestinal
segment
Mechanism
of fistula
Initial
presentation
Later
presentation
Third part of
duodenum
Gunshot 5 years
prior
Hematemesis
and pain
Hematemesis
Survived
Resections
and saphenous
vein graft
N/A
1976
10
Proximal branch Second part of Pancreatic cancer
of the SMA
duodenum
Hematemesis
and melena
Hematemesis
Embolization
Died
Not described
1987
11
Branch of the
SMA
Third part of
duodenum
Melena
Melena
Vasopressin
infusion
Died
Massive pulmo- 1991
nary embolism
12
Branch of the
SMA
Second part of Pancreatic cancer
duodenum
after radiation
Emesis and
melena
Emesis
Embolization
Died
Exsanguination
2002
13
SMA
Third part of
duodenum
Gunshot 1 month
prior
Retroperitoneal
hematoma
Hematemesis
Ligation of
SMA
Died
Cardiac arrest
in OR
2002
14
Pancreaticoduodenal artery
Duodenum
Repaired aneurysm
Unknown
Unknown
Ligation
Survived
N/A
2004
15
SMA
Duodenum
Tuberculosis
Massive
hematemesis
Massive
hematemesis
Duodenectomy
Died
Exsanguination
2004
16
SMA
Third part of
duodenum
Pseudoaneurysm
Abdominal pain
Hematemesis
SMA reconstruction
Survived
N/A
2008
17
Inferior pancreaticoduodenal
artery
Duodenum
Ruptured pseudoaneurysm
Indigestion,
weight loss,
jaundice
Hematemesis
Patient refused
surgery
Died
Exsanguination
2009
18
Vessel
SMA
Metastatic lung
cancer to
duodenum
Management
Cause of
Outcome death
Year
published Ref.
SMA indicates superior mesenteric artery; OR, operating room.
with aortoenteric fistulas (9). The vast majority of cases of arterioenteric fistula involve the aorta, but a small number of cases
are fistulas from the SMA (or its branches). Including the case
described herein, the mortality rate of SMA-duodenal fistulas
is 60%, as calculated by collecting all published cases (Table 1).
9.
10.
11.
1.
2.
3.
4.
5.
6.
7.
8.
32
Budimir I, Nikolić M, Supanc V, Ljubicić N, Krpan T, Zovak M, Sabol M.
Secondary arterio-enteric fistula: case report and review of the literature.
Acta Clin Croat 2012;51(1):79–82.
Bergqvist D, Björck M. Secondary arterioenteric fistulation—a systematic
literature analysis. Eur J Vasc Endovasc Surg 2009;37(1):31–42.
Barry PA, Molland JG, Falk GL. Primary aortoduodenal fistula. Aust N
Z J Surg 1998;68(3):243–244.
Lopez-Viego MA, Snyder WH 3rd, Valentine RJ, Clagett GP. Penetrating abdominal aortic trauma: a report of 129 cases. J Vasc Surg
1992;16(3):332–335.
Schwab CW, McMahon DJ, Phillips G, Pentecost MJ. Aortic balloon control of a traumatic aortoenteric fistula after damage control laparotomy:
a case report. J Trauma 1996;40(6):1021–1023.
Bleau BL, Gostout CJ, Sherman KE, Shaw MJ, Harford WV, Keate RF,
Bracy WP, Fleischer DE. Recurrent bleeding from peptic ulcer associated
with adherent clot: a randomized study comparing endoscopic treatment
with medical therapy. Gastrointest Endosc 2002;56(1):1–6.
Javid G, Masoodi I, Zargar SA, Khan BA, Yatoo GN, Shah AH, Gulzar
GM, Sodhi JS. Omeprazole as adjuvant therapy to endoscopic combination injection sclerotherapy for treating bleeding peptic ulcer. Am J Med
2001;111(4):280–284.
Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair
P; International Consensus Upper Gastrointestinal Bleeding Conference
Group. International consensus recommendations on the management
of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern
Med 2010;152(2):101–113.
12.
13.
14.
15.
16.
17.
18.
Grande JP, Ackermann DM, Edwards WD. Aortoenteric fistulas. A
study of 28 autopsied cases spanning 25 years. Arch Pathol Lab Med
1989;113(11):1271–1275.
Maloney RD, Nealon TF Jr, Roberts EA. Massive bleeding from a
ruptured superior mesenteric artery aneurysm duodenum. Arch Surg
1976;111(3):286–288.
Thorstad BL, Keller FS. Fistula from the superior mesenteric artery to
duodenum: a rare cause of death from pancreatic carcinoma. Gastrointest
Radiol 1987;12(3):200–202.
Steinhart AH, Cohen LB, Hegele R, Saibil FG. Upper gastrointestinal bleeding due to superior mesenteric artery to duodenum fistula:
rare complication of metastatic lung carcinoma. Am J Gastroenterol
1991;86(6):771–774.
Liu B, Howard JM. Vascular-enteric fistulas associated with radiation
therapy in patients with pancreatic adenocarcinoma. HPB (Oxford)
2002;4(2):83–86.
Miglietta MA, Tanquilut EM, Madlinger RV, Prial MM, Scalea TM.
Superior mesenteric artery-duodenal fistula presenting as a late complication of an abdominal gunshot wound. J Trauma 2002;52(3):554–
555.
Sessa C, Tinelli G, Porcu P, Aubert A, Thony F, Magne JL. Treatment
of visceral artery aneurysms: description of a retrospective series of 42
aneurysms in 34 patients. Ann Vasc Surg 2004;18(6):695–703.
Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review
of the literature. Can J Surg 2004;47(5):364–368.
Zhao J. Massive upper gastrointestinal bleeding due to a ruptured
superior mesenteric artery aneurysm duodenum fistula. J Vasc Surg
2008;48(3):735–737.
Colak MC, Kocaturk H, Bayram E, Karaca L. Inferior pancreaticoduodenal artery false aneurysm: a rare cause of gastrointestinal bleeding diagnosed by three-dimensional computed tomography. Singapore Med J
2009;50(10):e346–349.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Removal of an embedded crochet needle in the mouth
Victoria Klovenski, MD, Andrew Juergens, MD, Kyla Lappo, BS, and Kyle Marshall, MD
A 3-year-old child presented to the emergency department with a crochet
needle lodged in her posterior oral cavity. To localize the needle and significant surrounding anatomic structures, bedside transcavitary ultrasound
was employed. After careful localization, the needle was removed using
a modified needle cover technique. A review of barbed foreign object
removal techniques, including advance-and-cut, retrograde, string-yank,
and needle cover techniques, is presented. Important considerations
while planning any procedure include risk, benefit, availability of staff,
and availability of equipment. Proper anesthesia is paramount to the
success of these procedures, and sedation in pediatric patients may
prove necessary. Postprocedure wound care and follow-up must also
be arranged. This case demonstrates the importance of adaptation of
well-documented techniques to remain flexible for any situation that may
present to the emergency department.
T
he removal of barbed foreign objects presents a particular
challenge in the emergency department. Most publications regarding this topic discuss the removal of fish
hooks. Less discussed are methods for removal of other
types of barbed objects, including sewing needles and aquatic animal spines. This report describes barbed foreign object removal
using bedside ultrasound and a modified technical approach.
CASE REPORT
A 3-year-old girl presented to a children’s emergency department for foreign body removal. The patient was running with a
crochet needle in her mouth when she fell forward. The needle
went into her mouth and became lodged (Figure 1). Upon arrival, the child was crying and anxious. She had no respiratory
distress or hemodynamic instability, and her vital signs were
normal. Examination of the mouth revealed intact dentition
and midline uvula. An acrylic crochet needle was penetrating
the left buccal mucosa just lateral to the pterygomandibular
raphe. No hemorrhage or hematoma was noted.
In an attempt to define the track of the needle, a computed
tomography scan was performed, but proved not to be helpful
as the needle was the same density as the soft tissue (Figure 2).
Transcavitary ultrasound under sedation revealed shadowing
at the end of the crochet needle (Figure 3). This allowed for
measurement to determine the depth of the needle, and using
Proc (Bayl Univ Med Cent) 2016;29(1):33–35
Figure 1. Modeled image of a crochet needle embedded in a child’s mouth.
the Doppler feature of the ultrasound, we were able to ensure
that no vascular structures were involved. This suggested that
safe removal in the emergency department was possible.
DISCUSSION
With any foreign body removal in the emergency department, an important initial step in evaluation is localization.
This allows the physician to determine the need for involvement
of surgical subspecialties. In some instances, such as foreign
bodies to the eye, the need for involvement of a subspecialist is
more obvious (1–4). In this case, the decision had to be made
regarding the safety of removing the needle in the emergency
department versus removal in the operating room with an otolaryngologist.
From Baylor Scott & White Healthcare and Texas A&M Health Science Center
College of Medicine, Temple, Texas.
Corresponding author: Victoria Klovenski, MD, Department of Emergency
Medicine, Baylor Scott & White Healthcare, MS-11-AG062, 2401 S. 31st Street,
Temple, TX 76508 (e-mail: vklovenski@sw.org).
33
Table. Techniques for barbed foreign body removal
Technique
Description
Retrograde
Apply downward pressure on
the shank while simultaneously removing the hook in a
retrograde fashion
String-yank
Tie a string around the bend
of the hook. Apply downward
pressure to the shank while
simultaneously applying
strong, retrograde tension on
the string
Illustration
Advance and cut Advance the hook until the
barb is external to the skin,
cut the shaft, and remove
the remainder of the hook in
retrograde fashion
Needle cover
Figure 2. CT image showing the embedded crochet needle having a density
similar to that of soft tissue, making localization difficult.
Four techniques for hooked or barbed foreign body removal
are well described and are summarized and illustrated in the
Table (5–9). These techniques are based upon hooked objects
such as fish hooks that have a large gap between the shank and
the barb. With the crochet needle, the gap was less than a centimeter, making the often successful advance-and-cut technique
difficult. In this technique, a small incision is made over the
location of the end of the foreign body, typically in anesthetized skin. The barb is then advanced through the remaining
soft tissue. Once external to the skin, the shank is cut, and the
remainder of the barb is backed out of the skin. This technique
Figure 3. Transcavitary ultrasound image displaying shadowing at the needle’s
tip. Ultrasound allowed for measurement of depth and localization of vessels
using Doppler.
34
Insert a large-gauge needle
along the path of entry until
reaching the barb, cover the
barb with the lumen of the
needle, and remove the barb
and needle simultaneously in
retrograde fashion
is the most successful of the four described in fish hook removal,
as it can be used on deeply embedded hooks; however, its utility
is limited in barbed objects of other shapes (5, 7–9).
The less invasive retrograde technique was unsuccessful due
to the inability to dislodge the barb. An inability to dislodge
the barb is the limiting factor in this technique. In fact, this
technique was shown to be successful in only 40% of fish hook
removals (10). The percent of success with all barbed objects
remains unknown.
The string-yank method, which is related to the retrograde
technique but is less traumatic to soft tissues, was not possible
due to the bend of the hook itself being lodged in the tissue.
With this technique, the downward pressure used with the
retrograde technique is applied to the shank. Simultaneously,
a string is tied around the bend, and the object is pulled in a
retrograde fashion. Limitations of this technique include lack
of applicability to deeply embedded objects and the potential
for secondary injury due to the projectile nature of the newly
dislodged object (5, 7–9).
A modified needle cover technique proved successful. In
most cases, a needle is inserted at the point of entry and traced
along the bend of the hook. Once the barb is located, the lumen
of the needle is slipped over the barb so that both the needle
and hook may be removed simultaneously (5, 7–9). Since the
Baylor University Medical Center Proceedings
Volume 29, Number 1
barb of the crochet needle was larger than a needle lumen, we
inserted a needle driver into the entry site, traced the bend until
the barb was encountered, covered the barb with the needle
driver, dislodged the barb from the tissue, and removed the
needle and needle driver simultaneously.
The patient was monitored for several hours, but no signs
of hemorrhage or hematoma developed. A small 0.5 centimeter
punctate lesion remained in her left buccal mucosa. The patient
was discharged with follow-up with her pediatrician in 1 week.
1.
2.
3.
Aiello LP, Iwamoto M, Taylor HR. Perforating ocular fishhook injury.
Arch Opthalmol 1992;110(9):1316–1317.
Swanson JL, Augustine JA. Penetrating intracranial trauma from a
fishhook. Ann Emerg Med 1992;21(5):568–571.
White MF, Owens SD, Dooley CD, Kimble JA, Witherspoon CD.
Fishing related eye injuries: a report of 27 cases. Invest Opthalmol Vis
Sci 1990;31:21–22.
January 2016
4.
Deramo VA, Maus M, Cohen E, Jeffers J. Removal of a fishhook in
the eyelid and cornea using a vertical eyelid-splitting technique. Arch
Ophthalmol 1999;117(4):541–542.
5. Lantsberg L, Blintsovsky E, Hoda J. How to extract an indwelling
fishhook. Am Fam Physician 1992;45(6):2589–2590.
6. Morris JA, Swiontkowski MF, Merrmann HJ. Wilderness trauma emergencies. In Auerbach PS, ed. Wilderness Medicine: Management of Wilderness
and Environmental Emergencies, 3rd ed. St. Louis: Mosby, 1995:342–362.
7. Haynes JH. Fishhook removal. In Pfenninger JL, Fowler GC, eds.
Procedures for Primary Care Physicians. St. Louis: Mosby, 1994:128–132.
8. Diekema DS, Quan L. Fishhook removal. In Henretig FM, King C, eds.
Textbook of Pediatric Emergency Procedures. Baltimore: Williams & Wilkins,
1997:1223–1227.
9. Rudnitsky GS, Barnett RC. Soft tissue foreign body removal. In Roberts
JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine, 3rd ed.
Philadelphia: Saunders, 1998:623–624.
10. Doser C, Cooper WL, Ediger WM, Magen NA, Mildbrand CS, Schulte
CD. Fishhook injuries: a prospective evaluation. Am J Emerg Med
1991;9(5):413–415.
Removal of an embedded crochet needle in the mouth
35
Bilateral cavernous sinus and superior ophthalmic vein
thrombosis in the setting of facial cellulitis
Almas Syed, MD, Bruce Bell, MD, Joseph Hise, MD, Joseph Philip, MD, Cedric Spak, MD, MPH, and
Michael J. Opatowsky, MD, MBA
Cavernous sinus thrombosis is a rare, potentially fatal cause of cerebral
venous thrombosis. Infectious causes typically arise from the mid face,
orbit, or sinonasal region. We present a case of bilateral cavernous sinus
and superior ophthalmic thrombosis secondary to an extreme case of
facial cellulitis.
CASE REPORT
A 25-year-old woman initially presented with complaints of
a headache and had reportedly injected methamphetamine into
her left cheek. She was diagnosed with left facial cellulitis with
an open ulceration, sinusitis, and methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, for which she was being
treated. On presentation to our facility, she was obtunded with
left greater than right chemosis and anisocoria. The left maxillary and periorbital regions were swollen. A chest radiograph
revealed a multifocal nodular and patchy infiltrate. She was
intubated due to worsening respiratory distress and obtundation. Laboratory analysis revealed a neutrophilic-predominant
leukocytosis (21.5 K/uL), metabolic acidosis (pH 7.2), and
substantial electrolyte derangements, including a serum sodium
level of 160 mEq/L. Repeat blood cultures showed MRSA.
(1,3)-Beta-D-glucan (Fungitell) assay was negative for associated fungal infections.
An unenhanced computed tomography (CT) scan of the
brain and contrast-enhanced CT angiogram demonstrated
multiple abnormal findings, including multiple acute infarcts
in the bilateral frontal and parietal lobes and left superior cerebellum. Thrombus was present in the left internal jugular vein,
left sigmoid and transverse sinuses, cavernous sinuses bilaterally, and the superior ophthalmic veins bilaterally, as confirmed
on magnetic resonance imaging (MRI) (Figure 1). Substantial
vasospasm was noted involving the cavernous segment of the
left internal carotid artery (Figure 1a). Extensive bilateral acute
cerebral infarcts were apparent within the bilateral anterior
circulation as well as developing ischemic injury to the pons,
cerebellum, hypothalamus, and mammillary bodies (Figure 2a).
The MRI examination also showed diffuse left facial cellulitis in
conjunction with sites of venous thrombosis within the bilateral
cavernous sinuses, superior ophthalmic veins, left transverse sinus, sigmoid sinus, and left internal jugular vein (Figure 2b, 2c).
36
Attempts were made to hemodynamically stabilize the patient and to gradually correct the hypernatremia. She was initially placed on broad-spectrum antibiotic coverage that was
later refined to vancomycin and rifampin based on positive
blood cultures for MRSA. Heparin was started. The patient
rapidly succumbed.
DISCUSSION
While not rare, thrombosis of the cerebral veins is a relatively
uncommon clinical presentation. Venous thrombosis is thought
to be associated with 0.5% to 1% of all strokes (1). Cavernous
sinus thrombosis (CST) is a potentially devastating condition
associated with a mortality rate approaching 30% (2). When
precipitated by highly aggressive infections, CST can result
in rapid neurologic deterioration, permanent impairment, or
death. Prompt diagnosis and emergent treatment are crucial to
ensure survival and to prevent permanent disability.
Patients with infection-induced CST will present with a
nonspecific fever and headache. Often, accompanying proptosis,
chemosis, periorbital swelling, and cranial nerve palsies will be
encountered (2). An understanding of the underlying venous
anatomy allows for a better appreciation of the pathophysiology and clinical presentation of CST. The cavernous sinuses
reside bilaterally adjacent to the pituitary-containing sella turcica. They are formed by a separation of the dura mater with
multiple trabeculae forming the “cavernous” appearance of these
venous spaces. Unique to the cavernous sinuses is the intimate
association of flowing venous channels with a number of critical
cranial nerves as well as a robust anastomotic vascular network.
The horizontal segment of the internal carotid artery and the abducens nerve (CNVI) are enveloped by and traverse this venous
sinus. The oculomotor nerve (CN III), trochlear nerve (CN
IV), and the first and second divisions of the trigeminal nerve
(CN V) are intimately associated with the lateral walls of the
cavernous sinuses (3). Intracavernous pathology can alter ocular
motility by preferentially affecting CNVI function. This might
From the Department of Radiology (Syed, Bell, Hise, Philip, Opatowsky) and the
Division of Infectious Diseases (Spak), Baylor University Medical Center at Dallas.
Corresponding author: Almas Syed, MD, Department of Radiology, Baylor
University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX 75246
(e-mail: Almas.Syed@baylorhealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):36–38
a
b
c
d
Figure 1. (a) CT angiogram demonstrating the attenuated appearance of the left supraclinoid internal carotid artery
secondary to inflammatory vasospasm (arrow). (b) Contrast-enhanced MR revealing lack of enhancement and enlargement of the left cavernous sinus with a convex margin (arrow). (c) T2-weighted MR sequence showing enlarged bilateral
superior ophthalmic veins with lack of flow-related signal due to thromboses (arrows). (d) Contrast-enhanced MR also
showing a lack of expected flow-related signal in the setting of bilateral superior ophthalmic venous thromboses (arrows).
a
b
Figure 2. (a) Diffusion-weighted MR sequence demonstrating bilateral frontoparietal areas of diffusion restriction
(arrows) consistent with acute infarctions (confirmatory ADC maps not shown). (b) Enhanced MR demonstrating
lack of enhancement of the left sigmoid sinus consistent with dural venous sinus thrombosis (arrow).
January 2016
be seen clinically as an inability of
the affected globe to achieve normal
conjugate temporal gaze.
The veins from the middle third
of the face are interconnected to the
cavernous sinus through the pterygoid plexus and ophthalmic veins.
With progressive CST, venous engorgement and stasis often will be
appreciated clinically by developing proptosis and chemosis (4). It
is thought that this interconnected
vascular network, with its unique
pattern of venous drainage accompanied by valveless veins, leads to the
propensity for infections from the
middle third of the face to spread to
the cavernous sinuses.
Th e contribution of valveless
veins as a risk factor for the dissemination of facial or orbital infections into the cavernous sinuses
has been debated in the literature.
At least one report in the literature
indicated finding valves in the facial and superior ophthalmic veins
(5). The cavernous sinuses can also
communicate with one another
across the anatomic midline via
the anterior and posterior intercavernous veins, potentially serving as a source for bilateral seeding
of thrombophlebitis. The cavernous sinuses drain into the petrosal
sinuses with eventual downstream
drainage into the internal jugular veins, placing them at risk for
thrombosis as well (4).
Diagnosis of CST is best established on clinical grounds and
confirmed by radiographic studies.
Radiologic findings include expansion of a cavernous sinus with reversal of its typical concave outer
margin, asymmetrically diminished enhancement with filling defects, and narrowing or occlusion
of the cavernous portion of the
internal carotid artery (Figure 1).
Due to obstruction or marked
narrowing and compromise, upstream venous congestion can be
seen in the ophthalmic veins with
resultant extraocular muscle enlargement and induration of the
retrobulbar fat (5–7).
Bilateral cavernous sinus and superior ophthalmic vein thrombosis in the setting of facial cellulitis
37
1.
2.
3.
4.
Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara
B, Cushman M, deVeber G, Ferro JM, Tsai FY; American Heart Association Stroke Council and the Council on Epidemiology and Prevention.
Diagnosis and management of cerebral venous thrombosis: a statement for
healthcare professionals from the American Heart Association/American
Stroke Association. Stroke 2011;42(4):1158–1192.
DiNubile MJ. Septic thrombosis of the cavernous sinuses. Arch Neurol
1988;45(5):567–572.
Lucarilli MJ, Kim N. Applied anatomy of the orbit. In Mallajosyula S, ed.
Surgical Atlas of Orbital Disease, 1st ed. Maryland Heights, MO: Jaypee
Brothers, 2009:8–9.
Ebright JR, Pace MT, Niazi AF. Septic thrombosis of the cavernous sinuses.
Arch Intern Med 2001;161(22):2671–2676.
Zhang J, Stringer MD. Ophthalmic and facial veins are not valveless. Clin
Experiment Ophthalmol 2010;38(5):502–510.
6. Roth E, Wiant A, Sperling V. Cavernous sinus thrombosis [American
College of Radiology Case in Point, 2012]. Retrieved from https://3s.acr.
org/CIP/ArchiveCaseView.aspx?CaseId=MuJzbBK185U%253d; accessed
October 26, 2015.
7. Komatsu H, Matsumoto F, Kasai M, Kurano K, Sasaki D, Ikeda K.
Cavernous sinus thrombosis caused by contralateral sphenoid sinusitis: a
case report. Head Face Med 2013;9:9.
8. Coutinho J, de Bruijn SF, Deveber G, Stam J. Anticoagulation
for cerebral venous sinus thrombosis. Cochrane Database Syst Rev
2011;(8):CD002005.
5.
Avocations
Mount Rainier
I
Loosed of the digital collar
and the wireless leash,
strolled on a vibrant carpet
laid by the fallen leaves.
Yellow, gold, shades of red,
sprayed on the sloping canvas.
Mixture of the fertile lava
and plethora of decay
furnished elements for the paint.
Summer having bid adieu,
approaching winter nudged the sun
on a southerly course.
A shared kingdom of serenity,
everyone was welcome.
Each whiff of mountain air
cleansed my defiled lungs,
choked by the inhaled soot
in the urban labyrinth;
healing my cyanotic soul.
—Amanullah Khan, MD, PhD
Copyright © 2013 by Amanullah Khan. Reprinted from Sifting Shades (Dog Ear Publishing, 2013). Dr. Khan (e-mail: aman1963@
gmail.com) is a member of the Poetry Society of Texas and an oncologist on the medical staff of Baylor Medical Center at McKinney.
38
Baylor University Medical Center Proceedings
Volume 29, Number 1
Coccidioidomycosis with diffuse miliary pneumonia
David Sotello, MD, Marcella Rivas, MD, Audra Fuller, MD, Tashfeen Mahmood, MD, Menfil Orellana-Barrios, MD,
and Kenneth Nugent, MD
Coccidioidomycosis is a well-known infection in the southwestern United
States, and its occurrence is becoming more frequent in endemic areas.
This disease can have a significant economic and medical impact; therefore,
accurate diagnosis is crucial. In conjunction with patient symptoms, residence in or travel to an endemic area is essential for diagnosis. Diagnosis
is usually made with serology, culture, or biopsy and confirmed with DNA
probe technology. Pulmonary disease is the most common presentation and
is seen in almost 95% of all cases. One-half to two-thirds of all Coccidioides
infections are asymptomatic or subclinical. Most pulmonary infections are
self-limited and do not require treatment except in special populations.
When treatment is warranted, itraconazole and fluconazole are frequently
used. Diffuse miliary pneumonia is uncommon and is especially rare in immunocompetent patients. Herein we describe a rare presentation of miliary
coccidioidomycosis in a nonimmunocompromised patient.
C
occidioidomycosis is a well-known infection in the
southwestern US (1, 2) that has become more frequent
in endemic areas, with an increase from 5.3 new cases per
100,000 persons in 1998 to 42.6 new cases per 100,000
in 2011 (3). The increase is likely influenced by population migration, an increased number of immunosuppressed patients, and
increased awareness of the disease (1, 2, 4). Pulmonary disease is
the most common presentation of coccidioidomycosis. Most cases
are asymptomatic or resolve spontaneously, but some patients with
diverse risk factors may develop severe disease. Diffuse miliary
pneumonia is uncommon, and it is usually found in immunocompromised patients, in whom it has a poor prognosis (1, 4, 5, 6).
CASE DESCRIPTION
A previously healthy 49-year-old black man was sent from a
prison unit to the emergency center. He presented with 2 weeks
of new-onset progressive dyspnea associated with dry cough and
intermittent fevers and chills. His blood pressure was 124/75
mm Hg; temperature, 97.5°F; heart rate, 105 beats/minute; and
respiration, 28 breaths/minute with an oxygen saturation of 86%
on room air. His body mass index was 20.4 kg/m². He was in
moderate respiratory distress and had bilateral fine crackles. His
leukocyte count was 12.4 K/μL with neutrophil predominance
and eosinophilia of 1.4 K/μL. Chest radiography and computed
tomography of the chest are shown in Figure 1. The patient was
Proc (Bayl Univ Med Cent) 2016;29(1):39–41
a
b
Figure 1. (a) A chest x-ray shows bilateral miliary infiltrates. (b) Chest computed
tomography scan without contrast shows bilateral miliary infiltrates and bilateral
pleural effusions (arrows).
From the Department of Internal Medicine, Texas Tech University Health Sciences
Center, Lubbock, Texas.
Corresponding author: Kenneth Nugent, Department of Internal Medicine, Texas
Tech University Health Sciences Center, 3601 4th Street, Lubbock, TX 79430
(e-mail: kenneth.nugent@ttuhsc.edu).
39
Table 1. Atypical pneumonia evaluation
Test performed
Procalcitonin (ng/mL)
Patient’s
value
Reference
range
0.13
0.51–1.99
HIV ELISA
Negative
Negative
Influenza (A and B) PCR
Negative
Negative
Sputum culture
Negative
Negative
1:512
<1:2
Coccidioides complement fixation antibody
Urine Legionella antigen
Mycoplasma pneumoniae culture
(1,3) B-D Glucan (pg/mL)
Quantiferon-TB
Urine Histoplasma galactomannan antigen (ng/mL)
Not detected Not detected
Negative
Negative
146
<60
Negative
Negative
<0.5
<0.5
ELISA indicates enzyme-linked immunosorbent assay; PCR, polymerase chain reaction.
given ceftriaxone and azithromycin but his fever and hypoxemia
persisted, and fluconazole was started on the third day of hospitalization.
Additional laboratory tests were obtained to evaluate for
atypical pneumonia (Table 1). A transbronchial biopsy showed
loose granulomas with moderate chronic and mild acute inflammation and occasional spherules with interstitial fibrosis.
Bronchial washing cultures were positive for Coccidioides immitis
per DNA probe. He was discharged on oral fluconazole 400 mg
daily and supplemental oxygen. Approximately 1 month later,
he no longer required oxygen supplementation (with an oxygen
saturation of 94% on room air), and it was recommended he
complete 1 year of antifungal therapy.
DISCUSSION
Coccidioides sp., a dimorphic fungus present in the soil
as a mold, is found only in the Western hemisphere and
is endemic in the southwestern US, northern Mexico, and
South America. Arthroconidia disperse into the air and can
be inhaled by animals or humans. Within the human body,
they transform into spherical structures called spherules
that eventually grow and break open, releasing hundreds to
thousands of endospores, which perpetuate the cycle. Endospores may spread via hematogenous and/or lymphatic
drainage (1, 4). Two species have been described: C. immitis
(which seems to be limited to the San Joaquin Valley) and
C. posadasii (2, 4).
One-half to two-thirds of these infections are asymptomatic or subclinical (4, 5). Individuals older than 60 years and
patients with congestive heart failure, chronic lung disease, cancer, AIDS, or other immunocompromised states are prone to
symptomatic disease (5). Immunosuppressed patients, pregnant
women in the third trimester, persons of Filipino or African
American ancestry, diabetics, the elderly, and smokers are at increased risk for severe or disseminated disease (4, 6). This disease
has five main clinical presentations: acute pneumonia, chronic
progressive fibrocavitary pneumonia, pulmonary nodules and
40
cavities, extrapulmonary nonmeningeal disease, and meningitis
(1). Pulmonary disease is seen in almost 95% of cases (4, 6).
Acute pneumonia is an acute respiratory infection that usually occurs 1 to 3 weeks after exposure (1, 5) and can be associated
with generalized symptoms and/or cutaneous manifestations (1,
4). The chest x-rays of patients with acute pneumonia are similar
to those for other etiologies of community-acquired pneumonia
(1, 4). Coccidioidomycosis can account for 17% to 29% of
cases of community-acquired pneumonia in endemic areas (3).
Residents and recent travelers to endemic areas with compatible symptoms should be evaluated for coccidioidomycosis (5).
Diffuse miliary pneumonia is uncommon and presents as
bilateral reticulonodular or miliary infiltrates on imaging studies. It can be associated with large inoculums, fungemia, or
lymphatic spread. The presence of diffuse miliary pneumonia
suggests underlying immunodeficiency, and those patients are
usually critically ill, with the vast majority developing acute
respiratory distress syndrome (ARDS) (1, 4, 5). ARDS has a
mortality of nearly 100% in immunosuppressed patients (4, 6).
Miliary disease in immunocompetent patients is very rare. The
largest series of immunocompetent patients with diffuse miliary pneumonia reported 8 patients, 2 of whom were pregnant;
5 (62.5%) developed ARDS, and 3 (37.5%) died (7).
Diagnosis is usually made with serology, culture, or biopsy
(4). All cultures should be confirmed with DNA probe technology (6). The finding of spherules in any body fluid or tissue
is always indicative of infection. Serologic testing is based on
finding antibodies to a coccidioidal-related antigen. Diagnosis
is also based on immunologic evidence of disease in the form
of detection of IgM or IgG by immunodiffusion, enzyme immunoassay, latex agglutination, tube precipitin, or complement
fixation (8, 9). Skin testing (coccidioidin) cannot differentiate
between recent or past infection (10).
Most pulmonary infections are self-limited and do not require treatment. Treatment should be considered for patients at
high risk for severe disease (1, 4–6). Itraconazole and fluconazole
are the most commonly used drugs (1, 5). Galgiani et al compared fluconazole to itraconazole in a randomized controlled
trial and found that itraconazole had better outcomes (11).
Fluconazole has excellent bioavailability and tissue penetration
and few drug interactions, making it the agent of choice (4).
Treatment is usually given for 3 to 6 months for acute pneumonia (1, 4, 5). Diffuse miliary pneumonia may require several
weeks of amphotericin B, followed by maintenance therapy with
an azole for a year or indefinitely (4, 6).
1.
2.
3.
4.
5.
Parish JM, Blair JE. Coccidioidomycosis. Mayo Clin Proc 2008;83(3):343–
348.
Ampel NM. Coccidioidomycosis: a review of recent advances. Clin Chest
Med 2009;30(2):241–251.
Centers for Disease Control and Prevention. Increase in reported coccidioidomycosis—United States, 1998–2011. MMWR Morb Mortal Wkly
Rep 2013;62(12):217–221.
Thompson GR 3rd. Pulmonary coccidioidomycosis. Semin Respir Crit
Care Med 2011;32(6):754–763.
Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Johnson RH, Stevens DA,
Williams PL; Infectious Diseases Society of America. Coccidioidomycosis.
Clin Infect Dis 2005;41(9):1217–1223.
Baylor University Medical Center Proceedings
Volume 29, Number 1
6.
7.
8.
9.
Spinello IM, Munoz A, Johnson RH. Pulmonary coccidioidomycosis.
Semin Respir Crit Care Med 2008;29(2):166–173.
Arsura EL, Kilgore WB. Miliary coccidioidomycosis in the immunocompetent. Chest 2000;117(2):404–409.
Malo J, Luraschi-Monjagatta C, Wolk DM, Thompson R, Hage CA,
Knox KS. Update on the diagnosis of pulmonary coccidioidomycosis.
Ann Am Thorac Soc 2014;11(2):243–253.
Hector RF, Rutherford GW, Tsang CA, Erhart LM, McCotter O,
Anderson SM, Komatsu K, Tabnak F, Vugia DJ, Yang Y, Galgiani JN.
The public health impact of coccidioidomycosis in Arizona and California.
Int J Environ Res Public Health 2011;8(4):1150–1173.
10. Deus Filho AD. Chapter 2: coccidioidomycosis. J Bras Pneumol
2009;35(9):920–930.
11. Galgiani JN, Catanzaro A, Cloud GA, Johnson RH, Williams PL, Mirels LF,
Nassar F, Lutz JE, Stevens DA, Sharkey PK, Singh VR, Larsen RA, Delgado
KL, Flanigan C, Rinaldi MG; Mycoses Study Group. Comparison of oral fluconazole and itraconazole for progressive, nonmeningeal coccidioidomycosis.
A randomized, double-blind trial. Ann Intern Med 2000;133(9):676–686.
Acknowledgment of reviewers for BUMC Proceedings, volume 28
O
ur thanks to those who reviewed and critiqued manuscripts submitted to Baylor University Medical
Center Proceedings for publication in volume 28. Reviewing scientific papers is an often unrecognized,
arduous, and time-consuming task. We are grateful to our 68 editorial board members and to the
following additional reviewers for contributing their valuable comments and suggestions.
William Abramovits, MD
Manish D. Assar, MD
David J. Ballard, MD, PhD
Robert D. Black, MD
Preston H. Blomquist, MD
Christine Brown, MD
Paul Brown, MD
Charles S. Bryan, MD
Michael L. Chikindas, PhD
Arpitha Chiruvolu, MD
Tuoc N. Dao, MD
Patricia de Leon, DO
Howard C. Derrick III, MD
Simon Driver, PhD
Cara A. East, MD
Kathleen Ellis, MSN, PhD
Adam Falcone, MD
John S. Fordtran, MD
Michael Foreman, MD
W. Bruce Fye, MD
Robert M. Goldstein, MD
Cara Govednik, MD
January 2016
Robert Gunby Jr., MD
Shelley A. Hall, MD
Rita Hamilton, DO
Baron L. Hamman, MD
Susan Houston, RN, PhD
Robert W. Inzer, MD
Ronald C. Jones, MD
Kartik Konduri, MD
Nicholas G. Kounis, MD, PhD
Robert C. Kowal, MD, PhD
Johannes J. Kuiper, MD
Richard Lange, MD
Kennith F. Layton, MD
David M. Lee, MD
Bennett Lorber, MD
Carolyn M. Matthews, MD
Ankit N. Mehta, MD
James D. Meler, MD
Larry B. Melton, MD, PhD
Piers D. Mitchell, PhD
Ariel Modrykamien, MD
Adan Mora Jr., MD
Coccidioidomycosis with diffuse miliary pneumonia
Richard C. Naftalis, MBA, MD
John C. O’Brien, MD
W. Clyde Partin Jr., MD
Suraj Reddy, MD
Robert L. Rosenthal, MD
Caitriona Ryan, MD
Marta San Luciano, MD
Syed A. Sarmast, MD
William Schiavone, DO
John C. Schwartz, MD
William P. Shutze, MD
Louis M. Sloan, MD
Cedric W. Spak, MD
Robert C. Stoler, MD
James F. Trotter, MD
Ivan Vrcek, MD
Jennifer Wells, MD
Matthew V. Westmoreland, MD
Jonathan Whitfield, MD
Michael Wiederkehr, MD
Barry N. Wilcox, MD
41
Choriocarcinoma presenting with thyrotoxicosis
David Sotello, MD, Ana Marcella Rivas, MD, Victor J. Test, MD, and Joaquin Lado-Abeal, MD, PhD
We describe a 26-year-old man with metastatic choriocarcinoma who
presented with hyperthyroidism associated with elevated β-human chorionic gonadotropin (B-HCG) and respiratory failure secondary to diffuse
lung metastasis. After the first cycle of chemotherapy, the concentration
of B-HCG dramatically decreased and the patient became euthyroid,
allowing us to discontinue antithyroid medications. The patient’s hyperthyroidism was caused by stimulation of the thyroid gland by high B-HCG
levels, as shown by the marked improvement of the patient’s thyroid
function panel after chemotherapy.
H
uman chorionic gonadotropin (HCG)–induced
hyperthyroidism is a rare cause of hyperthyroidism. It
is seen in patients suffering from conditions associated
with extremely high levels of HCG, such as hyperemesis gravidarum, hydatidiform moles, and germ cell tumors. At
very high levels, HCG can stimulate the TSH receptor, causing
hyperthyroidism (1). We present the case of a 26-year-old man
diagnosed with metastatic choriocarcinoma and concomitant
hyperthyroidism related to extremely high levels of β-human
chorionic gonadotropin (B-HCG). The patient’s hyperthyroidism resolved as the B-HCG decreased because of chemotherapy.
CASE DESCRIPTION
A previously healthy 26-year-old man presented with a
3-week history of fever, chills, cough, hemoptysis, and dyspnea.
He also reported anxiety, palpitations, hand tremors, and a
30-pound weight loss in a 3-month period. A chest radiograph
showed multiple diffuse nodules of 1 to 3.5 cm throughout
both lung fields (Figure 1). Upon presentation at our hospital,
his heart rate was 136 beats per minute, and his respiratory rate
was 25 breaths per minute. On initial exam he had fine crackles
in both lung bases. The thyroid gland and scrotal examinations
were unremarkable. His free thyroxine was 4.14 ng/dL (normal,
0.93–1.7); free triiodothyronine, 10.6 pg/mL (normal, 2.3–
4.2); thyroid-stimulating hormone (TSH), <0.01 mcIU/mL
(normal, 0.27–4.20); B-HCG, 616,433 MIU/mL (normal,
1–5); lactate dehydrogenase, 1232 IU/L (normal, 135–225);
alanine aminotransferase, 53 IU/L (normal, 7–40); and aspartate aminotransferase, 61 IU/L (normal, 10–42). The patient
was started on methimazole, dexamethasone, and propranolol.
42
Figure 1. Posteroanterior chest radiograph showing numerous metastatic
pulmonary nodules bilaterally.
Testicular ultrasound showed a heterogeneous right testicle
with microlithiasis and a 10 mm septated upper pole cyst, with
moderate right hydrocele. Computed tomography (CT) of the
head, chest (Figure 2), abdomen, and pelvis suggested diffuse
metastasis of the brain, lungs, liver, and retroperitoneal lymph
nodes. CT-guided biopsy of one of the lung nodules was consistent with metastatic choriocarcinoma based on positive staining
for B-HCG.
The patient was treated with bleomycin, etoposide, and cisplatin. After completing his first chemotherapy cycle, his serum
B-HCG decreased significantly and the thyroid function panel
improved to near normalization (Table 1). Methimazole was decreased from 45 mg to 10 mg daily and was discontinued 3 weeks
after he completed the first cycle of chemotherapy. At discharge,
From the Department of Internal Medicine (Sotello, Rivas), Division of Pulmonary/
Critical Care Medicine (Test), and Division of Endocrinology (Lado-Abeal), Texas
Tech University Health Science Center, Lubbock, Texas.
Corresponding author: Ana Marcella Rivas, MD, Department of Internal
Medicine, Texas Tech University Health Science Center, 3601 4th Street, Lubbock,
TX 79430 (e-mail: amarcellarivas@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):42–43
Figure 2. Computed tomography of the chest with intravenous contrast
demonstrating numerous intraparenchymal pulmonary nodules (cannonball
appearance) of varying sizes and diffuse superior mediastinal lymphadenopathy.
a radical orchiectomy and radiation for brain metastasis was
planned, but unfortunately the patient was lost to follow up.
DISCUSSION
HCG is a glycoprotein hormone that has intrinsic thyroidstimulating activity (2). HCG-alpha subunit is common to
all the glycoprotein hormones (follicle-stimulating hormone,
luteinizing hormone, TSH). HCG and TSH-beta subunit are
highly homologous (3): both contain 12 half-cysteine residues and one N-linked oligosaccharide, and three disulphide
bonds from a cysteine knot structure are identical in both
hormones and essential for binding to the receptor (4). HCG
is, therefore, able to cross-react with the TSH receptor (5)
and can induce hyperthyroidism when the HCG levels are
high enough (3).
Testicular tumors account for 1% of male malignancies in
the USA, and more than 95% originate from germ cells that
are classified as seminomatous or nonseminomatous germ cell
tumors (NSGCT) (6). NSGCT can secrete HCG, and some
patients can develop hyperthyroidism as a paraneoplastic phenomenon (1). The prevalence of hyperthyroidism in patients
with NSGCT presenting with elevated levels of HCG is not
known, although in a large cohort of 144 patients with NSGCT,
hyperthyroidism was found in 5 patients (3.5%) with HCG
levels >50,000 mIU/mL. The prevalence of hyperthyroidism
in those with serum HCG >50,000 mIU/mL was 50% (1). In
another series of 17 patients with NSGCT, hyperthyroidism
was reported in 7 patients (41%) with HCG >50,000 mIU/mL.
The fact that some patients, but not all with very high
levels of HCG, present with hyperthyroidism is thought
to be due to secondary modifications of HCG such as sialylation or glycosylation that can affect HCG bioactivity and
the sensitivity of the TSH receptor to HCG (5). Haddow et
al reported that in a series of 9562 pregnant women, TSH
was substantially suppressed when the ratio of HCG to TSH
was >200,000. In another series, Lockwood et al collected 69
serum samples with HCG > 200,000 IU/L and found a suppressed TSH in 100% of specimens with HCG concentrations
>400,000 IU/L (7). In general, it is accepted that 25,000 U/L
of HCG is roughly equivalent to 1 mU/L of TSH activity (3),
and although there is not a precise threshold at which HCG
causes hyperthyroidism, thyroid functions should be measured
in all patients with HCG >50,000 IU/L, regardless of the cause
of HCG excess (1, 8).
The primary treatment for paraneoplastic HCG secretion
consists of NSGCT-directed chemotherapy along with symptomatic treatment of hyperthyroidism. Chemotherapy may produce an initial HCG surge, and patients should be monitored
for signs of thyrotoxicosis or thyroid storm, but it is usually
followed by normalization of thyroid function if the underlying
disease is responsive to treatment (1, 3).
Oosting SF, de Hass EC, Links TP, de Bruin D, Sluiter WJ, de Jong IJ,
Hoekstra HJ, Sleijfer DT, Gietema JA. Prevalence of paraneoplastic hyperthyroidism in patients with metastatic non-seminomatous germ-cell
tumors. Ann Oncol 2010;21(1):104–108.
2. Clain HJ, Pannall PR, Kotasek D, Norman RJ. Choriogonadotropinmediated thyrotoxicosis in a man. Clin Chem 1991;37(6):1127–1131.
3. Meister LH, Hauck PR, Graf H. Hyperthyroidism due to secretion of
human chorionic gonadotropin in a patient with metastatic choriocarcinoma. Arq Bras Endocrinol Metabol 2005;49(2):319–322.
4. Hershman JM. Physiological and pathological aspects of the effect of human chorionic gonadotropin on the thyroid. Best Pract Res Clin Endocrinol
Metab 2004;18(2):249–265.
5. Kohler S, Tschopp O, Jacky E. Paraneoplastic hyperthyroidism. BMJ Case
Rep 2011;2011:1–3.
6. Goldman L, Schafer AI. Testicular cancer. In Goldman L, Schafer AI, eds.
Goldman-Cecil Medicine, 25th ed. New York: Elsevier, 2016.
7. Lockwood CM, Grenache
DG, Gronowski AM. SeTable 1. Follow-up laboratory results during hospitalization
rum human chorionic gonadotropin concentrations
1 week after 3 weeks after
greater than 400,000 IU/L
completion of completion of
are invariably associated
first cycle of
first cycle of
Reference
Upon
with suppressed serum thyvalues
presentation chemotherapy chemotherapy
rotropin concentrations.
Thyroid 2009;19(8):863–
1–5
616,433
419,664
22,240
β-human chorionic gonadotropin, quantitative (MIU/mL)
868.
Thyroid-stimulating hormone (mcIU/mL)
0.27–4.20
<0.01
0.01
0.25
8. Heda P, Cushing G. Testicular choriocarcinoma presentFree thyroxine (ng/dL)
0.93–1.7
4.14
2.15
1.03
ing as hyperthyroidism. Am
Free triiodothyronine (pg/mL)
2.3–4.2
10.6
1.97
1.70
J Med 2013;126(11):e1–e2.
January 2016
1.
Choriocarcinoma presenting with thyrotoxicosis
43
Kidney stones and crushed bones secondary
to hyperparathyroidism
K. P. Sreelesh, MD, G. Nair Sreejith, DNB, DM, and K. Prabhakaran Pranab, MD
a
b
Here we report a 65-year-old woman with multiple
brown tumors and renal stones secondary to primary
hyperparathyroidism. This case highlights the need
for early recognition of parathyroid hyperactivity.
CASE DESCRIPTION
A 65-year-old postmenopausal Indian
woman with no notable medical history presented with progressive height loss over 5 years.
She denied bone pain, abdominal pain, hematuria, or mental status changes. Examination
revealed severe kyphoscoliosis and a 2 × 2 cm
anterior neck mass which rose with swallowing.
c
d
Plain films of the left hand revealed subperiosteal bone resorption (Figure 1a). Chest x-ray
showed kyphoscoliosis and irregular lytic lesions
with septae in the humeral region bilaterally consistent with multiple brown tumors (Figure 1b).
Dense opacity in the left lumbar region was suggestive of staghorn calculus (Figure 1b). Lateral
views of the skull showed a widened cortex (Figure 1c). Multiple vertebral compressions were
seen in the lumbar spine, with brown tumors
in the pelvis (Figure 1d). Laboratory evaluation
showed hypercalcemia with a serum calcium
level of 3.67 mmol/L (normal 2.05–2.55) and
a highly elevated serum intact parathyroid hormone level of 3566 ng/L (normal 10–65). Her Figure 1. Patient imaging. (a) Radiograph of hands showing subperiosteal bone resorption (arrows).
serum creatinine level was 0.8 mg/dL, and se- (b) Chest radiograph revealing the brown tumors (arrows) and renal calculi (arrowheads). (c) Lateral
rum 25-hydroxyvitamin D, 20 ng/mL (normal radiograph of the skull showing widened cortex (arrows). (d) Abdominal radiograph showing brown
14–60). Ultrasound of the neck showed a solid tumors in the pelvis (white arrows).
mass posterior to the thyroid gland measuring
2 × 2 cm with increased uptake on technetium-99m–labeled sesin developed countries (1), but such cases may still be found
tamibi scintigraphy, which was consistent with the diagnosis of a
in developing countries like India. Our patient had classical
right inferior parathyroid gland adenoma. Our patient was referred
for surgical resection but refused.
From the Department of Medical Oncology, Regional Cancer Centre,
DISCUSSION
Primary hyperparathyroidism with such severe bony
destruction and heavy renal calculi burden is rarely observed
44
Thiruvananthapuram, Kerala, India.
Corresponding author: K. P. Sreelesh, MD, Department of Medical Oncology,
Regional Cancer Centre, Thiruvananthapuram-695011, Kerala, India (e-mail:
sreelukp@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):44–45
parathyroid bone disease and renal disease. The bone manifestations in severe primary hyperparathyroidism, known
collectively as osteitis fibrosa cystica, may include bone pain,
skeletal deformity, pathological long bone fractures, and brown
tumors (2). Bone mineral density is usually extremely low, but
is reversible with surgical resection of the tumor. The brown
tumors are formed due to excess osteoclast recruitment and
activation. The characteristic brown color is due to the presence
of old hemorrhages into the lesion. Multiple brown tumors
may co-occur, mimicking the appearance of metastatic lytic
lesions (3). Renal involvement was present in 60% to 70% of
patients prior to 1970. With earlier detection, renal complications have occurred in <20% of patients in many recent series
(4). In occasional patients, repeated episodes of nephrolithiasis
January 2016
may lead to urinary tract obstruction, infection, and loss of
renal function (5).
1.
2.
3.
4.
5.
Marcocci C, Cetani F. Primary hyperparathyroidism. N Engl J Med
2011;365(25):2389–2397.
Bandeira F, Cusano NE, Silva BC, Cassibba S, Almeida CB, Machado
VC, Bilezikian JP. Bone disease in primary hyperparathyroidism. Arq Bras
Endocrinol Metabol 2014;58(5):553–561.
Meydan N, Barutca S, Guney E, Boylu S, Savk O, Culhaci N, Ayhan
M. Brown tumors mimicking bone metastases. J Natl Med Assoc
2006;98(6):950–953.
Mihai R, Farndon JR. Parathyroid disease and calcium metabolism. Br J
Anaesth 2000;85(1):29–43.
Lila AR, Sarathi V, Jagtap V, Bandgar T, Menon PS, Shah NS. Renal
manifestations of primary hyperparathyroidism. Indian J Endocrinol Metab
2012;16(2):258–262.
Kidney stones and crushed bones secondary to hyperparathyroidism
45
Successful treatment of pegaspargase-induced acute
hepatotoxicity with vitamin B complex and L-carnitine
Gary Lu, MD, PhD, Vinit Karur, MD, PhD, Jon D. Herrington, PharmD, and Mary G. Walker, MD
Pegaspargase is a chemotherapy drug used in the treatment of acute
lymphoblastic leukemia (ALL). One of the adverse effects of pegaspargase
is hepatotoxicity, which can rapidly lead to liver failure and death. We
report a patient with ALL who developed pegaspargase-induced severe
hepatotoxicity that was rescued by treatment with vitamin B complex
and L-carnitine. Our patient had a quicker response than prior reported
cases, suggesting this treatment might be a better regimen.
A
cute lymphoblastic leukemia (ALL) in young adults is
frequently treated with pediatric-inspired multiagent
chemotherapy. Some of these treatments include asparaginase as an integral part of the regimen. Asparaginase
has a significant adverse effect profile, including risk of thrombosis, bleeding, pancreatic hypersensitivity, and hepatotoxicity.
Asparaginase toxicity on the liver can be quite severe and may
produce a rapid functional decline and even lead to death (1).
Typical therapy for this adverse event is supportive care. We
report a patient with ALL who developed pegaspargase-induced
severe hepatotoxicity that dramatically recovered after treatment
with a regimen of vitamin B complex and L-carnitine.
CASE REPORT
A 23-year-old man with precursor B-cell ALL was treated
with an induction chemotherapy regimen of augmented Berlin-Frankfurt-Münster. This pediatric regimen includes weekly
doxorubicin at 25 mg/m2, weekly vincristine at 2 mg for three
doses, one dose of pegaspargase at 2500 unit/m2 (intravenous,
on day 4), and prednisone at 60 mg twice daily for 1 month.
The patient also received prednisone and palonosetron. On day
8, his total bilirubin level started to increase from a baseline of
0.8 mg/dL, gradually reaching 13.5 mg/dL on day 22. Over
the same time period, his international normalized ratio also increased from 1.1 to 1.9. Subsequently, his alkaline phosphatase,
aspartate aminotransferase, and alanine aminotransferase rose to
495 U/L, 150 U/L, and 416 U/L, respectively, on days 27 to 29.
He did not develop encephalopathy or ascites. He had no history of smoking, drinking alcohol, or using recreational drugs.
His body mass index and his fasting cholesterol level were within
normal limits. Testing for viral hepatitis A, B, and C, herpes
simplex virus, human immunodeficiency virus, Epstein-Barr
46
a
b
Figure 1. (a) Total bilirubin and (b) alkaline phosphatase, aspartate aminotransferase, and alanine aminotransferase values after treatment. The arrow on day 4
indicates one dose of pegaspargase, and the 11 arrows on days 20 to 31 indicate
administration of vitamin B complex and L-carnitine.
virus, cytomegalovirus, parvovirus B19, mononucleosis screen,
and bacterial infections was negative. Abdominal ultrasound
with Doppler revealed no venoocclusive disease. An abdominal
computed tomography (CT) scan revealed an enlarged steatotic
liver with normal gallbladder.
Vitamin B complex (Dialyvite; one tablet containing vitamin C 100 mg, thiamine 1.5 mg, riboflavin B2 1.7 mg, niacin
20 mg, pantothenic acid 10 mg, vitamin B6 10 mg, folic acid
1 mg, vitamin B12 6 mcg, and biotin 300 mcg), one tablet twice
daily, and intravenous levocarnitine 75 mg/kg every 4 hours
were started on day 20 and continued for 11 days. The patient’s
From the Department of Hematology/Oncology, Division of Internal Medicine,
Baylor Scott & White Health, Temple, Texas.
Corresponding author: Gary Lu, MD, PhD, Baylor Scott & White Health, 2401
South 31st Street, Temple, TX 76508 (e-mail: galu@sw.org).
Proc (Bayl Univ Med Cent) 2016;29(1):46–47
these two classes of medications
are similar and involve drugrelated mitochondrial toxicities.
L-carnitine and vitamin B complex are mitochondrial cofactors.
By supplementing these cofactors, the mitochondrial toxicities
can be corrected (5, 6). Only one
case report describes how asparaginase-related liver dysfunction
can be managed by a combination of L-carnitine and vitamin B
Figure 2. Liver CT, under liver window, showing fatty liver, induced by aspargase, (a) at day 14 and (b) resolved
complex (6). Overall, we believe
2 months later.
that the vitamin B complex and
levocarnitine regimen may be an effective and safe therapy for
total bilirubin level started to decrease 3 days after treatment.
pegaspargase-induced hepatotoxicity.
Within 1 week, his total bilirubin level was 4.6 mg/dL, and it
normalized on day 40. Simultaneously, his transaminase and
1. Bodmer M, Sulz M, Stadlmann S, Droll A, Terracciano L, Krähenbühl S.
prothrombin time also normalized, as shown in Figure 1. A CT
Fatal liver failure in an adult patient with acute lymphoblastic leukemia
scan 2 months later showed a resolution of fatty liver (Figure 2).
a
b
DISCUSSION
Asparaginase, a major drug component in the therapy for
ALL, depletes the circulating asparagine pool, thereby inhibiting protein synthesis and producing apoptosis (2). Administration of asparaginase in all dosages has been associated with
disturbance of hepatic function and lipid metabolism (3). An
asparaginase dosing strategy based on its pharmacokinetic characteristics in adults has been reported (4), but 20% of patients
with this regimen have to discontinue their treatment due to
severe hepatic toxicities. L-carnitine and vitamin B complex
have been used in the treatment of nucleoside reverse transcriptase inhibitor–induced mitochondrial toxicities with success
(5). The underlying mechanisms of hepatotoxicity induced by
January 2016
2.
3.
4.
5.
6.
following treatment with L-asparaginase. Digestion 2006;74(1):28–32.
Pui CH, Evans WE. Treatment of acute lymphoblastic leukemia. N Engl
J Med 2006;354(2):166–178.
Whitecar JP Jr, Bodey GP, Harris JE, Freireich EJ. L-asparaginase. N Engl
J Med 1970;282(13):732–734.
Douer D, Aldoss I, Lunning MA, Burke PW, Ramezani L, Mark L,
Vrona J, Park JH, Tallman MS, Avramis VI, Pullarkat V, Mohrbacher
AM. Pharmacokinetics-based integration of multiple doses of intravenous
pegaspargase in a pediatric regimen for adults with newly diagnosed acute
lymphoblastic leukemia. J Clin Oncol 2014;32(9):905–911.
Brinkman K, Vrouenraets S, Kauffmann R, Weigel H, Frissen J. Treatment
of nucleoside reverse transcriptase inhibitor-induced lactic acidosis. AIDS
2000;14(17):2801–2802.
Al-Nawakil C1, Willems L, Mauprivez C, Laffy B, Benm’rad M, Tamburini J, Fontaine H, Sogni P, Terris B, Bouscary D, Moachon L. Successful
treatment of L-asparaginase–induced severe acute hepatotoxicity using
mitochondrial cofactors. Leuk Lymphoma 2014;55(7):1670–1674.
Successful treatment of pegaspargase-induced acute hepatotoxicity with vitamin B complex and L-carnitine
47
Recurrent lumbosacral herpes simplex virus infection
Janna M. Vassantachart, BS, and Alan Menter, MD
We present the case of a 54-year-old white woman with episodic lumbosacral lesions that she had been treating as psoriasis. Evaluation revealed
classic herpes simplex virus (HSV) infection. The discussion reviews the
significance and potential complications of recurrent lumbosacral HSV
infection.
H
erpes simplex virus (HSV) is a DNA virus responsible
for recurrent skin infections presenting with clusters of
fluid-filled vesicles on an erythematous base. The lesion
forms a characteristic scalloped border as the vesicles
progress to crusting, erosions, and/or ulcerations. The lesions
usually resolve fully in 2 to 4 weeks, frequently leaving a residual
area of discoloration at the site of involvement. The virus infects
a susceptible person through contact with mucous membranes
or open, abraded skin. Most infections are recurrent, with subsequent episodes reappearing at or near the same anatomical
location due to the viral invasion, latency, and reactivation within
sensory dorsal root ganglions. The outbreaks can be triggered by
trauma, ultraviolet light, temperature extremes, emotional stress,
or immunosuppression (1).
CASE PRESENTATION
A 54-year-old white woman presented to our dermatology
clinic for her biannual skin evaluation. She had a history of
rosacea and psoriasis, but no personal or family history of skin
cancer. She had previously been on doxycycline for her rosacea
with an evident flare since being taken off the month prior to her
evaluation due to high liver enzymes. She was given a prescription for topical ivermectin 1% to apply to her face once a day.
Her psoriasis was adequately controlled with clobetasone spray
1 to 2 times per day applied regularly to her arms, scalp, and
legs. The patient stated that she also used the spray on her lower
back when she had a “psoriasis” flare with less than adequate
response in that region. On direct questioning, she stated that
the episodes on her back were associated with an initial burning
sensation in addition to being more painful and tender than
the rest of her psoriasis plaques.
Examination of the face revealed moderate erythema and
telangiectasia with accompanying papules on her cheeks and
nose, typical of rosacea. The patient also had scattered psoriasis
48
Figure 1. Location and presentation of two lumbosacral clusters of vesicles in
different stages of development and healing.
scaly plaques on her arms and occipital scalp. Evaluation of the
patient’s lumbosacral region revealed two well-circumscribed
clusters of small vesicles to the left of midline (Figure 1). The
cluster directly at the base of her spine measured 15 × 10 mm
and showed crusts and scabbed, deroofed vesicles. The cluster to
the left measured 15 × 15 mm and showed multiple thin-walled
fluid-filled vesicles on an erythematous base. These findings
were indicative of HSV infection with a characteristic history
of prelesion “burning” symptoms and recurrences in the same
anatomical area.
DISCUSSION
HSV is categorized as type 1 and 2 viruses which typically
cause infections on the oral and genital mucosa, respectively
(2). HSV-2 causes 70% to 90% of genital herpes infections
(3). Nonoral and nongenital sites are not infrequently involved,
possibly due to self-inoculation, primary acquisition, or viremic
spread (4). Although recurrences predominantly occur at the
same location, studies have shown that 21% of patients with
From Loma Linda University School of Medicine, Loma Linda, California
(Vassantachart), and the Division of Dermatology, Baylor University Medical
Center at Dallas (Menter).
Corresponding author: Alan Menter, MD, Baylor University Medical Center,
3900 Junius Street, Suite 125, Dallas, TX 75246 (e-mail: amderm@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):48–49
Figure 2. Distribution of sacral nerve ganglia dermatomes within the perineal
region.
primary genital herpes develop nongenital involvement (5).
The sites most often affected are the lumbosacral area and legs,
as the pudendal nerve which innervates the external genitalia
originates from the sacral nerve ganglia of S2-4 (Figure 2) (5–7).
With evidence of genital herpes recurrence at nongenital
sites, patients with primary infection should be counseled to
look for the development of lesions in the sacral ganglia distribution, as in our patient. On the other hand, patients with
nongenital herpes should also be evaluated for genital herpes.
Patients should be warned of viral shedding from the genital
area, as data have shown concomitant shedding with reactivation in the buttock area even in the absence of active genital
lesions (8). To minimize transmission of infection, patients are
counseled to avoid sexual contact during recurrences (8). The
viral shedding also raises concern for neonatal herpes infection
during delivery. Women most commonly shed from the vulva,
cervix, and perianal areas, and genital shedding at delivery causes
a 300-fold higher risk of transmitting the virus (9, 10).
Palliative or bedridden patients are at additional risk for
HSV. Although macerated dermatitis, Candida infections,
and pressure sores are most commonly seen in the posterior
lower body area, a lesion that does not heal despite appropriate treatment should be assessed for HSV-2. Early detection
and management can decrease complications and pain (11).
Recurrences of HSV-2 lesions on the buttocks occur less
frequently than genital recurrences but tend to last longer,
January 2016
thus making intermittent rather than suppressive therapy
possible (5).
Our patient noted that the episodes on her lower back occurred approximately once or twice a year. While the pain usually subsided within a few weeks, the lesions themselves took up
to 2 to 3 months to completely heal. The recurrences had been
occurring for many years with no patient recall of ever having
genital lesions. She had a hysterectomy several years previously.
The patient was prescribed valacyclovir, and her obstetrician
was notified of her condition. Prophylactic treatment was not
recommended, and the patient was advised to take valacyclovir
at the very first sign of a flare, particularly early stinging or
burning in the lumbosacral region.
1.
Mendoza N, Madkan V, Sra K, Willison B, Morrison LK, Tyring SK.
Human herpesviruses. In Bolognia JL, Schaffer JV, eds. Dermatology.
London: Elsevier Saunders, 2012.
2. Lafferty WE, Coombs RW, Benedetti J, Critchlow C, Corey L. Recurrences after oral and genital herpes simplex virus infection. Influence of
site of infection and viral type. N Engl J Med 1987;316(23):1444–1449.
3. Nahmias AJ, Lee FK, Beckman-Nahmias S. Sero-epidemiological and
-sociological patterns of herpes simplex virus infection in the world. Scand
J Infect Dis Suppl 1990;69:19–36.
4. Corey L, Spear PG. Infections with herpes simplex viruses (1). N Engl J
Med 1986;314(11):686–691.
5. Benedetti JK, Zeh J, Selke S, Corey L. Frequency and reactivation of
nongenital lesions among patients with genital herpes simplex virus. Am
J Med 1995;98(3):237–242.
6. Shafik A, el-Sherif M, Youssef A, Olfat ES. Surgical anatomy of the pudendal nerve and its clinical implications. Clin Anat 1995;8(2):110–115.
7. Perry CP. Somatic referral. In Howard F, Perry C, Carter J, El-Minawi
A, eds. Pelvic Pain: Diagnosis and Management. Philadelphia: Lippincott
Williams & Wilkins, 2000.
8. Kerkering K, Gardella C, Selke S, Krantz E, Corey L, Wald A. Isolation of
herpes simplex virus from the genital tract during symptomatic recurrence
on the buttocks. Obstet Gynecol 2006;108(4):947–952.
9. Brown ZA, Wald A, Morrow RA, Selke S, Zeh J, Corey L. Effect of serologic status and cesarean delivery on transmission rates of herpes simplex
virus from mother to infant. JAMA 2003;289(2):203–209.
10. Gupta R, Wald A, Krantz E, Selke S, Warren T, Vargas-Cortes M, Miller G,
Corey L. Valacyclovir and acyclovir for suppression of shedding of herpes
simplex virus in the genital tract. J Infect Dis 2004;190(8):1374–1381.
11. Toutous-Trellu L, Vantieghem KM, Terumalai K, Herrmann FR, Piguet
V, Kaiser L, Vuagnat H, Zulian G. Cutaneous lumbosacral herpes simplex
virus among patients hospitalized for an advanced disease. J Eur Acad
Dermatol Venereol 2012;26(4):417–422.
Recurrent lumbosacral herpes simplex virus infection
49
Disseminated cutaneous histoplasmosis in newly
diagnosed HIV
Gabriela M. Soza, BS, Mahir Patel, MD, Allison Readinger, MD, and Caitriona Ryan, MD
We present a woman with a widespread
severe papulopustular eruption, fever,
and fatigue of 5 weeks’ duration. HIV infection was diagnosed, with an absolute
CD4+ count of 3 cells/μL. The eruption
was consistent with disseminated cutaneous histoplasmosis. The clinical manifestations and management of cutaneous
histoplasmosis are reviewed.
a
b
CASE DESCRIPTION
A 55-year-old white woman
presented to the emergency department reporting a rash of 5 weeks’
duration, severe fatigue, and a fever.
Initially the rash was present on a
localized area of her back, but it
rapidly progressed to involve her
trunk, face, arms, and legs. She had
presented to the emergency department on four separate occasions and Figure 1. (a) The truck showing scattered erythematous papules and plaques with central necrosis and ulceration
was prescribed multiple courses of and some cases of secondary impetiginization. (b) A few larger plaques on the left shoulder.
antibiotics, antihistamines, and corticosteroids without significant improvement. Review of systems
showed multifocal nodular opacities and mediastinal lymphwas negative for cough, myalgias, arthralgias, and weight loss.
adenopathy. The patient was initiated on intravenous liposomal
+
A rapid HIV test was positive with an absolute CD4 count
amphotericin B for histoplasmosis and antiretroviral therapy for
HIV. Itraconazole was commenced a few days later for long-term
of 3 cells/μL.
treatment of histoplasmosis. Amphotericin B was discontinOn examination, the patient had a widespread papulopusued after 3 weeks due to acute kidney injury, and voriconazole
tular eruption with lesions coalescing into necrotic plaques with
was substituted for itraconazole due to concomitant infection
central ulceration over the trunk and extremities. There was
with Sporothrix schenckii. There was considerable improvement
secondary impetiginization in places (Figure 1). Punch biopof the cutaneous lesions, and 1 month after discharge the pasies were obtained for histopathologic examination and culture
tient was recommenced on itraconazole for her histoplasmosis.
(Figure 2).
Histopathology revealed dermal parasitized macrophages
with small intracytoplasmic round organisms with surroundFrom the Texas A&M College of Medicine, Bryan, Texas (Soza), and the Department
ing mild chronic inflammation. Stains demonstrated periodic
of Dermatology, Baylor University Medical Center at Dallas, Dallas, Texas (Patel,
acid-Schiff (PAS)–positive and Gomori methenamine silver
Readinger, Ryan).
(GMS)–positive yeast within macrophages in the dermis, conCorresponding author: Caitriona Ryan, MD, Department of Dermatology, Baylor
sistent with histoplasmosis. A Fungitell blood test (1,3 beta-DUniversity Medical Center, 3900 Junius Street, Suite 145, Dallas, TX 75246
glucan) was positive. Computed tomography (CT) of the chest
(e-mail: Caitrionaryan80@gmail.com).
50
Proc (Bayl Univ Med Cent) 2016;29(1):50–51
with varying degrees of respiratory, hepatic, and reticuloendothelial system
involvement (3).
The nonspecific skin lesions in
disseminated cutaneous histoplasmosis (DCH) can make the diagnosis
challenging; thus, a high index of suspicion is necessary. Histopathologic
examination of cutaneous lesions is
the gold standard diagnostic test, in
combination with culture, and is
done using special stains including
PAS and GMS. These stains highlight
numerous intracellular yeast forms 2
to 4 μm in diameter that fill a macrophage and appear as basophilic dots
with a pseudocapsule (2, 4). There
are a wide variety of histopathologic
features, such as necrotizing “tuberculoid” and nonnecrotizing granuFigure 2. Punch biopsy from a vesicle on the back. (a) Superficial dermal and perivascular diffuse histiocytic infiltrate
lomas with small intracellular yeasts,
(hematoxylin and eosin [H&E], original magnification ×40). (b) Superficial dermis filled with parasitized macrophages
diffuse dermal histiocytosis, and difwith small round organisms stuffing their cytoplasm (H&E, original magnification ×200).
fuse dermal karyorrhexis (2). This appearance of karyorrhexis may mimic
leukocytoclastic
vasculitis
at first glance (4, 5). These varied
After 3 months of follow-up, the patient had minimal scattered
findings, in addition to the range of clinical manifestations in
papules and pustules on the face and extremities.
DCH, demonstrate a wide spectrum of reaction patterns in this
AIDS-defining illness (2).
DISCUSSION
Histoplasma antigen detection, which can be performed on
Histoplasmosis, the most common endemic mycosis in
samples of urine, serum, cerebrospinal fluid, and bronchoalAIDS patients, is caused by the dimorphic fungus H. capsuveolar lavage fluid, is the most sensitive method of diagnosing
latum, a primary pathogen that can cause opportunistic infecdisseminated disease (1). Radiographic imaging should be pertions in immunocompromised hosts. In the United States, it is
formed to assess for pulmonary involvement, although initial
prevalent in the Mississippi and Ohio River valleys; worldwide
radiographs may be normal. Common radiographic findings
it is endemic in areas of Mexico, Central and South America,
include diffuse interstitial or reticulonodular infiltrates, while
Africa, and Asia. The fungus is found in soil enriched with
pleural effusions, mediastinal adenopathy, and calcified granubird or bat excreta and is acquired via inhalation of microcolomas can also be observed (3).
nidia into the alveoli, where they convert to the yeast form.
In immunocompetent hosts, histoplasmosis can present as a
1. Chang P, Rodas C. Skin lesions in histoplasmosis. Clin Dermatol
self-limiting illness (1). Patients with advanced AIDS and CD4
2012;30(6):592–598.
lymphocyte counts <100 cells/μL typically present with a more
2. Ramdial PK, Mosam A, Dlova NC, B Satar N, Aboobaker J, Singh SM.
severe, wasting presentation of the disease.
Disseminated cutaneous histoplasmosis in patients infected with human
Histoplasmosis has been described in three different forms:
immunodeficiency virus. J Cutan Pathol 2002;29(4):215–225.
acute pulmonary, chronic cavitary, and disseminated histoplas3. Wheat LJ, Connolly-Stringfield PA, Baker RL, Curfman MF, Eads ME,
Israel KS, Norris SA, Webb DH, Zeckel ML. Disseminated histoplasmosis. Of the disseminated cases, 10% to 25% have a wide specmosis in the acquired immune deficiency syndrome: clinical findings,
trum of mucocutaneous manifestations (2). These polymorphous
diagnosis and treatment, and review of the literature. Medicine (Baltimore)
lesions include erythematous macules and papules, plaques,
1990;69(6):361–374.
nodules, ulcers, pustules, acneiform eruptions, molluscum-like
4. Eidbo J, Sanchez RL, Tschen JA, Ellner KM. Cutaneous manifestations of
lesions, and generalized dermatitis. Varying morphologic presenhistoplasmosis in the acquired immune deficiency syndrome. Am J Surg
Pathol 1993;17(2):110–116.
tations can occur in a patient, with the face, oropharynx, extremi5.
Grayson
W. The HIV-positive skin biopsy. J Clin Pathol 2008;61(7):802–
ties, and trunk most commonly affected (1). Nonspecific findings
817.
such as fever and weight loss, cough, and dyspnea are common,
a
January 2016
b
Disseminated cutaneous histoplasmosis in newly diagnosed HIV
51
Disseminated Kaposi sarcoma with osseous metastases
in an HIV-positive patient
Bruce M. Bell Jr., MD, Almas Syed, MD, Susanne W. Carmack, MD, Cody A. Thomas, MD, and Kennith F. Layton, MD
Kaposi sarcoma is a neoplasm commonly associated with human herpesvirus 8 and HIV/AIDS. We present a 44-year-old African immigrant
woman who presented to the emergency department after several months
of abdominal pain. She was found to be HIV positive, and computed tomography demonstrated numerous lesions of the lungs, liver, and spleen,
gastric wall thickening, and several lytic lesions of the spine. Fluoroscopyguided biopsy of a lytic lesion of the spine yielded the diagnosis of Kaposi
sarcoma. AIDS-related Kaposi sarcoma with osseous involvement is rare,
with approximately 30 cases reported in the literature. When osteolytic
lesions are encountered in an HIV-positive patient, Kaposi sarcoma should
remain in the differential.
K
aposi sarcoma (KS) is a neoplasm consisting of fibrosarcoma-like cells and capillaries and is commonly associated with human herpesvirus 8 and HIV/AIDS (1, 2).
AIDS-related KS with osseous involvement is rare, with
approximately 30 cases reported in the literature. We present an
HIV-positive woman from East Africa with disseminated KS
with several lytic lesions in the spine.
CASE REPORT
A 44-year-old female East African immigrant without
significant past medical history presented to the emergency
department with several months of diffuse abdominal pain,
anorexia, and significant weight loss. A computed tomography
(CT) scan of the abdomen and pelvis demonstrated gastric
wall thickening with numerous subcentimeter hepatic, splenic,
and pulmonary lesions (Figure 1a, 1b). There were also small
scattered lytic lesions in the thoracolumbar spine (Figure 1c)
compatible with metastatic disease with concern for a primary
gastric malignancy. Endoscopic biopsy of the stomach revealed
severe chronic gastritis but no evidence of malignancy. Additionally, the patient was found to be HIV positive. Brain
magnetic resonance imaging (MRI) demonstrated abnormal
bone marrow signal within the calvarium (Figure 2) that was
also compatible with metastatic disease. An ultrasound-guided
core needle biopsy of the liver lesions was unsuccessful due to
the small size and location. A fluoroscopy-guided core needle
biopsy of the L1 lesion was successful and yielded a histologic
diagnosis of KS (Figure 3). No cutaneous lesions were reported.
52
Of note, the patient’s CD4 count was 5 cells/μL and viral load
was 2.5 million copies/mL. The patient was started on highly
active antiretroviral therapy (HAART) prior to discharge. She
is reportedly undergoing further therapy at an outside hospital.
DISCUSSION
KS is an angioproliferative mesenchymal neoplasm first
described by the Hungarian dermatologist Dr. Moritz Kaposi
in 1872. There are four major clinical variants of KS: 1) classic,
2) African endemic, 3) immunosuppression associated, and
4) AIDS-related. AIDS-related KS differs clinically from the
classical and endemic variants (3). Classical KS typically presents with cutaneous involvement of the lower extremities and is
predominantly seen in elderly men of Jewish and Mediterranean
descent (4). AIDS-related KS is more widespread and aggressive.
While KS can be seen at any stage of HIV infection, advanced
disease with multifocal involvement usually occurs with a CD4
count <200 cells/μL (5).
AIDS-related KS is generally multifocal and most often
involves the skin, oral mucosa, lymph nodes, gastrointestinal tract, lungs, liver, and spleen (5). Osseous involvement
of AIDS-related KS is rare, but when it does occur, the axial
skeleton is most often affected (5). In a recent literature review
of 66 patients with KS of the musculoskeletal system conducted
by Caponetti et al, 27 patients had osseous KS of the AIDSrelated variant. Of these 27 patients, 22 had axial skeleton involvement, four appendicular, and one both. Of the 22 patients
with axial skeleton involvement, 10 patients had involvement
of the spine (6). It was previously recognized that osseous KS
lesions are in general the result of contiguous invasion from a
nonosseous lesion (7). However, of the 10 cases of osseous KS
involving the spine from the Caponetti et al literature review,
there were no reports of extension from a nonosseous lesion
(6), which was also true of our case.
Radiographically, typical features of osseous KS include cortical erosion, osteolysis, and periosteal reaction. However, these
From the Departments of Radiology (Bell, Syed, Layton) and Pathology (Carmack,
Thomas), Baylor University Medical Center at Dallas.
Corresponding author: Bruce M. Bell Jr., MD, Department of Radiology, Baylor
University Medical Center, 3500 Gaston Avenue, Dallas, TX 75246 (e-mail: bruce.
bell@baylorhealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):52–54
a
b
c
Figure 1. CT images. (a) Transaxial contrast-enhanced CT image of the upper abdomen demonstrating a single hypodense lesion in the posterior right lobe of the liver
(black arrow), a smaller hypodense lesion in the spleen (white arrow), and circumferential gastric wall thickening (white arrowheads), radiologically concerning for primary
gastric malignancy with hepatic and splenic metastases. Gastric biopsy was later diagnosed as Kaposi sarcoma. (b) Transaxial contrast-enhanced CT image of the lower
lung fields demonstrating numerous bilateral pulmonary nodules (black arrow) compatible with metastatic disease. (c) Coronal CT image of the abdomen and pelvis demonstrating a hypodense lesion within the right lateral aspect of the L1 vertebral body (white arrow). There is a second smaller, more subtle lesion in the right lateral aspect
of the L4 vertebral body. Radiologically, these lesions are concerning for metastatic disease. The L1 lesion was biopsied, with histology demonstrating Kaposi sarcoma.
changes are not generally appreciated on spine radiographs. On
CT imaging, lytic bone lesions are typical with potential osteoblastic changes. In our case and the 10 cases from the Caponetti
et al review, the spinal lesions were purely osteolytic. MRI may
demonstrate nonspecific marrow signal abnormalities, as in
our case. MRI better demonstrates potential adjacent soft tissue lesions. The above findings are nonspecific and can be seen
with lymphoma and osteomyelitis, which are top differential
diagnoses for osteolytic lesions in HIV/AIDS patients (8).
Sequential thallium-201 and gallium-67 nuclear medicine
studies can be useful to differentiate KS from lymphoma and
osteomyelitis. KS will typically demonstrate uptake on the thallium-201 scan but no uptake on the gallium-67 scan. Lymphoma and osteomyelitis are typically gallium-67-avid and
demonstrate uptake (1).
KS is the most common AIDS-defining malignancy (4). A
low CD4 count (<200 cell/mm3) and elevated HIV RNA are
strong predictors of KS (9). In the age of HAART therapy, the
incidence of KS has decreased dramatically (10). However, when
the described radiological findings of the spine are encountered
a
b
Figure 2. Sagittal T1-weighted MRI image of the brain demonstrating hypointense
marrow signal within the calvarium, which was also concerning for metastatic
disease in light of the CT findings.
January 2016
Figure 3. L1 vertebra biopsy results. (a) Hematoxylin and eosin staining showing
an atypical spindle cell lesion. (b) Human herpesvirus 8 immunostain highlighting the neoplastic spindle cells. Findings are compatible with Kaposi sarcoma.
Disseminated Kaposi sarcoma with osseous metastases in an HIV-positive patient
53
in an HIV-positive patient, KS should remain in the differential.
Biopsy is necessary for definitive diagnosis (1).
1.
2.
3.
4.
5.
54
Thanos L, Mylona S, Kalioras V, Pomoni M, Batakis N. Osseous Kaposi
sarcoma in an HIV-positive patient. Skeletal Radiol 2004;33(4):241–243.
Yergiyev O, Mohanty A, Curran-Melendez S, Latona CR, Bhagavatula R,
Greenberg L, Silverman JF. Fine-needle aspiration cytology of disseminated
Kaposi sarcoma of the bone in an AIDS patient. Acta Cytol 2015;59(1):113–
117.
Tappero JW, Conant MA, Wolfe SF, Berger TG. Kaposi’s sarcoma. Epidemiology, pathogenesis, histology, clinical spectrum, staging criteria and
therapy. J Am Acad Dermatol 1993;28(3):371–395.
Nguyen C, Lander P, Begin LR, Jarzem P, Grad R. AIDS-related Kaposi
sarcoma involving the tarsal bones. Skeletal Radiol 1996;25(1):100–102.
Tehranzadeh J, Ter-Oganesyan RR, Steinbach LS. Musculoskeletal dis-
orders associated with HIV infection and AIDS. Part II: non-infectious
musculoskeletal conditions. Skeletal Radiol 2004;33(6):311–320.
6. Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz L. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer
2007;109(6):1040–1052.
7. Krishna G, Chitkara RK. Osseous Kaposi sarcoma. JAMA 2003;289(9):1106.
8. Mu A, Nassar N. A man with oral lesions, constipation and back pain.
Int J STD AIDS 2013;25(7):526–528.
9. Yanik EL, Napravnik S, Cole SR, Achenbach CJ, Gopal S, Olshan A,
Dittmer DP, Kitahata MM, Mugavero MJ, Saag M, Moore RD, Mayer
K, Mathews WC, Hunt PW, Rodriguez B, Eron JJ. Incidence and timing
of cancer in HIV-infected individuals following initiation of combination
antiretroviral therapy. Clin Infect Dis 2013;57(5):756–764.
10. Gopal S, Achenbach CJ, Yanik EL, Dittmer DP, Eron JJ, Engels EA. Moving
forward in HIV-associated cancer. J Clin Oncol 2014;32(9):876–880.
Baylor University Medical Center Proceedings
Volume 29, Number 1
A giant splenic hydatid cyst
Rikki Singal, MS, Karamjot Singh Sandhu, Amit Mittal, Samita Gupta, and Gunjan Jindal
A 16-year-old girl presented with pain in the left hypochondrium, which
had been progressing for 5 months. Examination revealed large splenomegaly, and ultrasonography showed a huge hydatid cyst in the spleen.
Preoperative planning and postoperative care lead to successful management of this entity. Radiological investigations also play a major role in
diagnosis and decrease morbidity.
E
chinococcosis (hydatid disease) primarily affects the liver;
however, secondary involvement due to hematogenous
dissemination may be seen in almost any anatomic
location. Isolated hydatid disease of the spleen is rare
(1, 2). It is caused by the larval form of the tapeworm Echinococcus granulosus, E. multilocularis, E. vogeli, or E. oligarthrus.
E. granulosus is the most common organism involved, with
dogs as the definitive host and sheep as an intermediate host.
Human beings exposed to certain stages of the life cycle of the
organism are also an intermediate host (3). Human hydatid
disease can involve the liver (55%–70%), lung (18%–35%),
spleen, kidney, peritoneal cavity, skin and muscles (<2%) and
rarely the remaining parts of the body (4–8).
CASE DESCRIPTION
A 16-year-old girl presented with a 5-month history of pain
in the left hypochondrium. The pain had progressively increased.
There was no jaundice, fever, abdominal distension, or bowel and
bladder symptoms. Examination revealed a distended abdomen
and a large palpable mass in the left hypochondrium. Ultrasonography showed a bulky hydatid cyst, measuring 12 × 8 cm,
entirely within the intact splenic capsule, situated at the hilum
of the engorged spleen with numerous daughter cysts within the
mother hydatid cyst. Computed tomography revealed a large
well-defined cystic lesion involving almost the entire spleen and
measuring 12 × 9 cm (Figure 1). Routine investigations were
within standard range, and her chest radiograph was normal.
A left subcostal incision was made and a large cyst was
found involving the spleen. The capsule of the spleen was intact
(Figure 2). The cyst was not adherent to the adjoining structures.
Splenic vessels were of normal dimension. Splenectomy was
completed in toto without rupture of the capsule and minimal
handling of the specimen. A cut section of the excised spleen
Proc (Bayl Univ Med Cent) 2016;29(1):55–57
Figure 1. Computed tomography scan revealing a large cyst in the spleen.
Figure 2. Operative picture showing the spleen with a yellowish color and a
tense cystic area.
From the Department of Surgery (Singal, Sandhu) and the Department of
Radiodiagnosis and Imaging (Mittal, Gupta, Jindal), Maharishi Markandeshwer
Institute of Medical Sciences and Research, Mullana (Distt-Ambala), Haryana, India.
Corresponding author: Rikki Singal, MS, Dr Kundan Lal Hospital, Ahmedgarh,
Distt-Sangrur, Punjab, Pin Code-148021, India (e-mail: singalsurgery@yahoo.com).
55
Figure 3. Gross specimen of the cyst and spleen and cut section showing multiple daughter cysts.
revealed a tense cyst with clear fluid (Figure 3). The diagnosis of
hydatid cyst was established on histopathological examination
of the specimen (Figure 4). Postoperatively, the patient received
a pneumococcal vaccine.
DISCUSSION
The liver, being the foremost sieve for the portal circulation
containing the ovum, is the most frequent site of hydatid invasion. The retrograde course of blood drained from the bowel
shipping echinococcus ova towards the spleen is believed to cause
the isolated splenic hydatid disease which spares the liver and
other organs. Arterial dissemination of the ovum, which is only
30 to 37 micron in size, is feasible if it escapes the liver and lung
filters (9). In such cases, it can lodge, differentiate, and develop
into cysts in almost any part of the body. Rupture of hydatid
cyst of the spleen may lead to an anaphylactic reaction. Harefuah
described a 20-year-old combatant who presented with anaphylactic shock due to rupture of a splenic echinococcal cyst induced
by blunt trauma to the left chest wall and upper abdomen (10).
Diagnosis of splenic hydatidosis on the basis of history and
clinical examination is often easier said than done. To reach
the diagnosis, different serological tests are needed, including
hydatid immunoelectrophoresis, enzyme-linked immunosorbent assay (ELISA), latex agglutination, and indirect hemagglutination test. The ELISA test has a sensitivity of about 90%
and a specificity of 90% for hepatic cysts, 55% for lung hydatid
disease, and 45% for hydatid disease in other organs. These
tests, however, may be negative because the capsule isolates the
parasite from the host’s immune system (11, 12).
Surgery, either open or laparoscopic, is the most commonly
used treatment. If cysts are inactive and superficial, located either
at the upper or lower poles of the spleen, then conservative surgical techniques, such as partial splenectomy, cyst enucleation,
deroofing with omentoplasty, internal drainage with cystojejunal
anastomosis, and external drainage can be done, for which a sufficient amount of splenic parenchyma will remain after surgery
(13, 14). Splenectomy is preferred in adults and is required when
the cyst is large. Limited excision of the spleen may be used
Figure 4. Histopathological examination showing an acellular fibrous wall of hydatid cyst, with a germinal layer and scolices in the center (×100).
56
Baylor University Medical Center Proceedings
Volume 29, Number 1
for younger patients who may have increased pneumococcal
infections following total splenectomy.
Intraoperatively, the use of scolicidal agents such as cetrimide,
hypertonic saline, alcohol, or 0.5% silver nitrate solution before
opening the cavities tends to kill the daughter cysts and prevent
further spread or anaphylactic reactions. Alcohol sclerosis of
hydatid cysts has proven to be a safe and effective therapeutic
option, with a reduction in size ranging from 73% to 99% (15).
Risks involved in treatment include perforation, infection, and
fistula formation. After treatment, screening and postoperative
follow-up for recurrence are required.
5.
6.
7.
8.
9.
10.
11.
1.
2.
3.
4.
Sharif MA, Mahmood A, Murtaza B, Malik IB, Khan A, Asghar Z,
Arif A. Primary perisplenic hydatid cyst. J Coll Physicians Surg Pak
2009;19(6):380–382.
Singal R, Goyal S, Goyal R, Mittal A, Gupta S. Primary splenic
hydatid cyst in a young boy—an uncommon entity. West Indian Med J
2011;60(3):374–376.
Kalinova K. Giant pseudocyst of the spleen: a case report and review of
the literature. J Indian Assoc Pediatr Surg 2005;10:176–178.
Sawarappa R, Kanoi A, Gupta M, Pai A, Khadri SI. Isolated splenic
hydatidosis. J Clin Diagn Res 2014;8(6):ND03–ND04.
January 2016
12.
13.
14.
15.
Kouskos E, Chatziantoniou J, Chrissafis I, Anitsakis C, Zamtrakis S. Uncommon locations of hydatid cysts. Singapore Med J 2007;48(4):e119–e121.
Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res 2014;4(3):447–452.
Pawar I, Mittal A, Bugga P, Aggarwal A. Large hydatid cyst in thigh: a rare
case with clinico-radio-pathological profile. J Musculoskel Res 2010;13:153.
Khoury G, Abiad F, Geagea T, Nabout G, Jabbour S. Laparoscopic treatment
of hydatid cysts of the liver and spleen. Surg Endosc 2000;14(3):243–245.
Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects
of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev
2004;17(1):107–135.
Gupta A, Singal RP, Gupta S, Singal R. Hydatid cyst of thigh diagnosed
on ultrasonography—a rare case report. J Med Life 2012;5(2):196–197.
Thambidurai L, Santhosham R, Dev B. Hydatid cyst: anywhere, everywhere. Radiol Case Rep 2011;6:486.
Dalal U, Dalal AK, Singal R, Naredi B, Gupta S. Primary hydatid cyst masquerading as pseudocyst of the pancreas with concomitant small gut obstruction—
an unusual presentation. Kaohsiung J Med Sci 2011;27(1):32–35.
Singal R, Dalal U, Dalal AK, Singh P, Gupta R. Subcutaneous hydatid
cyst of the thigh. South Med J 2010;103(9):965–966.
Malik AA, ul Bari S, Younis M, Wani KA, Rather AA. Primary splenic
hydatidosis. Indian J Gastroenterol 2011;30(4):175–177.
Rasheed K, Zargar SA, Telwani AA. Hydatid cyst of spleen: a diagnostic
challenge. N Am J Med Sci 2013;5(1):10–20.
A giant splenic hydatid cyst
57
Segmental ischemia in testicular torsion
Binnur Tavaslı, MD, Hikmet Köseoğlu, MD, and Halime Çevik, MD
Testicular torsion is a rare but important entity in the discipline of
urology, as urgent action is required to save the testicle anatomically
and functionally. Occurring mainly in the young prepubertal or pubertal male, testicular torsion is also seen in young adults. The annual
incidence has been estimated to be 4.5 cases per 100,000 male
subjects. The outcome of testicular torsion, in cases of unsuccessful
emergent intervention, is total or partial infarction of the testicular tissue. We present a case of partial testicular ischemia due to
testicular torsion.
T
esticular torsion, though rare, is mainly encountered
in emergency departments and requires urgent treatment. The annual incidence of testicular torsion has
been estimated to be 4.5 cases per 100,000 male subjects (1). Although it can be encountered in any age group, it
is mostly seen in males younger than 21 years and comparatively rarely in young adults (2, 3). The outcome of testicular
torsion, in cases of unsuccessful emergent intervention, is
total or partial infarction of the testicular tissue (4–9). Some
cases with partial ischemia, as in our case, can be challenging
to manage.
CASE PRESENTATION
A 25-year-old man was admitted to the emergency department with acute progressive left scrotal pain lasting
approximately 12 hours. His past medical history was unremarkable. Examination revealed normal scrotal skin, left
minimal hydrocele, and bilateral testicles in the scrotum
with minimal pain on the left side with palpation, without varicocele, testicular mass, or hernia. Complete blood
count, urinalysis, serum alpha-fetoprotein, and human
chorionic gonadotropin β subunit tests were normal. Color
Doppler ultrasonography of the scrotum revealed a normalsized testicle with thickened tunica albuginea and minimal
hydrocele on the left side. No arterial or venous blood flow
was detected in the left testicle, sparing only the superior
part (Figures 1a and 1b). Emergent surgical exploration with
a scrotal approach was performed. When the hydrocele was
incised, the cord was found to be twisted one total turn, with
bluish discoloration at the twist of the cord. After detorsion,
58
the discoloration on the cord was corrected. An ultrasound
24 hours postoperatively revealed normal echogenicity and
vascularity in the left testicle (Figure 1c).
DISCUSSION
Testicular torsion is rare but requires urgent action to
save the testicle (1). Before radiologic diagnostic tests were
available, 90% of these patients lost their testes, mostly due
to orchiectomy and rarely ischemic atrophy (4). The orchiectomy rate has declined to 2% to 34% in the era of advanced
imaging (1, 3). Th e timing of surgery after the onset of
testicular torsion is the most important parameter for saving
testicular tissue (5).
While color Doppler ultrasonography has high sensitivity
and specificity for testicular torsion, normal ultrasonography
can detect only about a quarter of the cases of testicular torsion among patients admitted to the clinic with acute scrotum
(6, 7). Therefore, although ultrasonography is helpful, high
clinical suspicion is still important for emergent surgical intervention in challenging cases. Some cases of testicular torsion
result in segmental testicular infarction (8, 9). In the rare
cases when segmental ischemia progresses to segmental testicular infarction, it is usually diagnosed following orchiectomy
(9). In these cases, the most common differential diagnosis
is testicular tumor, due to the ultrasonographic resemblance
of the two entities.
The time period of ischemia is an important factor in the
outcome of the patient with partial testicular ischemia resulting from torsion. The testis can be saved, but a longer period
of infarction results in either partial loss of testicular mass or
orchiectomy. In our case, the period of ischemia was approximately 12 hours, and the high suspicion of testicular torsion,
with testicular pain and uncommon partial ischemia of the
testis on Doppler ultrasonography, drove emergent surgical
intervention, which saved the testis.
From the Departments of Radiology (Tavaslı, Çevik) and Urology (Köseoğlu),
Başkent University, Istanbul, Turkey.
Corresponding author: Hikmet Köseoğlu, MD, Department of Urology, Başkent
University, Valide-i Atik Mah, Çinili Mescit Sok, Yıldız Apt. No:33 D:16, Istanbul,
Turkey (e-mail: hikmet.koseoglu@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):58–59
a
b
c
Figure 1. Color Doppler ultrasonography. (a) Preoperative image of both testes demonstrating absent flow in the left testis. (b) Preoperative image demonstrating minimal blood flow in the superior part of the left testis. (c) Image 24 hours postoperatively demonstrating uniform echogenicity and flow throughout
the left testicle.
1.
2.
3.
4.
5.
Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for
orchiectomy. Arch Pediatr Adolesc Med 2005;159(12):1167–1171.
Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion.
J Urol 2002;167(5):2109–2110.
Tajchner L, Larkin JO, Bourke MG, Waldron R, Barry K, Eustace PW.
Management of the acute scrotum in a district general hospital: 10-year
experience. ScientificWorldJournal 2009;28(9):281–286.
Barker K, Raper FP. Torsion of the testis. Br J Urol 1964;36:35–41.
King LM, Sekaran SK, Sauer D, Schwentker FN. Untwisting in delayed
treatment of torsion of the spermatic cord. J Urol 1974;112(2):217–221.
6.
7.
8.
9.
Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG. An analysis of
clinical outcomes using color Doppler testicular ultrasound for testicular
torsion. Pediatrics 2000;105(3 Pt 1):604–607.
Bentley DF, Ricchiuti DJ, Nasrallah PF, McMahon DR. Spermatic cord
torsion with preserved testis perfusion: initial anatomical observations.
J Urol 2004;172(6 Pt 1):2373–2376.
Costa M, Calleja R, Ball RY, Burgess N. Segmental testicular infarction.
BJU Int 1999;83(4):525.
Shen YH, Lin YW, Zhu XW, Cai BS, Li J, Zheng XY. Segmental testicular
infarction: a case report. Exp Ther Med 2015;9(3):758–760.
Avocations
Wildebeest migrating in enormous numbers through the Mara Triangle of the Maasai Mara National Reserve in Kenya in September 2014. A small number of Burchell’s
zebras can be seen in the foreground. This is a pan merger of five separate photographs. Photo copyright © Greg Dimijian, MD. Dr. Dimijian and his wife, Mary Beth,
are the authors of For the Love of Wild Places and Animal Watch: Behavior, Biology, and Beauty.
January 2016
Segmental ischemia in testicular torsion
59
Warfarin-induced skin necrosis following heparin-induced
thrombocytopenia
Bilal Fawaz, BS, Nicole M. Candelario, MD, Nicole Rochet, MD, Connie Tran, BA, and Cristina Brau, MD
Anticoagulants, such as heparin and warfarin, are commonly used in the
treatment and prevention of thromboembolic events. The risk of developing warfarin-induced skin necrosis (WISN) with warfarin is reported to be
<1%. However, the risk of WISN may be increased with the initiation of
warfarin in the setting of heparin-induced thrombocytopenia and thrombosis syndrome (HITT). WISN can lead to catastrophic tissue necrosis
requiring amputations and mass debridement. This report describes
a case of WISN following HITT and discusses the appropriate medical
management of patients with HITT to avoid secondary WISN.
W
arfarin is considered essential in the treatment of
various hypercoagulable conditions (1). However,
it is known to paradoxically cause hypercoagulable
conditions, including warfarin-induced skin necrosis
(WISN) and venous limb gangrene (1). These complications
rarely occur in the setting of warfarin therapy, but the risk of
developing them may be increased following heparin-induced
thrombocytopenia and thrombosis syndrome (HITT) (1). We
report the case of a 64-year-old woman who developed WISN
4 days following her diagnosis of HITT.
CASE REPORT
A 64-year-old Hispanic woman with a past medical history
of myocardial infarction, hypertension, and diabetes mellitus was
admitted to the hospital due to a non–ST elevation myocardial
infarction. The patient underwent cardiac catheterization and
received several medications, including heparin. Her platelet
count on admission was 184,000/mm3. After 10 days of heparin
therapy, she developed bilateral lower extremity cyanosis and a
decrease in platelet count to 121,000/mm3. HITT was suspected,
and both a heparin PF4 antibody test and 14C-serotonin release
assay were positive, confirming the diagnosis. Heparin was discontinued, and the patient was started on argatroban and warfarin.
Four days after initiation of therapy, and while the patient was
still on both agents, she developed ecchymosis of the right breast
along with multiple hemorrhagic bullae. Her platelet count at the
time was 132,000/mm3. Examination revealed a well-demarcated
ecchymotic patch with overlying hemorrhagic blisters and areas
of retiform purpura on the right breast (Figure 1a). Pronounced
tenderness upon palpation of the right breast was also present.
60
Bilateral lower extremities showed violaceous livedoid patches
and retiform purpura on the plantar and dorsal feet and ankles,
in addition to cyanosis involving all digits (Figure 1b). Laboratory
evaluation demonstrated a hemoglobin of 10.8 g/dL, a hematocrit
of 31.8%, a prothrombin time of 37 seconds, and an international
normalized ratio of 3.5. Histopathologically, a biopsy of the right
breast demonstrated widespread epidermal necrosis, thrombosed
vessels containing fibrin deposits throughout the dermis, and
extravasation of erythrocytes (Figure 2).
The clinical picture, along with the physical examination and
the histopathologic findings, was consistent with the diagnosis
of WISN. Warfarin was thus immediately discontinued, and the
patient remained on monotherapy with argatroban. A right mastectomy was performed one day after the onset of the skin necrosis.
DISCUSSION
Heparin-induced thrombocytopenia (HIT) occurs in about
1% to 5% of patients receiving heparin, and only a third of patients progress to develop arterial or venous thrombosis (2). Two
distinct forms of HIT exist: type I and type II (2). Type I HIT
is a nonimmunologic response in which heparin induces platelet
aggregation and sequestration, thus causing transient thrombocytopenia (2). Type II HIT is caused by the formation of antibodies
that activate platelets, leading to a hypercoagulable state. The diagnosis is made largely based on clinical findings (2). It is confirmed
by laboratory testing that demonstrates either >50% reduction in
platelet count or thrombocytopenia in the setting of HIT antibody
seroconversion (2). HITT is diagnosed when the criteria for HIT
are met along with evidence of vascular thrombosis (2).
As for WISN, it is estimated to occur in approximately 0.01%
to 0.1% of patients receiving warfarin (1). This rare adverse effect is
characterized by the acute onset of paresthesia and swelling of the
affected areas, followed by petechiae, ecchymosis, and eventually
hemorrhagic bullae (3). Histopathologically, dermal microthrombi
are found in the venules, veins, and capillaries, in addition to
ischemic skin necrosis and erythrocyte extravasation (4).
From Texas A&M College of Medicine, Baylor Scott & White Health, Dallas, Texas
(Fawaz, Tran); Cockerell Dermatopathology, University of Texas Southwestern
Medical Center, Dallas, Texas (Candelario); and the University of Puerto Rico
School of Medicine, San Juan, Puerto Rico (Rochet, Brau).
Corresponding author: Bilal Fawaz, Baylor Scott & White Health, 3500 Gaston
Avenue, Dallas, TX 75246 (e-mail: bfawaz7@gmail.com).
Proc (Bayl Univ Med Cent) 2016;29(1):60–61
a
b
avoided until complete platelet recovery is
achieved (5, 15). Once the thrombocytopenia has resolved, modest doses of warfarin should be used during the transition
from the direct thrombin inhibitor (5).
1. Howard-Thompson A, Usery JB, Lobo BL,
Finch CK. Heparin-induced thrombocytopenia complicated by warfarin-induced
skin necrosis. Am J Health Syst Pharm
2008;65(12):1144–1147.
2. Ahmed I, Majeed A, Powell R. Heparin induced thrombocytopenia: diagnosis
and management update. Postgrad Med J
2007;83(983):575–582.
Figure 1. (a) Right breast showing an erythematous ecchymotic patch with overlying hemorrhagic bullae. (b) 3. Nazarian RM, Van Cott EM, Zembowicz A,
Duncan LM. Warfarin-induced skin necrosis.
Lower extremities showing violaceous livedoid patches and retiform purpura on the plantar and dorsal feet, in
J Am Acad Dermatol 2009;61(2):325–332.
addition to cyanosis involving all digits.
4. Miura Y, Ardenghy M, Ramasastry S, Kovach
R, Hochberg J. Coumadin necrosis of the skin: report of four patients.
Warfarin can induce a paradoxical hypercoagulable state in
Ann Plast Surg 1996;37(3):332–337.
the early stages of treatment, usually within 3 to 10 days of ther5. Srinivasan AF, Rice L, Bartholomew JR, Rangaswamy C, La Perna L,
apy initiation, associated with inadequate overlap with heparin
Thompson JE, Murphy S, Baker KR. Warfarin-induced skin necrosis and
(3). The mechanism is thought to be due to a disturbance in the
venous limb gangrene in the setting of heparin-induced thrombocytopenia. Arch Intern Med 2004;164(1):66–70.
balance between the anticoagulant and procoagulant pathways
6. Lewandowski K, Zawilska K. Protein C concentrate in the treatment
(5). The anticoagulants protein C and protein S have a shorter
of warfarin-induced skin necrosis in the protein C deficiency. Thromb
half-life than other vitamin K–dependent factors, such as factors
Haemost 1994;71(3):395–399.
II, IX, and X (6). The net result is a deficiency in both proteins
7. Warkentin TE, Sikov WM, Lillicrap DP. Multicentric warfarin-induced
early in the treatment, which increases the chance of thrombosis
skin necrosis complicating heparin-induced thrombocytopenia. Am J
Hematol 1999;62(1):44–48.
and subsequent skin necrosis (5).
8. Celoria GM, Steingart RH, Banson B, Friedmann P, Rhee SW, Berman
The risk of WISN may be increased in the setting of HIT (5).
JA. Coumarin skin necrosis in a patient with heparin-induced thromboNumerous case reports have described an association between the
cytopenia—a case report. Angiology 1988;39(10):915–920.
two conditions (7–11). The generation of procoagulant, platelet9. Drakos P, Uziely B, Nagler A, Gillis S, Eldor A. Successful administraderived microparticles observed in HIT is postulated to accelerate
tion of low molecular weight heparin in a patient with heparin-induced
the rate of protein C consumption, thus contributing to the early
thrombocytopenia and coumarin-induced skin necrosis. Haemostasis
1993;23(5):259–262.
warfarin-induced protein C deficiency and an increased state of
10.
Shahak A, Pósán E, Szücs G, Rigó J, Boda Z. Coumarin-induced skin
hypercoagulability (7, 12, 13). These microparticles, along with
necrosis following heparin-induced thrombocytopenia and thrombosis.
the procoagulant HIT antibodies, may also contribute to an inA case report. Angiology 1996;47(7):725–727.
crease in thrombin, which predisposes the patient to the develop11. White CA, Chung DA, Thomas M, Marrinan MT. Warfarin-induced skin
ment of microvascular thrombosis during warfarin treatment (7,
necrosis and heparin-induced thrombocytopenia following mitral valve replacement for marantic endocarditis. J Heart Valve Dis 2006;15(5):716–718.
14). The combination of these factors can lead to catastrophic
12. Warkentin TE, Hayward CP, Boshkov LK, Santos AV, Sheppard JA, Bode
hypercoagulable consequences, as noted in our patient. Patients
AP, Kelton JG. Sera from patients with heparin-induced thrombocytopenia
with HIT should thus immediately discontinue heparin. Those
generate platelet-derived microparticles with procoagulant activity: an explanawho require anticoagulation should be initiated on a thrombin
tion for the thrombotic complications of heparin-induced thrombocytopenia.
inhibitor, such as lepirudin or argatroban, and warfarin should be
Blood 1994;84(11):3691–3699.
13. Tans G, Rosing J, Thomassen MC, Heeb
MJ, Zwaal RF, Griffin JH. Comparison of
a
b
anticoagulant and procoagulant activities of
stimulated platelets and platelet-derived microparticles. Blood 1991;77(12):2641–2648.
14. Visentin GP, Ford SE, Scott JP, Aster RH. Antibodies from patients with heparin-induced
thrombocytopenia/thrombosis are specific
for platelet factor 4 complexed with heparin
or bound to endothelial cells. J Clin Invest
1994;93(1):81–88.
15. Pravinkumar E, Webster NR. HIT/HITT and
alternative anticoagulation: current concepts.
Br J Anaesth 2003;90(5):676–685.
Figure 2. Punch biopsy from the right breast demonstrating widespread epidermal necrosis, thrombosed vessels
containing fibrin deposits throughout the dermis, and extravasation of erythrocytes.
January 2016
Warfarin-induced skin necrosis following heparin-induced thrombocytopenia
61
Metastatic thymoma involving the bone marrow
Mhair Dekmezian, MD, Stella Wenceslao, MD, and John R. Krause, MD
Although relatively rare, thymomas can be involved in a considerable
variety of clinical presentations. Clinicians should be mindful of the
breadth of associations with other diseases, including autoimmune disorders and many secondary nonthymic malignancies. For the pathologist, knowledge of the extremely varied histopathologic presentation of
thymoma is vital to formulate a proper differential, workup, and diagnosis. The presented case illustrates the finding of very rare metastatic
thymoma involvement of bone marrow, identified during evaluation for
pancytopenia. The history of prior prostate cancer and an uncharacterized
pancreatic lesion, as well as the familial presentation, also suggests a
possible underlying hereditary syndrome.
T
umors of the thymus gland (thymomas) are rare.
Thymomas have a strong clinical association with
autoimmune disorders, including myasthenia gravis,
polymyositis, systemic lupus erythematosus, myocarditis, pure red cell aplasia, rheumatoid arthritis, scleroderma,
Sjögren’s syndrome, and Graves disease, with a varying frequency of presentation. It is extremely rare for thymomas to
metastasize to the bone marrow. We report a case of metastatic
thymoma discovered on a bone marrow biopsy submitted for
evaluation of pancytopenia.
CASE REPORT
A 77-year-old man with a history of prostate cancer presented with an acute onset of back pain and was found to have
a circumferential epidural tumor at T12, with significant cord
compression and edema. Following spinal radiation, he received
six cycles of paclitaxel and carboplatin chemotherapy for presumed metastatic carcinoma. A follow-up computed tomography (CT) scan showed an enlarging mediastinal mass as well
as a solitary low-density liver lesion. CT-guided core biopsy of
the mediastinal mass showed a carcinoma that was positive for
squamous markers p63 and high-molecular-weight keratin; a
minor component of lymphocytes was predominantly CD4+/
CD8+ T cells. Although a thymic neoplasm was considered,
pulmonary non–small cell carcinoma was favored. Tests for
ALK gene rearrangement by fluorescent in situ hybridization
and EGFR mutation by polymerase chain reaction were both
negative.
62
Subsequent imaging showed increasing disease activity
in the chest and a 0.5 cm liver lesion, with no bone disease.
Single-agent docetaxel was started but discontinued 6 months
later due to neuropathy. On follow-up, the liver lesion was
enlarging, and a new pancreatic tail lesion was identified with
a radiologic impression of a low-grade neuroendocrine tumor.
Liver biopsy showed a lesion with a prominent component
of thymic-type, CD1a-positive lymphocytes and epithelial
cells consistent with thymoma, World Health Organization
(WHO) type B2. Chemotherapy for relapsing thymoma,
including cisplatin, doxorubicin, and cyclophosphamide,
was started; pancytopenia refractory to erythropoietin with
normal iron studies prompted a posterior iliac crest marrow
biopsy.
The trephine biopsy showed extensive involvement by predominantly small lymphocytes, with scattered, cytologically
bland epithelial cells and broad bands of connective tissue forming lobules (Figure 1a). Immunohistochemistry testing showed
a background of cells positive for cytokeratin (Figure 1b), with
the lymphoid cells predominantly positive for CD3 and CD1a
(Figure 1c). Among other stains, CD20 showed rare B cells,
CD34 highlighted less than 1% positive cells, EMA was dim
and patchy, PAX8 was negative, and CD71 showed virtually
absent erythroid precursors; prostate-specific antigen immunostains were negative. The hematopoietic cells in the marrow
biopsy, although displaced by the thymoma, showed no significant dyspoietic changes. Iron stores as assessed by Prussian
blue stain were adequate. Chromosomal analysis demonstrated
a normal karyotype, and flow cytometry found no evidence of
lymphoproliferative disease.
These findings are consistent with metastatic thymoma
involving the bone marrow. Treatment with the kinase inhibitor sunitinib was started. Interestingly, it was discovered that one
of the patient’s immediate family members also had metastatic
thymoma.
From the Department of Pathology, Baylor University Medical Center at Dallas
and Baylor Charles A. Sammons Cancer (Dekmezian, Krause); and med fusion
Laboratory, Lewisville, Texas (Wenceslao).
Corresponding author: Mhair Dekmezian, MD, Department of Pathology, Baylor
University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX 75246
(e-mail: mhair.dekmezian@BaylorHealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):62–64
a
c
b
Figure 1. Trephine bone marrow biopsy with thymoma involvement. (a) A low-power view (100×) with hematoxylin and eosin stain shows disruption of the usual
arrangement of hematopoietic cells among bony trabeculae. (b) A cytokeratin immunostain highlights a thin fibrillary network surrounding the T cells (100×).
(c) A CD3 immunostain shows that the majority of lymphocytes are T cells (400×). CD1a shows a similar distribution (not pictured).
DISCUSSION
Thymoma refers to neoplasms of thymic epithelial cells, usually in the anterior mediastinum (1). These lesions are rare,
with an incidence of 0.13 per 100,000 person-years. An agerelated rise in incidence in middle age is seen, peaking in the
seventh decade (2). Clinical presentation is most often myasthenia gravis, followed by compression of mediastinal tissues
(3); systemic symptoms such as fever, malaise, or weight loss
may occur. Radiologic appearance varies, with benign lesions
appearing more regular and malignant thymomas appearing
more irregular and uneven.
The clinical association with autoimmune disorders should
be emphasized: 40% of thymoma patients have a (presumably
paraneoplastic) autoimmune condition, most commonly myasthenia gravis (4). Other associated entities include polymyositis,
systemic lupus erythematosus, peripheral neuropathy, myocarditis, graft-versus-host-disease–like symptoms, hypogammaglobulinemia, pure red blood cell aplasia, aplastic anemia, rheumatoid
arthritis, scleroderma, Sjögren syndrome, and Graves disease.
Such strong autoimmune correlations merit consideration of
thymoma as a component of a syndrome (5). Due to the rarity
of thymomas, identification of a distinct genetic link has proven difficult; however, epidemiological clustering of thymomas
and neuroendocrine tumors is observed in relation to multiple
endocrine neoplasia syndrome (6), which is associated with
pituitary adenomas, parathyroid hyperplasia, and pancreatic
neuroendocrine tumors.
The gross appearance of a thymoma is often a solid yellow
mass with a lobular configuration accentuated by prominent
fibrous trabeculae (3), with variable necrosis, hemorrhage, or
cystic spaces or degeneration, features of which do not portend a poor prognosis (7). Circumscription and encapsulation
correspond to less aggressive lesions. Care should be taken
to distinguish cystic thymomas from reactive multilocular
thymic cysts (8). The histologic classification of thymomas
has undergone frequent revision. The most recent WHO classification defines categories based on histology of the neoplasJanuary 2016
tic epithelial cells: uniformly bland, spindled, or oval-shaped
(type A); round or polygonal (type B1, B2, or B3); or both
(type AB) (1).
Type A thymomas, also known as “spindle cell” or “medullary” thymomas, represent a small portion of thymomas, less associated with myasthenia gravis, with a bland spindled pattern
and rare immature cortical-type CD4+/CD8+ lymphocytes.
Type AB, characterized by components of both lymphocytepoor type A and lymphocyte-rich type B histology, shows
predominantly small, polygonal epithelial cells, with round,
oval, or spindled nuclei and inconspicuous nucleoli. Type A
and AB thymomas have a favorable prognosis; most can be
treated surgically.
Type B1, or lymphocyte-rich, thymomas closely resemble the histology of normal thymus, with cortical areas of
immature lymphocytes, many scattered foci of medullary differentiation, and scant neoplastic epithelial cells, typically with
a well-defined capsule. These are often found during workup of
myasthenia gravis, and although slightly more aggressive than
A or AB, type B1 thymomas tend toward a favorable prognosis.
Type B2, or cortical, thymomas are very strongly correlated
with myasthenia gravis (30%–82%). Histology shows a lobular
architecture with a more prominent epithelial component and
less lymphocytic infiltrate compared to the B1 type. The T cells
show an immature cortical phenotype, with mature T cells in
rare medullary islands.
Type B3, or well-differentiated, thymomas are also strongly
correlated with myasthenia gravis, with frequent local compressive symptoms and local invasion. These often present at higher
stages, resulting in poorer overall survival. Histology shows few
lymphocytes, with sheets of tumor cells in lobules separated by
thick hyalinized septae.
In cases with overt cytological atypia, the tumor is classified
as a thymic carcinoma, or “type C thymoma.” Many variants
exist, but they lack autoimmune associations and the immature
T-cell phenotype; Epstein-Barr virus may play an etiologic role
in poorly differentiated squamous or undifferentiated thymic
Metastatic thymoma involving the bone marrow
63
carcinomas. Notably, thymomas can contain any combination
of histologic subtypes; adequate sampling is vital to ensure
proper characterization of the tumor.
Staging is integral to prognosis and treatment and depends
primarily on capsular invasion, either microscopic or macroscopic, or local invasion if no distinct capsule is present. Curiously, the histologic subtype of thymic tumors, independent
from stage, correlates less well with survival (9). A favorable
prognosis for thymic neoplasms is associated with five discrete
factors: the presence of myasthenia gravis, younger age, completeness of resection, low stage, and tumor type A or B (10).
Treatment of stage I and II tumors depends on complete surgical
resection, with most deaths due to other causes (11). Advanced
disease, often exhibiting pericardial or pleural implants, can
benefit from postexcisional radiotherapy (12). The preferred
chemotherapy for metastatic lesions is cisplatin with vincristine,
doxorubicin, and etoposide (13).
Distant metastases are rare and have been reported in lymph
nodes, lung, liver, ovary (type B1) (14), and breast (type AB)
(15). Bone involvement is reported, but often as direct invasion
into adjacent ribs and vertebrae (16). True thymoma metastases
to the bone marrow are extremely unusual, with only rare cases
reported in the literature (17).
1.
2.
3.
4.
64
Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, eds. World
Health Organization Classification of Tumours: Pathology and Genetics of
Tumours of the Lung, Pleura, Thymus and Heart. Lyon, France: IARC Press,
2004:154–166.
Engels EA. Epidemiology of thymoma and associated malignancies.
J Thorac Oncol 2010;5(10 Suppl 4):S260–S265.
LeGolvan DP, Abell MR. Thymomas. Cancer 1977;39(5):2142–2157.
Tormoehlen LM, Pascuzzi RM. Thymoma, myasthenia gravis, and
other paraneoplastic syndromes. Hematol Oncol Clin North Am
2008;22(3):509–526.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Souadjian JV, Enriquez P, Silverstein MN, Pépin JM. The spectrum of
diseases associated with thymoma. Coincidence or syndrome? Arch Intern
Med 1974;134(2):374–379.
De Toma G, Plocco M, Nicolanti V, Brozzetti S, Letizia C, Cavallaro
A. Type B1 thymoma in multiple endocrine neoplasia type 1 (MEN-1)
syndrome. Tumori 2001;87(4):266–268.
Moran CA, Suster S. Thymoma with prominent cystic and hemorrhagic
changes and areas of necrosis and infarction: a clinicopathologic study of
25 cases. Am J Surg Pathol 2001;25(8):1086–1090.
Izumi H, Nobukawa B, Takahashi K, Kumasaka T, Miyamoto H, Yamazaki
A, Sonobe S, Uekusa T, Suda K. Multilocular thymic cyst associated with
follicular hyperplasia: clinicopathologic study of 4 resected cases. Hum
Pathol 2005;36(7):841–844.
Weissferdt A, Moran CA. Staging of thymic epithelial neoplasms:
thymoma and thymic carcinoma. Pathol Res Pract 2015;211(1):2–11.
Chalabreysse L, Roy P, Cordier JF, Gamondes JP, Thivolet-Bejui F.
Correlation of the WHO schema for the classification of thymic epithelial neoplasms with prognosis: a retrospective study of 90 tumors. Am J
Surg Pathol 2002;26(12):1605–1611.
Wilkins KB, Sheikh E, Green R, Patel M, George S, Takano M,
Diener-West M, Welsh J, Howard S, Askin F, Bulkley GB. Clinical and
pathologic predictors of survival in patients with thymoma. Ann Surg
1999;230(4):562–574.
Uematsu M, Kondo M. A proposal for treatment of invasive thymoma.
Cancer 1986;58(9):1979–1985.
D’Andrea MA, Reddy GK. Management of metastatic malignant
thymoma with advanced radiation and chemotherapy techniques: report
of a rare case. World J Surg Oncol 2015;13:77.
Martín-Hernández R, Villanueva MM, Sánchez MN, López EC. Ovarian
metastasis of a thymoma: report of a case and literature review. Int J Gynecol
Pathol 2015;34(4):374–378.
Huang PW, Chang KM. Solitary metastasis to the breast after complete
resection of encapsulated type AB thymoma: a case report. J Med Case
Rep 2015;9:63.
Lemann II, Smith J. Primary carcinoma of the thymus, report of a case.
Arch Intern Med (Chic) 1926;38(6):807–815.
Rotter G, Schneider U, Tunn PU. Thymoma with primary osseous and
pulmonary metastases. Case report and review of the literature [article in
German]. Orthopade 2001;30(8):559–564.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Mullerian adenosarcoma of the cervix with heterologous
elements and sarcomatous overgrowth
Varsha Podduturi, MD, and Karen R. Pinto, MD
Cervical adenosarcomas are exceedingly infrequent tumors that occur
most often in women of reproductive age. Adenosarcomas comprise
benign epithelial elements and malignant stromal elements. The malignant stromal elements can either be homologous, such as fibroblasts or
smooth muscle, or heterologous, like cartilage, striated muscle, or bone.
We report a case of adenosarcoma of the cervix with heterologous elements and sarcomatous overgrowth in a 38-year-old woman.
A
denosarcomas are rare malignant mixed mullerian
tumors that are composed of benign epithelial and
malignant stromal components. These entities occur
most often in the endometrium, ovary, or pelvis and
less often in the cervix. The presence of sarcomatous overgrowth
and heterologous elements are two histopathologic features associated with a worse prognosis. Sarcomatous overgrowth is
diagnosed when the pure sarcomatous portion of the neoplasm
constitutes >25% of the primary tumor. Heterologous elements
are features present in the tumor that are not native to the
primary site and include cartilage, skeletal muscle, or bone.
Adenosarcomas rarely have distant metastases, but they have a
propensity for local recurrence (1, 2). We present the findings
in a young woman with a cervical mullerian adenosarcoma with
sarcomatous overgrowth and heterologous elements.
CASE REPORT
A 38-year-old G3, P3, white woman with genital herpes
presented to her gynecologist with postcoital spotting and light
brown discharge. Examination found a cervical polyp, which
was subsequently biopsied. Microscopically, it consisted of polypoid fragments of endocervical mucosa and squamous mucosa
on the surface. Small blue cells with scant cytoplasm, ovoid nuclei, and bundles of spindled cells were underneath the surface
epithelium, resembling a cambium layer (Figure 1a), and within
the endocervical stroma (Figure 1b). There was a section of
dense proliferation of blue cells around small vessels (Figure 1c).
Numerous mitotic figures and apoptotic cells were present. A
focus of striated muscle cells consistent with rhabdomyoblasts
was also identified (Figure 1d). The biopsy had up to 4 mitotic
figures per 10 high-power fields in hypercellular areas. Scattered
groups of stromal cells were strongly immunohistochemically
Proc (Bayl Univ Med Cent) 2016;29(1):65–67
reactive for estrogen and progesterone receptors, myogenin, and
desmin. The stromal cells were immunohistochemically negative for WT1. On biopsy, an embryonal rhabdomyosarcoma,
botryoid type, was diagnosed. The patient underwent three
cycles of chemotherapy with cyclophosphamide, vincristine,
and actinomycin D. Three months later, she underwent a radical hysterectomy, bilateral salpingectomy, and bilateral pelvic
lymph node dissection.
The uterus measured 8.5 × 6.0 × 3.5 cm and weighed 92 g.
The ectocervix was remarkable for a protuberant, red-brown
endocervical mass measuring 2.3 × 2.3 × 1.8 cm located at
the 1:00 to 4:00 position. Microscopically, the tumor had dilated benign glands with focal periglandular stromal cuffing
(Figure 2a) and stromal condensation underneath the surface
epithelium (Figure 2b). Heterologous elements included foci
of benign cartilage (Figure 2c) and elongated strap cells with
muscle striations consistent with rhabdomyoblasts (Figure 2d).
Sarcomatous overgrowth was also present. The stromal cells
were immunohistochemically reactive for estrogen receptor,
progesterone receptor, and CD10. No myometrial invasion was
present. The vaginal mucosa, parametrium, and the 21 lymph
nodes were not involved by tumor.
DISCUSSION
In our case, the diagnosis of embryonal rhabdomyosarcoma
was based on the morphology and immunohistochemical
staining pattern, in particular the positive desmin stain. After
assessing the entire lesion in the main resection specimen and
the immunohistochemical stains, the lesion was best diagnosed
as an adenosarcoma.
Clement and Scully (1) first described mullerian adenosarcoma as an uncommon variant of malignant mixed mullerian
tumors that were composed of benign epithelial elements and
malignant stromal elements. The malignant stromal elements
may be homologous (fibroblasts or smooth muscle) or heterologous (cartilage, striated muscle, or bone) (1). A review disclosed
few reported cases of cervical adenosarcoma with heterologous
From the Department of Pathology, Baylor University Medical Center at Dallas.
Corresponding author: Varsha Podduturi, MD, Department of Pathology, Baylor
University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX 75246
(e-mail: Varsha.podduturi@gmail.com).
65
average age was 31 years, with onethird of patients presenting before
age 15 (11). The most common presentation is abnormal vaginal bleeding. Examination usually shows a
polypoid lesion protruding through
the external cervical os. Distant metastases are rare (1), but these tumors
can recur locally.
The histopathologic diagnosis
of an adenosarcoma includes the
following: the formation of peric
d
glandular cuffing and intraglandular protrusions of cellular stroma;
noninvasive glands lined by benignappearing mullerian epithelium
of various types showing mild to
marked nuclear atypia; an average of
≥2 mitotic figures per 10 high-power
fields in the stromal component; and
more than mild nuclear atypia of the
stromal cells (1, 11).
Factors indicating a poor progFigure 1. (a) Stromal condensation underneath the endocervical surface epithelium (hematoxylin and eosin [H&E]
nosis
include cytologic atypia, high
100×). (b) Small round blue cells within the endocervical stroma (H&E 400x). (c) Small round blue cells surrounding
proliferation
rate, sarcomatous overvessels (H&E 400×). (d) Foci of skeletal muscle consistent with rhabdomyoblasts (H&E 100×).
growth, presence of heterologous
elements, deep myometrial invasion,
a
b
necrosis, and extrauterine spread (9,
11). Of the aforementioned factors,
sarcomatous overgrowth and myometrial invasion are consistently
associated with poor prognosis and
recurrence (1, 11). Sarcomatous overgrowth is present when it accounts for
at least 25% of the tumor area (16).
The differential diagnosis of
an adenosarcoma of the cervix
includes benign lesions such as
c
d
adenofibroma, atypical endocervical
polyp, and adenomyoma of the
cervix and malignant neoplasms including uterine adenosarcoma with
secondary involvement of the cervix,
carcinosarcoma, and embryonal
rhabdomyosarcoma (17).
As evidenced by this case, adenosarcomas with rhabdomyoblastic differentiation and/or those with
Figure 2. (a) Periglandular cuffing of stromal cells (hematoxylin and eosin [H&E], 200×). (b) Stromal overgrowth areas of sarcomatous overgrowth are
underneath the surface epithelium (H&E 200×). (c) Foci of benign cartilage (H&E 200×). (d) Foci of rhabdomyoblasts sometimes difficult to distinguish
present within the main resection specimen (H&E 400×).
from embryonal rhabdomyosarcomas. In 1985, Chen reported a case
of rhabdomyosarcomatous adenosarcoma of the uterine cervix
elements or sarcomatous overgrowth (1–16). Even fewer cases
(6). It is now believed that these two entities are distinct. In 2013,
have both sarcomatous overgrowth and heterologous elements.
Fanghong et al discussed the morphologic and immunohistoCervical adenosarcomas have been reported in a wide age range
chemical clues to differentiate between the two. Adenosarcomas
of women (11–67 years of age), but in a study of 12 cases, the
a
66
b
Baylor University Medical Center Proceedings
Volume 29, Number 1
should exhibit foci with intraluminal polypoid projections and a
phyllodes-like growth pattern (18). Intraluminal polypoid projections can be focally present in an embryonal rhabdomyosarcoma;
however, a phyllodes-like growth pattern should be absent (18).
Immunohistochemical stains are also very helpful in differentiating between an adenosarcoma and an embryonal rhabdomyosarcoma. Adenosarcomas exhibit estrogen and progesterone receptor
reactivity, but embryonal rhabdomyosarcomas should be negative
for hormone receptors (18).
Treatment and clinical management of patients with cervical
adenosarcomas is not well defined and continues to be under
intense investigation. No radiation or chemotherapy guidelines
exist for cervical adenosarcomas due to lack of evidence that
any one treatment is more advantageous than other therapies
(19–21). Much of the clinical management of cervical adenosarcomas is based on experience with uterine adenosarcomas
(17). At 10 months postoperatively, our patient remains free
of disease.
1.
2.
3.
4.
5.
6.
7.
8.
Clement PB, Scully RE. Mullerian adenosarcoma of the uterus: a
clinicopathologic analysis of 100 cases with a review of the literature.
Hum Pathol 1990;21(4):363–381.
Verschraegen CF, Vasuratna A, Edwards C, Freedman R, Kudelka
AP, Tornos C, Kavanagh JJ. Clinicopathologic analysis of mullerian
adenosarcoma: the M.D. Anderson Cancer Center experience. Oncol
Rep 1998;5(4):939–944.
Roth LM, Pride GL, Sharma HM. Mullerian adenosarcoma of the uterine
cervix with heterologous elements: a light and electron microscopic study.
Cancer 1976;37(4):1725–1736.
Martinelli G, Pileri S, Bazzochi F, Serra L. Mullerian adenosarcoma of
the uterus: a report of 5 cases. Tumori 1980;66(4):499–506.
Zaloudek CJ, Norris HJ. Adenofibroma and adenosarcoma of the uterus:
a clinicopathologic study of 35 cases. Cancer 1981;48(2):354–366.
Chen KT. Rhabomyosarcomatous uterine adenosarcoma. Int J Gynecol
Pathol 1985;4(2):146–152.
Gal D, Kerner H, Beck D, Peretz BA, Eyal A, Paldi E. Mullerian adenosarcoma of the uterine cervix. Gynecol Oncol 1988;31(3):445–453.
Gast MJ, Radkins LV, Jacobs AJ, Gersell D. Mullerian adenosarcoma of the
cervix with heterologous elements: diagnostic and therapeutic approach.
Gynecol Oncol 1989;32(3):381–384.
January 2016
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
Kerner H, Lichtig C. Mullerian adenosarcoma presenting as cervical
polyps: a report of seven cases and review of the literature. Obstet Gynecol
1993;81(5 Pt 1):655–659.
Zichella L, Perrone G, De Falco V, Pelle R, Eleuteri Serpieri D. Adenosarcoma mesodermico eterologo dell’endocervice: descrizione di un
caso clinico. [Heterologous mesodermal adenosarcoma of the endocervix.
Description of a clinical case]. Minerva Ginecol 1994;46(9):511–514.
Jones MW, Lefkowitz M. Adenosarcoma of the uterine cervix: a clinicopathological study of 12 cases. Int J Gynecol Pathol 1995;14(3):223–239.
Feroze M, Aravindan KP, Malini T. Mullerian adenosarcoma of the uterine
cervix. Indian J Cancer 1997;34(2):68–72.
Clement PB, Zubovits JT, Young RH, Scully RE. Malignant mullerian
mixed tumors of the uterine cervix: a report of nine cases of a neoplasm
with morphology often different from its counterpart in the corpus. Int
J Gynecol Pathol 1998;17(3):211–222.
Ramos P, Ruiz A, Carabias E, Piñero I, Garzon A, Alvarez I. Müllerian
adenosarcoma of the cervix with heterologous elements: report of a case
and review of the literature. Gynecol Oncol 2002;84(1):161–166.
Bagga R, Keepanasseril A, Srinivasan R, Dey P, Gainder S, Saha SC,
Dhaliwal LK, Patel F. Adenosarcoma of the uterine cervix with heterologous elements: a case report and review of literature. Arch Gynecol Obstet
2010;281(4):669–675.
Clement PB. Mullerian adenosarcomas of the uterus with sarcomatous
overgrowth: a clinicopathological analysis of 10 cases. Am J Surg Pathol
1989;13(1):28–38.
Seagle BL, Falter KJ 2nd, Lee SJ, Frimer M, Samuelson R, Shahabi S.
Mullerian adenosarcoma of the cervix: report of two large tumors with
sarcomatous overgrowth or heterologous elements. Gynecol Oncol Case
Rep 2014;9:7–10.
Li RF, Gupta M, McCluggage WG, Ronnett BM. Embryonal rhabdomyosarcoma (botryoid type) of the uterine corpus and cervix in adult
women: report of a case series and review of the literature. Am J Surg
Pathol 2013;37(3):344–355.
Krivak TC, Seidman JD, McBroom JW, MacKoul PJ, Aye LM, Rose
GS. Uterine adenosarcoma with sarcomatous overgrowth versus uterine
carcinosarcoma: comparison of treatment and survival. Gynecol Oncol
2001;83(1):89–94.
Tanner EJ, Toussaint T, Leitao MM Jr, Hensley ML, Soslow RA, Gardner
GJ, Jewell EL. Management of uterine adenosarcomas with and without
sarcomatous overgrowth. Gynecol Oncol 2013;129(1):140–144.
Bernard B, Clarke BA, Malowany JI, McAlpine J, Lee CH, Atenafu EG,
Ferguson S, Mackay H. Uterine adenosarcomas: a dual-institution update
on staging, prognosis and survival. Gynecol Oncol 2013;131(3):634–639.
Mullerian adenosarcoma of the cervix with heterologous elements and sarcomatous overgrowth
67
Neuroendocrine carcinoma of the prostate gland
Pamela Hoof, MD, Ginger Tsai-Nguyen, MD, Scott Paulson, MD, Almas Syed, MD, and Adam Mora Jr., MD
Small cell prostate carcinoma (SCPC) has a clinical course and prognosis that is markedly different from that of common adenocarcinoma of
the prostate. The patient in this case presented with fever of unknown
origin, dyspnea, and near spinal cord compression. He was subsequently
found to have widely metastatic high-grade neuroendocrine carcinoma
of prostatic origin. This case emphasizes that despite the commonality
of prostate cancer, there are rare presentations of this common disease.
S
mall cell prostate carcinoma (SCPC) is a rare form of
extrapulmonary high-grade neuroendocrine carcinoma
accounting for <0.5% to 1% of all prostate cancers (1).
It is characterized by an aggressive clinical course and
portends a poor prognosis. Locally advanced or metastatic disease is common at the time of presentation. SCPC shares many
clinical and morphologic features with small cell carcinoma of
the lung. Given the rarity of this malignancy, treatment is frequently extrapolated from experience with small cell carcinoma
of the lung. Presented is a case of a lung nodule found to be
an extrapulmonary high-grade neuroendocrine carcinoma of
prostatic origin.
CASE PRESENTATION
A 78-year-old man with chronic obstructive pulmonary disease presented with a 6-month history of fever of unknown origin.
Over the preceding months he had nonproductive cough, night
sweats, dyspnea, intractable back pain, and a 20 lb unintentional
weight loss. Radiographs showed no focal lesions. Despite multiple rounds of antibiotics, the fever continued with no identifiable
etiology. Examination revealed crackles in the left lung base and
pain to palpation along the thoracic vertebrae. His white blood
cell count was 12.7 cells/mcL; C-reactive protein, 13.5 mg/L;
erythrocyte sedimentation rate, 40 mm/hr; and carcinoembryonic antigen, 46.5 mcg/L. His body mass index was 31.1 kg/m2.
Computed tomography of the chest and abdomen/pelvis revealed innumerable pulmonary and pleural lesions and a large,
necrotic hepatic mass (Figure 1). The prostate gland measured
5.6 × 7.8 cm. Magnetic resonance imaging of the thoracic and
lumbar spine also revealed diffuse bone involvement. The patient
underwent lung nodule biopsy. Histologic study disclosed a poorly
differentiated neuroendocrine carcinoma, small cell variant, with
68
markers positive for synaptophysin, chromogranin, and prostatic
acid phosphatase (Figure 2). An MIB-1 fraction (a cellular marker
of proliferation) was measured at 40%, consistent with G3 (highgrade) disease. Transrectal ultrasound-guided prostate needle biopsy demonstrated adenocarcinoma of the prostate gland, Gleason
9 with high-grade neuroendocrine differentiation focally noted.
Systemic chemotherapy, radiation, and hormonal therapy
were initiated with a combination of carboplatin and etoposide.
Following six cycles of systemic therapy and segmental radiation to the spine, the patient’s symptoms significantly improved.
Repeat imaging revealed significant reduction of metastatic lesions
with diffuse improvement in his widespread bone disease.
DISCUSSION
SCPC was first described by Wenk et al in 1977 (2). It
accounts for <1% to 2% of all small cell cancers and occurs
in 0.5% to 1% of men with prostate cancer (3). It has an aggressive clinical course. At the time of diagnosis, approximately
75% of patients have advanced stage disease. Common sites of
metastasis include the lung, bladder, liver, and bone (4). Patients
typically present with symptoms related to enlarged prostate,
specifically changes in urine stream. Interestingly, our patient
presented only with shortness of breath, fever, and back pain.
The diagnosis of SCPC was made only after the lung nodule was
biopsied and stained positive for prostate-specific antigen (PSA).
The low-grade fevers our patient experienced were ultimately
attributed to his underlying malignancy.
SCPC can occur concomitantly with adenocarcinoma or as
isolated disease; approximately one-half of patients have mixed
tumors (5). Positive staining for neuroendocrine markers including chromogranin, CD-56, synaptophysin, and neuron-specific
enolase are frequently noted in the diagnosis of SCPC (6). The
presence of at least one such marker occurs in 90% of SCPC
cases (3). Although SCPC and prostatic adenocarcinoma can
occur concomitantly, serum PSA levels do not correlate with
From the Department of Internal Medicine (Hoof, Tsai-Nguyen), Department of
Oncology (Paulson), Department of Radiology (Syed), and Division of Pulmonary
Disease (Mora), Baylor University Medical Center at Dallas.
Corresponding author: Adan Mora Jr., MD, Division of Pulmonary Disease,
Baylor University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX
75246 (e-mail: adam.mora@baylorhealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):68–69
a
c
b
Figure 1. Lung nodule with positive staining for (a) prostatic acid phosphatase, (b) synaptophysin, and (c) chromogranin.
burden of disease (7). Our patient’s PSA was mildly elevated
at 6.25 ng/mL; however, imaging revealed diffusely metastatic
disease. Typically, such elevations of PSA are seen in cases of
combined adenocarcinoma and SCPC.
Given the lack of randomized data for any high-grade
neuroendocrine carcinomas of extrapulmonary origin, frontline treatments for SCPC derive their origin from commonly
accepted therapies for small cell lung cancer. Accepted frontline treatment generally involves a platinum-based therapy plus
etoposide, with radiation included as appropriate. In the setting
of advanced disease there is currently no curative therapy.
One study by Hindson et al used a treatment regimen of
cyclophosphamide, doxorubicin, and vincristine but could only
induce a 4-month remission in patients with widely metastatic
disease (8). General survival ranges from 9 to 13 months (9).
However, there is limited data regarding survival difference in
pure SCPC versus combined adenocarcinoma with concomitant
SCPC. In a study by Asmis et al, the overall survival time was
9.5 months for combined prostate adenocarcinoma and small
cell prostate carcinoma, with similar survival for pure small cell
carcinoma (9).
Given widespread metastatic disease, systemic chemotherapy and radiation were pursued in our patient. Hormonal
therapy has utility if concomitant prostatic adenocarcinoma is
present. The patient in our case received a month-long course
of bicalutamide followed by scheduled leuprorelin injections
on a 3-month basis. At the time of discharge, he was able to
walk out of the hospital without dyspnea. Nine months after
discharge, the patient was still alive and in hospice.
1.
Abbas F, Civantos F, Benedetto P, Soloway MS. Small cell carcinoma of
the bladder and prostate. Urology 1995;46(5):617–630.
2. Wenk RE, Bhagavan BS, Levy R, Miller D, Weisburger W. Ectopic
ACTH, prostatic oat cell carcinoma, and marked hypernatremia. Cancer
1977;40(2):773–778.
3. Nadal R, Schweizer M, Kryvenko ON, Epstein JI, Eisenberger MA. Small
cell carcinoma of the prostate. Nat Rev Urol 2014;11(4):213–219.
4. Rubenstein JH, Katin MJ, Mangano MM, Dauphin J, Salenius SA,
Dosoretz DE, Blitzer PH. Small cell anaplastic carcinoma of the prostate:
seven new cases, review of the literature, and discussion of a therapeutic
strategy. Am J Clin Oncol 1997;20(4):376–380.
5. Têtu B, Ro JY, Ayala AG, Johnson DE, Logothetis CJ, Ordonez NG.
Small cell carcinoma of the prostate. Part I. A clinicopathologic study of
20 cases. Cancer 1987;59(10):1803–1809.
6. Wang W, Epstein JI. Small cell
carcinoma of the prostate. A morphologic and immunohistochemical
b
a
study of 95 cases. Am J Surg Pathol
2008;32(1):65–71.
7. Oesterling JE, Hauzeur CG, Farrow
GM. Small cell anaplastic carcinoma
of the prostate: a clinical, pathological and immunohistological study
of 27 patients. J Urol 1992;147(3 Pt
2):804–807.
8. Hindson DA, Knight LL, Ocker JM.
Small-cell carcinoma of prostate. Transient complete remission with chemotherapy. Urology 1985;26(2):182–184.
9. Asmis TR, Reaume MN, Dahrouge
S, Malone S. Genitourinary small
cell carcinoma: a retrospective review
of treatment and survival patterns at
Figure 2. Imaging. (a) Noncontrast axial CT chest image shows multiple bilateral pulmonary nodules consistent with
The Ottawa Hospital Regional Cancer
pulmonary metastatic disease. (b) Postcontrast sagittal T1-weighted MRI of the lumbar spine demonstrates multiple
Center. BJU Int 2006;97(4):711–715.
predominantly peripheral enhancing osseous metastases on a background of diffuse marrow signal abnormality.
January 2016
Neuroendocrine carcinoma of the prostate gland
69
Seronegative neuromyelitis optica after cardiac
transplantation
Elecia Kim, MD, Michael Van Vrancken, MD, Mohamed Shaji, MD, Osman Mir, MD, Cedric W. Spak, MD, MPH,
Manu Gupta, MD, and Sadat A. Shamim, MD
We report a case of a 42-year-old man who presented with progressive
weakness and blindness over the course of several months and met
criteria for seronegative neuromyelitis optica. This presentation was in
the setting of immunosuppression following cardiac transplant. No infectious causes were found within the neuroaxis, and he ultimately died
with complete blindness, quadriplegia, and respiratory failure attributed
to panmyelitis and brain stem inflammation despite aggressive therapies.
N
euromyelitis optica (NMO) is a rare inflammatory
demyelinating disease that affects the optic nerves,
brainstem, and spinal cord, resulting in varying degrees
of blindness and paralysis. Once considered a subclass
of multiple sclerosis, it has emerged as its own entity with the
discovery of an associated autoantibody, aquaporin-4, present
in a majority of patients (1). The antibody is absent in a subset
of patients (2) where other antibodies are thought to play a
role. The anti-MOG antibody may be linked to NMO, but was
commercially unavailable for testing at the time of our patient’s
illness (3). Current treatments are noncurative and include trials
of immunosuppressants and immunomodulators (4). We report
a case of a patient who, despite being on immunosuppression
after a heart transplant, presented with seronegative NMO.
CASE DESCRIPTION
A 42-year-old black man with prior orthotopic heart transplant for nonischemic cardiomyopathy and end-stage renal disease from immunosuppressant therapy presented with severe
burning pain in his legs bilaterally. The symptoms were first
noticed about 2 years posttransplant and had gradually worsened over 2 months. Initial examination showed hyperesthesia
from L2 on the right and L1 on the left. The patient refused a
lumbar puncture at that time, citing improved pain with gabapentin, and wished to go home with outpatient follow-up. The
patient was fully ambulatory at the time of discharge.
He gradually developed weakness in his legs and noticed
some blurry vision. Examination on his second admission,
5 weeks later, showed weakness in both legs, distal (3 of 5) greater
than proximal (4- of 5). Deep tendon reflexes were hyperreflexive
at the knees with clonus at the ankles. Strength in the upper
extremities was mildly decreased (4 of 5). He had a bilateral
70
T8 sensory level, but was not incontinent. Visual acuity was
decreased in his right eye with large sluggishly reactive pupils.
Repeat magnetic resonance imaging (MRI) of his spine
showed increased T2 hyperintensity throughout the central gray
matter with diffuse cord signal change and minimal cord expansion (Figure 1). MRI of the orbits showed fluid attenuation inversion recovery (FLAIR) hyperintensity of the bilateral anterior
optic pathway, and MRI of the brain showed brainstem FLAIR
signal elevation with subtle contrast enhancement. The cerebral
hemispheres showed only some encephalomalacia from known
previous asymptomatic strokes that occurred at the time of his
cardiac transplant with no signs of demyelination. Comprehensive rheumatologic and infectious workups were unremarkable
(Table 1). Aquaporin-4 IgG was negative. Cerebrospinal fluid
analysis disclosed an elevated protein (62 mg/dL) with a normal
cell count and differential.
Within a week of hospitalization, the patient was quadriplegic,
ventilator dependent, incontinent, and completely blind. He was
treated with broad-spectrum antibiotics, antifungals, and antivirals. He was treated for presumed NMO aggressively with highdose methylprednisolone and plasmapheresis (five cycles) followed
by intravenous immunoglobulin (2.3 g/kg), with no response. His
hospital course was complicated by healthcare-associated pneumonia and later a gastrointestinal bleed secondary to cytomegalovirus
colitis. The patient remained cognitively intact and was transitioned to comfort care per his wishes and died shortly thereafter.
The patient and his father granted an autopsy. His fixed
brain weighed 1550 g with significant gyral flattening and sulcal
narrowing consistent with edema. The cranial nerves appeared
grossly intact, except the right optic nerve appeared smaller than
the left. On coronal sectioning, no gross abnormalities were seen
throughout the cerebral hemispheres. Sectioning through the
cerebellum found a 1.1 × 0.8 cm wedged-shaped area of volume
loss with brown discoloration at the left medial posterior aspect.
No gross abnormalities were identified in the pons, midbrain,
medulla, or spinal cord.
From the Department of Internal Medicine (Kim), Department of Pathology (Van
Vrancken), Division of Neurology (Mir, Shamim), Division of Infectious Diseases (Spak),
and Division of Neuroradiology (Gupta), Baylor University Medical Center at Dallas.
Corresponding author: Sadat A. Shamim, MD, 3600 Gaston Avenue, Wadley
Tower Suite 1155, Dallas, TX 75246 (e-mail: sadatsha@baylorhealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):70–72
a
c
b
Table 1. Extensive negative laboratory workup
Negative testing
Infectious
• Adenovirus, PCR bronchoalveolar lavage
• Arbovirus panel (Eastern Equine, California, St. Louis,
Western Equine, West Nile virus), serum and CSF
• Bartonella antibody panel, serum
• Cytomegalovirus, PCR CSF
• Cryptococcal antigen, CSF
• Venereal Disease Research Laboratory, CSF
• Epstein-Barr virus antibodies, PCR CSF
• Herpes simplex virus antibodies, PCR CSF
• HIV antibody, serum
• JC virus, PCR CSF
• Legionella pneumophila direct fluorescent antibody
• Lyme disease, PCR serum
• Mycobacterium tuberculosis amplified
• Mycoplasma antibodies
• Toxoplasma gondii antibodies, serum and CSF
• Varicella zoster antibodies, PCR CSF
• Blood cultures
• CSF cultures
• Fungal cultures
d
Figure 1. MRI. (a) Sagittal and (b) axial FLAIR hyperintensity in the substantia
nigra, medulla, and cervical spinal cord. (c) Cervical and (d) thoracic sagittal T2weighted images showing cord edema. Subtle pathological enhancement was
seen in the cervical spine and lower medulla (not shown).
Microscopically (Figure 2), there was a remote incomplete
infarct with marked neuron and volume loss in the left cerebellar
hemisphere corresponding to the lesion seen grossly. The most
significant lesions seen microscopically were located within the
midbrain, pontomedullary junction, multiple levels of the spinal cord, and the optic nerves. These areas all showed similar
histologic findings characterized by extensive areas of pallor
and vacuolization with an inflammatory infiltrate composed
predominantly of macrophages. Extensive myelin loss was identified throughout these areas and was highlighted with a Luxol
fast blue stain. Additionally, focal axonal loss was also confirmed
by a neurofilament immunohistochemical stain. The characteristic features of cytomegalovirus infection were not identified.
DISCUSSION
Devic and Gault first described patients with NMO in 1894
(5). It is an inflammatory demyelinating disease that initially
spares the brain but attacks the optic nerves and spinal cord with
varying severity. The condition affects women nine times more
frequently than men, with the median age in the fourth decade.
The prognosis is poor, as no current therapies are curative.
Originally categorized as a subclass of multiple sclerosis,
NMO was later established as a separate disease with the discovery of a specific biomarker, aquaporin-4 IgG (1). Aquaporin-4
is the major water channel in the brain, optic nerve, and spinal
cord and thus a major contributor to water homeostasis (6). The
sensitivity of this antibody has been reported to be 73% and the
January 2016
Category
Rheumatologic •
•
•
•
•
•
•
•
Other
Aldolase
Anti-neutrophil cytoplasmic antibody
Anti-cardiolipin antibodies
Angiotensin-converting enzyme
Anti-citrullinated protein antibody
Anti-DNA antibodies
Anti-nuclear antibodies
Extractable nuclear antigen (Ro, La, RNP, Smith, Jo 1,
SCL 70 antibodies)
• Paraneoplastic autoantibody panel, CSF (ANNA-1,
ANNA-2, ANNA-3, AGNA-1, PCA-1, PCA-2, PCA-Tr,
Amphiphysin Ab, CRMP-5 IgG)
• Oligoclonal bands
• Immunoglobulin G synthesis index
CSF indicates cerebrospinal fluid; PCR, polymerase chain reaction.
specificity, 91% (1, 7). A 2012 retrospective study reported that
the presence or absence of the NMO antibody did not alter the
overall mortality rate, age of presentation, or relapse rate. Those
with seronegative NMO were more likely to have a monophasic
course, bilateral eye involvement, and concurrent optic neuritis
and myelitis (7), similar to our case.
In 2006, Wingerchuk and colleagues revised the diagnostic
criteria for NMO to include the discovered autoantibody (8). The
patient must present with optic neuritis and acute myelitis. In addition, two of three of these criteria must be met: 1) MRI shows
a spinal cord lesion that spans >3 vertebral segments; 2) patient
does not meet the criteria for multiple sclerosis based on MRI;
and 3) patient tests positive for aquaporin-4 IgG.
Treatment is limited and usually focused on immunosuppression. The typical algorithm is to start the patient having active
Seronegative neuromyelitis optica after cardiac transplantation
71
a
no effect on the disease process
and may even be harmful (4).
Our patient failed to respond to any of these therapies.
Furthermore, he had already
been immunosuppressed with
tacrolimus, mycophenolate
mofetil, and prednisone. Thus,
how he developed this condition in the setting of immunosuppression was puzzling.
e
b
1.
Lennon VA, Wingerchuk DM,
Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, Nakashmia
I, Weinshenker BG. A serum
autoantibody marker of neuromyelitis optica: distinction
from multiple sclerosis. Lancet
2004;364(9451):2106–2112.
2. Jarius S, Ruprecht K, Wildemann
B, Kuempfel T, Ringelstein M,
c
Geis C, Kleiter I, Kleinschnitz
C, Berthele A, Brettschneider J,
Hellwig K, Hemmer B, Linker
RA, Lauda F, Mayer CA, Tumani
H, Melms A, Trebst C, Stangel
M, Marziniak M, Hoffmann F,
Schippling S, Faiss JH, Neuhaus
g
O, Ettrich B, Zentner C, Guthke
K, Hofstadt-van Oy U, Reuss R,
Pellkofer H, Ziemann U, Kern
P, Wandinger KP, Bergh FT,
d
Boettcher T, Langel S, Liebetrau
M, Rommer PS, Niehaus S,
Münch C, Winkelmann A, Zettl
U, Metz I, Veauthier C, Sieb JP,
Wilke C, Hartung HP, Aktas O,
Paul F. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a
multicentre study of 175 patients.
J Neuroinflammation 2012;9:14.
3. Kitley J, Woodhall M, Wates P,
Figure 2. (a) Hematoxylin and eosin–stained section from the optic nerve showing a central area of vacuolization and
Leite MI, Devenney E, Craig
degeneration (×40). (b) Immunohistochemical stain for CD68 of the optic nerve showing increased macrophages infiltrating
J, Palace J, Vincent A. Myelinthroughout the nerve (×40). (c) Luxol fast blue stain of the optic nerve showing a loss of myelin, which is more pronounced
oligodendrocyte glycoprotein
centrally (×40). (d) Immunohistochemical stain for neurofilament showing a decreased number of axons within the optic
antibodies in adults with a neunerve (×40). (e) Hematoxylin and eosin–stained section of the spinal cord showing significant vacuolization and pallor
romyelitis optica phenotype. Neu(×100). (f) Immunohistochemical stain for CD68 highlighting background infiltrating macrophages within the spinal cord
rology 2012;79(12):1273–1277.
(×100). (g) Luxol fast blue stain of the spinal cord showing significant myelin loss (×100).
4. Collongues N, de Seze J. Current
and future treatment approaches
for neuromyelitis optica. Ther Adv Neurol Disord 2011;4(2):111–121.
demyelination on 1 g per day of intravenous methylprednisolone.
5. Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG.
If the patient fails to respond or if the symptoms are severe, adminThe spectrum of neuromyelitis optica. Lancet Neurol 2007;6(9):805–815.
6. Pittock SJ, Weinshenker BG, Lucchinetti CF, Wingerchuk DM, Corboy
istration of 2 g/kg of intravenous immunoglobulin, sometimes preJR, Lennon VA. Neuromyelitis optica brain lesions localized at sites of
ceded by plasma exchange, may be considered. Some reports suggest
high aquaporin 4 expression. Arch Neurol 2006;63(7):964–968.
that NMO is more responsive to plasma exchange than to either
7. Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker
steroids or intravenous immunoglobulin (4). To reduce relapses,
of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel.
immunosuppression is used, with rituximab, azathioprine, cycloJ Exp Med 2005;202(4):473–477.
8. Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenphosphamide, and mycophenolate the agents of choice (4). There
ker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology
are no randomized controlled trials comparing these treatments.
2006;66(10):1485–1489.
f
Interferon and other therapy used for multiple sclerosis usually have
72
Baylor University Medical Center Proceedings
Volume 29, Number 1
Successful heart transplantation using a donor heart
afflicted by takotsubo cardiomyopathy
Yazhini Ravi, MD,* Ryan Campagna, MD,* Paola C. Rosas, MD, PhD, RPh, Essa Essa, MD, Ayesha K. Hasan, MD,
Robert S. D. Higgins, MD, MHA, Sitaramesh Emani, MD, and Chittoor B. Sai-Sudhakar, MD
Takotsubo cardiomyopathy, also known as apical ballooning syndrome,
stress cardiomyopathy, or broken heart syndrome, is a disease characterized by transient ventricular dysfunction in the absence of obstructive
coronary artery disease. Herein, we present a case in which a heart with
mild takotsubo cardiomyopathy was utilized as the donor organ for an
orthotopic heart transplant.
CASE REPORT
A 61-year-old man with ischemic cardiomyopathy in New
York Heart Association Class IV heart failure despite optimal
therapy was listed for cardiac transplantation. Four months
later, a donor heart became available from a 17-year-old woman
without significant past medical history who was involved in a
motor vehicle accident. During the evaluation for organ donation candidacy, echocardiography demonstrated apical ballooning suggestive of takotsubo cardiomyopathy (TC) (Figure 1).
Because of the donor’s age and risk profile, epicardial coronary
artery disease was not considered to be a factor in the causation
of the localized wall motion abnormality. The left ventricular
apical ballooning was directly observed at procurement as well,
and palpation of the epicardial coronary arteries did not reveal
any gross pathology, areas of atheromatous disease, or calcium.
An orthotopic heart transplant was carried out in the recipient
using the bicaval technique following closure of a patent foramen
ovale in the donor heart. Total ischemic time was 240 minutes.
Following the completion of the procedure, an intraoperative
echocardiogram demonstrated complete resolution of the TC.
The patient was extubated on postoperative day 1 and was weaned
off all inotropic support within 48 hours. A transthoracic echocardiogram obtained on postoperative day 3 revealed no evidence
of TC (Figure 2). The postoperative course was uneventful.
Following the transplant, the patient continued to do well. The
first biopsy done 1 week posttransplant showed grade 2 rejection
(revised grade 1R) with evidence of reperfusion injury. Subsequent
biopsies have been 1A-2 (revised grade 1R), with all biopsies after
24 months being 1A (revised grade 1R). Annual assessments of his
left ventricular function have continued to show normal wall motion and function. To date, two annual angiographic assessments
have shown no evidence of coronary allograft vasculopathy. The
patient is doing well 46 months after his heart transplantation.
Proc (Bayl Univ Med Cent) 2016;29(1):73–74
Figure 1. Echocardiography showing left ventricular apical ballooning in the donor.
DISCUSSION
To date, there are no reports of TC in the context of cardiac transplantation. TC and cardiac transplantation have been
From the Division of Cardiothoracic Surgery, Baylor Scott & White Healthcare,
Temple, Texas (Ravi, Sai-Sudhakar); the College of Medicine, The Ohio State
University, Columbus, Ohio (Campagna); the Department of Medical Physiology,
Texas A&M Health Science Center, Temple, Texas (Rosas); the Division of
Cardiology, The Ohio State University, Columbus, Ohio (Essa, Hasan, Emani);
and the Department of Surgery, Johns Hopkins University School of Medicine,
Baltimore, Maryland (Higgins).
*Contributed equally.
Corresponding author: Sitaramesh Emani, MD, Division of Cardiology, The Ohio
State University, Wexner Medical Center, 473 W. 12th Avenue, Suite 200 DHLRI,
Columbus, OH 43210 (e-mail: Sitaramesh.emani@osumc.edu).
73
Figure 2. Echocardiogram in the recipient showing normal wall motion.
indirectly associated with one another via brain death–induced
cardiomyopathy (BDIC), a phenomenon that shares pathologic
similarities with TC. Brain death is a common scenario within
which cardiac donation is considered, yet the speculation of
brain death–induced myocardial stunning as a reversible cardiomyopathy has only occurred recently (1).
BDIC and TC share a number of traits, the most important
of which are excessive catecholamine exposure and transient
ventricular dysfunction. The excess circulatory catecholamines
present in BDIC and TC arise from different pathological etiologies, namely, stress-induced catecholamine release in TC and
a loss of brainstem parasympathetic outflow/disinhibition of
sympathetic tone in BDIC. The resultant “catecholamine surge”
then imparts damage through a variety of proposed mechanisms,
leading to clinically significant ventricular dysfunction. Despite
differences in the most prevalent location of the ventricular
dysfunction (right and left in BDIC and TC, respectively), the
conditions share a plethora of additional pathological characteristics, including electrocardiographic findings, microscopic
findings, and extracardiac features (1).
We propose in this case that the donor’s cardiac function
was affected by the intense physiologic stress caused by the motor vehicle accident and resultant fatal injuries. Many potential
cardiac donors suffer traumatic brain injury, and poor cardiac
function (often mediated by ventricular dysfunction) is the most
common cause for declining a donor heart for transplant (2).
Therefore, a better understanding of BDIC and its pathophysiological relation to reversible TC could lead to an increased use
of donor hearts that would otherwise be rejected because of
transient ventricular dysfunction. Future research efforts should
aim to understand these phenomena both separately and alongside one another as reversible cardiomyopathies.
1.
2.
Berman M, Ali A, Ashley E, Freed D, Clarke K, Tsui S, Parameshwar J, Large
S. Is stress cardiomyopathy the underlying cause of ventricular dysfunction
associated with brain death? J Heart Lung Transplant 2010;29(9):957–965.
Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Rahmel
AO, Kucheryavaya AY, Hertz MI. Registry of the International Society for
Heart and Lung Transplantation: twenty-fifth official adult heart transplant
report—2008. J Heart Lung Transplant 2008;27(9):943–956.
Invited Commentary
Using “broken hearts” for cardiac transplantation: a risky venture or
fruitful endeavor?
F
irst described in 1990 (1), takotsubo cardiomyopathy
(TC), known also as “broken heart syndrome” and
“stress-induced cardiomyopathy,” remains a perplexing
pathophysiologic condition. This transient clinical disorder is classically precipitated by intense emotional stress and
manifests with signs and symptoms mimicking acute coronary
syndrome in the absence of angiographically evident coronary
disease. The echocardiographic sine qua non of TC includes left
ventricular (LV) systolic dysfunction with apical ballooning that
spontaneously resolves on serial exams over days to weeks. From
a mechanistic standpoint, most postulate that TC is the culmi74
nation of a “perfect storm,” encompassing an intricate interplay
between neurohormonal and/or other physiologic stressors that
incite a catecholamine surge in susceptible patients with predisposing cardiovascular risk factors and comorbidities (2, 3).
In the current issue of Baylor Proceedings, Ravi and colleagues (4) describe one of the only reported cases of a donor
heart with TC successfully used for cardiac transplantation.
The donor, a 17-year-old female with no prior cardiac history,
suffered brain death following a high-impact motor vehicle collision. A confirmatory coronary angiogram was not performed,
but the echocardiographic findings were clearly indicative of
Proc (Bayl Univ Med Cent) 2016;29(1):74–75
TC, including both LV dysfunction and apical ballooning. The
authors correctly surmised this was a reversible state and that
once removed from the stressful catecholamine milieu of the
donor, the heart function would normalize and the recipient
would thrive. By the third postoperative day, this newly implanted heart exhibited no signs of TC and the patient had an
uneventful course.
While the authors should certainly be applauded for their
courage and astute clinical judgment in this case, it is unfortunate to note that many, if not most, other transplant centers
would likely have declined this donor heart offer. Such widespread reluctance is based largely on the prevalent concern
that donor hearts with LV dysfunction will exhibit a greater
proclivity for primary graft dysfunction following implantation. Such fears often persist, even when structural heart disease, such as coronary artery disease or valvular abnormalities,
has been excluded as an etiologic factor. A number of studies
examining outcomes of donor hearts with LV dysfunction
would refute the notion that such hearts would have intrinsically worse outcomes (5–7). In a study by Mohamedali and
colleagues (5) of 11 potential heart donors with compromised
ejection fraction, LV systolic function normalized, regardless
of the pattern of abnormalities. Similarly, in a Cleveland Clinic
study of 50 donor hearts with >70 echocardiographic abnormalities (6), the vast majority exhibited normalized parameters following transplantation. When examining outcomes
of “marginal donor hearts” in the alternative heart transplant
program at Duke, we found no increased risk of subsequent
graft dysfunction (7).
These and other studies suggest that TC may very well be
part of the spectrum of so-called neurogenic stress cardiomyopathy, an increasingly acknowledged phenomenon accompanying
nearly 50% patients with brain death (8). The salient feature
of this clinical entity is its reversibility, i.e., the spontaneous
normalization of cardiac function. As such, potential heart
donors exhibiting LV dysfunction should not be readily dismissed. Time permitting, serial echocardiographic evaluations
should be conducted to document improvement. Conversely,
the absence of structural heart disease, as confirmed by coronary angiography and echocardiography, along with the absence
of cardiovascular risk factors, may itself justify acceptance for
transplantation in many of these scenarios.
January 2016
Given the exponential growth in the number of patients
with advanced heart failure and the purported shortage of donor organs, the therapeutic paradigm has increasingly evolved
towards mechanical circulatory support to meet the growing
demand. However, cardiac transplantation remains the gold
standard therapy for these patients, and the oft-reported “shortage” of donor organs may be self-imposed, where clinically
unfounded exclusion criteria are rampantly applied, thereby
disqualifying many potentially viable donor hearts. In light of
the published data, case reports such as this should not represent
isolated aberrations in clinical practice, but a growing trend in
our collective approach to heart donor selection.
—Brian Lima, MD
Department of Cardiac Surgery
Baylor University Medical Center at Dallas
(E-mail: brian.lima@baylorhealth.edu)
1.
2.
3.
4.
5.
6.
7.
8.
Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning
due to simultaneous multivessel coronary spasms: a review of 5 cases.
J Cardiol 1991;21(2):203–214.
Pelliccia F, Greco C, Vitale C, Rosano G, Gaudio C, Kaski JC. Takotsubo
syndrome (stress cardiomyopathy): an intriguing clinical condition in
search of its identity. Am J Med 2014;127(8):699–704.
Peters MN, George P, Irimpen AM. The broken heart syndrome: takotsubo
cardiomyopathy. Trends Cardiovasc Med 2015;25(4):351–357.
Ravi Y, Campagna R, Rosas PC, Essa E, Hasan AK, Higgins RSD, Emani
S, Sai-Sudhakar CB. Successful heart transplantation using a donor
heart afflicted by takotsubo cardiomyopathy. Proc (Bayl Univ Med Cent)
2016;29(1):73–74.
Mohamedali B, Bhat G, Zelinger A. Frequency and pattern of left ventricular dysfunction in potential heart donors: implications regarding use
of dysfunctional hearts for successful transplantation. J Am Coll Cardiol
2012;60(3):235–236.
Sopko N, Shea KJ, Ludrosky K, Smedira N, Hoercher K, Taylor DO,
Starling RC, Gonzalez-Stawinski GV. Survival is not compromised
in donor hearts with echocardiographic abnormalities. J Surg Res
2007;143(1):141–144.
Lima B, Rajagopal K, Petersen RP, Shah AS, Soule B, Felker GM, Rogers
JG, Lodge AJ, Milano CA. Marginal cardiac allografts do not have increased primary graft dysfunction in alternate list transplantation. Circulation 2006;114(1 Suppl):I27–I32.
Berman M, Ali A, Ashley E, Freed D, Clarke K, Tsui S, Parameshwar
J, Large S. Is stress cardiomyopathy the underlying cause of ventricular dysfunction associated with brain death? J Heart Lung Transplant
2010;29(9):957–965.
Using “broken hearts” for cardiac transplantation: a risky venture or fruitful endeavor?
75
Utility of indium-111 octreotide to identify a cardiac
metastasis of a carcinoid neoplasm
Mohammed Farooqui, MD, Sulaiman Rathore, MD, and Timothy Ball, MD, PhD
Carcinoid heart disease is classically described as right-sided
valvular pathology. Solid cardiac
metastases from carcinoid tumors
are seldom reported. A multimodality imaging approach is needed to
diagnose and localize this disease.
Biopsy remains the gold standard
to confirm the diagnosis of carcinoid. Octreotide uptake is characteristic of carcinoid tumor but
not myxoma; thus, an indium-111
octreotide scan is very specific for
the diagnosis of carcinoid tumor
and helps in assessing the extent
of carcinoid disease. We present
a case in which an indium-111
octreotide scan revealed uptake in
three distinct masses in the colon,
liver, and right ventricle. The results
of the scan were contradictory to
the biopsy results, which were diagnostic for hepatic carcinoid and
cardiac myxoma.
C
a
c
d
Figure 1. Multimodality imaging. (a) CT of the abdomen revealed a cardiac mass ( ) measuring approximately 5 cm
involving the right ventricle and interventricular septum. (b) Transthoracic echocardiogram revealed a 5.2 × 6.2 cm
homogeneous, circumscribed, infiltrating mass ( ) in the right ventricle. (c and d) Cardiac MRI demonstrated a smooth
circumscribed mass ( ) in the right ventricular inflow tract, mid-cavity, and apex measuring 4.6 × 6.1 cm in the largest
dimension, which enhances on T2 late gadolinium enhancement and signal loss with fat-saturated imaging.
arcinoid tumors are rare and aggressive malignancies with a reported prevalence of 1.2 to 2.1 per
100,000 persons in the general population per year
(1). Prompt recognition and diagnosis is of utmost
importance (2). Solid carcinoid tumors rarely metastasize,
and metastasis to the heart is even more rare (3). Carcinoid
disease is diagnosed with a composite of clinical symptoms,
5-hydroxyindoleacetic acid assessment, appropriate imaging
to localize the disease, and biopsy, which remains the confirmatory test. The telltale signs of carcinoid heart disease are
involvement of right-sided heart valves with characteristic
echocardiographic findings. Radionuclide scanning following
intravenous 111 indium–labeled octreotide (111In-DTPApentetreotide) provides a sensitive and noninvasive method
of localizing somatostatin-positive tumors (somatostatin
76
b
receptor, SS-R expressed) and to monitor the effi cacy of
treatment (4–6).
An octreotide scan has an 86% sensitivity in detecting a
carcinoid tumor (7). The false-positive rate for octreotide scans
is around 12% and is mostly due to renal parapelvic cysts, accessory spleens, ventral hernias, or thyroid or breast disease (8).
Many benign and malignant tumors are known to take up 111
indium–labeled octreotide, but uptake by myxomas has not
been described in the literature. We report an intriguing case
of a biopsy-confirmed myxoma with significant uptake on the
indium-111 octreotide scan.
From Virginia-Tech Carilion School of Medicine and Research Institute, Roanoke,
Virginia.
Corresponding author: Mohammed Farooqui, MD, 127 McClanahan Avenue,
Suite 300, Roanoke, VA 24014 (e-mail: mafarooqui@carilionclinic.org).
Proc (Bayl Univ Med Cent) 2016;29(1):76–78
a
b
c
d
Figure 2. Biopsy results. Liver biopsy with (a) synaptophysin immunohistochemistry and (b) hematoxylin and eosin staining
consistent with neuroendocrine (carcinoid) cells. (c and d) Right ventricular tissue biopsy with hematoxylin and eosin staining
depicting mucopolysaccharides suggestive of myxomatous tissue with no neuroendocrine cells, consistent with myxoma.
Given the rarity of carcinoid metastasis to the
heart, the possibility of two
unrelated primary tumors
was entertained, and an endomyocardial biopsy was
performed to make the diagnosis. The patient underwent
cardiac catheterization with
coronary angiography (Figure
3), left and right heart catheterization, along with endomyocardial biopsy of the RV
mass under fluoroscopic and
intracardiac echocardiography guidance. The specimens
obtained were adequate for
analysis and revealed findings
consistent with a benign cardiac myxoma (Figures 2c and
2d). To verify the diagnosis,
an indium-111 octreotide
scan was performed with the
expectation that the liver mass
would demonstrate uptake
while the cardiac mass would
CASE REPORT
A 48-year-old woman presented to the emergency department with severe epigastric pain. Computed tomography (CT)
of the abdomen revealed a liver mass and a cardiac mass involving the right ventricle (RV), measuring about 5 cm in diameter
(Figure 1a). A transthoracic echocardiogram confirmed a 5.2
× 6.2 cm homogeneous, well-circumscribed, infiltrating RV
mass (Figure 1b). The tricuspid valve was noted to be in close
proximity to the tumor mass. The patient subsequently underwent cardiac magnetic resonance imaging (MRI), which showed
evidence of a T2-enhancing RV mass (Figure 1c and 1d). Liver
biopsy results were positive for carcinoid (Figures 2a and 2b).
Figure 3. A right coronary angiogram demonstrating hypervascularity and tumor
perfusion from the right posterior descending and posterolateral coronary arteries.
January 2016
Figure 4. An octreotide scan revealing indium-111 octreotide uptake by the right
ventricular mass (black arrow) along with normal physiological uptake in the liver,
spleen, kidneys, and urinary bladder.
Utility of indium-111 octreotide to identify a cardiac metastasis of a carcinoid neoplasm
77
not. The octreotide scan revealed significant uptake by an undiagnosed mass in the cecum and in the liver mass; surprisingly,
the RV mass also demonstrated significant octreotide uptake
(Figure 4). This finding suggests a cecal primary with metastasis
to both the liver and the RV. Treatment of the carcinoid tumor
with octreotide was initiated, and the patient has been referred
to determine if the cardiac tumor is suitable for resection.
DISCUSSION
This case demonstrates the ability of an indium-111
octreotide scan (9–11) to aid in defining the metabolic characteristics of multiple masses suspected of being carcinoid and to
make a comprehensive assessment of the tumor burden, which
is required for the development of a comprehensive treatment
plan. More interestingly, this case reports a myxoma, confirmed
histologically at endomyocardial biopsy, that demonstrated
octreotide uptake on indium-111 octreotide scanning. Heretofore, no case of myxoma has been reported as demonstrating
octreotide uptake. We believe this case represents a case of primary carcinoid tumor with metastasis to both liver and heart
based on the results of octreotide scanning. Furthermore, this
case widens the differential for RV mass lesions (12), suggesting the consideration of a metastatic carcinoid tumor that may
present as a solid metastatic lesion to the heart.
1.
2.
78
Modlin IM, Sandor A. An analysis of 8305 cases of carcinoid tumors.
Cancer 1997;79(4):813–829.
Dobson R, Burgess MI, Pritchard DM, Cuthbertson DJ. The clinical
presentation and management of carcinoid heart disease. Int J Cardiol
2014;173(1):29–32.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
Pandya UH, Pellikka PA, Enriquez-Sarano M, Edwards WD, Schaff HV,
Connolly HM. Metastatic carcinoid tumor to the heart: echocardiographic-pathologic study of 11 patients. J Am Coll Cardiol 2002;40(7):1328–
1332.
Critchley M. Octreotide scanning for carcinoid tumours. Postgrad Med J
1997;73(861):399–402.
Janson ET, Westlin JE, Eriksson B, Ahlström H, Nilsson S, Oberg K.
[111In-DTPA-D-Phe1]octreotide scintigraphy in patients with carcinoid
tumours: the predictive value for somatostatin analogue treatment. Eur J
Endocrinol 1994;131(6):577–581.
Fuster D, Navasa M, Pons F, Vidal-Sicart S, Mateos JJ, Lomeña F, Rodes
J, Herranz R. In-111 octreotide scan in a case of a neuroendocrine tumor
of unknown origin. Clin Nucl Med 1999;24(12):955–958.
Kwekkeboom DJ, Krenning EP. Somatostatin receptor imaging. Semin
Nucl Med 2002;32(2):84–91.
Gibril F, Reynolds JC, Chen CC, Yu F, Goebel SU, Serrano J, Doppman
JL, Jensen RT. Specificity of somatostatin receptor scintigraphy: a prospective study and effects of false-positive localizations on management
in patients with gastrinomas. J Nucl Med 1999;40(4):539–553.
Krenning EP, Kwekkeboom DJ, Bakker WH, Breeman WA, Kooij PP,
Oei HY, van Hagen M, Postema PT, de Jong M, Reubi JC, Visser TJ,
Reijs AE, Hofland LJ, Koper JW, Lamberts SW. Somatostatin receptor
scintigraphy with [111In-DTPA-D-Phe1]- and [123I-Tyr3]-octreotide: the
Rotterdam experience with more than 1000 patients. Eur J Nucl Med
1993;20(8):716–731.
Yarbro JW, Bornstein RS, Mastrangelo MJ, eds. Somatostatin receptor
imaging: tumor localization, detection, and therapeutic implications.
Semin Oncol 1994;21(Suppl 13):1–71.
Krenning EP, Kwekkeboom DJ, Pauwels S, Kvols K, Reubi JC. Somatostatin receptor scintigraphy. In Freeman LM, ed. Nuclear Medicine Annual
1995. New York: Raven, 1995:1–5.
Gopal AS, Stathopoulos JA, Arora N, Banerjee S, Messineo F. Differential
diagnosis of intracavitary tumors obstructing the right ventricular outflow
tract. J Am Soc Echocardiogr 2001;14(9):937–940.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Angiosarcoma of the right atrium presenting as hemoptysis
Charles H. Choi, MD, Subbareddy Konda, MD, and Jay G. Shake, MD
This case report describes a previously healthy 32-year-old man who
presented with several weeks of hemoptysis. Initially he was treated with
antibiotics with a preliminary diagnosis of pneumonia. With increasing
hemoptysis and additional symptoms, he was referred to our institution.
Cardiac magnetic resonance imaging suggested a diagnosis of right
atrial angiosarcoma with extensive pulmonary metastases. His extensive
pulmonary tumor burden caused the hemoptysis. Pulmonary biopsy was
well tolerated, and he was referred to medical oncology for adjuvant therapy. Following the first cycle of chemotherapy, his hemoptysis lessened.
P
rimary cardiac angiosarcoma is rare (1). It is typically
located in the right atrium and manifests as right-sided
heart failure or cardiac tamponade (2–4). Most patients
are symptomatic at presentation and when disease is
discovered, it is often late in its course, resulting in a poor prognosis. We describe a case of cardiac angiosarcoma first presenting
with hemoptysis due to the large pulmonary metastasis burden.
CASE PRESENTATION
A healthy 32-year-old man presented to his physician after
2½ weeks of hemoptysis. He was started on antibiotics for suspected pneumonia. Over the next few weeks, the hemoptysis
worsened and he developed abdominal pain and was referred
to our institution. On arrival he was dyspneic, hypotensive, and
tachycardic. Examination revealed distended jugular veins, distant heart sounds, and diminished lung sounds at the bases. A
transthoracic echocardiogram demonstrated a large circumferential pericardial effusion with evidence of cardiac tamponade.
Emergent pericardiocentesis evacuated 500 mL of serosanguinous
fluid, and agitated saline injected into the pericardium revealed
a large mass in the wall of his right atrium. Cardiac magnetic
resonance imaging demonstrated the extent of the mass and its
involvement of surrounding tissue. A multiplanar half-Fourier
single-shot turbo spin-echo (HASTE) examination and steadystate free precession cine magnetic resonance imaging revealed
a 3 × 4 cm tumor invading the right atrium. The right coronary
artery was encased in the tumor and dynamic first-pass perfusion
(TurboFLASH) images suggested that the mass was extremely
well vascularized. Numerous bilateral pulmonary nodules were
seen, along with bilateral pleural effusions. A mini-right anteProc (Bayl Univ Med Cent) 2016;29(1):79–80
rior thoracotomy was performed in the fourth intercostal space.
Approximately 800 mL of sanguinous pleural fluid was evacuated, and a pericardial window was produced. The right atrial
mass was easily palpable and well visualized through the incision.
The right lung was full of numerous transparent bright pink to
dark purple masses, from a few millimeters to roughly 2 cm in
diameter (Figure), and were easily amenable to a wedge biopsy.
A reticulating Endo GIA stapler was used to resect several of the
lung masses. Microscopic sections showed metastatic angiosarcoma. The patient tolerated the procedure well and was referred to
medical oncology for adjuvant therapy. Following the first cycle of
chemotherapy, he had significant improvement in his hemoptysis.
DISCUSSION
Primary cardiac angiosarcomas are rare. Most patients
present with symptoms related to heart failure. The patient
described here had numerous extensive pulmonary metastases
and hemoptysis. Some common chest radiographic findings
include a generalized globular and massive cardiac silhouette
with a prominent right cardiac border (3). The majority of the
primary tumor site is located in the right atrium, and the most
common site for metastasis is the lung or the pericardium (3).
Echocardiography confirms the diagnosis of a cardiac mass.
Computed tomography scanning has been a valuable adjunct
to echocardiography. Magnetic resonance imaging is rapidly
becoming the imaging modality of choice for evaluating pericardial and cardiac tumors due to its accurate evaluation of the mass
and extension into neighboring structures. In addition, tumor
types have characteristic magnetic resonance imaging findings
that can often offer a diagnosis even before an invasive means.
Cine magnetic resonance imaging can also aid in the evaluation of cardiac function in the case of large obstructing masses.
From the Division of Cardiothoracic Surgery, Department of Surgery, Texas A&M
Health Science Center at Scott & White Memorial Hospital, Temple, Texas (Choi,
Konda, Shake); the Department of Medicine, Wake Forest University Baptist
Medical Center, Winston-Salem, North Carolina (Choi); and the Division of
Cardiothoracic Surgery, Department of Surgery, University of Mississippi Medical
Center, Jackson, Mississippi (Shake).
Corresponding author: Jay G. Shake, MD, MS, Division of Cardiothoracic
Surgery, Department of Surgery, University of Mississippi Medical Center, 2500
N. State Street, Jackson, MS 39216 (e-mail: jshake@umc.edu).
79
a
b
Figure. Right lung masses. Numerous pulmonary masses were seen and many were peripherally located, ideal for wedge resection biopsy. The right lung was full of
numerous transparent bright pink (smaller white arrows) to dark purple masses (large white arrow), from a few millimeters to roughly 2 cm in diameter.
1.
2.
Strans R, Merliss R. Primary tumor of the heart. Arch Pathol Lab Med
1945;39:74–78.
Majano-Lainez RA. Cardiac tumors: a current clinical and pathological
perspective. Crit Rev Oncog 1997;8(4):293–303.
3.
4.
Meng Q, Lai H, Lima J, Tong W, Qian Y, Lai S. Echocardiographic and
pathologic characteristics of primary cardiac tumors: a study of 149 cases.
Int J Cardiol 2002;84(1):69–75.
Glancy DL, Morales JB Jr, Roberts WC. Angiosarcoma of the heart. Am
J Cardiol 1968;21(3):413–419.
Avocations
Snow Day at Lakeside, Highland Park, Texas. Photo copyright © Rolando M. Solis, MD. Dr. Solis (e-mail: rmsolis@mac.com) is an interventional cardiologist with
Baylor Scott and White Health and practices at Baylor Medical Center at Garland and The Heart Hospital Baylor Plano.
80
Baylor University Medical Center Proceedings
Volume 29, Number 1
Rupture of a left internal mammary artery during
cardiopulmonary resuscitation
Chhaya Patel, MD, Austin Metting, MD, Brydan Curtis, DO, and Timothy Mixon, MD
We present a rare case of a left internal mammary artery rupture during cardiopulmonary resuscitation (CPR). This case demonstrates that
intrinsic cardiac/vascular injuries can occur even with manual CPR, and
each patient should be monitored closely, considering the very subtle
signs that can clue the physicians into the diagnosis.
C
ardiopulmonary resuscitation (CPR) has the potential
to cause a myriad of complications, the most common
of which include rib fractures, lung injury such as pneumothorax or aspiration pneumonia, abdominal organ
injury, and chest/abdominal pain (1). Injuries during CPR are
more commonly seen when using mechanical rather than human compression-decompression devices (1). Our case discusses
a complication involving rupture of the left internal mammary
artery (LIMA) after manual CPR.
CASE PRESENTATION
An 80-year-old man with previous heart failure, atrial fibrillation, recent cardioversion, and venous thromboembolism on warfarin presented to the emergency department with
complaints of syncope while at rest. He was bradycardic on
telemetry, and his international normalized ratio was 3.4. On
day 2, he began complaining of heartburn. Telemetry showed
sinus rhythm with numerous atrial and ventricular premature
complexes. A few minutes later he had cardiac arrest and was
found to be in ventricular fibrillation. Advanced cardiac life
support was started, and there was return of spontaneous circulation after one round of CPR and one defibrillation shock.
A follow-up electrocardiogram showed atrial fibrillation with
rapid ventricular response and a right bundle branch block. He
was fully awake and alert after resuscitation. A transthoracic
echocardiogram revealed a dilated ventricle with paradoxical
septal motion, global left ventricular systolic dysfunction, and
tachycardia with an ejection fraction of 30%.
The patient complained of chest pain after CPR, which
persisted through the night despite pain medication. He slowly
Proc (Bayl Univ Med Cent) 2016;29(1):81
became more hypotensive, eventually requiring vasopressor
support. A scan showed a mediastinal hematoma and a large
right-sided hemothorax with leftward mediastinal shift. The
computed tomography scan was unable to localize the bleeding
source. Selective angiography showed active extravasation of the
LIMA. The LIMA was embolized and a right-sided chest tube
was placed. He received a blood transfusion and was successfully liberated from vasopressors, but ultimately died 7 days
after the resuscitation.
DISCUSSION
Many cardiac complications can occur after CPR, such as
atrial and ventricular rupture, papillary muscle tear, cardiac
hemorrhage, and vascular injuries. More common but often
unrecognized complications include pulmonary fat embolus,
occurring in 20% of nonsurvivors of CPR, as well as sternal
fractures (2). Our case is unusual because it reveals a rare complication of CPR: rupture or avulsion of the internal mammary
artery. In this case, it was fairly subtle and managed to go unnoticed until the patient became hemodynamically unstable. In
the case of cardiac injuries, cardiac and pericardial injury may
occur in the absence of associated thoracic injury, making the
post-CPR diagnosis challenging (3).
1.
2.
3.
Nagel EL, Fine EG, Krischer JP, Davis JH. Complications of CPR. Crit
Care Med 1981;9(5):424.
Miller AC, Rosati SF, Suffredini AF, Schrump DS. A systematic review
and pooled analysis of CPR-associated cardiovascular and thoracic injuries.
Resuscitation 2014;85(6):724–731.
Platenkamp M, Otterspoor LC. Complications of mechanical chest
compression devices. Neth Heart J 2014;22(9):404–407.
From the Division of Internal Medicine (Patel, Metting) and the Division of
Interventional Cardiology (Curtis, Mixon), Department of Medicine, Baylor Scott
and White Health, Temple, Texas.
Corresponding author: Chhaya Patel, MD, MS-01-161B, Division of Internal
Medicine, Department of Medicine, Baylor Scott and White Health, 2401 South
31st Street, Temple, TX 76508 (e-mail: cpatel@sw.org).
81
High-intensity cardiac rehabilitation training of a commercial
pilot who, after percutaneous coronary intervention,
wanted to continue participating in a rigorous strength and
conditioning program
Sanjay Shrestha, BS, Jenny Adams, PhD, Anne Lawrence, RN, and Jeffrey M. Schussler, MD
After undergoing elective percutaneous coronary intervention, a 64-yearold commercial pilot was referred to cardiac rehabilitation. His stated
goals were to continue participating in a rigorous strength and conditioning program at a community workout facility and to resume working
as a pilot. To help him meet those goals, we designed and implemented
a regimen of high-intensity exercises, with quick transitions between a
variety of tasks that are not typically included in cardiac rehabilitation
programs (e.g., medicine ball throws, push-ups, dead lifts, squats, military presses, sprints, and lunges). The training was symptom limited,
enabling the patient to reach extreme levels of physical exertion in a
controlled, monitored setting. By studying his training data (heart rate,
blood pressure, and rating of perceived exertion), we were able to give
him specific recommendations for controlling his exercise intensity after
graduating from our program. More than 18 months later, he continues
to exercise vigorously 3 days per week and is working as a commercial
pilot.
I
nstead of capping peak exercise intensity during cardiac
rehabilitation (CR), we use a symptom-limited approach
and offer customized high-intensity training for patients
who have a strong desire to return to strenuous activities.
We report the unconventional CR regimen of one such patient and the exercise prescription we provided for his future
workouts.
CASE REPORT
A 64-year-old commercial pilot with previous hypertension saw a cardiologist because of a recent marked decrease in exercise tolerance. A longtime fitness enthusiast,
the patient participated regularly in a rigorous strength and
conditioning program at a community workout facility. A
nuclear stress test showed an anteroseptal reversible defect.
Left-sided heart catheterization revealed a left ventricular
ejection fraction of 60%, normal wall motion, and severe
obstructive coronary artery disease in the mid left circumflex. Placement of a drug-eluting stent in that narrowing
resulted in a TIMI (thrombolysis in myocardial infarction)
flow of grade 3 with no stenosis. The patient was subsequently referred to CR.
82
At CR enrollment, the patient’s lipid levels (reported as
mg/dL) were as follows: total cholesterol, 187; high-density
lipoprotein cholesterol, 57; low-density lipoprotein cholesterol,
120; and triglycerides, 77. His family history was negative for
premature coronary artery disease, and his physical examination
was unremarkable. His body mass index was 25.7 kg/m2 and
his waist circumference was 39.5 inches. Medications included
omeprazole, simvastatin, lisinopril, aspirin, and clopidogrel.
When asked about his goals for CR, the patient indicated that
he wanted to be fit so he could 1) participate confidently in the
strength and conditioning program and 2) resume and maintain
his job as a commercial pilot.
With the use of our facility’s specificity of training equipment, we designed and implemented a regimen of highintensity exercises that mimicked the modes and progressions
of the strength and conditioning program. CR staff members
provided the clinical testing and exercise training over the
course of 30 sessions. Each exercise session started with a warmup and ended with a cool-down. The patient’s heart rate and
rhythm were monitored by telemetry throughout each session.
Blood pressure was measured before the warm-up, during peak
exercise, and after the cool-down was completed. The patient
reported his rating of perceived exertion (RPE; scale, 1 to 10)
at peak exercise.
The first two exercise sessions were standard CR workouts
that allowed the nurse to evaluate the patient’s vital signs in
response to exercise and to ensure that he had no adverse symptoms that would preclude continued training. We recorded
From the Department of Kinesiology, University of Texas at Arlington (Shrestha);
the Cardiac Rehabilitation Department, Baylor Jack and Jane Hamilton Heart
and Vascular Hospital (Adams, Lawrence, Schussler); and Texas A&M College
of Medicine (Schussler). Mr. Shrestha is now with the Carter Rehabilitation and
Fitness Center at Baylor All Saints Medical Center in Fort Worth.
Grant support was provided by the Harry S. Moss Heart Trust and the Baylor Health
Care System Foundation, Dallas, Texas, through the Cardiovascular Research
Review Committee and in cooperation with the Baylor Heart and Vascular Institute.
The authors thank the committee for their continued support of cardiovascular
rehabilitation research projects.
Corresponding author: Jenny Adams, PhD, Cardiac Rehabilitation Department,
Baylor Heart and Vascular Hospital, 411 N. Washington, Suite 3100, Dallas, TX
75246 (e-mail: jennya@BaylorHealth.edu).
Proc (Bayl Univ Med Cent) 2016;29(1):82–84
a
c
b
Figure. The patient performing (a) a box jump, (b) a kettlebell swing, and (c) a military press.
complete blood pressure data during 28 of the 30 sessions.
The 3rd and 30th sessions included a metabolic treadmill stress
test during which the patient’s oxygen consumption data were
captured by a calibrated desktop metabolic system (Fitmate
MED, Cosmed USA Inc., Chicago, IL). The maximal stress test
protocols included 3-minute stages at speeds of 1.7 to 5 mph
and changes in grade from 0% to 20%. American College of
Sports Medicine guidelines were followed to determine the end
of the test (1).
The remaining 26 sessions consisted of high-intensity exercises, with quick transitions between a variety of tasks such as
a medicine ball run, rope-jumping, box jumps, sit-ups, planks,
kettlebell swings, medicine ball throws, push-ups, dead lifts,
squats, military presses, sprints, and lunges (Figure). During
these sessions, the patient had no arrhythmias, angina pectoris,
or other adverse events that would have required the training
to be stopped.
The patient’s mean peak blood pressure and heart rate values
during these high-intensity sessions were 202/75 mm Hg and
160 beats/minute, respectively, and his mean rating of perceived
exertion was 8. His highest peak heart rate was 172 beats/minute
during one high-intensity session. During another, his systolic
blood pressure reached 270 mm Hg; this was one of 5 sessions
in which his rate-pressure product (RPP, calculated by multiplying heart rate and systolic blood pressure) exceeded 36,000,
which we use as a cautionary threshold for training intensity.
His highest RPP was 45,090.
DISCUSSION
With our symptom-limited approach to CR training, the
patient was able to reach extreme levels of physical exertion in
January 2016
a controlled, monitored setting. A thorough review of the heart
rate, blood pressure, RPP, and RPE data from his high-intensity
CR sessions enabled us to identify specific exercise modes and
progressions that caused his RPP to exceed 36,000. As a result,
we advised him to avoid those combinations in the future, when
he would be exercising without our supervision. We also recommended that he wear a heart rate monitor to control his exercise
intensity after graduating from CR, as it was unlikely that he
would monitor his blood pressure while exercising on his own.
Upon graduation, his exercise prescription was to keep his RPP
under 36,000; to meet that goal, we advised him to limit his
heart rate to 160 beats/minute.
Commercial pilots are required to undergo an annual or a
biannual medical examination during which they are screened
for medical conditions that could impair their ability to pilot.
Because their continued employment depends on maintaining
good health, most pilots are motivated to maintain a healthy
lifestyle (2). According to the Federal Aviation Administration’s Guide for Aviation Medical Examiners, pilots who have
undergone coronary angioplasty must perform a graded exercise stress test for at least 9 minutes (which is equal to 10
metabolic equivalents) and reach 100% of their age-predicted
maximal heart rate (3). During his final stress test in CR,
the patient reached not only his age-predicted maximal heart
rate of 157 beats/minute but also 15 metabolic equivalents, a
value that ranks him between the 95th and 100th percentiles
of the physical fitness standards for men aged 56 to 65 years
(4). More than a year after graduating from the CR program,
he remains active as a pilot and stays in shape by performing
rigorous workouts 3 days a week, with no negative cardiovascular symptoms.
High-intensity cardiac rehabilitation training
83
Acknowledgments
We thank the patient for allowing his story and photos to
be published. We also thank Beverly Peters, MA, ELS, for help
in preparing the manuscript.
1.
American College of Sports Medicine. ACSM’s Guidelines for Exercise
Testing and Prescription, 9th ed. Philadelphia: Wolters Kluwer/Lippincott
Williams & Wilkins Health, 2014:131.
2.
Sykes AJ, Larsen PD, Griffiths RF, Aldington S. A study of airline pilot
morbidity. Aviat Space Environ Med 2012;83(10):1001–1005.
3. Federal Aviation Administration. Decision considerations: disease
protocols—graded exercise stress test requirements. 2015 Guide for
Aviation Medical Examiners. Available at https://www.faa.gov/about/
office_org/headquarters_offices/avs/offices/aam/ame/guide/dec_cons/
disease_prot/graded_exercise/; accessed August 31, 2015.
4. Pollock ML, Wilmore JH. Exercise in Health and Disease: Evaluation and
Prescription for Prevention and Rehabilitation, 2nd ed. Philadelphia: W.B.
Saunders, 1990:684, 676.
Reader comments
HEALTHCARE PROFESSIONALS SHOULD SEPARATE THEIR
PERSONAL AND PROFESSIONAL SOCIAL MEDIA
everal problems have recently been highlighted (1)
with the recommendations from the American College of Physicians and the Federation of State Medical Boards (2), which urge physicians to separate
their personal and professional social media. DeCamp et al.
(1) argued that this separation is impossible. They described
the following problems with the guidelines: there is a lack
of user consensus about the guidelines, the separation of
online identities is operationally impossible and is inconsistent with the general concept of professional identity, and
maintaining two identities can generate a psychological or
physical burden.
The term social media is usually applied to describe the
various types of media content that are publicly available
and created by end users (3). Kaplan et al. (3) have proposed
a classification of social media that includes collaborative
projects (e.g., Wikipedia), blogs or microblogs (e.g., Wordpress, Twitter), content communities (e.g., Flickr, YouTube),
social networking sites (e.g., Facebook, LinkedIn), virtual
game worlds (e.g., Xbox, PlayStation), and virtual social
worlds (e.g., Second Life). However, having two or more
social media accounts does not mean having more than
one identity.
On Facebook, people often share family time by uploading
photos from vacations and special events, share videos from
parties with people who did not attend, invite coworkers to
office events, and play games with friends. However, as a physician, would you be comfortable sharing these things with your
patients or professional society? I would not want to share personal photos and videos with people in my professional world.
S
84
Healthcare professionals should exclude the public and their
patients from their social media profiles.
One way to clarify your goals is to formulate a personal
social media strategy. For example, if you want to maintain
contact with your family and friends, Facebook is an appropriate venue, but if you want to collaborate with your professional
society and peers, LinkedIn or Twitter is appropriate (4). Interconnecting various types of social media is easy, and the user
can decide how the different types interconnect. Social media is
a relatively new concept that is continually being transformed
(5) and is also now a permanent fixture in society; social media
are here to stay. Proactive participation in social media can be
a powerful tool, but healthcare professionals should choose the
platform that is right for them.
—Silvio A. Ñamendys-Silva, MD, MSc
Instituto Nacional de Cancerología
Mexico City, Mexico
E-mail: snamendys@incan.edu.mx
1.
2.
3.
4.
5.
DeCamp M, Koenig TW, Chisolm MS. Social media and physicians’
online identity crisis. JAMA 2013;310(6):581–522.
Farnan JM, Snyder Sulmasy L, Worster BK, Chaudhry HJ, Rhyne
JA, Arora VM. Online medical professionalism: patient and public
relationships. Policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med
2013;158(8):620–627.
Kaplan AM, Haenlein M. Users of the world, unite! The challenges and
opportunities of social media. Bus Horiz 2010;53(1):59–68.
Dutta S. What’s your personal social media strategy? Harv Bus Rev
2010;88(11):127–130, 151.
Hamm MP, Chisholm A, Shulhan J, Milne A, Scott SD, Given LM,
Hartling L. Social media use among patients and caregivers: a scoping
review. BMJ Open 2013;3(5):e002819.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Electrocardiogram read by the computer as arm-lead
reversal
D. Luke Glancy, MD, Roberto E. Quintal, MD, PhD, and Timothy D. McShurley, MD
Figure 1. Electrocardiogram recorded with the leads in the usual locations. See text for explication.
T
he electrocardiogram shown in Figure 1 was read by the
computer as arm-lead reversal. The computer reading
went on to say that no further analysis would be attempted. This clearly is a programming mistake because
the precordial leads make the diagnosis.
Although we would estimate that 95% of electrocardiograms
with negative P, QRS, and T waves in lead I are due to armlead reversal, a small number are due to situs inversus totalis
with mirror-image dextrocardia. In this condition, the left-sided
precordial leads show progressive diminution in the size of the
complexes from leads V1 to V6 as the leads are placed ever
farther away from the right-sided heart (Figure 1). In contrast,
the left-sided precordial leads are unaffected by simple arm-lead
reversal. Another diagnostic point is that the QRS morphology is
similar in leads I and V6 in mirror-image dextrocardia, whereas
it is quite different in those leads in simple arm-lead reversal (1).
Situs inversus totalis with mirror-image dextrocardia is perhaps the most common of the congenital cardiac malpositions
Proc (Bayl Univ Med Cent) 2016;29(1):85–86
and is only infrequently associated with hemodynamically
significant congenital cardiac malformations. In contrast, situs
solitus with congenital dextrocardia, sometimes called isolated dextrocardia or dextroversion, is usually associated with
significant malformations, as is situs inversus with isolated
levocardia (2).
This patient, a 52-year-old man, came to the hospital
because of intermittent leg claudication with walking. He had
no other cardiovascular symptoms. When the limb leads were
reversed and the precordial leads were recorded on the right side
of the chest (Figure 2), his electrocardiogram was normal except
for voltage criteria for left ventricular hypertrophy, probably due
to systemic arterial hypertension (3).
From the Sections of Cardiology, Louisiana State University Health Sciences
Center and the Touro Infirmary, New Orleans, Louisiana.
Corresponding author: D. Luke Glancy, MD, 1203 West Cherry Hill Loop, Folsom,
LA 70437 (e-mail: dglanc@lsuhsc.edu).
85
Figure 2. Electrocardiogram recorded with the limb leads reversed and the precordial leads on the right side of the chest. See text for explication.
1.
2.
86
Harumi K, Chen CY. Miscellaneous electrocardiographic topics.
Artifactual ECG abnormalities. In MacFarlane PW, Lawrie TDV, eds.
Comprehensive Electrocardiology. Theory and Practice in Health and Disease,
Volume 1. New York: Pergamon Press, 1989:715–720.
Hagler DJ, O’Leary PW. Cardiac malpositions and abnormalities of atrial
and visceral situs. In Allen HD, Gutgesell HP, Clark EB, Driscoll DJ,
3.
eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents,
Including the Fetus and Young Adults, 6th ed. Philadelphia: Lippincott
Williams & Wilkins, 2001:1151–1164.
Sokolow M, Lyon TP. Th e ventricular complex in left ventricular
hypertrophy as obtained by unipolar precordial and limb leads. Am
Heart J 1949;37(2):161–186.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Baylor news
■ Newly identified biomarker may
help doctors predict colon cancer
progression and personalize therapy
Researchers at Baylor Research Institute
have identified a small RNA molecule, SNORA42,
that appears to enable certain colorectal cancers
to become especially aggressive, resistant to
treatment, and likely to migrate and invade normal tissue. This is the first RNA molecule of its
kind to be identified as a biomarker for colorectal
cancer. Because this type is more stable than
other RNA molecules, the researchers believe
noninvasive blood or stool tests eventually
may be developed to quickly and easily detect
SNORA42 and other biomarkers that may be
discovered in the future.
“The majority of patients with stage 2
colorectal cancer will be cured with surgery
alone, but some will relapse and eventually die.
Molecular biomarkers, such as SNORA42, could
help determine which patients might have a better prognosis with more aggressive treatment.
They also provide us with targets for the development of very specific, personalized anticancer
interventions,” said Ajay Goel, PhD, director of
the Center for Gastrointestinal Cancer Research
at Baylor Research Institute, the study’s lead
investigator and senior author of an article in
the October 15, 2015, issue of Gut.
Goel and his colleagues studied levels of
SNORA42 in six established colorectal cancer
cell lines and in 250 samples of cancer tissue
taken from patients, comparing these with
24 matched specimens from normal tissue.
According to their results, SNORA42 was overexpressed in colorectal cancer cells, compared
with normal tissue, and its expression significantly correlated with disease progression.
Overexpression resulted in cancer cells’ ability
to multiply rapidly, form tumors, migrate, invade
normal tissue, and survive a natural cell death
process. Additionally, when SNORA42 was experimentally suppressed, these effects were
reversed, and elevated expression appeared to
be a predictor for recurrence and poor prognosis
in patients with colorectal cancer.
■ Stand up to Cancer® melanoma
research trial expands to Texas
Baylor Charles A. Sammons Cancer Center
at Dallas, in collaboration with the Translational
Genomics Research Institute (TGen), is helping
launch a multicenter clinical trial that will investigate the application of innovations in precision
medicine to treat advanced melanoma. Baylor
Sammons Cancer Center is the only clinical site
in Texas to offer this clinical trial, sponsored by
Stand up to Cancer (SU2C) and the Melanoma
Research Alliance. These clinical trials are the
culmination of nearly 4 years of research under
a SU2C Melanoma Dream Team grant.
The study leverages advances in genomics,
informatics, and health information technology,
which may yield more precise medical treatments
for patients with this devastating disease. It is
unique in researching more than 20 different
treatment options in a single trial. By leveraging the power of cancer genomics, researchers
believe they can provide each patient with the
best drug for his or her individual situation. This
design offers patients a huge advantage over the
old model of treating all patients the same way
and testing only one drug at a time.
“Inherent in the phrase ‘trial and error’ is
the word error. This new way of approaching
cancer therapy greatly increases the chance of
getting the right treatment to the right patient
the first time, without having to try multiple treatments, hoping to find one that works,” said Alan
Miller, MD, chief of oncology for Baylor Scott &
White Health–North Texas. “By offering over 20
different investigational treatments directed by
analyzing the tumor at the molecular level, the
odds of successful outcomes should increase
dramatically. We are honored to be part of the
SU2C team.”
■ New device for heart failure patients
offers “smart pillow” monitoring
Patients with moderate heart failure have a
new option to help manage their chronic disease and reduce their chance of being readmitted to a hospital. Cardiologists on the medical
staff at Baylor Jack and Jane Hamilton Heart
and Vascular Hospital recently implanted a new
miniaturized, wireless heart monitoring sensor
ACCOLADES
Steve Hoeft, senior vice president of operations excellence, and Robert W. Pryor, MD,
president and chief medical officer, received the
Shingo Research and Professional Publication
Award for their recently released book, The Power
of Ideas to Transform Healthcare: Engaging Staff
by Building Daily Lean Management Systems.
The publication shows how all employees can
generate ideas and solutions that lead to better
health care for patients.
Scott & White Hospital–Round Rock
earned the 2015 Mission: Lifeline® Gold Plus
Receiving Center award from the American
Heart Association/American Stroke Association.
Baylor Medical Center at Garland and Baylor
Regional Medical Center at Grapevine both
earned the Silver Plus Receiving Center award.
Proc (Bayl Univ Med Cent) 2016;29(1):87–90
These honors recognize a hospital’s commitment to and success in providing prompt,
evidence-based treatment for patients suffering
from the most deadly type of heart attack, STelevation myocardial infarction.
Scott & White Hospital–Round Rock received renewal of its full accreditation with percutaneous coronary intervention from the Society
of Cardiovascular Patient Care. The Accredited
Chest Pain Center’s protocol-driven and systematic approach to patient management allows
physicians to reduce time to treatment during the
critical early stages of a heart attack and to better
monitor patients when it is not clear whether or
not they are having a coronary event.
Baylor Jack and Jane Hamilton Heart
and Vascular Hospital and The Heart
Hospital Baylor Plano were named by
Becker’s Hospital Review among the “150
Great Places to Work in Healthcare.” Baylor
Heart and Vascular Hospital was recognized
in part for its “Stupid List,” which asks employees to tell leadership what is ineffective
around the organization. As for The Heart
Hospital Baylor Plano, Becker’s noted its
92.4% employee retention rate and its commitment to supporting employees’ education
goals.
Baylor Scott & White–Irving’s comprehensive wound center has received accreditation from the Undersea and Hyperbaric Medical
Society. Out of over 1200 hyperbaric facilities in the United States, only 214 have been
accredited.
87
that’s designed to communicate with a “smart
pillow” and then transmit critical information to
a clinician on a regular basis. The implantable
monitor, smart pillow, and home monitoring unit
comprise the US Food and Drug Administration–
approved heart monitoring system.
During a surgical procedure, the team implants the miniaturized, wireless monitor into
the patient’s pulmonary artery. The patient then
receives the smart pillow and an electronic unit
for the home. Through education provided at
the hospital, the patient learns the importance
of lying on the smart pillow at approximately
the same time daily. The patient presses a button on his or her external monitoring unit and
listens for the pillow to “speak,” indicating that
readings are successfully occurring. The smart
pillow communicates via safe radiofrequency to
the device implanted into the patient’s pulmonary artery. The implant has a microelectronic
medical system. Once the readings are finished,
typically in 2 to 3 minutes, the pillow tells the
patient that the reading is finished.
UPCOMING CME PROGRAMS
The A. Webb Roberts Center for Continuing Education of Baylor Scott & White Health is
offering the following programs:
Complex Care: Treatment Trends and Improved Outcomes, January 16, 2016, Royal
Oaks Country Club, Dallas, Texas
Direct Anterior Hip Approach–Orthopedic Workshop, February 13, 2016, Baylor
University Medical Center at Dallas (limited to 12 orthopedic surgeons)
19th Annual Tyler Breast Cancer Conference, March 18, 2016, Harvey Convention
Center, Tyler, Texas
Second Annual Skin Cancer Conference, April 2, 2016, Baylor Charles A. Sammons
Cancer Center, Dallas, Texas
IBD Conference, April 16, 2016, Roberts Hospital, 17th Floor Conference Center, Dallas, Texas
Palliative Care and Oncology, April 16, 2016, Baylor Charles A. Sammons Cancer Center,
Dallas, Texas
Third Annual Oncology Update for Primary Care Providers, April 30, 2016, Sheraton
McKinney, McKinney, Texas
Seventh Annual Stroke and Neurological Disease Conference, May 21, 2016, Westin
Galleria, Dallas, Texas
For more information, call 214.820.2317 or visit www.cmebaylor.org.
RECENT GRANTS
• Aspirin and cancer prevention
in Lynch syndrome: from cell to
population data
Principal investigator: Ajay Goel, PhD
Sponsor: National Cancer Institute
Funding: $571,122
Award period: 9/1/2015–8/31/2016
• Patient-centric risk model for medication
safety during care transitions
Principal investigator: Yan Xiao, PhD
Sponsor: Agency for Healthcare Research
and Quality
Funding: $498,484
Award period: 9/30/2015–9/29/2016
• Physically realistic virtual surgery
Principal investigator: Ganesh
Sankaranarayanan, PhD
Sponsor: Rensselaer Polytechnic
Institute/National Institutes of Health
Funding: $67,473
Award period: 7/1/2015–7/31/2016
• Development and validation of virtual
electrosurgical skill trainer (VEST)
Principal investigator: Ganesh
Sankaranarayanan, PhD
Sponsor: Rensselaer Polytechnic
Institute/National Institutes of Health
Funding: $41,265
Award period: 7/1/2015–8/31/2015
88
• A human lung-oriented approach to
correlates of risk in tuberculosis—the
TB-HART study
Principal investigator: Tawanda Gumbo, MD
Sponsor: University of Cape Town Lung
Institute
Funding: $438,288
Award period: 12/1/2014–12/31/2017
• Pharmacometric optimization of
second-line drugs for multidrug
resistant tuberculosis treatment
Principal investigator: Tawanda Gumbo,
MD
Sponsor: University of Cape Town/National
Institutes of Health
Funding: $22,393
Award period: 2/15/2015–1/31/2016
• Glycemia reduction approaches in
diabetes: a comparative effectiveness
study (GRADE)
Principal investigator: Priscilla Hollander,
MD, PhD
Sponsor: George Washington University/
National Institutes of Health
Funding: $237,491
Award period: 8/1/2015–7/31/2016
• Immune tolerance network
Principal investigator: Goran Klintmalm,
MD, PhD
Baylor University Medical Center Proceedings
Sponsor: Benaroya Research Institute/
National Institutes of Health
Funding: $39,029
Award period: 2/1/2015–1/31/2016
• Hepatitis B research network clinical
centers
Principal investigator: Robert Perillo, MD
Sponsor: UT Southwestern/National
Institutes of Health
Funding: $140,000
Award period: 9/1/2015–5/31/2016
• North Texas traumatic brain injury
model system
Principal investigator: Shahid Shafi, MD,
MPH
Sponsor: Administration for Community
Living/Disability and Rehabilitation
Research Program
Funding: $447,500
Award period: 9/30/2015–9/29/2016
• Immune activation and isoniazid
metabolism in HIV tuberculosis
Principal investigator: Tawanda Gumbo,
MD
Sponsor: University of Pennsylvania/
National Institute of Allergy and Infectious
Diseases
Funding: $40,694
Award period: 4/1/2015–8/31/2015
Volume 29, Number 1
PHILANTHROPY NOTES
■ Largest provider of highly trained
assistance dogs opens flagship
Texas training center in first-ever
collaboration with a health care
system
A series of events in November marked
the opening of Canine Companions for
Independence at Baylor Scott & White Health–
Kinkeade Campus, the first assistance dog
training center campus in the nation connected
to a health care system. The campus will provide
highly trained assistance dogs and ongoing
support cost-free to individuals with physical
and developmental disabilities who qualify
through the application process. “We have a
long history of innovation and collaboration,
and we are proud to add this moment to that
history,” said Joel T. Allison, CEO of Baylor Scott
& White Health. “This is another example of how
we’re working to take care of the total patient.”
The events kicked off with a private preview
for donors, to thank those who have helped
Baylor Health Care System Foundation raise
more than $7.2 million in support of this
initiative, including a $2 million pledge from
The Hal and Diane Brierley Foundation and
a $2 million grant from The Rees-Jones
Foundation. The following day, the Kinkeade
Campus held its first graduation ceremony.
This celebration marks the end of an assistance
dog’s professional training and the beginning
of a partnership between a human in need and
a canine that will provide endless service and
companionship. The four teams of graduates
included US Army Captain Michael Caspers,
who was honored for his service during the
halftime show of the Dallas Cowboys Veterans
Day game, with his service dog, Vincent, at
his side.
The new campus will serve children,
veterans, and other people with disabilities
whose independence and quality of life would
benefit from an assistance dog. Professionals
working for organizations that provide physical
“Even with good medications and appropriate
dietary monitoring, patients can decompensate,”
said Shelley Hall, MD, chief of transplant cardiology,
mechanical circulatory support, and heart failure,
Baylor University Medical Center. “When this occurs, many heart failure patients experience excess fluid, high blood pressure, and inflammation.
Patients may wait until a situation is nearly critical
January 2016
or mental health care to clients who would
benefit from interaction with a facility dog are
also encouraged to apply. The new campus
will eventually be able to graduate up to 60
dog and recipient teams per year.
■ New models of care for older adults
Earlier this year, Baylor Health Care System
Foundation received a $6.9 million grant from
the Deerbrook Charitable Trust. This significant
grant will help Baylor Scott & White Health test
a new model of care that aims to keep one
of our most vulnerable groups of patients,
older adults, out of hospitals by focusing on
prevention and wellness. This new model
would help expand the capacity of primary
care practices for high-risk older adults in
Baylor-affiliated primary care practices by
adding clinical pharmacists, licensed social
workers, and community health workers.
This newest project builds on momentum
from an earlier project also funded by a grant
from the Deerbrook Charitable Trust. The goal
of the program was to reduce readmissions
by using a risk-stratification software tool
that helped predict whether a patient would
be readmitted. Low-risk patients were given
an 800 number to call if they had questions
about their care. The results of those questions
were visible to the Transitional Care Team.
When necessary, these patients would
receive additional interventions. Medium-risk
patients received the 800 number, plus phone
calls from a nurse on the third, seventh, and
21st days after discharge. High-risk patients
received the medium-risk interventions, plus
an in-home visit by a nurse practitioner 30
days after their discharge.
This latest grant builds on previous
experience and allows Baylor to pilot a program
that could improve patients’ lives outside the
hospital setting. If we’re successful, we will
provide better care for our patients and improve
patient outcomes at a lower cost. And if we can
to seek help and may end up seeking emergency
care. Monitoring conditions daily is a part of a proactive treatment plan for heart failure patients.”
■ New CT scanner captures single
heartbeat, high-definition images
Cardiologists at the Heart Hospital Baylor
Plano can now capture high-definition images of
Baylor news
do this, we’re impacting not just patients within
our system but potentially patients and health
care systems around the country.
■ Giving back for good: board and
employees support show their support
Baylor Scott & White Health–North Texas is
blessed with dedicated and caring employees
who give of their time, service, and expertise to
patients and their families each and every day.
Again this year, employees, physicians, staff,
and supporters from such organizations as
Aramark, CBRE, Medco, Select, and HealthTexas
Provider Network demonstrated the depth of
their compassion and commitment by donating
more than $1.65 million in the 2015 Baylor
Health Care System Foundation Employee
Giving Campaign. The annual spring campaign
supports a variety of initiatives across the
system, including Faith in Action, the Employee
Assistance Fund, nursing scholarships, and
medical education, among others.
In addition, for the fourth consecutive
year, 100% of board members across
Baylor participated in the 2015 Board
Giving Campaign by making a gift or pledge.
Representing 16 boards across Baylor Scott
& White Health–North Texas, 287 board
members exhibited their commitment and
dedication by participating in this annual effort.
“Philanthropic support from our employees
and board members has a positive ripple effect
and sends an important message to our patients,
donors, and the community—a message that
they not only believe in, but also support the
great work that occurs in our hospitals every
day,” said Rowland K. Robinson, Baylor Health
Care System Foundation president. “There is
no greater testament to the work that we do
than the resounding support of those who
know us best.”
For information on how you can support
these or other initiatives at Baylor, please contact the Foundation at 214.820.3136.
a patient’s heart in only a fraction of a second using a single heartbeat, giving physicians a unique
four-dimensional analysis of a patient’s heart
condition. Using Texas’ first Revolution 256-slice
computed tomography (CT) scanner, physicians
are better able to view and diagnose coronary
artery disease and valvular heart disease. The
new CT scanner will enable cardiologists on the
89
medical staff to treat more challenging patients,
such as patients with high heart rates, by “freezing” the motion of a heart with superior image
quality. One-beat, motion-free cardiac imaging in
high definition at any heart rate, with or without
beta-blockers, delivers the clinical information
needed for improved patient management.
“One spin around the heart captures the
entire heart in a fraction of a second, giving an
excellent high-definition imaging of the heart and
arteries,” said Ambarish Gopal, MD, FACC, FSCCT,
FSCAI, medical director of cardiovascular CT imaging services at the Heart Hospital Baylor Plano.
“We are proud to offer our guests one of the most
advanced CT scanning technologies in the world.
The time taken to scan a patient is significantly
reduced due to this high-speed technology. The
new scanner also requires lower radiation and
contrast doses and is quieter. This affords our
patients a safer, more comfortable experience
while undergoing the diagnostic test.”
■ Baylor University Medical Center
performs record number of organ
transplants
Surgical teams took part in a record-setting
day of organ transplantation at Baylor University
Medical Center at Dallas. Surgeons on the medical staff performed nine organ transplants on
seven patients in one calendar day. The successful day of surgeries broke the previous
Texas record of eight organ transplants performed in one calendar day.
The nine organ transplants took place at
Baylor University Medical Center at Dallas on
90
September 1. Three additional organs were transplanted in the early morning hours of September
2, bringing the total to 12 organs transplanted in
24 hours. According to the United Network for
Organ Sharing, an average of seven transplants
are performed each day in Texas.
“I am very proud of this milestone,” said
Goran Klintmalm, MD, PhD, FACS, chief and
chairman of Baylor Annette C. and Harold C.
Simmons Transplant Institute. “This is a collaboration of more than 150 people coming together
in a short amount of time to change the lives of
these patients.”
“There are only a handful of centers that
have the infrastructure, the personnel, and
the ability to pull resources together in a short
amount of time, and that is why people come
from around the world to Baylor,” said Gonzalo
Gonzalez-Stawinski, MD, chief of heart transplantation and mechanical circulatory support
for Baylor Dallas.
A leader in solid organ transplant in the
United States, the Baylor Annette C. and Harold
C. Simmons Transplant Institute has successfully transplanted more than 8200 organs over
the last 30 years. In 2014, the team performed
102 cardiac transplants in 1 year, becoming
one of the top two programs by volume in the
country for heart transplantation, with excellent
outcomes.
■ North Texans team up to deliver
medical supplies to Syrian refugees
Baylor Scott & White Health’s Faith in Action
Initiatives joined forces with Sarah and Ross
Baylor University Medical Center Proceedings
Perot Jr. to help Syrian refugees who have been
displaced by civil war. An estimated 9 million
Syrians have fled their homes since the outbreak
of hostilities in March 2011.
The Perots underwrote the costs associated
with delivering essential medical supplies and
equipment. This vital cargo was provided by
Baylor Scott & White’s Faith in Action Initiatives
to Hungarian Baptist Aid workers in Hungary,
one of the countries in which Syrian refugees
are seeking asylum. The delivery was made by a
specially configured cargo-capable Boeing 737
operated by Fort Worth–based ATX Air Services,
a Perot company. The shipment included supplies donated through Baylor Scott & White:
defibrillators, pulse oximeters, forehead thermometers, baby formula, canned food, gauze,
gloves, masks, exam beds, syringes, crutches,
walkers, mattresses, stethoscopes, and equipment to provide eye, ear, and foot care. Many of
the refugees are in desperate need of medical
attention. As a result, these items are in high
demand.
“As part of our commitment to health
and healing, Baylor Scott & White Health
works through our Faith in Action Initiatives
program to stretch medical resources and
expertise to regions around the globe, which
are underserved or in need,” said Don Sewell,
director of Faith in Action Initiatives. “These
supplies can make a tremendous difference
to the organizations that are providing
medical care to refugees from Syria. We are
honored to have the support of the Perots in
this effort.”
Volume 29, Number 1
John M. T. Finney: distinguished surgeon and Oslerphile
Marvin J. Stone, MD, MACP
John Finney (1863–1942) was born near Natchez, Mississippi. After
receiving his medical degree from Harvard, he interned at Massachusetts
General Hospital and then went to Baltimore to become one of the first
interns at the new Johns Hopkins Hospital. He met William Osler the
day the hospital opened and became a lifelong admirer of “the Chief.”
Finney specialized in gastrointestinal surgery and was recognized for
his expertise in the field. Osler recommended Finney to a physician colleague, writing, “You could not be in better hands. . . . Finney has been
most successful and his judgment is so good.” Finney served for 33
years under William Halsted at Hopkins. After Halsted’s death, Finney
was offered the chair of surgery at Johns Hopkins but declined. He was
a founder and first president of the American College of Surgeons. He
also served as president of the American Surgical Association and the
Society of Clinical Surgery. Finney became chief surgical consultant for
the Allied Expeditionary Forces in World War I. He was decorated by the
United States, France, and Belgium. Finney was a master surgeon and
a role model for generations of students and physicians.
J
ohn M. T. Finney (1863–1942), the son of a clergyman,
was born near Natchez, Mississippi, in a plantation house
in the midst of a Civil War battle. After the death of his
mother when he was only a few months old, he lived
with four different foster mothers (1). His fourth foster mother,
“Aunt Lizzie,” had a major impact on his life, enabling him to
attend Princeton University and taking care of him later in
Boston when he was a medical student. Finney was the only
person to play varsity football at both Princeton and Harvard.
He received his medical degree from Harvard in 1888 and interned at Massachusetts General Hospital, following which he
moved to Baltimore in 1889 to join the new Johns Hopkins
Hospital and Medical School.
Finney served 33 years under Chief of Surgery William
Halsted. During this prolonged period of time, he received
only one compliment from Halsted. Finney was a member of
the “All-Star” surgical team (Figure 1) (2). He performed an
appendectomy on Halsted’s wife, Carolyn Hampton Halsted.
Finney developed special interest and expertise in abdominal
surgery, especially surgery of the stomach and duodenum, and
was one of the pioneers in the operation of pyloroplasty. He
saw a number of private patients, particularly at the Union
Proc (Bayl Univ Med Cent) 2016;29(1):91–93
Figure 1. Halsted and the “All-Star” surgical team. The occasion was the opening of the new surgical building at Johns Hopkins in 1904. Halsted is operating
on a patient with osteomyelitis of the upper femur. He is performing a resection
holding a wooden hammer. Finney is first assistant and is directly across the table
from Halsted. Harvey Cushing is on Finney’s right. Photo: Alan Mason Chesney
Medical Archives of The Johns Hopkins Medical Institutions.
Protestant Hospital, and developed a first-rate surgical program
at that hospital. Later on he was able to admit private patients
at Johns Hopkins and held the appointment of professor of
clinical surgery.
Finney had a long and close relationship with William Osler.
The two met when the hospital first opened in 1889, and Finney
referred to him as “the Chief.” Finney was a lifelong admirer of
Osler. In his autobiography, Finney described Osler on rounds:
But in order to get a glimpse of the real “Chief,” of the many
sides of his character; his wonderful memory for cases, the inexhaustible storehouse of medical lore with which his mind was
filled, his remarkable insight into human nature, his intimate
knowledge of disease and its protean manifestations; in order
From the Departments of Internal Medicine and Oncology and the Charles
A. Sammons Cancer Center, Baylor University Medical Center at Dallas; the
Departments of Internal Medicine and Humanities, Texas A&M College of
Medicine; and the School of Arts & Humanities, The University of Texas at Dallas.
Presented in part at the 45th Annual Meeting of the American Osler Society,
Baltimore, MD, 2015.
Corresponding author: Marvin J. Stone, MD, MACP (e-mail: marvstonemd@
gmail.com).
91
Figure 2. Osler with the first resident staff at Hopkins, 1889–1890. Finney is in
the back row, second from the left. Photo: Osler Library of the History of Medicine,
McGill University. William Osler Photo Collection.
to feel the magic of his personality,
one must watch him by the bedside of his patient, surrounded by
his students, the ideal clinician and
teacher. There he sits in characteristic pose in the midst of them, his
exquisite hands palpating the patient or toying with a stethoscope,
of thoughtful mien, his mind alert,
never missing an opportunity to
direct attention to some point of
interest illustrated by the case or to
point out to the students some way
in which by study and research additions could be made to existing
knowledge. Nor does he fail to
take advantage of the opportunity to try in his own delightful
way to stimulate in the minds of
his students the desire for real accomplishment in their work (3).
Finney was a member of the
first resident staff at John’s Hopkins
(Figure 2) (4, 5). Finney recommended William Thayer, his medical school classmate at Harvard, to
replace Henry Lafleur, Osler’s first
chief resident. Thayer stayed on in
that capacity with Osler for 7 years.
Harry Friedenwald, an ophthalmologist and son of Aaron Friedenwald, also an ophthalmologist,
contacted Osler in Canada when the
elder Friedenwald became ill with an
abdominal mass. Osler wrote a letter back to Friedenwald recommending surgical exploration by Finney,
saying, “You could not be in better
92
hands.” Moreover, Osler said, “Finney has been most successful . . . and his judgment is so good.” Not only was Finney an
Oslerphile, but Osler was quite definitely a Finneyphile.
Figure 3 shows Osler’s handwritten letter to Friedenwald
(author’s collection). Osler said he would not be able to do
anything other than urge surgical exploration because of the
progressive loss of weight, the discomfort and uneasiness in
the abdomen, and a palpable abdominal mass. Later on in the
letter, Osler concluded by saying, “Do give your father my
kindest regards and best wishes, and if he is anxious to see me
or if you feel my presence would be a source of comfort to him
or to your mother let me know and I will come at once.” The
letter was signed, “Sincerely yours, Wm Osler.”
Finney had a number of offers during his career, one of which
was to become the president of Princeton. After consideration,
he decided not to do that but did become a life trustee of the
university. After Halsted’s death, Finney was offered the chair
Figure 3. Osler’s handwritten letter to Harry Friedenwald about his father. The elder Friedenwald died 16 days after
this letter was written.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Figure 4. Finney at age 50 when he was elected first president of the American
College of Surgeons. Photo: American College of Surgeons.
of surgery at Hopkins but declined, feeling that he was too old
and that the post should go to a younger person. At one point
he was touted to run for senator from Maryland, but he did
not really pursue that opportunity.
Finney received a number of prestigious job offers during
his career, including becoming a founder and first president
of the American College of Surgeons (Figure 4) (6, 7). He
served on the editorial board of Surgery Gynecology & Obstetrics
from 1913 until his death. Finney was also the president of
the American Surgical Association and the Society of Clinical
January 2016
Surgery. He was a member of the board of trustees at Lincoln
University and received a number of other honors and degrees
throughout his career.
Finney served in the Armed Services during World War I,
achieving the rank of brigadier general in the US Army Medical
Corps. He also served as chief surgical consultant to the Allied
Expeditionary Forces and participated in a number of studies
for new methods of wound care. Finney was decorated by the
United States, France, and Belgium and received the Legion of
Honor from France.
Finney had a long career as mentor and counselor to students and young physicians in training. He made a number of
addresses to Princeton college students in an informal medical
club atmosphere. These were collected in a small book called
The Physician (8). Twenty-one topics were published, including
chapters on experience, ethics, criticism of colleagues, altruism,
humor, the grateful patient, and causes of failure.
At the conclusion of his autobiography Finney stated, “The
true physician is supremely happy in his work. He could not
be happy doing anything else. Once having caught the vision
as it unfolds before his gaze, all else fades into insignificance.”
John M. T. Finney died in 1942 at the age of 78 and is buried in Churchville, Maryland. He was an outstanding clinician
and a master surgeon who rose to international prominence during his long career at Johns Hopkins. His standards and ideals
were of the highest caliber. Finney was an inspiration and role
model for generations of students and physicians.
1.
2.
3.
4.
5.
6.
7.
8.
Finney JMT. A Surgeon’s Life: The Autobiography of J.M.T. Finney. New
York: Putnam, 1940.
Harvey AM, Brieger GH, Abrams SL, Fishbein JM, McKusick VA. A
Model of Its Kind: A Pictorial History of Medicine at Johns Hopkins, Vol 2.
Baltimore, MD: Johns Hopkins Press, 1989:81.
Finney JMT, A Surgeon’s Life: 280.
Harvey AM et al., A Model of Its Kind: 39.
Bliss M. William Osler: A Life in Medicine. New York: Oxford University
Press, 1999: 213–214.
Finney JMT. Presidential address, American College of Physicians, first
convocation, November 13, 1913.
Cameron JL. John Miller Turpin Finney: the first president of the
American College of Surgeons. J Am Coll Surg 2009;208(3):327–332.
Finney JMT. The Physician. New York: Scribner, 1923.
John M. T. Finney: distinguished surgeon and Oslerphile
93
Reflections of Churchill’s personal cardiologist
John Davis Cantwell, MD, assisted by Charles Wilson, MD†
I
have long been an admirer of Sir Winston Churchill, having
visited his birth home (Blenheim Palace), his underground
war rooms in London (where one can hear recordings of his
stirring speeches), and his grave site in St. Martin’s churchyard. With a lot of imagination and relying heavily on Lord
Moran’s entertaining diaries (1–3), I have tried to conceive what
it might have been like to serve as Churchill’s personal cardiologist, as the text below represents.
NOTES OF CHURCHILL’S CARDIOLOGIST: A HISTORICAL FICTIONAL
ACCOUNT
When Sir Winston Churchill (Figure 1) became prime
minister (PM) in 1940, at age 65, certain members of the cabinet decided I should become his personal cardiologist. He wasn’t
happy about it, when I approached him, stating that there was
nothing wrong with his heart, only that he had some dyspepsia.
He proceeded to show me his self-treatment of the latter, moving
his big white belly up and down during some breathing exercises.
I knew it wouldn’t be an easy job, but I felt up to the task, having
been influenced by the teachings of great British cardiologists like
Sir James Mackenzie and Sir Thomas Lewis and influenced via
textbooks by the American, Paul Dudley White, and, later, by
our own Paul Wood.
The next year (1941) he had his first cardiac symptom.
While straining to open a window on a hot evening, he noticed
left precordial discomfort, which radiated down his left arm and
was associated with dyspnea. It passed within a few minutes.
I decided not to say anything, as America had just entered the
war and the PM couldn’t possibly take 6 weeks of bedrest. If
his symptoms should reoccur (which they fortunately did not),
I was going to consult with my colleague, Sir John Parkinson.
While on one of our travels together, we flew in General
George Marshall’s plane from Washington to Florida to get
some rest. The PM decided to float in the ocean, basking “halfsubmerged” like a “hippopotamus in a swamp.” He can be quite
amusing when he isn’t exasperating.
I have been criticized by some colleagues for traveling with
the PM instead of tending to my duties as an officer in the Royal
College of Physicians. It is hard to please everyone. I think his
health care is more important, especially in these critical times.
In a Russian hotel he wants to take a bath. The taps are different and the Russian lettering isn’t helpful. I took a chance
94
Figure 1. Sir Winston Churchill. Source: Library of Congress Prints and
Photographs Division, reproduction number LC-USW33-019093-C.
and turned on a faucet. A gush of icy water hit him “amidships.”
He gave a loud shriek and “cursed me for incompetence.” I’ll
have to be more careful so he doesn’t lose confidence in my
medical abilities.
The PM desired to walk in the woods while in Moscow. This
surprised me as he “hardly ever walks for the sake of exercise”! He
mainly wanted to reflect upon his meeting with Joseph Stalin.
From Piedmont Heart Institute, Atlanta, Georgia (Cantwell). †Deceased (aka Lord
Moran).
Corresponding author: John Davis Cantwell, MD, MACP, FACC, Piedmont
Heart Institute, 275 Collier Road, NW, Suite 500, Atlanta, GA 30309 (e-mail:
john.cantwell@piedmont.org).
Proc (Bayl Univ Med Cent) 2016;29(1):94–96
Much later that night, he got ready for bed and put on his
black eyeshade. It was about 4 am. His stamina is amazing. His
only apparel at bedtime is a silk vest, leaving a “big, bare, white
bottom.” There is no hour of the night when I can be sure he
is in bed and asleep. Needless to say, he can be exhausting to
be around.
His hobby is painting, but the only picture he painted during the war years was while we were in Morocco. In later years
this hobby would provide a great source of relaxation for him.
Shortly after our return to London, the PM developed a
fever. I heard some rales in his left lung base. An x-ray the next
day confirmed pneumonia. Apart from his appendix, he has
remained remarkably healthy at age 69, despite having abused
his body.
When ill, the PM generally does as he is told, as long as he
is given a good reason to do so. He is partial to quacks, which
makes my job more difficult. He does listen to me, as long as
he agrees with what I am saying.
His relationship with his wife, Clementine, is interesting.
She doesn’t argue with him because he “shouts her down,” so
instead she writes him notes. She tells him the truth about
himself. He might not always like what she says, but knows that
she loves him and cares for him more than anyone.
It is hard to believe that the PM was “tongue-tied” as a youth
and dreaded giving speeches in his early years in the House of
Commons. Supposedly he was bullied and beaten as a youth and
was apprehensive and spoke with a stutter. Yet, his philosophy
of never giving in enabled him to persevere. His main attribute
was his iron will.
The PM had another bout of pneumonia, associated with
a fast and irregular pulse. He had rales in the lung bases, and
his liver edge was palpable. I started him on digitalis and the
pulse became regular 4 hours later. Three days later, he again
had atrial fibrillation, lasting about 90 minutes.
We were flying to Italy, an area where malaria is prevalent.
I wanted the PM to take prophylactic medicine. He felt it unnecessary. To support his view he phoned Buckingham Palace
and spoke with the king, who had been to Italy and hadn’t taken
any preventive medicine. So, instead of consulting several malaria experts in England, he contacts the king, who is no expert
on this. It is certainly challenging to be his personal physician.
The PM says to look at one’s eyes and see if more of the
head is above than below, to tell the size of one’s brain. Where
he got that I have no idea.
Flying to Naples, the PM was dozing. His oxygen mask had
slipped off and oxygen was hissing out close to the PM’s lighted
cigar. It’s a wonder we didn’t all go up in flames.
The PM asked if I carefully looked at patients’ hands. He
became interested in doing so after reading what Gorky wrote
about Tolstoy’s hands, “Knotted with swollen veins and yet full
of singular expression and power of creativeness.” Accordingly,
I now pay more attention to the hands during my physical
examinations.
According to his wife, the PM knows nothing of the life of
ordinary people. He has never been on a bus, and his only trip
on the underground resulted in his going round and round until
January 2016
he was eventually rescued. He is selfish, even though he doesn’t
mean to be, and an egoist.
The PM was fussing about our lunch. After two very stiff
whiskies and a brandy, his “black clouds” dispersed.
After being voted out of office shortly after the end of the
war, Churchill had to rely on his “red tablet” to sleep, to keep
“futile speculations” from filling his mind. I sometimes had to
also add a “green tablet” so he could be well rested. He began to
develop problems with his eyes, ears, throat, heart, and lungs,
and his diverticulitis flared. Now he has added an inguinal hernia. He flooded me with questions about the latter: Why should
he have it since he hardly exercised? Would it rupture? We got
him a truss, and that seemed to settle him down.
He turned once again to his paint box, which had helped
him cope with the last time he was turned out of office 30 years
ago. It helped him deal with political disappointments and gave
him something to focus on.
Churchill has now developed conjunctivitis. Initially penicillin ointment helped, but now it seems resistant. Churchill
planned to call Sir Alexander Fleming, who had discovered
penicillin. Fleming seemed uninterested in him as a patient, but
more interested in the unusual bug, a Staphylococcus resistant to
penicillin. Churchill said, “The bug seemed to have caught my
truculence. This is its finest hour.” He laughed.
Churchill was upset hearing that President Roosevelt said he
had 100 ideas a day and that only four of them were good. He
felt it was impertinent of Roosevelt to say that, since he hadn’t
any ideas at all. In truth they are good friends and during the
war years had personal visits 11 times and exchanged 1,700
letters and telegrams.
In 1949, while playing cards late at night, Churchill had
numbness and weakness of his right leg. As usual, he demanded
an explanation of the pathology of the episode. I tried to explain
the circulation of the brain as best I could.
The last 10 years of his life were hard on both of us. He
had four strokes between 1949 and 1953, yet was able to finish
multiple volumes of The Second World War.
In the last few years, until his death at 90 in 1965, he had
given up reading and seldom spoke. He didn’t seem to know
his friends, yet he hung on. I’d think he’d be gone by the next
morning and would issue a bulletin to alert the public. I finally
stopped doing that after he had pulled through time after time.
Finally, his breathing became more shallow and labored and
then ceased. I got up, bent over the bed, but he truly was gone.
His body lay in state for 3 days in Westminster Abbey, where
thousands of his countrymen paid tribute to the man “who had
saved them and saved their honor.” He was buried in Bladon,
his body “committed to English earth, which in his finest hour
he held inviolate.”
REFLECTIONS
It has been 50 years since the death of Sir Winston, and
perhaps it is time to reflect upon the care I rendered to him
during our 25 years together. Although an old man now myself,
and long retired from my cardiology practice, I have tried to
keep up with the incredible advances in my field.
Reflections of Churchill’s personal cardiologist
95
I am thankful for Sir Alexander Fleming’s discovery, for
penicillin was of great help during Churchill’s several bouts of
pneumonia.
I wish that we had known more about the importance of
anticoagulation beyond aspirin for paroxysmal atrial fibrillation,
for it might have prevented at least some of his multiple strokes.
Lord Russell Brain thought he had bilateral carotid artery disease, so carotid ultrasound, angiography, and endarterectomy
surgery might have been of benefit.
I would like to have had access to blood troponin tests, to
help study the severity of several episodes of prolonged chest
pain when serial electrocardiograms weren’t conclusive. On at
least one occasion he had signs and symptoms of congestive
heart failure, and echocardiography would have been useful,
as well as perhaps cardiac catheterization, potent diuretics,
beta-blockers, angiotensin receptor antagonists, and statin
drugs.
I was with him during his two terms as PM (1940–1945,
1951–1955) and on most of the 100,000 miles of trips he made
during the war years. I had a front row seat for many of his
famous speeches. My favorites were, of course: “I have nothing
to offer but blood, toil, tears, and sweat” and “We shall fight
on the beaches, we shall fight on the landing grounds, we shall
fight in the fields and in the streets, we shall fight in the hills,
we shall never surrender.”
My grandchildren would refer to Churchill as “a piece of
work.” I am amazed that he made it to age 90. He was fat,
sedentary, and stressed; he smoked cigars and drank alcohol to
excess; and he kept terribly irregular hours. His family history
didn’t reflect genetic tendencies for longevity, as his father died
at age 45. I guess he was just one of those survivors, having been
under fire many times in his early military career. I don’t recall
that he was ever wounded. He did once escape from a prison
camp while in South Africa.
I don’t think he was depressed, just at times fatigued by his
great responsibilities. At least he was never treated with whatever
antidepressant was available then. Later in life he was somewhat
96
Figure 2. The memorial to Churchill in Westminster Abbey. Source: Westminster
Abbey.
debilitated from his multiple strokes. I sometimes had to give
him amphetamines before important tasks.
Recently a memorial stone was placed in the nave of Westminster Abbey (Figure 2) by Churchill’s great-great-grandchildren, imploring us to remember him. How could I ever forget
this great man who for 25 years was my (usually) compliant
patient and dear friend? I agree with historian Max Hastings,
who considered him “the greatest war leader his country had
ever known, a statesman whose name rang across the world like
no other Englishman in history.”
Acknowledgments
My thanks to Karen Galloway for preparing the manuscript
and to Stacie Waddell for assisting with the figures.
1.
2.
3.
Mather JH. Churchill: Taken from the Diaries of Lord Moran. Boston, MA:
Houghton Mifflin, 1966.
Winston Churchill. Wikipedia. Available at https://en.wikipedia.org/wiki/
Winston_Churchill.
Hastings M. Winston’s War. Churchill 1940–1945. New York: A. A. Knopf,
2009.
Baylor University Medical Center Proceedings
Volume 29, Number 1
An alternative approach to prescribing sternal precautions
after median sternotomy, “Keep Your Move in the Tube”
Jenny Adams, PhD, Ana Lotshaw, PT, PhD, CCS, Emelia Exum, PT, DPT, Mark Campbell, BSc, MSc,
Cathy B. Spranger, DrPH, Jim Beveridge, RN, PCCN, Shawn Baker, PT, DPT, MS, Stephanie McCray, RN,
Tim Bilbrey, MBA, Tiffany Shock, BS, Anne Lawrence, RN, Baron L. Hamman, MD, and Jeffrey M. Schussler, MD
Traditional sternal precautions, given to sternotomy patients as part of
their discharge education, are intended to help prevent sternal wound
complications. They vary widely but generally include arbitrary load
and time restrictions (lifting no more than a specified weight for up to
12 weeks) and may prohibit common shoulder joint and shoulder girdle
movements. Having observed the negative effects of restrictive sternal
precautions for many years, our research team performed a series of
studies that measured the forces exerted during various common activities and their relationship to the sternum. The results, though informative, led us to realize that the goal of identifying “the” appropriate load
restriction to prescribe for sternotomy patients was futile. The alternative
approach that we introduce applies standard kinesiological principles and
teaches patients how to perform load-bearing movements in a way that
avoids excessive stress to the sternum.
C
oronary artery bypass grafting (CABG) and other procedures involving median sternotomy carry the risk
of sternal wound complications that can lead to increased morbidity, reduced quality of life, prolonged or
repeated hospitalizations, increased health care costs, and, for
serious cases, mortality rates of 15% to 40% (1–3). Because the
consequences of sternal complications can be grave, sternotomy
patients require educational guidance before being discharged
from the hospital.
Authors of the first discharge education materials focused on
restricting the loads patients could lift for specific time periods
that were considered appropriate for sternal healing (4, 5). The
resulting sternal precautions likely stemmed from expert opinion or were based on anecdotal rather than direct evidence (6)
and, consequently, vary widely among hospitals and rehabilitation centers around the world. In general, sternal precautions
are very restrictive. Beyond imposing arbitrary load restrictions,
they often prohibit common shoulder joint and shoulder girdle
movements, including shoulder flexion/extension and abduction/adduction, along with scapular retraction/protraction,
elevation/depression, and upward/downward rotation. Specific
examples from the USA and abroad include lifting no more
than a specified weight (usually between 5 and 20 pounds) for
up to 12 weeks (7–10); not pushing up when rising from sitting to standing (11); and performing only pain-free bilateral
Proc (Bayl Univ Med Cent) 2016;29(1):97–100
arm movements (horizontal, backwards, or over the shoulder)
(1, 12).
THE CASE FOR CHANGE
Sternal precautions are intended to help protect patients
after median sternotomy, but instead they may inadvertently
impede recovery. A restriction such as “don’t lift more than
5 pounds” can reinforce fear of activity (13), leading to the
substantial muscle atrophy that occurs during short-term disuse (14). Resistance exercise training is necessary for regaining
muscle mass lost during a period of disuse; therefore, “don’t
lift more than 5 pounds” is the opposite of what patients need
to hear. Physical activity restrictions can also delay or prevent
a return to work by patients whose physically demanding jobs
require them to handle loads and exert force in excess of current
recommendations (15). When patients cannot resume job
duties, they and their families suffer (16).
Worldwide, median sternotomies are performed during an
estimated 800,000 CABG procedures (17), 5000 transplants
(18), and an indeterminate number of cardiac valve surgeries
each year, so the potential scope of problems arising from the
ongoing use of restrictive sternal precautions is sobering. With a
goal of identifying “the” appropriate load restriction to prescribe
for sternotomy patients, we began a series of cardiovascular research studies in the mid-1990s that measured the forces exerted
during various common activities and their relationship to the
sternum (7, 19–21):
1. We conducted 6 sessions of a simulated lawn-mowing
protocol that matched the push and pull forces (36 and
39 force/pounds, respectively) of mowing outdoors, and
the activity did not negatively affect the sternal incision,
electrocardiogram findings, blood pressure, or heart rate of
13 male sternotomy patients (3 to 7 weeks post-CABG).
From Baylor Heart and Vascular Hospital (Adams, McCray, Bilbrey, Shock,
Lawrence, Schussler); Baylor University Medical Center at Dallas (Lotshaw,
Exum, Beveridge, Hamman, Schussler); Baylor Institute for Rehabilitation (Baker);
Darwen Leisure Centre, Darwen, UK (Campbell); and Seton Medical Center Austin,
Austin, Texas (Spranger).
Corresponding author: Jenny Adams, PhD, Cardiac Rehabilitation Department,
Baylor Heart and Vascular Hospital, 411 North Washington, Suite 3100, Dallas,
TX 75246 (e-mail: jennya@BaylorHealth.edu).
97
2. We measured the force required for common load-bearing
activities, such as pulling out a full dishwasher rack
(5 pounds), removing a gallon of milk from a refrigerator
(10 pounds), and pushing a glass door to exit the hospital
(22 pounds).
3. We found that the force across the sternum during a cough
(regularly tolerated by sternotomy patients) was 60 pounds,
or greater than the force exerted while lifting two 20-lb
weights simultaneously.
4. We compared the force across the sternum during a sneeze
with the force exerted during a bench press exercise and
found that a sneeze exerted a force of 90 pounds and was
not significantly different than the force exerted while lifting
70% of one-repetition maximum.
Because sternotomy patients commonly endure coughing
and sneezing without incident during recovery, these research
findings may seem to imply that lifting loads in the range
of 60 to 90 pounds is safe. This is definitely not the case, as
sternal wound dehiscence from intense coughing has been
reported (22), and sneezing may also pose a risk (1). This
knowledge, coupled with the fact that sternal complications
have been linked to risk factors such as obesity, diabetes mellitus, and smoking (23), led us to realize that our research
efforts to determine a single ideal load restriction were futile.
As a result, our team pursued an alternative approach to
sternal precautions.
INTRODUCING KEEP YOUR MOVE IN THE TUBE
We moved away from load and time restrictions and instead
used standard kinesiological principles to develop this new approach. Because Keep Your Move in the Tube is based on the
ergonomics that shorten the length of the outstretched arm
(lever arm reduction), it enables patients to perform previously
contraindicated movements.
The first step in applying this approach is to explain to patients in layman’s terms what happened to their sternum during
surgery, using an illustration of the attachments of the pectoralis
major on the sternum, the humerus, and the clavicle (Figure 1).
Figure 1. Illustration used to teach patients about their sternotomy, the attachments of the pectoralis major, and the imaginary truncal tube that is the basis
of the Keep Your Move in the Tube approach.
98
This brief anatomy lesson provides the foundation for understanding the concept behind the Keep Your Move in the Tube
graphic (Figure 2): By keeping their upper arms close to their
body, as if they were inside an imaginary truncal tube, patients
can modify load-bearing movements and thus avoid excessive
stress to the sternum. More specifically, limiting the movement
of the humerus minimizes the lateral pull on the sternum and
decreases the leverage of the hand and forearm during loadbearing actions such as rolling a wheelchair, opening a heavy
door, or lifting a toolbox. The graphic’s simple drawings show
movements that are “in the tube” (green) versus “out of the tube”
(red). These color-coded differences are easy to comprehend,
and the overall format overcomes barriers related to language
preference and reading ability.
In addition to information on basic movement patterns,
sternotomy patients need instruction on basic mobility skills.
Immediately after surgery, they often find it painful to sit
up from a supine position or to stand up from a chair. The
left side of the Keep Your Move in the Tube graphic contains
visual tips for staying “in the tube” while performing commonly recommended techniques for getting out of bed, such
as side-lying and placing one or both hands in front of the
body, leaning forward, and pushing up to a sitting position
(11); log rolling (24); and/or the elbow method (leg rolling
and counterweighting) (1). However, for non–load-bearing
activities such as personal hygiene, patients are allowed to
reach “out of the tube” (above the head, out to the side, or
behind the back).
With traditional sternal precautions, patients in the hospital are advised not to use their arms to push up during bed
mobility and transfers. As a consequence, they often require
assistance from the nursing staff, the therapy team, or family
members to complete these movements. Toward the end of the
hospital stay, the therapy team’s assessment of mobility status
is a major determinant of whether a patient needs rehabilitative care after being discharged. Instead of going home with a
physician referral for outpatient cardiac rehabilitation, patients
who have no available friends or family to help with mobility
may be sent to an inpatient rehabilitation facility. Keep Your
Move in the Tube, by contrast, enables patients to use their arms
and thus perform bed mobility and transfers more efficiently,
which may increase the likelihood that they will be discharged
to their home.
Because individual patient healing time can be affected by
factors such as age, underlying medical conditions, nutritional
status, medications, and use of tobacco, our educational approach does not impose time limits during which loads are restricted. We allow patients to resume their normal load-bearing
activities at their own pace, within pain-free limits, as long as
they stay “in the tube.” With an emphasis on partnership and
creative problem solving, we also suggest ways that family
members can help the patient during recovery without being
overprotective or overly controlling (e.g., using the correct
“in the tube” movements, the patient can mow the grass, but
only after a family member pulls the cord to start the mower’s
engine).
Baylor University Medical Center Proceedings
Volume 29, Number 1
At this writing, Keep Your Move in
the Tube is being used at four facilities in Texas. Three are within Baylor
Scott & White Health: Baylor Institute for Rehabilitation, where it has
replaced traditional sternal precautions in physician order sets; Baylor
Heart and Vascular Hospital, where it
is included in presurgical educational materials; and Baylor University
Medical Center at Dallas, where it
has been added to the therapy team’s
mobility criteria. The fourth is Seton
Medical Center Austin, where it is
used in phase I cardiac rehabilitation. As a multidisciplinary team,
we are united in the belief that Keep
Your Move in the Tube encourages
active living after sternotomy and
thus offers a useful alternative to
traditional sternal precautions.
Figure 2. Keep Your Move in the Tube graphic used to teach load-bearing upper extremity movements to patients recovering from median sternotomy. A teaching script is available from the corresponding author or from
http://www.baylorhealth.edu/Documents/BUMC%20Proceedings/2016_Vol_29/No_1/29_1_Teaching_Script.pdf.
IMPLEMENTATION
Several essential elements have emerged during the implementation of Keep Your Move in the Tube. First, the approval of cardiologists and cardiothoracic surgeons has been crucial, along with
acceptance by nursing staff members. Furthermore, the ongoing
process of including nurses from the intensive care unit is necessary to ensure that patients receive consistent educational advice
throughout their hospital stay. Finally, our success to date can be
attributed to a positive collaboration between physical therapists,
occupational therapists, and cardiac rehabilitation specialists.
January 2016
Acknowledgments
Grant support was provided by
the Cardiovascular Research Review
Committee in cooperation with the
Baylor Heart and Vascular Institute.
The authors thank the committee
for their encouragement and support of cardiovascular rehabilitation
research projects. Sincere thanks also
go to Barbara Bullock and Jillian
Carbone for their artistic expertise in
developing the tools; Beverly Peters,
MA, ELS, for editorial assistance in
preparing the manuscript; Nancy
Vish, RN, PhD, for empowering
the exercise professionals at Baylor
Heart and Vascular Hospital to have
freedom in exercise prescription;
and Barbara “Bobbi” Leeper, MN,
RN-BC, CNS-MS, CCRN, for the
years of motivating the cardiac rehabilitation staff to find an alternative
to traditional sternal precautions.
1. Brocki BC, Thorup CB, Andreasen JJ. Precautions related to midline
sternotomy in cardiac surgery: a review of mechanical stress factors
leading to sternal complications. Eur J Cardiovasc Nurs 2010;9(2):77–
84.
2. Loop FD, Lytle BW, Cosgrove DM, Mahfood S, McHenry MC,
Goormastic M, Stewart RW, Golding LA, Taylor PC. J. Maxwell
Chamberlain memorial paper. Sternal wound complications after isolated
coronary artery bypass grafting: early and late mortality, morbidity, and
cost of care. Ann Thorac Surg 1990;49(2):179–186.
3. Lucet JC; Parisian Mediastinitis Study Group. Surgical site infection after
cardiac surgery: a simplified surveillance method. Infect Control Hosp
Epidemiol 2006;27(12):1393–1396.
An alternative approach to prescribing sternal precautions after median sternotomy, “Keep Your Move in the Tube”
99
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
100
Hansen M, Laughlin J, Pollock ML, Schmidt DH. Heart Care After Heart
Attack. Redmond, WA: Medic Publishing Co, 1984:12.
Burrows SG, Gassert CA. Moving Right Along After Open Heart Surgery.
Atlanta, GA: Pritchett & Hull Associates Inc, 1990:21.
Cahalin LP, Lapier TK, Shaw DK. Sternal precautions: is it time for
change? Precautions versus restrictions—a review of literature and recommendations for revision. Cardiopulm Phys Ther J 2011;22(1):5–15.
Adams J, Cline MJ, Hubbard M, McCullough T, Hartman J. A new
paradigm for post-cardiac event resistance exercise guidelines. Am J Cardiol
2006;97(2):281–286.
Royal College of Surgeons of England. Get well soon: helping you to
make a speedy recovery after surgery to bypass a damaged blood vessel
that supplies blood to the heart. Available at http://www.rcseng.ac.uk/
patients/recovering-from-surgery/cabg; accessed May 27, 2015.
Tuyl LJ, Mackney JH, Johnston CL. Management of sternal precautions following median sternotomy by physical therapists in Australia: a
web-based survey. Phys Ther 2012;92(1):83–97.
Overend TJ, Anderson CM, Jackson J, Lucy SD, Prendergast M, Sinclair
S. Physical therapy management for adult patients undergoing cardiac
surgery: a Canadian practice survey. Physiother Can 2010;62(3):215–221.
Westerdahl E, Möller M. Physiotherapy-supervised mobilization and
exercise following cardiac surgery: a national questionnaire survey in
Sweden. J Cardiothorac Surg 2010;5:67.
Balachandran S, Lee A, Royse A, Denehy L, El-Ansary D. Upper limb
exercise prescription following cardiac surgery via median sternotomy: a
web survey. J Cardiopulm Rehabil Prev 2014;34(6):390–395.
Parker RD, Adams J. Activity restrictions and recovery after open chest
surgery: understanding the patient’s perspective. Proc (Bayl Univ Med
Cent) 2008;21(4):421–425.
Wall BT, Dirks ML, van Loon LJ. Skeletal muscle atrophy during shortterm disuse: implications for age-related sarcopenia. Ageing Res Rev
2013;12(4):898–906.
Mital A, Shrey DE, Govindaraju M, Broderick TM, Colon-Brown K,
Gustin BW. Accelerating the return to work (RTW) chances of coronary
heart disease (CHD) patients: part 1—development and validation of a
training programme. Disabil Rehabil 2000;22(13-14):604–620.
16. Mital A, Desai A, Mital A. Return to work after a coronary event.
J Cardiopulm Rehabil 2004;24(6):365–373.
17. Nalysnyk L, Fahrbach K, Reynolds MW, Zhao SZ, Ross S. Adverse events
in coronary artery bypass graft (CABG) trials: a systematic review and
analysis. Heart 2003;89(7):767–772.
18. Taylor DO, Edwards LB, Boucek MM, Trulock EP, Aurora P, Christie
J, Dobbels F, Rahmel AO, Keck BM, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: twenty-fourth
official adult heart transplant report—2007. J Heart Lung Transplant
2007;26(8):769–781.
19. Adams J, Pullum G, Stafford P, Hanners N, Hartman J, Strauss D,
Hubbard M, Lawrence A, Anderson V, McCullough T. Challenging traditional activity limits after coronary artery bypass graft surgery: a simulated lawn-mowing activity. J Cardiopulm Rehabil Prev
2008;28(2):118–121.
20. Parker R, Adams JL, Ogola G, McBrayer D, Hubbard JM, McCullough
TL, Hartman JM, Cleveland T. Current activity guidelines for CABG
patients are too restrictive: comparison of the forces exerted on the median
sternotomy during a cough vs. lifting activities combined with Valsalva
maneuver. Thorac Cardiovasc Surg 2008;56(4):190–194.
21. Adams J, Schmid J, Parker RD, Coast JR, Cheng D, Killian AD,
McCray S, Strauss D, McLeroy Dejong S, Berbarie R. Comparison
of force exerted on the sternum during a sneeze versus during low, moderate-, and high-intensity bench press resistance exercise with
and without the Valsalva maneuver in healthy volunteers. Am J Cardiol
2014;113(6):1045–1048.
22. Santarpino G, Pfeiffer S, Concistré G, Fischlein T. Sternal wound
dehiscence from intense coughing in a cardiac surgery patient: could it
be prevented? G Chir 2013;34(4):112–113.
23. Crabtree TD, Codd JE, Fraser VJ, Bailey MS, Olsen MA, Damiano RJ
Jr. Multivariate analysis of risk factors for deep and superficial sternal
infection after coronary artery bypass grafting at a tertiary care medical
center. Semin Thorac Cardiovasc Surg 2004;16(1):53–61.
24. Irons SL, Hoffman JE, Elliott S, Linnaus M. Functional outcomes of
patients with sternectomy after cardiothoracic surgery: a case series.
Cardiopulm Phys Ther J 2012;23(4):5–11.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Delivering bad news to patients
Kimberley R. Monden, PhD, Lonnie Gentry, MTh, and Thomas R. Cox, PsyD
When physicians lack proper training, breaking bad news can lead to
negative consequences for patients, families, and physicians. A questionnaire was used to determine whether a didactic program on delivering
bad news was needed at our institution. Results revealed that 91% of
respondents perceived delivering bad news as a very important skill, but
only 40% felt they had the training to effectively deliver such news. We
provide a brief review of different approaches to delivering bad news and
advocate for training physicians in a comprehensive, structured model.
T
he biopsy confirmed her fear: inflammatory breast cancer.
Now Amanda, a second-year surgery resident, had to tell
her patient the bad news. Overwhelmed and saddened by
the task, she wondered how to tell a 62-year-old woman
that she had a high risk of recurrence, even with chemotherapy,
surgery, and radiation.
Delivering bad news is one of the most daunting tasks faced
by physicians. For many, their first experience involves patients
they have known only a few hours. Additionally, they are called
upon to deliver the news with little planning or training (1).
Given the critical nature of bad news, that is, “any news that
drastically and negatively alters the patient’s view of her or his
future” (2), this is hardly a recipe for success.
Historically, medical education has placed more value on
technical proficiency than communication skills. This leaves
physicians unprepared for the communication complexity and
emotional intensity of breaking bad news (3). The fears doctors
have about delivering bad news include being blamed, evoking a
reaction, expressing emotion, not knowing all the answers, fear
of the unknown and untaught, and personal fear of illness and
death (2). This can lead physicians to become emotionally disengaged from their patients (1). Additionally, bad news delivered
inadequately or insensitively can impair patients’ and relatives’
long-term adjustments to the consequences of that news (4).
APPROACHES TO COMMUNICATING BAD NEWS
Given the negative results of delivering bad news poorly
for both patient and physician, physician training in delivering bad news is needed. The best training will embrace a
patient-centered approach that includes the patient’s family.
A patient- and family-centered approach not only keeps the
Proc (Bayl Univ Med Cent) 2016;29(1):101–102
patient at the center (5), but has also been shown to yield the
highest patient satisfaction and results in the physician being
perceived as emotional, available, expressive of hope, and not
dominant (6).
In a patient- and family-centered approach, the physician
conveys the information according to the patient’s and patient’s
family’s needs. Identifying these needs takes into account the
cultural, spiritual, and religious beliefs and practices of the family (7). Upon conveying the information in light of these needs,
the physician then checks for understanding and demonstrates
empathy. This is in contrast to an emotion-centered approach,
which is characterized by the physician emphasizing the sadness
of the message and demonstrating an excess of empathy and
sympathy. This approach produces the least amount of hope
and hinders appropriate information exchange (6).
Additionally, the best training will include a protocol for
delivering bad news (8). Several protocols have been proposed
and tested in the literature. Buckman has written extensively
on this subject (2, 9, 10), including his landmark 1992 book,
How to Break Bad News: A Guide for Health Care Professionals
(11). His criteria for delivering bad news include delivering it
in person, finding out how much the patient knows, sharing the
information (“aligning”), assuring the message is understood,
planning a contract, and following through (2).
Fine proposed a protocol with five phases. Phase 1, preparation, involves establishing appropriate space, communicating
time limitations, being sensitive to patient needs, being sensitive
to cultural and religious values, and being specific about the
goal. Phase 2, information acquisition, includes asking what
the patient knows, how much the patient wants to know, and
what the patient believes about his or her condition. Phase 3,
information sharing, entails reevaluating the agenda and teaching. Phase 4, information reception, allows for assessing the
information reception, clarifying any miscommunication, and
handling disagreements courteously, while Phase 5, response,
includes identifying and acknowledging the patient’s response
to the information and closing the interview (7).
From the Department of Surgery, Baylor University Medical Center at Dallas.
Corresponding author: Kimberley R. Monden, PhD, Department of Surgery,
Baylor University Medical Center at Dallas, 3500 Gaston Avenue, Dallas, TX
75246 (e-mail: kimberley.monden@baylorhealth.edu).
101
Baile et al proposed a protocol called SPIKES (10): S, setting
up the interview; P, assessing the patient’s perception; I, obtaining
the patient’s invitation; K, giving knowledge and information to
the patient; E, addressing the patient’s emotions with empathic
responses; and S, strategy and summary. VitalTalk (www.vitaltalk.
org) makes use of the SPIKES protocol and incorporates many
articles and videos that describe and illustrate each step.
Rabow and McPhee also proposed a model for delivering
bad news called ABCDE: A, advance preparation; B, build a
therapeutic environment/relationship; C, communicate well; D,
deal with patient and family reactions; and E, encourage and
validate emotions (12). Additionally, numerous other published
articles deal with communication skills relating to delivering
bad news to patients.
Other factors to consider when delivering bad news include
the physical and social setting and the message (13). Specifically,
the location should be quiet, comfortable, and private. With
regard to structure, bad news should be delivered when it is convenient to the patient, with no interruptions, with ample time,
and in person. Ideally, those receiving the bad news should be
given the choice to be accompanied by someone in their support
network. With regard to the message being delivered, physicians
should be prepared, find out what the patient already knows,
convey some measure of hope, allow for emotional expression
and questions, and summarize the discussion. The message
should be delivered with empathy and respect and in language
that is understandable to the patient, free from medical jargon
and technical terminology.
As evidenced above, ample resources are available for
improving one’s skill in delivering bad news, from numerous
published articles to online tools such as VitalTalk. However,
there is no guarantee that these resources are being utilized by
faculty and residents. We therefore asked whether a didactic
intervention was needed in our department.
NEEDS ANALYSIS
To address this deficiency, we administered a preliminary
questionnaire to gather baseline information about surgeons’
experiences and attitudes when delivering bad news at our
institution. The questionnaire was also used to evaluate the need
for specific training to improve communication skills related
to the delivery of bad news and gather pilot data for future
research/intervention. The questionnaire was administered to
54 participants (17 women, 37 men) in the Department of
Surgery at Baylor University Medical Center at Dallas. Thirtyfour respondents were residents and 20 were attendings.
Results revealed that 93% of respondents perceived delivering bad news to be a very important skill and 7% a somewhat
important skill; however, only 43% of respondents felt they
had the training to effectively deliver such news. Furthermore,
85% felt they needed additional training to be effective when
delivering bad news. Of the 85% of participants who felt they
needed additional training, 59% were residents and 26% were
attendings. No differences in reported preparedness were revealed across gender. As anticipated, participants with more
102
experience (i.e., years in the profession) reported feeling better
prepared to deliver bad news than those with less experience.
DISCUSSION
Based on these results, the need to implement an educational
intervention to improve the communication skills of faculty and
residents in the Department of Surgery has become evident. To
address this gap in training, a follow-up study has been initiated
to determine the effectiveness of Rabow and McPhee’s ABDCE
approach (12), with modifications and additional material from
other sources including VitalTalk. Additionally, the study incorporates the use of standardized patients, three different bad news
scenarios, video recording of the interactions, and individualized
feedback. If this approach proves successful, it will form the basis
of our department-wide educational intervention.
Professionalism and interpersonal communication skills are
two of the six core competencies required by the Accreditation
Council for Graduate Medical Education for all specialties.
Unlike more concrete competencies, such as medical knowledge, which can be evaluated with in-training examinations,
the assessment of professionalism and communication skills
is more subjective and difficult. As opposed to continuing the
tradition of implicitly learning professionalism by observing
how attendings behave in a clinical setting, we believe that
explicit, structured learning via formal curricula is necessary.
It is our hope that by building communication skills training
into our surgical education curriculum, residents and staff will
feel better prepared to face this daunting task.
1.
2.
3
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Orlander JD, Fincke BG, Hermanns D, Johnson GA. Medical residents’
first clearly remembered experiences of giving bad news. J Gen Intern Med
2002;17(11):825–831.
Buckman R. Breaking bad news: why is it still so difficult? Br Med J (Clin
Res Ed) 1984;288(6430):1597–1599.
VandeKieft GK. Breaking bad news. Am Fam Physician 2001;64(12):1975–
1978.
Fallowfield L. Giving sad and bad news. Lancet 1993;341(8843):476–
478.
Fine RL. Keeping the patient at the center of patient- and family-centered
care. J Pain Symptom Manage 2010;40(4):621–625.
Schmid Mast M, Kindlimann A, Langewitz W. Recipients’ perspective
on breaking bad news: how you put it really makes a difference. Patient
Educ Couns 2005;58(3):244–251.
Fine RL. Personal choices—communication among physicians and
patients when confronting critical illness. Tex Med 1991;87(9):76–82.
Cunningham CC, Morgan PA, McGucken RB. Down’s syndrome: is
dissatisfaction with disclosure of diagnosis inevitable? Dev Med Child
Neurol 1984;26(1):33–39.
Buckman R. Communication skills in palliative care: a practical guide.
Neurol Clin 2001;19(4):989–1004.
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP.
SPIKES—a six-step protocol for delivering bad news: application to the
patient with cancer. Oncologist 2000;5(4):302–311.
Buckman R. How to Break Bad News: A Guide for Health Care Professionals.
Baltimore: Johns Hopkins University Press, 1992.
Rabow MW, McPhee SJ. Beyond breaking bad news: how to help patients
who suffer. West J Med 1999;171(4):260–263.
Ptacek JT, Fries EA, Eberhardt TL, Ptacek JJ. Breaking bad news to
patients: physicians’ perceptions of the process. Support Care Cancer
1999;7(3):113–120.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Cool it
Allen B. Weisse, MD
A
man awakens one morning and finds that one of his hands
is painfully swollen. He rushes to his doctor’s office. The
physician examines the hand and instructs his patient to go
home and soak it in the hottest water bearable and return
the next morning. The patient dutifully follows these instructions
but finds, after immersing his hand in the tub, that instead of
improving, the swelling and pain grow worse.
At this point his housekeeper arrives and notices his dreadful state. She asks her employer why he is using hot water for the
problem.“I always use cold water for something like this,” she states.
With nothing to lose, the patient substitutes ice water for the hot
tub and, miraculously, the swelling and pain subside. The following
morning he appears before his doctor.
“How is the hand?” the doctor inquires.
“It’s just fine now, but no thanks to you.”
“What do you mean?”
“I put my hand in hot water the way you told me to and it got
worse. My housekeeper just happened to come by and she saw what
was happening and told me that she always uses cold water for this
problem. So I switched to cold water and it all cleared up perfectly.”
Visibly perplexed, scratching his head, the doctor replies, “That’s
funny. My housekeeper says always use hot water.”
As with many funny stories, buried within an obvious absurdity there lies a kernel of truth. It would be absurd for any
physician to handle the problem as described, while having a
half dozen diagnostic modalities and a myriad of pharmaceuticals available to him. Nor would he ever consider calling in
his housekeeper for a consultation. The kernel of truth lies in
the fact that, for many minor illnesses and injuries that occur,
patients see no need for professional care. They rely instead
upon inherited traditions of home care, which we might well
characterize as folk medicine. In this case we are confronted
with competition between heat and cold for the treatment of
the fictional illness described.
The frequent use of heat or cold as home care remedies
calls to mind the very prominent role these modalities have
also played well within the arena of clinical medicine. This is
especially notable in the use of hypothermia. In the early 1950s,
when cardiac surgery was really getting under way, the use of
hypothermia was critical (1). When it was found that under
hypothermia the human brain could tolerate a cardiac arrest
of 6 to 8 minutes without harm, deft cardiac surgeons could
Proc (Bayl Univ Med Cent) 2016;29(1):103–104
open the heart for repair of an atrial septal defect within this
time period. Although later introduction of reliable heart-lung
machines enabled longer periods of surgery for more complicated abnormalities, hypothermia has frequently been used in
concert with such procedures.
In the presence of traumatic brain injuries, neurosurgeons
routinely cool the body of the patient to minimize or avoid brain
damage (2). It has been shown experimentally that induced
hypothermia after potentially lethal hemorrhage can improve
chances of survival (3). Perhaps, eventually, this will improve
survival of humans as well after severe blood loss.
Donated organs are packed in ice while in transit to
recipients to maintain viability. A new twist on this has recently
been introduced for kidney transplantation (4). In the deceased
donor, it has been found that inducing mild hypothermia prior
to removal of the organ results in a significantly reduced rate of
delayed graft function in the recipients. The future of kidney
and other organ transplants may be made brighter through the
institution of this simple adjustment in preparation.
The clinical use of hyperthermia has historically been less
beneficial. When hypothermia occurs in patients subjected to
freezing or subfreezing conditions, warming the body is clearly
the naturally preferred mode of treatment. Beyond this, one
looks in vain for examples of raising body temperature above
normal resulting in improvements or cures. Indeed, one of the
rare major blunders of the Nobel Prize committees occurred as a
result of such an intervention. In 1927 Julius Wagner-Jauregg, a
psychiatrist, was awarded the Nobel Prize in Medicine or Physiology for his treatment of neurosyphilis by infecting patients
with malaria in hopes that the high fevers induced by malaria
would be of benefit in combating the disease. They were not.
All of which brings us back to consideration of the more
mundane type of complaint in question. For such local swellings, more likely to occur traumatically than in the joke above,
what should be our guide? The body’s initial response involves
the delivery of certain cellular elements and biologically active
substances into the affected area. This creates an inflammatory
response which, rather than blocking or alleviating the pain
From the Department of Medicine (retired), Rutgers–New Jersey Medical School.
Corresponding author: Allen B. Weisse, MD, 164 Hillside Avenue, Springfield,
NJ 07081 (e-mail: allenweisse@gmail.com).
103
and swelling, actually exacerbates them. Applying heat will only
worsen the situation by increasing blood flow to the affected
area. The use of cold compresses instead, by causing vasoconstriction, can limit the inflammatory response.
My dentist apparently agrees with this approach to therapy.
I am prone to repeated periodontal problems. After each dental
surgery, my periodontist gives strict instructions to apply ice
packs over the treated area for several hours into the evening to
prevent swelling. The one time I did not follow such instructions
to the letter, swelling and discomfort resulted over the treated
area. In the field of sports medicine, the local application of cold
is also recommended for a number of conditions (5). To varying
extents in various locations, boxers, baseball pitchers, tennis
players, and others apply cryotherapy for a variety of similar
types of self-induced or external causes of trauma.
With such abundant evidence about the benefits of cooling,
one wonders why heat continues to be advocated by some as the
preferred home treatment for the type of injury described. Perhaps
this is related to the well-known benefit of heat in relieving the
pain of many chronic nagging musculoskeletal conditions—what
104
old-timers would refer to as “rheumatism.” Perhaps the memory
of soothing hot springs or spas in America and Europe helps
propagate such beliefs. But for this observer, the proper choice
is a “no-brainer.” As long as it is recognized that some serious
neurological or musculoskeletal problems might initially appear
with minor symptoms, once this is ruled out the way to go is
cool—no matter what my housekeeper says.
1.
2.
3.
4.
5.
Cooper DKC. Open Heart. The Radical Surgeons Who Revolutionized Medicine. New York: Kaplan, 2010:105–142.
Winn HR, ed. Youman’s Neurological Surgery, 5th ed., Vol 4. Philadelphia:
Saunders, 1996.
Alam HB, Rhee P, Honma K, Chen H, Ayuste EC, Lin T, Toruno K,
Mehrani T, Engel C, Chen Z. Does the rate of rewarming from profound
hypothermic arrest influence the outcome in a swine model of lethal
hemorrhage? J Trauma 2006;60(1):134–146.
Niemann CU, Feiner J, Swain S, Bunting S, Friedman M, Crutchfield
M, Broglio K, Hirose R, Roberts JP, Malinoski D. Therapeutic hypothermia in deceased organ donors and kidney-graft function. N Engl J Med
2015;373(5):405–414.
Scuderi GR, McCann PD. Sports Medicine: A Comprehensive Approach,
2nd ed. Philadelphia: Elsevier/Mosby, 2005:592–593.
Baylor University Medical Center Proceedings
Volume 29, Number 1
In memoriam
HASSAN IMAM BUKHARI, MD
Department of Vascular Surgery, Baylor University Medical
Center at Dallas
Dr. Hassan Bukhari, a vascular surgeon born in Gujranwala,
Pakistan, died on September 16, 2015, at the age of 77. He
received his medical degree from King Edward Medical College in Lahore and moved to the United States in 1964 with his
wife, Dr. Talat Hassan Bukhari, a psychiatrist. He completed his
residency in general surgery at Tucson Medical Center and then
completed fellowships in hematology at the Wadley Institute
and in vascular surgery at Baylor University Medical Center at
Dallas. In 1972, he entered private practice as a vascular and
general surgeon and was based at Baylor for 40 years, where
he mentored numerous general surgery and vascular fellowship trainees and was highly respected. Dr. Bukhari founded
the Islamic Association of North Texas, which built mosques
in Grand Prairie and Richardson; the Association of Pakistani
Physicians of North America, for which he served as president
in 1986–1987 and chairman in 2004; and the Hassan and
Talat Bukhari Foundation, which assists developing economies
with health care, higher education, disaster relief, and recovery
programs. Among his numerous professional and civic affiliations, he served as a fellow and director of the Thanks-Giving
Foundation.
MATTHEW L. DAVIS, MD, FACS
Department of Surgery, Baylor Scott & White Health,
Temple, Texas
Matthew L. Davis, MD, FACS, director of trauma, emergency surgery, and surgical critical care and system director
of trauma, Baylor Scott & White, died in a mountain climbing accident on September 3, 2015. He was 41 years old. He
graduated from Tarleton State University in 1997 and from
the University of Texas Medical Branch in 2002. Afterwards,
he completed his surgical residency at Baylor Scott & White
and a trauma/critical care fellowship at Shock Trauma Center
in Baltimore. As trauma director of Baylor Scott & White,
he led the team through two successful Level 1 trauma center
certifications. He also trained numerous residents in the art and
discipline of surgery and trauma. He was a diplomate of the
American Board of Surgery and the American Board of Surgical
Critical Care, an associate professor at the Texas A&M Health
Science Center College of Medicine, an active member and
leader of numerous professional organizations, and a medical
expert for KCEN TV in Temple. He is survived by his wife and
three children.
Proc (Bayl Univ Med Cent) 2016;29(1):105
LUDWIG ALEXANDER MICHAEL, MD
Department of Otolaryngology, Baylor University Medical
Center at Dallas
Ludwig Michael, MD, born on July 20, 1919, in New York
City, died on October 1, 2015, at the age of 96. Dr. Michael was
educated at New York University and the NYU College of Medicine and trained at St. Louis City Hospital and Barnes Hospital in
St. Louis. He then served in the US Army Medical Corps, specializing in audiology. He came to Dallas in 1948, where he practiced
otolaryngology on the medical staff of Baylor University Medical
Center at Dallas for over 60 years and served two tenures as chief
of otolaryngology. He also served on the faculty of the University
of Texas Southwestern Medical School for over 50 years. Dr.
Michael was instrumental in the growth and development of the
Callier Center for Communication Disorders, serving for 4 years
as foundation president. Additionally, he served as an audiology
consultant for the Veterans Administration and on the advisory
board of the Institute on Deafness and Other Communication
Disorders. Dr. Michael was chairman of the editorial committee
of the Dallas Medical Journal for 24 years and was a member
and fellow of numerous professional organizations and an active
volunteer and board member of many health and educational
organizations, including the Lamplighter School.
JAMES HOUSTON SHELTON, MD
Division of Cardiology, Baylor University Medical Center at Dallas
Dr. James Shelton, born in 1944, died unexpectedly in his
home on September 13, 2015. The oldest of three, he grew up in
Dallas and graduated from St. Mark’s School of Texas, where he
was soccer team captain as well as an Eagle Scout. He graduated
with honors from Harvard College in 1966 followed by Harvard
Medical School. In 1970, he married Nancy Breard Shelton and
moved to San Diego, California, for his internship, residency, and
cardiology fellowship with Dr. Eugene Braunwald. He served in
the US Army until 1977 and then joined Dr. John W. Hyland
and Cardiology Associates at Baylor University Medical Center
at Dallas, a practice that later became HeartPlace. Dr. Shelton
was one of the early practitioners of invasive cardiology in Dallas.
He was a founding partner of ESP Cardiology, which became
North Texas Heart Center, and served as director of nuclear cardiology at Baylor. Throughout his 37 years as a physician, Dr.
Shelton was known for a keen sense of humor, a quick wit, and
ready jokes. He served on the boards of the American Heart Association, the Harvard Club, the Jack and Jane Hamilton Heart
and Vascular Hospital, and Cistercian Preparatory School. His
hobbies included flying planes, studying history, and traveling.
105
From the Editor
Facts and ideas from anywhere
HEALTH CARE SAVINGS ACCOUNTS
AND HIGH-DEDUCTIBLE PLANS
According to Scott Atlas and
John Cogan of Stanford University’s Hoover Institution, there are
only two ways to bring down the
costs of health care in this country,
and they are high-deductible insurance coverage and health savings
accounts (HSAs) (1). These authors
William C. Roberts, MD.
point out that the consolidation in
the insurance industry and among
providers will likely drive health care costs even higher. Welldesigned high-deductible insurance in which the individual pays
a few thousand dollars for most health care services before the
plan kicks in to cover claims restores the fundamental purpose
of health insurance: to reduce the financial risk of large and
unanticipated medical expenses. HSAs allow individuals to set
aside money, tax free, for out-of-pocket expenses, including
routine care. These accounts are owned by individuals and are
not dependent on their place of employment.
When consumers pay directly for their care, as they would
from HSAs, they have an incentive to choose wisely and to
demand that the prices charged by providers become visible.
HSAs significantly reduce health spending. When these highdeductible plans were paired with HSAs, health care spending
reductions averaged at least 15% annually.
High-deductible plans and HSAs continue to grow despite
the restrictions of the Affordable Care Act. In 2014, the number of HSAs increased by 29% and reached a record high of
14.5 million as of mid-2015. Nearly one-third of all employers
(31%) now offer some type of HSA, up from 4% in 2005. HSA
account holders deposited $21 billion in 2014. As of June 30,
2015, HSA assets averaged $14,654 per account.
According to the authors’ study, annual health expenditures would fall by an estimated $57 billion if only half of
those Americans with employer-sponsored insurance enrolled
in consumer-directed plans with deductibles as low as $1000.
ObamaCare’s current legal requirement that an individual
or family have coverage with government-specified deductibles
to open an HSA is counterproductive. It eliminates the possibilities of HSAs with other more tailored plans that could
106
cover necessary care subject to a lower deductible for particular services and medicines, especially for chronically ill people.
ObamaCare restrictions on eligibility for high-deductible plans
and broad coverage mandates should also be eliminated to allow
individuals greater flexibility to purchase high-deductible plans
that best suit their health care needs.
MEDICARE PART B PREMIUMS IN 2016
For 70% of Medicare beneficiaries, 2016 costs per month
will be $104.90 for their Medicare Part B premium, the same
as in 2015 (2). For about 30% of Medicare beneficiaries, however, roughly 7 million Americans, the increase could rise 52%
to $159.30 per month. For individuals whose income exceeds
$85,000 annually, premiums could rise from $223.00 per
month to as much as $509.80. The explanation has to do with
the law that addresses cost-of-living adjustments for Social Security benefits. That law limits the dollar increase in the premium
to the dollar increase in an individual’s Social Security benefit.
The Consumer Price Index is not likely to increase in the period
used to determine the cost-of-living adjustments for 2016. That
means it is likely that 70% of Social Security recipients—for just
the third time since automatic adjustments started in 1975—
will not see an increase in their benefit. Who are the persons
who must pay the higher Medicare Part B premium? This group
includes individuals who enroll in Part B for the first time in
2016; enrollees who do not receive a Social Security benefit;
beneficiaries who are directly billed for their Part B premium;
current enrollees who pay an income-related higher premium;
and dual Medicare-Medicaid beneficiaries, whose premiums are
paid by state Medicaid programs.
THE NEW ICD-10 SYSTEM
Physicians, hospitals, and insurers began a massive new
coding system on October 1, 2015, for describing illnesses and
injuries (3). There will now be 70,000 ways to classify ailments.
Cardiologists will now have not one but 845 codes for angioplasty. Dermatologists will now need to specify which of eight
kinds of acne a patient has. Gastroenterologists who don’t know
what’s causing a patient’s stomachache will be asked to specify
where the pain is and what other symptoms are present—gas,
eructation, belching—since there is a separate code for each.
In all, the number of diagnostic codes physicians must use
Proc (Bayl Univ Med Cent) 2016;29(1):106–114
to get paid is expanding from 14,000 to 70,000 in this new
version of the International Classification of Diseases, or ICD10. A separate set of ICD-10 procedure codes for hospitals
is expanding from 4000 to 72,000! Hospitals and physician
practices have spent billions of dollars on training programs,
boot camps, apps, flash cards, and practice drills to prepare for
the conversion, which has been postponed three times since
the original date in 2011. Some coding experts warn that claim
denials could double as providers and payers get used to the
new, more specific codes.
The ICD codes are an international system for recording
diseases, injuries, and other conditions set by the World Health
Organization; federal agencies developed the more elaborate
version for the US. To get paid, physicians submit both diagnostic and procedure codes that describe the services performed.
Private and government insurers scrutinize the ICD codes to
judge whether the service was medically necessary.
PHYSICIANS IN STATE LEGISLATURES
According to a 2014 compilation by the American Medical
Association, the Texas Legislature ranks third in its percentage
of physician lawmakers—6 of 181 (3.3%) (4). Only in Nevada
and Utah did physicians wield a bigger presence, with 4.8% in
each. Utah, however, has only five physician lawmakers and
Nevada, three. All six in Texas are Republicans.
THE NEW CARDIOPULMONARY RESUSCITATION
Time is of the essence when cardiac arrest strikes, and bystanders shouldn’t wait for paramedics to help (5). The best
technique is now hands-only CPR without mouth-to-mouth
contact. Just keep pumping until the paramedics arrive. After
calling 911, use both hands to push hard into the center of the
person’s chest. The American Heart Association recommends
doing CPR to the tempo of “Staying Alive.”
ELEPHANTS AND CANCER
Joshua Schiffman and colleagues (6, 7) published an article
in JAMA demonstrating that certain animals—elephants, bowhead whales, and rock hyrax—have cancer rates <5%, whereas
humans have cancer death rates from 11% to 25%. In contrast,
African wild dogs have cancer death rates of 8% and cheetahs,
>20%. These authors also indicated that it’s a myth that sharks
don’t get cancer. Because cancer tends to attack the older populations and because elephants live 100 years or so, they might have
a high cancer rate. Elephants weigh about 200 pounds at birth
and up to 12,000 pounds as adults. All that growth involves
cell division, a process that provides opportunities for potentially lethal genetic mistakes. Yet cancer is rare in elephants.
These authors suggest a likely reason: elephants have 20 times as
many copies of a key cancer-fighting gene as humans. Humans
typically have just two copies of a tumor-blocking gene called
TP53, inheriting one from their mother and one from their
father. Elephants have 40 copies. TP53 appears to play a vital
role in preventing cancer. Schiffman described this gene as the
“guardian of the genome,” scanning cells for genetic mistakes
and destroying ones that can’t be fixed.
January 2016
ROBOTS REPLACING HUMANS
Thomas G. Donlan has a weekly column in Barron’s. His
September 7, 2015, column featured comments on C. G. P.
Grey’s YouTube video entitled “Humans Need Not Apply”
about the certainty that many important jobs will soon be filled
by robots (8): 45% of American jobs—from truck driving to
retail sales—could be filled by robots using technology that is
already available.
Horses used to be our substitute for human muscle power,
and we still measure the work done by machines in horsepower.
But machinery has not created new jobs or horses. The number
of horses in the world peaked in 1915. Nearly all horses now
exist for human entertainment.
As Donlan states, “Machinery created new jobs for the machines.” In 1950, 488,000 Americans worked in coal mines and
produced 560 million tons of coal—1150 tons per miner. In
2013, 80,000 people operated machines that dug 982 million
tons of coal. A sixth of the former workforce produced almost
twice as much coal, 12,000 tons per miner. The symbol of the
new economy in coal is the giant power shovel, whose skilled
operator has replaced hundreds of men with shovels.
Nearly a century ago, semiautomatic machines drove most
laborers off the farms, and most of the owners of most of the
family farms soon followed. The survivors learned to control
complex machinery and make practical decisions about planting, irrigation, and harvesting with the aid of computers. Nevertheless, most of them make most of their money in towns on
alternate jobs that have little or nothing to do with the farms.
The few remaining farmers feed the larger nation with greater
abundance and variety at lower prices for most food. What
happened to the family farm will happen to the family fast-food
franchise and perhaps family restaurants. Machines for taking
food orders and preparing food, from frying French fries to flipping hamburgers, are taking jobs in the fast-food chains, where
several generations of young people have learned the basic labor
skills of showing up on time and following instructions. They
will have to be better prepared for their first real job in some
other way. It will not be long before a robot with vision and
soft hands can clear a restaurant table, carry a tray, and load
the dishwasher at a price that beats a minimum wage busboy.
If robots, as Thomas Donlan writes, rise and create enormous output per unit of labor, they may well support a welfare
system that provides an income earned today by a hardworking
physician. Autodocs may replace real doctors. Most Americans
would then be able to choose an occupation based on satisfaction without concern for whether they can live on its salary.
MURDERS IN THE US INCREASING
Crime data reporting has always been voluntary, and only
some of the country’s 18,000 police departments provide crime
data to the Federal Bureau of Investigation’s National IncidentBased Reporting System (9). Only one-third of the US population is included in the database. Nevertheless, based on that
data, it appears that there has been a sudden and dramatic
upsurge in murders in the period from January 1 to July 15,
2015, compared with the same period in 2014. The number of
Facts and ideas from anywhere
107
murders in Chicago rose from 198 to 235; in Houston, from
113 to 154; in New Orleans, from 84 to 103; in St. Louis,
from 64 to 94; in Milwaukee, from 39 to 85; in Dallas, from
54 to 75; and in Atlanta, from 45 to 52. The reason for this
increase is unclear.
US FOREIGN-BORN POPULATION
The percentage of people living in the USA who were born
outside the country reached 13.7% in 2015 and is projected
to hit a record 14.9% by 2025 (10). A high of 14.8% was set
in 1890 when Irish, Italian, Polish, and other immigrants were
coming to the USA. The term “foreign-born” includes naturalized citizens, legal permanent residents, visa holders, and
undocumented immigrants.
COMMERCIAL AIRLINE SEATS
People are getting bigger, seats are getting smaller, and the
legroom is diminishing (11). In 1960, the average US adult
woman weighed 140 pounds and the average man, 166 pounds.
Now the average woman weighs 166 pounds and the average
man, 196, and both are about one inch taller. In most commercial airlines, the leg room in coach has shortened from 35 to
31 inches, and the average seat width has narrowed from about
18 to 17 inches or less. It is no wonder why commercial airline
flights are less pleasant now than in years past.
these salad ingredients. Tamar Haspel (14) argues that lettuce
occupies precious crop acreage, requires fossil fuels to be shipped
refrigerated around the world, and adds only crunch to the
plate. She argues that the makings of a green salad—a head of
lettuce, a cucumber, and a bunch of radishes—cost about $3
at her supermarket. She indicates for that price she could buy
>2 pounds of broccoli, sweet potatoes, or almost any frozen
vegetable, which would be a much more nutritious side dish
than the salad. Lettuce is the top source of food waste, with >1
billion pounds of uneaten salad every year. It is also the chief
culprit for foodborne illnesses. According to the Centers for Disease Control and Prevention, green leafy vegetables accounted
for 22% of all foodborne illnesses from 1998 to 2008. Maybe
salad should not be the staple many of us think it is.
SUGAR-SWEETENED SOFT DRINKS
The British organization Action On Sugar sent an e-mail
calling for sugar-sweetened soft drink manufacturers to set
global sugar reduction targets to halt the worldwide obesity
epidemic set to reach 1.12 billion by 2030 (15). The survey,
which reviewed 274 sugar-sweetened soft drinks produced
across the world, found that every single product (with available nutrition data) would receive a dangerously high red colorcoded label if it were consumed in a standard 330 mL can.
Furthermore, 88% of products (with available nutrition data)
contained more than an adult’s entire recommendation for the
day. Indeed, if a 330 mL can of Coca-Cola, Pepsi, and 7 Up
were consumed anywhere in the world, 100% contain more
than an entire adult’s maximum daily amount of free sugars for
the day (25 g—6 teaspoons/day). The countries with the highest free sugars content per 330 mL can were in North America
(either Canada or the USA), whereas countries in Europe had
the lowest sugar content (Table 1).
HOT PEPPERS
In an article in the British Medical Journal online on August
4, 2015, the authors studied nearly half a million Chinese adults
and followed them for >7 years (12, 13). Those who ate dishes
with fresh or dried chili peppers several times a week were 14%
less likely to die during the study period than those who hardly
ever ate them. Capsaicin, the hot compound in chili peppers,
lowers blood pressure, reduces the risk of cancer, fights inflamALEXANDER VON HUMBOLDT (1769–1859)
mation, is an antioxidant, has antibacterial activity, and is a great
Andrea Wulf has provided a magnificent book on Alexander
source of vitamins C, A, B6, and K and potassium. Which of
Von Humboldt, the Prussian naturalist (16) (Figure 1). He is
these nutrients might be contributing to the apparent health
nearly forgotten now in the English-speaking world, but at the
benefits of hot chili peppers is unclear. Capsaicin is used in
liniments for sore joints, and the Food and
Drug Administration approved a capsaicin
cream, Zostrix, to treat the painful rash of
Table 1. Differences in highest and lowest free sugars content of popular
sugar-sweetened soft drinks
shingles. Others have found capsaicin to
work against resistant plantar warts, and
Highest
Sugars
Sugars
some have found it useful to stop bad miProduct name
country
(g/330 mL)
Lowest country
(g/330 mL)
graines.
Schweppes Tonic Water USA
45
Argentina
16
FOODS WITHOUT NUTRITIONAL VALUE
They are salad ingredients: cucumbers,
radishes, lettuce, celery, and eggplant. The
nutritional value of these five foods can
be explained by one fact: they are almost
all water. Charles Benbrook and Donald
Davis developed a nutrient quality index,
a way to rate foods based on how much of
27 nutrients they contain per 100 calories.
Four of the five lowest-ranking foods are
Sprite
Thailand*
47
Austria,† Poland†
19
Fanta Orange
India, Vietnam
43
UK,† Ireland,† Argentina
23
Dr. Pepper
USA
36
Germany*
22
Coca-Cola
Canada*
39
Thailand
32
Pepsi
Japan‡
39
UK, Greece, Serbia, Switzerland
35
7 Up
Canada
39
USA
35
108
Baylor University Medical Center Proceedings
*No ingredients list found online to verify if noncaloric sweeteners were added.
†With added noncaloric sweeteners (e.g., Stevia).
‡Carbohydrate labeled, not sugars. (Sugars will be the main source of carbohydrate.)
Source: Action on Sugar (15).
Volume 29, Number 1
time of his death, he was the
most famous scientist in the
world. His funeral in Berlin
was the grandest ever recorded
to a private German individual:
a procession of tens of thousands of mourners followed for
a mile behind the hearse pulled
by the king’s horses. American
newspapers eulogized him as
the “most remarkable man ever
born” and lamented the end
of the “age of Humboldt.” A
decade later on the centennial
of Humboldt’s birth, parades,
Figure 1. The Invention of Nature.
concerts, and firework shows
were held in Moscow, Alexandria, Buenos Aires, Mexico City, Melbourne, and dozens of
American cities. Fifteen thousand marched in Syracuse. President Ulysses S. Grant joined the huge celebration in Pittsburgh,
and 25,000 assembled in Central Park in New York.
Humboldt was born during the era in which human beings
stopped fearing nature and began to control it. The steam engine, the smallpox vaccine, and the lightening rod were rapidly
redefining man’s relationship with the natural world. Timekeeping and measuring systems became standardized.
Humboldt’s father was a chamberlain in the Prussian court
and a confidant to the future king, who was godfather to Humboldt; his mother was the daughter of a wealthy manufacturer
and member of the Prussian civil service. After university he
became an inspector in the Ministry of Mines, a job that satisfied
his mother’s desire for him to ascend the ranks of the Prussian
civil service, while allowing him to travel widely across the kingdom and conduct personal experiments in geology, anatomy,
and electricity. It was not until his mother died of cancer in
1796 when he was 27 that he felt free.
Supported by a large inheritance, he abandoned his mining
career and planned “a great voyage” to a distant location. He
settled on South America once he was offered a passport to the
Spanish colonies from King Carlos IV himself. Nor did he have
any specific object of study. He would analyze everything, from
wind patterns and cloud structures to insect behavior and soil
composition. He would collect species, make measurements,
and take temperatures. He wanted to discover how “all forces of
nature are interlaced and interwoven.” He took as the premise
of his expedition that the Earth was “one great living organism
where everything was connected.”
An account of his 5-year trip to South America was collected
in his 34-volume Voyage to the Equinoctial Region of the New
Continent, published between 1807 and 1826. On his voyage
Humboldt explored Venezuela, Cuba, Mexico, Colombia, and
Peru, visiting many regions never before observed by scientists.
He identified 2000 new plant species at a time when only 6000
species were known. (More plants, animals, minerals, and places
are named after Humboldt than anyone else!) He discovered
the magnetic equator. He was the first European to explore
January 2016
and map the Casiquiare River, the only natural canal on Earth
to link two major river systems, the Orinoco and the Amazon.
He was the first to conduct experiments on electric eels, which
he dissected and held in his hands, enduring violent shocks.
Humboldt went to extremes in his voracious quest for
knowledge. He drank river water (the Orinoco was particularly disgusting, while the Atabapo was “delicious”), chewed
bark, copied and translated scientific manuscripts, made astronomical observations, gauged the balloonists of the sky with a
cyanometer, transcribed the vocabularies of indigenous tribes,
and sketched Incan monuments and hieroglyphs of ancient
civilizations deep in the Amazonian rainforest. He studied his
own lice with a microscope. On the Chimborazo Volcano,
17,000 feet above sea level, Humboldt crawled along a 2-inchwide ridge between a sheer icy cliff and a 1000 foot drop with
“almost perpendicular walls covered with rocks that protruded
like knife blades.” Humboldt bathed in the Orinoco among
crocodiles, gigantic boa constrictors, herds of capybaras, and
jaguars. He contracted fevers, dysentery, blood infections, and
horrific Amazonian diseases. With his companion, the naturalist
Aimë Bonpland, he scaled every peak he could see in the Andes.
When his shoes disintegrated, he continued barefoot. While
traveling from Cuba to the Atlantic seaboard, he sailed straight
into a hurricane which lingered for 6 days, inundating the ship
so that the passengers had to swim through the captain’s cabin
while sharks circled the turbid waters.
After his 5-year voyage through Latin America, Humboldt
landed in the USA in May 1804. He spent a week in Washington, regaling President Thomas Jefferson, Secretary of State
James Madison, and Treasury Secretary Albert Gallatin with
information about the Spanish colonies, which to that point
had largely been closed to American contact. Jefferson was then
in a border dispute with Spain over the land between the Sabine
and Rio Grande Rivers. Humboldt convinced Jefferson that the
land—today the state of Texas—despite its deserts and savanna
was worth fighting for.
Humboldt initially settled in Paris where he set to writing
and lecturing about his voyage. He skipped meals and barely
slept. He had brought back about 60,000 species in his trip.
His maps, political essays about the colonies, and the data he
collected about agriculture, manufacturing, geology, botany,
zoology, fluidology, and meteorology revolutionized each of
these fields. He met often with politicians, scientists, and the
aristocracy. He appears to have been nearly universally adored.
Humboldt’s most consequential finding derived from his conception of the world as a single unified organism. “Everything,” he
said, “is interaction and reciprocal.” Although this view appears
commonplace today, the concept was Humboldt’s invention. The
thinking at the time echoed Aristotle’s view that “nature has made
all things specifically for the sake of man.” Particularly heterodox
was the implication that the decline of one species might have
cascading effects on others. The possibility that animal life might
not be inexhaustible had been proposed previously but was not
widely accepted. The idea that human beings might interfere with
the natural order of things was a radical rejection of prevailing
views about man’s domination over nature.
Facts and ideas from anywhere
109
Charles Darwin appears to have been the most slavish of his
acolytes: he wrote in his journal that Humboldt “like another
Sun illuminates everything I behold.” It was Humboldt’s Personal
Narrative, a 7-volume subsection of Voyage, that inspired Darwin
to travel in distant countries and led him to volunteer as the naturalist in His Majesty’s ship, Beagle. He brought his personal copy
of the Narrative on the Beagle with him and read it. Humboldt’s
“gradual transformation of species” that specifically limited species’ numbers through “long-continued contest for nourishment
and territory, with only the strongest surviving” was new with
Humboldt. That view, of course, would become essential to Darwin’s concept of natural selection. Wulf also points out that the
final crowning paragraph of Origin of Species is a nearly verbatim
plagiarism of a passage in Humboldt’s Personal Narrative.
If everything in nature interacted, then it stood to reason
that the natural world was not stable but prone to dynamic
changes. It followed that man, by disrupting the natural order,
might inadvertently bring about catastrophe. Humboldt was
among the first to write of the perils of deforestation, irrigation,
and cash crop agriculture, asserting that the brutal repercussions
of man’s “insatiable avarice” were already “incalculable.”
During his year-long expedition to Russia in 1829 he gave
a speech at the Imperial Academy of Sciences in St. Petersburg
calling for vast international collaboration in which scientists
around the world would collect data related to the effects of
deforestation, the first global study of man’s impact on climate,
and a model for the International Intergovernmental Panel on
Climate Change assembled 160 years later.
THE MEDICALS IN PARIS (1830–1900)
David McCullough has
come up with another great
book: The Greater Journey: Americans in Paris (17) (Figure 2).
The Greater Journey is the enthralling and inspiring story
of adventurous American artists, writers, physicians, politicians, architects, and others of
high aspiration who went to
Paris between 1830 and 1900,
anxious to excel in their work.
The journey across the Atlantic
was hazardous. Most had never
left home, never experienced a
Figure 2. The Greater Journey.
different culture. None had a
guarantee of success. That they
achieved so much for themselves and their country altered
American history.
One who made the journey to the City of Light was Charles
Sumner, who enrolled in the Sorbonne because of a desire to
know more about everything. Later, he became the most powerful unyielding voice for abolition in the US Senate. Two staunch
friends, James Fenimore Cooper and Samuel F. B. Morse, worked
unrelentingly in Paris, Cooper writing and Morse painting. From
something he saw in France, Morse conceived of the telegraph,
110
which he later invented. Pianist Louis Moreau Gottschalk from
New Orleans launched his spectacular career performing in Paris.
George P. A. Healy became one of the most celebrated portrait
painters of the day. His subjects included Abraham Lincoln. Writers Ralph Waldo Emerson, Nathaniel Hawthorne, Mark Twain, and
Henry James all discovered Paris—marveling at the treasures in
the Louvre, or out with the Sunday throngs strolling the city’s
boulevards and gardens. These also included Harriet Beecher
Stowe, seeking escape from the notoriety Uncle Tom’s Cabin had
brought her. The genius of sculptor Augustus Saint-Gaudens and
painters Mary Cassatt and John Singer Sargent, three of the greatest American artists ever, would flourish in Paris, inspired by the
examples of brilliant French masters and by Paris itself.
Nearly all of these Americans, whatever their troubles learning French, their spells of homesickness, and their sufferings in
the raw cold winters by the Seine, spent many of the happiest
days and nights of their lives in Paris. McCullough tells this
fascinating story with power and intimacy.
A chapter on “The Medicals,” Paris Médicale, described Paris’
numerous hospitals; illustrious physicians, nurses, interns, and
several thousand students from every part of France and much
of the world; patients, numbering in the many thousands; and a
celebrated medical school, the École de Médecine. Visitors were
welcomed to the hospitals and surgical amphitheaters, and more
often than not what they saw, the dedication and kindness of the
nurses, the orderliness and scale of the care given, seemed everything that could be desired. As a place to learn, it had no equal.
Of the many hospitals in Paris, three dominated: Hótel Dieu,
the largest with 1400 beds, built in 1602; Hópital de la Pitié,
the second largest with 800 beds; and Hópital de la Charité,
with 400 beds. All three were in walking distance of each other
and also of the famous medical school, École de Médecine,
founded in 1776. The first children’s hospital in the world was
there, Hópital de Enfants Malades; the first asylum for indigent
and deranged women, Hópital de la Salpêtrière; and the first
asylum for indigent and deranged men, Hópital de Bicétre. The
first hospital for diseases of the skin—Hópital Saint-Louis—was
also in Paris.
In 1833, the year following the cholera epidemic, a total
of 12 Paris hospitals provided treatment for just under 66,000
patients. In Boston, by comparison, the Massachusetts General
Hospital and the McLean Hospital together cared for fewer
than 800 patients.
The heart of medical Paris was the three largest hospitals and
the nearby École de Médecine. Here, at these three hospitals
primarily, and at the medical school, the great luminaries of
French medicine, many of international reputation, held forth
in the lecture halls and allowed students to accompany them as
they made their rounds of the patients in the wards.
Auguste François Chomel was a leading clinical physician
whose bedside comments during the morning rounds at the
Hótel Dieu attracted a large following. Guillaume Dupuytren
held the supreme position of chief surgeon at the same hospital.
Alfred-Armand-Louis-Marie Velpeau lectured at La Charité and
the École de Médecine. He wrote the treatise on surgery used
by most students and was considered an example of a man who
Baylor University Medical Center Proceedings
Volume 29, Number 1
by merit and hard work had risen from obscure beginnings to
the forefront of his profession. He was the son of a blacksmith.
Philippe Ricord was a noted specialist in syphilis and one of
the few medical professors who spoke English. Gabriel Andral
lectured at the École on internal pathology and, in the view of
many students, was the most eloquent professor of them all.
Pierre Charles Alexandre Louis, though neither eloquent nor
especially popular, was to have the greatest influence on the
American students. Louis stood foremost in insisting on evidence—facts—as essential to diagnosis and was greatly admired
as the best man in Paris with a stethoscope.
A public institution, the École de Médecine was a showpiece
of French education. Since the Revolution of 1789, opportunities for medical education had been made available to a degree
unimaginable earlier. The profession of medicine opened to
all qualified young men irrespective of wealth or background.
In the spirit of opening wide the door, French, not Latin, had
been made the language of instruction. A college education or
equivalent was required for admission, as was not the case at
American medical schools, but foreign students at the École did
not have to meet this requirement. Further, for foreign students,
including Americans, there was no tuition. For them, as at the
Sorbonne, lectures were free.
Nothing in the United States remotely compared to the
École de Médecine. Medical education in the US at the time
was barely underway. In the 1830s, the US had only 21 medical
schools, or on average <1 per state, and they were small, with
faculties of only 5 or 6 professors. Most aspiring physicians in
America never attended medical school but learned by apprenticing themselves to “respectable” practitioners, most of whom
had been poorly trained.
At the École de Médecine, the faculty of 26 delivered lectures on anatomy, physiology, physics, medical hygiene, medical
natural history, accouchement (birth), surgical pathology, pharmacology, organic pharmacology and organic chemistry, medical pathology, therapeutics, pathological anatomy, operative
surgery, clinical surgery, clinical medicine, clinical midwifery,
diseases of women and children, and legal medicine. Enrollment was as high as 5000 students, or approximately twice the
number of students then in all medical schools in the USA. The
American students at the École in the 1830s and 1840s were but
a tiny part of enrollment, numbering only 30 to 50 annually.
For those American students newly arrived in Paris, however, the
prospect of entering such a world was exciting and unnerving,
quite apart from the considerable problem of language.
At the request of his physician father back in Boston, Mason
Warren described what constituted a typical day, once he was
seriously involved:
I commonly rise a little after 6:00. The servant comes in every
morning to wake me and light my candle. From 6 until 8 I
attend Chomel at Hótel Dieu, a man at present very celebrated
for his knowledge of diseases of the lungs. At 8 Dupuytren
commences his visit which lasts an hour, that is till 9 and he
afterwards lectures and has his consultations and operations,
which occupies the time until 11. I then breakfast.
January 2016
Breakfast over, he attended a lecture on surgery, followed by
another on surgical pathology until 4:00. Dinner was at 5:00.
Evenings were occupied with reading and lessons in French
from a private tutor.
Students at the École de Médecine chose “lines of study” in
either general medicine or surgery, and while they all attended
lectures in both as part of their training and made the rounds
of the hospitals with both physicians and surgeons, those training in surgery followed a different curriculum. Thus, Warren’s
schedule had little resemblance to that of his friends, Jackson,
Bowditch, and Holmes, none of whom aspired to be surgeons.
As a student, Warren was not on a level with James Jackson—
but then no one was—and he was slower than others learning
French. As the son and grandson of famous surgeons, Warren
had long known how much was expected of him. Like James
Jackson, he was obliged to report regularly to his father. It was not
just that John Collins Warren cared greatly about the well-being
and professional progress of his son but that he insisted on being
kept continuously apprised of all that was new and innovative in
surgical practice abroad. Like James Jackson, Warren provided his
father with a detailed, running chronicle of how he was making
use of his time, the procedures he was observing, his professors
and what he thought of them, and the books and professional
journals he was reading. His letters, written in a strong, generally clear hand, customarily ran 5 to 8 pages. In this way he
would contribute the fullest descriptions of the many accounts
by Americans of student life in the medical world of Paris.
Inside the ancient Hótel Dieu, the long wards were each
like the great hall of a castle, with rows of beds down both sides
numbering nearly 100. The waxed oak floors were polished to a
high gloss. All were quite orderly. Each of the beds was enclosed
with its own white curtains, and high on the walls above each
bed a good-sized window provided ample light and ventilation.
Even with as many as 1200 patients in the hospital, it did not
feel crowded.
Scores of Soeurs de la Charité nuns of the order of Saint Augustine, wearing large white caps, went briskly about their tasks
as nurses. Accounts by the Americans frequently expressed appreciation for “those excellent women,” their skill and kindness.
For students, the great advantage of study in a hospital of
such size was the number of sick and wounded of all descriptions, and thus in the number of different diseases and ailments
to be observed firsthand. They might attend a physician’s examination of half a dozen or more cases of tuberculosis, say, not just
one or two, or any of a dozen of other maladies. Over a period
of a few months, a student might take part in the examination
of as many as 50 cases of tuberculosis. In the USA, in all but
a few medical schools, no experience of any kind in hospitals
was required of students!
The first rounds on the wards began before dawn at 6:00.
They were conducted by candlelight, and when led by one of
the more eminent physicians, attended by as many as 200 or
300 students, which for most made it nearly impossible to get
near enough to the beds to see much. To the Americans, the
French students seemed inordinately eager to get as close as
possible, and competition for vantage point could be fierce.
Facts and ideas from anywhere
111
Wendell Holmes would remember students piling up on the
back of the chief surgeon, Baron Guillaume Dupuytren, in an
effort to see as he bent over a patient, to the point where he
would shake them off from his broad shoulders.
Dupuytren, one of the medical giants of France, let no one
doubt he was the reigning presence in the Hótel Dieu. He was
handsome, squarely built, and intimidating. Napoleon made
him a baron. Clad in his long white apron, he marched heavily
through the wards, like “a lesser-kind of deity.” He reputedly
spent most nights at one of the better gambling houses at the
Palais Royal. To see Dupuytren at work with scalpel in hand was
to witness a great performance, according to Wendell Holmes.
He talked the whole time he worked and loved to “make a show.”
To the French, it seemed, everything was theater, even surgery.
Mason Warren watched as Dupuytren, working by candlelight, removed cataracts from the eyes of several patients, and,
from another, a tumor of the tongue the size of a peach. He
saw Dupuytren extract stones from the bladder of a child and
performed the operation for an artificial anus for which he was
also famous. Warren attended as well the lectures and operations of surgeon Philibert Joseph Roux at the Hótel Dieu and
Jacques Lisfranc at La Charité, both known for their skill at
amputation. That the eminent Dupuytren and other surgeons
used no anesthetics or washed their hands before operations or
sterilized their instruments was not recorded or remarked upon
by Mason Warren or others for the reason that no one as yet
knew anything about such precautions. Nor did Warren write
of the screams of the patients.
The attitude of several of the French surgeons toward their
patients troubled Warren and others considerably. Lisfranc was
a phlebotomist, a great believer in drawing blood. On one occasion, Wendell Holmes saw him order 10 or 15 patients to be
bled. (The Hótel Dieu maintained a ready supply of leeches for
the purpose and a full-time keeper of leeches was part of the
staff.) Too often it seemed to some of the Americans that the
French surgeons’ primary motivation was the desire to operate with little or no consideration for the patient. By Warren’s
estimate, more than two-thirds of those upon whom amputations were performed died afterward. In fact, most patients who
survived surgery of any kind at the hands of the most skilled
surgeons later died and nearly always of infection. The work
of the French chemist Louis Pasteur on the role of bacteria and
the spread of disease, and that of the English physician Joseph
Lister in antiseptic surgery, was still in the future.
In addition to the quality of the hospitals, the number of
patients, the ability and eminence of the faculty, and the variety
of instruction provided, medical training in Paris offered two
further important advantages over medical training in the USA.
Both had almost entirely to do with the difference in how people
saw things in the two countries. The first was that students
making the rounds on the wards in the hospitals of Paris had
ample opportunity to examine female patients as well as men.
This was not the case in the US, where most women would have
preferred to die than have a physician, a man, examine their
bodies. The French women on the contrary knew nothing at all
of this queasy American sensibility. The second great difference
112
was in the supply of cadavers for dissection. In the US, because
of state laws and public attitudes, dead bodies for medical study
were hard to obtain and consequently expensive. Until 1831,
trade in dead bodies in Massachusetts had been illegal, which led
many American students of early years, including Mason Warren’s father, to become grave robbers. The new Massachusetts
law permitted only the use of corpses buried at public expense,
which meant mainly the bodies of those who died in prison.
In Paris, there was not the least prejudice against dissections.
Even mortally ill patients in the hospitals, “aware of their fate”
and knowing that two-thirds of the dead were carried off to the
dissecting rooms, did not seem to mind. Beyond the hospitals,
due in large part to the ravages of disease and poverty, cadavers
were readily available and cheap, about 6 francs for an adult,
or $2.50, and still less for a child.
Delivery time for corpses at the Amphithéâtre d’Anatomie,
on the Rue d’Orléans near the Hópital de la Pitié, was at noon.
Wendell Holmes wrote how he and a Swiss student split the cost
of their “subject” and by evening had “cut him into inch pieces.”
Thus could all parts of the human body—nerves, muscles, organs, blood vessels, and bones—be studied, and this, Holmes
stressed, could hardly be done anywhere in the world but in
Paris. The size of the stone-floored amphitheater was such that
600 students could practice operations at the same time. The
stench in the thick air was horrific. Disposal of the discarded
pieces was managed by feeding them to dogs kept in cages
outside. In summer, dissecting was suspended because in the
heat the bodies decomposed too rapidly.
The “medicals” found their Paris quite as inspirational as
would the Americans who came to write or paint or study or
imbibe in ideas in other fields. In Paris they felt the exhilaration of being at the center of things, as Wendell Holmes tried
to convey to his father:
I never was so busy in my life. The hall where we hear our
lectures contains nearly a thousand students and it is every day
filled to overflowing. . . . The whole walls around the École de
Médecine are covered with notices of lectures. . . . The lessons
are ringing aloud through all the great hospitals. The students
from all lands are gathered.
“Not a day passes,” declared James Jackson, “that I do not
gain something new in itself or something old with renewed
force.” In addition to the hospitals and lectures was the library of
the École with its 30,000 volumes. (By comparison, the library
of the College of Physicians and Surgeons of New York City
had only 1200 volumes. The library of the Harvard Medical
School had fewer still.) There were, besides, the world-renowned
exhibits and lectures nearby at the Musée d’Histoire Naturelle at
the Jardin des Plantes.
Henry Bowditch was another of those with an illustrious
father, Nathaniel Bowditch, the self-taught astronomer and
mathematician, who in 1802, after sailing much of the world,
had published The New American Practical Navigator, which
made his name known everywhere. Henry Bowditch worked
hard and caught on quickly. James Jackson’s friendship was a
godsend to Bowditch. Jackson was the trailblazer, the guiding
Baylor University Medical Center Proceedings
Volume 29, Number 1
spirit, the one, they were all certain, destined to make a great
mark in time to come. Jackson “devotes himself heart and soul
to his profession,” Bowditch wrote. “I love him much.” Jackson
made sure Bowditch was headed in the right direction, stressing
especially that he attach himself to Pierre Louis. Great as was
Jackson’s admiration for the eloquent Gabriel Andral, he had
come to idolize Louis as the “Master of the Age” in diagnosis.
Only on Sundays did it appear that these Americans turned
from work to the pleasures of Paris. Warren, Jackson, Bowditch,
Holmes, and others would cross the Seine to attend the opera or
theater and dine at their favorite restaurant where “full of warm
blood, of mirth, of gossiping,” they delighted in the French
cuisine and their favorite Burgundy.
Of the celebrated teachers and practitioners of medicine
who held their sway in Paris in the middle of the 19th century,
none was so esteemed by the American students, or had such influence on them, as Pierre Charles Alexandre Louis. For 20 years
and more he was to inspire American medical students as did
no other French physician. He was neither spellbinding nor
flamboyant. He could never have filled the amphitheater at the
École as did Gabriel Andral. He spoke quietly. Henry Bowditch
would remember him as ill at ease as a teacher and awkward
when lecturing. Yet he had a power. What set him apart from
the others was his clearheaded approach to the treatment of
disease, his insistence on the need for analysis based on evidence,
on “facts.” As Holmes said, he taught “the love of truth.” That
he was married to the sister of Victor Hugo gave him an added
importance. Also, like the surgeon Velpeau, Louis was partial
to American students, and like Velpeau, he saw promise in this
particular group of Americans—Jackson, Warren, Bowditch,
and Holmes. Jackson was the master’s favorite, and working
with Louis during the cholera epidemic had left Jackson in
even greater awe of him. He had come to think of Louis as a
second father. And Louis, as he would later tell James Jackson
Sr., thought of James as a son.
Between 1830 and 1860, nearly 700 Americans came to
Paris to study medicine, and nearly all returned home to practice
their profession greatly benefiting by what they had learned.
And much of this they would pass on to others. Decades later,
in the 1890s, William Osler would write that “modern scientific
medicine” had had its rise in France in the early days of the “century.” More than any others it was the pupils of Pierre-Louis who
gave “impetus to the scientific study of medicine” in the US.
YOGI BERRA (1925–2015)
Yogi Berra (18–20), a New York Yankee for nearly 20 years,
was a catcher and later an outfielder. He led the Yankees in
runs batted in for seven consecutive seasons (1949–1955) on a
team that also included Mickey Mantle and, for three of those
seasons, Joe DiMaggio. Berra was an 18-time All-Star, a member of a record 14 American League pennant winners and 10
World Champion Yankee teams, and a 1972 inductee into the
Baseball Hall of Fame.
Berra, who dropped out of school after the eighth grade to
help support his family, is nearly as well known for his unique
use of the English language as he is for his baseball heroics. He
January 2016
fought for his country on the beaches of Normandy on D-Day
in 1944. He delighted in the joys of family and brought roaring
laughter with his words wherever he went. His wit and wisdom
have not only found their way into the American lexicon but
also into Bartlett’s Familiar Quotations. Some of Yogi’s quotes
are the following:
• “I never said most of the things I said.”
• “Half the lies they tell about me aren’t true.”
• “Always go to the other people’s funerals; otherwise
they won’t come to yours.”
• “If you don’t know where you are going, you’ll end up
someplace else.”
• “You can observe a lot just by watching.”
• “It ain’t over ’til it’s over.”
• “The future ain’t what it used to be.”
• “Cut my pie into four pieces; I don’t think I could
eat eight.”
• “In theory, there is no difference between theory and
practice. But in practice, there is.”
• “Nobody comes here anymore; it’s too crowded.”
• “Ninety percent of the game is half mental.”
• “I wish I had an answer to that because I’m tired of
answering that question.”
• “If the world were perfect, it wouldn’t be.”
• “Okay you guys, pair up in threes!”
• “Déjà vu all over again.”
• “We made too many wrong mistakes.”
• “I’d give my right arm to be ambidextrous.”
• “You wouldn’t have won if we’d beaten you.”
• “We lost, but we’re making good time.”
• “A nickel ain’t worth a dime anymore.”
• “It’s tough to make predictions, especially about the
future.”
• “I’m not going to buy my kids an encyclopedia. Let
them walk to school like I did.”
• “You have to give 100% in the first half of the game.
If that isn’t enough, in the second half, you have to
give what’s left.”
• “If you ask me anything I don’t know, I’m not going
to answer.”
• “It’s getting late early.”
• “It ain’t the heat, it’s the humility.”
• “He must have made that before he died.”
• “Even Napoleon had his Watergate.”
• “If you can’t imitate him, don’t copy him.”
• “Little League baseball is a very good thing because it
keeps the parents off the streets.”
• “No matter where you go, there you are.”
• “If the fans don’t wanna come out to the ballpark, no
one can stop ’em.”
• “Pitching always beats batting—and vice-versa.”
• “Ninety percent of all mental errors are in your head.”
•
“It ain’t over until the fat lady sings.”
• “If I didn’t wake up, I’d still be sleeping.”
• “Love is the most important thing in the world, but
baseball is pretty good, too.”
Facts and ideas from anywhere
113
•
“I tell the kids, somebody’s gotta win, somebody’s gotta
lose. Just don’t fight about it. Just try to get better.”
9.
10.
11.
12.
William Clifford Roberts, MD
November 12, 2015
1.
2.
3.
4.
5.
6.
7.
8.
114
Atlas SW, Cogan JF. Two essential tools for repairing the ObamaCare
damage. Wall Street Journal, September 2, 2015.
Powell R. Medicare Part B premiums to rise 52% for 7 million. USA
Today, October 9, 2015.
Beck M. 70,000 ways to classify ailments. Wall Street Journal, September
28, 2015.
Garrett RT. Expertise, if not remedies. Dallas Morning News, September
5, 2015.
Unknown. The new, simpler CPR saves lives. Time, August 3, 2015.
Abegglen LM, Caulin AF, Chan A, Lee K, Robinson R, Campbell MS,
Kiso WK, Schmitt DL, Waddell PJ, Bhaskara S, Jensen ST, Maley CC,
Schiffman JD. Potential mechanisms for cancer resistance in elephants
and comparative cellular response to DNA damage in humans. JAMA
2015;314(17):1850–1860.
Szabo L. Elephants carry cancer shield. USA Today, October 9, 2015.
Donlan TG. The end of labor? A robotic economy might do away with
human work. Barron’s, September 7, 2015.
13.
14.
15.
16.
17.
18.
19.
20.
Barrett D. Wanted: decent crime stats. Wall Street Journal, October 9,
2015.
Gomez A. U.S. foreign-born population on pace to break 125-year record.
USA Today, September 28, 2015.
Unknown. As Americans get larger, airline seats keep shrinking. USA
Today, September 23, 2015.
Lv J, Qi L, Yu C, Yang L, Guo Y, Chen Y, Bian Z, Sun D, Du J, Ge P,
Tang Z, Hou W, Li Y, Chen J, Chen Z, Li L; China Kadoorie Biobank
Collaborative Group. Consumption of spicy foods and total and cause
specific mortality: population based cohort study. BMJ 2015;351:h3942.
Graedon G, Graedon T. Some like it hot—and enjoy health benefits.
Dallas Morning News, September 6, 2015.
Haspel T. Down with salad. Dallas Morning News, September 13, 2015.
Action on Sugar. Call for sugar-sweetened soft drink manufacturers to set global sugar reduction targets to help halt worldwide obesity epidemic set to reach 1.12 billion by 2030 [Press
release, October 1, 2015]. Available at http://www.actiononsalt.org.uk/
actiononsugar/Press%20Release%20/164330.html#sthash.j9yZjLBR.
dpufhttp://www.actiononsalt.org.uk/actiononsugar/Press%20Release%20
/164330.html.
Wulf A. The Invention of Nature: Alexander Von Humboldt’s New World.
New York, NY: Alfred A. Knopf, 2015 (473 pp.).
McCullough D. The Greater Journey: Americans in Paris. New York, NY:
Simon & Schuster, 2011 (558 pp.).
AP. Yogi was ‘good-luck’ charm. Dallas Morning News, September 30, 2015.
Serby S. Yogi Berra was an icon with more substance than style. New York
Post, September 30, 2015.
Boswell T. Beloved Yankee truly one of a kind. Dallas Morning News,
September 24, 2015.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Instructions for authors
B
aylor University Medical Center Proceedings welcomes research articles, review articles, case studies, and editorials
from Baylor and non-Baylor authors. Manuscripts containing Baylor data are particularly desired. Send all manuscripts
and editorial correspondence to William C. Roberts, MD, Editor in
Chief, Baylor Scientific Publications Office, 3500 Gaston Avenue, Dallas, Texas 75246; phone: 214-820-9996; fax: 214-820-4064; e-mail:
cynthiao@BaylorHealth.edu.
MANUSCRIPT SUBMISSION
Submit the word processing document by e-mail to cynthiao@
BaylorHealth.edu. Large files may be sent using YouSendIt or SendNow.
Cover letter and attachments: According to journal policies outlined below, list suggested reviewers and discuss potential conflicts
of interest in your cover letter and provide as attachments copies of
institutional review board approval or exemption, written permission
for reprinting tables or figures, copies of any published material that
could be considered duplicative, and release authorization forms for
photographs.
Schedule: The journal operates on a rolling schedule, but in general
authors are encouraged to aim for the following submission deadlines
for each issue: January issue, September 1; April issue, December 1; July
issue, March 1; and October issue, June 1. The editorial office cannot
guarantee that any manuscript submitted by these deadlines will be
published in the specified issue; variables include the peer review and
revision process and the number of articles already accepted.
ARTICLE TYPES
In addition to multipatient studies (original research articles),
Proceedings publishes several other article types.
Case studies: Include an abstract, a single-paragraph introduction,
a case description of 0.5 to 2 double-spaced pages, and a discussion
of 1 to 5 double-spaced pages. Up to 25 references are acceptable
(although many case reports have 5 to 10). The maximum number of
figures and tables (combined) is 6.
Historical studies: Abstracts are recommended. There is no word
limit, but most historical studies are 1500 to 3500 words.
Editorials: There is no word limit, but most editorials are 800
to 1600 words.
Book reviews: See past issues for format. There is no word limit,
but most book reviews are 800 to 1600 words.
Avocations: Submit an image file for your painting or photograph
or a discussion of your hobby for a maximum of 300 words.
Reader comments (letters to the editor): Both responses to
previously published material and brief reports or observations are
considered for this section. The limit is 1200 words.
MANUSCRIPT PREPARATION
Format: Type manuscripts double spaced, leaving 1-inch margins.
Number all pages, including the title page. Indent paragraphs. Start the
Proc (Bayl Univ Med Cent) 2016;29(1):115–116
first paragraph of the text and the beginning of the reference section
on a new page and place figures on separate pages.
Title page: Include on the first page the article’s title; the authors’
names, highest degree(s), and affiliations; and the name, address, e-mail
address, and phone number of the corresponding author. Acknowledge
any grant support.
Abstract: Provide a one-paragraph double-spaced abstract of
150 to 250 words. Abstracts are required for original articles and
case studies and are recommended for reviews and long historical
articles.
Conclusions: Conclusion paragraphs at the end of the discussion
section are rarely needed and are often cut if included.
References: Number references according to the order in which
they are cited in the text and type them double spaced at the end of
the manuscript. Do not use the footnote or endnote functions of word
processing software. The numbers in the text should be on line and
in parentheses, such as (14, 16, 17). The references should conform
to the following style, listing all authors:
Journal article: O’Shaughnessy J, Osborne C, Pippen JE, Yoffe
M, Patt D, Rocha C, Koo IC, Sherman BM, Bradley C. Iniparib
plus chemotherapy in metastatic triple-negative breast cancer. N
Engl J Med 2011;364(3):205–214.
Book chapter: Ramsay M. Liver transplantation and portopulmonary hypertension. In Milan Z, ed. Cardiovascular Diseases
and Liver Transplantation. New York: Nova Biomedical Books,
2011:83–97.
Book: Gulati G, Filicko-O’Hara J, Krause JR. Case Studies in
Hematology and Coagulation. Chicago, IL: American Society for
Clinical Pathology Press, 2012.
Authors using Endnote can access Proceedings’ reference style
by downloading an EndNote style file, available at http://www.
baylorhealth.edu/Research/Proceedings/SubmitaManuscript/Pages/
ManuscriptPreparation.aspx. Personal communications and unpublished data should not be used as references; they should be
identified in parentheses in the text.
Tables and figures: Number tables and figures in the order in which
they are discussed in the text. Include call-outs in the text and place the
tables at the end of the document as Word files using the Word table function. Figures can be embedded in the text at the end of the document or
provided as separate files, with legends in the Word file. Provide enough
details in titles, footnotes, and legends so that the tables and figures can be
understood apart from the text. Submit photographs as 350-ppi tiff or jpeg
files. Submit graphs and diagrams as electronic files (EPS format preferred).
Use of color: Authors are asked to pay $100 for each color figure
or table. Generally, color is suggested only when clinically required
(as with certain pathology and radiology images). Avoid using color
when creating charts and graphs. If photographs (such as those in
interviews) are originally in color, they can be converted to black and
white during journal production. Articles that use color are generally
grouped together in the issue to decrease overall printing expenses.
115
Style issues: Use generic names for drugs; capitalize any trade names
when they are used. Limit the number of abbreviations in a manuscript
to five, and do not abbreviate single words, such as intravenous. Spell
out all abbreviations on first usage. Proceedings follows the style guide
of the American Medical Association. As further guidance, prospective
authors are encouraged to consult the “Authors’ submission toolkit” (1)
and an article on medical publishing by the editor in chief (2).
MANUSCRIPT PROCESSING
Peer review: All manuscripts are subject to peer review by editorial
board members or other selected reviewers; however, the final decision
as to which articles are published will be made by the editor in chief. At
the time of manuscript submission, authors are encouraged to suggest
reviewers, within or outside Baylor Scott & White Health, and to list
any reviewers they feel should not be used because of potential bias.
If a manuscript was previously reviewed by another journal, authors
should submit those reviews and clearly indicate any revisions that
have been made. Such manuscripts will receive expedited processing,
since they usually will not be sent out for re-review.
Editing: All manuscripts will be edited for clarity and conformity
to Proceedings’ style. The corresponding author will have the opportunity to review editing either before or at the page proof stage.
Reprints: Authors can order reprints using the form provided
through an e-mail link from the printer. Reprints are delivered approximately 4 weeks after the issue comes out. Authors receive a copy
of the printed journal, and PDF files of articles are freely available to
the authors and the general public.
JOURNAL POLICIES
Duplicate publication: When submitting the manuscript, provide a copy of any published or submitted article that is similar to
what is being submitted to Proceedings, so that the editor can judge
whether the manuscript in question would be a duplicate publication.
Once manuscripts are accepted, authors transfer copyright to Baylor
University Medical Center at Dallas.
Authorship: All authors listed in the manuscript must have participated in the design or analysis of the project. In addition, all authors
must review the final text and be prepared to take public responsibility
for its content.
Ethical treatment of research subjects: For reports of experimental investigations of human or animal subjects, indicate institutional
review board approval or exemption within the manuscript. Authors
should also explain in the Methods section the procedures followed
to obtain informed consent.
Conflict of interest: Grant support for a particular study must be
indicated on the title page. In addition, authors must communicate to
the editor in the cover letter any affiliations that could be perceived as
potential conflicts of interest. Examples include honoraria, educational
grants, participation in speakers’ bureaus, expert testimony, patent
licensing arrangements, consultancies, and stock ownership.
116
Use of protected health information: Authors should not refer
to patients by name or initials or provide other specific identifying
information, such as Social Security number or medical record number.
Authors are further encouraged to avoid including extraneous social
details about patients. Patient authorization forms are required for all
identifying photographs. For a copy of Proceedings’ full privacy policy,
contact the managing editor.
Permissions: Permission is required for reproduction of any material, including figures and tables, that has been published elsewhere.
When submitting manuscripts, provide written documentation that
permission has been obtained or notify the editorial staff of the need
to request permission (providing all necessary source information). For
photographs in which the subject can be recognized, submit release
authorizations at the time of manuscript submission.
For additional information, please contact Cynthia Orticio, managing editor, at 214-820-9996 or cynthiao@BaylorHealth.edu.
1.
2.
Chipperfield L, Citroma L, Clark J, David FS, Neck R, Evangelista
M, Gonzalez J, Groves T, Magan J, Mansa B, Miller C, Mooney LA,
Murphy A, Shelton J, Wilson PD, Weigl A. Authors’ submission toolkit:
a practical guide to getting your research published. Cur Med Res Open
2010;26(8):1967–1982.
Roberts WC. Formulating an answerable question, displaying data, illustrating, writing, reviewing, and editing manuscripts for publication
in medical journals. Am J Cardiol 2012;110(2):290–306.
MANUSCRIPT SUBMISSION CHECKLIST
— The entire manuscript is double-spaced and in one Word file, in
the following order: title page, abstract, text, references, tables,
figures (either figure legends only or figures embedded plus
legends). Page numbers appear on the bottom of each page.
— The title page has required elements: title, authors (with full
names and degrees), affiliations, and address for corresponding author.
— A single-paragraph abstract of 150 to 250 words is included.
— For case studies: After the abstract, the manuscript includes
a single-paragraph introduction, a case discussion of 0.5 to
2 double-spaced pages, and a discussion of 0.5 to 5 doublespaced pages. The manuscript does not exceed the limit of
25 references or 6 figures and tables.
— Figures are high-resolution. Photographs are 350-ppi tiff or
jpeg files.
— References include all authors, the full article title, the journal
abbreviation from Index Medicus, the volume and issue number,
and inclusive page numbers. References in the text appear in
parentheses, rather than in superscript or footnotes or endnotes.
— All authors have approved the version to be submitted.
Manuscripts that do not meet these requirements may be returned to
authors before peer review is initiated.
Baylor University Medical Center Proceedings
Volume 29, Number 1
Volume 29
Number 1
January 2016
The peer-reviewed journal of Baylor Scott & White Health
Scott & White Hospital -Brenham
McLane Children’s Scott & White Hospital - Temple
Baylor Medical Center at McKinney
Metroplex Health System - Killeen
Baylor All Saints Medical Center at Fort Worth
Baylor Scott & White Hospital - Hillcrest
Baylor Regional Medical Center at Grapevine
Baylor University Medical Center Proceedings
Baylor University Medical Center at Dallas
Volume 29, Number 1 • January 2016
Pages 1–116
www.BaylorScottandWhite.com
The largest not-for-profit health care system in Texas,
and one of the largest in the United States, Baylor Scott
& White Health was born from the 2013 combination of
Baylor Health Care System and Scott & White Healthcare.
For more information on our 43 hospitals and more than
500 patient care sites, please visit www.BaylorHealth.com
and www.sw.org.
Original Research
3 Meta-analysis of the effect of proton pump inhibitors on
obstructive sleep apnea symptoms and indices in patients with
gastroesophageal reflux disease by S. Rassameehiran et al
7 Serum hyperchloremia as a risk factor for acute kidney injury
in patients with ST-segment elevation myocardial infarction
undergoing percutaneous coronary intervention by N. Patel et al
12 Frequency of fluid overload and usefulness of bioimpedance in
patients requiring intensive care for sepsis syndromes
by T. R. Larson et al
16 Surgical management of carotid body tumors: a 15-year
single institution experience employing an interdisciplinary
approach by J. L. Dixon et al
21 Surgeons’ perspective of a newly initiated electronic medical
record by R. Frazee and H. T. Papaconstantinou
23 Invited commmentary by C. Couch
24 Abstracts from the 10th annual Baylor Scott & White Department
of Surgery Research Day by H. T. Papaconstantinou et al
Case Studies
30 Superior mesenteric artery–duodenal fistula secondary to a
gunshot wound by C. M. Fielding et al
33 Removal of an embedded crochet needle in the mouth
by V. Klovenski et al
36 Bilateral cavernous sinus and superior ophthalmic vein
thrombosis in the setting of facial cellulitis by A. Syed et al
39 Coccidioidomycosis with diffuse miliary pneumonia
by D. Sotello et al
42 Choriocarcinoma presenting with thyrotoxicosis by D. Sotello et al
44 Kidney stones and crushed bones secondary to
hyperparathyroidism by K. P. Sreelesh et al
46 Successful treatment of aspargase-induced acute hepatotoxicity
with vitamin B complex and L-carnitine by G. Lu et al
48 Recurrent lumbosacral herpes simplex virus infection
by J. M. Vassantachart et al
50 Disseminated cutaneous histoplasmosis in newly diagnosed HIV
by G. M. Soza et al
52 Disseminated Kaposi sarcoma with osseous metastases in an
HIV-positive patient by B. M. Bell Jr. et al
55 A giant splenic hydatid cyst by R. Singal et al
58 Segmental ischemia in testicular torsion by B. Tavaslı et al
60 Warfarin-induced skin necrosis following heparin-induced
thrombocytopenia by B. Fawaz et al
62 Metastatic thymoma involving the bone marrow
by M. Dekmezian et al
65 Mullerian adenosarcoma of the cervix with heterologous elements
and sarcomatous overgrowth by V. Podduturi and K. R. Pinto
68 Neuroendocrine carcinoma of the prostate gland by P. Hoof et al
70 Seronegative neuromyelitis optica after cardiac transplantation
by E. Kim et al
73 Successful heart transplantation using a donor heart afflicted by
takotsubo cardiomyopathy by Y. Ravi et al
75 Invited commentary: Using “broken hearts” for cardiac
transplantation: a risky venture or fruitful endeavor? by B. Lima
76 Utility of indium-111 octreotide to identify a cardiac metastasis
of a carcinoid neoplasm by M. Farooqui et al
79 Angiosarcoma of the right atrium presenting as hemoptysis
by C. H. Choi et al
81 Rupture of a left internal mammary artery during
cardiopulmonary resuscitation by C. Patel et al
82 High-intensity cardiac rehabilitation training of a commercial
pilot who, after percutaneous coronary intervention, wanted to
continue participating in a rigorous strength and conditioning
program by S. Shrestha et al
85 Electrocardiogram read by the computer as arm-lead reversal
by D. L. Glancy et al
Historical Articles
91 John M. T. Finney: distinguished surgeon and Oslerphile by M. J. Stone
94 Reflections of Churchill’s personal cardiologist by J. D. Cantwell
Editorials
97 An alternative approach to prescribing sternal precautions after
median sternotomy, “Keep Your Move in the Tube” by J. Adams et al
101 Delivering bad news to patients by K. R. Monden et al
103 Cool it by A. Weisse
From the Editor
106 Facts and ideas from anywhere by W. C. Roberts
Miscellany
2
38
41
59
80
84
Clinical research studies enrolling patients
Avocations: Poem by A. Khan
Acknowledgment of reviewers for BUMC Proceedings, volume 28
Avocations: Photograph by G. Dimijian
Avocations: Photograph by R. Solis
Reader comments: Healthcare professionals should separate their
personal and professional social media by S. A. Ñamendys-Silva
86 Baylor news
105 In memoriam
115 Instructions for authors
www.BaylorHealth.edu/Proceedings
Indexed in PubMed, with full text available through PubMed Central