Office of Human Research - Memorial Healthcare System
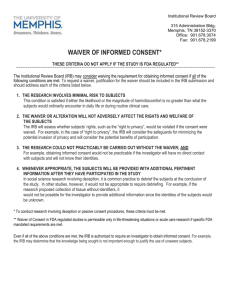
advertisement

Office of Human Research The Office of Human Research at Memorial Healthcare System was founded in September 2011 in order to centralize the research performed at MHS and to provide the infrastructure to conduct the research safely and efficiently. Our vision is to offer a research study to any patient that walks through our doors and to support and enable any physician who wants to perform research at MHS. The goal of the Office of Human Research (OHR) is to provide a strong foundation to enable and enhance human research at Memorial Healthcare System. By providing educational and informational support, the OHR strengthens the advancement of patient and community healthcare by ensuring high quality, ethical, cost effective, research at the highest level of research participant safety. This manual provides guidelines for safe, effective, and efficient conduct of clinical research, with attention to compliance with all relevant regulations and Good Clinical Practice guidelines. It has been compiled to assist investigators, coordinators, and other research team members throughout the course of a research project – from study inception to study close-out. Chapter 1: Introduction Page 1 of 17 Office of Human Research Abbreviations ACRP Association of Clinical Research Professionals ADE Adverse Drug Experience ADR Adverse Drug Reaction AE Adverse Event CBER Center for Biologics Evaluation and Research CDER Center for Drug Evaluation and Research CFR Code of Federal Regulations CRA Clinical Research Associate CRC Clinical Research Coordinator ICH International Conference on Harmonization IDE Investigational Device Exemption IEC Independent Ethics Committee IND Investigational New Drug (application) IRB Institutional Review Board/ Independent Review Board IVRS Interactive Voice Response System/Service NDA New Drug Application NIH National Institutes of Health CRF Case Report Form OHRP Office for Human Research Protections CRO Contract Research Organization PHI Protected Health Information DCF Data Clarification Form PI Principal Investigator DHHS Department of Health and Human PMA Premarket Application Services PMN Premarket Notification [510(k)] DIA Drug Information Association PMS Postmarketing Surveillance DSMB Data and Safety Monitoring Board QA Quality Assurance EC Ethics Committee QI Quality Initiative eCRF electronic Case Report Form QOL Quality of Life EDC Electronic Data Capture RCT Randomized Controlled Trial FDA Food and Drug Administration SAE Serious Adverse Event FWA Federalwide Assurance SMO Site Management Organization GCP Good Clinical Practice(s) SoCRA Society of Clinical Research Associates GLP Good Laboratory Practice(s) GMP Good Manufacturing Practice(s) HIPAA Health Insurance Portability and SOP Standard Operating Procedure WMA World Medical Association Accountability Act Chapter 1: Introduction Page 2 of 17 Office of Human Research Chapter 1: Introduction 1. Defining Clinical Research This manual was written for researchers who work with human subjects. Human subject research encompasses a diverse array of activities, such as epidemiological studies, evaluations of therapeutic interventions, behavioral investigations, translational research etc. Human Research is defined as any activity that: • Meets the Department of Health and Human Services (DHHS) definition of “Research” and involves one or more “Human Subjects” as defined by DHHS regulations Or • Meets the Food and Drug Administration (FDA) definition of “Research” and involves one or more “Human Subjects” as defined by FDA regulations 1.1 Health and Human Services Definitions Research 45 CFR 46.102(d) defines research as a systematic investigation, including research development, and testing and evaluation, designed to develop or contribute to generalizable knowledge. Human Subject 45 CFR 102(f) defines a human subject as an individual about whom an investigator conducting research obtains data through intervention or interaction with individual and identifiable private information. Intervention or Interaction includes physical procedures performed on an individual, manipulation, communication, or interpersonal contact with an individual or manipulation of an individual’s environment Private information includes information that an individual can reasonable expect will not be made public, and information about behavior that an individual can reasonably expect will not be observed or recorded. Identifiable means that the identity of the individual is or may be readily ascertained by the investigator or associated with the information. 1.2 Food and Drug Administration Definitions Research 21 CFR 50.3(c) defines research as an experiment that involves a test article and one or more human subjects that is subject to IND or IDE regulations or which collects data to be submitted to or held for inspection by FDA. Research is subject to the IND regulations when it involves any use of a drug except the use of a marketed drug in the course of medical practice (21 CFR §312.3). Chapter 1: Introduction Page 3 of 17 Office of Human Research Human Subject 21 CFR 50.3(e) defines human subject as an individual who is or becomes a participant in research, either as a recipient of a test article or as a control. In the case of research involving a medical device, a human subject also includes an individual on whose specimen a medical device is used. Test Article 21 CFR 50.3 (j) defines test article as any drug (including a biological product) for human use, medical device for human use, human food additive, color, adaptive, electronic product, or any other article subject to regulation under the jurisdiction of the FDA. The Institutional Review Board (IRB) may provide additional guidance on determining whether or not an activity meets the definition of human research. 2. Research Roles This section contains information regarding the roles and responsibilities that each position will have for the conduct and management of a research study. 2.1 Principal Investigator (PI) The Principal Investigator (PI) conducts the investigation and is responsible for the study at his/her site. The PI is responsible for following federal regulations and meeting Good Clinical Practice (GCP) standards. The PI is ultimately responsible for the conduct of the study, and is held accountable for his/her study team. The PI’s responsibilities include the following: • • • • • • • • • Ensure self and staff are qualified to conduct research Have adequate resources Comply with the protocol Ensure that Informed Consent is obtained in the appropriate manner Provide medical care and follow-up to subjects Notify IRB and Sponsor of safety information Communicate with the IRB and study Sponsor Manage and maintain subject data Inventory and dispense investigational product Please refer to “Guidance for Industry: Investigator Responsibilities” to learn more (FDA Guidance for Industry: Investigator Responsibilities) 2.2 Sponsor The Sponsor is an individual, company, or organization who takes the responsibility for the initiation, administration, and management of an investigation. A Sponsor is responsible for assuring that the study is conducted in accordance with federal regulations and GCP standards. Chapter 1: Introduction Page 4 of 17 Office of Human Research The Sponsor’s responsibilities include the following: • • • • • • • • • • • Design research project Define and allocate study-related duties Provide finances Select and train qualified investigators Assure protocol adherence by principal investigators Monitor quality assurance and quality control Confirm IRB approval Notify regulatory authorities and study sites of safety information Manage and maintain study data Submit and maintain Investigational New Drug (IND) or Investigational Device Exemption (IDE) applications to the FDA Oversee manufacturing, packaging, labeling, and handling of investigational agents Please refer to General Responsibilities of Sponsors to learn more (Sponsor Responsibilities) A Sponsor-Investigator is an individual who would hold the same responsibilities as the Sponsor in terms of upholding federal regulations and GCP standards, as well as those of a PI, for study conduct at a site level. Sponsor-Investigators’ protocols are often referred to as Investigator-initiated research. 2.3 Institutional Review Board (IRB) The IRB is an independent group (either within MHS or external) responsible for ensuring adequate protection of the rights and safety of human subjects. The IRB encompasses national, local, and community ethical standards. A research project cannot be implemented without IRB approval. The IRB’s responsibilities include the following: • • • • • • • • Protect the rights and welfare of human research subjects Review new and ongoing research Obtain/maintain applicable regulatory documents Review qualifications of investigators Determine that research adequately addresses the ethical concerns Determine that research meets regulatory requirements Develop and evaluate institutional policies Educate investigators and the community 2.4 Clinical Research Coordinator/Clinical Research Nurse The Clinical Research Coordinator (CRC) or Clinical Research Nurse (CRN) is an individual who assists the PI with the conduct of the study by overseeing day-to-day Chapter 1: Introduction Page 5 of 17 Office of Human Research responsibilities of the study. The CRC helps ensure that the study is conducted in accordance with federal regulations and GCP standards. Typically, a nurse specific to the area of research under study fills this position. The CRC’s responsibilities include the following: • • • • • • • • • • • • Organize and maintain regulatory documentation Recruit subjects Participate in the informed consent process Conduct assessment and collect medical history Coordinate study procedures and follow-up visits Monitor patient care, assess patient status, monitor treatment effects Serve as a liaison for subjects, investigators, IRB, sponsor, and other health care providers Coordinate activities in team in caring for patients Maintain investigational drug/device accountability Provide oversight of administration of medicines, study drugs, study interventions Capture and report study data Collect information on adverse events 2.5 Clinical Research Assistant (CRA) A Clinical Research Assistant typically assists the CRC or CRN in performing routine administrative activities. A CRA’s responsibilities may include: • • • • • • • Assist in organizing and maintaining all documentation, case report forms and study binders Assist in obtaining appropriate signatures for regulatory forms Assist in preparation of documents needed for initiation, monitoring, and closeout visits with sponsors and or clinical research organizations (CRO) Assist in preparation and submission of regulatory documents (including continuing review, amendments, and adverse event reporting) to the IRB Maintain telephone follow-up with study patients Screen for potential patients for research studies, in collaboration with the PI, CRC or CRN Processing and shipping of blood, urine, serum, and other specimens for clinical trials 3. Regulations and Ethical Considerations 3.1 Federal Regulations Clinical research is regulated by several federal agencies and must adhere to the respective Code of Federal Regulations (CFR). The key regulations for human subject research are: Chapter 1: Introduction Page 6 of 17 Office of Human Research 45 CFR 46 (Office of Human Research Protections – OHRP) (45 CFR 46) The Office of Human Research Protections (OHRP) is the federal agency with primary responsibility for the oversight of Institutional Review Boards (IRB) and for ensuring compliance with the DHHS regulations (45 CFR 46). The OHRP grants the IRBs the authority to review and approve research through a Federal-wide Assurance. All research at MHS requiring IRB approval must, therefore, adhere to the 45 CFR 46 regulations. These regulations are divided into 4 subparts: • Subpart A – Basic HHS Policy for Protection of Human Research Subjects (IRB membership, function, operation & Informed consent requirements) • Subpart B – Additional protections for Pregnant Women, Human Fetuses, and Neonates • Subpart C - Additional Protections Pertaining to Biomedical and Behavioral Research Involving Prisoners as Subjects • Subpart D - Additional Protections for Children Involved as Subjects in Research 21 CFR (Food & Drug Administration – FDA) (21 CFR) The FDA is the federal agency responsible for the review of research data on drugs and devices. FDA regulations exist for the protection of human subjects and apply to any studies that involve FDA-regulated products. The research-specific FDA regulations include the following sections of the 21 CFR, and are collectively referred to as “GCP Regulations”: • Part 11 – Electronic Records; Electronic Signatures • Part 50 – Protection of Human Subjects • Part 54 – Financial Disclosure by Clinical Investigators • Part 56 – Institutional Review Boards • Part 312 – Investigational New Drug Application • Part 314 – Applications for FDA Approval to Market a New Drug • Part 601 – Licensing • Part 812 – Investigational Device Exemptions • Part 814 – Premarket Approval of Medical Devices 45 CFR 160 & 164 (Office of Civil Rights – OCR) (45 CFR 160 & 164) Otherwise known as HIPAA regulations, 45 CFR 160 & 164 provide for the privacy of patients and clinical research subjects. These regulations include restrictions for the collection, use, and disclosure of protected health information. Chapter 1: Introduction Page 7 of 17 Office of Human Research The Office of Human Research Protections has developed a comprehensive listing of laws, regulations, and guidelines that govern human subjects’ research in many countries around the world. This document can be downloaded from the OHRP website at: International Compilation of Human Research Protections 4. Federal Agency Oversight The nature of the study determines which federal agency will be involved. The study may need to be submitted to and approved by any of the following agencies. 4.1 Food and Drug Administration (FDA) If the study involves the use of an FDA-regulated product, the investigator may be required to notify the FDA of the study. The investigator may also be required to notify the FDA if the study involves any investigational agent to potentially cure, treat, diagnose, prevent, or mitigate a disease, or otherwise affect a body structure or function. The FDA uses two processes to ensure the protection of human subjects; if the safety of the product under investigation is not known, the FDA may require the submission of an application known as an Investigational New Drug (IND) application, or an Investigational Device Exemption (IDE). These applications provide the FDA with evidence that the investigational product is reasonably safe for human research. Although the FDA is primarily a regulatory agency, it also serves as a funding agency for an extremely small number of research projects. 4.2 Department of Health and Human Services (DHHS) If the institution is engaged in human subjects research (not otherwise exempt, and is supported by HHS), the institution must have an Office for Human Research Protectionsapproved assurance of compliance with the HHS regulations for the protection of human subjects. Protection of Human Subjects (Office for Human Research Protections, HHS) 45 CFR 46 – text of the federal regulation Policy Guidance (Office for Human Research Protections, HHS) Arranged by topic Office for Human Research Protections (HHS) Home page provides links to all aspects of the human research protections topic, including registration of an Institutional Review Board (IRB) or Independent Ethics Committee (IEC). 4.3 National Institutes of Health (NIH) To obtain funding from NIH, researchers must submit their grant for scientific review. Funding is based upon the quality and importance of the research. Chapter 1: Introduction Page 8 of 17 Office of Human Research 5. Ethical Considerations Ethical considerations play a crucial role in conceptualizing, evaluating, and designing clinical research studies. Past ethical violations have led to many of the current regulations, guidelines and safeguards. Several important documents exist to provide guidance on ethics in research: • Declaration of Helsinki - WMA Declaration of Helsinki • Belmont Report - NIH Belmont Report The Belmont Report describes three basic ethical principles that should underlie human research: 1. Respect for Persons – Respect centers upon two primary ethical convictions: individuals are characterized as autonomous with respect to the decision to participate in research, and individuals with diminished mental capacity are dependent upon others to act on their behalf when deciding to participate in research. Respect for persons imposes that participation is both voluntary and informed, and that privacy should be protected. Elements to consider: • • • Informed Consent Privacy and Confidentiality Protection of Vulnerable Subjects 2. Beneficence – Beneficence is an obligation to make every effort to secure a subject’s well-being during research participation. Two concepts express the complementary convictions of beneficence: (1) do no harm, and (2) maximize the possible benefits and minimize the possible harms. Elements to consider: • • • • Risk-to-Benefit Ratio Research Design (to minimize risks) Investigator Qualifications Conflicts of Interest 3. Justice – The concept of justice embodies an obligation to ensure that those bearing the risks of the research study are selected fairly (i.e. are representative of the reference population and not chosen simply because of their easy availability for research), and are likely to have access to any benefit derived from the research. Elements to consider: • • Balance of Burdens/Benefits Population of Inference Chapter 1: Introduction Page 9 of 17 Office of Human Research • • Eligibility Criteria Representative of Population Equitable Recruitment Methods 6. Vulnerable Populations Some populations are considered vulnerable and deserving of additional research protections. Vulnerable subjects are individuals who may be unduly influenced by the expectation, whether or not justified, of the benefits of participation, or from fear of retaliation from refusal to participate. There are specific federal regulations designed to provide additional protection for pregnant women/fetuses/neonates (45 CFR 46 Subpart B), prisoners (45 CFR 46 Subpart C), and children (45 CFR 46 Subpart D). Other examples of vulnerable populations may include patients with incurable diseases, subjects who are cognitively impaired, and employees or students of researchers. Research in vulnerable populations can usually take place if they represent the appropriate target population and the risks are minimized. However, the IRB often requires additional safeguards to prevent coercion and to protect the integrity of the informed consent process. Please refer to the website for more information on vulnerable populations - Research Involving Subjects with Questionable Capacity to Consent 6.1 Children/Minors Federal regulations define “children” as persons who have not attained the legal age for consent to treatments or procedures involved in the research, under the applicable law of the jurisdiction in which the research will be conducted. In Florida, the legal age of consent is 18 years of age. All under the age of 18 are considered children or minors. Note the following exceptions: Emancipated Minors - In Florida, the following categories of children are legally authorized to consent to participation in research on their own behalf: • Children who have had the "disability of nonage"(e.g. considered a child) removed by a circuit court. (See Chapter 743, Florida Statutes). • Children who are married or have been married may consent to medical care and treatment, including participation in experimental procedures. • An unwed pregnant child may consent to the performance of medical or surgical care of services relating to her pregnancy by a hospital or clinic or by a licensed physician. This category includes research relating to her pregnancy. Except for emancipated minors, the IRB will not approve the enrollment in research of persons under the age of 18 without parental permission unless the investigator can demonstrate that enrollment is permissible under and consistent with Florida law and meets the requirements set forth in 45 CFR 46, Subpart D and 21 CFR 50 Subpart D. Individuals who are defined as “children” will be afforded the protections under the regulations that protect children involved as subjects in research (Subpart D, 45 CFR 46.401 - 409 and 21 CFR 50.50 - 54). Additionally, the IRB may determine that minors Chapter 1: Introduction Page 10 of 17 Office of Human Research who are not children (such as a person meeting one of the exceptions noted above) are potentially vulnerable, at which point the IRB might apply additional protections. Research involving children must fit into one of four categories: 1. Research not involving greater than minimal risk. 2. Research involving greater than minimal risk, but presenting the prospect of direct benefit to an individual participant. 3. Research involving greater than minimal risk with no prospect of direct benefit, but likely to yield generalizable knowledge. 4. Research that is not otherwise approvable, but which presents an opportunity to understand, prevent, or alleviate a serious problem affecting the health or welfare of children...(and) the research will be conducted in accordance with sound ethical principles. With children, emotional and psychological risks are given more consideration than normally given to adult subjects. If possible, research involving greater than minimal risk should be conducted first in adults and then in mature minors before young children are involved. Consent is obtained from a parent or guardian and assent is obtained from the child. 6.2 Limited Decision-Making Capacity Decisionally impaired adults are individuals who have a diminished capacity for judgment and reasoning due to a psychiatric, organic, developmental, or other disorder that affects cognitive or emotional functions. Other individuals may be considered decisionally impaired or have limited decision-making ability because they are under the influence of or dependent on drugs or alcohol, suffering from degenerative diseases affecting the brain, are terminally ill, or have severely disabling physical handicaps. There are no universal criteria for determining competence. If competence is in question, the subject’s decision-making capacity should be assessed in a manner appropriate for that population. The IRB takes special care to consider issues such as the selection of participants, privacy and confidentiality, coercion and undue influence, and risk-benefit analysis. Decisions should be made with the utmost deference to the ethical principles underlying human research as set forth in the Belmont Report. When designing a study that includes subjects with limited decision-making capacity, the investigator should outline how the assessment process will be used to tailor informed consent. It is suggested that consultation or collaboration be sought from departments experienced in dealing with cognitive capacity issues in the population being studied. The following criteria should be taken into consideration for adult participants with impaired decision-making capacity involved in a research protocol: • The objectives of the research cannot be met by conducting the research in a population that does not have the disorder that may affect decision making capacity. Chapter 1: Introduction Page 11 of 17 Office of Human Research • The research is designed for a disease or condition relevant to the vulnerable population under study. • The research is either minimal risk, more than minimal risk with a prospect of direct benefit, or more than minimal risk without a prospect of direct benefit, but of vital importance to the vulnerable population. • Adequate provisions are made for obtaining consent from the participant’s legally authorized representative. • Adequate provisions are made for obtaining assent from the participant, unless the IRB determines that assent is not appropriate as a condition of participation or that some or all participants are not capable of providing assent. • The protocol must describe when and how the participants will be assessed for capacity for formal consent or assent and understanding of the proposed research, and the process for a second confirming assessment. Competency should be evaluated on an individual basis to avoid incorrect assumptions as to an individual’s ability to make decisions. Criteria for determining competence might vary according to the degree of risk or discomfort presented by the research procedures and the extent to which therapeutic gain can be anticipated. • The IRB will consider additional safeguards to protect participants. These include: o Requiring the involvement of participant advocates o Requiring independent monitoring o Requiring waiting periods o Appointing a monitor to supervise the informed consent process IRB decisions may be based on the amount of risk involved in the research and the likelihood that participants will derive health benefits from their participation. 6.3 Pregnant Women, Fetuses, and Neonates Pregnancy is the condition from conception to delivery, a fetus is the product of conception from implantation until the time of delivery, and a neonate is a newborn up to 28 days. Researchers studying women, fetuses, and neonates must not have any input in the decisions as to the timing, method, or procedures used to terminate a pregnancy or in determining the viability of a neonate. Pregnant Women/Fetuses Before approving research involving pregnant women, the following conditions must be present: • Where appropriate, preclinical and clinical studies (studies on pregnant animals and non-pregnant women) have been conducted to assess potential risks. • The research must fit into one of two categories: Chapter 1: Introduction Page 12 of 17 Office of Human Research o Risks are acceptable and the research offers the prospect of direct benefit to the pregnant woman, the fetus, or both. o Risks are minimal and the research purpose is to obtain knowledge that cannot be obtained by any other means. • No inducements will be offered to terminate a pregnancy. • Informed consent will be obtained from: o Only the pregnant woman: if there is possibility of direct benefit to the pregnant woman -or- benefit both the pregnant woman and the fetus -orthe risk to fetus is minimal. o Both the pregnant woman and the father: if the only potential benefit is to the fetus (unless the father is unavailable, incompetent, temporarily incapacitated, or the pregnancy is a result of rape or incest). Neonates of Uncertain Viability Before approving research involving neonates of uncertain viability, the following conditions must be present: • Where appropriate, preclinical and clinical studies have been conducted to assess potential risks to neonates. • The research must fit into one of two categories: • o Risks are minimized and the research has the potential to enhance the probability of the neonate's survival to the point of viability. o Research involves no additional risks and the purpose is to obtain knowledge that cannot be obtained by any other means. Informed consent will be obtained from: o Either parent - If neither parent is able to consent because of unavailability, incompetence, or temporary incapacity, informed consent can be obtained from either parent's legally authorized representative. Nonviable Neonates Before approving research involving nonviable neonates, ALL of the following conditions must be present: • The research will not artificially maintain vital functions. • The research will not terminate the heartbeat or respiration. • The research must fit into one of two categories: o Risks are minimized and the research has the potential to enhance the probability of the neonate's survival to the point of viability. o Research involves no additional risks and the purpose is to obtain knowledge that cannot be obtained by any other means. Chapter 1: Introduction Page 13 of 17 Office of Human Research • Informed consent will be obtained from: o Both parents - If one parent is unable to consent because of unavailability, incompetence, or temporary incapacity, informed consent can be obtained from only one parent. If the pregnancy is a result of rape or incest only the mother's consent is necessary. 6.4 Prisoners A prisoner is any individual involuntarily confined or detained in a penal institution. Persons under house arrest and persons court-ordered to residential treatment facilities are considered prisoners. Prisoners may only be used for research that is material to their lives as prisoners or offers the prospect of therapeutic benefits. An IRB reviewing this type of research must be specifically constituted to include at least one member who has the appropriate background to serve as a prisoner representative. The benefits and selection criteria of the research project must be carefully examined. Incentives that would not entice non-prisoners could be coercive to this population due to the limited choices available. Assurances should be established to prevent research participation from influencing parole. Likewise, the selection criteria should be fair and equitable. Subject selection criteria should not be subject to influence by prisoners or prison authorities. For DHHS-supported research involving prisoners, the Office of Human Research Protection (OHRP) must also be involved prior to implementation of the project. 7. Risk to Subjects Risk is the likelihood of harm occurring to research subjects. Risk can be social, psychological, or physical. The amount of risk involved with a study will determine: • What level of IRB (Institutional Review Board) review (Expedited vs. Full) is required • Whether the study qualifies for a waiver of consent or HIPAA Authorization • How much oversight and safety monitoring is needed An IRB uses the following categorizations to assess the level of risk. 7.1 Minimal Risk Eligible for Expedited IRB Review Probability and magnitude of harm/discomfort no greater than daily life or routine physical/psychological exams. Examples • • • • Survey research Venipuncture Taste and observation studies Contrast MRI studies Chapter 1: Introduction Page 14 of 17 Office of Human Research • Non-invasive procedures 7.2 Minimal Risk NOT Eligible for Expedited IRB Review Generally includes studies that normally would be considered minimal risk, but involve: • • • • • • DEXA scans Collection of >550mL of blood in an 8 week period or more than 2 venipunctures within a 2-week period in healthy subjects Phase IV studies Biopsies Catheter placement Contrast MRI studies 7.3 Greater than Minimal Risk Examples: • • • • • • • • HIV/AIDS and Hepatitis C studies Most Phase III studies Some studies that include a "washout" period or placebo use in an otherwise treatable disease Investigational drug/device utilizing invasive procedures Phase I studies of new chemical entities or class of test article having unknown expectations of toxicity Gene transfer research Emergency studies with waiver of informed consent Xenotransplantation The IRB will consider the following in determination of the risk level: • • • • • • That the risks to participants are minimized as much as possible That the risks are reasonable in relation to the anticipated benefits The adequacy of the informed consent process and documentation Where appropriate, that the protocol contains provisions for monitoring Where appropriate, that there are adequate provisions to protect the privacy of subjects and confidentiality of data Where appropriate, that there are additional safeguards in place to protect vulnerable populations 8. Conflict of Interest The conduct of clinical research often goes hand-in-hand with commercialization ventures and involvement with companies with financial interests in the outcomes of the research. As per the Memorial Healthcare System policy on Conflict of Interest, “… the institution has the responsibility for maintaining objectivity in research by ensuring that the design, conduct, or reporting of research will not be biased by any Chapter 1: Introduction Page 15 of 17 Office of Human Research conflicting financial interest of investigators responsible for the research in accordance with PHS 42 CFR part 50” The conduct of clinical research must always be insulated from potential conflicts of interest that might be perceived to influence its conduct or outcome. Conflict of interest issues applies to anyone responsible for the design, conduct or reporting of research. At MHS, the Office of Human Research (OHR) is responsible for research integrity, which includes the management of conflict of interest in research. The OHR offers a comprehensive collection of MHS policies and guidelines, federal policies and guidelines, and other resources. This office, in accordance with federal regulations, also administers the Conflict of Interest Committee (CIC), requires financial disclosure by investigators, and enforces conflict of interest management mechanisms and sanctions. 8.1 Types of Conflict Several types of conflicts of interest exist: Conflict of Research Integrity Investigators should maintain the highest level of scientific integrity in the conduct of research. The complete, objective, and timely dissemination of new findings through publications and presentations is essential for research integrity. Conflict of Financial Interest In general, this concept refers to an investigator in a relationship with a commercial entity with financial interests in the company. In the context of clinical trials, this policy defines the triggers that constitute a Significant Financial Interest as well as the mechanisms for disclosing and managing such interests. Definition The following triggers of a Significant Financial Interest apply to the researcher, his/her spouse and dependent children, and any corporation, foundation, trust or other entity controlled or directed by the investigator or his/her spouse. Significant Equity Interest • • Owning a significant equity interest of any company or entity that sponsors or supports the clinical trial during the time of study and for 1 year following completion of the study. Significant equity interest includes: o Any ownership, stock options, or other financial interest which cannot be readily determined through reference to public prices (generally, interests in a non-publicly traded corporation) o Equity Interest in a publicly traded corporation that exceeds $10,000 (or exceeds 5% ownership) Excluded is interest in any publicly traded diversified mutual fund. Proprietary Interest • Owning a proprietary interest in the tested product. Proprietary interest is property or other financial interest in the product including, but not limited to, a Chapter 1: Introduction Page 16 of 17 Office of Human Research patent, trademark, copyright or licensing agreement, or right to receive income in connection with the development or sale of the tested product. Significant Payments • Receiving significant payments from any company or entity that sponsors or supports the clinical trial during the time of the study and for 1 year following completion of the study. • These are payments (e.g., retainers, honoraria, gifts) made by or on behalf of the sponsor of the study that are more than $10,000 per year, exclusive of the costs of conducting the study. • Excluded are payments to a department or school from the sponsor. Service on Board • Serving on the Board of Directors or as an officer with fiduciary responsibility of any company or entity that sponsors or supports the clinical trial. An officer with fiduciary responsibility is someone who is entrusted with the management of property for, or with the power to act on behalf of and for the benefit of, another. Disclosure Whether or not a significant financial interest exists, all investigators conducting clinical trials are required to submit a Financial Disclosure Form. This form is submitted either in connection with a submission of a grant application, or with a submission of a protocol to the Institutional Review Board (IRB) for approval, to the Sponsor, as well as the IRB. The IRB or the Sponsor reviews all disclosures to determine if it appears that the investigator has a Significant Financial Interest as defined above. Following are some examples of conditions or restrictions that might be imposed to manage, reduce, or eliminate actual or potential conflicts of interest: • Public disclosure of Significant Financial Interests • Monitoring of research by independent reviewers • Modification of the research plan • Disqualification from participation in the portion of the funded research that would be affected by the Significant Financial Interests • Divestiture of Significant Financial Interests • Severance of relationships that create actual or potential conflicts Reporting potential undisclosed conflicts of interest Any staff member who is concerned about a potential conflict of interest that may be impacting the study or the safety and welfare of the subjects should first attempt to speak directly to the investigator, informing him/her of the Conflict of Interest policy. If this option is uncomfortable or does not result in a satisfactory resolution, the OHR can be contacted to assist. Chapter 1: Introduction Page 17 of 17 Office of Human Research Chapter: 2 Study Preparation This section of the manual covers those activities that are conducted during the process of preparing a research study, from assessing the feasibility of the research project through protocol and study document development, submission and approval, and initiating the research site. 1. Project Feasibility Assessment When developing a potential research study, there are several aspects that require careful consideration to determine whether or not the project is feasible. This section attempts to outline some of the initial questions that need to be answered early in the study planning stage. This section will expose the researcher to the various areas that need to be assessed: 1.1 Scientific Validity Is there sufficient scientific validity to proceed with the project? Conduct a thorough literature review to evaluate the merit of a proposal with these questions in mind: • Will the project contribute to the field? • Will the project replicate or challenge existing findings in the literature? What type of study will be conducted? A critical step early in the feasibility phase is to determine and clearly define the type of project being considered. The complexity of the project will impact the resources that will be needed. Potential project types include: Least Complex – Case Reports, Retrospective Cohort Studies, Prospective Cohort Study, Analysis of Secular Trends More Complex – Using routine clinical procedures in collaboration among departments, Involving non-standard clinical procedures, Innovative treatment for the purpose of policy change (change in standard of care) Most Complex – Submitting an IND and IDE 1.2 Resource Assessment Is there department/institute/center support? Discuss the project with key persons in the department, center, or institute with the following questions in mind: Chapter 2: Study Preparation Page 1 of 5 Office of Human Research • Is there an experienced mentor, collaborator, or consultant that can be involved in the project? • Is there institutional support from the department director? • Does the study reflect the values and principles of the department and institution? • Is the institution willing to accept responsibility for the level of risk involved? • Are there departmental resources that can be used to support the project? • Who are the key persons and staff who will contribute to the effort? • Do the faculty & staff have the ability and qualifications to carry out the methods and procedures of the project? What is the length of time required to obtain approval of a study? The length of time for approval depends upon several factors including the type of project, the amount of time the investigator and study team can dedicate to preparing the study for approval, whether or not contract negotiation is required, etc. Obtaining approval to commence a study involves more than just the IRB submission. There are multiple processes involved, each with their own time lag. 1.3 Recruitment Potential Are there enough subjects available to complete the project? It is important to ascertain whether or not there exist enough subjects eligible to be enrolled into the research study to achieve the proposed aims. To do this, first identify how many people will meet the study's eligibility criteria. Next, estimate what percentage of the targeted population can be accessed and realistically be expected to participate and use this information to decide whether there are enough subjects to meet the enrollment objectives. Memorial Healthcare System has an extensive network of physicians, hospitals, clinics, treatment centers, and community practices. All of these sites can be viewed as potential sources for research subjects with specific diagnoses. Regardless, investigators must identify methods for recruiting from their targeted audience via medical records review, advertisements, word of mouth, or referrals. 1.4 Financial Feasibility Funding for a study can come from a variety of sources that include federal agencies, pharmaceutical companies, public charities, or foundations. It is important to analyze the financial feasibility to determine whether there is enough funding to support the project. A thorough analysis of financial feasibility can be accomplished by preparing a study cost budget. Chapter 2: Study Preparation Page 2 of 5 Office of Human Research 2. Research Personnel and Staffing 2.1 Recruitment and Selection Sources for Research Staff Recruitment Effective research personnel recruitment requires a clear understanding of the position being filled and related qualifications. The job description must accurately reflect the expectations of the position, required experience, and education. This will ensure that the position is properly graded and that a competitive offer can be made to the final candidate. Successful recruitment requires the manager to understand the area market for the specific position and who else is competing for these same individuals (i.e. pharmaceutical companies, contract research organizations, colleges and universities, temporary agencies), and area salary information (if available). There are many sources for research staff recruitment including national clinical research associations, internet based career sites, area colleges and universities, area newspapers, hospitals, employment agencies. The posting should reflect the essential elements of the job description along with characteristics unique to the position (i.e. fulltime, part-time, temporary, permanent, prior experience in clinical trials, etc.). National Clinical Research Associations: 1. Association of Clinical Research Professionals http://careers.acrpnet.org/ 2. Society of Clinical Research Associates http://www.socra.org/ Key Characteristics & Skills The roles in research are multi-faceted, with a wide range of responsibilities, from patient care to administrative. The following skills are essential for success in research: 1. Organizational skills 2. Ability to multi-task 3. Detail-oriented 4. People-oriented 5. Self-confident 6. Flexible 7. Able to manage time well 8. High energy level 2.2 Retention Strategies Turnover of Clinical Research Coordinators (CRC) presents a costly impact on study operations. A recent Thomson CenterWatch survey of 256 hiring decision makers found that only 56% of Clinical Research Coordinators (CRC) have been in their positions for less than 3 years, and that many CRCs were switching to careers in industry as study monitors (CenterWatch Monthly, July 2004). This trend affects the study site with a loss of productivity, money and time spent training replacements, and an overall less experienced staff. Chapter 2: Study Preparation Page 3 of 5 Office of Human Research The most commonly encountered reasons for the high rate of turnover among CRCs include: • Heavy Workload (>40 hours per week) • Compensation • Personal Life Changes • Competitive hiring by other sites as CRC • Transition from CRC to study monitor in search of higher compensation and flexibility • Lack of recognition and professional respect • Loss of funding on the part of the site Burnout is a commonly reported occurrence among CRCs. Burnout is associated with perceived daily workload, job satisfaction and low endurance and nurturance personality traits. Aside from turnover, burnout can also affect productivity, data quality and subsequently may have a financial impact on the clinical trial. Several strategies are recommended for improving CRC retention and preventing burnout. It is anticipated that implementation of the career paths identified earlier in this section will contribute to improvement of CRC retention by providing a clear path for the CRC and CR Nurse to advance within their profession. Preventing Burnout Respecting a realistic and flexible schedule for CRCs is another critical step toward preventing burnout. It is recommended that CRCs be expected to work no more than 40 hours per week, with the exception of emergency situations. The hours may vary to accommodate patient recruitment and visit needs, but the CRC should not routinely be expected to work beyond 40 hours. Investigators who set these expectations should consider that while the extra hours may reward the investigator with benefits such as professional recognition, tenure, and other opportunities, there are very few such career benefits for the CRC. If the workload is such that extra hours are required for the CRC to accomplish necessary duties, it may be prudent to hire another CRC, or at minimum a Clinical Research Assistant to reduce to burden on the CRC. Professional Recognition The CRC has long been an underappreciated role. Promoting a perception of being appreciated and recognized for their contributions can greatly improve CRC retention. This can be accomplished in several ways: • Supporting membership in professional organizations such as ACRP or SoCRA • Providing continuing education opportunities such as attendance at professional conferences • Supporting pursuit of professional certification • Team Building Strategies Chapter 2: Study Preparation Page 4 of 5 Office of Human Research • Attendance to seminars to build skills • Acknowledgement for good or exceptional work via email, certificates, gift cards 2.3 Education and Training 2.3.1 Required Research Training Collaborative IRB Training Initiative (CITI) Training All personnel engaging in human research must have documented discipline-appropriate training in human research protections. The Collaborative Institutional Training Initiative (CITI) web-based modules satisfy this requirement. The "CITI Protection for Human Subjects Training" course is available in CITI Training Initiative. Create your login and affiliate yourself with MHS/Jo-DiMaggio to take the MHS-prescribed courses. Health Insurance Portability and Accountability Act (HIPAA) Training All research staff having contact with patient information are required to complete HIPAA training. HIPAA regulations include specific rules about how protected health information is used and protected in research. Researchers must complete the HIPAA training offered on the CITI training website. (HIPS) Dangerous Goods Regulations Training The Occupational Safety & Health Administration (OSHA) requires relevant training for employees who work with or ship hazardous substances including: • • Chemicals Human blood, blood products, fluids, and human tissue specimens Through its Dangerous Goods Regulations and a comprehensive and effective training program, the International Air Transport Association (IATA) ensures that shippers, forwarders, and carriers have the tools and resources to ship dangerous goods safely. Before you are allowed to ship these specimens, online training and certification must be obtained. This is done through an invitation from Medialab. Please contact OHR for further details. The Florida Department of Health (DOH) sponsors training for health professionals in “Infectious Substances Packaging and Shipping Training”. Please refer to the Florida DOH website for details and schedules Professional Research Associations The following organizations offer training and certification programs for clinical research. • • • Association of Clinical Research Professionals (ACRP) http://www.acrpnet.org/ Drug Information Association (DIA) http://www.diahome.org/diahome/ Society for Clinical Research Associates (SoCRA) http://www.socra.org/ Chapter 2: Study Preparation Page 5 of 5 Office of Human Research Chapter 3: Grant Writing Grants are written to obtain research funding from federal agencies, private foundations, pharmaceutical companies, etc. Each agency has its own requirements for grant writing. This section will concentrate upon the requirements for the National Institute of Health (NIH). NIH uses activity codes (e.g. R01, R43, etc.) to differentiate the wide variety of research-related programs. A comprehensive listing of different programs and activity codes can be found at Types of Grant Programs Deadlines for new NIH grant applications vary depending on the type of grant. Information on NIH grant deadlines can be found at: Standard Due Dates for Grant Applications New investigators should estimate that the writing process will take between 2-6 months. Applications for NIH research support are made on Grant Application Form PHS 398. NIH also provides Grant Writing information and tutorials, available at: NIH Grant Tutorial. Information regarding about the process can be found at Grants - How to Apply General writing tips include: • Write clearly and concisely • Proofread • Write for technically diverse reviewers • Avoid unnecessary complexity • Collect preliminary data • Follow instructions carefully • Obtain outside opinions Grant Writing Services The Office of Human Research (OHR) can provide assistance with writing and editing large, multidisciplinary proposals, such as program project (P01) and specialized center (P50) grants. The OHR will help ensure: • Integration of distinct projects to create a cohesive proposal • Consistency of style and tone throughout the proposal • Clarity in the presentation of ideas, goals, and strategies • Polished grammar for maximum readability Chapter 3: Grant Writing Page 1 of 13 Office of Human Research 1. Components of an NIH Grant Abstract An abstract is a summary of the grant written for the educated non-specialist. It is a concise description of the background, specific aims, the research methods, and significance. The abstract is used to assign a grant to a study section. Study section members (who are not primary reviewers) will rely heavily on the abstract. The researcher may choose to write the abstract last to ensure the content of the entire proposal is well summarized. Specific Aims The specific aims section is generally a page explaining the long-term goals, the hypothesis, and the specific aims or objectives (Specific Aim #1, Specific Aim #2, Specific Aim #3, etc.). The hypothesis should be clear and focused. The aims should be related. Explain how the specific aims will be used to support the hypothesis. Background/Significance The background/significance section is generally 3 pages describing the problem, current knowledge, remaining questions, and importance of the research. The investigator should provide a balanced review of the literature. Elaborate upon how the knowledge gained from the hypothesis and specific aims will improve the field and/or other related areas. Preliminary Results/Progress Report The preliminary data section is generally 6-8 pages describing what current and prior work has done to support the feasibility of the study. Identify how each of the specific aims in the work has been addressed and interpret the results critically. Demonstrate that the investigator has the experience and capabilities to conduct the proposed project. The investigator may include unrelated studies if they demonstrate his/her competence to perform the experimental techniques. Experimental Design/Methods The research design and methods section is no more than 25 pages (items "a" through "d") providing a concrete explanation of how the study aims will be accomplished. A detailed and technical description of the study procedures and methods should be incorporated. Avoid "shot gun" approaches or fishing expeditions. This section should address potential problems or limitations in the experimental design and, if possible, provide alternatives or solutions. Reference Section The reference section should accurately reflect the citations used throughout the grant. Consortium and/or Consultant Arrangements Describe collaborators at other institutions or other local experts who may be providing support or advice. This should include documentation substantiating their participation. Chapter 3: Grant Writing Page 2 of 13 Office of Human Research The grant application may also include: • A biographical sketch • Budget and justification • A description of other research support • Conflict of interest disclosures • Assurances/regulatory (IRB) approval • A description of resources and environment and letters from the department chair. The grant will be assigned to an Institute or Center (IC) who then sends it to a scientific review group or "study section." The study section will review the grant and assign it a priority score for funding. Please refer to the NIH website for further information regarding the grant application process - Application Guide for NIH Grants 2. Grant Revisions Approximately 40% of the grants reviewed by a study section are resubmissions. Do not be discouraged if you receive a poor priority score and need to resubmit your grant. Identify the problems: • The most common criticisms include: o Grant is poorly written- the plan is unclear, incorrect, or incomplete o Aims cannot be supported- the sample size is inadequate or uncertain o Plan is not well conceptualized- the methods are incomplete o Insufficient expertise- missing talent, usually statistical o Poorly chosen population of inference - poor subject selection, usually controls o Not enough evidence to support the planned response rates- need pilot data o Plan is unfocused- hypothesis is absent or unclear • Ask for advice from experienced researchers • Address the problems o If there are problems with the review (reviewers were not interested, did not have suitable expertise, or were biased), revise, resubmit, and request a new study section Chapter 3: Grant Writing Page 3 of 13 Office of Human Research 3. Research Methods and Statistical Design It is beyond the scope of this manual to provide information on various statistical approaches and models. The following is meant as a high-level overview of the basic elements of study design and clinical research statistics. The researcher's goals influence the size, scope, and direction of the investigation. The intended purpose of biomedical research varies and usually falls along a continuum: Basic research is research to advance scientific knowledge and understanding across a wide variety of areas such as physiology, pathophysiology, chemistry, etc., but is not focused on a specific practical application of that knowledge. Translational research, often called "bench-to-bedside research," focuses on assessing the feasibility of translating basic research findings and knowledge into clinical therapies. The interface between basic research and clinical application includes elements of bench research necessary to support application to human medical care (e.g. biologic mechanism of action, pharmacokinetics, toxicology, etc.) and early stage research in humans. Clinical application/development produces and evaluates materials, devices, systems, or methods as they apply to human healthcare. Clinical trials and certain translational research activities are components of this category. A clinical trial is any investigation involving human subjects intended to identify the clinical, pharmacological or other effects of an investigational product (drug or device) to measure its safety and/or efficacy. The overall objectives of a clinical trial vary with the phase of investigation: • Phase I - first study of a drug in humans, most commonly healthy adults; safety and dose ranging tolerability; basic metabolism or mechanism studies (generally small studies of 20 or less subjects) • Phase II - first study of drug in target populations (patients); safety, dose ranging in patients; preliminary efficacy assessment (generally >100 subjects) • Phase III - larger study to prove efficacy and increase experience with safety (generally large studies ranging from >100 to >1000 subjects ---- Phase III cardiovascular studies have enrolled higher than 40,000 subjects) • Phase IV - post-marketing studies; vary in size; often to provide ongoing safety data. If a researcher is conducting research in human subjects, a clear hypothesis is necessary in order to choose the study design. The study design, in turn, will impact which techniques will be used to minimize bias and how the statistical analysis will be conducted. The involvement of a statistician in the preparation of the statistical plan and analysis is an indispensable part of this. Please contact the OHR for more information. 3.1 Basic Elements of Study Design Once the purpose of the investigation is understood and the hypothesis and objectives have been formulated it is necessary to identify the study design to be used for the project. Chapter 3: Grant Writing Page 4 of 13 Office of Human Research To help determine the appropriate research design: • Identify the condition and outcome of interest. o • Select the type, order and frequency of observations and measurements. o • What methods will be used to obtain data? How, when, and in what order will these observations and measurements occur? Identify the nuisance variables. o • Will manipulation of the variable(s) occur or will observational methods be used? Are there any identifiable sources of variation which can confound the results? Can their impact be minimized or controlled? Identify the population of interest. o What sample size will be needed? How will sampling occur? Is there only one group or will multiple groups be used for comparison? 3.2 Basic Types of Study Design Study designs can be classified into two broad categories: experimental studies and observational studies. Experimental Studies In an experimental study, the selection and allocation or assignment of individuals for the experiment is under the control of the investigator. The controlled conditions help validate a cause-and-effect relationship between the treatment and the outcome within the population enrolled in the study (internal validity). However, it is important to remember that findings from experimental studies do not always accurately reflect findings under real-world conditions (external validity) since there are many factors in the real-world that cannot be fully captured in a carefully controlled experiment (e.g. natural variations in physiology and concomitant diseases or medications, patient compliance with the treatment, etc.). General characteristics that differentiate experimental research designs from each other include the use of a control group, random assignment, and blinding. When used correctly, these characteristics can significantly strengthen the ability to infer cause and effect from experimental research. Control Groups Controls are subjects who are included in an investigation for comparison to the intervention/treatment group. Controls are not given the intervention, or are given a different intervention, or, depending on the type of experiment, do not have the condition, background, or risk factor under investigation. A control group may be enrolled concurrently with the intervention group, may be the same population as the intervention group, or may be studied independently (as an external or historical control). Chapter 3: Grant Writing Page 5 of 13 Office of Human Research Some common examples of control-group designs include: 1. A cross-over design is a type of experimental study where subjects act both as a control and as an actively treated subject. Generally, subjects are enrolled into one treatment group, then after a waiting or wash-out period (i.e. time for the treatment effect to be eliminated or "washed-out"), are enrolled into an alternate treatment group. In this type of design the subjects act as both the comparator group and the active treatment group. This approach reduces the variability in comparing active to treated subjects, but it is susceptible to bias if carry-over effects from the first treatment occur. 2. A parallel groups design is a type of study where different treatment groups are running simultaneously. The parallel-groups approach is susceptible to non-comparability between groups if the subjects are not properly allocated or assigned (i.e. the baseline characteristics may not be equal between the two groups to such a degree that the groups are not truly comparable). o A matched pairs group is a type of parallel study design in which subjects with similar, pre-determined traits are first paired and then randomized into different study arms for comparison. 3. A series group design assesses exposure to the study treatment in phases- one treatment group is completed before beginning the next treatment group. This design is most commonly used in Phase I doseescalations studies as a safety measure, allowing full evaluation of the results from the first treatment group before subjecting another treatment group to the next higher dose. Random Assignment Non-randomized: In a non-randomized investigation, subjects are assigned to a treatment group as they appear for the study or based upon certain characteristics. Randomized: In a randomized investigation, subjects are assigned to treatment groups on the basis of chance. The process of assigning subjects to treatment or intervention groups affects internal validity. The overall goal of randomization is to produce comparable groups across the study. Randomization strengthens the foundation for statistical procedures and, when properly executed in an experimental study, provides the strongest empirical evidence of any study design. The following summarizes some typical methods of randomization. 1. Simple randomization - This type of randomization does not involve any restrictions. Since the treatment assignment is totally random there is no way to guarantee that there will be an even distribution between groups. For example, one site of a randomized multi-center drug trial may receive a majority of active drug rather than placebo simply by random chance. This type of randomization scheme can result in an unequal numbers of subjects receiving a specific treatment at a given site or over a given period of time. Chapter 3: Grant Writing Page 6 of 13 Office of Human Research 2. Random permuted blocks - This type of randomization compensates for potential of simple randomization to unbalance treatment assignment. With this approach a randomization block size is chosen (e.g. 4, 8, or more subjects) in which the BALANCE OF TREATMENT ASSIGNMENTS is kept proportional according to study design. For example if a block size of 4 is chosen and the protocol defines two study groups, 1 active vs. 1 placebo drug group, then the block will contain 2 active study drug kits and 2 placebo study drug kits. Since the entire block of 4 kits is randomly assigned a treatment number, the subjects will receive their treatment assignment randomly over a given period of time. 3. Stratified randomization - This type of randomization assigns study treatment on the bases of certain baseline characteristics such as gender, age, weight, etc. (i.e. a specific 'stratum' of the population being studied). The goal of this approach is to balance the number the subjects with the characteristic of interest in each treatment group to ensure comparable groups. This type of randomization is most commonly used in smaller studies where fully random assignment of study treatment could result in an imbalance of subjects with a given baseline characteristic (e.g. the majority of obese subjects in one treatment group vs. non-obese in the other, or the majority of females in one treatment vs. males in the other.). Large-scale studies, due to their size, usually have balance of baseline characteristics and therefore less often require stratified randomization. There are a variety of programs available to generate random allocation sequences. An example of an on-line program can be found at: http://www.randomization.com/. Blinding and Placebo Control Blinded: Blinding is the act of keeping the identity of a study intervention secret (in other words, it would not be known if a study treatment was active treatment or placebo). Single-blind means only the research subject is blind to the actual intervention. Double-blind means two parties (usually the subject and the investigator/research team) are blind to the actual intervention. Occasionally the less-frequently used term of triple-blind is used to emphasize that non-study personnel are also blind to the study intervention (e.g. study monitors/auditors, end-point assessment committees, etc.). Blinded studies involving investigational products may use placebos and double-dummy treatments to disguise treatment assignment. A placebo is a study intervention designed to look like the active treatment but having no active properties. A double-dummy treatment is a method of blinding two treatments whose appearances are dissimilar by administering both treatment forms - one active and one placebo. For example, in designing a study comparing heparin (intravenously delivered) vs. a low molecular weight heparin (subcutaneously delivered) if the study were to be double-blinded, it would be necessary to have two types of placebo (two "dummy" treatments), an intravenous placebo and a subcutaneous placebo. Un-blinded: In an un-blinded study, the subject, investigator and evaluator are aware of the actual study treatment. Un-blinded studies involving investigational products are referred to as open-label. Chapter 3: Grant Writing Page 7 of 13 Office of Human Research Observational Studies In an observational study, specific events or findings within the study-defined population are collected without any intervention by the researcher. In other words, the researcher observes and studies findings in a setting outside of a randomized, blinded or placebocontrolled design. This type of design is usually used in investigations where it would be unnecessary, infeasible or unethical to assign factors (e.g. smoking in pregnant women). Like experimental studies, observational studies often use control groups for comparison, but because a treatment is not assigned, randomization is not possible. Observational studies have the potential for introducing confounding biases due to the risk of an unknown association between the factor under study and the outcome. Analytical Cohort study: A cohort study examines specific events or outcomes in a group of subjects who are followed over time. This study design compares the incidence of a given event/outcome in exposed and unexposed groups in an effort to determine an association. The common association measurement for a cohort study is relative risk (see definition below). Cohort studies can be prospective or retrospective. Prospective cohort studies are expensive and time-consuming, but because of their prospective nature, cohort studies can provide stronger empirical evidence than case-control studies. Retrospective cohort studies are often less expensive to conduct, but may be subject to data collection obstacles (e.g. the investigator has no mechanism of ensuring documentation of a specific type of event or outcome). Case-control study: A case-control study is a type of retrospective observational study comparing persons with a disease, condition, or exposure (the cases) and persons without the disease, condition or exposure (the control), assessing differences in events or outcomes between the groups. The two groups are otherwise comparable across all the relevant baseline characteristics. The common association measure for a case-control study is the odds ratio (see definition below). Case-control studies are usually used for broad-based, inexpensive evaluation of risk factors and are also useful for evaluating rare conditions or risk factors with long induction periods. Descriptive Cross-sectional study: A cross-sectional study is a descriptive study of the relationship between diseases and other factors at one point in time in a defined population. Cross-sectional studies determine the prevalence (presence) of an exposure and disease, but lack information on timing of exposure. Crosssectional studies generally cannot be used to draw causal inferences and are usually used for hypothesis generation. Case reports and Case series: A case report is a description of a single patient and usually includes a discussion of medical conditions and treatments along with adverse events and outcomes. A case series is a group of case reports describing patients that have been exposed to a specific treatment or agent. Due to the typically small numbers of cases in a case series and the lack of a control group, the value of interpreting the reported findings is limited. These types of presentations are best used for hypothesis generation. Chapter 3: Grant Writing Page 8 of 13 Office of Human Research 4. General Guide to Statistical Consultation The importance of early involvement of a statistician in the design of a clinical study cannot be overstated. To consult a statistician after an experiment is finished is often merely to ask him to conduct a post mortem examination. He can perhaps say what the experiment died of. - R.A. Fisher (in his 1938 address to the First Indian Statistical Congress) Most often the assistance of a statistician will be required for the selection of an experimental design, the development of the corresponding analysis plan and the subsequent interpretation of parameter estimates and test results. Meaningful involvement of a statistician in study development can permit significant contributions to the following study elements: • • • • • • • • • • • • • • • • • Problem Formulation Background and significance Methods and materials Experimental design Study flowcharts Study schema Feasibility of design Sample size or power estimates Statistical analysis plan Data management plan Case Report Form design Choice of statistical software Choice of Database Software Implications of probable/possible results Responses to reviewer comments Help with resubmission References Even when the analytic needs of the investigator seem obvious, review of the research plan by the "new eyes" of the statistician may lead to alternative methods that should improve efficiency or lead to new insights. Since statistics is evolving science, not static technology, new advances may replace or change analysis recommendations over time. Dialogue between investigator and statistician will almost always help to clarify research objectives, prioritize study aims, and lead to more informed and appropriate selection of tests of hypotheses. Ideally, such exchanges will lead researcher to view statistician as collaborator, rather than consultant, which should lead to improved research designs, more comprehensive analyses and better scientific insight. 4.1 The initial meeting with the biostatistician Preparation for an initial meeting with a statistician should include a written description of the proposed project stating the general objectives of the study and the questions that the investigator hopes to answer. The following are the key elements of the researcher's proposed study that the statistician will need in order to best assess study design and statistical approach: Chapter 3: Grant Writing Page 9 of 13 Office of Human Research • Study Objectives • Population(s) targeted by the study (e.g. healthy volunteers, patients with a specific disease or combination of diseases, etc.) • Response variables of interest • Relevant classification (e.g. gender, race, severity type, smoking status, etc.) • Important variables associated with the response variable of interest (i.e. covariates) • Background information from a variety of sources: o pilot studies (i.e. a small version of the full study being proposed) o previous studies (i.e. similar study population or intervention) o scientific literature (i.e. theoretical basis for proposal, animal studies) o collegial exchanges (e.g. scientific meetings, workshops, e-mail) o anecdotal observation (e.g. poor sense of smell in schizophrenics) Construction of a Study Flowchart, often called a Time and Events Chart, and/or study schema diagrams can summarize and communicate the study design, most effectively. From the above information, the statistical consultant can assist with development of a list of specific aims, which the researcher will classify as primary, secondary or exploratory aims. These aims will give rise to null and alternative hypotheses (see definitions in Basic Statistical Terms below) which may be subjected to statistical tests of significance. The statistical consultant needs to understand the purpose and context of the proposal, rather than viewing the research as an abstract statistical problem. In addition to general and technical details of the proposed study, the researcher should be prepared to provide answers to the most basic questions concerning the study and core discipline. These questions might require explanation of fundamental elements of the disease, disorder or biological process being studied. For example, the statistician may not know whether the origins of a process to be studied are genetic, environmental or both and such information is important to the analysis approach to be used. Attention to this upfront planning for a study will lead to a solid development of clear and comprehensive narratives that will comprise the background, methods and other sections of a researcher's protocol. 4.2 Basic Statistical Terms To facilitate interaction with the biostatistician, the investigator should be familiar with some basic statistical terminology. The following defines some basic terms. Alpha error: A statistical error in testing an hypothesis, often referred to as type I error (the "first type of error"), which incorrectly concludes that a treatment or intervention is proven effective when it is actually is not effective; sometimes referred to as a false positive result. Chapter 3: Grant Writing Page 10 of 13 Office of Human Research Beta error: A statistical error, often referred to as type II error (the "second type of error"), which incorrectly concludes that a treatment or intervention is proven ineffective when it is actually effective; often referred to as a false negative result. Confidence Intervals (CI): Confidence intervals are a way of expressing a level of confidence in a specific statistical finding. If a study were repeated, the results of the repeated study would not be exactly the same as the first study. If a study were repeated many times, one would eventually establish a particular range of results in which the "real" result that would prove (or disprove) the study are likely to be found. This range is called the confidence interval. Therefore a 95% confidence interval would mean there is a 95% chance that the "real" result of the study analysis falls within the stated interval or range. The wider the confidence interval the greater the variability of the result, and the narrower the confidence interval, the lesser the variability of the result, though there are other factors to consider in determining whether the result likely proves or disproves the study hypothesis. For example, in a study of a treatment vs. placebo, if the study outcome showed the treatment to have a 10% decrease in events, and the calculated range of likely values in which this result lies is found to be -1.2% to 12%, it would generally be expressed as: endpoint reduction in the treatment arm of 10% (95% CI 1.2% to 12%). In this case, since the lower range of the confidence interval crosses over 0% (i.e. a value showing no difference in the treatment arm from placebo) if the result was being viewed as either proving or disproving a difference in the study treatment arms, it could be argued that the trial was negative since a result of 0% lies within the range of possible results given the confidence interval. However, adopting a "likelihood" approach to the study finding, the majority of the range of the confidence interval extends in the positive direction beyond 0% (i.e. most of the likely values are greater than 0%), one could argue that it is more likely that the study does show a reduction in events by the treatment. (Excerpted from: T. Greenhalgh, BMJ No 7105 Volume 315, August 16, 1997) Null hypothesis (H0): A mathematical statement of the converse of (one of) the specific aims of the study. Following the example used in the definition for the alternative hypothesis, the corresponding null hypothesis would be that the proportion of children who play video games and exhibit at least one violent incident is equal to or less than (i.e. no worse than) the proportion of children who do not play video games. The null hypothesis is the converse of the alternative hypothesis. Odds ratio: An odds ratio compares the odds of an event in one group with the odds of an event in a comparator group. Odds ratios are a common way to express outcomes in observational studies. For example, a case-control study of two cohorts, one with an exposure to a presumed noxious element and one without, included 100 subjects in each group and looked at death rates after 5 years. In this example there were 20 subjects that died in the exposed group (case group) vs. 5 who died in the unexposed group (control group). The odds of dying in the case group is the ratio of subjects who died to subjects who did not die, i.e. 20/80, or 1/4, which can be expressed as 0.25. The odds of dying in the control group would then be 5/90, or 0.05. Therefore the odds ratio of the event rate comparing the case group to the control group would be displayed as: 0.25/0.05, or 5. Thus the odds of death in exposed group are 5 times the odds of death in the unexposed group. Chapter 3: Grant Writing Page 11 of 13 Office of Human Research Outlier: An extreme deviation from the mean (i.e. a data point that lies an abnormal distance away from other values). P value: A way of expressing statistical significance. Standard practice (which was arbitrarily decided) is that a 5% likelihood that the study outcome is due to chance (i.e. a 95% likelihood the study outcome is not due to chance) is statistically significant. This 5% likelihood is expressed as P=0.05. A 1% likelihood that a study outcome is due to chance (i.e. 99% likelihood that study outcome is not due to chance), is expressed as P=0.01 and considered highly statistically significant. A criticism of the use of a P value test of significance is that it relies on an arbitrary cut-off in answering a yes-no question on a finding. An alternative approach is to look at a range of likelihood that a statistical finding expresses reality (see Confidence Intervals). Power: Power is defined to be equal to 1- ß; that is the probability of not committing a Beta (Type II) error. Power is an index of sensitivity, since it is the probability of rejecting a false null hypothesis. An analogous index of specificity is 1- ?, the probability of not rejecting a true null hypothesis; although there is no common statistical name for this probability. Risk, relative risk, and risk reduction Risk is a simple calculation of the number of subjects in a group that experience an event divided by the total number of subjects in that group. The equation is: (number of subjects with event/total number of subjects assessed for the event). Relative risk compares the risk of an event in one group to the risk in a comparator group. To show the relative risk of an event in a control group vs. a treatment group, the equation is: (risk of event in control group/risk of event in the treatment group). Absolute risk reduction shows the absolute amount of reduction in the risk of an event in one group vs. a comparator group. To show the absolute risk reduction in a treatment group vs. a control (non-treatment) group the equation is: (control group risk - treatment group risk). Relative risk reduction expresses the reduction in risk as the difference in the risk of an event in one group vs. a comparator group divided by the overall risk of the event in the first group (i.e. the amount of risk reduction relative to the overall risk). To show the relative risk reduction in a treatment group vs. a control (non-treatment) group the equation is: ([Control group risk - treatment group risk]/control group risk). To illustrate the above definitions of risk, relative risk and risk reduction, consider the following example: A study of a target disease compares usual care to a new treatment by measuring the number of deaths in each group. Two hundred subjects are enrolled in each study arm and results are measured over the five-year duration of the study. The table below shows the number of deaths in each group at 5 years. Chapter 3: Grant Writing Page 12 of 13 Office of Human Research Treatment intervention Total number of patients Number of Deaths Control Group 200 40 Treatment Group 200 10 Risk: (subjects with events/total number subjects studied) In the placebo group, the risk of death is 40/200, which is 0.20 or 20%. For the treatment group, the risk of death is 10/200, which is 0.05 or 5%. In other words, at five years, there is a 20% risk of dying in patients with the target disease if not treated compared to a 5% risk of dying if treated. Relative Risk: (risk in control group/risk in treatment group) Relative risk compares the risk in one group relative to the risk in the other group. The relative risk between the control group and the treatment group is .020/0.05, which is 4, meaning patients who do not receive treatment are at 4 times the risk of death than similar patients who receive the active treatment. Absolute risk reduction: (risk in control group - risk in treatment group) The control group risk of death is 20%, the treatment group risk of death is 5%, therefore the absolute amount of risk that was reduced by treatment is 20% - 5%, which is 15%. In other words, out of 200 patients treated 15% (or 30 patients) avoided death at five years. Relative Risk reduction: [(risk in control group - risk in treatment group)/risk in control group] In the example noted above the relative risk reduction would be [(20% - 5%)/20%], or 15/20, or 0.75, most often expressed as a percent: 75%. Relative risk reduction is usually more clinically useful than absolute risk reduction when trying to conceptualize the benefit of a treatment. In other words, while the control grouped showed 40 patient deaths and the treatment group showed 10, the relative risk reduction illustrates that this reduction of 30 deaths represents 75% of the overall risk of death; i.e. the treatment reduced the overall risk of death by 75%. Statistical significance: The likelihood that a particular study outcome has arisen by chance. This is commonly expressed as a P value. Note: Statistical significance does not necessarily mean a finding is clinically significant. Study arm: The different groups in a study. Each group represents an arm of the study. A single-arm study would have only one group; a double-arm study would have two groups, and so on. Chapter 3: Grant Writing Page 13 of 13 Office of Human Research Chapter 4: Protocol Design/Review The protocol is a document that describes the objectives, design, methodology, statistical considerations, and organization of a research study. The protocol explains the specific procedures of the study and outlines the scientific, organizational, administrative, and financial aspects of the research study. The protocol is distinct from the research grant. While the grant provides a broad overview of the study procedures, the protocol clearly defines and operationalizes the details of study implementation. The required elements of a study protocol are dictated in the Good Clinical Practice (GCP) guidelines. Part I: Elements of a Study Protocol The following sections describe the elements of a GCP standard protocol and are contained in a template attached as an appendix to this chapter. Please contact the Office of Human Research (OHR) for an electronic version of the template that uses functionalities in Microsoft Word to create automated formatting and generation of a table of contents. Various sections also contain suggested language that is compliant with federal regulations (e.g. safety section, adverse event reporting requirements, etc.). Note: This template was developed for drug studies, but can be adapted for other types of studies. The National Cancer Institute (NCI) also has protocol templates available for cancer studies at Protocol Development Guidelines and Templates. Title Page The protocol title page is the "front cover" of the study protocol and displays the title prominently. Other information to include on the title page: • Principal Investigator name • Sponsor name • Protocol version/version date Table of Contents Very short protocols of only a few pages may not require a table of contents. Larger protocols should have a table of contents to aid study personnel in easily finding a specific protocol section or item. Executive Summary It is useful to develop a brief protocol summary and include it as part of the protocol, typically located after the protocol table of contents. Generally only 1-3 pages in length, the protocol summary provides a way to quickly grasp the key elements of the protocol. This is a useful tool when trying to communicate with various parties about the study. The Executive Summary can be written with headings and associated text, or summarized succinctly in table form. The key elements of a protocol summary follow: Chapter 4: Protocol Design & Review Page 1 of 35 Office of Human Research Title Full title of protocol Short title Shortened title, if one is typically used by you or your Center/Dept. Protocol number The standard protocol number used to identify this study. Phase Clinical study phase (e.g. Phase 1, 2, 2a, 2b, 3, 3a, 3b or 4) Methodology Design attributes such as single blind, double blind or open label; Randomized, placebo or active placebo control; crossover design, etc. Study duration Estimated duration for the main protocol (e.g. from start of screening to last patient processed and finishing the study) Study centers Single-center or multi-center. If multi-center, note number of projected centers to be involved. Objectives Brief statement of primary study objectives Number of subjects Number of subjects projected for the entire study (e.g. not for simply one site, rather for entire study, all sites combined) Diagnosis and Note the main clinical disease state under study and the key main inclusion inclusion criteria (i.e. not the entire list that will appear later in criteria the protocol -rather only the key inclusion criteria) Study Study drug name (generic name, though can also state product, dose, marketed name if name-brand used in the study). Also dose, route, regimen dose route and dose regimen Duration and Total duration of drug product administration (including any administration open-label lead-in, if applicable). Reference therapy Note if there is a standard reference therapy against which the study product is being compared, or if the reference is a placebo Statistical Methodology A very brief description of the main elements of the statistical methodology to be used in the study. (As few lines as possible). Chapter 4: Protocol Design & Review Page 2 of 35 Office of Human Research 1. Introduction The introduction should open with remarks that state that this document is a clinical research protocol and the described study will be conducted in compliance with the protocol, Good Clinical Practices standards and associated Federal regulations, and all applicable MHS research requirements. The rest of the introduction should include the following subsections. 1.1 Background This section should contain a background discussion of the target disease state to which the investigational product(s) hold promise and any pathophysiology relevant to potential study treatment action. 1.2 Investigational Agent This section should contain a description of the investigational product, its make-up, chemical properties and any relevant physical properties, including any available pharmacologic data. (A good example for this section is the "Description" and "Pharmacology" sections for drugs listed in the Physicians' Desk Reference) 1.3 Preclinical Data Summarize the available non-clinical data (published or available unpublished data) that could have clinical significance. 1.4 Clinical Data to Date Summarize the available clinical study data (published or available unpublished data) with relevance to the protocol under construction - if none is available, include a statement that there is no available clinical research data to date on the investigational product. 1.5 Dose Rationale and Risk/Benefits Describe the rationale used for selection of the dose for the protocol under construction. This should be based on non-clinical and clinical data available to date. It should include justification for route of administration, dosage, dosage regimen, and dosage period. Discuss why the risks to subjects are reasonable in relation to the anticipated benefits and/or knowledge that might reasonably be expected from the results. 2. Study Objectives Describe the overall objectives and purpose of the study. This should include both primary and any secondary objectives, e.g.: Chapter 4: Protocol Design & Review Page 3 of 35 Office of Human Research 2.1 Primary Objective To assess the efficacy of XXXX on decreasing infarct size as measured by Sestamibi scanning. 2.2 Secondary Objective To assess the safety and tolerability of two doses of XXXX in subjects with acute myocardial infarction. 3. Study Design 3.1 General Design Include: • The type/design of the study (e.g. Phase, randomized, double-blind, parallel group, etc.) • A schematic diagram of the trial design, procedures and stages is advisable • Expected duration of subject participation • A description of the sequence and duration of all trial periods including followup, if any 3.2 Primary Study Endpoints Describe the primary endpoint to be analyzed in the study (e.g. could be safety or efficacy, depending on the main objective of the study). 3.3 Secondary Study Endpoints Describe any secondary endpoints to be analyzed in the study 3.4 Primary Safety Endpoints All studies should include the primary safety endpoints to be measured. If the primary objective of the study is a safety study and therefore the Primary Endpoint(s) of the study are safety endpoints, then it should be noted in section 3.1 above and this subsection 3.3 can be deleted. 4. Subject Selection and Withdrawal 4.1 Inclusion Criteria Create a numbered list of criteria subjects must meet to be eligible for study enrollment (e.g. age, gender, target disease, concomitant disease if required, etc.) Generally should include items such as: "subjects are capable of giving informed consent", or if appropriate, "have an acceptable surrogate capable of giving consent on the subject's behalf." Chapter 4: Protocol Design & Review Page 4 of 35 Office of Human Research 4.2 Exclusion Criteria Create a numbered list of criteria that would exclude a subject from study enrollment. If appropriate, this list should generally include that subjects cannot be homeless persons, or have active drug/alcohol dependence or abuse history. If exposure to certain medications or treatments at screening is prohibited, that must be noted in the exclusion criteria; if there are prohibited concomitant medications during the study period, that should be noted here as well. 4.3 Subject Recruitment and Screening Describe how subjects will be recruited for the study, e.g. from investigator or subinvestigator clinical practices, referring physicians, advertisement, etc. Note in this section that information to be disseminated to subjects (handouts, brochures, etc.) and any advertisements must be approved by the IRB for the site; include a sample of such information in the attachment section of the protocol. Also in this section, list any screening requirements such as laboratory or diagnostic testing necessary to meet any noted inclusion or exclusion criteria (greater detail of timing, etc. can be included later in section 6 "Study Procedures" section of the protocol). 4.4 Early Withdrawal of Subjects When and How to Withdraw Subjects: Describe the scenarios under which a subject may be withdrawn from the study prior the expected completion of that subject (e.g. safety reasons, failure of subject to adhere to protocol requirements, subject consent withdrawal, disease progression, etc.) Also, if abrupt termination of study treatment could affect subject safety (e.g. in an antihypertensive study, abrupt withdrawal without other intervention might cause hypertensive rebound), describe procedure to transition subject off the study drug or to alternate therapy. Data Collection and Follow-up for Withdrawn Subjects Even though subjects may be withdrawn prematurely from the study, it is imperative to collect at least survival data on such subjects throughout the protocol defined follow-up period for that subject (though careful thought should be give to the full data set that should to be collected on such subjects to fully support the analysis). Such data is important to the integrity of the final study analysis since early withdrawal could be related to the safety profile of the study drug. If a subject withdraws consent to participate in the study, attempts should be made to obtain permission to record at least survival data up to the protocol-described end of subject follow-up period. IT MUST BE A HIGH PRIORITY TO TRY TO OBTAIN AT LEAST SURVIVAL DATA ON ALL SUBJECTS LOST TO FOLLOW-UP AND TO NOTE WHAT METHODS SHOULD BE USED BEFORE ONE CAN STATE THE SUBJECT IS TRULY LOST TO FOLLOW-UP (e.g. number of phone calls to subject, phone calls to next-of-kin if possible, certified letters, etc.). Chapter 4: Protocol Design & Review Page 5 of 35 Office of Human Research 5. Study Drug 5.1 Description This section should be a very brief synopsis of section 1.2 "Investigational agent", along with how the how the drug product will appear (e.g. as tablets or capsules of "X" mg, as a liquid with "X" mg dissolved in 10ml 5% dextrose and water, etc.) 5.2 Treatment Regimen Describe dose, route of administration, and treatment duration. 5.3 Method for Assigning Subjects to Treatment Groups Describe how a randomization number and associated treatment assignment will be made. This could be selection of a sequentially numbered drug kit/box, or communication with a randomization center that assigns a number associated with a specific treatment kit/box, etc. 5.4 Preparation and Administration of Study Drug Describe in detail all the steps necessary to properly prepare study treatment. Include whether the drug preparation will be done in a pharmacy or by a study team member. Fully describe how the study treatment is to be administered. If study drug is stored, mixed/prepared or dispensed from the Investigational Drug Service, that should be noted here, including the contact number to that service office. 5.5 Subject Compliance Monitoring Describe how the study team will assess and track subject compliance with the study treatment regimen, and what procedures must be followed for any subject who is significantly non-compliant with the study treatment regimen. 5.6 Prior and Concomitant Therapy In this section, describe: • What prior and/or concomitant medical therapy will be collected (if applicable). • Which concomitant medicines/therapies (including rescue therapies) are permitted during the study • Which concomitant medicines/therapies are not permitted during the study (if applicable) Chapter 4: Protocol Design & Review Page 6 of 35 Office of Human Research 5.7 Packaging • Describe how the study drug and any comparator agent will be packaged along with the amounts (e.g. "20 ml vials containing 30 mg", or "bottles containing 30 tablets of .", etc.) along with any associated labeling • Describe if drug is to be shipped in bulk (e.g. Study drug will be shipped in boxes of 30 vials each, etc.) or as separate subject-specific kits/boxes • When subject drug kits are constructed, describe all the contents of the kit/box and associated labeling. 5.8 Blinding of Study Drug Describe how the drug is blinded (refer back to Section 8.4 "Unblinding Procedures"). 5.9 Receiving, Storage, Dispensing and Return Receipt of Drug Supplies Describe how drug will be obtained i.e. what entity will ship the drug to the investigative site, and to what location at the site, (e.g. investigational pharmacy, etc.) Storage Describe storage temperature requirements, whether supplies must be protected from light, and the location of the supplies (e.g. study pharmacy). Describe any special handling requirements during storage Dispensing of Study Drug Describe how the drug will be assigned to each subject and dispensed. This section should include regular drug reconciliation checks (i.e. how much drug was assigned and whether subjects actually received assigned dose or received dose properly, how much remains, how much drug was inadvertently damaged, etc. For e.g. "Regular study drug reconciliation will be performed to document drug assigned, drug consumed, and drug remaining. This reconciliation will be logged on the drug reconciliation form, and signed and dated by the study team."). Return or Destruction of Study Drug This section should note the procedures for final reconciliation of the site's drug supply at the end of the study, and whether study drug is to be shipped back to a source or destroyed on site. If drug is to be shipped back to a source, note the address and contact information here. 6. Study Procedures In this section, describe all the procedures and treatments required at each visit, broken out by visit. Create a study procedures flowchart/table that describes the activities and procedures to be followed at each visit. Include this flowchart/table in the Attachment section and refer to that attachment in this section. Chapter 4: Protocol Design & Review Page 7 of 35 Office of Human Research 7. Statistical Plan 7.1 Sample Size Determination Describe the statistical methods for determining the sample size for the study. 7.2 Statistical Methods Summarize the overall statistical approach to the analysis of the study. The section should contain the key elements of the analysis plan, but should not be a reiteration of a detailed study analysis plan. The full Statistical Analysis Plan can then be a "standalone" document that can undergo edits and versioning outside of the protocol and therefore not trigger an IRB re-review with every version or edit, as long as the elements of the study plan do not change. Be clear on primary as well as any applicable secondary analyses 7.3 Subject Population(s) for Analysis This section should be very specific in defining the subject populations whose data will be subjected to the study analysis - both for the primary analysis and any applicable secondary analyses. Examples of such populations include: • All-randomized population: Any subject randomized into the study, regardless of whether they received study drug • All-treated population: Any subject randomized into the study that received at least one dose of study drug • Protocol-compliant population: Any subject who was randomized and received the protocol required study drug exposure and required protocol processing 8. Safety and Adverse Events Procedures for eliciting reports of, recording, and reporting adverse events should be specified. Note: See the protocol template from the OHR for GCP-compliant standard language examples for subsections 8.1 though 8.3. The subsections include: 8.1 Definitions 8.2 Recording of Adverse Events 8.3 Reporting of Serious Adverse Events Include the following: • Sponsor Reporting by Investigator • IRB Notification by Investigator • FDA Notification by Sponsor Chapter 4: Protocol Design & Review Page 8 of 35 Office of Human Research 8.4 Unblinding Procedures While the safety of the subject always comes first, it is still important to seriously consider if unblinding the study therapy is necessary to ensure a subject's safety. This section should clearly describe the procedures for unblinding study therapy on a subject, including documentation of this in the subject's source document. For investigators, state that the investigator must inform the sponsor of all subjects whose treatment was unblinded - and describes the timelines for such reporting. In most cases, the unblinding will be part of managing an SAE, and will be reported with the SAE, however, in cases where unblinding was not associated with an SAE, such actions should be reported in a timely manner. While there is no regulation governing this timeline, it is suggested to use the same timeline requirements for investigator reporting of SAEs, (i.e. notification of sponsor within 24 hours by phone or fax, followed by a written narrative of the event within 48 hours.) 8.5 Stopping Rules In studies with a primary safety endpoint or studies with high risk to study subjects, rules should be developed that clarify the circumstances and procedures for interrupting or stopping the study. If a central Data and Safety Monitoring Board (DSMB) or Committee (DSMC) is set up for the study, the stopping rules should be incorporated into their safety analysis plan as well. 8.6 Medical Monitoring Refer to Monitoring Plan Development (Chapter 6 of this manual) for more information about Medical Monitoring. 9. Data Handling and Record Keeping Specifics should be provided for the handling of data to ensure the proper handling of data and records. Note: See the protocol template for GCP-compliant standard language examples for subsections 9.1 though 9.4. The subsections should include: • Confidentiality • Source Documents • Case Report Forms • Records Retention 10. Study Monitoring, Auditing, and Inspecting It is recommended that the monitoring plan be referred to as a separate attachment. Include a statement that direct access to source data/documents will be provided for monitoring, audits, IRB review, and regulatory inspections. Monitoring plan development is covered in more detail in Monitoring Plan Development. Include specific provisions for the following: Chapter 4: Protocol Design & Review Page 9 of 35 Office of Human Research 11. • Auditing and Inspecting • Study Monitoring Plan Ethical Considerations Include a statement that the study will be conducted in accordance with the protocol, GCP, and applicable regulatory requirements. Provide specific reference as to how consent will be obtained, and that IRB approval will be obtained before the study is initiated. Standard language for this section is provided in the protocol template. 12. Study Finances 12.1 Funding Source This section should describe how the study will be financed, but should not contain specific dollar amounts (e.g. "This study is financed through a grant from the US National Institute of Health", or "a grant from the American Heart Association", etc.) 12.2 Conflict of Interest Reference SOP 105 (Prohibition of Financial Conflict). 12.3 Subject Stipends or Payments Describe any subject stipend or payment here. 13. Publication Plan This section should include the requirements any publication policies of the Memorial Healthcare System. If, in addition to the investigator, other investigators are involved with the study, identify who holds the primary responsibility for publication of any results of the study. Also define the need to first obtain approval from the primary responsible party before any information can be used or passed on to a third party. 14. References This is the bibliography section for any information cited in the protocol. It should be organized as any standard bibliography. 15. Attachments This section should contain all pertinent documents associated with the management of the study. The following list examples of potential attachments: • Investigator Agreement (for any investigator, other than sponsor-investigator, who participates in the study) Chapter 4: Protocol Design & Review Page 10 of 35 Office of Human Research • Sample Consent Form • Study Procedures Flowchart/Table • Core Lab Instructions To Investigators • Specimen Preparation And Handling (e.g. for any specialized procedures that study team must follow to process a study specimen, and/or prepare it for shipment) • Drug Conversion Plan (e.g. if there is a special regimen for transitioning a subject from their baseline medication over to study medication) • Antidote Preparation And Delivery (e.g. special instructions for preparing and delivering any therapy designed to reverse the effects of the study drug, if applicable) Part II: Protocol Review 16. Review of Protocol from Sponsor For industry-sponsored studies, the protocol is written by the sponsor and provided to the on-site investigator. It is the responsibility of the investigator to be thoroughly familiar with the protocol, and to conduct the study in strict accordance with the protocol. If the investigator meets the prescribed qualifications, the sponsor will forward a confidentiality agreement. The confidentiality agreement is a legally binding document that prohibits the investigator from disclosing the proprietary and confidential information found within the protocol. The confidentiality agreement must submitted to the Office of Human Research to be routed for internal approvals. Once finalized by the Legal department, it can be returned to the sponsor. Once the agreement is received, the sponsor will forward a study protocol (and Investigator's Brochure, if applicable), the contract, and budget to the investigator for review. The investigator and his or her study team will read and review the proposed protocol. An overall evaluation of the study will include clinical interest and feasibility. The process of evaluating the feasibility of conducting a research trial is complex and multi-factorial. Some considerations that determine the difficulty of a protocol are summarized below: 17. • Study duration – short, moderate, or prolonged • Paperwork – can existing records be used, or are there additional requirements • Follow-up – will office visits be necessary, or will telephone calls suffice • Procedures – are they “standard of care” or would they require specialized expertise IRB Protocol Summary The IRB requires a protocol summary as part of the IRB submission. This document includes much of the information from the Executive Summary. The IRB provides detailed guidance on constructing the IRB protocol summary. Chapter 4: Protocol Design & Review Page 11 of 35 Office of Human Research 18. Study Flowchart The Study Flowchart (also known as the Time and Events Chart or Schedule of Events) is a table that is created to display the schedule of study procedures. It outlines the planned chronological occurrence of events that research subjects will undergo during their study participation. The unified, visual format of a Study Flowchart helps promote organization and communication. A Study Flowchart facilitates several study processes including: • Project feasibility assessment • Statistical design • Case Report Form and Informed Consent Form development • Institutional Review Board (IRB) review • Site orientation and in-service presentation • Database construction • Subject enrollment and follow-up The Study Flowchart can be included as an element of the protocol or presented as an appendix to the study protocol. 19. Study Schematic The Study Schematic is a diagram illustrating key concepts of the study design, such as sampling, randomization, and/or blinding. The unified, visual format of a Study Schematic helps promote organization and communication. A Study Schematic facilitates several study processes including: • Protocol design and implementation • Statistical design and analysis • IRB review • Site orientation and in-service presentation The Study Schematic can be included as an element of the protocol or presented as an appendix to the study protocol. See example below. Chapter 4: Protocol Design & Review Page 12 of 35 Office of Human Research Chapter 4: Protocol Design & Review Page 13 of 35 Office of Human Research APPENDIX – PROTOCOL TEMPLATE INSERT TITLE OF THE PROTOCOL [Include phase (e.g. phase I, phase II, etc.), design (e.g. randomized, double blind, placebo controlled, etc), if the study is multi-centered, the investigational drug, and target disease(s)] Example title: A phase II, randomized, double-blind, placebo-controlled, multi-center study of the effects of XXXX on infarct size in subjects with diabetes mellitus presenting with acute myocardial infarction. Regulatory Sponsor: Insert the Name of the Sponsor-Investigator Insert Department Name Insert Address Insert Phone Number Funding Sponsor: Insert the Name of Primary Funding Institution Insert Address Insert Phone Number Study Product: Insert Study Drug Name – Generic, followed by marketed name if applicable Protocol Number: Insert Protocol Number Used by Sponsor IND Number: Insert IND Number if applicable Date: Amended: Administrative Change: CONFIDENTIAL This document is confidential and the property of Memorial Healthcare System. No part of it may be transmitted, reproduced, published, or used by other persons without prior written authorization from the study sponsor. Chapter 4: Protocol Design & Review Page 14 of 35 Office of Human Research Table of Contents STUDY SUMMARY .................................................................................................................................... 17 1 INTRODUCTION ............................................................................................................................... 18 1.1 1.2 1.3 1.4 1.5 BACKGROUND ............................................................................................................................. 18 INVESTIGATIONAL AGENT ............................................................................................................. 18 PRECLINICAL DATA ...................................................................................................................... 18 CLINICAL DATA TO DATE .............................................................................................................. 18 DOSE RATIONALE AND RISK/BENEFITS ......................................................................................... 18 2 STUDY OBJECTIVES ....................................................................................................................... 19 3 STUDY DESIGN ................................................................................................................................ 19 3.1 3.2 3.3 3.4 4 GENERAL DESIGN........................................................................................................................ 19 PRIMARY STUDY ENDPOINTS........................................................................................................ 19 SECONDARY STUDY ENDPOINTS .................................................................................................. 19 PRIMARY SAFETY ENDPOINTS ...................................................................................................... 19 SUBJECT SELECTION AND WITHDRAWAL ................................................................................. 20 4.1 INCLUSION CRITERIA .................................................................................................................... 20 4.2 EXCLUSION CRITERIA .................................................................................................................. 20 4.3 SUBJECT RECRUITMENT AND SCREENING ..................................................................................... 20 4.4 EARLY W ITHDRAWAL OF SUBJECTS .............................................................................................. 20 4.4.1 When and How to Withdraw Subjects .................................................................................. 20 4.4.2 Data Collection and Follow-up for Withdrawn Subjects ........................................................ 21 5 STUDY DRUG ................................................................................................................................... 21 5.1 DESCRIPTION .............................................................................................................................. 21 5.2 TREATMENT REGIMEN.................................................................................................................. 21 5.3 METHOD FOR ASSIGNING SUBJECTS TO TREATMENT GROUPS ....................................................... 21 5.4 PREPARATION AND ADMINISTRATION OF STUDY DRUG .................................................................. 21 5.5 SUBJECT COMPLIANCE MONITORING ............................................................................................ 22 5.6 PRIOR AND CONCOMITANT THERAPY ............................................................................................ 22 5.7 PACKAGING ................................................................................................................................. 22 5.8 BLINDING OF STUDY DRUG........................................................................................................... 22 5.9 RECEIVING, STORAGE, DISPENSING AND RETURN ......................................................................... 22 5.9.1 Receipt of Drug Supplies ...................................................................................................... 22 5.9.2 Storage ................................................................................................................................. 23 5.9.3 Dispensing of Study Drug ..................................................................................................... 23 5.9.4 Return or Destruction of Study Drug..................................................................................... 23 6 STUDY PROCEDURES .................................................................................................................... 23 6.1 6.2 6.3 7 STATISTICAL PLAN ......................................................................................................................... 24 7.1 7.2 7.3 8 VISIT 1 ........................................................................................................................................ 24 VISIT 2 ........................................................................................................................................ 24 ETC. ............................................................................................................................................ 24 SAMPLE SIZE DETERMINATION ..................................................................................................... 24 STATISTICAL METHODS ................................................................................................................ 24 SUBJECT POPULATION(S) FOR ANALYSIS ...................................................................................... 24 SAFETY AND ADVERSE EVENTS .................................................................................................. 24 8.1 DEFINITIONS................................................................................................................................ 24 Chapter 4: Protocol Design & Review Page 15 of 35 Office of Human Research RECORDING OF ADVERSE EVENTS ............................................................................................... 27 8.2 8.3 REPORTING OF SERIOUS ADVERSE EVENTS.................................................................................. 27 8.3.1 Study Sponsor Notification by Investigator ........................................................................... 27 8.3.2 IRB Notification by Investigator ............................................................................................. 28 8.3.3 FDA Notification by Sponsor ................................................................................................. 28 8.4 UNBLINDING PROCEDURES .......................................................................................................... 28 8.5 STOPPING RULES ........................................................................................................................ 29 8.6 MEDICAL MONITORING ................................................................................................................. 29 8.6.1 Internal Data and Safety Monitoring Board........................................................................... 29 8.6.2 Independent Data and Safety Monitoring Board .................................................................. 30 9 DATA HANDLING AND RECORD KEEPING .................................................................................. 31 9.1 9.2 9.3 9.4 10 CONFIDENTIALITY ........................................................................................................................ 31 SOURCE DOCUMENTS.................................................................................................................. 31 CASE REPORT FORMS ................................................................................................................. 31 RECORDS RETENTION ................................................................................................................. 32 STUDY MONITORING, AUDITING, AND INSPECTING .................................................................. 32 10.1 10.2 STUDY MONITORING PLAN ........................................................................................................... 32 AUDITING AND INSPECTING........................................................................................................... 32 11 ETHICAL CONSIDERATIONS .......................................................................................................... 33 12 STUDY FINANCES ........................................................................................................................... 33 12.1 12.2 12.3 FUNDING SOURCE ....................................................................................................................... 33 CONFLICT OF INTEREST ............................................................................................................... 33 SUBJECT STIPENDS OR PAYMENTS............................................................................................... 34 13 PUBLICATION PLAN ........................................................................................................................ 34 14 REFERENCES .................................................................................................................................. 34 15 ATTACHMENTS................................................................................................................................ 34 Chapter 4: Protocol Design & Review Page 16 of 35 Office of Human Research Study Summary Title Short Title Protocol Number Full title of protocol Shortened title, if one is typically used by you or your Center/Dept. The standard protocol number used to identify this study. Diagnosis and Main Inclusion Criteria Clinical study phase (e.g. Phase 1, 2, 3 or 4) Design attributes such as single blind, double blind or open label; Randomized, placebo or active placebo control; crossover design, etc. Estimated duration for the main protocol (e.g. from start of screening to last subject processed and finishing the study) Single-center or multi-center. If multi-center, note number of projected centers to be involved. Brief statement of primary study objectives Number of subjects projected for the entire study (e.g. not for simply one site, rather for entire study, all sites combined) Note the main clinical disease state under study and the key inclusion criteria (i.e. not the entire list that will appear later in the protocol –rather only the key inclusion criteria) Study Product, Dose, Route, Regimen Study drug name (generic name, though can also state marketed name if name-brand used in the study). Also dose, dose route and dose regimen Phase Methodology Study Duration Study Center(s) Objectives Number of Subjects Total duration of drug product administration (including any open-label lead-in, if applicable). Note if there is a standard reference therapy against which Reference therapy the study product is being compared, or if the reference is a placebo A very brief description of the main elements of the Statistical statistical methodology to be used in the study. (As few lines Methodology as possible). Duration of administration Chapter 4: Protocol Design & Review Page 17 of 35 Office of Human Research Introduction The introduction should open with remarks that state that this document is a clinical research protocol and the described study will be conducted in compliance with the protocol, Good Clinical Practices standards and associated Federal regulations, and all applicable MHS research requirements. The rest of the introduction is broken out into subsections. Example language for the first paragraph under “Introduction” and before the section “1.1 Background”: This document is a protocol for a human research study. This study is to be conducted according to US and international standards of Good Clinical Practice (FDA Title 21 part 312 and International Conference on Harmonization guidelines), applicable government regulations and Memorial Healthcare System research policies and procedures. Background This section should contain a background discussion of the target disease state to which the investigational product(s) hold promise, and any pathophysiology relevant to potential study treatment action. Investigational Agent This section should contain a description of the investigational product, its makeup, chemical properties and any relevant physical properties, including any available pharmacologic data. (A good example for this section is the “Description” and “Pharmacology” sections for drugs listed in the Physicians’ Desk Reference) Preclinical Data Summarize the available non-clinical data (published or available unpublished data) that could have clinical significance. Clinical Data to Date Summarize the available clinical study data (published or available unpublished data) with relevance to the protocol under construction -- if none is available, include a statement that there is no available clinical research data to date on the investigational product. Dose Rationale and Risk/Benefits Describe the rationale used for selection of the dose for the protocol under construction. This should be based on non-clinical and clinical data available to date. It should include justification for route of administration, dosage, dosage regimen, and dosage period. Discuss why the risks to subjects are reasonable in Chapter 4: Protocol Design & Review Page 18 of 35 Office of Human Research relation to the anticipated benefits and/or knowledge that might reasonably be expected from the results. Study Objectives Describe the overall objectives and purpose of the study. This should include both primary and any secondary objectives, e.g.: Primary Objective To assess the efficacy of XXXX on decreasing infarct size as measured by Sestamibi scanning. Secondary Objective To assess the safety and tolerability of two doses of XXXX in subjects with acute myocardial infarction. Study Design General Design Include: • The type/design of the study (e.g. Phase, randomized, double-blind, parallel group, etc.) • A schematic diagram of the trial design, procedures and stages is advisable • Expected duration of subject participation • A description of the sequence and duration of all trial periods including follow-up, if any Primary Study Endpoints Describe the primary endpoint to be analyzed in the study (e.g. could be safety or efficacy, depending on the main objective of the study). Secondary Study Endpoints Describe any secondary endpoints to be analyzed in the study Primary Safety Endpoints All studies should include the primary safety endpoints to be measured. If the primary objective of the study is a safety study and therefore the Primary Endpoint(s) of the study are safety endpoints, then it should be noted in section 3.1 above and this subsection 3.3 can be deleted. Chapter 4: Protocol Design & Review Page 19 of 35 Office of Human Research Subject Selection and Withdrawal Inclusion Criteria Create a numbered list of criteria subjects must meet to be eligible for study enrollment (e.g. age, gender, target disease, concomitant disease if required, etc.) Generally should include items such as: “subjects are capable of giving informed consent”, or if appropriate, “have an acceptable surrogate capable of giving consent on the subject’s behalf.” Exclusion Criteria Create a numbered list of criteria that would exclude a subject from study enrollment. If appropriate, should generally include that subjects cannot be homeless persons, or have active drug/alcohol dependence or abuse history. If exposure to certain medications or treatments at screening is prohibited, that must be noted in the exclusion criteria—if these are also prohibited concomitant medications during the study period that should be noted here as well. Subject Recruitment and Screening Describe how subjects will be recruited for the study, e.g. from investigator or sub-investigator clinical practices, referring physicians, advertisement, etc. Note in this section that information to be disseminated to subjects (handouts, brochures, etc.) and any advertisements must be approved by the IRB for the site; include a sample of such information in the attachment section of the protocol. Also in this section, list any screening requirements such as laboratory or diagnostic testing necessary to meet any noted inclusion or exclusion criteria (greater detail of timing, etc. can be included later in section 6 “Study Procedures” section of the protocol). Early Withdrawal of Subjects When and How to Withdraw Subjects Describe the scenarios under which a subject may be withdraw from the study prior the expected completion of that subject (e.g. safety reasons, failure of subject to adhere to protocol requirements, subject consent withdrawal, disease progression, etc.) Also, if abrupt termination of study treatment could affect subject safety (e.g. in an antihypertensive study, abrupt withdrawal without other intervention might cause hypertensive rebound), describe procedure to transition subject off the study drug or to alternate therapy. Chapter 4: Protocol Design & Review Page 20 of 35 Office of Human Research Data Collection and Follow-up for Withdrawn Subjects Even though subjects may be withdrawn prematurely from the study, it is imperative to collect at least survival data on such subjects throughout the protocol defined follow-up period for that subject (though careful thought should be give to the full data set that should to be collected on such subjects to fully support the analysis). Such data is important to the integrity of the final study analysis since early withdrawal could be related to the safety profile of the study drug. If a subject withdraws consent to participate in the study, attempts should be made to obtain permission to record at least survival data up to the protocoldescribed end of subject follow-up period. IT MUST BE A HIGH PRIORITY TO TRY TO OBTAIN AT LEAST SURVIVAL DATA ON ALL SUBJECTS LOST TO FOLLOW-UP AND TO NOTE WHAT METHODS SHOULD BE USED BEFORE ONE CAN STATE THE SUBJECT IS TRULY LOST TO FOLLOW-UP (e.g. number of phone calls to subject, phone calls to next-of-kin if possible, certified letters, etc.). Study Drug Description This section should be a very brief synopsis of section 1.2 “Investigational agent”, along with how the how the drug product will appear (e.g. as tablets or capsules of “X”mg, as a liquid with “X”mg dissolved in 10ml 5% dextrose and water, etc.) Treatment Regimen Describe dose, route of administration, and treatment duration. Method for Assigning Subjects to Treatment Groups Describe how a randomization number and associated treatment assignment will be made. This could be selection of a sequentially numbered drug kit/box, or communication with a randomization center that assigns a number associated with a specific treatment kit/box, etc. Preparation and Administration of Study Drug Describe in detail all the steps necessary to properly prepare study treatment. Include whether the drug preparation will be done in a pharmacy or by a study team member. Fully describe how the study treatment is to be administered. If study drug is stored, mixed/prepared or dispensed from the Investigational Pharmacy Service, that should be noted here, including the contact number to that office. Chapter 4: Protocol Design & Review Page 21 of 35 Office of Human Research Subject Compliance Monitoring Describe how the study team will assess and track subject compliance with the study treatment regimen, and what procedures must be followed for any subject who is significantly non-compliant with the study treatment regimen. Prior and Concomitant Therapy In this section, describe: • What prior and/or concomitant medical therapy will be collected (if applicable). • Which concomitant medicines/therapies (including rescue therapies) are permitted during the study • Which concomitant medicines/therapies are not permitted during the study (if applicable) Packaging • • • Describe how the study drug and any comparator agent will be packaged along with the amounts (e.g. “20 ml vials containing 30 mg”, or “bottles containing 30 tablets of …”, etc.) along with any associated labeling Describe if drug is to be shipped in bulk (e.g. Study drug will be shipped in boxes of 30 vials each, etc.) or as separate subject-specific kits/boxes When subject drug kits are constructed describe all the contents of the kit/box and associated labeling Blinding of Study Drug Describe how the drug is blinded (refer back to Section 8.4 “Unblinding Procedures”). Receiving, Storage, Dispensing and Return Receipt of Drug Supplies Describe how drug will be obtained i.e. what entity will ship the drug to the investigative site, and to what location at the site, (e.g. investigational pharmacy, etc.) Upon receipt of the of the study treatment supplies, an inventory must be performed and a drug receipt log filled out and signed by the person accepting the shipment. It is important that the designated study staff counts and verifies that the shipment contains all the items noted in the shipment inventory. Any damaged or unusable study drug in a given shipment (active drug or comparator) will be documented in the study files. Chapter 4: Protocol Design & Review Page 22 of 35 Office of Human Research The investigator must notify study sponsor of any damaged or unusable study treatments that were supplied to the investigator’s site. Storage Describe storage temperature requirements, whether supplies must be protected from light, and the location of the supplies (e.g. study pharmacy). Describe any special handling requirements during storage Dispensing of Study Drug Describe how the drug will be assigned to each subject and dispensed. This section should include regular drug reconciliation checks (i.e. how much drug was assigned and whether subjects actually received assigned dose or received dose properly, how much remains, how much drug was inadvertently damaged, etc. --- eg. “Regular study drug reconciliation will be performed to document drug assigned, drug consumed, and drug remaining. This reconciliation will be logged on the drug reconciliation form, and signed and dated by the study team.”) Return or Destruction of Study Drug This section should note the procedures for final reconciliation of the site’s drug supply at the end of the study, and whether study drug is to be shipped back to a source or destroyed on site. If drug is to be shipped back to a source, note the address and contact information here. At the completion of the study, there will be a final reconciliation of drug shipped, drug consumed, and drug remaining. This reconciliation will be logged on the drug reconciliation form, signed and dated. Any discrepancies noted will be investigated, resolved, and documented prior to return or destruction of unused study drug. Drug destroyed on site will be documented in the study files. Study Procedures In this section, describe all the procedures and treatments required at each visit, broken out by visit. Create a study procedures flowchart/table that describes the activities and procedures to be followed at each visit. Include this flowchart/table in the Attachment section and refer to that attachment in this section. Chapter 4: Protocol Design & Review Page 23 of 35 Office of Human Research Visit 1 Visit 2 etc. Statistical Plan Sample Size Determination Describe the statistical methods for determining the sample size for the study Statistical Methods Summarize the overall statistical approach to the analysis of the study. The section should contain the key elements of the analysis plan, but should not be a reiteration of a detailed study analysis plan. The full Statistical Analysis Plan can then be a “stand-alone” document that can undergo edits and versioning outside of the protocol and therefore not trigger an IRB re-review with every version or edit –AS LONG AS THE KEY ELEMENTS OF THE ANALYSIS PLAN DO NOT CHANGE. Be clear on primary as well as any applicable secondary analyses Subject Population(s) for Analysis This section should be very specific in defining the subject populations whose data will be subjected to the study analysis – both for the primary analysis and any applicable secondary analyses. Examples of such populations include: • All-randomized population: Any subject randomized into the study, regardless of whether they received study drug • All-treated population: Any subject randomized into the study that received at least one dose of study drug • Protocol-compliant population: Any subject who was randomized and received the protocol required study drug exposure and required protocol processing Safety and Adverse Events Definitions Chapter 4: Protocol Design & Review Page 24 of 35 Office of Human Research Adverse Event An adverse event (AE) is any symptom, sign, illness or experience that develops or worsens in severity during the course of the study. Intercurrent illnesses or injuries should be regarded as adverse events. Abnormal results of diagnostic procedures are considered to be adverse events if the abnormality: • results in study withdrawal • is associated with a serious adverse event • is associated with clinical signs or symptoms • leads to additional treatment or to further diagnostic tests • is considered by the investigator to be of clinical significance Serious Adverse Event Adverse events are classified as serious or non-serious. adverse event is any AE that is: • fatal • life-threatening • requires or prolongs hospital stay • results in persistent or significant disability or incapacity • a congenital anomaly or birth defect • an important medical event A serious Important medical events are those that may not be immediately life threatening, but are clearly of major clinical significance. They may jeopardize the subject, and may require intervention to prevent one of the other serious outcomes noted above. For example, drug overdose or abuse, a seizure that did not result in in-patient hospitalization, or intensive treatment of bronchospasm in an emergency department would typically be considered serious. All adverse events that do not meet any of the criteria for serious should be regarded as non-serious adverse events. Adverse Event Reporting Period The study period during which adverse events must be reported is normally defined as the period from the initiation of any study procedures to the end of the study treatment follow-up. For this study, the study treatment followup is defined as 30 days following the last administration of study treatment. Preexisting Condition A preexisting condition is one that is present at the start of the study. A preexisting condition should be recorded as an adverse event if the frequency, intensity, or the character of the condition worsens during the study period. Chapter 4: Protocol Design & Review Page 25 of 35 Office of Human Research General Physical Examination Findings At screening, any clinically significant abnormality should be recorded as a preexisting condition. At the end of the study, any new clinically significant findings/abnormalities that meet the definition of an adverse event must also be recorded and documented as an adverse event. Post-study Adverse Event All unresolved adverse events should be followed by the investigator until the events are resolved, the subject is lost to follow-up, or the adverse event is otherwise explained. At the last scheduled visit, the investigator should instruct each subject to report any subsequent event(s) that the subject, or the subject’s personal physician, believes might reasonably be related to participation in this study. The investigator should notify the study sponsor of any death or adverse event occurring at any time after a subject has discontinued or terminated study participation that may reasonably be related to this study. The sponsor should also be notified if the investigator should become aware of the development of cancer or of a congenital anomaly in a subsequently conceived offspring of a subject that has participated in this study. Abnormal Laboratory Values A clinical laboratory abnormality should be documented as an adverse event if any one of the following conditions is met: • The laboratory abnormality is not otherwise refuted by a repeat test to confirm the abnormality • The abnormality suggests a disease and/or organ toxicity • The abnormality is of a degree that requires active management; e.g. change of dose, discontinuation of the drug, more frequent follow-up assessments, further diagnostic investigation, etc. Hospitalization, Prolonged Hospitalization or Surgery Any adverse event that results in hospitalization or prolonged hospitalization should be documented and reported as a serious adverse event unless specifically instructed otherwise in this protocol. Any condition responsible for surgery should be documented as an adverse event if the condition meets the criteria for and adverse event. Neither the condition, hospitalization, prolonged hospitalization, nor surgery are reported as an adverse event in the following circumstances: • Hospitalization or prolonged hospitalization for diagnostic or elective surgical procedures for a preexisting condition. Surgery should not be reported as an outcome of an adverse event if the purpose of the surgery was elective or diagnostic and the outcome was uneventful. Chapter 4: Protocol Design & Review Page 26 of 35 Office of Human Research • • Hospitalization or prolonged hospitalization required to allow efficacy measurement for the study. Hospitalization or prolonged hospitalization for therapy of the target disease of the study, unless it is a worsening or increase in frequency of hospital admissions as judged by the clinical investigator. Recording of Adverse Events At each contact with the subject, the investigator must seek information on adverse events by specific questioning and, as appropriate, by examination. Information on all adverse events should be recorded immediately in the source document, and also in the appropriate adverse event module of the case report form (CRF). All clearly related signs, symptoms, and abnormal diagnostic procedures results should recorded in the source document, though should be grouped under one diagnosis. All adverse events occurring during the study period must be recorded. The clinical course of each event should be followed until resolution, stabilization, or until it has been determined that the study treatment or participation is not the cause. Serious adverse events that are still ongoing at the end of the study period must be followed up to determine the final outcome. Any serious adverse event that occurs after the study period and is considered to be possibly related to the study treatment or study participation should be recorded and reported immediately. Reporting of Serious Adverse Events Study Sponsor Notification by Investigator A serious adverse event must be reported to the study sponsor by telephone within 24 hours of the event. A Serious Adverse Event (SAE) form must be completed by the investigator and faxed to the study sponsor within 24 hours. The investigator will keep a copy of this SAE form on file at the study site. Report serious adverse events by phone and facsimile to: [Name of Sponsor contact phone fax] At the time of the initial report, the following information should be provided: Chapter 4: Protocol Design & Review Page 27 of 35 Office of Human Research • • • • • • Study identifier Study Center Subject number A description of the event Date of onset Current status • • • Whether study treatment was discontinued The reason why the event is classified as serious Investigator assessment of the association between the event and study treatment Within the following 48 hours, the investigator must provide further information on the serious adverse event in the form of a written narrative. This should include a copy of the completed Serious Adverse Event form, and any other diagnostic information that will assist the understanding of the event. Significant new information on ongoing serious adverse events should be provided promptly to the study sponsor IRB Notification by Investigator Reports of all serious adverse events (including follow-up information) must be submitted to the IRB within 10 working days. Copies of each report and documentation of IRB notification and receipt will be kept in the Clinical Investigator’s binder. FDA Notification by Sponsor The study sponsor shall notify the FDA by telephone or by facsimile transmission of any unexpected fatal or life-threatening experience associated with the use of the drug as soon as possible but no later than 7 calendar days from the sponsor’s original receipt of the information. If a previous adverse event that was not initially deemed reportable is later found to fit the criteria for reporting, the study sponsor will submit the adverse event in a written report to the FDA as soon as possible, but no later than 15 calendar days from the time the determination is made. Unblinding Procedures While the safety of the subject always comes first, it is still important to seriously consider if unblinding the study therapy is necessary to ensure a subject’s safety. This section should clearly describe the procedures for unblinding study therapy on a subject, including documentation of this in the subject’s source document. For investigators, other than the sponsor-investigator, state that the investigator must inform the sponsor of all subjects whose treatment was unblinded – and describe the timelines for such reporting. In most cases, the unblinding will be part of managing an SAE, and will be reported with the SAE, however, in cases where unblinding was not associated with an SAE, such actions should be reported in a timely manner. While there is no regulation governing this timeline, Chapter 4: Protocol Design & Review Page 28 of 35 Office of Human Research it is suggested to use the same timeline requirements for investigator reporting of SAEs, (i.e. notification of sponsor within 24 hours by phone or fax, followed by a written narrative of the event within 48 hours.) Stopping Rules In studies with a primary safety endpoint or studies with high risk to study subjects, rules should be developed that clarify the circumstances and procedures for interrupting or stopping the study. If a central Data and Safety Monitoring Board (DSMB) or Committee (DSMC) is set up for the study, the stopping rules should be incorporated into their safety analysis plan as well. Medical Monitoring It is the responsibility of the Principal Investigator to oversee the safety of the study at his/her site. This safety monitoring will include careful assessment and appropriate reporting of adverse events as noted above, as well as the construction and implementation of a site data and safety-monitoring plan (see section 9 Auditing, Monitoring and Inspecting). Medical monitoring will include a regular assessment of the number and type of serious adverse events. Internal Data and Safety Monitoring Board The description and requirements of this Board are an MHS local convention (i.e. is not a description from federal regulations or ICH guidelines). An Internal Data and Safety Monitoring Board (DSMB) is a group of professionals, experienced in clinical care and/or clinical research, assembled to provide additional safety and oversight to a clinical study. This type of oversight committee can include the sponsor and selected investigators, though must include other members who are independent of the study (can include members from within or external to the sponsor or investigator’s institution). The DSMB will look only at blinded data. This section should describe the above noted DSMB attributes. Also include: • Number of members and roles (e.g. clinicians, biostatisticians, bioethicists, etc.). It is not necessary to list the names or contact information of DSMB members in the protocol. However, the names and contact information of DSMB members should be reported to the EC/IRB and also maintained in the sponsor study file. • How often the DSMB will meet (and if by phone, face-to-face, or webassisted conferencing) • Type of safety information that will be assessed • How the safety data will be supplied to the DSMB • Summary of number and type of safety assessments the DSMB will conduct • How the DSMB will record the summary of its various meetings Chapter 4: Protocol Design & Review Page 29 of 35 Office of Human Research • • How the DSMB will report it’s findings and/or recommendations, and to whom Reference the DSMB charter in the Attachments section of the protocol If there is no internal DSMB, delete this section. Independent Data and Safety Monitoring Board The description and requirements of this Board are an MHS local convention (i.e. is not a description from federal regulations or ICH guidelines). A Data and Safety Monitoring Board (DSMB) is a group of professionals, experienced in clinical care and/or clinical research, assembled to provide additional safety oversight to a clinical study (and at least one biostatistician). This type of oversight differs from a Internal DSMB in that the Independent DSMB is independent of the investigator and sponsor, and is therefore generally also independent of the sponsor’s and investigator’s institution. Another important difference is that the DSMB can, and most typically does, conduct unblinded analyses. The DSMB should have a charter describing its function as well as an analysis plan for a pre-planned safety analysis(es). This section should describe the above noted DSMB attributes. Also include: • Number of members and roles (e.g. clinicians, biostatisticians, bioethicists, etc.) Since DSMBs typically review unblinded analyses, in that case, they must be independent of the study. Therefore names and/ or contact information of DSMB members should not be noted in the protocol. However, the names and contact information of DSMB members should be reported to the IRB and also maintained in the sponsor study file. • How often the DSMB will meet (and if by phone, face-to-face, or webassisted conferencing) • Type of safety information that will be analyzed • How the safety data will be supplied to the DSMB • Summary of number and type of interim analyses the DSMB will conduct, and who will conduct the actual analyses (including plans/safeguards to keep any unblinded data or DSMB analyses confidential • How the DSMB will record the summary of its various meetings • How the DSMB will report it’s findings and/or recommendations, and to whom • Reference the DSMB charter in the Attachments section of the protocol If there is no Independent DSMB, delete this section. Chapter 4: Protocol Design & Review Page 30 of 35 Office of Human Research Data Handling and Record Keeping Confidentiality Information about study subjects will be kept confidential and managed according to the requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Those regulations require a signed subject authorization informing the subject of the following: • What protected health information (PHI) will be collected from subjects in this study • Who will have access to that information and why • Who will use or disclose that information • The rights of a research subject to revoke their authorization for use of their PHI. In the event that a subject revokes authorization to collect or use PHI, the investigator, by regulation, retains the ability to use all information collected prior to the revocation of subject authorization. For subjects that have revoked authorization to collect or use PHI, attempts should be made to obtain permission to collect at least vital status (i.e. that the subject is alive) at the end of their scheduled study period. Source Documents Source data is all information, original records of clinical findings, observations, or other activities in a clinical trial necessary for the reconstruction and evaluation of the trial. Source data are contained in source documents Examples of these original documents, and data records include: hospital records, clinical and office charts, laboratory notes, memoranda, subjects’ diaries or evaluation checklists, pharmacy dispensing records, recorded data from automated instruments, copies or transcriptions certified after verification as being accurate and complete, microfiches, photographic negatives, microfilm or magnetic media, x-rays, subject files, and records kept at the pharmacy, at the laboratories, and at medico-technical departments involved in the clinical trial. Case Report Forms The study case report form (CRF) is the primary data collection instrument for the study. All data requested on the CRF must be recorded. All missing data must be explained. If a space on the CRF is left blank because the procedure was not done or the question was not asked, write “N/D”. If the item is not applicable to the individual case, write “N/A”. All entries should be printed legibly in black ink. If any entry error has been made, to correct such an error, draw a single straight line through the incorrect entry and enter the correct data above it. All such changes must be initialed and dated. DO NOT ERASE OR WHITE OUT Chapter 4: Protocol Design & Review Page 31 of 35 Office of Human Research ERRORS. For clarification of illegible or uncertain entries, print the clarification above the item, then initial and date it. Records Retention For non-FDA regulated studies, summarize the record retention plan applicable to the study (taking into account any applicable Department, Division or Research Center requirements) For FDA-regulated studies the following sample language is appropriate: It is the investigator’s responsibility to retain study essential documents for at least 2 years after the last approval of a marketing application in their country and until there are no pending or contemplated marketing applications in their country or at least 2 years have elapsed since the formal discontinuation of clinical development of the investigational product. These documents should be retained for a longer period if required by an agreement with the sponsor. In such an instance, it is the responsibility of the sponsor to inform the investigator/institution as to when these documents no longer need to be retained. Study Monitoring, Auditing, and Inspecting Study Monitoring Plan This study will be monitored according to the monitoring plan in Attachment ___. The investigator will allocate adequate time for such monitoring activities. The Investigator will also ensure that the monitor or other compliance or quality assurance reviewer is given access to all the above noted study-related documents and study related facilities (e.g. pharmacy, diagnostic laboratory, etc.), and has adequate space to conduct the monitoring visit. Auditing and Inspecting The investigator will permit study-related monitoring, audits, and inspections by the IRB, the sponsor, government regulatory bodies, and Memorial Healthcare System compliance and quality assurance groups of all study related documents (e.g. source documents, regulatory documents, data collection instruments, study data etc.). The investigator will ensure the capability for inspections of applicable study-related facilities (e.g. pharmacy, diagnostic laboratory, etc.). Chapter 4: Protocol Design & Review Page 32 of 35 Office of Human Research Participation as an investigator in this study implies acceptance of potential inspection by government regulatory authorities and applicable MHS compliance and quality assurance offices. Ethical Considerations This study is to be conducted according to US and international standards of Good Clinical Practice (FDA Title 21 part 312 and International Conference on Harmonization guidelines), applicable government regulations and Institutional research policies and procedures. This protocol and any amendments will be submitted to a properly constituted Institutional Review Board (IRB), in agreement with local legal prescriptions, for formal approval of the study conduct. The decision of the IRB concerning the conduct of the study will be made in writing to the investigator and a copy of this decision will be provided to the sponsor before commencement of this study. The investigator should provide a list of IRB members and their affiliate to the sponsor. All subjects for this study will be provided a consent form describing this study and providing sufficient information for subjects to make an informed decision about their participation in this study. See Attachment ___ for a copy of the Subject Informed Consent Form. This consent form will be submitted with the protocol for review and approval by the IRB for the study. The formal consent of a subject, using the IRB-approved consent form, must be obtained before that subject is submitted to any study procedure. This consent form must be signed by the subject or legally acceptable surrogate, and the investigator-designated research professional obtaining the consent. Study Finances Funding Source This section should describe how the study will be financed, but should not contain specific dollar amounts (e.g. “This study is financed through a grant from the US National Institute of Health”, or “… a grant from the American Heart Association”, etc.) Conflict of Interest Any investigator who has a conflict of interest with this study (patent ownership, royalties, or financial gain greater than the minimum allowable by their institution, etc.) must have the conflict reviewed by a properly constituted Conflict of Interest Committee with a Committee-sanctioned conflict management plan that has Chapter 4: Protocol Design & Review Page 33 of 35 Office of Human Research been reviewed and approved by the study sponsor prior to participation in this study. All Memorial Healthcare System (MHS) investigators will follow the MHS conflict of interest policy. Subject Stipends or Payments Describe any subject stipend or payment here. If there is no subject stipend/payment, delete this section. Publication Plan This section should include the requirements any publication policies of MHS. If, in addition to the sponsor-investigator, other investigators are involved with the study, identify who holds the primary responsibility for publication of the any results of the study. Also define the need to first obtain approval from the primary responsible party before any information can be used or passed on to a third party. Delete or modify the following sample language: Neither the complete nor any part of the results of the study carried out under this protocol, nor any of the information provided by the sponsor for the purposes of performing the study, will be published or passed on to any third party without the consent of the study sponsor. Any investigator involved with this study is obligated to provide the sponsor with complete test results and all data derived from the study. References This is the bibliography section for any information cited in the protocol. It should be organized as any standard bibliography. 1. Author, Title of work, periodical and associated information. 2. Author, Title of work, periodical and associated information. Attachments This section should contain all pertinent documents associated with the management of the study. The following list examples of potential attachments: • Investigator Agreement (for any investigator, other than sponsorinvestigator, who participates in the study) • Sample Consent Form • Study Procedures Flowchart/Table • Core Lab Instructions To Investigators Chapter 4: Protocol Design & Review Page 34 of 35 Office of Human Research • • • Specimen Preparation And Handling (e.g. for any specialized procedures that study team must follow to process a study specimen, and/or prepare it for shipment) Drug Conversion Plan (e.g. if there is a special regimen for transitioning a subject from their baseline medication over to study medication) Antidote Preparation And Delivery (e.g. special instructions for preparing and delivering any therapy designed to reverse the effects of the study drug, if applicable) Chapter 4: Protocol Design & Review Page 35 of 35 Office of Human Research Chapter 5: Research Involving Drugs and Devices Part I: Investigational Drug Studies One of the Food and Drug Administration's (FDA) primary mechanisms for ensuring the safety of research subjects is through an Investigational New Drug Application (IND). An IND Application is a request for authorization from the FDA to administer an investigational drug or biological product to humans. The IND provides assurance that the investigational product has sufficient preclinical safety data before it is used. The IND holder is the person or company who has filed the IND with the FDA. The IND Holder, often referred to as the Regulatory Sponsor, holds an additional set of responsibilities. Essentially, the IND holder is responsible for keeping the FDA informed of safety data from the study. This is critical for monitoring the safety of a drug. The FDA may be receiving multiple safety reports of a drug from several IND studies being conducted across the country and this allows them to identify safety trends more quickly. 1. Clarifying the "New" in IND The term IND can be misinterpreted, leading researchers to conclude that if the drug they are studying is already approved by the FDA, it is not a "new" drug and, therefore, does not need an IND Application. THIS IS INCORRECT! There are many other considerations for whether a drug being investigated is "new". The FDA approves a drug as safe with any or all of the following specifications. Altering these specifications could result in the FDA determining the drug to be "new". • "New" route of administration • "New" dose or duration of exposure • "New" form of the drug (e.g. capsule vs. tablet) • "New" treatment indications (e.g. target disease, age, gender) • "New" use with concomitant meds The FDA-approved labeling includes chemical structure, preclinical and human safety information, as well as dosing information. A study that uses a "new" aspect of the drug's use (i.e. different indication, dose, population, etc.) usually requires the filing of an IND. Therefore, an IND can be required for studies of a drug that is already approved for marketing. In most situations where the study is sponsored by a pharmaceutical company, the sponsor holds the IND with the FDA for the investigational product. In this case, the PI holds responsibility for communicating with the sponsor in a timely manner so the sponsor can communicate in turn with the FDA. When there is not an IND in place for a drug study sponsored by a pharmaceutical company, the researcher should consult with the Office of Human Research. Chapter 5: Research Involving Drugs and Devices Page 1 of 8 Office of Human Research Any investigator-initiated research study involving a drug or device should consult with the Office of Human Research (OHR) to determine whether or not an IND application needs to be filed. If it is possible that an IND exemption is appropriate for a study, the researcher should complete the IND Determination Assessment Form and submit it to the Office of Human Research for final determination. For investigator-initiated clinical research involving drugs, the IRB requires either an IND or Documentation of Exemption through a written communication from the FDA. For more information regarding the IND process, please refer to the FDA website: Investigational New Drug Application 2. IND Facts Did you know? • A single IND can have multiple projects/studies running under it. • For investigator-initiated research in which an IND is required, the investigator may be able to reference an existing IND to support the preclinical requirements of their application. • The FDA grants INDs, but does not "approve" specific studies. Therefore, an IND study should never be referred to as "FDA-approved." • "Acknowledgement" (rather than approval) of IND research comes in the form of non-objection to a study. • Unless otherwise noted, a study may proceed 30 days after the receipt date on the FDA's IND acknowledgement letter. The letter acknowledges receipt of an IND application. 3. IND Submission The IND application is prepared using FDA Forms 1571 and 1572. The required information includes: • Sufficient preclinical data, including toxicity data • Details of the chemistry, manufacturing and controls to provide adequate quality control information for the production of the agent and to describe the mechanism of action of the agent • Background and rationale for intended clinical use • Proposed protocol for Phase I human use The instructions and FDA Forms 1571 and 1572 can be found online at FDA Forms. The Office of Human Research can assist in providing essential elements, guidance and formatted documents in which to prepare an IND submission to the FDA. Chapter 5: Research Involving Drugs and Devices Page 2 of 8 Office of Human Research 4. IND Holder Responsibilities The IND holder is responsible for: • Selecting qualified investigators • Ongoing monitoring of all studies under the IND • The validity of the data from all sites conducting research under the IND • Maintaining adequate records of receipt, shipment, and disposition of the investigational drug • For multi-site studies, ensuring that all sites are kept informed of adverse events and safety updates • Communication with the FDA of any protocol changes, drug changes, and safety data. The Office of Human Research provides a detailed outline of IND Holder Responsibilities in the form of a checklist. Part II: Investigational Device Studies An Investigational Device Exemption (IDE) is the medical device equivalent of an IND Application for drug studies. The IDE application is a request to the FDA for authorization to use an unapproved medical device in humans. An Investigational Device Exemption is required when the study poses a Significant Risk to participants. This categorization is determined by the IRB, although the FDA makes the ultimate decision in determining whether a device study poses a Significant or Non-Significant Risk. The risk determination should be based on the proposed use of a device in a study, NOT on the device alone. 5. Significant Risk (SR) Device Study An SR Device presents a potential risk to the health, safety, or welfare of a subject AND is • An implant, or • Used in supporting or sustaining human life, or • Of substantial importance in diagnosing, curing, mitigating, or treating disease, or otherwise prevents impairment of human health, or • Otherwise presents a potential serious risk to the health, safety, or welfare of a subject. • An IDE Submission to the FDA AND IRB approval is required prior to initiation of an SR device study. An IDE Submission to the FDA AND IRB approval is required prior to initiation of an SR device study. Chapter 5: Research Involving Drugs and Devices Page 3 of 8 Office of Human Research 6. Non-Significant Risk (NSR) Device Study For device studies that do not meet the criteria of Significant Risk, the IRB can approve the study without an IDE. The study may begin immediately after IRB approval Please refer to SOP 201 Attachment H to determine if an IDE would be required. Additional IDE Resource from FDA: • 7. Instructions for IDE Application: IDE Application Investigator's Brochure The Investigator's Brochure is a compilation of all preclinical, clinical and non-clinical data on the investigational product that are relevant to human subjects. Its function is to assist investigators in understanding the rationale behind the protocol, particularly dose, dose frequency/interval, methods of administration, overdosing information, and safety reporting/monitoring. The type and extent of information available will vary with the stage of development of the investigational product. While there is no federal regulatory requirement that the Investigator's Brochure be submitted to the Institutional Review Board (IRB), there are regulatory requirements for submission of specific product information that can normally be found in the Investigator's Brochure. If, for instance, a study involves an approved drug that does not require an IND , the FDA-approved labeling found in the Physician's Desk Reference (PDR) or package insert can be used to provide the required regulatory information to the IRB. 8. Special Provisions for Drug/Device Research In certain research and clinical practice scenarios, investigational products may be used to try to treat serious or life-threatening conditions either for a single subject or for a group of subjects. Individuals may accept greater risks from investigational products that offer the possibility of treating life-threatening, rare, or debilitating illnesses when they have no viable alternatives. Under these circumstances, federal regulations provide mechanisms to expand access to promising investigational products without compromising subject protection measures. These mechanisms include: • Humanitarian Device Exemption (HDE) • Treatment IND o Group C Treatment IND • Compassionate Use / Single Patient Use • Emergency Use Chapter 5: Research Involving Drugs and Devices Page 4 of 8 Office of Human Research Comparison of Special Research Provisions Humanitarian Treatment Device Exemption IND (HDE) IND/IDE Number Emergency Use Yes from sponsor, manufacturer, or FDA; Prospective IRB approval required Retrospective IRB notification Compassionate Use Yes N/A No Yes Informed Consent Yes** ** exception found under emergency use # of Patients multiple single subject (in rare instances may be multiple subjects) 8.1 Humanitarian Device Exemption (HDE) A Humanitarian Device Exemption (HDE) is a mechanism used by the FDA to provide access to devices that are developed to treat rare diseases and conditions. These devices are listed on the FDA website (Designating Humanitarian Use Devices) and are termed Humanitarian Use Device (HUD). By definition a HUD is intended to treat or diagnose a disease or condition that affects less than 4,000 individuals in the United States per year. HUDs are exempt from the effectiveness requirements normally required by the FDA for approval. Investigations involving HUDs usually occur through standard research protocols, which must be IRB approved. If an investigator wishes to use a HUD for treating a single individual, the investigator must follow the procedures outlined below for compassionate use or emergency use. 8.2 Treatment INDs A Treatment IND is a mechanism for providing eligible subjects with investigational drugs for the treatment of serious and life-threatening illnesses for which there are no satisfactory alternative treatments. A Treatment IND may be granted by the FDA after sufficient data have been collected to show that the drug "may be effective" and does not have unreasonable risks. A sponsor applies a Treatment IND to an existing IND. Treatment protocols are planned and cover an unspecified number of patients. Chapter 5: Research Involving Drugs and Devices Page 5 of 8 Office of Human Research There are four requirements: i. The drug is intended to treat a serious or immediately life-threatening disease ii. There is no satisfactory alternative iii. The drug is already under investigation iv. The sponsor is actively pursuing marketing approval Treatment IND protocols require full IRB review. The process for obtaining IRB approval is the same as that for standard research protocols. Please refer to the FDA website for more information: Treatment INDs 8.3 “Group C” Treatment IND The "Group C" treatment IND was established through an agreement between the FDA and the National Cancer Institute (NCI). The Group C program is a means for the National Institute of Health to distribute investigational agents to oncologists for the treatment of cancer under NCI protocols outside a controlled clinical trial. Most Group C drugs have undergone Phase III testing and have some preliminary evidence of efficacy in a specific tumor type. 8.4 Compassionate Use / Single Patient Use In specific situations, a physician may be granted special permission to use an investigational product for treatment purposes. Compassionate use involves a single patient who is unresponsive to standard therapy or for whom no standard therapy is available and there is reasonable scientific evidence to support the use of the investigational product. (If the situation is a life-threatening emergency, emergency use guidelines apply.) Compassionate Use is not defined by the FDA; it falls under Treatment IND or Humanitarian Device Exemption (HDE) regulations. However, an investigator must follow additional Penn procedures in order to obtain approval to use an investigational product for a single patient use (see procedures that follow). 8.5 Emergency Use Emergency Use is defined as the use of an investigational product in a human subject with a life-threatening condition in which no standard acceptable treatment is available and in which there is insufficient time to obtain IRB approval. All of the following conditions must be met to justify emergency use: i. There is a high likelihood of death unless the course of the disease is interrupted ii. No alternative method or recognized therapy is available that provides an equal or greater likelihood of saving the subject's life Chapter 5: Research Involving Drugs and Devices Page 6 of 8 Office of Human Research iii. The subject is in a life-threatening situation requiring intervention before review at a convened meeting. Data from emergency-use situations may not be utilized for investigational purposes. FDA regulations require that any subsequent use of the investigational product have prospective IRB approval. Please refer to the FDA website for more information: Single Use IND for Compassionate or Emergency Use To obtain approval for Compassionate or Emergency Use • Contact the manufacturer of the investigational product and request permission to use the drug/device under the manufacturer's IND, IDE, or HDE. • If the sponsor requests acknowledgement that the IRB is aware and recognizes such emergency use, an acknowledgement letter can be obtained from the IRB • If an IND/IDE/HDE does not exist OR if sponsor is unwilling to sponsor a physician under an existing IND, the FDA may issue an IND/IDE/HDE directly to the physician. Contact the OHR for assistance in reaching the appropriate FDA department. A licensed physician must take responsibility for the study. This includes a commitment to the manufacturer to complete data collection forms, if applicable. For a project involving an investigational drug, the investigator must submit an FDA-1572 and Curriculum Vitae. • A consent form must be prepared. Most manufacturers should be able to provide a template; however, the consent must conform to MHS IRB standards. • Submit the protocol/treatment plan to the IRB for approval. Or, in an emergency situation in which insufficient time is available, notify the IRB of the planned use and obtain an independent assessment by a physician uninvolved with the patient's care confirming the emergency status. • Investigational devices may be sent to the investigator's office or clinic. • Investigational drugs should be shipped to the appropriate Investigational Drug Services Pharmacist • Obtain written informed consent from the subject prior to administering the investigational product. Exception: subjects who are in need of emergency medical intervention but cannot give informed consent because of their life-threatening medical condition and who do not have a proxy to represent them. In such circumstances, the investigator and a second physician who is not otherwise participating in the investigation or care of the patient must document: o the criteria that the patient met for emergency use of investigative product o AND the lack of alternatives o AND the inability to obtain consent from the subject Chapter 5: Research Involving Drugs and Devices Page 7 of 8 Office of Human Research o AND the methods used to reach a legal representative and/or relatives o AND the lack sufficient time to obtain the aforementioned consent • Place a copy of the protocol/treatment plan in the location where the subject is being treated. • A written report must be sent to the IRB within 5 working days of the start of treatment. This letter must include 1-2 paragraphs about the situation that required treatment, the protocol, and a copy of the signed consent form. Chapter 5: Research Involving Drugs and Devices Page 8 of 8 Office of Human Research Chapter 6: Monitoring Plan Development The monitoring of a clinical trial is an essential element of study processes designed to ensure the protection of the subject's rights, the safety of subjects enrolled in the trial and the integrity and quality of the resulting data. It is important to note that monitoring encompasses both data and safety oversight. Both activities complement one another to ensure that the study is safe and ethical. The degree of oversight will vary based upon the risk level, the size and complexity of the study, the nature of the investigation, the regulatory requirements, and the study sponsor. A monitoring plan specifies a course of action to oversee the integrity of the study data. This plan typically details who will be responsible for monitoring (roles), what will be monitored (scope), and when monitoring will occur (timing). 1. Roles The Principal Investigator is always responsible for ensuring that the protocol is followed, the data is accurate, and the research subjects at his or her site are safe. The Principal Investigator may designate some responsibilities to other study team members, but ultimately he or she will be held accountable for their activities. Depending on the risk level of the study, the following individuals or groups may review the adverse events, safety data, and research activities and recommend a course of action to ensure the safety of research participants. 1.1 Study Monitor or Clinical Research Associate (CRA) The primary role of a study monitor is to verify data integrity and compliance to the protocol. A study monitor reviews source data/medical records, Case Report Forms, and regulatory documents for accuracy, completeness, and legibility in accordance with the study protocol. A monitor need not be a person qualified to diagnose and treat the disease or other condition under investigation. 1.2 Medical Monitor The medical monitor is a licensed physician with clinical expertise in the area under investigation. Typically, the PI is the medical monitor, however when the PI is not an MD, a physician must be involved as the medical monitor. The medical monitor reviews and interprets adverse events, relevant animal and toxicology studies, and other safety data throughout the conduct of a research study and issues recommendations to maintain subject safety. The medical monitor's role and responsibilities within the research project should be clearly outlined prior to initiation. NOTE: In cancer studies, the medical monitor must be independent from the study. 1.3 Safety Monitoring Committee Chapter 6: Monitoring Plan Development Page 1 of 3 Office of Human Research A Safety Monitoring Committee is a group of individuals responsible for the oversight of the study. The terms Safety Monitoring Committee may be used to refer to a less formal group than a Data and Safety Monitoring Board, though the terms are sometimes used interchangeably. 1.4 Data and Safety Monitoring Board (DSMB) A Data and Safety Monitoring Board is an independent group of experts convened to protect the safety of research subjects and to ensure that the scientific goals of the project are being met. DSMBs are generally used in large multi-center studies, but may also be used in early-phase investigations of high risk medical interventions or studies with vulnerable populations. Factors that suggest a DSMB is needed: • A large study population • Multiple study sites • Highly toxic therapies or dangerous procedures • High expected rates of morbidity or mortality in the study population • High chance of early termination of the study. DSMBs should have a charter that outlines the structure and operation of the Board. A charter typically includes: the board's composition, operating procedures, frequency of ongoing monitoring, the data submitted to the DSMB, plans for statistical analysis and review, and the content of reports issued by the DSMB. The DSMB should have a broad multi-disciplinary representation including a biostatistician and a physician with relevant clinical expertise. The DSMB's analysis plan describing what data will be reviewed, how the data set will be prepared for analysis, and the specific type of analysis used to assess safety. Generally, these analyses are performed on un-blinded data. After conducting the planned analysis (or analyses), the DSMB should issue a report either permitting the study to continue or recommending halting the study. Typically, the DSMB disseminates an 'open' report that contains aggregate data and administrative recommendations while also maintaining a 'closed' report that contains confidential data, un-blinded statistical reviews, and individual discussions. 2. Scope Items typically monitored include study regulatory files, Case Report Forms, tracking logs (e.g. for enrollment, drug storage and dispensing, etc.), subject Informed Consent Forms, and study source documents. The monitoring plan should include a plan for collecting study data (Case Report Form). The plan should outline the procedures used to verify that the data collected on the CRF is correct and that the protocol has been followed. Chapter 6: Monitoring Plan Development Page 2 of 3 Office of Human Research The protocol defines procedures for reporting, reviewing, and analyzing safety data and plans for intervening (e.g. stopping rules or un-blinding procedures). The monitoring plan ensures that these procedures have been followed. 3. Timing The occurrence of monitoring activities depends primarily upon the risk of the study. The higher the risk to subjects, the more frequently monitoring should be conducted. Monitoring frequency will also depend upon the size of the research study, the accrual rate, and the complexity of the Case Report Form. In general, there is a need for on-site monitoring before, during, and after the study. Chapter 6: Monitoring Plan Development Page 3 of 3 Office of Human Research Chapter 7: Informed Consent Form Development The consent form is a document used to inform potential subjects about research participation. It is important to recognize that Informed Consent is an ongoing process that includes disclosure of information, comprehension, and voluntary choice. The consent form is used as a tool to help researchers fully disclose information. The elements of the consent form are specifically regulated in 45 CFR 46 and 21 CFR 50, as well as outlined in the Good Clinical Practice (ICH) Guidelines. The IRB scrutinizes the consent form during its review to ensure that the proper elements are present, the form is written in lay language, and no coercive or misleading statements are included. The investigator cannot employ the informed consent form until it has received final IRB approval. The MHS IRB (or any IRB of record) indicates this approval by stamping the consent form with valid dates. An informed consent template to assist researchers in developing an Informed Consent Form that is understandable, written in lay language, and includes all of the required elements of the consent form can be found in this Chapter, or by referring to SOP 601 Attachment A. Please contact the OHR for an electronic version of the template. For non-investigator-initiated studies, the research sponsor may provide investigators with a consent form template. This template should be integrated with the Memorial Healthcare System IRB’s informed consent requirements and approved language. The revised consent should be forwarded to the sponsor for comments and approved prior to submitting to the IRB. At the IRB Subcommittee, further consent form changes may be recommended and should be incorporated before submission to the sponsor and IRB final submission. 1. General ICF Writing Tips Do's and Don'ts • DO view the consent form as an instructional tool rather than a legal tool • DO, if using published data that is not part of the FDA-approved label to discuss safety and/or efficacy, clarify that this is "research data" and not FDA-endorsed or FDA-approved as evidence of safety or efficacy of the study agent • DON'T make claims that a study is FDA-approved. The FDA does not "approve" non-significant risk device studies; it only approves medical treatments and devices for marketing. • DON"T make statements that would suggest a subject is waiving his/her rights in any way (refer to Exculpatory Language below). • DON'T make statements that would suggest a subject, the PI or study sponsor is relieved from liability for negligence (refer to Exculpatory Language below). • DON'T make claims about safety/efficacy of the study agent that haven't been demonstrated (i.e. approved by the FDA), or are not applicable to the study population. Chapter 7: Informed Consent Form Development Page 1 of 18 Office of Human Research 2. Content • • • • 2.1 Be brief, but include complete information o sentences should be short, simple, and direct o paragraphs should convey one idea at a time Be comprehensible o written towards a reading age commensurate with the proposed subjects. It is recommended that consent forms not exceed the 8th grade reading level in most cases. o use lay language and avoid technical words or jargon o where use of technical terms are unavoidable, provide clear definitions o use the same words consistently when referring to a condition or treatment o use words that are concrete rather than abstract o use verbs that are active rather than passive Help people remember information o state ideas explicitly rather than implicitly o restate important points throughout and/or summarize critical study issues at the beginning or end o highlight important points by underlining, bolding, or boxing information Facilitate discussion o organize the form logically o use numbering or lists when presenting facts o use charts and visual aids Lay Term Glossaries A number of institutions have developed lay term glossaries, which may be helpful in defining and describing procedures and risks in informed consent forms. Please note that the IRB has not reviewed or approved any of these definitions, and so use of these does not guarantee IRB acceptance of the definitions. • PRISM: http://www.nhlbi.nih.gov/crg/pdf-docs/ghchs_readability_toolkit.pdf • Stanford: Stanford Glossary of Terms for Lay Terms for Informed Consent • Partners Human Research Committee: Alternative Terms • National Cancer Institute: NCI Dictionary • University of Kentucky: Glossary of Lay Terms • Lawrence Berkley National Laboratory: Glossary of Lay Terminology Chapter 7: Informed Consent Form Development Page 2 of 18 Office of Human Research 3. Exculpatory Language The consent form is not a legally binding contract. The researcher should view the consent form as an instructional tool rather than a legal document. Exculpatory language is not allowed, which means the consent form cannot waive or appear to waive legal rights or release the investigator, sponsor, or institution from liability for negligence. 3.1 Examples of Exculpatory Language: In the following examples, subjects are being asked to agree with and accept these unfavorable conditions. • I waive any possibility of compensation, including any right to sue, for injuries that I may receive as a result of participation in this research. • If you suffer a research-related injury, neither the institution nor the investigator can assume financial responsibilities for the expenses of treatment for such injury. • In the event that you suffer a research-related injury, your medical expenses will be your responsibility or that of your third party payer. 3.2 Examples of Acceptable Language In the following examples, the intent and policies are set forth in a factual manner, but subjects are not being asked to agree with or accept the conditions as part of their participation in the research. • Although future research that uses your samples may lead to the development of new products, you will not receive payments for these new products. • By agreeing to this use, you are giving up all claims to any money obtained by the researchers from commercial or other use of these specimens. • By consenting to participate in this research, I give up any property rights I may have in bodily fluids or tissue samples collected during this research. • In the event that you suffer a research-related injury, your medical expenses will be your responsibility or that of your third-party payer. You are not giving up any legal rights to sue for injury related to malpractice, fault, or blame on the part of those involved in research. Examples adapted from Office for Human Research Protections (OHRP) Cooperative Oncology Group Chairpersons Meeting guidance document "'Exculpatory Language’ in Informed Consent." OHRP Exculpatory Language in Informed Consents 4. Format • The second person pronoun (you and your) should be used consistently throughout the document. Chapter 7: Informed Consent Form Development Page 3 of 18 Office of Human Research • Type should be easy to read. o • • Use standard margins. o White space increases readability. o Do not sacrifice font size or margin space for fewer numbers of pages. Leave paragraphs unjustified. Double-space between paragraphs. o • 5. This reduces the speed of comprehension and reading. Place the Study Title, Principal Investigator, and Institution in the header of each page. o • This increases the speed and ease of reading. Avoid using sentences in all capital letters or italics. o • Use sans serif fonts, legible size (e.g. Arial 12 pt, Times Roman 12 pt, Verdana 12 pt). Consider adding the IRB Protocol Number as an additional identifier. Place the Page # of # and the Consent Form Version in the footer of each page. Elements of Informed Consent The elements of the Informed Consent Form required by Federal regulations and GCP guidelines are listed below. The Common Rule, FDA regulations and ICH guidelines have been harmonized to contain the same requirements (45 CFR 46.116, 21 CFR 50.25, ICH E6 4.8.10). • A statement that the study involves research. • An explanation of the purpose of the research. • An explanation of the expected duration of the subject's participation. • A description of the procedures to be followed. • *If applicable, include: o Aspects considered experimental o Procedures to be followed, including all invasive procedures and treatments o Probability for random assignment to each treatment. o Subject's responsibilities. • A description of any reasonably foreseeable risks or discomforts. • A description of any benefit to the subject or to others which may reasonably be expected from the research. When there is no intended clinical benefit to the subject, the subject should be made aware of this. • A disclosure of appropriate alternative procedures or courses of treatment, if any, that may be advantageous. Chapter 7: Informed Consent Form Development Page 4 of 18 Office of Human Research • • If applicable for a clinical trials regulated by the FDA, include verbatim wording, “A description of this clinical trial will be available on http://www.ClinicalTrials.gov, as required by U.S. Law. This Web site will not include information that can identify you. At most, the Web site will include a summary of the results. You can search this Web site at any time.” • If applicable, include: o Important risks and benefits of alternatives. o The option of choosing "no treatment" or doing nothing. • A statement describing the extent, if any, to which confidentiality of records will be maintained. • If applicable, include: o The possibility that the government agencies (e.g. FDA, NIH, etc.) may inspect records. o Records will be kept confidential, and to the extent permitted by law and/or regulations, will not be made publicly available. o Published results will not identify the subject. • For studies involving more than minimal risk, an explanation as to whether any treatment or compensation is available if injury occurs. • An explanation of whom to contact for answers to pertinent questions about the research, the research subject's rights, and in the event of a research-related injury. • A statement that participation is voluntary. • Statement that refusal to participate will involve no penalty/loss of benefits. A statement that the subject may discontinue at any time without penalty/loss of benefits. 5.1 When relevant, the informed consent must also include the following elements: • Unforeseeable risks to embryo, fetus, or nursing subject. • Anticipated circumstances under which a subject's participation may be terminated without regard to the subject's consent. • Any additional expenses that may result from participation in research. • *If applicable, include: o The anticipated prorated payment, if any, to the subject. • The consequences of a subject's decision to withdraw. A description of the procedures for termination. • A statement that the subject will be told of significant new findings or information that may be relevant to the subject's continued willingness to participate. Chapter 7: Informed Consent Form Development Page 5 of 18 Office of Human Research • Approximate number of subjects involved in the study. • That the monitor(s), the auditor(s), the IRB, and the regulatory authorities will be granted direct access to the subject’s original medical records for verification of clinical trial procedures and/or data, without violating the confidentiality of the subject, to the extent permitted by applicable laws and regulations. • It is recommended that the investigator inform the subject’s primary physician about the subject’s participation in the study if the subject has a primary physician and if the subject agrees to the primary physician being informed. • These elements are specific to ICH E6 Guidelines 6. Informed Consent Template The MHS IRB has created a template to aid in the construction of a research subject informed consent form. This standard form flows logically from a research subject perspective, and is designed to ensure all required elements of informed consent are captured as well as to improve the ease of IRB review. Please contact the OHR or MHS IRB for an electronic version of the Informed Consent template. The elements of the Informed Consent Form include the following: WHAT IS THIS STUDY ABOUT? • The subject is being invited to participate in a research study and why they are being asked to volunteer. • Participation is voluntary • The subject will get a copy of the consent form and should ask questions • The subject will be asked to sign this form if consent is given to participate • OPTIONAL: Can include some information about the study such as "a study of "X" (drug or device, etc.) in patients with "Y" disease We are asking you to take part in a research study. This form gives you information that will help you decide. If you do decide to take part, you will be given a copy of this form to keep. A research study tests treatments. The treatments could be study drugs or devices. They could be new ways to combine treatments to find out if the treatments are safe and if they work well for a particular disease. WHY IS THIS STUDY BEING DONE? • A concise explanation of the purpose of the research, incorporating any intent to assess safety +/- efficacy • A Clarification that the drug/device is investigational. Can note that the drug/device is approved for another indication if applicable, but must clarify that the use of the drug/device in this study is experimental Chapter 7: Informed Consent Form Development Page 6 of 18 Office of Human Research HOW MANY PEOPLE WILL TAKE PART IN THIS STUDY? • Total number of subjects in study • Number of subjects expected at MHS WHAT WILL HAPPEN TO ME ON THIS STUDY? • A high level overview of the major elements of the study and what is expected of the subject (i.e. note here only the major procedures and milestones) • Following the overview, provide a full list of procedures/tests by lay-term names; Consider including number of times each test will occur, amount, exposure if appropriate, etc. in easy lay terms • Describe each test/procedure in lay terms • Clearly identify which procedures are experimental • OPTIONAL: May be complimented by a simple table or chart and/or other additional materials may be inserted here or given as a handout; any such materials require IRB approval HOW LONG WILL I BE ON THIS STUDY? • Expected duration of a subject's involvement with the study • Expected total duration of study WHAT ARE THE RISKS OF THE STUDY? • Known risks from the study agent. May also be detailed in chart format and additional material inserted here or given as a handout. Any such materials require IRB approval. • Risks, discomforts/inconveniences of study-related procedures noted in the section “What am I being asked to do?”. If standard of care is testing is being changed, describe any resultant risk, if applicable. May also be detailed in chart format and additional material inserted here or given as a hand out. Any such materials require IRB approval. • Clarify that if the subject is injured, they should inform treating physician that they are in a research study. • Include information on reproductive issues, if appropriate. NOTE: If male contraception methods or warnings are warranted, the appropriate information must be provided in this section as well. • Do not make statements of proven safety unless that safety data is part of FDAapproved labeling. If the labeling safety data does not include data in the proposed study population for this study, make clear that there is no safety data in the population under study. Chapter 7: Informed Consent Form Development Page 7 of 18 Office of Human Research • Include a statement that the research may involve risks that are currently unforeseeable. Childbearing risks: It is not known how this treatment might affect an unborn child. It is not known how this treatment will affect male sperm. This treatment will not be offered to females who are pregnant. Females able to have children must be tested to prove they are not pregnant before starting the study. If you sign, this means you agree you will not have sex unless you use a study doctor approved method of birth control during the study. (APPROPRIATE ONCOLOGY- If it applies to you, your study doctor will tell you about ways to keep eggs or sperm outside the body, so that you might still have a chance of having children if this treatment makes you unable to naturally have children. ONCOLOGY ENDS) Females taking part in the study promise not to breast feed during this study. You agree to notify the study doctor if you become pregnant during this study. WILL I BENEFIT FROM THIS STUDY? • If direct subject benefits can reasonably be anticipated as a result of participating in the protocol then describe these possible benefits. Conclude with the following standard clause: “You may not get any benefit from being in this research study.” • If direct subject benefits are NOT anticipated, then use the following standard clause “You are not expected to get any benefit from being in this research study.” • Anticipated benefits to society ARE THERE OTHER OPTIONS? • Information on other treatments available. • Alternatives to entering the study including, when appropriate, supportive care with no additional disease-directed therapy • A statement that they may discuss alternatives with their personal physician WILL MY MEDICAL INFORMATION BE KEPT PRIVATE? AUTHORIZATION (PERMISSION) TO USE OR DISCLOSE (RELEASE) IDENTIFIABLE HEALTH INFORMATION FOR RESEARCH This research study will use records of current and/or future identifiable health information. This information will come from the records of your hospital, doctors’ offices, clinics, or other places you get healthcare. This information also comes from your healthcare billing records or insurance records. It includes information about the Chapter 7: Informed Consent Form Development Page 8 of 18 Office of Human Research cost of your treatments and care. The information you allow to be disclosed and used is described in the “What will happen to me on this study?” section of the consent for this study. It is also the information described in the consent under the section about coverage of research-related injuries (if applicable). This information will be used for the purpose of meeting the goals of this study. You allow the use and disclosure of this information to: • __________________________________(SPONSOR OF RESEARCH); • _______________________(maker of the study drug or device), if applicable; • any other research company or person who has a contract with the sponsor; • agents of the sponsor; • the researchers, doctors taking part in the study and their assistants; • Memorial Healthcare System Institutional Review Board; • the Food and Drug Administration; • the National Cancer Institute (if NCI study); • the U.S. Department of Health and Human Services (if NIH) • People and organizations acting for any of the above. Other people or organizations who help with this research may also get your medical information. They may get your blood, or body tissue samples, or slides. These other people and organizations include central laboratories, central review centers, and central reviewers. If it applies to your case, you give permission to use or disclose information about: • Acquired Immunodeficiency Syndrome (AIDS) • Human Immunodeficiency Virus (HIV) infection • mental or behavioral health or psychiatric care • or treatment for drug or alcohol abuse. You are letting Memorial Healthcare System and your healthcare facilities and providers give this information to the people, organizations, and parties listed above. You are also allowing blood or body tissue samples to be sent to a central laboratory to help with this study. The term “Protected Health Information” means the information about your health that is protected under the law. It includes new and existing medical records and test results that contain information that could be used to identify you. It means medical records that include ways to identify you, such as your name; address; telephone number; date of birth; and/or medical record number. This may include information in your medical record and information created or collected during this study. It includes long-term information about your general health status and the status of your disease. Chapter 7: Informed Consent Form Development Page 9 of 18 Office of Human Research Federal and state laws require your records to be kept private. However, no one can promise complete confidentiality. Your Protected Health Information will sometimes be used or disclosed in the ways described in this form. In addition, after the researcher discloses your records to others then the law may no longer protect the privacy of your records listed above. The results of this study may be published, but those publications will not identify you. Scientific data from this study may be presented at meetings. It may be published so that the information may be used to help others. Your participation in the study will not be made known and will be kept strictly confidential. This authorization is voluntary. You do not have to give it. But, if you will not allow the use and disclosure of your identifiable health information, you will not be allowed to be part of this study. You can cancel this authorization at any time. But if you cancel after you have started the study, you will be removed from the study. Your canceling this authorization will not affect any use or disclosure made before the cancellation. That information will continue to be used in the study. Blood and body fluids you gave to the study may continue to be used. It will not change any action that anyone had made because he or she relied on your authorization. It means that no new Protected Health Information about you will be used or disclosed. You may cancel this authorization by giving a written notice to: Dr. Name Address City, State zip. “BLINDED STUDIES: Until this study is over, you will not be given study information about yourself. You will not be told which study treatment you are getting. That has been kept secret from you during the study so that your beliefs about the drug will not change the results. You will be able to get this information at the end of the study. END OF BLINDED STUDY” NON-BLINDED: You have the right to see and copy your records related to the study for as long as the study doctor has this information. You do not have the right to review or copy records kept by ___________(sponsoring agency) or other researchers associated with this study. You will not get the results from the special research tests done on your donated specimens. This authorization does not have a fixed ending date. It stays in effect until it is cancelled. WHAT ARE THE COSTS (PAYMENTS) ASSOCIATED WITH THIS STUDY? • Procedures or tests that will be covered by the study • Procedures or tests that are not covered by the study, stating how they will be paid for (i.e., third party payer (payor), etc.) • Description of any monetary compensation (*payments/stipend), if subjects are being compensated for their time and travel. If there is no compensation for participation in this study, state that here Chapter 7: Informed Consent Form Development Page 10 of 18 Office of Human Research • You and/or your health insurance may be billed for the costs of medical care during this study if these expenses would have happened even if you were not in the study, or if your insurance agrees in advance to pay. The study drug(s) are free. So are the tests and other procedures that are needed because of the study. All of your other medical care will be charged and paid for in the same way it would be if you were not part of the study. You will not be charged extra for taking part in the study. No one will pay you to take part in this study. The study sponsor will (or will not) pay your healthcare provider for his or her services to you as part of the study. These payments (may be more than his or her costs of taking part in the study or These payments will not be more than his or her costs of taking part in the study. If this is a concern to you, please feel free to discuss this with the study doctor or study coordinator. WHAT IF I AM INJURED FROM TAKING PART IN THIS STUDY? • Provide contact information for research-related injury (i.e. can refer to the contact information noted in Consent header, if appropriate) • Describe what treatment will be provided for research related injuries • Explain how treatment for research related injuries would be paid • Describe procedure for emergency care • OPTIONAL: Subject's responsibilities relating to research related injuries There is a risk you may be hurt by this study. If you are hurt, medical care will be provided to you. All of that medical care will be charged and paid for in the same way it would be if you were not part of the study. Neither the study sponsor, nor the investigating doctors, nor the Hospital will pay for that care. Signing this form does not take away any of your legal rights. It does not release anyone from liability for negligence. (Insert sponsor statements here or if no sponsor statement for coverage then include) Funds to pay for pain, expenses, lost wages, and other damages caused by the injury are not routinely available. If you need help paying for losses or care caused by such an injury, ask the study doctor or a social worker about how you might get help. WHAT ARE MY RIGHTS AS A STUDY PARTICIPANT? • Note that the subject can elect to leave the study at any time • If early withdrawal could expose the subject to medical risks, describe and how those risks will be minimized or prevented (e.g. in a hypertensive study, it may be necessary to wean a subject off of the study medication or to transition them to alternate therapy) • A statement that if information about the safety of the study drug/device/study is discovered during the study, which may affect one's willingness to participate, the subject will be notified Chapter 7: Informed Consent Form Development Page 11 of 18 Office of Human Research You do not have to be in this research study. You can agree to be in the study now and change your mind later. Your decision will not affect your regular care. Your doctor’s attitude toward you will not change. There will be no penalty or loss of benefits. You are free to seek care from a doctor of your choice at any time. You will continue to receive medical care. You may be taken out of the study if: 1. Staying in the study would be harmful to you. 2. You need treatment not allowed in the study. 3. You fail to follow instructions. 4. You become pregnant (females). 5. The study is cancelled. We may learn about new things that might make you want to stop being in the study. If this happens, you will be informed. You can then decide if you want to continue to be in the study. (If appropriate, “Even if you stop taking part in the study your medical information will still be collected and shared as part of the study. This is to try to find out the long term results of the care you got while you were part of the study. However, none of your future medical information will be used or shared as part of the study, if you request that.”) WHAT IF I HAVE QUESTIONS OR PROBLEMS? The Principal Investigator, _________, can be contacted at (address) or (telephone number) (e-mail address). Ask the Principal Investigator any questions you have about the research. Let the Principal Investigator know if you have a research-related problem or injuries at any time during the study. If you have any questions about your rights in this study, you may contact in writing or by telephone: The Chairman of the Institutional Review Board Memorial Healthcare System 3501 Johnson Street, Hollywood, Florida 33021 Telephone number (954) 265-1857. WHERE CAN I GET MORE INFORMATION? (Cancer studies) You may call the National Cancer Institute’s Cancer Information Service at: 1-800-4-CANCER (1-800-422-6237) You may also visit the NCI Web site at http://cancer.gov/. Chapter 7: Informed Consent Form Development Page 12 of 18 Office of Human Research Or (Non-Cancer studies) You may also visit the following Web site at http://clinicaltrials.gov/ to learn more information about participating in research studies. If you want more information about this study, ask your study doctor. 7. Special ICF Language Requirements 7.1 Assent Forms Generally, minors and adults with limited decision-making capacity do not have the legal authority to provide consent for their own participation in a research study. However, an investigator should still seek affirmative agreement (assent) from such research subjects. An assent form is a simplified version of the consent form and should be written to the subject's level of understanding. A typical assent form explains a study's purpose, procedures, risks, benefits, confidentiality, and voluntary nature in simple terms. 7.2 Human Immunodeficiency Virus (HIV) Testing Florida state law requires HIV testing to be reported to the Florida Department of Health. If HIV testing is completed as part of the research procedures, prospective subjects must be informed of the reporting requirements. Sample consent form language for HIV testing: “Florida state law, like laws in most states, requires health care workers to report the names of people who test positive for HIV to the Florida Department of Health. The reason for this is to keep track of how many people in the U.S. have HIV infection, and to make sure that the U.S. government provides enough money to each state to support the medical care of people living with HIV. The Florida Department of Health does not share the names of HIV infected individuals with any other governmental or nongovernmental agency. This maintains the privacy of HIV infected individuals whose names are reported.” 7.4 Radiation If participants will be subjected to Radiation beyond that of common diagnostic procedures, and/or biological effects are anticipated from the radiation, then a statement about the biological effect must be included in the radiation risk statement. 7.5 Tissue or Blood Banking If a secondary aim of the research study is to bank tissue or blood for future genetic analyses, subjects should have the ability to refuse without jeopardizing overall study Chapter 7: Informed Consent Form Development Page 13 of 18 Office of Human Research participation. To do this, the consent form can include an opt-in/opt-out section or a separate consent form can be used for blood and tissue banking. 8. Variations in Informed Consent 8.1 Deception in Research Certain research studies are designed to test responses when the research subjects are intentionally misinformed or have had certain information withheld from them. This type of research is categorized as deception. To request approval from the IRB for the use of deception, the investigator should demonstrate that: • the use of deceptive techniques is unavoidable (alternatives are not feasible) • deception does not involve significant risk • subjects are not deceived about aspects of the study that would affect their willingness to participate • data collection will be followed by a sensitive debriefing session (explanation of the deception) that protects the rights and dignity of research subjects 8.2 Writing an informed consent form for a study that involves deception • the consent form cannot include anything that is untrue • the consent form should reveal as much information as possible without compromising the study aims • this may include a statement that the subject may not be told complete information due to the study design, but will be informed at the completion of the study • a separate post-debriefing consent form is recommended to give subjects the opportunity to opt-out of having their data included in the research 8.3 Waiver of the informed consent process In specific circumstances, the IRB may waive part or all of the informed consent process. For example, an investigator may want to conduct a retrospective study of existing, anonymous laboratory specimens without obtaining informed consent. To request a waiver of informed consent, the investigator must demonstrate in a letter to the IRB that all of the following conditions are met: • The research involves no more than minimal risk • The waiver will not adversely affect the rights or welfare of subject • The research could not practicably be carried out without a waiver • When appropriate, the subjects will be provided with additional, pertinent information after participation Chapter 7: Informed Consent Form Development Page 14 of 18 Office of Human Research Note: The investigator will also be responsible for requesting an exemption or waiver of the HIPAA authorization. 8.4 Translated Consent Forms The consent form must be written in a language understandable to the subject or the subject's representative. If non-English speaking subjects are anticipated to be enrolled into the study, or if it is found that more than a few subjects are enrolled who speak the same non-English language, the consent form must be translated. The IRB must approve the translated form before it can be used to consent subjects. Translated consent forms must be certified as correct. The translation service will be asked to provide a letter certifying that the translation is a true and accurate translation of the original English version. Please contact the OHR for MHS approved translation services. 9. HIPAA Authorization The Health Insurance Portability and Accountability Act (HIPAA) are privacy regulations that limit the collection and disclosure (defined below) of protected health information. Protected health information (PHI) is individually identifiable health information. PHI includes any of the following individually identifiable elements: • Names • Street address • Postal or street address information (some exclusions apply here) • All elements of dates (except year) related to an individual (including hospital admission and discharge dates) • Ages of individuals over 89 • Telephone and fax numbers • Email addresses • Social security numbers • Medical record, health plan, or other account numbers • Certificate/license numbers • Vehicle identifiers • Device identifiers • Web (URLs) and Internet (IP) addresses • Biometric identifiers • Full face photos • And any other unique identifying number Chapter 7: Informed Consent Form Development Page 15 of 18 Office of Human Research Investigators must obtain a signed HIPAA Authorization form or IRB Waiver of HIPAA Authorization from the subject to collect, use, or disclose protected health information for research. Disclosure refers to the release of PHI outside of the "covered entity." Each Informed Consent will list the entities that will have access to the participants’ PHI. 9.1 HIPAA Authorization Form The content of the HIPAA form is regulated in the Code of Federal Regulations in 45 CFR 160 and 164. A HIPAA authorization must include the following core elements: • Description of the protected health information (PHI) in a specific and meaningful way • Who may use or disclose the information • Who may receive the information • Purpose of the use or disclosure • An expiration date or event • Individual signature and date • Right to revoke the authorization including exceptions • Reference to the Notice of Policy Practices • Right to inspect or copy PHI disclosed • Right to signed copy of HIPAA • Covered entity may continue to use PHI pursuant to authorization • Covered entity may continue to use data to protect the integrity of the research • Re-disclosure of health information are no longer protected by HIPAA The HIPAA authorization may be incorporated into the research consent form or it may be kept as a separate document. The MHS IRB template has incorporated the HIPAA authorization into the informed consent template, but it may be a separate document in cases where other IRBs are utilized. A sponsor-supplied HIPAA Authorization form cannot be used in place of the MHS IRB HIPAA Authorization form. HIPAA regulations apply to the healthcare institution, not the industry sponsor. 9.2 IRB Exemption/Waiver of HIPAA Authorization Research Using De-identified Information De-identified information is health information that has been stripped of all identifiers and is no longer protected under HIPAA. A research study may use or disclose de-identified data for research purposes if it is an IRB-approved protocol that received an exemption Chapter 7: Informed Consent Form Development Page 16 of 18 Office of Human Research from IRB review. For exempt studies, the IRB Waiver of HIPAA Authorization form should be completed and submitted with the Request for Exemption form sent to the IRB. IRB Waiver of HIPAA authorization In certain instances, an investigator may access protected health information for research without obtaining a HIPAA authorization from subjects. In these situations, the IRB may waive part or all of the HIPAA authorization. For example, an investigator may request a HIPAA waiver to conduct a retrospective chart review. To request an IRB waiver, the investigator must contact the MHS IRB. To be granted a waiver of HIPAA authorization, the investigator must demonstrate that: • The disclosure involves no more than minimal risk and has in place the following: o Protection Plan: plan to protect identifiers from disclosure o Destruction Plan: plan to destroy identifiers at earliest opportunity o Assurances against Re-disclosure: information will not be reused or disclosed except as required by law • The research could not practicably be carried out without a waiver • The research could not be carried out without access to protected health information 9.3 Exception from HIPAA Requirements Research Using a Limited Data Set Investigators can use a “limited data set” without obtaining a HIPAA authorization, provided that the following identifiers have been removed: • names • street addresses (other than town, city, state and zip code) • telephone numbers • fax numbers • e-mail addresses • Social Security numbers • medical records numbers • health plan beneficiary numbers • account numbers • certificate license numbers • vehicle identifiers and serial numbers, including license plates • device identifiers and serial numbers Chapter 7: Informed Consent Form Development Page 17 of 18 Office of Human Research • URLs • IP address numbers • biometric identifiers (including finger and voice prints) • full face photos (or comparable images) A limited data set may include the following indirect identifiers: • dates such as admission, discharge, service, date of birth, date of death; • city, state, five digit or more zip code; and • ages in years, months or days or hours Please contact the MHS IRB when conducting research using a Limited Data Set. 9.4 Activities Preparatory for Research to Prepare a Protocol An investigator can obtain PHI for data collected "preparatory for research" without a HIPAA authorization provided that all of the following conditions are met: • The data is sought solely to review PHI as necessary for activities preparatory for research. • No PHI will be removed from MHS by the researcher in the course of review. • The PHI is necessary for the research purposes. "Preparatory for research" includes developing research questions, determining study feasibility, and determining study eligibility. Please note, that although HIPAA regulations consider determining study eligibility an activity preparatory to research, the actual process used to recruit subjects remains a research activity that requires IRB approval. 9.5 Research Using Decedent Information An investigator may use or disclose the protected health information of individuals who have died without a HIPAA Authorization or a Waiver of Authorization provided that the researcher can demonstrate in a letter to the IRB that: • The use is solely for research on the protected health information • The research could not be carried out without access to protected health information • Individuals are deceased Chapter 7: Informed Consent Form Development Page 18 of 18 Office of Human Research Chapter 8: Subject Recruitment Plan Successfully recruiting the desired number of subjects for a study is critical to its success. Subject recruitment can often be challenging. There are several methods that can be developed in a comprehensive subject recruitment plan to help meet this challenge. 1. Recruitment Strategies 1.1 Clinical Care Settings and Resources • Screening incoming patients in healthcare setting • Medical record reviews • Departmental databases and registries 1.2 Physician Referral • Networking with other practices and clinics • Educational forums for physicians, nurses and hospital staff • Mailings, referral packets 1.3 Community Awareness 2. • Advertising through news, magazine, and journal ads • Advertising through direct mail, posters, flyers, and brochures • Advertising to the general public through media such as radio, TV and the Internet • Participating in community health events and forums • Educational forums to patient advocacy groups and community • Press releases and media events Considerations for Subject Payments Subjects are sometimes offered monetary payments for their participation in research studies. While many differing perceptions exist on the ethics and effectiveness of this practice, the decision to provide payment to research subjects is generally made by the PI in order to facilitate timely recruitment of subjects for the study. The justification for payment to research subjects include the provision of an incentive to participate, reimbursement for expenses that the subject may incur to participate, or payment for the subject’s time and inconvenience. It is never acceptable to use payment as a benefit to offset the risks of a study. Chapter 8: Subject Recruitment Plan Page 1 of 5 Office of Human Research Several important ethical considerations should be weighed when considering whether or not to pay subjects, how much, and on what schedule. One important concern is that the payment may cause undue influence on the subject’s decision to participate in the study. That is, the financial incentive may render potential subjects less likely to fully weigh the potential risks. While there is no concrete guidance on what size payment may induce undue influence on a subject, it is essential to evaluate the nature of the study, the contributions and sacrifices made on the part of the research subject, vulnerabilities that may be inherent in the study population, and local and societal norms. Subject payments typically are classified as either reimbursement or remuneration. • Reimbursement refers to payment, monetary or other form, paid to a subject for out-of-pocket expenses such as study-related travel, lodging, meals or lost wages. • Remuneration refers to monies paid to subjects as repayment for their personal time and effort committed to study participation. NOTE: The term “compensation” should be used only to refer to payment or medical care provided to subjects injured in research. All subject payments should be described in the study protocol and informed consent form, which must be approved by the IRB prior to project initiation. 2.1 Determining the Amount of Payment Payments vary based upon the complexity of the study, the type and number of procedures, the time involved, and the anticipated inconveniences. Sponsors may offer up to a given maximum amount, and Investigators may calculate payments by estimating the number of biological samples collected, the amount of time spent on the project, the subject's anticipated out-of-pocket expenses, or a variety of other factors. Monetary inducements are not allowed solely for the purpose of attracting subjects for studies involving significant risk or excessive pain or discomfort, such as a bone marrow biopsy. 2.2 Payment Schedule Payment should be accrued or prorated as the study progresses and not be contingent upon the subject completing the entire study. Subjects who withdraw early from the study may be paid at the time they would have completed the study had they not withdrawn (unless it creates undue inconvenience or appears coercive). All information concerning the payment, including the amount and schedule of payment(s), should be described in the informed consent form. The investigator may include a small extra payment at the end of the study (bonus) as an incentive for completion, providing that it is not coercive. If a bonus is awarded it should be provided to all completed subjects, not just "favorite" or compliant subjects. The bonus should not be offered as an alternative to withdrawal if the subject wishes to discontinue participation in the study. Chapter 8: Subject Recruitment Plan Page 2 of 5 Office of Human Research 3. Privacy Rules Regarding Subject Recruitment 3.1 Acceptable Methods of Contacting the Subject (in order of priority) 1. The preferred method is to have the physician or other health care provider who has taken care of the patient in the past to contact the patient directly. Or the research staff can be authorized by the physician to contact the patient on the physician's behalf. 2. If this is impractical, the Investigator may develop a letter to be used to contact the patient. The letter must be approved and signed by a physician or other health care provider who has cared for the patient. Alternatively the physician may authorize the research staff to send a letter on the physician's behalf and signed by the research staff. The language of the letter must also be approved by the IRB. 3. If the first two methods are impractical, the Investigator may contact the potential subject directly. This method of recruitment will require specific IRB approval, and approval will only be granted if the impracticality of the first two methods is well-substantiated. 3.2 Advertisement Development Direct advertisements (radio, television, print, internet, telephone, brochures, websites, etc.) are used to recruit subjects for research in general and/or for specific studies. Direct recruiting advertisements are considered a part of the informed consent and subject selection process and, therefore, governable by federal regulations. Several federal regulations govern the use of advertisements (21 CFR 50, 21 CFR 56 and 21 CFR 812). These regulations stipulate that advertisements must not present any coercive or misleading information by implying a certainty of favorable outcome, claiming the safety or efficacy of an investigational product, implying the study is a medical treatment, promising free medical care, or overemphasizing payments. The IRB provides guidance on recruitment materials and will need to approve any materials intended to come in contact with potential participants. Advertisements are not limited to the printed word, such as appears in newspapers or brochures. Radio advertisement and videos (such as are used for television) also fall within this purview and are subject to the same guidelines and submission requirements. To recruit subjects, advertisements may include the following information: • Name and address of the investigator and/or research facility • Condition under study and/or the purpose of the research o Include the word research, investigational, or experimental o Specify if a placebo will be involved • Abbreviated description of criteria that will be used to determine eligibility • A brief list of participation benefits, if any Chapter 8: Subject Recruitment Plan Page 3 of 5 Office of Human Research • Time and/or expected commitment required of the subject • The person to contact for further information Well-designed advertisements are clear in phrasing and simply worded, using nonmedical terminology where possible. An appropriately worded advertisement may include the expected payment as long as it is not overemphasized so that it can be perceived as a benefit. 3.3 Recruitment Brochures Brochures are a type of advertisement tool used to help with the recruitment of subjects. Brochures are often created in the start-up phase of research. However, recruitment brochures are usually not subject to the space limitations of other written advertisements and, as such, their formatting may vary slightly. Recruitment brochures generally incorporate the elements of an advertisement in several distinct sections: Call to action This section notifies the potential subjects of the focus of the project. Typically this call to action is worded in question format asking the reader if they have experienced a given situation. e.g. Have you ever..?, Are you planning..? Do you have..? Have you and your provider discussed..? Study Significance This section explains the importance of the research project and the significance of the intended research. Typically this section is worded as a question drawing attention to the study importance. e.g. Why is this study important? Inclusion/Exclusion Criteria This section outlines the protocol-defined parameters for study eligibility. This section helps the targeted audience understand the likelihood of participation. Typically inclusion/exclusion criteria are worded as a directive guiding participation eligibility. e.g. You may participate if you: .. You may not participate if you. Study Procedures This section explains the study-related procedures and clearly discusses the activities as part of research participation. Typically this section outlines the activities in chronological order and directly correlates with the study protocol and informed consent form. Principal Investigator This section includes the name, title and affiliation of the Principal Investigator. Typically this section is located on the back of the brochure. Chapter 8: Subject Recruitment Plan Page 4 of 5 Office of Human Research e.g. Name of Principal Investigator Title of Principal Investigator Affiliation 4. Institutional Review Board (IRB) Submission Research advertisements must be approved by the IRB prior to implementation. The IRB must ensure that advertisements do not contain information that is misleading to potential research subjects. Most advertisements are reviewed in an expedited fashion. The IRB prefers that radio and video advertisements be submitted as transcripts rather than audio or video presentations. If an advertisement is translated, the translation must be submitted with a copy of the original English version for review and approval. Copies of recruitment letters to subjects and intermediaries ("Dear Doctor" letters) must also be submitted to the IRB. 5. Clinical Trials Web Posting All U.S. drug or device clinical trials must be registered on the ClinicalTrials.gov website in accordance with requirements published by the International Committee of Medical Journal Editors (ICMJE) and the FDA Amendment Act of 2007. The following clarifies who is responsible for registering your clinical trial: 1. Investigator holding IND or IDE applications with the FDA: the Investigator IND/IDE holder is required to register the clinical trials conducted under the IND/IDE application 2. Investigator-initiated, government-sponsored clinical trials: Generally the sponsoring federal or state agency is required to register the clinical trial 3. Industry-sponsored clinical trials: the industry sponsor is required to register the clinical trial In order to register your trials directly to ClinicalTrials.gov, you will need to designate a person who will be responsible for posting your clinical trials. The OHR and IRB are responsible for all clinical trial information that is released to ClinicalTrials.gov from the Memorial Healthcare System. Prior to releasing the trial information for public access, the OHR must ensure the following for each submission: 1. There are no system-generated red error warnings in the submission; 2. The study is IRB approved; and 3. If the listed collaborator is an industry sponsor, that written authorization for posting has been provided by the industry sponsor When entering your registration information into the ClinicalTrials.gov web form, please ensure that all red error warnings have been resolved prior to clicking the "Complete" button. The red error warnings indicate missing or discrepant information. For more information, visit ClinicalTrials.gov at http://www.clinicaltrials.gov/. If your study is already registered please visit Clinical Trials Login at https://register.clinicaltrials.gov/. Chapter 8: Subject Recruitment Plan Page 5 of 5 Office of Human Research Chapter 9: IRB Submission The Institutional Review Board (IRB) is an independent committee that oversees the protection of human subjects. This committee reviews research studies and the ongoing activities of approved research. In compliance with federal regulations, the IRB must include at least 5 people including men and women and representing various professions and affiliations. At least one member may not be affiliated with the institution. Minimal attendance at a meeting, called a quorum, is defined as a convened meeting with a majority of members present including one member whose primary concerns are nonscientific. The regulations require that a quorum be present in order for the full board to review full board actions, including new studies, amendments, continuing review of previously reviewed research, reports of unanticipated problems posing risk to subjects or others, and reports of serious or continuing noncompliance with the regulations. 1. Memorial Healthcare System IRB Review The Memorial Healthcare System IRB holds monthly meetings (typically convened the second Monday of each month). For new studies, the IRB application, Informed Consent, and Protocol will be reviewed at an IRB Subcommittee meeting (typically convened every other Wednesday) prior to formal submission to the IRB. The submission deadlines for IRB subcommittee meetings as well as IRB meetings are roughly three weeks prior to the meeting dates. Amendments to protocols, however, are to be submitted a week earlier than other full board submissions. Please contact the IRB or OHR for schedules of submission and meeting dates for IRB Subcommittee and IRB meetings. The IRB also offers guidance regarding required documents and number of copies of each needed for each type of submission (see below). 2. Determining IRB Review Type These are general guidelines to determine the level of risk and corresponding IRB review mechanism and submission requirements for research protocols involving human subjects. Other factors that may impact review type include: the involvement of vulnerable populations, the use of protected health information (PHI), privacy/confidentiality issues, psychological effects, conflicts of interest, experience of research team, etc. Assessing the review type for a study will determine the requirements for submitting the study to the IRB for review. Please note that the IRB makes the final determination of level of review. The first question one should consider when assessing the requirement for IRB review is whether the activity meets the regulatory definition of human research (see Chapter 1: Introduction). Anyone unsure about IRB review requirements and whether their proposed activity constitutes “human research” requiring IRB review should contact the Office of Human Research (OHR). If an activity does not meet the regulatory definition of human research, the IRB will, upon request, issue a letter stating that the project does not require IRB review or approval. Communication with the IRB office should occur prior to initiating the study. Chapter 9: IRB Submission Page 1 of 11 Office of Human Research Once it is determined that the project meets the definition of human research, the level of review must then be determined. The initial criteria used in determining the review level is ascertaining if a study meets the criteria for minimal risk. Minimal risk research may be eligible for either expedited or full board review. Minimal risk means that “the risk of harm anticipated in the proposed research that is not greater, considering the probability and magnitude, than those ordinarily encountered in daily life of a healthy individual or during the performance of routine physical or psychological examinations or tests.” Below are general guidelines for determining the review level. All research-related activities within a study must fall in their entirety within the exempt categories in order to qualify for exempt status. This is also true for expedited review. 2.1 Exempt from Review DHHS and FDA regulations allow specific categories of research to be exempt from human subject review. Research that is considered exempt from Committee review must still be filed with the IRB and screened for exempt status. Protocols qualifying for exempt status do not require annual continuing review. Investigators are required to notify the IRB if any changes are proposed that could alter the exempt status of the protocol. Categories of Exempt Research Following is a list of categories that are typically eligible for Exemption from IRB Review. Additional conditions and limitations exist for each category as specified in the IRB’s Claim of Exemption Instructions. NOTE: The FDA only allows research to qualify for Exempt from Review that falls under Category 6 below. All other categories of research that is subject to FDA regulations require Expedited or Full Board Review. Category 1 Research conducted in established or commonly accepted educational settings, involving normal educational practices, such as research on regular and special education instructional strategies, or research on the effectiveness of, or the comparison among instructional techniques, curricula, or classroom management methods. NOTE: This category may be applied to research involving children. NOTE: This category may not be applied to FDA regulated research. Category 2 Research involving the use of educational tests (cognitive, diagnostic, aptitude, achievement), survey procedures, interview procedures or observation of public behavior, unless: a) Information obtained is recorded in such a manner that human subjects can be identified, directly or through identifiers linked to the subjects and Chapter 9: IRB Submission Page 2 of 11 Office of Human Research b) Any disclosure of the human subjects' responses outside the research could reasonably place the subjects at risk of criminal or civil liability or be damaging to the subjects' financial standing, employability, or reputation. NOTE: The section of this category pertaining to standardized educational tests may be applied to research involving children. This category may also apply to research with children when the investigator observes public behavior but does not participate in that behavior or activity. This section is not applicable to survey or interview research involving children. NOTE: This category may not be applied to FDA regulated research. Category 3 Research involving the use of educational tests (cognitive, diagnostic, aptitude, achievement), survey procedures, interview procedures, or observation of public behavior that is not exempt under paragraph (b) above, if: a) The human subjects are elected or appointed public officials or candidates for public office or b) Federal statute(s) require(s) without exception that the confidentiality of the personally identifiable information will be maintained throughout the research and thereafter. NOTE: This category may not be applied to FDA regulated research. Category 4 Research involving the collection or study of existing data documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects. a) To qualify for this exemption the data, documents, records, or specimens must be in existence before the project begins. Investigator must describe where the information exists. b) Under this exemption, an investigator (with proper institutional authorization) may inspect identifiable records, but may only record information in a nonidentifiable manner. Investigator must describe how information will be obtained, what data elements will be recorded, and whether any links to identifiers will be recorded. NOTE: Inclusion of fetal tissue in the pathological specimens category of exempt research is prohibited by regulation and requires additional IRB review. NOTE: This category may not be applied to FDA regulated research. Chapter 9: IRB Submission Page 3 of 11 Office of Human Research Category 5 Research and demonstration projects which are conducted by or subject to the approval of federal Department or Agency heads, and which are designed to study, evaluate, or otherwise examine: a) Public benefit or service programs; this exemption is for federally supported projects and is most appropriately invoked with authorization or concurrence by the funding agency. The following criteria must be satisfied to invoke the exemption for research and demonstration projects examining "public benefit or service programs." i. The program under study must deliver a public benefit (e.g., financial or medical benefits as provided under the Social Security Act) or service (e.g., social, supportive, or nutrition services as provided under the Older Americans Act) ii. The research or demonstration project must be conducted pursuant to specific federal statutory authority. iii. There must be no statutory requirement that an Institutional Review Board review the project. iv. The project must not involve significant physical invasions or intrusions upon the privacy of participants. b) Procedures for obtaining benefits or services under those programs; c) Possible changes in or alternatives to those programs or procedures; d) Possible changes in methods or levels of payment for benefits or services under those programs. e) Before invoking this exemption, the IRB will obtain concurrence of the funding agency that this exemption can be applied. NOTE: This category may not be applied to FDA regulated research. Category 6 Taste and food quality evaluation and consumer acceptance studies if: a) Wholesome foods without additives are consumed or b) if a food is consumed that contains a food ingredient at or below the level and for a use found to be safe, or agricultural chemical or environmental contaminant at or below the level found to be safe, by the Food and Drug Administration or approved by the Environmental Protection Agency or the Food Safety and Inspection Service of the U.S. Department of Agriculture. NOTE: This category may be applied to children. NOTE: This category may be applied to FDA regulated research. Chapter 9: IRB Submission Page 4 of 11 Office of Human Research 2.2 Expedited Review To qualify for expedited review the following must apply: 1) Clinical studies of drugs and medical devices only when condition (a) or (b) are met. a) Research on drugs for which an investigational new drug application is not required. (Research on marketed drugs that significantly increases risks or decreases acceptability of risks is not eligible.) b) Research on medical devices for which (i) an investigational device exemption application is not required; or (ii) the device is cleared/approved for marketing and being used in accordance with its labeling. 2) Collection of blood samples by finger stick, heel stick, ear stick, or venipuncture a) From healthy, non-pregnant adults who weigh at least 110 pounds. The amounts drawn may not exceed 550 ml in an 8 week period and collection may not occur more frequently than 2 times per week; or b) from other adults and children, considering the age, weight, and health of subjects, collection procedure, amount of blood to be collected, and frequency with which it will be collected. The amount drawn may not exceed the lesser 50 ml or 3 ml/kg in an 8 week period and collection may not occur more frequently than 2 times per week. 3) Prospective collection of biological specimens for research purposes by noninvasive means: a) Hair and nail clippings in a non-disfiguring manner; b) Deciduous teeth at time of exfoliation or if patient care indicates a need for extraction; c) Permanent teeth if patient care indicates a need for extraction; d) Excreta and external secretions (including sweat); e) Uncannulated saliva collected in an unstimulated fashion or stimulated by chewing gumbase or wax or by applying dilute citric solution to the tongue; f) Placenta removed at delivery; g) Amniotic fluid obtained at the time of rupture of the membrane prior to or during labor; h) Supra- and sub-gingival dental plaque and calculus, provided the collection procedure is not more invasive than routine prophylactic scaling of the teeth and the process is accomplished in accordance with accepted prophylactic techniques; i) Mucosal and skin cells collected by buccal scraping or swab, skin swab, or mouth washings; j) Sputum collected after saline mist nebulization Chapter 9: IRB Submission Page 5 of 11 Office of Human Research 4) Collection of data through noninvasive procedures (not involving general anesthesia or sedation) routinely employed in clinical practice, excluding procedures involving xrays or microwaves. Where medical devices are employed, they must be cleared/approved for marketing. (Studies intended to evaluate the safety and effectiveness of the medical device are not generally eligible for expedited review, including studies of cleared medical devices for new indications). Examples include: a) physical sensors that are applied either to the surface of the body or at a distance and do not involve input of significant amounts of energy into the subject or an invasion of the subject’s privacy; b) weighing or testing sensory acuity; c) magnetic resonance imaging; d) electro-cardiography, electroencephalography, thermography, detection of naturally occurring radioactivity, electroretinography, ultrasound, diagnostic infrared imaging, Doppler blood flow, and echocardiography e) moderate exercise, muscular strength testing, body composition assessment, and flexibility testing where appropriate given the age, weight, and health of the individual. Examples of research eligible for expedited review: • Non-invasive medical procedures that do not involve x-rays or sedation (e.g. MRI, EKG, EEG) • Minimal blood draw amounts in healthy non-pregnant subjects • Prospective collection of biological specimens by noninvasive means (e.g. buccal scrapings, saliva, excreta, sputum) • Voice recordings; research on individual or group behavior such as interviews or focus groups. • Moderate exercise by healthy volunteers Note: HIPAA waiver applies to the extent that identifiable data sources are accessed & used. 2.3 Full Board Review Studies that do not qualify for expedited review require approval by an IRB panel composed of members trained to review research in that field (full board review). Examples of minimal risk research requiring full board review include: • DEXA scan for bone density • Any protocol involving X-Rays occurring for the purposes of the research Examples of greater than minimal risk research requiring full board review include: • Any survey or interview that is likely to be stressful for the subjects Chapter 9: IRB Submission Page 6 of 11 Office of Human Research • Research that involves experimental drugs or devices, invasive procedures • Involve increased risk due to the nature of the research or the population being evaluated. • Involve a washout period or placebo use in an otherwise treatable disease. • Involve “greater than minimal risk and no prospect of direct benefit to the individual subjects but likely to yield generalized knowledge about the subject’s disorder or condition” (CFR 45 Part 46.406}). 3. IRB Submission Requirements For a detailed listing of application procedures and required documents, please contact the OHR or IRB. 3.1 Tips for IRB Submission • Contact the IRB and OHR to ensure that correct version of submission forms, application forms etc. are used. • Include page numbers, version number & date on all study documents: protocol, protocol summary, informed consent, HIPAA Authorization, etc. 3.2 Submission Process Documents Needed for IRB Subcommittee Meeting • One (1) electronic version of the protocol (PDF) • MHS IRB application • Informed Consent Form using MHS Template (MS Word) • Recruitment or subject tools • Four (4) copies of the protocol • Two (2) copies of the investigator’s brochure (drugs) or Directions for Use (device) • One (1) FDA 1572 signed form (if applicable) • One (1) letter noting regulatory status of study device from sponsor The IRB will review all documents on a first come, first serve basis unless a patient is waiting to be treated. If there is a high volume of submissions, there is a chance that protocols will be reviewed at a later subcommittee date on the schedule, even if they are submitted on time. The subcommittee can review approximately three protocols per meeting, and typically, two subcommittee meetings are held per month. Additional subcommittee meetings may be convened as determined on a case-by-case basis. Chapter 9: IRB Submission Page 7 of 11 Office of Human Research Documents Needed for IRB Meeting: New Protocols • Two (2) copies of submitted original application and ONE ORIGINAL APPLICATION SIGNED AND DATED. • Two (2) copies of informed consents (and assents) AND ONE ORIGINAL CONSENT(S) (and ASSENTS, if applicable) TO BE STAMPED. • Two (2) copies of recruitment tools, subject tools. Re-Approval of Progress Reports and Informed Consent • One (1) signed original progress report including FORM A personnel and FORM B (deviations) • Two (2) copies of the signed progress report • One (1) copy of the current ORIGINAL CONSENT(S) (and ASSENTS and translations, if applicable) untracked without stamped IRB approval located on front page, • One (1) original of the current consent(s)/assent(s)for stamping. If you are making minor changes to the consent(s), assents, or consenting tools at this time then: • One (1) copy tracked version of the current document and • One (1) copy untracked version of the revised document for stamping. • One (1) copy of sponsor’s report on the status of the study (include all that apply such as data safety monitoring committee’s reports, Study Chair report, or Annual Device progress report). Revisions/Amendments • Submit one (1) electronic version (each) of the amendment, the amendment summary, protocol that incorporates the amendment • If amendment requires changes to MHS consent, submit one (1) sponsor’s consent sample and one (1) tracked version of current MHS consent with the changes required only by this amendment. The IRB office will review the consent changes requested for understandability, and completeness against the sponsor’s sample. Identified issues may need to be further discussed with the sponsor or MHS legal prior to final submission. At the IRB deadline, submit: • one (1) signed revision form, • two (2) hard copies of amendment summaries and ONE COMPLETE ORIGINAL AMENDMENT which includes the summary where applicable, Chapter 9: IRB Submission Page 8 of 11 Office of Human Research • ADDITIONALLY, one (1) copy of the protocol incorporating the amendment. If the amendment is not sufficient to describe the detailed changes then the IRB office reserves the right to request copies of the entire amendment. Revised Consent • One (1) signed revision form, • Two (2) copies of revised informed consents (red lined with changes with new revision date) • ONE (1) INFORMED CONSENT TO BE STAMPED (WITHOUT THE REDLINE). Unanticipated Problems that are Adverse Events or Unanticipated Problems that are not Adverse Events Report Forms (prompt reporting within 10 working day of becoming aware of issue) • One (1) signed original and • One (1) copy of the unanticipated problem reporting form including sponsor reports attached to each or supporting documentation (redact patient identifiers). If the study is closed at site and sponsor requires submission acknowledgement, then only submit one (1) original. Other Documents 4. • One (1) signed revision form, • One (1) original document, • One (1) copy. IRB Post-Review Actions Following the IRB review of the study, one of the following outcomes will result. The follow-up actions taken by the investigator depend upon the outcome of the IRB review. 4.1 Outcomes Approval No action is needed. The study can begin provided that approval has been received from all other applicable reviewing entities (Sponsor etc.). Approved with conditions that need to be satisfied for full approval The IRB will provide the investigator with specific modifications that are necessary for approval. Revise the study documents and/or provide clarifications as recommended. Return one copy with the revisions tracked or documentation requested. Response is reviewed and may not need to return to the full board Chapter 9: IRB Submission Page 9 of 11 Office of Human Research unless the conditions cannot be satisfied. The study cannot begin until the revised submission has been approved. Tabled The IRB will provide the investigator with specific questions that need to be addressed before approval will be considered. Revise the study documents as recommended. Tabled studies are re-reviewed by the full IRB. Investigators are encouraged to attend the IRB meeting following a tabled decision. Studies may be tabled if the investigator is unavailable to present the study to the IRB committee. The study cannot begin until the revised submission has been approved. Disapproval The investigator may discuss the review with the IRB Chairperson. The protocol must be resubmitted in its entirety as per the Submission Requirements. The study cannot begin until the new submission has been approved. Investigators whose studies are not approved can benefit from a consultation with the Office of Human Research on issues such as protocol design, informed consent and other human subject protection issues. For more information on the IRB process, please refer to the FDA website: Guidance Documents for IRBs, Sponsors & Investigators Please refer to the chart below to assist with determining the appropriate IRB review category for your study. Please note: The IRB makes the final determination of the review category. Chapter 9: IRB Submission Page 10 of 11 Office of Human Research Determining IRB Review Category – Exempt, Expedited, or Full Board Review Does the research pose less than minimal risk, i.e. no known physical, emotional, psychological, or economic rist? YES Does your research involve a vulnerable population? Meets the EXEMPT Category for IRB Review NO NO YES Does the research pose minimal risk typically encountered in daily life such as moderate exercise, minor stress from testing or surveys? YES Does your research involve a vulnerable population? YES NO Does the research pose greater than minimal risk typically encountered in daily life, such as maximal exercise, stressful psychological tests, questions about illegal activities? Chapter 9: IRB Submission Meets the EXPEDITED Category for IRB Review NO YES Meets the FULL BOARD Category for IRB Review Page 11 of 11 Office of Human Research Chapter 10: Contracts and Study Finances Contracts and Study Finances 1. Study Budget Development When requesting funding for a study, all study-related costs should be noted in the budget including personnel, consultants, equipment, supplies, travel, and other expenses. NIH applications have special Budget and Justification forms that contain detailed instructions. Investigators should develop a budget based upon the expected expenses at each site. Billing rates for the same procedure will vary from place to place. When participating in a sponsored study, it is the sponsor’s responsibility to provide a budget template. When considering an industry sponsored-study, all study related expenses should be determined and compared to the overall reimbursement offered by the sponsor to ensure the study is financially feasible. Depending on the funding source, items may or may not be included in the budget and expenses may have different associated overhead charges. The following is a list of potential expenses involved in the conduct of a study: a. Personnel Estimate the amount of time for the PI, the coordinator(s), Pharmacist(s), Data Managers, and any other staff that would be paid out of the study budget (i.e. research assistants, administrative staff, statisticians). This estimate should include not only salary, but also fringe benefit costs. b. Labs, Tests, and Procedures Technical Fees - A technical fee is the cost incurred for use of the mechanical equipment and processing. Tests/procedures that are study related and are not "standard of care" must be charged to the research budget. Every effort should be made to provide documentation to determine what tests/procedures would be considered “standard of care” (i.e. drug labeling information, established guidelines for monitoring/treating the particular disease, generally accepted practices by the medical community etc.). Professional Fees - The professional fee is the physician's charge for interpretation of diagnostic procedures/tests. It is important to note that if there is a professional fee associated with a test/procedure, that charge must be included in the expenses. A limited number of laboratory tests have professional fees associated with them. All radiology and cardiology procedures have a professional fee, as do various other procedures. c. Subject Reimbursement These charges may be incurred per visit or per subject. Examples include monetary compensation, meals and parking/transportation costs. Sponsors may not provide subject reimbursement for all studies d. Additional Study Expenses Other potential study expenses to consider: Page 1 of 4 Office of Human Research • Training/Seminars/Conferences (directly related to the research projects) • Institutional Review Board (IRB) fees • Investigational Drug Service (IDS) fees • Advertising/Recruitment • Monitoring • Non-refundable start-up costs • Screen failures • Supplies o E.g. blood collection tubes, chemicals, dry ice) o E.g. centrifuges, mass spectrometers, liquid simulation counters) o Technology (e.g. telephone, computer) o Shipping/Packaging Supplies (e.g. dry ice) • Service Contracts (e.g. instrument maintenance) • Archival fees • Site Visit & Site Initiation Costs e. Facilities and Administrative Cost Facilities and Administrative (F&A) cost is the indirect cost associated with the project or study; e.g. space, research administration, facilities, maintenance, human resources, etc. F&A can only be assessed on certain activities and items depending on whether or not the study is federally-funded (see the specific grant guidelines). For industry-sponsored studies, the contract may specify which items can include F&A, though typically F&A is applied to all costs for industry-sponsored studies. If you cannot locate the F&A rule on the Chart of Allowable Expenses, you can consult with the OHR. 2. Contract Submissions Contract Submission for Sponsored Research Contracts should be submitted with an appropriately developed budget to the Office of Human Research as soon as possible to ensure that negotiations with the sponsor are resolved and project initiation is not delayed. The following documents should be included in a contract submission packet, which is submitted to the Department Business Office (Business Administrator): • Clinical Trial Agreement (CTA) • Draft Budget • Protocol Page 2 of 4 Office of Human Research • Informed Consent • Any lab manuals, pharmacy manuals etc. The contract submission packet, for either Investigator-Initiated or Sponsored Clinical Trials follows the process below: 2.1 Clinical Trial Agreement (CTA) The Clinical Trial Agreement is a contract between the South Broward Hospital District (SBHD) and the industry research sponsor that includes provisions to define the scope of work, performance period and enrollment of subjects, cost and payment, proprietary rights, and publications. The CTA represents the legal agreement between the Sponsor and the SBHD and an acceptance of such by the Investigator. The elements of a research contract may include: (1) Scope of work, (2) Responsible investigator (Principal Investigator), (3) Performance period, (4) Record-keeping obligations, (5) Reimbursement, (6) Confidentiality of Information, (7) Patents and Inventions, (8) Advertising (mutual agreement covering use of institution or sponsor's name), (9) Indemnification (see below), (10) Termination of the Contract, (11) Publication Rights/Intellectual Property. 2.2 Budget Agreement The budget agreement is a part of the Clinical Trial Agreement and specifies the reimbursement to be paid per enrolled subject, the miscellaneous and non-subject expenses, and the reimbursement schedule. Refer to Study Budget Development for more details. The budget should be evaluated and negotiated during the review of the protocol or grant/proposal submission and should realistically capture all costs associated with conducting the research, including faculty time commitment. Payment is usually received by the Finance Manager at the OHR. 2.3 Indemnification Agreement The indemnification language of the Clinical Trial Agreement protects the investigator and institution from liability for damage incurred by a research subject as a result of study participation. This protection is contingent upon the investigator practicing standard of care medicine and complying with the protocol and regulatory requirements and GCP standards. The sponsor is held accountable for medical expenses incurred by research subjects as a result of study participation. It does not obligate the sponsor to reimburse for "standard medical care" or care that would have occurred irrespective of study participation. In certain types of research, the sponsor may not be accountable for all expenses incurred by a subject's participation in a study. One example is cancer research where expenses for certain procedures and drug regimens are often borne by the subject's insurance carrier. Page 3 of 4 Office of Human Research 2.4 Letter of Understanding When an investigator not employed by MHS wishes to conduct research within MHS facilities, a Letter of Understanding needs to be executed in order to inform the Investigator and his team of the responsibilities and obligations of MHS and Contractor pertinent to the project. Please contact the OHR for more information regarding this process. Page 4 of 4 Office of Human Research Chapter 11 Site Implementation Site Selection for Multi-Center Studies For multi-center studies, it is the responsibility of the sponsor to choose sites to participate in the research study. The sponsor may be an investigator collaborating with other institutions or a pharmaceutical company conducting a multi-center trial. Regardless, sponsors and sponsor-investigators should follow the criteria set forth in Good Clinical Practice Guidelines 5.6.1. The selection process identifies investigators who are qualified and have adequate resources to implement the protocol. The following items are evaluated during the site selection process: Suitability of the investigator • • • • • Does the investigator have expertise in the area being studied? Does the investigator have experience with this type of research? Is the investigator accessible? Does the investigator have appropriate training and qualifications in clinical research? Has the investigator ever been sanctioned for research misconduct? Presence and experience of staff • • • • Are research-designated staff members involved and are they qualified? Are the potential sub-investigators qualified for the protocol? Is there an affiliated IRB to review the protocol? Will there be a qualified pharmacist or research pharmacist? Adequacy of facilities/resources • • • Is there a research office? A location for monitoring? An examination office? Is there a secured location for storing study files and/or investigational products? Does the investigator have access to the technology and equipment needed for the study (e.g. centrifuge, freezers, computers, ultrasounds, etc.)? Access to subjects • • • How many individuals with the appropriate diagnosis are accessible? Are there any studies that may be competing for the same population? What is the investigator's enrollment history in previous studies? If the site fulfills the needed requirements for the study, the sponsor will notify the site of acceptability as an investigative site. The sponsor will begin the site initiation process. Sponsor-investigators often choose sites based upon their interactions with fellow researchers at other institutions. Whether sites are evaluated through a telephone Chapter 11: Site Implementation Page 1 of 3 Office of Human Research interview, documented correspondence, or on-site visits, the Sponsor-Investigator must take the appropriate measures to select and evaluate investigative sites. Generally, site selection is accomplished initially via questionnaires or surveys, and further evaluated during the site qualification visit by the monitor (CRA). The site qualification visit may include: • • • • Tour of facilities including: patient care areas, screening areas, lab processing area, research office, pharmacy (if applicable) and location for monitoring of study data Introduction to study personnel including: Principal Investigator, research coordinator(s), sub-investigators, and pharmacists Confirmation of secured location for storage of investigational materials: separate area/office for Case Report Forms (CRF) and an area for study drugs and/or devices (if the pharmacist is responsible for investigational drugs, there must be a separate locked area for storage within the pharmacy) Discussion of the investigator's responsibilities, monitoring plans, and review of the protocol. Site Orientation Prior to study initiation, the research team should be versed in the proper techniques to conduct the study in accordance with the protocol, federal regulations, and GCP. This is true regardless of whether a study involves one department or institutions from around the world. Study orientation may be accomplished through an investigator meeting, onsite training, online training, conference calls, or a combination of these methods. Chapter 11: Site Implementation Page 2 of 3 Office of Human Research Site orientation may include: Site Initiation During the site initiation visit, the study monitor (CRA) will have a list of criteria to evaluate and review. The monitor will also provide one-on-one instruction and reinforce protocol training/orientation with the research team. Sponsor-Investigators are similarly responsible for evaluating and initiating sites. For the monitor's Site Initiation Checklist, see the applicable forms in the Sponsor-Investigator SOPs (refer to SOP 402). A monitor's site initiation checklist may include: • • • • • • • Confirmation of regulatory documentation Collection of outstanding regulatory documentation Review of protocol procedures, amendments, case report form completion, etc. Review study monitor expectations Review consent form and consent process Inspect and inventory study supplies Inspect storage site and dispensation records of study drug and/or device Chapter 11: Site Implementation Page 3 of 3 Office of Human Research Chapter 12: Research Project Management Conducting a clinical research study requires a well-organized approach to project management. Many aspects of study conduct can be discussed in relation to individual subjects and are covered in detail in the Subject Management section of this manual. This section discusses the aspects of project management that relate to the overall project. While this manual defines the requirements and offers standards for research project management, general project management skills are critical to effective and efficient study conduct. These skills include the ability to: • develop project management strategies • effectively prioritize • translate strategies into step-by-step plans for action • develop logical and practical approaches to implementing action plans • organize large amounts of information by creating and maintaining well organized systems • monitor work progress to completion • pay close attention to detail • ensure timely documentation of study processes 1. General Guidelines of Study Management Effective project management involves careful planning, organization, and regular assessments of the progress of the study. This section of the Manual details important elements of project management. While it's important to tailor a project management plan to the logistics of a specific study, there are basic elements of effective management that are common to all clinical research studies: • • Measurement and tracking of key study progress and safety parameters o Screening/Enrollment o Adverse events o Data collection o Study finances Study management meetings between the Principal Investigator (PI) and Clinical Research Coordinator (CRC) 1.1 Tracking Key Parameters In patient care, it's important to ascertain basic parameters and to track them over time to best manage the health of a patient. Similarly, to manage the "health" of a clinical study there are certain basic parameters common to all research projects that should be Chapter 12: Research Project Management Page 1 of 12 Office of Human Research measured and tracked regularly at regular intervals during the course of the study. The following summarizes these key parameters: 1.1.1 Projections In the planning stages of the study, it is important to create projections of expected rates of the key study parameters of screening, enrollment, data collection activities, and adverse events. This becomes the benchmark against which regular measurement and tracking of actual rates of these parameters can be compared. 1.1.2 Screening and Enrollment While individual studies will vary, it has become a common statistic in academic settings for it to take two to three months for a site to enroll its first subject. Additional effort in upfront planning can reduce this lag from study site activation to first subject enrolled (see below: Subject Recruitment Plan). Screening and enrollment logs are essential in measuring the study enrollment progress and are required as part of Good Clinical Practice (GCP) guidelines. Assessing the number of individuals screened to the number enrolled is critical to time and effort projections as well as enrollment timeline projections. Once the study has actually started enrollment, it is important to frequently compare actual to projected enrollment rates per month. • Symptom: High screening rates Early in the course of a study, there may be a high ratio of screened-to-enrolled subjects as the study team adjusts to the process of screening for participants. However, if a high ratio of screened-to-enrolled subjects continues, it is an important flag to reassess the recruitment plan. • Symptom: Lags in projected versus actual enrollment rates Assuming screening to enrollment rates are acceptable, lags in projected enrollment usually indicate problems in research staff workload, study recruitment plans, or may be related to study staff vacations or seasonal variation in subject availability. Seasonal variation in subject availability has been noted in national and international studies and is thought to be related to study subject vacations. In creating the initial enrollment projections for a study site, staff vacations and seasonal variability in subject availability must be taken into account. Potential treatments: Careful planning of study recruitment techniques and research staff allocation, including seasonal variation in initial pre-study projections, is the most effect preventative action. If there are screening problems or enrollment lags despite this "preventative medicine," based on the above differential diagnoses, consider: o re-assessing screening techniques and process, (i.e. re-education to screening process may be required, or screening to enrollment rates may be acceptable but the screening process may be too laborious or overly involved) Chapter 12: Research Project Management Page 2 of 12 Office of Human Research o assessing Clinical Research Coordinator workload and impact on the screening or enrollment process o reassessing inclusion/exclusion criteria o adding additional recruitment outreach actions o If all recruitment/screening remedies have been exhausted and it is not possible to adjust the inclusion/exclusion criteria, re-project workload, cost and enrollment rates, the study team and Investigator need to determine if re-projections are acceptable and therefore whether the study is still feasible. 1.1.3 Adverse Events Collecting and reporting adverse events are important elements of GCP; however, it is essential that rates of specific adverse events be followed to effectively assess safety trends across the study. Adverse event rates can be hand-tallied from paper tracking logs, or on electronic spreadsheets (e.g. MS EXCEL). Electronic tracking generally allows easy sorting by event type so that rates of events can be easily assessed. If the study intervention has an expected rate of certain adverse events based on previous experience or clinical studies, it is important to track expected versus actual rates of those events. Additionally, in assessing events it is important to see if there are research subject factors that seem to be common to a specific type of adverse event such as concomitant illness, concomitant medications, age, gender, etc. Looking for such possible associations is essential in determining the best course of action when serious adverse event types or rates of events are out of range from expected. • Symptom: Higher than expected rates of serious adverse events or reason to be alarmed about an unexpected event (due to apparent severity or relationship to study intervention) It is possible that the SAEs are: o a sporadic event o related to interaction between intervention and research subject characteristic o related to dose and dosing regimen for drug studies or interventional techniques for non-drug studies o related to study intervention and risk ratio still acceptable o related to study intervention and risk ratio not acceptable Potential treatment: When in doubt about the reasons for a rise over expected rates of serious adverse events or if there is reason to be alarmed about an unexpected event, it is essential to interrupt study enrollment and do a prompt but in-depth evaluation of safety, or in certain cases involving investigational medications, stop all administration of study article. Based on findings, follow-up actions may include revising inclusion/exclusion criteria (if the issue appears to be related to research subject characteristics), reassessing and adjusting dose and dosing regimen for drug studies or interventional techniques for non-drug studies (if the issue appears related Chapter 12: Research Project Management Page 3 of 12 Office of Human Research to how the study intervention is implemented), continuing the study with additional safety monitoring techniques and efforts, or discontinuing the study. See Premature Discontinuation of Study for issues to consider when discontinuing study subjects or discontinuing a study prematurely. Remember to summarize findings and actions to the IRB for any of the interventions noted above. 1.1.4 Data collection It is important to transcribe data onto the study Case Report Forms (CRF) in an ongoing fashion during the course of a study rather than wait until the end of the study to perform this function. To avoid a back-up of work on data collection, tracking completed study visits vs. completed visit-related CRFs is an effective way to keep on top of the workload. Once CRFs have been submitted for data entry, another important workload issue is the number of data queries generated to resolve data discrepancies. Tracking the number of data queries received vs. the number of answered queries helps manage this data task. • Symptom: Lag in CRF completion vs. study visits completed, or Lag in responding to data queries vs. number of queries received Time management problems, project work overload, overly complex CRFs • Symptom: Large number of data queries Learning curve in completing CRFs, inadequate attention to detail in completing CRFs, confusing or overly complex CRFs Potential treatments: review of CRF completion process, team training on time management, reassessment and redistribution of workload, slowing of study enrollment until backlog caught-up, possible redesign of problematic CRFs 1.1.5 Financial tracking Generally, study payments are triggered by certain milestones such as specific activities (e.g. screening and enrollment), specific visits completed, or Case Report Forms completed. Different departments and divisions have various methods of tracking studyrelated payments. The Office of Human Research offers the use of a Clinical Trials Management System – CREDIT. Clinical Research Environmental Data Information Tracking (CREDIT©) is a comprehensive web-based software program for all aspects of clinical trials administration and patient scheduling. CREDIT simplifies the management of clinical trials administrative tasks including tracking of patient schedules, simplification of record-keeping and reporting, notification of patients regarding changing protocol information, and IRB-related activities. At MHS, CREDIT is routinely utilized to track study related milestones as well as invoicing and receivables. At a minimum, it is important to regularly track study milestones and their dollar value against payments received, and to compare total study budget versus expenditures. You Chapter 12: Research Project Management Page 4 of 12 Office of Human Research can work with the Office of Human Research for the optimum method of financial tracking for your studies. 1.2 Study Management Meetings It is imperative to hold regularly recurring meetings between the Principal Investigator and the Clinical Research Coordinator to review the key measures of study progress noted above in Tracking Key Parameters. The standard interval for these regularly occurring meetings will vary depending on type of study or portfolio of studies, however it is critical to set aside adequate time on a regular basis for such meetings. The structure of these meetings is decided in the study planning phase, so that when the study is up and active, everyone is aware of his or her role, the expected tracking reports and required update information for the meetings, and the date, time and interval of the meetings. It is important that the key tracking reports are completed and current at the time of the meeting, and that other issues for discussion are identified and ready for action (e.g. outstanding laboratory review, new operational issues or problems, etc.). 2. Study Documentation Management The research records provide vital historical documentation of the research activity, correspondence, and project management. Any clinical research study by nature both requires and produces a sizable amount of documentation. A methodical and wellexecuted system for managing these documents is critical for efficient project management and regulatory compliance, and is also a requirement of federal regulations and Good Clinical Practice (GCP) guidelines. The Principal Investigator (PI) is ultimately responsible for ensuring proper record maintenance. The PI often delegates this responsibility to the Clinical Research Coordinator (CRC). This section groups the various types of study documentation into four file systems: 2.1 Study Administrative File/Regulatory File Federal regulations require the existence and maintenance of documents relating to the study. These documents, when properly maintained, provide clear evidence that the study has been conducted according to federal regulations and GCP guidelines. The Study Administrative File is the central file for all of these critical regulatory documents. The structure and contents of the Study Administrative File are covered in this section. 2.1.1 Study Administrative File Contents The following is a list of the documentation that should be kept in the Study Administrative File, as well as guidelines for maintaining the binder. The order of the different sections may vary according to need. In general, the most frequently used sections should be closer to the beginning. Also consider dividing the contents of the Study Administrative File across more than one binder. For example, a study may have Chapter 12: Research Project Management Page 5 of 12 Office of Human Research 3 binders - 1 binder with all Correspondence, a second binder with all Study Documents and Research Personnel, and a third binder with all Study Tracking Logs. Protocol • • • Protocol o The document that describes the objective(s), design, methodology, statistical considerations, and organization of a research study. o Maintain all versions in file. Protocol Signature Page o Contains a statement that the Principal Investigator (PI) will comply with all protocol requirements and applicable research regulations and GCP o The PI must sign and date the protocol signature page Protocol Amendments o A written description of a change(s) to or formal clarification of a protocol o Each amendment should indicate a date of revision and version number o Note : Protocol amendments must be IRB-approved before being implemented Case Report Form Sample • Clean Copy of the paper Case Report Form o • All versions of the CRF should be maintained Case Report Form Completion Guidelines Curricula Vitae and Licenses • • • Curriculum Vitae (CV) o A summary of the educational and academic backgrounds, teaching and research experience, publications, presentations, awards, honors, affiliations of each research staff o CVs should be maintained for the PI, Sub-Investigators and Research Coordinators o CVs should be signed and recent (within 2 years) Medical Licenses o Current professional licensure should be present for physicians and other licensed personnel o The CV and license documents the qualifications and eligibility of staff to provide medical supervision and to conduct the study Training Certificates Chapter 12: Research Project Management Page 6 of 12 Office of Human Research o May include copies of relevant training certificates (Protocol training, GCP CITI training, HIPAA training, e-CRF, IATA, etc.) Signature/Delegation of Responsibility Log • • Signature Form o A document that contains examples of the signatures and initials of research staff o Any provision of signature authorities approved by the PI should be included Delegation of Authority Log o A document that identifies the study-related tasks that the PI has delegated to other research staff o The delegation log and signature form may be combined into a single document o May include a clear description of activities conducted by key staff at collaborating sites Informed Consent • • • Informed Consent Form o A copy of the IRB-approved Informed Consent Form must be kept on file o A consent form is not valid for subject use without an affixed IRB approval stamp on the first page o All versions of the approved consent are kept in the regulatory files: the original version and all revisions IRB Approved Educational Materials and Advertisements o Information describing the study that is to be presented to subjects in verbal or written form, including recorded audiovisual media o These material help substantiate that subjects were given appropriate information to support their ability to give fully informed consent HIPAA Authorization Form/Waivers o A copy of the HIPAA Authorization that was submitted to the IRB must be kept on file o All versions of the HIPAA Authorization forms are kept in the regulatory files: the original version and all revisions o If there is no HIPAA Authorization Form for the study, include the IRB Waiver of HIPAA Authorization letter or other documentation to support the fact that HIPAA Authorization is not required. Chapter 12: Research Project Management Page 7 of 12 Office of Human Research Laboratory Documents • • Laboratory Certifications and Licenses o Required for studies utilizing laboratory data or results o Provides evidence of the competence of the facility to perform the required test(s) and supports the reliability of the lab results o Certifications may include: the state laboratory license/permit (AHCA), an accreditation by The College of American Pathologists (CAP), Clinical Laboratory Improvement Amendment Accreditation (CLIA), and the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) , CV of laboratory license holder, medical license of laboratory director Normal Reference Ranges o • Laboratory reference ranges may vary from laboratory to laboratory; therefore, it is necessary to include documentation of the laboratory's normal range values. All updates to the laboratory ranges must also be maintained. Lab Manual(s), if appropriate Correspondence with Institutional Review Board (IRB) & Other Reviewing Entities • • IRB Correspondence o Correspondence between the research site and the IRB regarding the conduct of the study and the research subjects o IRB correspondence may include: approval letters, protocol amendments, changes to the consent form, study updates, protocol violations, adverse event reporting, continuing review reports, and notification of study termination IRB Membership/Assurance o MHS IRB issues a Federal Wide Assurance number (FWA00003898) that documents the IRB is in conformance to federal regulations. Please contact the IRB or OHR if further information regarding the FWA number is required. • Sponsors • Federal Agencies Subject Logs • Screening Log o Identifies who was evaluated for the study and documents the criteria that excluded them from study participation Chapter 12: Research Project Management Page 8 of 12 Office of Human Research o • Generally, subjects who were reviewed or consented for study participation, but were then found to be ineligible are considered screen failures Enrollment Log o Confidential list with identifiable information (e.g. name, date of birth, date of hospital admission) o Identifies subject enrollment in chronological order o Subjects who enrolled in the study and who withdrew or have been withdrawn General Correspondence o Includes relevant communication between investigative sites, clinical personnel, pharmacy, sponsor, etc. regarding study administration, study conduct, subject management, protocol violations, and adverse events o Correspondence may take the form of letters, facsimiles, telephone discussions, and emails Document correspondence in such a manner that the date, persons involved, and relevance to the study is apparent o Facsimile confirmations and shipping receipts should be saved and filed with the corresponding documents as proof (receipt) of communication o Telephone calls may be documented on a Telephone Contact Log Adverse Events o Adverse Events (AE) and Serious Adverse Events (SAEs) Tracking Log o Investigational New Drug (IND) Safety Reports (including MedWatch forms) o Data and Safety Monitoring Board or interim analyses reports o Documents tracking AE Reporting (e.g. IRB, sponsor, federal agencies, etc.) Protocol Deviations o All deviations from the protocol should be tracked on a Protocol Deviation Log Monitoring • Monitor Signature Log and Visit Record o • Tracking document that records the visits made by the monitor throughout the course of the study Study Initiation Reports o Letter documenting that the procedures were reviewed prior to study initiation and the site was determined to be suitable for enrollment Chapter 12: Research Project Management Page 9 of 12 Office of Human Research • Interim Monitoring Reports o • Close-Out Report o • Letter documenting the findings after each monitoring visit A report or letter documenting that the study had a final monitoring visit after the conclusion of the study to ensure any outstanding issues have been resolved Monitor Curriculum Vitae (CV) o If monitor is hired by the PI, a copy of the monitor's CV For studies involving drugs and devices, additional sections are required to be included the regulatory binder. 2.1.2 Regulatory Binder - Additional Elements for Drug and Device Research For studies involving an Investigational New Drug (IND) or Investigational New Device (IDE), these documents must be maintained in addition to the regulatory documentation required by GCP standards and federal regulations. FDA Form 1571 (if applicable) o FDA form cover sheet for Sponsor-Investigators filing an IND application o Prior to study initiation, an investigator submits a 1571 to propose studying an unapproved drug, or an approved product for a new indication or in a new patient population FDA Form 1572 o FDA form that declares the Principal Investigator's commitments and identifies the participating personnel, institution, and facilities in the study o The original, signed 1572 is be filed with the sponsor prior to study initiation and a copy will be placed in the regulatory files o If changes or additions are made, a new 1572 must be completed, resubmitted to the sponsor, and a copy is stored in the Regulatory Binder with previous versions o FDA regulations do not require a 1572 to be filed for device trials Investigator's Brochure and Product Labeling • Investigator's Brochure o Provides relevant and current scientific information about the investigational product o If an Investigator's Brochure will not be utilized, an equivalent packet of information (such as package insert) with safety information should be kept on file Chapter 12: Research Project Management Page 10 of 12 Office of Human Research o • Maintain most current brochure including updates and revisions Product Labeling and Handling Instructions o Maintain a sample of the label(s) attached to the containers o Include instructions for handling the investigational product o If applicable, include procedures for un-blinding Drug/Device Accountability • Accountability Forms o Drugs and devices must be inventoried via a tracking or accountability form o Documentation may include shipments, receipt, dispensation, return and destruction of the investigational product o Include shipment receipts and supply correspondence o For drug studies utilizing MHS Investigational Drug Services (IDS), these can be kept in the pharmacy during the study, but should be placed in the regulatory binder at study closeout o The National Cancer Institute (NCI) mandates use of the Agent Drug Accountability Record Form (DARF) for investigational medications. This template is available at Form, Templates & Documents. 2.2 Financial Documents File The financial documents include any agreements, contracts, disclosures, salaries or grant funding documents. Financial Records are not considered regulatory documents and should be kept in a separate confidential file. The structure and contents of the financial documents are covered in this section. Typically, this file will be maintained at the OHR. 2.2.1 Financial Documents DO NOT include financial documentation in the Regulatory Binder. Financial documents should be stored in a separate secure location in the OHR. • Contract o Financial Agreement o Insurance Statement o Indemnification • Salaries & Grant funding documents • Financial Disclosures Chapter 12: Research Project Management Page 11 of 12 Office of Human Research o For all MHS investigators, include copy of Confidential Financial Disclosure Form o For studies sponsored by other organizations (such as pharmaceutical companies), the Sponsor may provide a Financial Disclosure Template that would need to be maintained in the Regulatory File. o For FDA studies, study personnel must complete a Form FDA 3454 Financial Interests or 3455 Arrangements of Clinical Investigators which reveals all significant financial arrangements with the sponsor, proprietary interest in the investigational product, or significant equity interest while conducting the study and for a period of 2-3 years thereafter. These forms are available from the FDA Electronic Forms page FDA Forms 2.3 Informed Consent File While copies of the signed Informed Consent Forms are included in several places, it is recommended that the original signed Informed Consent Forms be kept together in one binder. Alternatively, original signed Informed Consent Forms may be maintained in the Regulatory File. Most regulatory auditors are interested in reviewing every consent form. Keeping the original informed consent forms in one file facilitates this review, removes the burden of collecting all subject files and reduces the likelihood of expanding the audit scope. 2.4 Subject Files/Case Report Files Each study subject should have an individual file, where copies of forms, data, and records of correspondence are maintained. The Subject File is described in more detail in Study Procedures. 3. Data Management At the heart of all research projects are the data to be collected and analyzed. Careful data management procedures are critical to maintaining data integrity. Proper procedures ensure that data are identifiable, verified, validated, retrievable and protected. The various components of data management include: data collection, data entry, data verification, and data validation. When properly executed these steps prepare data for statistical analysis. Chapter 12: Research Project Management Page 12 of 12 Office of Human Research Chapter 13: Investigational Product Inventory The Principal Investigator is responsible for securing, dispensing, and accounting for all study drugs or devices that are received. The sponsor is responsible for assuring that the investigator is meeting these requirements. Throughout the study, Drug/Device Accountability includes: • Documenting drug/device shipment and receipt • Dispensing/utilizing the investigational product according to protocol • Maintaining an accountability log • Maintaining randomization (if applicable) • Ensuring blinding (if applicable) • Ensuring proper and secure storage conditions • Documenting any drug/device that is returned to sponsor or destroyed Through investigational product inventory records, any member of the research team or an outside auditor should be able to track every unit of the investigational product from the time it leaves the manufacturer until the time it is used by a subject, destroyed or returned back to the manufacturer. The Investigational Drug Services (IDS) Pharmacists at MHS can be contracted to manage study drugs and non-significant risk devices, as well as maintain accountability for outpatient clinical studies. 1. Storage of Drugs/Devices 1.1 Storing Medications Generally, medications need to be: • kept in a locked room, drawer or cabinet with restricted access • secure and accessible only to authorized pharmacy staff or delegated members of the study team • stored separate from samples, food, blood products, and commercial drugs • adequately labeled • inventoried via a tracking or accountability form 1.2 Temperature Requirements "Room Temperature" is defined by the United States Pharmacopeial Convention (USPC) as 59º to 77ºF (15º to 25ºC). This is the recommended storage temperature for most medications. Some drugs, such as capsules or powders, may start to degrade when exposed to warmer temperatures or to moisture. Chapter 13: Investigational Product Inventory Page 1 of 5 Office of Human Research Medications requiring room temperature storage should be kept in a dry place, free from moisture. Storage near radiators, windows or sinks should be avoided to prevent exposing the medication to moisture. "Refrigeration" is defined by the USPC as 38º to 46ºF (2º to 8ºC). Note: Do not store refrigerated medications with food. A medication refrigerator must be used ONLY for medications; this is a Joint Commission on Accreditation of Healthcare Organizations (JCAHO) requirement. A thermometer should be kept in the refrigerator and checked regularly to assure that the refrigerator stays within the proper temperature range. The staff should maintain a temperature log, recording periodic temperature readings. Excursions outside of the approved temperature ranges must be reported to the sponsor expeditiously to assess the validity of the drug product. "Frozen" is defined by the USPC as -4º to 14ºF (-20º to -10ºC). If using a common household refrigerator with a freezer compartment, a lowtemperature thermometer should be obtained to check it regularly, as these freezers fluctuate in temperature throughout the day. The staff should maintain a temperature log, recording periodic temperature readings. Excursions outside of the approved temperature ranges must be reported to the sponsor expeditiously to assess the validity of the drug product. 1.3 Storing Devices Devices will generally be stored within the department it will be used in. The devices need to be: • kept in a locked drawer or cabinet with restricted access • secure and accessible only to authorized pharmacy staff or delegated members of the study team • adequately labeled • inventoried via a tracking or accountability form 2. Product Labeling Proper labeling of an investigational product is an essential part of Good Clinical Practice (GCP) guidelines and is important in reducing medication errors. Labeling of ANY prescription drug, whether marketed or investigational, is required by federal and state law. This is especially important if the subject is having an adverse reaction or if the subject is admitted to an outside healthcare institution. For investigational drugs, Florida Code outlines the following items to be included on a label: • Name of study drug (if blinded, see below for suggested wording) • Serial number of the prescription (optional for clinics, mandatory for pharmacies) • Name of the subject & unique identifier or randomization number Chapter 13: Investigational Product Inventory Page 2 of 5 Office of Human Research • Complete directions for use, including precautions • Name of the prescriber • Phone number that subject can call for assistance, typically a 24-hour contact number is used • The date dispensed • The following statement: "CAUTION: New Drug - Limited by Federal Law to Investigational Use" Note: To best document drug assignment, a copy of the label may also be included in the subject's file, typically affixed to the subject's CRF. The label can be designed with a perforation so that a removable copy can be detached at the time of dispensation. 2.1 Blinded Studies When conducting a blinded study, include the names of both study drugs and/or placebo on the label. A method for unblinding in the event of an emergency should be detailed in the protocol, and a member of the study team should have a means for breaking the blind. • Example: "Study Drug Name: Drug X / placebo 40 mg" • Example: "Study Drug Name: Drug X 40 mg / Drug Y 80 mg" 2.2 Supplemental Labels For industry-sponsored studies, the sponsor may provide investigational agents in prepackaged containers. However, the investigator is still required to supplement the sponsor's label with any missing information (discussed above) in a supplemental label. 3. Dispensing Drugs/Devices 3.1 Dispensing Medication If dispensing study drugs, the investigator or a member of the research team must properly store, secure, track, and inventory the study drug. The JCAHO requires that anyone administering an investigational product have a working knowledge of the drug including its purpose, side effects, and precautions. Therefore, the investigator should take care to in-service the clinical staff as well as provide access to written materials describing the investigational product. 3.2 Investigational Drug Service If utilizing MHS Investigational Drug Services (IDS), the research pharmacy will store and dispense the study drug, retain detachable labels, maintain shipping records and complete accountability/dispensation forms. Chapter 13: Investigational Product Inventory Page 3 of 5 Office of Human Research Study drugs ordered from the IDS should indicate the dose, frequency, and time of delivery in addition to the subject, the study and, when applicable, the subject weight. In randomized studies, the pharmacist may need to be informed of the randomization assignment or randomization numbers. Unused study drugs or returned empty containers should be returned to IDS for inventory and tracking. At the conclusion of the study, discrepancies are resolved through the coordinated efforts of the pharmacist, the research team, and the sponsor (if applicable). 3.3 Dispensing Devices Devices will be stored in a locked cabinet or drawer within the department it will be used in. Dispensing devices requires the same documentation mentioned with regards to drugs (i.e. shipping records, accountability/dispensing records etc.) 3.4 Drug/Device Accountability Records Accountability records may include the following documentation: • Certificates of analysis • Sample of labels • Handling instructions • Master randomization list • Un-blinding procedures • Shipping receipts • Accountability Log Accountability records should be incorporated into the regulatory binder. Depending upon the type of study and the delegated responsibilities, accountability records may be handled by the clinical research staff, pharmacist, or sponsor. 3.5 Accountability Log The accountability log is a standardized tool for documenting exactly what happens to a medication or device during the course of a study. The log documents the receipt, the dispensation, the transfer to other sites, and the return or destruction of the investigational product. Drugs and devices are inventoried by the lot and/or serial numbers. Note: All unused, expired or damaged products must be returned to the IND/IDE holder or manufacturer who supplied the products. If the investigator is the IND or IDE holder, he or she must carefully document destruction of the investigational. Chapter 13: Investigational Product Inventory Page 4 of 5 Office of Human Research Templates are available from the OHR. The National Cancer Institute (NCI) mandates use of the NCI Investigational Drug Accountability Record Form for investigational medications. This template is available at ctep.cancer.gov/forms/index.html. Chapter 13: Investigational Product Inventory Page 5 of 5 Office of Human Research Chapter 14: Adverse Events and Unanticipated Problems During the course of conducting clinical research, events occasionally occur that were not anticipated and involve risk to the subjects or others. Typically in drug and device trials, researchers think of abnormal reactions to a study medication and intercurrent medical problems as an event that needs to be documented and reported. However, in addition there exists a much broader set of “events” that require attention and reporting, generally classified as “Unanticipated Problems Involving Risk to Subjects or Others.” It’s important to consider this broader definition when assessing an event. 1. Definitions (Adverse Events/Unanticipated Problems) Unanticipated Problems Involving Risk to Participants or Others This is an event that: • Was unanticipated --and-- • Suggests that participants or others are at greater risk of harm than was previously known or recognized. This definition specifically includes the following: • Information that indicates a change to the risks or potential benefits of the research, in terms of severity or frequency. For example: o An interim analysis indicates that participants have a lower rate of response to treatment than initially expected o Safety monitoring indicates that a particular side effect is more severe, or more frequent than initially expected o A paper is published from another study that shows that an arm of your research study is of no therapeutic value • Change in FDA labeling or withdrawal from marketing of a drug, device, or biologic used in a research protocol. • Breach of confidentiality. • Incarceration of a participant when the research was not previously approved under Subpart C and the investigator believes it is in the best interest of the subject to remain on the study. • Event that requires prompt reporting to the sponsor • Complaint of a participant when the complaint indicates unexpected risks or the complaint cannot be resolved by the research team. • Protocol violation (meaning an accidental or unintentional change to the IRB approved protocol) that placed one or more participants at increased risk, or has the potential to occur again. • Sponsor imposed suspension Chapter 14: Adverse Events & Unanticipated Problems Page 1 of 7 Office of Human Research Unexpected/Unanticipated An event is classified as “unanticipated” when the specificity or severity is not reflected in the study documents including the protocol, informed consent document, or the investigator brochure. In most cases, an unexpected or unanticipated event heightens the urgency for reporting. Related to Study Procedures The determination of how likely the event is related to the study procedures is made by the principal investigator, the classification of which may vary. The IRB asks if the event is "more likely than not" related to the study procedures. FDA regulations consider an adverse event associated if is "reasonably" or "probably" caused by the drug. Involved Risk to Participants or Others "Participants or others" may involve anyone, including research subjects, research staff, or others not directly involved in the research. The unanticipated problem can occur in either clinical or non-clinical research. "Risks" include physical, psychological, economic, legal or social consequences. 2. Drug and Device Research Definitions When involved in drug and device research, researchers must also be familiar with terminology used to define and classify unanticipated problems. Adverse Event (drug and biologics research) An Adverse Event (AE) is a subcategory of the broader category of "Unanticipated Problems Posing Risk to Participants or Others", most commonly used in drug and device studies. An adverse event is defined as: • any unfavorable or unintended sign (including an abnormal laboratory finding), symptom, or disease occurring at any stage of the study • may include an exacerbation of a pre-existing condition, intercurrent illness, drug interaction, drug overdose, failure of expected action or significant worsening of the disease under study • an event that may compromise the rights, safety, or welfare of research subjects Any event that could be characterized by the definitions above is an AE whether or not considered related to the study or product. Chapter 14: Adverse Events & Unanticipated Problems Page 2 of 7 Office of Human Research Serious Adverse Event (drug and biologics research) An AE becomes a Serious Adverse Event (SAE) when any of the following outcomes occurs: Death Life-threatening experience Inpatient hospitalization or prolongation of hospitalization Persistent or significant disability/incapacity Congenital anomaly/birth defect in the subject's offspring An important medical event that, based upon appropriate medical judgment, may jeopardize the subject and may require medical or surgical intervention to prevent one of the outcomes listed above. Unanticipated Adverse Device Effect (device research) Any serious adverse effect caused by or associated with a device that was not previously identified in nature, severity, or degree of incidence in the investigational plan or application; or any other unanticipated serious problem associated with a device that relates to the rights, safety, or welfare of subjects. Investigators who hold an IDE for a device study must conduct an immediate investigation of any unanticipated adverse device effects. If the sponsor determines that the effect poses an unreasonable risk to subjects, the sponsor must terminate all investigations that present that risk as soon as possible, but within 5 working days after the determination. A terminated study may not be resumed without IRB approval (for Non-Significant Risk Device studies) or FDA and IRB approval (for Significant Risk Device studies). 3. Documentation (Adverse Events/Unanticipated Problems) 3.1 Documenting Non-serious Adverse Events Non-serious AE's are typically documented in the appropriate source documents where applicable (i.e. medical chart or subject record), the Case Report Form, and the Adverse Event log of the Regulatory Binder for the study. Documentation should include the following information: • Protocol name and numbers • Subject identifiers • Date and time of onset and outcome • Course • Intensity Chapter 14: Adverse Events & Unanticipated Problems Page 3 of 7 Office of Human Research • Action taken • Relationship (causality) to the study • Outcome 3.2 Documenting Serious Adverse Events An SAE Form should be used to document all SAEs for the study. The form should capture the following information: • Protocol name and number • Subject identifiers • Demographic data • Nature of the event • Severity of the event • Probable relationship (causality) of SAE to study or investigational product • Date and time of SAE onset • Date and time of SAE resolution, if available • Clinical assessment of subject conducted at time of SAE • Results of any laboratory tests and/or diagnostic procedures • Autopsy findings (if appropriate) • Outcome • Follow-up plan • Studies involving an investigational article • Lot number and expiration date • Possible test articles involved (investigational product, comparator, or placebo) with administration start/stop date • Dose, frequency, and route of administration • Concomitant medications and therapies: the Sponsor-Investigator and/or the reporter should separately list the concomitant medications that the subject was taking for the treatment of his/her underlying medical conditions and also the concomitant medications plan The SAE Form is often provided by the sponsor as part of the CRF for industrysponsored studies, but needs to be developed on-site for investigator-initiated and grantfunded studies. A suggested SAE form template is available for download to customize for a specific study. 4. Reporting Serious Adverse Events Chapter 14: Adverse Events & Unanticipated Problems Page 4 of 7 Office of Human Research Depending on the nature of the event and the study, Unanticipated Problems Posing Risk to Subjects or Others and Serious Adverse Events (see previous section for definitions) are required to be reported to one or more of the following: • The IRB • The Sponsor (for industry-sponsored studies) • The FDA (for sponsor-investigators) • Participating sites (for sponsor-iInvestigator of multi-center studies) • Federal funding agencies If more time is needed to prepare a complete report than the reporting time requirement allows, then the immediate report can be incomplete, and then supplemented as soon as possible with a more detailed, written report. When reporting adverse events, the subject should not be identified by name. Study identifiers should be used to protect subject confidentiality. 5. IRB Reporting The IRB should be notified of Adverse Events only when they are both: • Unexpected AND • More likely than not related to the study Adverse Events and other "Unanticipated Problems Posing Risk to Subjects or Others" that meet the criteria above should be reported to the IRB promptly, defined as within 10 days. Several MHS studies are currently under the review of the Western IRB (WIRB); the WIRB website provides access to forms and instructions for submitting Unanticipated Problems that ARE and ARE NOT adverse events (http://www.wirb.com/Pages/DownloadForms1c.aspx) 5.1 Expedited IRB and Sponsor Reporting • When a death of a research subject indicates that subjects or others are at increased harm, that event must be reported to the IRB within 24 hours. • When death of a research subject occurs in an investigator-sponsored research project the death must be reported to the IRB within 72 hours, regardless of relationship to the study or study investigational agents. 5.1.1 Reporting Mechanisms The IRB is should be notified promptly when an SAE becomes known to the study team. The MHS IRB Principal Investigator’s Adverse Event Reporting Form must be completed and submitted according to the reporting requirements. Chapter 14: Adverse Events & Unanticipated Problems Page 5 of 7 Office of Human Research 5.1.2 Sponsor Reporting As a general rule, Serious Adverse Events should be reported promptly to the sponsor when applicable (the protocol may identify events that do not need to be reported to the sponsor). Although “promptly” is not defined in FDA regulations in terms of reporting to the sponsor, an industry standard for reporting to the sponsor is within 24 hours of discovery of the event. 5.5.3 Expedited Sponsor Reporting • Any event that is life-threatening or fatal is required to be reported immediately to the sponsor in industry-sponsored research. 5.5.4 Reporting Mechanisms • 6. Sponsor reports of Serious Adverse Events are typically submitted through a form provided by the sponsor. When not provided, the SAE form discussed in the previous section is recommended FDA Reporting (Drug, Biologic and Device Studies) Serious Adverse Events that are not “unexpected” - whether or not they are associated with the use of the drug or device - are reported to the FDA in the Annual Safety Report. 6.1 Expedited FDA Reporting • An SAE that is drug-related and unexpected must be reported to the FDA within 15 calendar days of discovery of the event • An SAE that is drug-related, unexpected and life-threatening or fatal must be reported to the FDA within 7 calendar days of discovery of the event • An unanticipated adverse effect involving a Significant Risk device that is devicerelated and unanticipated must be reported to the FDA within 10 working days of discovery of the event. o If such an event is found to pose an unreasonable risk to subjects, the study must be terminated within 5 days after the sponsor makes this determination and no later than 15 days after discovery of the event 6.2 FDA Reporting for Studies that are IND Exempt Good Clinical Practice standards apply for all drug and device research at MHS regardless of IND or IDE status. Although the regulations do not define specific timelines for spontaneous reporting, it is recommended in the case of such a need for an INDexempt study, that the IND standards of 15 days for non-life threatening, and 7 days for life-threatening serious, unexpected, drug-related adverse events are followed. Chapter 14: Adverse Events & Unanticipated Problems Page 6 of 7 Office of Human Research However, there is no requirement for providing the FDA with an annual safety report (I.e. the annual IND report). 6.3 Reporting Mechanism The FDA is notified using the MedWatch form. The MedWatch form can be downloaded from the FDA web site (www.fda.gov/opacom/morechoices/fdaforms). 21 CFR 312.32(c) 6.4 Reporting to Federal Funding Agencies NIH and other federal agencies that provide funding for clinical studies often have additional reporting requirements. Examples of some federal funding agency reporting requirements are: • National Cancer Institute ( NCI ) o • National Heart, Lung, and Blood Institute (NHLBI) o 7. NCI utilizes ADEERS (Adverse Event Expedited Reporting System), a web-based system for submitting serious and/or unexpected events. All trials using a NCI -sponsored investigational agent are required to use this system, which can be accessed at: ctep.cancer.gov/reporting/adeers.html NHLBI requires additional reporting to its agency, according to guidelines which can be found at: http://www.nhlbi.nih.gov/funding/policies/adverse.htm Reporting for Participating Sites Sponsor-Investigators (holding an IND or IDE) of studies that are being conducted at multiple sites are also required to report SAEs to the investigators at those participating sites. For both drug and device studies, this notification should be done concurrently with notification to the FDA. 21 CFR 312.32(c) (1), 21 CFR 812.150(b) (1) Resources: Western Institutional Review Board forms and instructions for submitting Unanticipated Problems that ARE and ARE NOT adverse events Chapter 14: Adverse Events & Unanticipated Problems Page 7 of 7 Office of Human Research Chapter 15: Data and Safety Monitoring 1. Data Monitoring Data monitoring is necessary to verify the study data and assess compliance with the protocol. A study monitor (which can be a Clinical Research Associate, or CRA) reviews study documentation to assess the initiation, progress, and conduct of the research study in order to ensure the scientific integrity of the data and the protection of study subjects. The industry standard is that the monitor is independent of the conduct of the study. In drug or device studies conducted under an Investigational New Drug (IND) application or an Investigational Device Exemption (IDE), it is the responsibility of the IND/IDE holder to conduct periodic data monitoring visits. The industry sponsor will send a monitor to the study site. All federally-funded studies must have a data and safety monitoring plan. Refer to the funding agency for data and safety monitoring plan guidelines. In investigator-initiated studies where the MHS investigator holds the IND or IDE, monitoring services are often contracted with an external agency or contractor. The Office of Human Research will also conduct periodic monitoring visits. The investigator should ensure that monitoring visits are conducted at intervals specified in the Data and Safety Monitoring Plan. The frequency of monitoring activities depends primarily upon the risk of the study. The higher the risk to subjects, the more frequently monitoring should be conducted. Monitoring frequency can also depend upon the size of the study, the accrual rate, and the complexity of the Case Report Form (CRF). In general, there is a need for on-site monitoring before, during and after the study. The monitor may also conduct unscheduled visits as needed based upon reports or evidence of potential noncompliance with the protocol or other concerns about the proper conduct of the study or research subject safety. Significant increases in enrollment rates and changes in the protocol or key study personnel may also trigger an unscheduled monitoring visit. The monitor will confirm the date and logistics of the monitoring visit in writing and provide the investigator with a list of records and source documents (e.g. hospital charts, laboratory records, etc.) that will be reviewed during the monitoring visit. At each visit, the monitor must sign the site visit log in the regulatory documents. Monitoring should take place in a private area with access limited to the project and subject record(s) under review. The goals of the study monitor are to assess compliance with the research protocol, federal regulations and Good Clinical Practice (GCP). Chapter 15: Data & Safety Monitoring Page 1 of 3 Office of Human Research The review activities will vary from visit to visit and may include any or all of the following: • Informed Consent o • Drug and/or Device Accountability o • Confirm that all enrolled subjects met inclusion/exclusion criteria for study participation and documentation exists to verify the fulfillment of eligibility criteria Adverse Events/Serious Adverse Events (AEs/SAEs) o 2. Confirm contents of the Regulatory Binder fulfill regulatory and GCP guidelines Eligibility Criteria o • Confirm that the data recorded on the CRF is consistent with the corresponding data in the source documents. Regulatory Documents o • Confirm proper documentation of receipt, storage, dispensation, and return or destruction of the study drug/and or devices Source Data o • Confirm appropriate documentation of the informed consent process Confirm that AEs/SAEs are captured, accurately documented, and reported in a timely manner. Communicating Findings At the conclusion of each monitoring visit, the monitor should meet with the Principal Investigator and/or Research Coordinator to review any monitoring findings and discuss management to determine appropriate action and resolution. It is the PI's responsibility to ensure that the recommended actions are implemented. 3. Safety Analysis Safety analyses are an essential element of study oversight that involves periodic assessments of the study population. A safety analysis protects the well-being of the study population by ensuring a comprehensive review of the overall data and safety information, compliance to the protocol, and other factors that can affect subject safety. A safety analysis should also incorporate factors external to the study, including scientific or therapeutic developments in the disease under study. This process facilitates an ongoing evaluation of the risk-to-benefit ratio. Safety monitoring involves reviewing the available data, preferably through a safety analysis, and making recommendations to continue, modify, or terminate the research Chapter 15: Data & Safety Monitoring Page 2 of 3 Office of Human Research study. Safety monitoring is always managed by the Principal Investigator for his or her subjects. In addition, safety monitoring can also be conducted by an independent medical monitor, committee, or Data & Safety Monitoring Board. The timing of a safety analysis will be dependent upon several factors including the likelihood of risk, the actual occurrence of adverse events, the natural history of the disease, the effect of the intervention, and the power of the study design. The number of events that occurs in a group determines the power of the study. A multi-center, high-risk study involving a patient population with a large number of adverse events will require more frequent oversight than a small, minimal risk study involving healthy volunteers. The data reviewed during a safety analysis will vary based upon the study design, but usually includes reports on the subject population, enrollment, adverse events, laboratory findings, protocol compliance, and study endpoints. It is important to monitor for imbalances between the expected and actual rates of adverse events. A safety analysis will not only look for clear evidence of benefits or harms, but will also monitor concerning data trends. Good clinical judgment and a working knowledge of the population are crucial to the decision-making process. In certain patient populations, there may be no other way other than by statistical analysis, to know whether the adverse events are related to the study or the underlying disease and a formal interim analysis may be necessary. Note: If new risks or benefits are discovered during the course of a safety analysis, the investigator is responsible for notifying the appropriate regulatory/oversight groups, revising the Informed Consent Form, and re-consenting previously enrolled subjects. 4. Interim Analysis An interim analysis is a preplanned analysis conducted at some point during the study to assess safety and in some studies, efficacy. There can be more than one interim analysis depending on the safety plan. The interim analysis provides an opportunity to invoke 'stopping rules' to prevent research subjects from being exposed to unnecessary risk. For example, the study may be stopped early because the new intervention is better, a substantial number of subjects experience serious side effects, or there is clear evidence that the study is going to be negative. Generally, stopping rules are asymmetrical- a more conservative boundary is reserved for adverse effects than for beneficial effects. Since the interim analysis is conducted on a data set smaller than planned for the final study analysis, it is important that the statistical plan employ accepted methods designed for interim analyses. These methods require a more extreme result than the conventional p< 0.05 to account for the decreased statistical power. Each time an interim analysis is performed, it has an effect on the power of the final analysis of the study. Therefore the overall statistical analysis plan for a study must be designed to account for effects on power from planned interim analysis. Chapter 15: Data & Safety Monitoring Page 3 of 3 Office of Human Research Chapter 16: Protocol Modifications 1. Protocol Amendments An amendment is any change to the research protocol that is approved by the Principal Investigator (PI) of the study. Amendments to the protocol may be initiated by the study sponsor, the PI, or may be recommended by an Institutional Review Board (IRB) or other regulatory entity. Protocol amendments include administrative changes, clarifications, study modifications and changes to the study design. The investigator will notify the IRB, Food and Drug Administration (FDA), and other investigative sites of the protocol amendment (as described below). The investigator is also responsible for notifying the appropriate individuals, groups, or departments that may be affected by a change in the study plan. This may include other individuals providing care, fellow research team members, and the departments responsible for implementing study procedures. 2. Submission to IRB Amended protocols must be forwarded to the IRB for review and approval. Protocol amendments may not be initiated until the IRB has granted its approval. If the changes are minor or present no more than minimal risk, the amended protocol can be submitted for Expedited Review and approval by the IRB chair. Major protocol revisions will require a Full Board Review. If the amendment necessitates changes to the consent form, a revised consent form should also be submitted to the IRB for review and approval. It may be necessary to have previously consented subjects sign the revised consent form. Previously enrolled subjects must be re-consented if there are changes made to the procedures they will undergo, the consent includes pertinent new information, or the revisions may affect their willingness to participate. Consult the IRB if you are uncertain whether this is necessary. Protocol changes may require modification of other IRB-approved study documents, such as advertisements, HIPAA Authorization, or subject data collection forms given to the subject. These revisions must also be submitted to the IRB for approval. The most current version of the IRB-approved documents should always be used with study subjects. 2.1 Updates/Minor Changes Occasionally, there may be new information or changes that do not necessarily require a formal protocol amendment. Examples include location or staff changes, updated information on investigational products (such as its approval in another therapeutic area), or interim analysis of study data. Pertinent information should be communicated to the IRB in a timely manner. If a new Principal Investigator or sub-investigator is added to the protocol, the following documents must be submitted to the IRB: investigator's Curriculum Vitae (CV), CITI GCP training certificate, financial disclosure form or Conflict of Interest disclosure, and a Chapter 16: Protocol Modifications Page 1 of 7 Office of Human Research memo from the PI with a signature indicating acceptance of the sub-investigator’s role on the project. 3. Submission to FDA (Sponsor-Investigators) Protocol amendments made by the Sponsor must also be submitted to the FDA when the revisions significantly affect the safety of participants and/or significantly affects the scope of investigation or scientific quality of the study. Significant protocol changes cannot be implemented without a submission to the FDA and an approval from the IRB (and other applicable regulatory authorities, if applicable). Protocol amendment submissions should include: • Summary page describing the changes made • Copy of the amended protocol clearly showing the revisions • Clean copy of the new protocol amendment • Copy of the IRB approval letter 3.1 Minor Changes Minor changes, which include editorial changes, correcting typographical errors and appropriate scientific or technical clarifications can be made to the protocol and related documents. These changes should be documented in a Table of Modifications, and submitted to the FDA at the time of the next protocol amendment submission. The FDA also permits modifications to the experimental design of Phase I protocols that do not affect critical safety assessments to be reported to the FDA only in annual reports. 4. Submission to other investigative sites (Sponsor-Investigators) Sponsor-Investigators conducting a multi-center study are responsible for submitting protocol amendments and updates to all participating centers. The investigator at each center, in turn, is responsible for submitting the amendments to their institution's IRB. 5. Protocol Deviations and Violations Protocol deviations and violations refer to both purposeful and accidental variances from the approved study protocol. There is no regulatory definition of a protocol violation that differentiates itself from a protocol deviation - both indicate a variance from the approved study protocol. For the purpose of this manual, a protocol violation is considered to have a greater potential effect on the study than a deviation, i.e. could affect a subject (rights, safety, or wellbeing) or the data integrity (safety and efficacy endpoints). Chapter 16: Protocol Modifications Page 2 of 7 Office of Human Research 5.1 Protocol Deviations Non-Serious Variances Non-serious variances to the protocol will not jeopardize the safety or integrity of the research project. Examples of protocol deviations include: failing to perform minor study related tasks, performing follow-up visits or testing just outside the window, and minimally exceeding the number of IRB-approved enrollment numbers. These types of deviations usually do not require IRB reporting. However, if a pattern of non-serious deviations becomes apparent, this should be reported to the IRB and an amendment to the protocol should be considered. Prospective Approval Some variances in the protocol that have the potential to change the risk/benefit ratio can be prospectively approved by the IRB, the sponsor (if applicable) and other appropriate reviewing entities. In these situations, when prospective approval is granted, the variance is considered a Protocol Deviation, even though the variation is more serious in nature. For example, an investigator may want to enroll a subject into a research study who does not meet the eligibility requirements. An exception can be granted on a one-time only basis, if the subject’s enrollment will not compromise his or her safety. This will require pre-approval by the IRB and the study sponsor, if applicable. The request should include information on the project, the criteria causing exclusion, and the justification for enrollment. If an investigator finds that eligibility exceptions are required more than once, he or she should consider submitting an amendment to the IRB that revises the eligibility criteria. 5.2 Protocol Violations Serious variances to the protocol have the potential to change the risk/benefit ratio, the validity of the study results, or a subject’s rights or well-being. When such a variance occurs and prospective approval was not obtained (see "Prospective Approval" above), this is then considered a Protocol Violation. Examples of protocol violations include: subjects enrolled who did not fulfill eligibility criteria, failing to obtain informed consent, confidential information disclosed, enrolling subjects during a lapse in IRB approval, conducting unapproved research tests or procedures, and administering investigational medications in a manner not specified in the study protocol. The IRB should be notified of any protocol violations promptly after the violation is discovered. The investigator should include a detailed plan of how to prevent serious protocol violations from occurring in the future. If necessary, the IRB has the authority to intervene by terminating approval for the project or suspending an investigator for extremely serious or repeated non-compliance issues. 5.3 Reporting Requirements Non-serious protocol deviation – Reporting to IRB not required Chapter 16: Protocol Modifications Page 3 of 7 Office of Human Research Prospective protocol deviation - Reporting to Sponsor and IRB required prior to event Protocol Violations - Promptly the deviations/violations may be required to be reported to the sponsor. Sponsor reporting should be defined in the protocol. 5.4 Food & Drug Administration (FDA): In studies being conducted under an Investigational New Drug (IND) application or an Investigational Device Exemption (IDE), a protocol violation can have the impact of a protocol amendment or a change in the investigational plan. Serious protocol variances must be reported to the FDA. This can be done in the form of a letter outlining the nature of the variance. 5.5 Documentation Any deviation or violation as defined above must be documented regardless of outcome. Documentation should be placed: • In the Case Report Form • In the appropriate source documents where applicable (i.e. medical chart) • In correspondence with Investigator or Sponsor, Pharmacy, IRB, or other regulatory entities 6. Premature Discontinuation of a Study Studies can be discontinued prematurely for a variety of reasons, such as subject safety (discovered through regular safety assessments or a pre-planned interim safety analysis), study finances, poor enrollment, a business decision (in the case of industrysponsored research), or even early proof of efficacy or lack of efficacy noted in a preplanned interim analysis. Regardless of the reason for discontinuing a study before its planned end, there are a number of issues to consider and manage. • Research subject safety - The first consideration when prematurely discontinuing a study should be for the welfare of the study subjects. For interventional studies, the research team must think about the effect the withdrawal of the study treatment will have on research subjects. It may be necessary to wean a study drug rather than discontinue abruptly, or to transition from study treatment to another appropriate therapy. Additionally, if the study was discontinued due to safety concerns about the study treatment, it may be necessary to evaluate subjects for residual effects and to work out the best follow-up plan to evaluate possible lasting effects from the study intervention. • Communication - The study sponsor initiates the communication about the study discontinuation. It is the investigator's responsibility to inform the IRB, other reviewing entities and research offices, and the team involved in the study. Careful thought and planning should go into the communication of the decision and any follow-up plans to the study subjects. • Study Finances - Study contracts and grants address the costs and method of payment for work done on research studies. In industry-sponsored research, it is important to have the study agreement clarify the sponsor's responsibility to Chapter 16: Protocol Modifications Page 4 of 7 Office of Human Research cover any unforeseen costs incurred due to a premature discontinuation of a study not related to investigator or site performance problems. • Data management - Any changes to the protocol-defined data management plans depend upon the reason for study discontinuation. When a study has been stopped earlier than planned for safety or efficacy reasons, finalization of the data and data analysis is essential for the full characterization of the safety or efficacy issue. The investigator and sponsor should work together to clarify the data management plan in light of the early study discontinuation. • Record retention - Regardless of the reasons for early study termination, the sponsor and investigator must still retain study records according to Good Clinical Practice (GCP) standards and the contract stipulations. 7. Continuing Review/Renewal 7.1 Institutional Review Board (IRB) Continuing Reviews Research must be reviewed by the IRB at least once every twelve months, but may be reviewed more frequently depending upon the level of risk. The MHS IRB will notify investigators by email 2-3 months prior to the expiration of IRB approval with a continuing review form. It is the responsibility of the Principal Investigator (PI) to submit regardless of having received notification. Continuing review forms should be completed and submitted to the IRB within 60 days of expiration to assure uninterrupted activity. If an investigator has failed to provide continuing review information to the IRB or the IRB has not reviewed and approved a research study by the continuing review date specified by the IRB, the research must stop, unless the IRB finds that it is in the best interests of individual subjects to continue participating in the research interventions or interactions. Enrollment of new subjects cannot occur after the expiration of IRB approval. Copies of IRB Continuing Review documents and correspondence should be retained in the regulatory binder even when the study is being terminated or enrollment is closed. 7.2 National Institutes of Health (NIH) Renewals The National Institutes of Health (NIH) requires an annual renewal update for NIHfunded studies. Progress reports must be submitted two months before the beginning date of the next budget period. The NIH uses a renewal form, PHS 2590, also known as the Streamlined Non-Competing Grant Progress Report (SNAP form), which requests the following information: Progress Report Summary • The title of the project, grant number, funding agency, and Principal Investigator name • Information concerning any changes to: o Support of key personnel since last reporting period Chapter 16: Protocol Modifications Page 5 of 7 Office of Human Research o Level of effort for key personnel from what was approved for the project o Estimates of un-obligated balance that will be greater than 25% of the current year's total budget • Outcomes to date • Projected plans for the future years of the project • Significance of findings and publications Personnel Report • List of the key personnel and a renewal of the percent effort Enrollment • List of enrolled subjects distributed by ethnic category, racial category and sex/gender Budget • Updated budget for the renewal year It is recommended that the investigator work directly with the grants department that handles the funding distribution of the grant in order to correctly revise the budget each renewal year. • Year-to-year Carryover Justification At year's end, if the study budget has an unobligated carryover (i.e. unspent funds) greater than 25%, a justification will need to be provided in the NIH renewal to the funding agency. More information about this can be found at http://grants2.nih.gov/grants/policy/nihgps_2003/NIHGPS_Part7.htm 7.3 No-Cost Extension The forms and instructions for completing PHS 2590 can be downloaded from http://grants1.nih.gov/grants/funding/2590/2590.htm. If it becomes necessary to extend the project beyond the original grant expiration date, a No-Cost Extension can be granted. NIH can approve a No-Cost Extension for up to 12 months provided that no additional funds are required, there will be no change in the project's original objectives, and adequate justification is provided. More information about submitting a No-Cost Extension can be found at http://era.nih.gov/index.cfm 8. Food and Drug Administrations (FDA) Annual Reports 8.1 Document Submission for Investigator-Initiated Research Sponsors are required to submit an annual report to the FDA of any studies being conducted under an Investigational New Drug (IND) application or Investigational Device Exemption (IDE). The elements of this report are described under the IND regulations. • Summary of each study in progress including, for each study: o The title, protocol number, purpose, subject population, statement of whether or not completed; Chapter 16: Protocol Modifications Page 6 of 7 Office of Human Research • o Information about the number of subjects anticipated, entered, completed, and dropped out; tabulate by age group, gender, and race; o Any available study results Summary from the year, including: o Summary of most frequent and most serious adverse experiences by body system o Summary of all IND Safety Reports o List of subjects who died during participation, with cause of death o List of subjects who dropped out in association with any adverse experience o Description of what was obtained pertinent to an understanding of the drug's actions o List of preclinical studies completed or in progress during the past year; summary of findings o Summary of any significant manufacturing or microbiological changes made • Plan for coming year, in the format of the IND submission • Description of any significant Phase I protocol modifications made • Summary of significant foreign marketing developments with the drug Chapter 16: Protocol Modifications Page 7 of 7 Office of Human Research Chapter 17: Financial Accounting Pre-Award Process Chapter 17: Financial Accounting Page 1 of 5 Office of Human Research PRE AWARD PROCESS a. PURPOSE: To define the pre-award procedures necessary to determine financial feasibility for each sponsored research project. b. POLICY: Sponsored Research projects are administered in accordance with the terms and conditions specified in the grant or contract and applicable regulatory requirements. During the Pre Award process OHR will perform: 1) Medicare Coverage Analysis 1.1 Research Manager reviews protocol schema and clinical trial agreements for study details 1.2 Performs analyses using the most current policies and guidelines of the Centers for Medicare & Medicaid Services; 1.3 Submits completed coverage analyses/reviews to a query able database where other relevant members of the clinical research team can access information about a study 1.4 If applicable, seek advice from the PI or outside staff to determine whether a procedure meets the standard of care in research. 2) Labor Worksheet 2.1 OHR Finance provides a custom labor worksheet specific for the protocol for the Nurse Manager to complete 2.2 Nurse Manager provides an estimate of the time required for each event in the protocol 2.3 Estimates include effort for Principal Investigator, Research Nurse, Pharmacy, and Regulatory staff 2.4 Research time is inclusive of o Lab and procedure: processing, scheduling, shipping, authorization o Data collection, interpretation and analysis 3) Budget Development 3.1 OHR’s budget matrix is inclusive of three sections: Non Billable, Billable, and Labor 3.2 Non-Billable Items : These are events in the protocol which the study team has identified as Standard of Care (SOC) or Routine Care that will be billed to the patient’s insurance Chapter 17: Financial Accounting Page 2 of 5 Office of Human Research 3.3 Billable Items: These events are procedures which can be identified by CPT codes. We use our pre-negotiated rates from our hospitals and/or physician group partners 3.4 Labor: Nursing Labor Worksheet used to determine applicable study hours. 4) Feasibility Analysis & Negotiations w/ Sponsor 4.1 Upon completion of our per patient budget, OHR Finance will negotiate the budget and terms & conditions with the sponsor 4.2 MHS institution’s overhead is 28% and OHR’s non-refundable start-up includes (but not limited to) the following activities: administrative review, regulatory set-up, pharmacy, storage and archive, study close out, and marketing/advertising 4.3 Once OHR & Sponsor agree to terms, document are routed for signatures POST AWARD PROCESS 5) Billing and Collection a. PURPOSE: To define the billing and collection procedures necessary to maintain an appropriate level of internal controls over Research revenue collection operations. b. POLICY: Sponsored Research projects are administered in accordance with the terms and conditions specified in the grant or contract and applicable regulatory requirements. OHR Finance is responsible for: • determining sponsor financial terms and conditions; • maintaining all Accounts Receivable records, including open bills awaiting payment; • ensuring that Sponsors are accurately and promptly billed; • ensuring that all invoices are properly paid, or otherwise adjusted; and • allocating payments appropriately to projects and cost centers. 5.1 Billing/Invoicing An invoice should be issued each time a project reaches payment milestones, direct costs or other costs as defined by the grant, trial or agreement with the Sponsor. When a project reaches a milestone, an invoice generated by OHR Finance staff enters the receivable into CREDIT, OHR’s Clinical Trials accounting system. The accounting system assigns sequential invoice numbers, which: • appear on each invoice; and • enable OHR staff to track payment Chapter 17: Financial Accounting Page 3 of 5 Office of Human Research The invoice directs the Sponsor to send all payments directly to OHR Payment Address, and provides the name and telephone number of the appropriate contact person(s) in OHR Finance. Statement or other notices or reports may accompany the invoice, but should not be substituted for the invoice. 5.2 Collection OHR Finance is responsible for collecting the amounts billed, recording the collections, and following up on outstanding invoices. When an invoice is not paid within a reasonable time, normally thirty to sixty days, OHR Finance will investigate the reason for the payment delay and take appropriate follow-up action. OHR Finance will record and apply payments received to the corresponding invoices, and investigate and reconcile any variance between an invoice and its payment. 5.3 Document Aging Each month OHR Finance will review the list of accounts receivable to verify balances are correct. Invoices 60-90 days past due are investigated i.e. sponsors are contacted for payment status and documented in the OHR monthly Financial report – Aging Report. 6) OHR Monthly Financial Reporting a. PURPOSE: To define the reconciliation procedures required to account for financial activity/transactions on each active Sponsored Research project. b. POLICY: A verification of all income and expenses against each active Sponsored Research project, as well as necessary corrections is required each month to ensure the OHR monthly financial reports are correct. 6.1 Clinical Trial Reconciliation Each month OHR Finance will perform a financial review of all income/expense transactions posted to each Sponsored Research project to ensure that account assignments and activity allocations are correct for OHR Monthly Financial Reports. Financial review consists of cash receipts reconciliation, payment allocation, invoicing and billing, direct payables, direct cost and other miscellaneous reimbursements. Any errors found are corrected and documented before the close of the accounting period following the period the charges were processed. Chapter 17: Financial Accounting Page 4 of 5 Office of Human Research 6.2 Monthly Reports By the 10th of each month OHR will prepare and distribute the following financial reports to its stakeholders: • Clinical Trial Summary (profit and loss summary by Trial) • Invoicing & Payment Summary • Payment & Invoicing Details • Payment Summary • Invoice Aging Chapter 17: Financial Accounting Page 5 of 5 Office of Human Research Chapter 18: Audits Any clinical research study being conducted at Memorial Healthcare System is subject to audits by a number of sources. Although there are many types of audits, generally speaking, an audit of a clinical research study seeks to validate the quality of the clinical study and assures that the rights and welfare of the human subjects in the study have been protected. An on-site audit may be conducted by federal government agencies, by internal MHS offices, or by the industry sponsor of the study. Depending on what agency/office is conducting the audit, there may be specific methods for preparing for and conducting the audit. 1. External Auditing Sources 1.1 Food & Drug Administration (FDA) • Applicable to any research study using an FDA-regulated product • May be Routine (determined by subject accrual rate or amount of data being obtained) or For Cause (potentially based upon a complaint of non-compliance) 1.2 National Institutes of Health (NIH) and any of its Centers or Institutes (e.g. NCI) • Applicable to any study being funded by an NIH Center or Institute or where the cooperative group holds the IND 1.3 Study Sponsor • Applicable to industry funded studies, investigator-sponsor initiated studies 1.4 Cooperative Groups, Data Collection Agencies • 2. Applicable to studies conducted through Cooperative groups such as eg. National Cancer Institute - NCCTG, COG, etc. Internal Auditing Sources 2.1 Office of Human Research (OHR) 3. • Applicable to any research conducted within MHS • May be Prospective (such as a Pre-FDA Audit) or in response to a complaint of potential non-compliance or routine Audit Procedures The investigator must notify the Office of Human as soon as possible if an audit has been scheduled: Chapter 18: Audits Page 1 of 5 Office of Human Research 3.1 FDA Audits The Office of Human Research (OHR) has extensive knowledge and experience in research regulations and will assist investigators and their study teams in the preparation and conduction of an FDA inspection. OHR will provide a Pre-Audit Review, facilitate the inspection, and provide assistance in responding to the FDA's inspection observation. For more information, please contact the OHR. 3.2 NCI Audits The OHR will coordinate and facilitate all NCI audits. 3.3 Site Responsibilities In anticipation of an audit, the Principal Investigator (PI) needs to ensure the following: • Time and flexibility in his/her schedule to meet with the inspector • A controlled environment in which the investigation will be conducted • The inspector has access to all necessary source documentation (medical and clinical records), study records (case report forms or electronic data capture systems), and regulatory documentation. • FDA AUDITS: 4. o Always ask for the inspector's identification. They are required to present their identification and you are required to ask for it prior to handing over any confidential documentation for review. o The inspector will present the investigator with an FDA Form 482 Notice of Inspection. The Principal Investigator will sign the 482 and receive a copy. Audit Areas 4.1 Protocol The inspector will review all versions of the protocol to document that all versions received proper IRB approval and that NO CHANGES to the protocol were implemented prior to IRB approval. 4.2 Authority and Administration The inspector will review the regulatory documentation, including monitoring log, delegation of responsibility log, CV's, IRB and sponsor communications and lab information to determine: • How the investigator is informed of his/her requirements regarding the study protocol and, if applicable, accountability of the test article • Proper delegation of various study related tasks Chapter 18: Audits Page 2 of 5 Office of Human Research • List of individuals performing study tasks and their positions • Name and address of the laboratory facility and its ability to perform studyspecific tasks 4.3 Subject Records The inspection of subject records is an effort to confirm: • The existence of all subjects • Validity of data (case report form data versus source documentation) • Proper documentation of AEs/SAEs • Accurate documentation of concomitant medications and medical history • Subject eligibility (inclusion criteria met, no subjects meeting exclusion criteria were enrolled) • The handling of subjects who come to meet exclusion criteria during the course of the study • Complete and accurate records kept on the subject throughout exposure to the investigational product and during the course of the study • Proper documentation of adverse events • The proper follow-up and management of all study dropouts For paper case report forms and/or source documentation, the inspector will need to assure that records are secure from tampering, and that they can be maintained for the required period of time after the conclusion of the study. 4.4 Consent of Human Subjects The inspector is required to verify that informed consent was obtained from all subjects prior to study entry and in accordance with the regulations. The inspector may review all consent forms on subjects enrolled and screened. Therefore it is considered best management practices to maintain all original consent forms in one study file for ease of verification and to avoid the need to pull all subject records (copies of the original signed consent form can be kept with the subject records). 4.5 IRB Communications The audit may typically include a review of the investigator's reports and communications with the IRB. This includes submission of reports, protocol deviations/violations, protocol amendments, informed consent amendments, advertisements, and adverse events. Chapter 18: Audits Page 3 of 5 Office of Human Research 4.6 Sponsor Communications The investigator's communication with the study sponsor will also be inspected to ensure that both sponsor and investigator have met all regulatory obligations. The inspection will include review of: • The IRB-approved consent form • Periodic reports from the investigator • Adverse events (within the required timeframes) • On-study illness and concomitant medication information • Timely Case Report Form (CRF) submissions In addition, the inspector may be verifying that the sponsor conducted adequate monitoring of the study's progress. 4.7 Investigational Product Accountability Maintenance of investigational product inventory and records is critical in verifying accountability. Proper documentation of investigational product accountability includes: • Receipt dates and quantity • Dates and quantity dispensed with subject ID • Distribution of investigational product only to subjects enrolled in the study • Quantity, frequency, duration, and route of administration • Investigational product disposition (what was received from, used, and sent back to the sponsor) • Comparison of receipt and usage against shipping records Investigational product accountability also includes proper storage of the investigational product with adequate security in a controlled environment. Inspectors will also want to confirm the investigational product was dispensed and administered by qualified and authorized personnel. 4.8 Electronic Records/Record Retention 21 CFR Part 11 provides specific regulations governing the management of electronic records and electronic signatures. 21 CFR 11 regulations apply to any records required to be maintained according to Food and Drug Administration (FDA) Good Clinical Practice (GCP), Good Manufacturing Practice (GMP) and Good Laboratory Practice (GLP) regulations if such records are maintained primarily in electronic form. Since these regulations were created to support GCP, GMP and GLP, they apply to all studies using FDA-regulated products, regardless of whether data will be submitted to the FDA. If there is any doubt whether a given electronic system is subject to 21 CFR 11 regulations, please contact the OHR for assistance. Chapter 18: Audits Page 4 of 5 Office of Human Research 5. Common Audit Findings A report published by the FDA's Office of Inspector General in June of 2000, reviewed 184 official actions taken by the FDA since 1994. These actions were then categorized into different types of violations. (The full report can be viewed at http://oig.hhs.gov/oei/reports/oei-05-99-00350.pdf). In summary, the report found of those violations reviewed: • 85% were based on documentation problems, including missing data, data discrepancies, falsification of data, and poor data collection. • 82% were protocol violations, including enrollment violations, failure to follow the protocol, problems with investigator agreements, and violations related to drug use • 74% were reporting violations, including failure to submit to the IRB or sponsor reports, consent forms, protocols, advertisements, and adverse events. • 67% were human subject protections violations, most often surrounding the use of a deficient informed consent form, not obtaining signed informed consent prior to performing a study procedure, or missing signatures or dates on the informed consent form. • 44% were drug/device/biologic control violations, citing poor control of the receipt, use and disposition of investigational drugs, devices, or biologics. Chapter 18: Audits Page 5 of 5 Office of Human Research Chapter 19: Subject Management This section focuses on the management and conduct of research activities that are specific to the research subject. 1. Screening The screening process identifies individuals who fulfill the inclusion and exclusion criteria in the protocol and are therefore eligible to participate. Screening methods will vary depending upon the type of study, the population, and the setting. Screening should not be confused with recruiting. Recruitment refers to the systematic gathering of a population that meets prescribed characteristics. Recruitment almost always takes longer than originally anticipated and new recruitment strategies may be needed to identify appropriate candidates for screening. 1.2 Gathering Screening Information Appropriate screening questions specifically address eligibility and adherence to the protocol (such as an individual's ability to complete research procedures). It is not appropriate during the screening process to collect information that does not directly address inclusion/exclusion criteria or suitability for the study. It is also inappropriate to use the collected data for purposes other than screening for the particular study. Screening may require: 1. Obtaining data from existing records (e.g. medical records, databases) 2. Obtaining data directly from potential subjects: o through interviews (e.g. discussions, questionnaires) o through assessments, tests, or procedures (e.g. physical exams, lab results) It may be helpful for investigators to develop a checklist for study staff to use during the screening process. A checklist contains a list of the inclusion and exclusion criteria and may also contain a signature line for the person completing the screening. Reviewing records A researcher may need to access charts and existing records to determine eligibility and/or to contact someone about a study. If it has been approved by the Institutional Review Board (IRB), the researcher does not need to obtain a written consent or HIPAA authorization to review records. HIPAA regulations (preparatory to research) allow researchers under the covered entity to review existing records provided that the information is not removed from the covered entity. However, researchers should not “cold-call” prospective subjects identified during a record review without first obtaining permission from them. This permission can be obtained through their health care provider or through a letter of introduction. Chapter 19: Subject Management Page 1 of 15 Office of Human Research Interviewing During a screening interview, the researcher will ask the prospective subject questions to help determine eligibility, suitability, and interest in the study. The screening interview may precede or be a part of the consenting process. Before the screening interview begins, potential subjects should be informed who they are speaking to, why they are being approached, who referred them, and the purpose and nature of the inquiry. To screen MHS patients, the following contact methods in descending order of preference are: 1. By the Health Care Professional who has taken care of the patient. 2. By another health care professional from within the covered entity using a cover letter agreed upon by the health care provider who has taken care of the patient and containing script approved by the IRB. 3. By the researcher. When both of the other two alternatives are impractical, direct recruitment by a researcher who has not taken care of the patient will require specific IRB approval. Phone Screening If a prospective subject is being approached for the first time by telephone, they should be informed who they are speaking to, how long the discussion will take, the purpose and nature of the questions, the purpose and voluntary nature of the research, and how confidentiality will be protected. If the person is interested, the interviewer should obtain verbal permission to proceed with the questions. Often, the IRB will request a script of a planned telephone dialogue. Minimally, the researcher should provide the IRB with the following information regarding procedures for telephone scripts: 1. How is the personal information conveyed to the appropriate person for further eligibility determination? 2. What happens to the personal information if the caller ends the interview or simply hangs up? 3. Are the data gathered by a marketing company? If so, are names, etc. released to others? 4. Are names of non-eligible subjects maintained in case they would qualify for another study? If so, how are they maintained? What is the procedure for ensuring confidentiality and security of this information? 5. Are paper copies of telephone screening records shredded or are readable copies put out as trash? Questionnaires As with any written instrument that is administered to a subject during a study, screening questionnaires must be submitted to the IRB for review prior to their use. Chapter 19: Subject Management Page 2 of 15 Office of Human Research 2. Performing Assessments, Tests and Procedures The investigator must obtain informed consent prior to conducting any clinical assessments, tests, or procedures solely for the purpose of determining eligibility for research. This may include complete medical histories, physical exams, blood work, and withdrawal from medication (wash-out). This does not include procedures that are performed as part of the standard practice of medicine for clinical purposes. Only a physician can make a medical diagnosis that determines eligibility. PhysicianInvestigators should take extra care with their patients to differentiate between examinations and procedures for research purposes and those for medical (nonresearch) purposes. 3. Screening Documentation As part of the research records, investigators should have documentation to verify that a subject has met the eligibility criteria for a study. This may include existing medical records, a physician referral letter, a written account of screening interviews, questionnaires, and/or results from research tests. To protect confidentiality, investigators should minimize the amount of identifying information that is collected during the screening process. For example, the investigator may record non-identifiers during the pre-screening process (e.g. first name, initials), contact information during the screening process (e.g. full name, telephone number), and additional identifiers after enrollment (e.g. birth date, medical record number). Identifiable information may be retained until it is clear that an individual will not be enrolled. After that point, the investigator must either obtain a HIPAA authorization or destroy the identifiers. 3.1 Screening Logs A screening log includes information on all the individuals that were screened for a research study, regardless of whether they were enrolled. Screening logs can provide useful information about the population and may help identify barriers to enrolling eligible candidates. 3.2 Screen Failures Screen failures are individuals who are evaluated for participation in a study, but not enrolled. Screen failures either do not meet the eligibility criteria or decline participation. An investigator may only retain identifiable health information about a screen failure if a HIPAA authorization has been obtained. If a HIPAA authorization is not obtained, the segments of the screening records that contain identifiers should be blacked out or removed as soon as it becomes obvious that the individual is not eligible for participation. Chapter 19: Subject Management Page 3 of 15 Office of Human Research 4. Consenting Informed consent is a process by which a subject acts autonomously to make an informed and voluntary decision to participate in a research project. Informed consent involves an ongoing exchange between the researcher and/or research staff and the subject. This process starts before any documents are signed and continues through the completion of the entire study. Subjects tend to recall more about the practical aspects of a study than the theoretical aspects and tend to forget risks more quickly than benefits. Because of this, researchers will need to re-discuss information throughout study participation to promote ongoing understanding. 4.1 Underlying Principles of Consent A valid informed consent requires: • Voluntary Choice • Disclosure • Understanding 4.1.1 Voluntary Choice A voluntary choice involves the exercise of free will and is free of undue duress. Undue duress can be introduced to the consent process by means of coercion, manipulation or force. Subjects may be coerced by the promise of excessive inducements (e.g. large payments or access to expensive treatments) or the threat of retribution (e.g. fear of receiving poor medical care or a failing grade). Subjects may be manipulated if they are improperly informed about the research, their role, or their rights. Subjects may feel forced if they are not given an opportunity to decline. Researchers must be aware of the subtle factors that influence the decision-making process. Relationships that have a high level of trust and dependency, such as the doctor/patient or professor/student relationship, can introduce feelings of indebtedness and obligation. When researchers are involved in a dual relationship with the subject, for example as the treating physician and the study investigator, the scope of the relationship in each situation must be clearly defined and delineated. Likewise, certain populations, such as those that are restricted, dependent, or compulsorily detained, may feel unduly pressured by figures of authority. This may include not only prisoners, but also members of the armed services and residents of chronic care institutions. During the consent process, researchers should remain cognizant of these factors and keep the consent process as neutral as possible. This can be done by involving research team members in the consent process who do not evoke feelings of authority or dependency. This can also be done by clearly communicating to subjects that they can refuse participation without fear of negative repercussions. 4.1.2 Disclosure The elements of disclosure can be scrutinized by reviewing the content of the informed consent form; however, long, detailed consents may be confusing and overwhelming for Chapter 19: Subject Management Page 4 of 15 Office of Human Research subjects. Disclosure, in and of itself, does not constitute informed consent. Obtaining a signature on a consent form without having discussed its contents violates the principles of informed consent. Researchers must carefully balance full disclosure with comprehension and understanding. Legal criteria state that researchers should disclose any risks to which a reasonable person would attach significance in that particular situation. Researchers must develop the skills necessary to identify how much information each subject needs to make an informed decision. 4.1.3 Understanding A well-written consent form and a carefully planned dialogue alone cannot guarantee understanding on the part of the subject. Information must be presented in a manner that is both meaningful and culturally sensitive to promote comprehension. It is often difficult to identify whether a subject has adequate understanding. Researchers should try to assess a subject's level of understanding by asking them to describe the research in their own words. Through this interchange, the investigator can identify any lost information and rearticulate the information until it is understood. Therapeutic misconception occurs when a person believes that a research study will provide personalized medical care that imparts direct benefits. The purpose of research, its risks and benefits may often be disclosed, but presented in a manner so that it is misunderstood as treatment. Presentation factors that influence understanding include descriptors (innovative, cutting-edge), quantitative vs. qualitative presentations (uncommon versus 5%), and framing ("lives saved" versus "lives lost"). Investigators conducting therapeutic research should explain the difference between research and standard medical care. Therapeutic research should always be presented as choice between participating and receiving standard care. Research should also be framed in neutral terms that do not over-emphasize potential benefits nor under-emphasize potential risks. An effective method of communicating magnitude and probability of risk is to use visual aids. 4.2 Obtaining Informed Consent It is the responsibility of the Principal Investigator (PI) to ensure that informed consent has been properly obtained. This activity may be delegated to a research coordinator or other research staff who are knowledgeable about the study, the research subject, the subject's alternative choices, as well as informed consent regulations. The PI remains accountable for the actions of any research staff to whom the responsibility of obtaining informed consent has been delegated. During the consent process, the investigator should: 1. Approach the prospective subject to introduce the research team and the project. o The discussions should take place in an area where privacy and confidentiality can be respected. o Subjects must be given sufficient time to comprehend the research. Chapter 19: Subject Management Page 5 of 15 Office of Human Research 2. Review the research study and the informed consent form with the subject. o The researcher should clearly explain the background/purpose, voluntary nature, commitment, risks, benefits, alternatives, and other elements making sure to include all the necessary elements of informed consent. 3. Answer any preliminary questions. 4. Allow the subject time to review the informed consent form independently. o In non-emergency situations, subjects should be given at least 30 minutes for reflection and 24 hours whenever possible. o Provide the subject with a sample consent form to review prior to the consenting process and study appointment. o If possible, subjects should be given time to discuss participation with family or friends. 5. Evaluate the subject's understanding by asking open-ended questions about the study and address any misperceptions or unanswered questions. Possible questions include: Can you describe the study in your own words? What more would you like to know? Would you please explain to me what we are asking you to do? What are your concerns? 6. If willing, ask the subject to sign and date the consent document. o Subjects must personally sign and date the most recent IRB-approved version of the informed consent form o The consent form must contain an approval stamp from the IRB. o The person obtaining consent and, if necessary, the witness should also sign and date the informed consent form. 7. Give the subject a copy of the signed and dated informed consent form. 8. Document the informed consent process (see below). A signed informed consent form must be obtained prior to initiating any research procedures. This includes procedures conducted solely for the purpose of determining eligibility for research and drug washout periods. If the subject consents to participation, the original consent form is kept with the research records, a copy is given to the subject, and a copy may be placed in his or her medical records (if applicable). 4.3 Documenting the Informed Consent Process A note in the chart and/or research records should include: • Name of study and subject Chapter 19: Subject Management Page 6 of 15 Office of Human Research • Date and time of consent • Statement that the benefits, risks, commitment and alternatives were discussed • Presence of any family members, friends, or witnesses • Specific, relevant criteria not otherwise captured (e.g. time frames of screening tests that are not apparent in records) Outside auditors may prefer a narrative, handwritten note over a checklist or printed template language, however there is no regulatory requirement to that effect. A sample informed consent note may look like the following: “On 11/21/11, I reviewed the research protocol [study title] with [patient's name]. She was given an opportunity to read the consent form and was given ample time to ask questions and have them answered. The study's purpose, procedures involved, voluntary nature, risks and benefits were discussed with her. She indicated her decision to participate and signed the consent form. I provided her with a copy of the signed informed consent and HIPAA authorization form. The informed consent form was signed prior to any study related procedures outside of standard of care were performed.” 5. Consenting Special Populations In certain circumstances the informed consent process must be tailored to meet the needs of special populations including minors, adults with a limited decision-making capacity, and individuals who are blind, illiterate, or do not speak English. 5.1 Assent Generally, children and adults with limited decision-making capacity do not have the legal authority to provide consent for their own participation in a research study. However, an investigator should still seek affirmative agreement (assent) from such research subjects. An assent form is a simplified version of the consent form and should be written to the subject's level of understanding. A typical assent form explains a study's purpose, procedures, risks, benefits, confidentiality, and voluntary nature in simple terms. 5.1.1 Children/Minors Definitions Federal regulations define "children" as persons who have not attained the legal age for consent to treatments or procedures involved in the research, under the applicable law of the jurisdiction in which the research will be conducted. Under Florida law, persons under the age of 18 will generally meet the definition of "children" with the exceptions noted below. • In Florida, minors who are independent and living on their own may be declared emancipated minors by the court and may consent for themselves Chapter 19: Subject Management Page 7 of 15 Office of Human Research • Florida law permits a person under the age of 18 may consent to medical care or treatment if the person: o has graduated from high school; o is married; or, o is or has been pregnant Individuals who are defined as "children" will be afforded the protections under the regulations that protect children involved as subjects in research (Subpart D, 45 CFR 46.401 - 409 and 21 CFR 50.50 - 54). Additionally, the IRB may determine that minors who are not children (such as a person meeting one of the exceptions noted above) are potentially vulnerable, at which point the IRB might apply additional protections. 5.1.2 Parental Permission A parent or guardian must grant permission for the child to participate in research. If the research involves greater than minimal risk and offers no prospect of direct benefit, permission must be obtained from both parents (granted they have custody and are reasonably available). Parental permission is typically documented through having the parent(s) sign and date a Parental Permission Form. The Parental Permission Form looks like and contains all the same elements as an adult consent form, except that "You" is replaced with "Your child" throughout the document. 5.1.3 Child’s Assent Generally, children 7 to 18 years of age may be capable of providing assent. However, individual subjects may not have the cognitive and emotional maturity to understand the research project and decide whether or not to participate. So, even when the IRB requires that assent, an investigator must use discretion in determining whether the subject is capable of providing assent. Investigators need to document the rationale when assent is not obtained. It is important to note that assent must be affirmative, meaning that if a child says nothing or simply doesn't disagree, then assent has NOT been obtained. Additionally, parental permission does not override a child's assent, unless the child's health is at stake. The assent process must be tailored to the individual child's age, maturity and psychological state. 5.2 Documenting Assent In most situations, the IRB will allow the child to sign the parental permission/ consent form to indicate his or her willingness to participate. Parental consent/ permission forms should also include a separate section where investigators are required to document the reason(s) why it is not feasible or appropriate to obtain assent from a particular subject. In some situations, determined by the on a case-by-case basis, the IRB may require a separate assent form. This may apply in non-therapeutic studies that involve older Chapter 19: Subject Management Page 8 of 15 Office of Human Research children and adolescents. These assent forms must be simple and easy to understand. Investigators may Assent of the minor is not required when the IRB determines: 1. that the capability of a minor is so limited that he or she cannot reasonably be consulted, or 2. that the intervention or procedure involved in the research holds out a prospect of direct benefit that is important to the health or well-being of the child/adolescent and is available only in the context of the research 6. Pregnancy Testing in Minors Under FL state law, minors have the right to confidential pregnancy testing. If pregnancy testing is required as part of the study, it is required that both the assent form and the parental permission form include language that makes clear that the results will may be shared with parents. 6.1 Pregnant Minors Pregnant minors and minors with children are entitled to make decisions about their own health care and may make decisions on behalf of their fetus/child (except for decisions about abortion), this includes the ability to provide informed consent for their participation, or the participation of their children, in clinical research. However, the intent to enroll subjects from this special category of minor, or to permit this category of minor to consent to the enrollment of their children into research, must be stated in the protocol and have received IRB review and approval before it can be implemented. This is in order to conform to regulatory requirements for the protection of vulnerable populations (i.e. 45CFR46 subpart B, concerning pregnant women and fetuses), and to engage the IRB concerning any additional protections for this specialized group of minors. Minors that reach the age of majority (18 years) during the conduct of a research study will need to be re-consented as an adult in order to continue participation. Minors who become pregnant during their participation in a study should be re-consented in order to continue participation, presuming such subjects are permitted to continue participation according to the protocol and IRB approval. 7. Limited Decision-Making Capacity Decisionally impaired adults are individuals who have a diminished capacity for judgment and reasoning due to a psychiatric, organic, developmental, or other disorder that affects cognitive or emotional functions. Other individuals may be considered decisionally impaired or have limited decision-making ability because they are under the influence of or dependent on drugs or alcohol, suffering from degenerative diseases affecting the brain, are terminally ill, or have severely disabling physical handicaps. If an individual does not have the capacity to make an informed decision about participation in a research study and is not likely to acquire or regain that capacity, proxy Chapter 19: Subject Management Page 9 of 15 Office of Human Research consent may be obtained. Ideally, the proxy is a legally authorized representative who has firsthand knowledge of that individual's needs and wishes. Researchers should ask surrogates who are making decisions if they think that the subject would have decided in the same manner if they were competent. Even if a subject has been judged incompetent, the person should be considered competent to refuse participation and should be included in the informed consent process as much as possible. 8. Legally Authorized Representatives The following individuals may be considered legally authorized representatives of the subject and capable of providing surrogate consent: 1. A court-appointed guardian authorized to consent to the subject's participation in the protocol in a current court order issued within the subject's jurisdiction. 2. A health care proxy appointed by the subject in a power of attorney. 3. If neither of the above are designated, the investigator may obtain informed consent from one of the following individuals in the order listed: 1. Spouse 2. Natural or adoptive parent 3. Adult child 4. Adult brother or sister 5. Any other available adult relative related through blood or marriage known and documented to have made decisions for the subject in prior health care settings 6. An adult individual with significant personal relationship with the subject to warrant their authority outside the currently accepted legal spousal relationship. If it is appropriate to have a surrogate sign the informed consent form, indicate the surrogate's relationship to the research subject and, if available, attach a copy of the legal document which gives that individual the right to sign for the research participant. If a legal document is not available, the PI must document a statement that the individual is acting as the legally effective representative under the above conditions. 9. Non-English Speaking Subjects who do not speak English must be consented in a language understandable to them. This may require the use of a certified interpreter. The MHS intranet provides a list of certified interpreters by facility and language; the individuals listed are employed by the health care system, and must agree to provide the required services to interpret informed consents etc. A witness is required to confirm that the subject was reasonably informed about the clinical research study and consented freely to take part. If the interpreter is independent from the research team, the interpreter may serve as witness. Chapter 19: Subject Management Page 10 of 15 Office of Human Research Subjects who do not speak English should also be provided with a consent document written in a language understandable to them (or their authorized representative). 10. Re-Consenting A formal re-consenting process is required if new information becomes available that may impact a subject's willingness to continue participation in the study (e.g. newlyidentified risks or changes in the research procedures). Re-consenting requires a revised consent form. Revisions to the consent can take the form of a fully revised consent form or an additional addendum. The IRB must approve any revisions or addenda to the informed consent form prior to implementing them. Subjects who have been informed about substantive new information must sign and receive a copy of the revised IRB-approved consent form or addenda. 10.1 The following procedures should be used for re-consenting subjects with a revised consent form: 1. If the study is actively enrolling, previously enrolled subjects must be told about the new information at their next scheduled meeting. The subjects should sign the revised consent form as documentation of their willingness to continue in the research. 2. If the study is closed to accrual, but subjects are being followed, the subjects must sign either the revised consent form or an addendum to the original consent that presents the new findings. 3. If the study is closed to accrual, and subjects are being followed only through phone contact, the investigators may send the subjects a consent form addendum using certified or registered mail. Documentation of their receipt of this addendum may be noted in the research records at the time of their next phone contact. 4. If the study is closed to follow-up and the significant new findings may affect the long term health of the subject, the investigator shall attempt to send a letter to all prior subjects' last known address using certified mail. This letter should contain a name and phone number for the subject to contact should they require additional information. 10.2 Non-substantive changes to the study Subjects may be informed of non-substantive changes to the study (changes that would not impact their willingness to continue participation) verbally or through the use of a letter. Examples include a change in study team members or contact information. The date of the conversation or the date of the distribution of the letter informing the subject of the non-substantive study change should be documented in the subject's research file. Chapter 19: Subject Management Page 11 of 15 Office of Human Research 11. Enrollment 11.1 Enrollment Implementation The protocol should clearly delineate at what point a person is considered 'enrolled' to differentiate enrolled subjects from screen failures. The IRB has acknowledged that an enrolled subject is one who has • Signed informed consent and HIPAA authorization • Completed all research related screening tests • Has met all inclusion criteria - and • Has been appointed a study number If inclusion criteria have not been met, this can be considered a screen failure. If a subject has been enrolled and randomized to a treatment arm, if applicable, but never received study drug, this can be considered an early withdrawal. 11.2 Randomization Randomization is a process that assigns research subjects by chance to a study arm. Randomization prevents undue bias from affecting study results. The randomization process should be outlined in the study protocol. For blinded studies, an un-blinded person or group should hold responsibility for un-blinding and maintaining a master randomization list of all participants. Examples of randomization assignment methods include: • Interactive Voice Randomization System (IVRS) • Web-based randomization system • Randomization envelopes • Randomization schedules 11.3 Prioritizing At times, a research candidate may be eligible for more than one study. In such instances, the investigator and coordinator must examine the "best fit" for the subject (his or her interest in the study or willingness to complete the follow-up procedures), the priority of the research study, and the enrollment history. 11.4 Enrollment Documentation For many studies it is helpful to develop enrollment packets. An enrollment packet contains research tools and documents to complete screening, enrollment, and protocol procedures. Enrollment packets can be stored individually in folders or large envelopes in an easy access location where subjects will be screened. Chapter 19: Subject Management Page 12 of 15 Office of Human Research Possible documents/tools to include in an enrollment packet: Study-specific • Eligibility checklist (inclusion/exclusion criteria) • Source documents • Timeline/checklist of study procedures • Randomization tools Subject-specific • Screening forms • Forms requiring signatures o Informed Consent Form, HIPAA authorization, Medical Release, W9 tax form • Educational Materials/Instructions • Registration forms • Prescriptions • Wallet 'alert' cards • Vouchers Procedure-specific • Laboratory requisitions • Specimen labels • Questionnaires • Evaluation forms Once a subject is actively enrolled in the study, completed documents from the enrollment packet are transferred into the subject's study file (e.g. eligibility checklist, source documents, screening forms, consents, questionnaires, etc.). 11.5 Enrollment Tracking The investigator should establish enrollment goals to ensure successful and timely completion of the project. Enrollment goals specify how many subjects should be enrolled at each site over a certain period of time. By comparing expected to actual enrollment, problems can be identified and eliminated early. If enrollment is poor, the investigator should identify the problem: • Was the prevalence of the population overestimated? • Are advertisements reaching the appropriate audience? • Has there been any negative publicity associated with the research, investigator, or institution? • Are subjects being referred appropriately or in sufficient numbers? Chapter 19: Subject Management Page 13 of 15 Office of Human Research • Are enough resources devoted to screening? Are the resources distributed appropriately? • Are the eligibility requirements overly-rigorous? • Is there sufficient reimbursement for subjects? • Are the protocol requirements too demanding on subjects? • Are competing studies interfering with enrollment? Once the problems have been identified, the investigator can try to remove the barriers to enrollment. This may involve changing the design of the study, revising recruitment strategies, increasing payment, redistributing resources, or amending the protocol. 12. Study Procedures 12.1 Subject File It is recommended that the researcher develop a file specific to each subject. This enables the Clinical Research Nurse (CRN)/Clinical Research Coordinator (CRC), Principal Investigator (PI), Clinical Research Associate (CRA)/monitor, or other reviewer to quickly ascertain information about a particular subject's participation in the study. The Subject File should be filed according to an identifier rather than by name and access should be restricted and secured to protect confidentiality. Standard Operating Procedures (SOPs) should be created to dictate office standards and to assure uniformity. A Subject's File may include any and all records necessary to delineate the progression of the subject throughout the research project. The contents of the subject files will vary from study to study as well as from research office to research office. The Subject File should contain the following: • A copy of the Informed Consent form (the original should be filed in a separate Informed Consent Forms file) • Completed Case Report Form(s) • Source documents (see below) • Copies of pertinent medical records that may not be easily retrievable on site (e.g. lab work done by the subject's primary care physician between study visits) • Correspondence with or about the subject (e.g. a phone log) • Explanations (i.e. Notes to File) by the study staff explaining variances from protocol, discrepancies, missing data, etc. • Queries from the data coordinating center and the responses • Dosing or randomization documents Chapter 19: Subject Management Page 14 of 15 Office of Human Research 12.2 Source Documents Source documents prove the existence of a subject and substantiate the integrity of research data. They are the first documentation of any study observations or data. Source documents are the original hospital records/charts, laboratory data, x-rays, pharmacy records, study records, etc. Source documents may even include scraps of paper where information is first recorded. Together they comprise a subject's research records and delineate the details of his or her progress throughout the research project. To create a customized source document template: • Compare the protocol, the case report form (CRF), and current practice in existing records. • List data not routinely charted in the existing records. Focus upon capturing a comprehensive summation of information relevant to the subject's research status including, but not limited to, the information necessary to complete the CRF. • Create source documents that are as close to standard charting procedures as possible. • Create a line for the person gathering information to sign and date the source document. Chapter 19: Subject Management Page 15 of 15 Office of Human Research Chapter 20: Withdrawing a Subject 1. Withdrawing a Subject A subject may be withdrawn from a study for several reasons, including failure to follow the protocol after being enrolled or having an adverse reaction to the investigational article. It is also a subject's right to voluntarily withdraw at any time during study participation. 2. Follow-Up In the event that a subject is withdrawn, a final visit should be scheduled. Many study protocols require that follow-up be continued for a specified period of time after a subject is withdrawn, regardless of the reason, to maintain safety. Every effort should be made to monitor the subject's health; however, ultimately, a mentally competent individual has the right to refuse all follow-up even if it compromises his or her safety. If this is the case, it is important to document the subject's refusal of follow-up. 3. Notifications When a subject is withdrawn from a study for any reason, the study sponsor (if applicable) should be notified as soon as possible. The withdrawal must also be reported to the IRB at the time of continuing review. If the withdrawal is the result of an adverse event, this should be documented and reported following the AE reporting guidelines. 4. Data Management In the case of subject withdrawal, it is imperative to collect at least survival data on the subject throughout the follow-up period. This data is important to the integrity of the final study analysis since early withdrawal could be related to the safety profile of the study intervention. The protocol should clearly define what types of data should be collected and the follow-up period for withdrawn subjects. 5. Subject withdrawal of authorization to use protected health information In addition to withdrawing participation in a study, the subject also has the right to withdraw the authorization to use his or her protected health information. This authorization was provided when they signed the HIPAA Authorization Form as part of the Informed Consent Form and process. If a subject decides to withdraw from a study, the researcher should remind the subject of this right to withdraw HIPAA Authorization. The subject must withdraw their HIPAA authorization in writing as explained in the Informed Consent Form. If a subject verbally indicates that he/she would like to withdraw HIPAA authorization the investigator should re-inform the subject of the written withdrawal procedure. Chapter 20: Withdrawing a Subject Page 1 of 3 Office of Human Research If the subject withdraws HIPAA authorization, the investigator should • Inform the subject that no further information will be accessed for the research purposes as outlined in the HIPAA authorization; • Remind the subject that even though he/she has withdrawn authorization, the information already obtained may remain a part of the research as necessary to preserve the integrity of the research study; and • Withdraw the subject from the research study. 6. Lost to Follow-up (LTF) A subject is considered lost to follow-up (LTF) when they fail to return for a scheduled visit, cannot be contacted, and do not complete any final evaluations. Occasionally, subjects may become difficult to contact or may miss scheduled visits. The following sequence should be followed for contacting "lost" subjects: 1. Subjects should be contacted 2-3 times via telephone at varying times and dates. Document dates of contact and outcome in the subject's study file (e.g. left voicemail message, phone disconnected, etc.). 2. A telephone call should be placed to his or her contact person to determine the subject status. A contact person (that does not live with the subject) should be obtained at the onset of study participation. 3. A certified letter should be sent to the subject's mailing address. 4. The local Vital Records department may be contacted to determine if the subject has expired. Several methods should be used to try to contact subjects. After several unsuccessful attempts, the subject is considered lost to follow-up and must be withdrawn from the study. If this is the case, the coordinator should document the dates of attempted contact and the contact methods used in the Subject file. 7. Managing Adverse Events 7.1 Assessing Adverse Events The investigator and study coordinator should assess each participant for adverse events (AE) throughout study participation and during the follow-up period. This includes conducting a thorough investigation of any suspected AE that may come from a variety of sources: • Spontaneous reports by subjects • Observations by key study personnel • Reports to study staff by the subject's family or medical care providers • Possible AE documented in medical records, progress notes, etc. • Death of a subject Chapter 20: Withdrawing a Subject Page 2 of 3 Office of Human Research In addition to receiving reports of potential AE, the investigator and study coordinator should develop and implement a plan to consistently and routinely monitor for AE through proactive measures such as: • Interview subjects at every visit • Review lab reports • Review subject's medical records for additional information • Review subject's diaries (if applicable) • Communicate with subject's medical providers 7.2 Clinical Management of Adverse Events All appropriate resources should be directed toward subject safety and well-being by instituting therapeutic intervention/support measures for subjects experiencing an AE. This may include a discontinuation, reduced dosage or interruption of the therapeutic agent, the procedures for which would be defined in the protocol. The subject experiencing the AE should be followed and assessed until the AE is stabilized and resolved. The study team must fully document the occurrence and management of the AE in the appropriate source document. 7.3 Breaking the Study Blind If necessary for the immediate medical care of an AE in one of the subjects, the investigational product blind may be broken. The protocol should clearly describe the procedures for un-blinding study therapy on a subject. When the blind is broken, the data collected for that study subject must be excluded from the study. While the safety of the subject always comes first, it is still important to seriously consider if un-blinding the study therapy is necessary to ensure a subject's safety. It is a common misconception that the blind needs to be broken for every Serious AE, but this is only true if the breaking of the blind is necessary for the medical care of the subject or if the protocol requires it. In cases where the blind is broken and is not necessary for the care of the subject, valuable study data will be lost unnecessarily. If available, the investigator should consult with the study pharmacist to assist in breaking the blind. All incidences of un-blinding should be documented in the CRF and in the participant's file. If the unblinding is associated with the management of an AE, the event should be reported to the IRB. Chapter 20: Withdrawing a Subject Page 3 of 3 Office of Human Research Chapter 21: Study Closeout 1. Study Closeout Once the study has been closed to enrollment and all follow-up data have been collected, the study is considered to be in the Closeout Phase. It is during this phase that data are prepared for final analysis, regulatory and reviewing bodies are notified, the investigational product inventory is reconciled, and final reports are completed. 1.1 Study sites may be closed when: Externally or internally funded protocols When follow-up data are no longer being collected on subjects enrolled in a protocol AND database finalization has taken place. Industry-sponsored studies As above, AND after the site has been notified by the Industry sponsor that the site may be closed. The ultimate goal of a clinical research study is to further the knowledge and understanding of human behavior, physiology or pathophysiology, often in the context of testing a treatment intervention. Important to this goal is making such knowledge available to the research community and the public. Study findings can be communicated in a number of ways including publishing results, generally in peerreviewed journals, or presenting research results at regional, national or international conferences. The research may also result in important new discoveries which may lead to the need for intellectual property rights protection in the form of patents and copyrights. This section of the manual outlines the required steps necessary to close out a study and highlights issues and resources for communicating study findings and protecting intellectual property. 2. Final Reconciliations For industry-sponsored studies, the sponsor will determine the disposition of the remaining inventory of the study drug or devices. The sponsor may request that the unused product be returned or destroyed. In either case, it is important for the research staff to document the following information: • Identifying information (lot, batch, or serial numbers) • Quantity of drug or device used and unused • Shipping information (for returned drugs or devices) • Means of drug or device destruction and person responsible for destruction • Date of drug or device destruction (see below) The Investigational Product Accountability Log should also reflect the disposition of unused product(s). The Investigational Drug Services Pharmacist can assist with the necessary reconciliation of investigational drugs. Chapter 21: Study Closeout Page 1 of 16 Office of Human Research For investigator-initiated studies, the Investigator has the same responsibility for investigational product inventory as an industry sponsor. In addition to documenting the above information for his/her site, the Sponsor-Investigator must also ensure the same reconciliation/disposition information for investigational product at each participating site. 3. Destruction of Investigational Drugs and Devices The destruction of investigational drugs and devices must be tightly controlled with detailed record-keeping to capture study-specific information which will not be retrievable once the once the products are destroyed, as well as to assure that there is no loss or theft of the product. In addition to the Accountability log, the following forms should be completed when destroying investigational products: IF sponsor-specific forms are available Destruction should be documented on the sponsor-provided forms. However, any pertinent data which is not collected on those forms should be documented on a separate sheet and attached to the sponsor form. IF a sponsor-specific form is not available Destruction may be documented in a typed letter, other record, or on a destruction log provided by the Investigational Drug Services Pharmacist (IDS). IF the product is a Schedule II Narcotic Destruction should be documented on a DEA-41 form and signed by two licensed individuals http://www.deadiversion.usdoj.gov/21cfr_reports/surrend/41_form.pdf When investigational products are destroyed, the destruction forms should include detailed information about the items destroyed. This includes inventory numbers, lot numbers, serial numbers, subject identifiers, expiration dates, etc. The destroyer and a witness must sign and date the destruction forms (two witnesses are preferred). A copy of destruction documentation must be kept in the regulatory files. The IDS Pharmacist will provide you a copy of the SOPs used in drug destruction at MHS Please note: When destroying medications or devices, the date (of removal) in the accountability log should match the date (of destruction) recorded on the destruction form/log. 4. Database Finalization In order to conduct the statistical analysis, study data must be subjected to a series of processes to resolve data discrepancies (data management processes termed data edit check and query resolution, or simply "database cleaning") and to standardize certain aspects of the data. It is important to submit study data for database entry as soon as possible after processing a research subject visit in order to facilitate efficient and timely data management, and ultimately the final study analysis. Chapter 21: Study Closeout Page 2 of 16 Office of Human Research 4.1 Data Discrepancies and Coding Data discrepancies are generally assessed through a combination of: • direct monitoring of data collected against the original source of such data during data monitoring, and • the use of automated database edit checks. Any discrepancies or missing data are addressed by generating written queries to the research site requesting resolution of the discrepancy. Additionally, certain data must be converted to standard terminology in a process termed "data coding". The coding process can be manual, although it is typically facilitated with sophisticated automated coding programs. 4.2 Database Freeze and Standardization Before the database is considered truly finalized and ready for data analysis, it is often subjected to a final standardization process. This process occurs after data entry has been completed, all data queries have been resolved as best as possible, and data coding has been completed. Closing the database in such a manner is often referred to as "freezing the database." The subsequent data standards process defines, in a blinded fashion, the standards for managing outlier data (out of range values) or incomplete data elements. For example for a measured study event, if month/day/year information is required to define the timing of the event, and only month and year information is available, a data standards meeting would define the standard approach to assigning a "day" for events missing that data point. This standard would be used consistently every time that "day" information was missing. 4.3 Database Lock Once such data standards have been defined and applied, the database is considered finalized and can be formally closed to further data editing, a process often termed "locking the database." The statistical data analysis can be conducted once the database has been locked. It is important to have a well-defined and documented process for finalizing a database. The following overviews the steps to finalizing the clinical database: • Data entry • Data monitoring and edit checks for discrepancies and missing data • Data queries generated and sent to research sites to resolve data discrepancies • Database changes according to query results • Data coding • Database freeze • Data standards definitions and application Chapter 21: Study Closeout Page 3 of 16 Office of Human Research • Database lock • Statistical analysis These steps are typically performed by data management and biostatistical personnel, but generally require the cooperation and assistance of the research study staff. Once all the steps are complete, all relevant parties should be notified, edit access should be removed and the date documented. If errors are found after the database is locked and it needs to be re-opened, the same steps as above should be followed to re-lock it after the errors are corrected. 5. Post-Study Communication 5.1 Institutional Post-Study Notifications At the conclusion of a study, the investigator is required to notify the Institutional Review Board (IRB) by submitting a Study Closure Report. Study sites may be closed when: Externally or internally funded protocols When follow-up data are no longer being collected on subjects enrolled in a protocol AND database finalization has taken place. Industry-sponsored studies As above, AND after the site has been notified by the Industry sponsor that the site may be closed. 5.2 Final Reports For investigator-initiated studies, the Principal Investigator (PI) is responsible for preparing a Final Report of the study. This report is prepared using the guidelines of the recipient, and submitted to the following regulatory and funding entities as applicable: • Institutional Review Board • National Institutes of Health (NIH) funding agency - for NIH-funded studies • Food and Drug Administration (FDA) - for investigator-initiated studies conducted under an Investigational New Drug (IND) application or an Investigational Device Exemption (IDE) • Funding agency / Sponsor Institutional Review Board The PI should forward a copy of the Final Report to the IRB regarding the overall conduct of the study and any publications. Chapter 21: Study Closeout Page 4 of 16 Office of Human Research NIH NIH Grantees must submit the following reports within 90 days of the end of grant support: • Final Financial Summary Report (OMB269) • Final Progress Report - The final progress report should include a summary of progress toward the achievement of the research project's aims, a list of significant results (positive or negative), and a list of publications. The report should address the inclusion of gender, minorities and children, and include any data, research materials protocols, software, or other information resulting from the research that is available to be shared with other researchers with information on how it can be accessed. • Final Invention Statement and Certification (HHS 568) - The grantee must submit a Final Invention Statement and Certification regardless of whether or not the funded project results in any subject inventions. The HHS 568 must list all inventions that were conceived or first actually reduced to practice during the course of work under the project. If there were no inventions, the form should indicate “None.” http://grants.nih.gov/grants/hhs568.pdf All forms can also be found at http://grants.nih.gov/grants/forms.htm. Failure to submit timely final reports may affect future funding to the organization. FDA For FDA reporting, the final report should follow the format of the FDA annual report. This format can also be used to prepare the report for the IRB and the sponsor. This format includes the following information: • A statement that the study is completed • The title, protocol number, purpose, population • Information about the number of subjects anticipated, entered, completed and dropped out; tabulate by age group, gender, and race • Summary of study results • Summary of most frequent and most serious adverse experiences by body system • Summary of all IND Safety Reports • List of subjects who died during participation, with cause of death • List of subjects who dropped out in association with any adverse experience • Description of what was obtained pertinent to an understanding of the drug's actions • List of preclinical studies completed or in progress during the study; summary of findings • Summary of any significant manufacturing or microbiological changes made Chapter 21: Study Closeout Page 5 of 16 Office of Human Research • Description of any significant Phase I protocol modifications made • Summary of significant foreign marketing developments with the drug Funding Agency For studies conducted using funds from a foundation grant or other source, the funding agency often requires submission of a final report. If not required, it is a generally accepted courtesy to do so. The format of the report should be specified by the funding agency. 6. Subject Unblinding and Follow-Up 6.1 Unblinding In blinded studies, subjects often request information regarding their treatment group. This information may not be made available for many months or even years after followup has been completed. Although it is not required to divulge the treatment assignment, test results or research findings to research subjects, doing so is an important way to recognize the contribution the research subject has made and can enrich the research experience for completed subjects. In certain situations it may be necessary to supply such information when it could affect the quality of follow-up care to research subjects. Research subject notification usually involves composing a letter identifying the subject's group assignment, acknowledging their contributions, and, if possible, disclosing the research findings. In industry-sponsored studies, the investigative site may need to actively request this information from the sponsor following study termination. 6.2 Follow-Up It may also be necessary to follow-up with subjects who have completed participation in a research study if significant new findings are discovered that may affect the long-term health of the subject. Examples include a product recall on an implanted investigational device or carcinogenicity associated with an investigational drug. In these instances, the investigator should attempt to send all prior subjects an IRB-approved informational addendum (letter) to their last known address. This addendum should contain a name and phone number for the subject to contact should they require additional information. The investigator should retain evidence of the communication or attempts at communication through a delivery tracking method such as certified mail. 7. Storage and Archiving 7.1 Study Record Retention The Principal Investigator (PI) is responsible for storing regulatory documents, subject files and financial records for the period of time specified by law and the study sponsor. The time period for maintaining research records is defined in various regulations. If multiple regulations apply to a particular study, the longest retention period applies. Chapter 21: Study Closeout Page 6 of 16 Office of Human Research • HIPAA regulations require that any HIPAA-regulated information, authorizations, waivers, etc. must be maintained for at least 6 years subsequent to the Institutional Review Board (IRB) acknowledgement of the termination of the research project. • DHHS regulation (45 CFR 46.115) and FDA regulation (21 CFR 56.115) state that IRB records relating to research shall be retained for at least 3 years after completion of the research. • For research funded by the National Institutes of Health (NIH), research records must be retained for at least 3 years from the date the Final Financial Status Report is submitted. • Research involving an FDA Investigational New Drug application (IND) must additionally comply with 21 CFR 312.57 and 21 CFR 312.62 by retaining records for: o A period of 2 years following the date a marketing application is approved for the drug for the indication for which it is being investigated - or - o If no application is to be filed or if the application is not approved for such indication, until 2 years after the investigation is discontinued and FDA is notified The sponsor or funding agency may require that records be retained for a longer period of time, so it is important to determine the sponsor's or funding agency's requirement as per their contract. 7.1.1 General Tips for Record Retention • Maintain lists for tracking archived research records. • Check with department for policies on storage and destruction. • Keep research records secure and confidential. • Check with sponsor or funding agency for record retention requirements. • Obtain authorization prior to record destruction. o Maintain an accurate list of records destroyed. 7.1.2 Storage Location Study documents should be retained in a secured, limited access area. It is recommended that the Recall Miami (Brambles) be utilized for the purposes of archiving study records. The address for this facility is: RECALL MIAMI (BRAMBLES) 11800 NW 100 Rd., Medley, FL 33178 Phone: (305) 884 1733. Chapter 21: Study Closeout Page 7 of 16 Office of Human Research 7.2 Human Tissue Retention The plans and procedures for retaining research subject tissue samples (includes blood, serum, urine, other bodily fluids, hair, soft tissue, bone, etc.) should be fully addressed in the study protocol. The research consent form and HIPAA authorization form must also refer to any plans for tissue retention. The study protocol should describe how the tissues will be prepared for storage and who is responsible for such preparation, how samples will be stored, the procedures to track samples and associated information as well as the security procedures to prevent unauthorized access to samples and associated information. Ownership and sponsor retention requirements for human tissue samples are generally also addressed in the Clinical Trial Agreement (CTA). It is important to be aware of the contractual requirements for tissue retention in an industry-sponsored study. 7.2.1 When tissue retention constitutes general tissue banking When tissue samples are retained for reasons beyond use of the specific research study for which they were obtained (i.e. future possible research), it is considered general tissue banking. The IRB requires written procedures describing how samples are obtained, how consent to procure samples is obtained, how samples are prepared and stored, and a security plan preventing unauthorized access to the samples and their associated information. The Informed Consent must inform the patient about the purpose their tissue/blood 8. Publications and Presentations In order to fulfill the goal of contributing to generalizable knowledge, it is generally accepted and expected that research results should be shared with the research community and the public. There are a number of venues for communicating study findings, including: • Lecture or poster presentations at seminars and conferences • Professional peer-reviewed journals and books for the discipline of study • Press releases, newspaper articles 8.1 Clinical Trials Listing Requirement Researchers intending to publish research results should be aware of the recent requirements published by the International Committee of Medical Journal Editors (ICMJE), requiring that information about clinical trials be registered on a website supported by a non-profit organization and easily accessible. For more information about this requirement, as well as other information regarding publishing, refer to the ICMJE website at http://www.icmje.org/ Chapter 21: Study Closeout Page 8 of 16 Office of Human Research 8.2 Publication Rights 8.2.1 National Institutes of Health (NIH) In the case of research funded or supported by the NIH, investigators are encouraged and expected to submit publications based upon their work. The NIH requires acknowledgement of NIH grant support with a citation on the publication such as: "This publication was made possible by Grant Number ### from xxx. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of (awarding office)." 8.2.2 Industry-sponsored In the case of industry-sponsored research, or any research project conducted under a contract, a publication clause is usually included in the study contract. This clause specifies whether or not the Principal Investigator and the Institution has the right to publish study results, and if so, the specific requirements for that publication. It is therefore important to refer to the contract or Clinical Trial Agreement to determine publication rights. It is also expected that the industry sponsor/source of funding is acknowledged in the publication. 9. Responsible Authorship Whatever the venue, publications and authorship should present the study findings in an honest, unbiased manner. The Responsible Conduct of Research standards assert several principles that should be followed to ensure the practice of "responsible authorship." (Steneck, Nicholas H. 2004, Introduction to the Responsible Conduct of Research. Office of Research Integrity - http://ori.hhs.gov/documents/rcrintro.pdf). One of the more taxing decisions in publishing study findings is the names that will appear as authors and the order in which those names will appear. To fairly and accurately represent the person(s) responsible for the work, authorship should include only those individuals who make significant contributions to the work, including any or all of the following phases: • Study design • Data collection and interpretation • Drafting of the publication • Final approval of the publication In general, the first author listed is the person who contributed most to the work and is typically responsible for writing the first draft of the publication manuscript. The sequence of the other authors may be dependent upon relative contributions, but in some departments, are listed in order of importance. The practice of "honorary authorship" is strongly discouraged. In this practice, authors are listed solely on the basis that they are chair of the department, a mentor to the primary author, or have provided funding for the research. Those individuals that Chapter 21: Study Closeout Page 9 of 16 Office of Human Research contributed to the research project but do not qualify as authors should be credited in the Acknowledgement section. 10.1 Journal Submission There are often multiple journals in any given field of study. The publication author should consider the implications of the research, the most appropriate audience, and the intended message when selecting the potential journal to which the manuscript should be submitted. Editors require authors to submit manuscripts in a style and format specific to the given journal. Instructions to authors are published at least yearly in each journal and some may have instructions available online. 10.1.1 Elements of a Publication The following are widely-expected elements of any publication: Abstract Summary of the content of the publications; provides the reader with sufficient information to determine relevance of the publication Methods Detailed description of the scientific methods used in to conduct the research; establishes credibility of the results Results Presentation of the data analysis, but no interpretations in this section - just the facts; include all results, even those that are contradictory to the researcher's conclusions Discussion/Conclusion/Summary Presentations of the significance of the findings, identification of unresolved problems, future research needs; avoid bias and one-sided reporting Notes/Bibliography/Acknowledgements The editor will evaluate whether the paper is appropriate for their journal by evaluating: • Importance of the research question • Knowledge of the current literature • Appropriateness of research methods • Clearly stated and interesting conclusions Journals usually acknowledge receipt of submissions. Typically, journals will take 3-6 months to notify investigators of acceptance, rejection or requested revisions for publication. Chapter 21: Study Closeout Page 10 of 16 Office of Human Research 10.2 Poster Presentation Many researchers choose to present study findings in the form of a scientific poster at a regional or national professional conference. Unlike an abstract or journal submission, the researcher must pay special attention to the layout and design of a scientific poster. The visual appeal of a poster will greatly impact how effectively the information will be received by audience at the conference - poorly designed, cluttered posters will least likely be read over those that have a professional, creative, and well-organized "look and feel" to them. 10.2.1 Poster Presentation Content Posters/presentations generally should include the following sections: Title Page The title page lists the intended title of the poster/presentation and eventual paper, the authors and schools or centers affiliated with the project, and the grant number (if applicable). Background The background describes the basis for the research and refers to the indications and previous research results in this area of research. Abstract The abstract summarizes the research by providing a basic description of the sampling methodology and major findings. Demographic Table This table should include more specific information about the sample population, for example, age, race, gender, and study variables intended in the specified research. Measurement This section contains information pertaining to the measurements used for the results of the presented research. For example, interviews, standardized measurements, data abstraction, etc. Methods A description of the study design and sample detail for the indicated results. Results Detailed results are specified in the results section of a poster or presentation. Use tables in this section and be sure to state major findings. Tables Suggested tables should include basic demographic results, statistical results, and findings specific to the research presented. The tables presented should include the results from the statistical analysis. Discussion Chapter 21: Study Closeout Page 11 of 16 Office of Human Research The discussion explains the findings of the research, detailing the specific differences, causes, effects, likelihood, and/or predictions of the research. 10.2.2 Poster Preparation Design Advice The author of a poster can choose to design and develop his/her own poster or have a staff member design and develop it. There are several sites on the web which can assist with design. Some of them are listed below: • University of Medicine and Dentistry of New Jersey: http://cte.umdnj.edu/career_development/career_posters.cfm • Ph.D. Posters: http://phdposters.com/howto.php • Do’s and Don’t’s of Poster Presentation: http://www.stanford.edu/group/blocklab/dos%20and%20donts%20of%20poster% 20presentation.pdf • Scientific Posters Made Easy: http://www.postergenius.com/cms/?q=articles/readability Depending on the technical experience of the researcher/author, posters can be designed using standard office software (such as Microsoft PowerPoint or Microsoft Publisher) or professional design software (such as Adobe Illustrator, Quark Express, or Adobe InDesign). In designing the poster, plan ahead for the method of printing and desired format of the finished poster. One option is to print several smaller pages on an available color printer, and then arrange and affix those pages to a larger poster board. Alternatively, it may be more desirable to print a full-size poster, in which case professional print services (Kinko’s, for e.g.) should be sought. As an alternative to designing a poster in typical software programs, a number of commercial services dedicated to producing scientific posters have emerged that simplify the design process. These providers may offer templates, design, and printing services. Using these services, the author typically chooses a template, uploads the content for each section, and a final printed version is produced and mailed back to the author. Two such providers are: • PosterSession.com (http://www.postersession.com/) • SciencePresentations.com (http://www.sciencepresentations.com/) 10.3 Intellectual Property By the nature of research activities, it is often the case that a new discovery is made or important unique knowledge has been gained as the result of research. This discovery or knowledge may be considered Intellectual Property. While there are a number of definitions, generally speaking, Intellectual Property is any product of the human intellect that is unique, novel, not obvious and possesses commercial value. Chapter 21: Study Closeout Page 12 of 16 Office of Human Research Several legal mechanisms are available to protect Intellectual Property, granting the owners the right to decide who can use their property. The mechanisms usually used to protect Intellectual Property that is derived from clinical research are patents, trademarks, and copyrights. At times, more than one type of protection may apply to a particular discovery, with each type providing protection to different aspects of the discovery. The patent protects the test itself, while the trademark protects the name of the test. 10.3.1 Categories of Intellectual Property The type of legal protection that is sought depends on the type of Intellectual Property. Data In the context of human subjects, research data refers to the information collected and/or recorded in the course of conducting the research activities. Study data can take the form of laboratory notebooks, case report forms, subject records, and the study database itself. The National Institutes of Health (NIH) defines Research Data as the "recorded factual material commonly accepted in the scientific community as necessary to validate research findings, but not any of the following: preliminary analysis, drafts of scientific papers, plans for future research, peer reviews, or communications with colleagues." This 'recorded' material excludes physical objects (e.g. laboratory samples). Research data also do not include: 1. Trade secrets, commercial information, materials necessary to be held confidential by a researcher until publication of their results in a peer-reviewed journal, or information which may be copyrighted or patented; - and 2. Personnel and medical files and similar files the disclosure of which would constitute a clearly unwarranted invasion of personal privacy, such as information that could be used to identify a particular person in a research study. Invention An invention includes "technical information, trade secrets, developments, discoveries, know-how, methods, techniques, formulae, data, processes and other proprietary ideas or matter". Tangible Research Property Tangible Research Property includes unique research products such as biological materials or chemical moieties or engineered products. Examples including organisms, cells, viruses, cell products, cloned DNA, sample compounds, sensors, devices, or diagrams. Chapter 21: Study Closeout Page 13 of 16 Office of Human Research Copyrightable Works Copyrightable works includes creations such as books, journals, articles, text, administrative reports, studies or models, glossaries, bibliographies, study guides, instructional materials, laboratory manuals, syllabi, tests, proposals, lectures, musical or dramatic compositions, films, film strips, charts, transparencies, video or audio recordings or broadcast, computer software, CD ROMS, circuitry, microprocessor designs and other works that may be copyrightable under laws of the United States and other jurisdictions. 11. Intellectual Property Ownership at MHS 11.1 Intellectual Property All Intellectual Property made, discovered, or created by MHS employees while acting within the course and scope of their employment or while performing their job duties is deemed to be “Work for Hire” which means the work is the property of MHS. All Intellectual Property made, discovered, or created by MHS employees while acting within the course and scope of employment or while performing their job duties must be disclosed to MHS. MHS may, at its discretion, enter into agreements with its employees to develop Intellectual Property as part of their job duties, which agreements may contain provisions for the sharing of ownership of the Intellectual Property, and division of royalties or other payments associated with such Intellectual Property. Such agreements must be in writing and entered into in advance of the performance of any job duties associated with said development. For additional information, please refer to the MHS Standard Practice titled Intellectual Property. 11.2 Research Data All data and research records generated in MHS remain the property of MHS. It is important to note that the data does not belong to the investigator, meaning that if the investigator should leave the institution, the data continues to be the property of the MHS. Research Data that is collected under a National Institutes of Health (NIH) grant is subject to the Freedom of Information Act (FOIA) (http://grants.nih.gov/grants/policy/a110/a110_guidance_dec1999.htm). This policy ensures that all data will be made available to the public that is: 1. supported with federal funds - and -2. cited publicly and officially by a federal agency in support of an action that has the force and effect of law Also relevant to research data resulting from an NIH-funded study, NIH's Data Sharing Policy supports the sharing of final research data for use by other researchers in an Chapter 21: Study Closeout Page 14 of 16 Office of Human Research effort to expedite translation of research results into knowledge, products, and procedures to improve human health. All NIH grant applications requesting $500,000 or more must include a plan for data sharing. The NIH provides more information concerning the NIH Data Sharing Policy at http://grants.nih.gov/grants/policy/data_sharing/ 12. Intellectual Property Protection Mechanisms The following descriptions are taken directly from the US Patent and Trademark Office (http://www.uspto.gov/web/offices/pac/doc/general/whatis.htm) 12.1 Patent A patent for an invention is the grant of a property right to the inventor, issued by the Patent and Trademark Office. The term of a new patent is 20 years from the date on which the application for the patent was filed in the United States (U.S) or, in special cases, from the date an earlier related application was filed, subject to the payment of maintenance fees. US patent grants are effective only within the U.S., U.S. territories, and U.S. possessions. The right conferred by the patent grant is, in the language of the statute and of the grant itself, "the right to exclude others from making, using, offering for sale, or selling" the invention in the United States or "importing" the invention into the United States . What is granted is not the right to make, use, offer for sale, sell or import, but the right to exclude others from making, using, offering for sale, selling or importing the invention. 12.2 Copyright Copyright is a form of protection provided to the authors of "original works of authorship" including literary, dramatic, musical, artistic, and certain other intellectual works, both published and unpublished. The 1976 Copyright Act generally gives the owner of copyright the exclusive right to reproduce the copyrighted work, to prepare derivative works, to distribute copies or phone records of the copyrighted work, to perform the copyrighted work publicly, or to display the copyrighted work publicly. The copyright protects the form of expression rather than the subject matter of the writing. For example, a description of a machine could be copyrighted, but this would only prevent others from copying the description; it would not prevent others from writing a description of their own or from making and using the machine. Copyrights are registered by the Copyright Office of the Library of Congress. 12.3 Trademark A trademark is a word, name, symbol or device which is used in trade with goods to indicate the source of the goods and to distinguish them from the goods of others. A servicemark is the same as a trademark except that it identifies and distinguishes the Chapter 21: Study Closeout Page 15 of 16 Office of Human Research source of a service rather than a product. The terms "trademark" and "mark" are commonly used to refer to both trademarks and servicemarks. Trademark rights may be used to prevent others from using a confusingly similar mark, but not to prevent others from making the same goods or from selling the same goods or services under a clearly different mark. Chapter 21: Study Closeout Page 16 of 16