Cerebrovascular Accidents or Strokes
advertisement

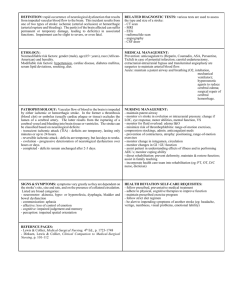
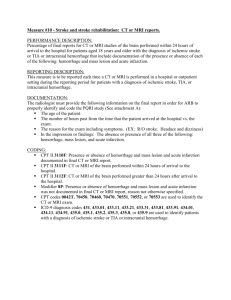
Cerebrovascular Accidents or Strokes Dr. Nusrum Iqbal Department of Medicine Lahore Medical & Dental College Lahore Definition •Stroke is a clinical condition with all the following features: –An acute neurological disorder –Produced by non-traumatic injury in the central nervous system that is vascular in origin –Accompained by focal rather than global neurologic dysfunction –Persist for longer than 24 hours or results in death within the first 24 hours Causes A. Infarction (80-85% cases) •Thrombosis •Embolism B. Hemorrhage (15-20% cases) •Intracerebral hemorrhage •Sub-arachnoid hemorrhage Clinical Classification of Stroke Depending upon the rate of development and reversibility 1. Transient ischemic attack 2. Stroke in evolution 3. Completed stroke Transient Ischemic Attack •Tranisent neurological deficit due to vascular insufficiency •Completely recovers within 24 hours •Usual duration is few minutes •Due to embolism in most cases •Risk of completed stroke is increased after TIAs •Stroke in evolution –Neurological deficity increases by step vise progression or there is a slow uninterrupted progression –May take 1-2 weeks to complete –Resembles space occupying lesions •Completed stroke –Neurological deficit lasts longer than 24 hours Pathologic Classification •Ischemic/cerebral infarction –Oclusion of cerebral artery –Thrombosis at the site of atheromatous lesions (commonest) –Embolic - Originates from thrombi in the left atrium (from atral fibrelation) and left ventrical (from acute MI) –Vegetations of endocarditis can also embolize Cerebral Hemorrhage •50% cases are due to intracerebral hemorrhage •Remaining 50% cases due to subarchnoid hemorrhage •common sites - internal capsule pons, and cerebellum Causes •Hypertension •Atherosclerosis •AV malformation •Bleeding disorders Symptoms •Sudden onset of focal neurological symptoms - limb weakness •Fever - 50% cases •Aphasia - infarction or left middle cerebral artery •Headache - raised intracranial pressure •Vomitting - raised intracranial pressure •loss of consciousness - common in intracerebral hemorrhage, massive infarction with cerebral oedema •Fits or seizures - focal seizures are common occurs within 24 hours Signs Main Artery Branch Signs Internal carotid Anterior Hemiplegia and cerebral hemianesthesia (legs are involved more than arms and face); incontinence of urine Signs Main Artery Branch Signs Internal carotid Middle Hemiplegia; cerebral hemianesthesia; dysphasia (if dominant side involved); hemianopia Signs Main Artery Branch Signs Vertebral Posterior Hemianopia, cerebral cortical blindness; pain. amnesia, thalamic Signs Main Artery Banch Signs Vertebral Basilar/ ataxia; cerebellar nystagmus; diplopia; dysarthria; dysphagia; hemiplegia/ hemianesthesia on Risk factors of stroke •Smoking •Hypertension •Diabetes Mellitus •Ischemic or valvular heart disease Investigations •Routine Tests –CBC and ESR –Blood glucose Urea creatinine and electrolytes –Lipid profile –ECG –chest x-ray facial weakness; opposite side •CT Scan –most useful investigation –infarction, intracerebral hemorrhage and subarchnoid hemorrhage or easily differentiated –Aneurysm and arteriovenous malformations may also be detected (MRI is most sensitive than CT scan) –Diagnostic yield is 50% lower when performed within 24 hours after infarction •MRI –Higher diagnostic yield than CT scans for bland infarctions (cerebellum and brainstem) –reserved for occasional case of suspected stroke in which CT scans are unrevealing •Lumbar puncture/ CSF examination –helpful if signs of meningeal irritation are present –subarchnoid hemorrhage –Not indicated in most cases –equivocal evidence of subarchnoid hemorrhage on CT scan •Echo cardiography –indicated when stroke is associated with atrial fibrilation acute MI or left sided endocarditis •Angiography - aneurysms and AV malformation •EEG - f seizures are suspected as the cause of the neurologic deficit Management Immediate Management •Admission to hospital •Secure airways, breathing and circulation •Monitor vital signs •Management of hypertension, antihypertensive treatment is indicated when the cystolic blood pressure is above 220 mmHg or when mean blood pressure is above 130 mm. –Nicardipine a calcium channel blocker that preserves cerebral blood flow –Ace inhibitors –Nitroglycerine and nitroprusside should be avoided (cerebral vesodilator) •Anti coagulations –Heparin •progressive ischemic stroke •recent studies reveals little or no benefit from full anticoagulation in progressive ischemic stroke •Thrombolytic therapy –It should be used in the first three hours after the onset of acute ischemic stroke •TPA (tissue palasminogen activator) –Proper protocol should be followed as described by National Institute of Neurologic Disorders and Stroke Increase intracranial Pressure •Elevating the head of the bed to 30 degree (promote venous return from the head) •endotracheal suctioning should be reduced in frequency and duration if possible •High dose steroids should be avoided in all cases of intracranial hypertension and can increase the risk of infection •Mannitol lowers intracranial pressure by growing water out of cerebral tissue •Hyperventilation to induce hypocapnia and reduce cerebral blood flow does not improve outcome Long term Management •Medical therapy –all risk factors should be identified and if possible, treated –Antihypertensive therapy –Antiplatelet therapy, soluble aspirin –Anticoagulants (heparin and warfarin) –polycythemia should be treated if found –baclofan (GABA agonist) is helpful in the management of severe spasticity Surgical Approaches •Internal carotid endarterectomy –patients who are shown to have internal carotid artery stenosis that narrows arterial lumen by more than 70% –risk of further TIA/stroke is reduced by approximately 75% following successful surgery –procedure has a mortality around 3% •Extracranial-intracranial bypass –there was no overall benefit, procedure is now largely obsolete Rehabilitation Physiotherapy and Speech Therapy •Helpful in relieving spasticity preventing contratures and teaching stroke patients to use walking ads •Speech therapy is recommended following aphasia •both physiotherapy and speech therapy have an undoubted psychological notes •modifications may be necessary at home e.g. stair rails, portable lavatory, bath rails, sliding boards, wheel chairs, tripods, modification of doorways and sleep arrangements •Laison between hospital occupational therapist and primary care physician is valuable Management of Hemorrhagic Stroke •General management is that of ischemic stroke •urgent neuro-surgical evacuation of the clot if it is expanding •hypertension should be controlled properly •dexamethasone is often prescribe to reduce cerebral oedema •nimodipine a calcium channel antagonist has been shown to reduce mortality Subarachnoid hemorrhage (SAH) •Is usually the result of aneurysmal rupture or bleeding from an arteriovenous malformation •SAH can differ from the other types of stroke in both presentation and management Clinical Presentation •Hallmark of the clinical presentation of SAH in headache •headache of SAH is usually abrupt in onset, persistent, progressive and worse with exertion •headache of SAH tends to be centered at the base of the skull in the cervical region •nausea, vomiting, mental status changes, stiff neck Diagnostic Evaluation •CT scans of the head (unenhanced) have a 90% sensitivity •initial diagnostic test of choice for suspected SAH •CT scans can miss SAH in the posterior fossa •a negative CT scan does not eliminate the possibility for SAH Management •Cerebral angiography is performed to identify the responsible vascular abnormality for surgical correction