handout 1 ( format)
advertisement

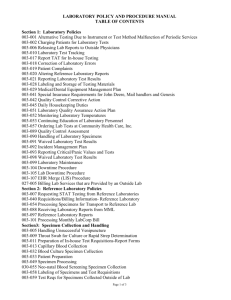
Millersville University Health Services Laboratory Procedure Manual The following 23 pages consist of some examples of laboratory policies. The first page is a list of contents for most policies. The following policies generally have been examined by our state health department on 7/11. The updates include recommendations made at that time and changes in the last 6 months as we moved to electronic health records. This change has not been reviewed by the state examiner. Chris Rooney RN BC chris.rooney@millersville.edu 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual M.U. Health Services Laboratory General Guidelines Purpose: The provision of laboratory services at Millersville University Health Services is integral to providing quality clinical care for students. Laboratory testing is completed for diagnostic purposes and to provide information for wellness initiatives upon MD/DO/NP order. General laboratory guidelines ensure consistency of practice to ensure accurate results through collections of quality laboratory specimens. Millersville University is licensed by the Pennsylvania Department of Laboratories as a moderately complex laboratory and holds a Clinical Laboratory Certificate of compliance for CLIA 88. Policy and procedure for laboratory activities are governed by state law and CLIA 88 requirements. The use of “in-house” laboratory testing as well as testing at reference laboratories provides patients with current, safe, accurate and affordable health care. MU Laboratory Testing In-House Directory of In-House Testing Blood Glucose Fecal Occult Blood Koh/Wet Preps Rapid Influenza A and B Rapid Mononucleosis Rapid Strep A Urinalysis Urine Microscopy Urine Pregnancy Each laboratory test has a procedure document that includes the following compliant with CLIA 88 and the PA State Department of Laboratories. a. Test name b. Specimen collection requirements c. Methodology with step by step directions and material required d. Quality control procedure, criteria for and documentation, remedial action procedures for unacceptable controls e. Derivation of results and limitation of methodology f. Normal/Expected ranges g. Alert Values h. Directions for preparation, storage of reagents, standards and controls i. Safety precautions j. Plan to follow if system inoperable with criteria for referral of specimens k. Documentation requirements l. Any special notes or references pertaining to test. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual The procedure manuals are physically present in the laboratory at all times as electronic documents, with Laboratory Director signed copy on file. Each procedure manual is reviewed annually and signed annually by the Laboratory Director. All staff will review and attest review on an annual basis. Updates, changes and amendments are made as needed, then documented and signed by the Laboratory Director. The Director will then convey the changes that were made to the laboratory staff by memo or meeting. Discontinued procedures are dated, signed and kept on file for two years from the date the procedure was last performed. All written test procedures will be supplemented with manufacturer’s package inserts, and/or instrument operator’s manuals. Procedures do contain direct references to manufacturer’s literature. Standing orders for all in-hours laboratory testing are reviewed and signed annually. See standing orders. MU Health Services Laboratory is enrolled in PaNEDDSS for the electronic processing of reportable conditions. A Quality Assurance Policy/Procedure manual fulfills the requirements for measuring and documenting Quality Control. All test results include the patients name, date and time test performed and identity of person performing test. All lab test results are maintained in the lab for two years. All quality control documents are maintained electronically and retained for two years. Electronic documents are password protected and backed up daily. Proficiency Testing is done for the following analytes as indicated: Blood Glucose (Waived) Not required as of 6/18/12 Fecal Occult Blood (Waived) Not required as of 6/18/12 KoH/Wet Preps (PPM) Peer review 2 x year Rapid Influenza A & B (Waived) Not required as of 6/18/12 Rapid Mononucleosis (Waived) Not required as of 6/18/12 Rapid Strep A (Waived) Not required as of 6/18/12 Urinalysis (Waived) Not required as of 6/18/12 Urine Microscopy (PPM) AAB Urine Pregnancy (Waived) Not required as of 6/18/12 Proficiency documents are maintained for two years. Quality assessment is performed monthly, reviewed by the Laboratory Director and documented. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Reference Laboratories MU Health Services utilizes three reference laboratories. Each laboratory provides a manual including a directory of services, step-by-step instructions for specimen collection and transport/storage. Courier services are provided by the reference laboratory. The reference laboratories are licensed in the State of Pennsylvania and adhere to state regulations and are compliant with CLIA ‘88. MU Health Service Laboratory uses an electronic tracking system for all labs sent out to a reference laboratory. Tracking system includes date, patient identifiers, test performed, reference laboratory used and status of reporting. This mechanism tracks which specimens are still pending from the reference lab. Documentation is backed-up and maintained for two years. See table below providing basic information regarding the three reference laboratories utilized by MU Health Services. Quest Diagnostics Manual Requisition Printed/Electronic Printed per manual Specimen Label Courier Printed/Numeric Reporting Paper copy by fax Person Pick-up 2:00 p.m. M-F Panic Phone for panic Values value – after office hour reporting per phone to ordering clinician Dr. Susan Northwall 717-538-8811, Jenny Monn 717 2011539, Anne Pryzbylkowski 717390-0754 Supplies Provided/Reorder PRN Paper Request/Faxed 6/08 Laboratory Procedure Manual ACM Medical Laboratory Printed/Electronic Printed per manual/Electronic Handwritten Center for Disease Detection Printed/Electronic Electronic PERLL Laboratory Printed/Electronic Printed Printed/Numeric Printed/Bar Code Fed Ex by 4:00 p.m. M-F Schedule pickup Paper copy by fax UPS Weekly/Wed 2 pm Schedule pick-up by calling PERRL 717-691-1500 Paper copy/fax Phone for panic value – after office hour reporting per phone to ordering clinician Dr. Susan Northwall 717-538-8811, Jenny Monn 717 201-1539, Anne Pryzbylkowski 717390-0754 Provided/Reorder PRN Paper request/faxed Secure email/ printed No Alert/Panic Values Electronic request/auto inventory Phone for panic value – after office hour reporting per phone to ordering clinician Dr. Susan Northwall 717538-8811, Jenny Monn 717 2011539, Anne Pryzbylkowski 717-390-0754 Provided /reorder PRN Paper Request/faxed Millersville University Health Services Laboratory Procedure Manual Standard Operating Procedures 1. Test Management Procedure In House Testing Client ID By Name, Date of Birth, MU ID/SSN Client Instruction Precedes all testing including Procedure, cost, normal result Specimen Labeling Specimen held for MD/DO/NP procedure Labeled with name and timed if not processed immediately Includes date, time, test, specimen source if applicable, client ID, results, testing personnel initials, test kit number and indication that internal controls were acceptable if applicable, legible. Results documented per procedure manual. Documentation Results Notification All results given to client at time of testing. Positive results reviewed by MD/DO/NP Reference Lab Selection by Staff 6/08 Laboratory Procedure Manual NA Reference Laboratory Name, Date of Birth, SSN (requested), Sex Precedes all testing including procedure, cost, method of results, notification/expected time frame Labeling per Reference lab manual – name date, specimen source and numeric label as applicable Requisition includes date, time, test, specimen source if applicable, client ID, ordering practitioner, legible, ICD codes and insurance information included. Person performing test initials order and documents collection of specimen in electronic health record. Electronic documentation in EHR of testing for results status. Reference laboratory provides report. Reviewed by ordering practitioner. Client informed of results as ordered; usually by phone with three attempts followed by email notification to call for results. Unable to contact referred back to ordering practitioner. PANIC values – results to MD/DO/NP or referral to ER/Urgent Care/PMD immediately. Patient notified of results is documented on the scanned laboratory result in the electronic health record includes date, time, special instructions from ordering provider and name off person notifying patient. No refrigerated specimens to ACM. PT and ESR to Quest/PERLL. CRP substitute for ESR for ACM. No insurance/cost concerns – review both ACM/Quest for student pricing, inform student. Millersville University Health Services Laboratory Procedure Manual CDD – STI testing $15 charged to student account – MUHS pays CDD Cost/Insurance Client informed of cost. Given option of Cash, Check, Marauder Gold or charge to University Account. No insurance billing done for in-house testing. Copy of electronic walk-out statement with ICD coding and CPT codes given to client. No Guarantee made to student regarding insurance reimbursement. Controls Performed by all staff per PADOH Laboratory and manufacturer’s recommendations on CLIA waived test kits. Documentation of control results maintained electronically for two years. Proficiency Testing Per PADOH Laboratory requirements. Performed by all testing personnel. Results reviewed by Laboratory Director. Corrective Action is score below 80% with documented evaluation. Stock supplies of test equipment and control solutions maintained and monitored to maintain minimums and stored per manufacturer’s specifications. No expired supplies used. New hire laboratory training with return demonstrations & 6 month review. Yearly procedure manual review and laboratory in-service including blood borne pathogen training. Staff informed of any lab changes by memo or meeting. Supply Ordering Staff Training 6/08 Laboratory Procedure Manual Clients informed of reference lab choice. Basic general cost estimates available from reference lab for client. It is the client’s responsibility to select reference lab if concerned about insurance payment. Insurance information provided by client. All billing from reference laboratory for ACM, PERLL and Quest. CDD will bill MU Health Services. Documentation of client choice in client chart as needed. Centrifuge RPM checked twice yearly and records maintained. Refrigerator temperature checked daily and recorded – to stay between 2-8° C. Refrigerator connected to emergency power source. N/A All staff responsible for monitoring reference lab supplies. Supplies provided by reference lab upon request. No expired supplies used. Yearly lab in-service to review reference lab procedures. New testing/equipment/changes per meeting or memo. Millersville University Health Services 2. 3. 4. 5. 6. Laboratory Procedure Manual All testing per MD/DO/NP order/standing order. Standing Laboratory Orders Millersville University Health Services Rapid Strep Urinalysis by dipstick or Clinitek Status Urine Pregnancy Rapid Mononucleosis Rapid Influenza A & B Blood Glucose by glucometer Fecal Occult Blood GC/Chlamydia by reference laboratory (urine) All positive results are referred to MD/DO/NP; PMD, Reproductive Health or Urgent Care/ER as applicable based on client condition. All staff competent to perform all waived testing – yearly testing of competency. All microscopy is provider performed. Maintenance of Universal Precautions and basic lab safety maintained in lab. MU Environmental Health and Safety Department maintains written plans for the health and safety of all laboratory personnel. MSDS available. Compliment/complaint forms are available and reviewed for corrective action by the Laboratory Director. Documents are maintained 2 years and reviewed monthly. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Millersville University Health Services Laboratory Procedure Manual Laboratory Director Date QUALITY ASSURANCE Policies and Standards It is the policy of the Millersville University Health Services Laboratory to follow the recommended guidelines of the manufacturer of the test performed and those standards that are dictated by the Commonwealth of PA and CLIA. Each test performed in the MU Laboratory has a procedure document which addresses patient preparation, sample collection, sample handling and storage, instructions for test performance, quality control testing and calibration and maintenance of equipment. Laboratory Training and Safety Basic safety procedures are posted in the laboratory. Universal precautions are maintained. A MSDS file along with a copy of the Right-To-Know law is maintained at MUHS. Each nurse is instructed in all laboratory procedures upon hire, followed by demonstration of competency. Records of training are maintained in the personnel manual. Yearly competency documentation is performed. See MU Personnel Policies for 6 month Review for new hires. Laboratory competency is documented in the 6 month MU evaluation. All staff performing tests in the MU laboratory will review each laboratory and procedure manual yearly. Staff in-services will be done at least yearly including review of quality control and quality assurance documentation, any changes to procedure or policy, and any staff concerns or suggestions. Documentation of all in-service/training is maintained in the personnel manual. Procedure Manuals Each test performed has a procedure document that describes the specific steps for performance of that test. Procedures are reviewed once a year and signed by the Laboratory Director. Changes in procedures must be approved by the Laboratory Director and staff informed of changes via in-service or memo. Competency testing will be done if procedural changes are significant. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Quality Control Testing Quality control on each test offered is completed according to manufacturer’s specification and state requirements. The control testing for the glucometer is performed every day of patient testing with a high and low control. Urinalysis controls for the Clinitek Status is performed once a week and with every new bottle of reagent strips with a positive and a negative control. Positive and Negative controls are run on the HcG Urine Pregnancy test with each new kit and monthly as per manufacturer’s specifications. Manufacturer provided external controls are run on Strep A, Mononucleosis and Influenza with each new test kit lot number. Each kit is assigned a number that is recorded on corresponding test results. The internal control is monitored with every patient testing and documented as “IC-OK” if Internal Controls are acceptable for patient testing. All test results include the initials of the testing personnel. All nursing staff are proficient in performing and documenting quality controls. Quality Control Remedial Actions Quality controls normally fall within the limits of test specification. Those outside set into motion the dictated steps for correction. The following quality control remedial actions are outlined. Observed control values acceptable? NO YES Report patient results Controls, reagents, calibrators and/or kits expired? NO YES Retest with acceptable materials Rerun unacceptable controls; Acceptable? NO YESReport Patient results Run new control, same lot#; Acceptable? NO YESReport patient results Run new control, different lot#; Acceptable? NO YESReport patient results Calibrate and/or perform maintenance; Acceptable? NO YESRerun Controls, Acceptable? NO YESRerun patient specimens, report new results Call Manufacturer for technical assistance. Store or send out all patient specimens. No patient testing is done if controls remain outside of acceptable limits. Document all actions taken. All quality control testing is recorded for each test. As new lot numbers of control or reagents are introduced, information will be documented. Instrument maintenance records with corrective actions are also maintained. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Calibrations and Maintenance of Instruments All laboratory testing equipment is calibrated per manufacturer’s specifications. Equipment with automatic internal calibration is defined. Internal controls of HcG – Urine Pregnancy, Strep A, Mononucleosis, Influenza and Fecal Occult Blood are recorded acceptable with each patient test result with “IC OK”. Instrument maintenance is per manufacturer’s specification and recorded. Microscope – Weekly cleaning and yearly maintenance check is performed. See Equipment maintenance manual for detailed explanation. Centrifuge – provided by reference laboratory. Semiannual recording of RPM’s by visual tachometer. Weekly cleaning performed. Specimen Refrigerator – Daily recording of temperature to maintain between 2and 8 C is documented and adjusted as needed. Refrigerator connected to Emergency Power source in the event of a power failure. Record Keeping All records of calibration and daily control testing are maintained for two years as required by the PA State Dept. of Laboratories and CLIA. Participation in Proficiency Testing Programs MU Laboratory is enrolled in the American Association of Bioanalyists, (AAB) Brownsville, Texas for Urine Sediment. Unknowns are sent quarterly for testing. All MD/DO/NP participate in proficiency testing on a rotating basis. Unknown results and final scores are documented in the Proficiency Testing Manual in the Laboratory. Scores are reviewed by the Laboratory Director. Any score below %100 is reviewed and evaluated. The corrective Action Checklist Form and Corrective Action Form are utilized per direction of the Laboratory Director. (See Attached.) Corrective actions are evaluated when next quarterly proficiency test scores are received. Corrective Action Forms are maintained in the Proficiency Testing Notebook. Peer review for Vaginal Wet Mounts and KOH Prep are performed by each provider performing provider performed microscopy two times every 6 months and documented. Proficiency testing for waived testing of Urinalysis, Strep A, Whole Blood Mononucleosis, Whole Blood Glucose, HcG Urine Pregnancy, Fecal Occult Blood is not required per the Pennsylvania State Department of Laboratories as of May 18, 2012, and CLIA “88. ____________________________________ Laboratory Director ________________ Date ____________________________________ Laboratory Director ________________ Date ____________________________________ Laboratory Director ________________ Date 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Blood Glucose Blood glucose measurement is done following MD/DO/NP order or when necessary by nursing protocol/standing orders. Capillary blood drawing procedure is explained to patient. Advise patient that a finger stick must be done using a lancet in order to obtain one droplet of bleed. Universal precautions for blood borne pathogens are maintained while handling specimen. Test procedure is per manufacturer’s specification. See package insert. Order and result are documented in the patient’s electronic medical record with patient name, date, time, result, time since last PO intake and testing personnel initials (documented in the comments section when adding results). Testing will only be performed if automatic calculation by glucometer is acceptable. Specimen rejection would be for insufficient droplet of blood used on test strip or improper seating of test strip into machine. Microscopic examination is not performed. No calculations are necessary. For step by step procedure, see instruction manual for glucometer. Machine calculates and displays results. Preparation and storage of test materials is listed on package inserts. Package insert describes control procedures, test methods, storage of test strips and control solution. The reportable control ranges are listed on test strip container and control solutions. External quality controls will be done every day of patient testing. Results documented on control log with glucometer and transferred to electronic quality control log every 6 months. See package insert for remedial action procedures for Quality Control Remedial action is per MU Laboratory QA/QC policy. If remedial action fails to bring controls within acceptable range – no patient testing is performed. Limitation and interfering substances are listed in package insert. Reference literature can be found in the glucometer manual, package inserts for test strips and control solutions. Normal range for patient population is 65 – 99. Correlating with patient symptoms. Panic values (less than 60 or greater than 400.) MD/DO/NP informed of panic values and if unavailable patient is referred to ER/Urgent Care or PMD. No proficiency testing required per PA Dept. of Laboratories as per CLIA ’88. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Fecal Occult Blood Fecal Occult Blood testing is performed according to package insert and with nursing standing order or MD/DO/NP order. Package insert attached. Specimen collection, processing and rejection are per package insert. Patient instructions for collection are attached. Internal controls are per package insert and are documented with results as “IC OK” in comment section of electronic results. No patient testing is reported if internal controls are not acceptable. If internal controls are unacceptable, remedial actions is per MU Laboratory Quality Assurance policy including remedial action. Reference laboratories will be used for testing as needed. Order for fecal occult blood and results are documented in electronic health record including result as “positive” or “negative,” name, date, time and initials of clinician performing test. Results are reported to ordering clinician. No calculations are required. Negative is normal result. No panic values are noted. Limitations and interfering substances are per package insert. Preparation and storage of materials is per package insert. Proficiency testing is not required per PA State Department of Laboratory and CLIA ’88 as a waived test. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual INFLUENZA A & B Influenza A & B testing is done per MD/DO/NP order or as deemed necessary by nurses according to nursing protocol and standing orders. Patient is informed of influenza testing procedure requiring a nasal swab (see Nasal Swab Procedure.) Universal precautions are maintained during procedure. Test is performed immediately on collection of specimen. Specimen rejection is per package insert and may include contamination of swab. Specimen is discarded according to OSHA regulations. Order and results are documented the patient’s electronic health record. Documentation also includes that procedural or internal controls were monitored and according to manufacturer’s specifications were acceptable with “IC OK.” The Test Kit number, IC OK monitoring and initials of performing clinician are documented in the comment section of the electronic lab result section of the electronic record. Test procedure is according to manufacturer’s specifications. See attached copy of insert. A copy of this report is maintained as a lab copy. MD/DO/NP is informed of results if available, nursing may provide care per Nursing Standing Orders. If clinical condition warrants, patient will be referred to PMD or ER/Urgent Care for evaluation. Manufacturer provided controls are run and documented each new lot number of kits. External controls are performed according to manufacturer specifications and documented in electronic control logs. Kits are numbered sequentially and this number is documented on the Quality Control Log and with each patient test result. Remedial action for unacceptable results for quality control is per Q. C. Remedial actions sheet. See attached and documented electronically on Remedial Action Log. Normal result is negative, panic/alert not applicable. No calibration or calculation required. All positive results are documented on Influenza Positive Log (attached) to facilitate mandatory electronic reporting to the Pennsylvania Department of Health. Enrollment in Proficiency testing is not required per the Pennsylvania Department of Laboratories and CLIA ‘88. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Microscopic Examination of Urine Microscopic examination of urine is performed by MD/DO/NP on a clean catch specimen of urine as ordered by MD/DO/NP or per nursing protocol, Physician Standing Orders. The urine specimen is collected per clean catch procedure and universal precautions. See Urinalysis procedure. Prior to microscopic examination, urinalysis is performed on the Seimens Clinitek Status. See Urinalysis Procedure. The microscopic examination is done immediately after collection and routine urinalysis. If not done within two hours of collection, specimen is refrigerated. Specimens left unrefrigerated for more than two hours are unacceptable. Minimum volume for microscopic examination is 1 milliliter. Centrifuged volumes less than 10 milliliters are indicated in the comment section of the lab result of the electronic health record. The urine specimen is prepared for examination by transferring 10 milliliters of urine into a disposable centrifuge tube. Urine is centrifuged for 5 minutes. The supernatant fluid is poured off, leaving 1 cc of sediment. If staining, one or two drops of Sedi-Stain are added to the precipitate. The Precipitate is rotated and re-suspended. One drop form the precipitate is placed on a glass slide using a pipette and covered with a glass cover slip. A microscopic examination using low/high power is carried out. Normal and abnormal finding are noted which include cells, crystals, casts, bacteria, etc. These findings are recorded in the lab result of the electronic health record. Comment section includes the initials of the examiner. The MD/DO/NP is performing the examination and will treat based on microscopic findings. Proficiency testing of microscopic urine sediment is done quarterly according to Pennsylvania Department of State Laboratories and performed by a certified Proficiency Testing agency. Quality assurance is per MU Health Services QA/QC protocol. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Whole Blood Mononucleosis Testing is done following MD/DO/NP request or when necessary according to nursing protocol and Physician Standing Order. Patient is informed of Mono testing procedure requiring a finger stick blood sampling. Test is performed immediately upon collection of specimen per manufacturer’s specifications using the CLIA waived whole blood method. See package insert attached. Universal precautions for blood borne pathogens are maintained during testing procedure. Specimen rejection is per manufacturer’s specification and may include inadequate amount or clotting. Order for and results are documented in the patient’s electronic health record. Documentation includes patient name, date, time, result as Positive or Negative, with indication that internal procedural control is acceptable with “IC OK,” box lot number and initials of testing personnel in the comment section of the electronic result. MD/DO/NP informed of test results; if not available, patient is referred to PMD or ER/Urgent Care as warranted by clinical condition and nursing standing orders. Test procedure is according to manufacturer’s specification. Testing is done only with whole blood, no serum or plasma testing is done at MUHS. See copy of testing insert. Storage and preparation of testing material is per package insert. External controls are run and documented with each new lot number of kit and each new operator as per manufacturer’s specifications. See electronic control log for documentation of external controls. Remedial action for unacceptable results for quality control is per Q.C. Remedial actions sheet. See QC/QA policy. No patient testing is done if controls are unacceptable. Specimen may be referred to reference laboratory. Negative is normal result, panic alert not applicable. Preparation and storage of testing material and controls is per package inserts. Enrollment in proficiency testing is not required per PA State Department of Laboratories in accordance with CLIA ’88 as this kit is CLIA waived for whole blood. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Urine HcG Pregnancy Testing is done following MD/DO/NP request or as deemed necessary by nurses according to nursing protocol and standing orders. Patient is instructed in collection of urine specimen, first AM voided specimen is preferred. Universal precautions are maintained during procedure. Test is performed immediately upon collection of specimen. Specimen rejection is per package insert . Order for and results are documented in the patient’s electronic medical record. MD/DO/NP is informed of positive results if available. Nursing care for positive result is per Nursing Policy and Procedure manual. If clinical condition warrants, patient will be referred to PMD or ER/Urgent Care for evaluation. Specimen is discarded according to OSHA regulations. Documentation in electronic medical record includes patient name, date, time, and result as either positive or negative. Indication that internal control was acceptable per manufacturer’s specifications with “IC OK,” assigned box number per electronic control log and initials of testing personnel is documented in the comment section of the electronic results. Referral to reference lab for confirmatory testing is per MD/DO/NP or standing orders. Test procedure is according to manufacturer’s specifications. Storage and preparation of materials is per package insert. See attached. Manufacturer provided external controls are performed per manufacturer’s specifications. External controls are documented for each lot of test kits and monthly. Each kit is assigned a number and documented on the electronic HcG Control Log and with each result. Remedial action for unacceptable results for quality control is per QC/QA procedure manual. See remedial action sheet. Normal result is negative. Panic/alert is not applicable. No calibration or calculation is required. Enrollment in proficiency testing is not required as of May 18, 2012 per the Pennsylvania State Dept. of Laboratories and CLIA’88 for waived testing. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Strep A Testing is done following MD/DO/NP request or as deemed necessary by nurses according to nursing protocol and standing orders. Patient is informed of Strep procedure requiring a throat swab. Universal precautions are maintained during procedure. Test is performed immediately upon collection of specimen. Specimen rejection is per package insert and may include contamination of swab by touching tongue. Order for and results are documented in the patient electronic medical record. MD/DO/NP is informed of positive results. Nursing care for positive result is per Nursing Policy and Procedure manual. If clinical condition warrants, patient will be referred to PMD or ER/Urgent Care for evaluation. Specimen is discarded according to OSHA regulations. Documentation in patient electronic medical record includes patient name, date, time, result as either positive or negative. The results comment section includes the performing technician’s initials, indication that internal control was acceptable per manufacturer’s specifications with “IC OK,” and assigned box number per electronic control log. Referral to reference lab for throat culture is per MD/DO/NP or standing orders. Test procedure is according to manufacturer’s specifications. Storage and preparation of materials is per package insert. See attached. Manufacturer provided external controls are performed per manufacturer’s specifications. External controls are documented for each lot of test kits. Each kit is assigned a number and documented on the electronic Strep A Control Log with result. Remedial action for unacceptable results for quality control is per QC/QA procedure manual. See remedial action sheet. Normal result is negative. Panic/alert is not applicable. No calibration or calculation is required. Enrollment in proficiency testing is not required as of May 18, 2012 per the Pennsylvania State Dept. of Laboratories and CLIA’88 for waived testing. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Throat Swab Purpose A throat swab is a technique for identifying disease bacteria in material taken from the throat. Most throat cultures are done to rule out infections caused by beta-hemolytic streptococci which cause strep throat. Hemolytic means that these streptococci destroy red blood cells. Equipment Gloves Tongue Blade Light as needed for Visualization Throat Swab or Culturette Rapid Strep Kid Waste Container Procedure: 1. Identify Patient 2. Explain procedure and purpose of testing. 3. Wear gloves and maintain Universal Precautions 4. The patient is instructed to tilt head back, open mouth wide and breathe out slowly trough mouth saying “Ah.” 5. With the tongue depressed with the tongue blade, swab the back of the throat and the tonsils with the sterile swab. The swab is applied to any area that appears wither very red or discharging pus. 6. The swab is removed gently without touching the teeth, gums or tongue. 7. The swab is immediately placed into the Rapid Strep cassette or the culturette container. The procedure is continued per Strep A Procedure or per Reference Lab Manual for throat culture with culturette. 8. Remove gloves, discard supplies in waste container per universal precautions. 9. Document procedure in electronic health record. Inform student of date of expected results and verify method of contacting student to inform of Culture results. _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Urinalysis Test is done per MD/DO/NP order or standing order. See Standing Orders. Patient is given clean cup for urine specimen. Patient informed of clean catch urine procedure per Urine Collection Procedure. Universal Precautions are maintained throughout procedure. Test is performed immediately upon collecting specimen. Reagent stick urinalysis is then performed with the Seimens Clinitek Status. Testing is performed per manufacturer’s instructions – see attached Seimens Clinitek Status documentation. Order for and results are documented in the patient’s electronic medical record. Documentation includes patient name, date, time, and test results. Electronic results include the initials of the performing clinician. Control log maintains inventory for testing materials. Labeled specimen is then centrifuged for five (5) minutes if microscopic analysis of urine sediment is ordered. Spun urine is given to provider for further preparation and examination per policy. A specimen would be rejected for the following (a) inadequate amount or (b) contamination. Specimen is disposed per OSHA regulations Test procedure is per manufacturer’s specifications. Preparation and storage of testing materials are per manufacturer’s insert. See insert. The Seimens Clinitek Status is self-calibrating by computer stored module. Problems with the automatic calibration are referred to manufacturer. No patient testing per Seimens Clinitek Status if calibration failure is not resolved. Dip stick urine with Seiman’s Multistix 10 SG is permissible in the event of Seimens Clinitek Status failure. See Seiman’s Multistix 10 SG package insert for test procedure specifications, limitations and interfering substances. External controls (positive and negative) are run once a week for Seimens Clinitek Status and with every new bottle of Seimen’s Multistix as per manufacturer recommendations. Controls are performed in same manner as procedure and documented in electronic control log. Remedial actions for unacceptable results for quality control are per QC remedial action sheet/QA/QC policy. No panic/alert values. No calculation or calibration is done. Referral to reference laboratory is per MD/DO/NP order/standing order. Reference ranges for patient population are listed on the electronic result. No calculations or derivations are required. Enrollment in proficiency testing is not required by Pennsylvania Department of Laboratories as of May 18, 2012 and CLIA ’88. _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director _____________________________________ Laboratory Director 6/08 Laboratory Procedure Manual ____________ Date ____________ Date ____________ Date ____________ Date Millersville University Health Services Laboratory Procedure Manual Wet Mount/KOH Procedure Definition/Purpose A sample of vaginal discharge is mixed with a salt solution on a microscope slide. The slide is checked for bacteria, white blood cells, and unusual cells called clue cells. If clue cells are present, it means bacterial vaginitis is present. KOH (potassium hydroxide) medium is used to enhance the recovery of fungi. Body fluid pH is calculated with the use of pH paper. The direct examination of a clinical specimen is the most rapid, cost-effective diagnostic aid in the laboratory. Microscopic examination of a sample is used to identify the motility and morphology of microorganisms, fungal elements, protozoan trophozoites and helminthes eggs and larvae. The visual examination assists the laboratory and the clinician in quickly identifying the causative agent of infection so treatment may begin. Proper sample collection is important in diagnosing infection. Samples may be treated with potassium hydroxide (KOH) to enhance the recovery of fungi or stained with iodine to enhance the recovery of trophozoite nuclei and vacuoles. Wet mount samples may be obtained from various clinical sites and sources. Equipment: Exam gloves Cotton tipped swabs (2) and Kova Tubes (2) Specimen (obtained during speculum examination for vaginal secretions or by clinician for other sources) Normal Saline, KOH, Sedi Stain (KOH – Protect from light) 2 clean microscope slides with cover slips Microscope pH paper Scalpel, tongue blade, skin curette, or other blunt object (Skin Scrapings) Red Hazardous Waste Container 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Procedure: Vaginal Wet Mount 1. Put on gloves. 2. Obtain the specimen with cotton tipped applicator. See Pelvic Exam Procedure. Specimens should be examined within two hours of collection. The sample should remain at room temperature. Proper specimen collection and handling of vaginal samples is crucial for accurate results. The vaginal vault and walls should be swabbed using one or two swabs. If any fluid has pooled in other areas, these areas should be swabbed as well. Use of vaginal lubricants, douches, tampons, contraceptive jelly, and medications may interfere with the examination. Patients should avoid using these items before sample collection. In some cases, the gram stain may be used to aid in the diagnosis of these patients. 3. Do one/or more of the following: a. Put one drop of normal saline in Kova tube; insert cotton-tipped applicator with specimen. Vigorously mix the swab (s) in and out of the saline making sure to collect all the material adhering to the side of the tube. Remove the swab from the saline and depress onto a clean, dry microscope slide expressing a small amount of fluid. b. Insert cotton-tipped applicator with specimen into dry Kova tube. Put one drop of potassium hydroxide (KOH) on the right third of the slide. Mix the sample of vaginal discharge on the wooden end of the cotton-tipped applicator with the drop of KOH on the slide. Use both a rolling and a stirring motion to mix the vaginal discharge with the drop of solution. c. Place cotton-tipped applicator with specimen in Kova tube. Use two clean microscope slides and put one drop of normal saline on the middle of one slide and one drop of potassium hydroxide on the middle of the second slide. Roll the plain wooden end of a cotton-tipped applicator in the specimen of vaginal discharge. Mix the sample of vaginal discharge on the wooden end of the cotton-tipped applicator with drop of normal saline on the slide. Repeat and mix the sample with the drop of potassium hydroxide if both solutions are being used. Use a rolling and a stirring motion to mix the vaginal discharge with the drop of solution. 4. The pH and the amine (“whiff”) test often are performed before the microscopic examination. The clinician test the pH at the time of sample collection a pH greater than 4.5 may indicate bacterial vaginitis (BV) or trichomoniasis. The amine test is performed prior to cover slipping the saline preparation. The fishy or amine odor is characteristic in the presence of Trichomonas vaginalis and Gardnerella vaginalis. 5. Cover the mixture of specimen sample and solution with a cover glass (coverslip) by sliding the coverslip onto and over the specimen. This is accomplished by putting the edge of one side on the coverslip into the mixed specimen/solution and drawing it to the longitudinal 6/08 Laboratory Procedure Manual Millersville University Health Services 6. 7. 8. 9. Laboratory Procedure Manual edge of the slide. When the specimen/solution is under the entire edge of the side of the coverslip, slide the coverslip over the rest of the mixed specimen/solution on the slide. The wet smear slide of vaginal secretions is now ready for microscopic evaluation. Examine secretions. The saline slide should be examined first to allow the KOH to properly digest other cellular elements in the sample such as epithelial and blood cells. 8. Begin the microscopic review of the slide by examining the saline preparation. The examination should begin using the 10x objective noting cellular distribution and obvious cellular and fungal elements. The 40x objective is used to identify the cells, motile Trichomonas, yeasts, and fungal hyphae. The KOH slide should be examined with the 10x objective for any yeast and hyphae. Discard slides in Red Hazardous Waste Containers and maintain universal precautions in glove disposal and hand washing. Skin Scrapings Skin scraping examinations are used to identify fungal infections of the skin, mouth and nails. Fungus lives in the stratum corneum layer of the skin. KOH is used to digest this layer of skin so that the fungal growth with its visible hyphae and spores is exposed. Skin scraping examinations are indicted in areas of broken hair or baldness, presence of scaly lesions on the skin, crumbling or scaly nails or nail beds, and white plaque in the mouth. The proper collection of a skin scraping sample is crucial to the recovery of the fungus. In obtaining and preparing the sample: 10. Clean the infected area with 70% alcohol. Scrape the infected area using a scalpel, skin curette, tongue blade, or other blunt object. Infected nails may require a portion of the infected nail to be clipped. 11. Place the sample on a microscopic slide and coverslip. 12. Apply gently heat (if practitioner desires) to enhance the digestive capabilities of the KOH. If 40% dimethyl sulfoxide (DMSO-KOH) is used, heating the sample is unnecessary. 13. Let the slide sit for 10 minutes to allow for KOH digestion. 14. Examine the slide using teh10x objective. All suspicious areas should be examined using the 40x objective. 15. Keep the light intensity of the microscope low. I the light intensity is too high, the fungal elements may not be seen. 16. Discard slides in Red Hazardous Waste Containers and maintain universal precautions in glove disposal and hand washing. 6/08 Laboratory Procedure Manual Millersville University Health Services Laboratory Procedure Manual Documentation Order for vaginal wet mount (vaginal wet prep) and results are documented in the patient electronic health record. Documentation includes the patient name, date, time, specimen source, and findings. The comment section of the result includes the initials of the examining clinician. Preparation and Storage of solutions (KOH and Sedi Stain) and pH paper is per manufacturer’s recommendation. See package inserts. MSDS on file. No calibration is required. No alert values. Specimens may be referred to a reference lab for testing as ordered. Quality Control Every 6 months clinicians will compare results from two patient specimens and document findings for peer review. Discrepancies will be discussed, comments will be documented. Laboratory Directory will review and sign Peer Review for Vaginal Smear Wet Mounts. (See attached copy.) _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date _____________________________________ Laboratory Director ____________ Date 6/08 Laboratory Procedure Manual