Cardio86-CardiacCycle
advertisement

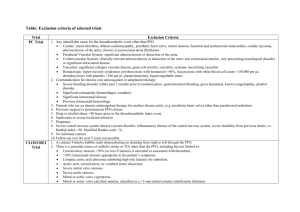
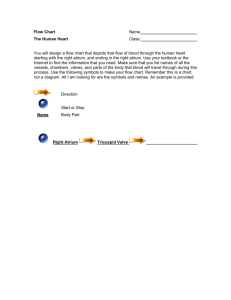
Checked by Dr. Smith Cardio #86 Fri, 01/29/03, 11am Dr. Smith Jennifer Uxer for Jaclyn Levan Page 1 of 4 Cardiac Cycle I. II. Introduction Practice questions will be posted for Monday’s workshop. Another set will then be posted to help with the week’s studies. Note that the last to ppt slides will not be addressed on this exam. Be able to construct elements of the Wigger’s Diagram because you understand the physiology. Refer to the Wigger’s Diagram as you’re studying Dr. Downey’s lectures. Learn how things relate to each other: know what’s going on in the contractile phase, how things relate in the P/V loop. Note that both Wigger’s Diagrams in the notes are from different sources. The 1st was used because it fits nicely on a slide and is the same as the one in our text. The second is helpful because it has things broken out for the left side of the heart and the right side of the heart. Be able to answer questions on differences in pressures. Pulmonary artery vs aorta pressure Right ventricular pressure vs left ventricular pressure. These pressures are the same in the chambers during diastole. There’s a problem if they’re not the same. Preload = end diastolic volume = the increase in the stretch in the chamber Wigger’s Digram (fig 23 – 10, p. 369) A. Overview 1. Systole and Diastole—think of these in terms of the electrical event or mechanical events 2. Mechanical vs Electrical ECG shows the electrical activation/inactivation Mechanical events are associated with the heart as a pump— contraction/relaxation. Compare the atrium and ventricle. If it’s not said explicity, the reference is to the left ventricle. Is the onset of atrial systole at the same time as ventricular systole? No. The electrical event precedes the mechanical event. The electrical simulation begins in the atrium, so it contracts (P wave) before the ventricle. B. Normal Valve Function 1. Pressure gradient determines if they are opened or closed. 2. Passive vs active: Valves are passive. Their opening and closing is dictated by the pressure gradient, a ‘swinging door’ effect. Leaflets prevent valves from swinging the wrong direction. Series of events: high pressure builds up, the valve opens, high pressure builds on the other side, and the valve closes. If the valves don’t work properly, there’s pathology (lecture in 2 weeks) Checked by Dr. Smith Cardio #86 Fri, 01/29/03, 11am Dr. Smith Jennifer Uxer for Jaclyn Levan Page 2 of 4 3. Papillary muscles are on the inside of the chamber, are tethered to the valves via the chordae tendineae, and keep the valves from prolapsing back. They’re needed on the AV valves. In the atrium there’s about 5 – 10 mmHg; in the ventricle there’s about 120 – 200 mmHg (upper end is hypertensive). A large pressure gradient is established between the 2 chambers and causes lots of strain on the valves. The papillary muscles are activated to keep the valve from flopping back. 4. Heart sounds aren’t really the sound of the valves closing. They’re due to the turbulence created in the blood flow and involve vibrations in the chamber walls. C. Atrial Systole 1. Ventricles fill just before systole. 2. Electric signal is generated from the SA node, and the electrical wave travels through the atria. (P wave on the ECG precedes atrial contraction) 3. The atrial contraction precedes the ventricular contraction generating a pressure wave. (Atria contract while the ventricle is relaxed.) Venous flow still continues into the atria, so if the AV valve is open, the atria is a conduit to the ventricle. 4. a wave (atrial pressure)—Dr. Smith’s not real concerned with this. 5. Volume increases in the atrium and the pressure slowly increases due to the additional volume. 6. Electrical event is started turning on contraction. The atrium squeezes and increases the pressure. When the valve opens, the atrium and ventricle are essentially the same chamber and their pressures are the same (changes track together). 7. When the atrium squeezes, the pressure increases and pushes a little extra blood into the ventricle. This “tops off” the ventricular filling. Most filling doesn’t happen during atrial contraction. At rest, this “topping off” atrial contribution is about 10% (CHANGE TO THE POWERPOINTS!!). During exercise, it can contribute up to 20-25%. Atrial fibrillation is a discoordinated sequence of activation. If this occurs, you lose the topping off of the ventricle. At rest, this is not a profound effect on preload. During exercise, it limits the cardiac output. 8. 4th heart sound (normal due to atrial contraction—uncommon) Heard in people with think chest and is associated with pressure and little extra flow. D. Ventricular Systole 1. Electrical activation starts with the QRS before contraction. 2. Contraction starts: Ventricular pressure increases because blood’s virtually incompressible and is rapidly greater than atrial pressure. Valve slams shut—a passive event with activated papillary muscles. During filling Patria = Pventricle and they track together. (Atrial pressure is a tad higher than ventricular to establish the gradient for flow) Checked by Dr. Smith Cardio #86 Fri, 01/29/03, 11am Dr. Smith Jennifer Uxer for Jaclyn Levan Page 3 of 4 Valve status at the beginning of contraction: miral valve—closed; aortic valve—closed (Mitral valve prolapse is when you get a clicking sound. It’s like a sail on a sailboat when you change directions. The sail pops. The valve is the same idea.) 3. Ventricular systole has 3 components 4. Component 1: Isovolumetic (no change in volume) contraction begins at end-diastolic volume QRS wave (ECG) precedes contraction Pv>Pa --AV valves close (no blood movement) 1st heart sound—blood slams against the valve creating turbulence 5. Component 2: Rapid ejection Pv>PA--aortic valve opens (rapid ejection of blood due to the large pressure head) ventricular volume decreases fastest aortic blood flow is at peak atrial pressure rises slowly as venous return continues 6. Reduced ejection T wave results from ventricular repolarization—repolarization is NOT complete until the T wave is finished Pv ≤ PA but aortic flow continues due to inertia of blood closure of aortic valve ends period completely depolarizing E. Ventricular Diastole 1. What contributes to the relaxation of the muscle? Ca2+ When this is sequestered back into the sarcoplasmic reticulum (SR) from the cytoplasm, the contraction stops = relaxation 2. Systolic pressure implies peak pressure; this occurs a few msec after peak aortic pressure. 3. In relaxation, ventricular pressure decreases. You still have blood flow due to the force that was generated on the blood. Momentum keeps it moving. Clarifying this: The incisura is where aortic pressure can actually be slightly above LV pressure during systole, yet flow continues and the valve remains open. This is due to the inertia of ther blood generated by the forceful contrcation-this inertia of forward blood movement keeps the valve open despite the possibility that aortic pressure is slightly greater than LVP. 4. Isovolumetric relaxation Pv < PA-- aortic valve closes (no blood movement)—both valves closed 2nd heart sound atria are filling (atrial pressure v wave) ventricular pressure rapidly decreasing 5. Rapid ventricular filling Pv < Pa-- AV valves open blood flows through atria to fill ventricles—acts as a conduit Checked by Dr. Smith III. Cardio #86 Fri, 01/29/03, 11am Dr. Smith Jennifer Uxer for Jaclyn Levan Page 4 of 4 3rd heart sound (usually turbulence due to high flow)—not usually heard Why’s there rapid filling at the beginning of diastole? 1. pressure has built up. 2. valve opens and the ventricle hasn’t finished relaxing—it’s extremely compliant and will accept blood. Therefore, pressure CONTINUES to decrease after the valve opens during the first few msec. 6. Reduced ventricular filling ventricular filling continues at a slower rate ventricular and atrial pressures slowly rise together 7. ECG in state of diastolic phase (T-P interval) All ventricular cells are at resting membrane potential 8. What’s the atrium doing wile the ventricle contracts? Filling because venous return doesn’t stop. 9. Electrical status of cell membrane resting potential is the same: ~ - 85 to 90mV. Things to play with and their effect on the cardiac cycle 1. Effect of heart rate Change in heart rate on a beat to beat basis How does slowing it down/speeding it up change the cardiac cycle duration? Slow HR, increase filling time, increase end diastolic volume, increase preload, increase stroke volume (assuming all else is constant—Starling’s Law) 2. Where’s preload on Wigger’s diagram? Think about changes in it. 3. Afterload Has different elements On the Wigger’s diagram, the effectiveness of systole is indicative of afterload Essentially, it’s the load to lift in isolated muscle. The pressure to overcome before the heart starts ejecting blood. Affected by changes in vascular resistance. Increase the resistance, must increase the pressure, more energy is spent overcoming afterload, decreased blood ejection (Ohm’s Law) 4. Contractility Increase the rate of ventricular pressure, increase the rate of increase in pressure (think about that one for a minute) Increase for given preload and afterload Rate of relaxation—leucotropy, diastolic function. Stimulation of the sympathetic nervous system—augment contraction, accelerate relaxation process.