Physiologic differences
advertisement

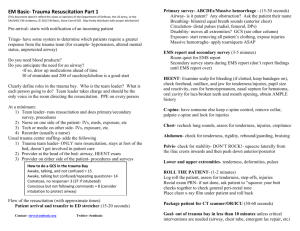
Age-specific differences Describe the anatomical and physiological differences that might affect resuscitation in the following groups a) Neonatal T Ex b) Infant T Ex c) Paediatric T Ex d) Elderly T Ex Neonatal/ Infant and Paediatric Resuscitation: THE FIRST FEW MINUTES of a neonate's life may be the most critical time to ensure a favorable future. A neonate in distress who is not immediately and effectively resuscitated is at risk for long-term physical, mental, and emotional disabilities. Resuscitation of the newborn infant presents a different set of challenges than resuscitation of the adult or even the older infant or child. The transition from dependence on placental gas exchange in a liquid-filled intrauterine environment to spontaneous breathing of air presents dramatic changes and physiologic challenges to the infant within the first minutes after birth. Newborn Resuscitation: Unique Features Right to Left shunting risk with hypoxia: In utero, the fetal pulmonary vascular resistance is higher than systemic resistance, so that most right ventricular output is shunted away from the lungs, through the ductus arteriosus, and toward the placenta. The low-pulmonary blood flow leads to a relatively low-left atrial pressure. The highpulmonary vascular resistance also leads to high-right ventricular end-diastolic pressure and high-right atrial pressure. The effect of the high-right atrial pressure, combined with a low-left atrial pressure, causes blood to be shunted across the foramen ovale from right atrium to left atrium. With the newborn's first breath, pulmonary vascular resistance drops dramatically. Blood flow to the lungs increases, thus increasing left atrial pressure and effectively closing the foramen ovale. The ductus arteriosus remains open from hours to days, and the foramen ovale remains patent by passage of a probe for years. As long as pulmonary vascular resistance remains low compared to systemic vascular resistance, clinically significant right to left shunting at these 2 sites is minimal. Hypoxia and acidosis → pulmonary vasoconstriction and systemic vasodilation → delay in permanent closure of fetal channels → Right to left shunting of venous blood to the systemic circulation through the foramen ovale or ductus arteriosus → worsens hypoxemia. Blood circulated through chest compressions may completely bypass the lungs; this situation is not likely seen in older children or adults. Liquid diffusion barrier in lungs In asphyxiated, nonbreathing neonates, the lung liquid remains in the alveoli, thus increasing the diffusion barrier to oxygen and decreasing the compliance. Artificial ventilation may be more difficult to deliver because of this lower compliance. The median airway pressure to cause adequate chest wall movement over the first 10 breaths of artificial ventilation was 40 cm H2 O. This inspiratory pressure exceeds the pressure-release valve on some resuscitation bag-valve assemblies, and exceeds the recommendations for inspiratory pressure in some texts. Not occluding the pop-off valve or using a different type of bag-valve assembly can lead to inadequate ventilation and an unsuccessful resuscitation. Laryngeal Airway Reflexes During ischemia, intense firing of laryngeal airway adductors causes airway obstruction manifested by absent airflow. This airway closure is believed to be a protective mechanism for retention of lung volume and is described clinically as “braking” or “grunting.” This obstruction may cause temporary difficulty in bag-mask ventilation, and may make tracheal intubation difficult until the laryngeal adductors relax. Neural Reflexes during artificial ventilation Overinflation of the lung can cause activation of the Herring-Breuer reflex that leads to apnea. Pressure from the face mask can stimulate the trigeminal reflex, which slows the heart rate. In summary, anatomic and physiologic differences in the newborn infant make cardiopulmonary resuscitation (CPR) significantly different than in the older child and adult. Physiologic differences Cardiovascular. Children have a higher cardiac output and oxygen consumption per kilogram than adults. They support this higher output with a higher baseline heart rate. Infants are heart rate dependent for their cardiac output. In other words, they have a fixed stroke volume, and must increase their heart rate to increase cardiac output. They may respond to stress, such as hypoxia, by becoming bradycardic, and therefore decreasing CO. This can make resuscitation quite difficult. Normal vital signs for children include higher heart rates and lower blood pressures than adults. Age Heart Rate Systolic Pressure Diastolic Pressure Preterm 1000g Newborn 130-150 45 25 110-150 60-75 27 6 Months 80-150 95 45 2 years 85-125 95 50 4 Years 75-115 98 57 8 Years 60-110 112 60 Respiratory. Minute volume is increased, corresponding with the increased cardiac output. This is supported by an increased respiratory rate. Tidal volume and dead space are equivalent to adults on a per kilogram basis. Children desaturate rapidly because of increased utilization of oxygen per kilogram , and because their FRC is decreased under anesthesia. FRC decreases under anesthesia because of small alveoli, and a very compliant chest wall. (No rigid box effect like adults have. ) Both of these things lead to increased atelectasis. Variable infant adult Respiratory frequency 30-50 12-16 Tidal Volume ml/kg 6-8 7 Dead space ml/kg 2-2.5 2.2 Alveolar vent. 100-150 60 FRC 27-30 30 Oxygen consumption 6-8 3 Temperature regulation Pediatric patients lose heat to the environment more readily than adults. This is due to an increased surface area per kilogram. This is compounded by cold intravenous fluids, dry anesthetic gases, and wound exposure. Hypothermia is a serious problem which can result in delayed awakening, cardiac irritability and respiratory depression. Infants cannot shiver, but must metabolize brown fat to maintain temperature. It is important to PREVENT heat loss with a warm operating room environment. Anatomic differences Airway anatomy. There are five key differences between the adult and pediatric airway . 1. Proportionately larger head and tongue 2. More anterior and cephalad larynx 3. Long, sometimes floppy epiglottis 4. Short trachea and neck. 5. THE NARROWEST POINT IN THE PEDIATRIC AIRWAY IS THE CRICOID CARTILAGE Children require a gentle mask fit, taking care not to obstruct the airway by compressing the soft tissues under the chin. A straight blade is generally more appropriate for intubating children because of the shape of the epiglottis. Because the airway is cone shaped, with the narrowest point at the cricoid cartilage, an uncuffed tube is adequate to seal the trachea. Using an uncuffed tube allows us to maximize the inner diameter of the tube, decreasing airway resistance and turbulence. Cardiac anatomy. Infants are born with an anatomically patent foramen ovale and ductus arteriosus. The ductus closes in the first day of life. The foramen ovale may remain probe patent for life, but physiologically closes in the first day of life. This can be important, because bubbles in IV fluid can cross the PFO and go directly to the brain. Pharmacologic Differences Pediatric drugs are generally dosed on a per kilogram basis Neonates are more sensitive to opiate analgesics during the first four weeks of life, leading to an increased risk of apnea. Inhalational anesthetics reach the brain faster in children , allowing us to perform inhalation inductions more easily. The volume of distribution for most drugs, including muscle relaxants, is increased in children, so a standard dose leads to a lower plasma level than in adults. However, children are more sensitive to the effects of muscle relaxants , so a lower plasma level leads to the same effective dose. Also read PDF document on neonatal differences in resuscitationdifferences betwe adult and pediatric trauma.pdf neonatal resuscitation differences from adults.pdf RESUSCITATION OF THE GERIATRIC PATIENT AIRWAY: EVALUATION AND MANAGEMENT The elderly have a significant loss of protective airway reflexes. Deliberate decision making and proper airway management are required to minimize complications and prevent life-threatening aspiration. Anatomically, the geriatric airway differs from the typical adult airway in a number of ways. The patient may be edentulous, or dentures may be in place. Teeth can be quite brittle and fracture easily. Well-fitting dentures make bag-valve-mask ventilation easier and more effective; however, all loosefitting or partial dentures should be removed. The mouth may not be able to be opened very wide, and immobility of the cervical spine, especially at the atlanto-occipital joint, may make visualization of the glottis difficult or impossible. Proper positioning of the patient with the neck flexed at the chest and head extended should be accomplished before induction. Hyperextension of the neck is counterproductive and often not possible. The oral cavity should be assessed prior to medication administration. A Miller blade has a smaller flange than a Macintosh and leaves more room for visualization of landmarks and passage of the endotracheal tube. Advanced airway management frequently requires rapid sequence induction: with coadministration of a sedative hypnotic and neuromuscular blocking agent to facilitate laryngoscopy and intubation. Additional drugs, such as opiates and lidocaine, are occasionally administered to blunt the increase in intracranial pressure from laryngoscopy. A small priming dose of nondepolarizing neuromuscular blocker may be administered before succinylcholine. In the elderly, such priming can abolish ventilation and airway reflexes completely and should be avoided. In addition, because the elderly are more sensitive to most induction agents, the doses of barbiturates, benzodiazepines, and etomidate should all be reduced between 20% and 40% to minimize the risk of cardiac depression and hypotension. Doses of opiates and lidocaine should also be reduced. The doses of neuromuscular blocking agents should not be reduced. BREATHING: MANAGEMENT OF RESPIRATORY FAILURE Humans undergo a series of changes in the respiratory system with age, including a decrease in fixed expiratory volume in 1 second (FEV1 ), functional vital capacity (FVC), FEV1 /FVC, and peak expiratory flow rate (PEFR). A decrease in diffusion capacity as well as changes in ventilation-perfusion mismatch result in a predictable decrease in baseline arterial oxygen tension with age. Consideration of this relationship is essential in the assessment of arterial hypoxemia: Changes in the compliance of both lung and chest wall result in an increased work of breathing with age. This coupled with frequent, underlying, nutritional deficiency and other factors make the elderly much more susceptible to respiratory failure. Because both ventilatory and heart rate responses to both hypoxia and hypercapnia are reduced in the elderly, geriatric patients are also at risk for occult respiratory insufficiency. A chest radiograph is an important adjunct in determining the cause of respiratory distress. An EKG is mandatory in all critical elderly patients, as silent myocardial ischemia is prevalent among many acute illnesses. Arterial blood gas analysis is helpful in determining the response to therapy and disposition of ED patients in respiratory distress; however it is rarely helpful in determining its cause; delaying acute resuscitation to draw a specimen is rarely worthwhile. Withholding oxygen to an elderly patient in extremis to document arterial saturation on room air is a practice that should be condemned. Similarly, withholding oxygen in a patient with COPD for fear of abolishing respiratory drive and inducing a respiratory acidosis is generally unfounded. If concern for CO 2 retention exists, a venturi mask should be used in conjunction with a pulse oximeter to provide the necessary inspired oxygen concentration to keep saturation between 85% and 90%. CIRCULATION: INITIAL ASSESSMENT OF PERFUSION AND SHOCK STATES The aging cardiovascular system undergoes a number of anatomic and functional changes including an agerelated decrease in heart rate and cardiac output, as well as decreased cardiopulmonary reflexes with changes in central venous pressure. These changes, coupled with a high incidence of pre-existing cardiovascular disease, result in decreased cardiac reserve and an inability to mount a cardiovascular response to stresses such as hypovolemia, sepsis, trauma, acute coronary ischemia, or respiratory failure. The initial approach to the geriatric patient in shock begins with the rapid intravenous access and appropriate use of resuscitative fluids in all patients without obvious signs of volume overload. Although aggressive fluid resuscitation may result in cardiogenic pulmonary edema in patients with limited cardiac reserve, multiple small (250 mL) fluid boluses, with repeated attention to physical examination signs, should prevent significant volume overload. Capillary refill and extremity temperature are late signs of impaired systemic perfusion in the elderly. One useful adjunct, if readily available, is a venous lactate level, which has been shown to be a highly sensitive marker for intensive care unit admission and death. The incidence of abnormal EKG findings increases with advancing age, making the EKG much less specific in the geriatric population. Prolongation of the PR and QT intervals, bundle branch patterns, and intraventricular conduction delays are common. The frequency of nonspecific ST and T wave changes increases as well. The availability and value of recent prior EKG tracings cannot be understated. TRAUMA: RESUSCITATION AND INITIAL EVALUATION Consideration of the geriatric trauma patient differs from that of the younger adult in several respects. The aging body loses mechanical strength and resilience so that musculoskeletal, intracranial, and thoracoabdominal injuries tend to be severer given equal amounts of kinetic energy. Both pre-existing disease and functional changes with age result in decreased ability of the patient to mount an adequate response to stress. Quite often some physiologic event may have triggered the injury (i.e., cardiac or neurologic events may precipitate falls or motor vehicle collisions), which if left undiagnosed could result in serious morbidity or mortality for the patient. The history, primary and secondary surveys, laboratory tests, and additional studies serve not only to diagnose the extent of injury, but to delineate the existence and potential impact of pre-existing conditions, and to ensure that concomitant acute disease processes do not exist. Pre-existing disease and age impact outcome sufficiently that recommendations have been made to triage patients with advanced age or significant medical illnesses directly to trauma centers. When the geriatric trauma patient arrives, the medical team should conduct itself as with any other trauma. Assessment of airway, breathing, and circulation should take into account the factors outlined earlier, with particular attention to airway reflexes and the adequacy and depth of respirations. Elderly victims with multiple injuries are a risk for impaired ventilation and oxygenation. During the secondary survey, attention should be paid to the chest examination. Each rib should be gently palpated for tenderness, and the lungs examined for evidence of congestive heart disease or chronic airway disease. Judicious, early use of pain medications in patients with severe chest wall injury but acceptable ventilation and gas exchange may avoid the development of subsequent pneumonia and respiratory failure. The abdomen should be examined with a high index of suspicion for occult injury. A low threshold for obtaining further studies must be maintained. The addition of thoracic and lumbar radiographs to the standard trauma series should be considered in high-energy injuries, as osteopenia makes fractures of the axial skeleton more common. The frequency of cardiovascular complications is much higher in the elderly (nearly 10%) than in younger patients (about 2%). A baseline EKG should be obtained before transfer out of the ED, and the patient should be assessed for the presence of pre-existing cardiac disease. SUMMARY The elderly represent the fastest-growing segment of the population. As the country ages, the number of elderly patients who present in extremis will undoubtedly increase. Emergency physicians must be cognizant of the fact that age alone is a poor predictor of outcome in the critically ill elderly patient. Premorbid status, including previous level of functioning and pre-existing disease, is more important than chronologic age in predicting outcome, guiding assessment, and deciding on therapy. Knowledge and consideration of the geriatric ABCs includes a fundamental understanding that loss of protective airway reflexes, occult respiratory insufficiency, and clinically unrecognized shock are especially prevalent in the sickest geriatric patients. Early recognition and treatment can minimize morbidity and mortality rates in the ED. Pediatric trauma – differences in pathophysiology, injury patterns and treatment compared to adults Accidents are leading cause of death among children aged 1-14 years in developed countries. Airway and breathing Difference Narrow subglottic area – narrowest at cricoid cartilage Larynx anterior and more cephalad Epiglottis omega shaped and attached to vocal cords at an more acute angle Trachea more complaint Deciduous teeth more loosely attached and easily dislodged Relatively large head to bdy ratio Respiratory gas exchange easily compromised by gastric insufflation (common) in children Management issues Cervical spine control Difference Though rare in children as compared to adults Large head to body ratio SCIWORA – in 67% of children C-spine x-ray interpretation more difficult Circulation Difference Maintain blood pressure until late in clinical course Loss of up to 25% circulatory volume without change in vitals may occur Indices of blood pressure, pulse rate and respiratory rate differ significantly Smaller total blood volume Signs of instability – mottling, hypo-/hyperventilation, erratic vitals, impaired glucose levels Control of airway in ‘sniffing position’ Neck slightly flexed on chest and head slightly extended on neck Occiput raised to level of shoulder with towel under head Over-extension of head on neck will result in obstruction of posterior pharynx Use of uncuffed tubes under age of 8 years Straight blades useful adjunct for lifting epiglottis Short time to desaturation – limited times for intubation Airway size – 4 + age/4 mm Management issues C-spine injury suspected in patients with head injury, ↓ LOC, neck pain Cervical immobilization without traction Traction may worsen ligamentous injury Spinal cord injury not ruled out by normal xrays Management issues Signs of inadequate perfusion and respiratory changes more sensitive markers Sys BP = 80 + (2xage in yrs.) Dias BP = 2/3 sys BP Blood volume = 85ml/kg Fluid boluses weight based – 20ml/kg initial Large scalp lacerations can cause significant compromise by itself due to decreased blood volume Drug dosing according to weight/ Bronslow charts Urine output >1ml/kg in children and >2ml/kg in infants target Thermoregulation Difference Poor hemostatic thermoregulation response Rapid heat loss due to larger BSA in relation to weight Venous access Difference Venous access recognized rate limiting step in resuscitation Management issues Temperature monitored regularly Radiant warmer used when necessary Management issues Shorter time allocation for venous access Early intraosseous access recommended Increased body fat and decreased intravascular volume may compound venous access Injury patterns Head injuries Difference 80% of children die from head injuries in multiple trauma as compared to 50% in adults due to larger head to body ratio compared to adults, less myelination, thinner cranial bones Increased risk of raised ICP Lower incidence of mass lesions 30% vs. 50% in adults More vulnerable to secondary brain injury due to increased risk of hypoxia and ↑ICP Glasgow coma scale guidelines revised according to age Abdominal injuries Difference Blunt trauma more common than penetrating Injuries to solid organ predominate due to flexible rib cage, relatively large organ to cavity ratio, less developed musculature Good results achieved with conservative management of most organ injuries as compared with adults Thoracic injuries Difference Elasticity and resilience of chest wall make fractures of ribs/sternum + flail chest less common Severe parenchymal injuries likely without visible external chest injuries Great mobility of heart and mediastinum make specific injuries more common e.g. transection Tremendous cardiac/pulmonary reserve may obscure signs of cardiac/pulmonary contusions Management issues Prevention of secondary brain injury more critical Early airway control and ventilation to prevent hypoxia/hypercarbia PCO2 – 30-35mmhg target Management issues Most liver/spleen injuries non-operatively managed Early abdominal CT to categorize injuries and direct therapy Management issues Little time for deliberation when hypotension/hypoxemia present Approach to resuscitation similar to adults Early need for airway control and ventilation Traumatic asphyxia occurs exclusively in children due to flexible thorax and absence of valves in SVC/IVC – disorientation, LOC, seizures, cervical/facial cyanosis, subconjunctival hemorrhage, respiratory distress, petechiae Abused child Consider child abuse as potential cause in all cases of traumatic injury Prompt recognition important due to definite tendency for recurrence with increased severity Psychological aspects Fear of doctors, strange faces, parental separation and painful procedures put considerable psychological strain on children – abnormal behavior, abnormal vitals, risk for long term psychologic problems Gentle, non-threatening approach, repeated explanations, parental presence and adequate forewarning of painful procedures.