Health Information Management Technology
advertisement
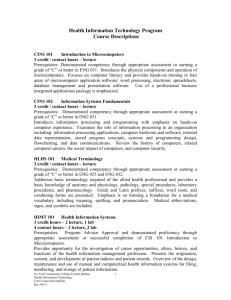
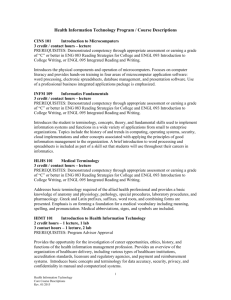
Allied Health Department Health Information Management Technology (HIMT) Program Outcomes Validation Report HIMT Degree Program Medical Coding Certificate Program July 14, 2010 Connie Grossman, M.Ed., RDH Chairperson, Allied Health Department Lisa Cerrato, MS, RHIA Health Information Management Technology Program Coordinator/Professor Jane Roberts, MS, RHIA Health Information Management Technology Professor Table of Contents Executive Summary Section 1: Introduction to the Program Allied Health Department Mission Statement HIMT Program Goals HIMT Program Mission Statement Description of Programs Health Information Management Technology Medical Coding Certificate Program Description of Students Section 2: Review Resources Section 3: Validation of Program Outcomes Section 4: Implications of Results and Specific Plans for Revision of Curriculum and/or Program Outcomes Appendix A – Program Outcomes Validation Survey Appendix B – Graduate Survey Appendix C- F/S Charts 2 Executive Summary The HIMT degree program at Columbus State is accredited by the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM). The accreditation process serves as a means of external validation of our program outcomes and what we teach within the HIMT degree program. In addition to program accreditation, a survey (external measure) was emailed to 24 central Ohio health information managers. Those surveyed work in the following settings: hospitals, mental health facility, cancer registry, student health center, health department, managed care organization, four-year academic HIM program, and a medical review company that audits providers and government agencies. Of the 24 surveys sent electronically, four surveys were returned (16.66% return rate). A review of documents published by our accrediting body (CAHIIM) is performed at least annually when the accreditation report is prepared. This review serves as an internal measure to make sure we are covering material pertaining to the entry-level competencies for HIM professionals. Students who complete the HIMT degree program are eligible to sit for the certification examination for Registered Health Information Technicians (RHIT). Students in the HIMT degree program and the Medical Coding Certificate program may also sit for the certification examination for Certified Coding Associates (CCA). Program outcomes were revised in both the HIMT degree program and the Medical Coding Certificate program. These changes are noted in Section 3: Validation of Program Outcomes. Section 1: Introduction to the Program Allied Health Department Mission Statement The Allied Health Professions Department is committed to providing accessible professional healthcare programs through quality curricula that meet rigorous accreditation standards. These technical programs maintain currency in content and advance as technology does. The programs are offered for students and in collaboration with the support of the clinical community. This community will be provided with graduates that are consistent with those of entry level practitioners in each of the specific disciplines. HIMT Program Goals Provide greater accessibility to the HIMT degree program and the Medical Coding Certificate program by accepting students each quarter. Expand face-to-face tutoring to include more courses within the HIMT. 3 Continue to develop more Virtual Lab assignments for use within the curriculum to decrease our dependence on clinical practicum sites and to make professional practice experiences (PPE) accessible to more students. Continue work with the semester conversion project. HIMT Program Mission Statement To provide up-to-date information that reflects the dynamic nature of the HIM profession and supports learning opportunities and professional practice experiences (PPE) that include didactic education to form the foundational knowledge and skill sets necessary for a career in health information management. Description of Programs The Health Information Management Technology (HIMT) program prepares the student to become a professional responsible for maintaining components of health information systems consistent with the medical, administrative, ethical, legal, accreditation, and regulatory requirements of the health care delivery system. In all types of health care facilities, the health information management technician possesses the technical knowledge and skills necessary to process, maintain, compile, and report health information data for reimbursement, facility planning, marketing, risk management, utilization management, quality assessment and research; to abstract and code clinical data using appropriate classification systems; and to analyze health records according to standards. The health information management technician also may be responsible for functional supervision of the various components of the health information system. Health Information Management Technology Associate Degree COURSE Quarter 1 ENGL 101 BIO 121 CIT 101 HIMT 135 TOTAL CREDIT HOURS Quarter 2 ENGL 102 BIO 122 CIT 102 HIMT 141 CR Beginning Composition Anatomy &Physiology I PC Applications I Health Data Management 3 5 3 5 16 Essay and Research Anatomy &Physiology II PC Applications II Pharmacology and Health Information Management 3 5 3 3 4 HIMT 256 HIMT 267 TOTAL CREDITS HOURS Clinical Data Analysis Principles of Management 3 3 20 Quarter 3 MATH 102 HIMT 133 HIMT 243 HIMT 245 HIMT 257 TOTAL CREDIT HOURS Beginning Algebra I Legal Aspects of Health Information Comparative Health Settings in HIMT ICD-9-CM Coding Introduction to Health Statistics 4 3 3 5 3 18 Quarter 4 COMM 105 COMM 110 COMM 200 HIMT 255 HIMT 292 HIMT 112 TOTAL CREDIT HOURS Speech (or) Conference and Group Discussion Business Communications CPT-4 Coding Practical Applications in HIMT I Electronic Health Concepts Quarter 5 CIT 233 HIMT 113 HIMT 259 HIMT 265 HIMT 275 HIMT 294 TOTAL CREDIT HOURS Expert Access Managed Care Trends Quality and Resource Management Medical Reimbursement Intermediate Coding Practical Applications in HIMT II 3 3 5 4 2 17 3 2 3 3 5 4 20 Quarter 6 SSCI XXX HUM XXX HIMT 270 HIMT 290 HIMT 296 Social Science 100, 101, 102, 105 or GEOG 240 HUM 111, 112, 113, 151, 152 or 224 Case Management in Health Care HIMT Capstone Practical Medical Coding Applications in HIMT 5 5 2 2 4 5 TOTAL CREDIT HOURS TOTAL DEGREE CREDIT HOURS 18 109 Note: BIO 261 Human Anatomy, BIO 262 Human Physiology, and BIO 263 Human Pathophysiology can be taken in place of BIO 121 and BIO 122. The Medical Coding Certificate program prepares students with entry-level skills needed to code, classify, and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval and statistical analysis. Principles in ICD-9-CM coding, CPT coding, and third-party reimbursement will be emphasized. Medical Coding Certificate COURSE Quarter 1 BIO 121 CIT 101 HIMT 135 TOTAL CREDIT HOURS CR Anatomy & Physiology I PC Applications 1 Health Data Management 5 3 5 13 Anatomy & Physiology II Pharmacology and Health Information Management Clinical Data Analysis 5 Quarter 3 HIMT 245 ENGL 101 TOTAL CREDIT HOURS ICD-9-CM Coding Beginning Composition 5 3 8 Quarter 4 HIMT 255 TOTAL CREDIT HOURS CPT-4 Coding 5 5 Managed Care Trends 2 Quarter 2 BIO 122 HIMT 141 HIMT 256 TOTAL CREDIT HOURS Quarter 5 HIMT 113 3 3 11 6 HIMT 265 HIMT 275 TOTAL CREDIT HOURS Medical Reimbursement Intermediate Coding 3 5 10 Quarter 6 HIMT 296 Practical Medical Coding Applications in HIMT TOTAL CREDIT HOURS TOTAL CERTIFICATE CREDIT HOURS 4 4 51 Note: BIO 261 Human Anatomy, BIO 262 Human Physiology, and BIO 263 Human Pathophysiology can be taken in place of BIO 121 and BIO 122. The Health Information Management Technology degree program and the Medical Coding Certificate program are Web-based programs. All technical coursework is offered online except for HIMT 292, HIMT 294, and HIMT 296. Completion of the associate degree in Health Information Management Technology will permit graduates to sit for the Registered Health Information Technician (RHIT) certification examination and the Certified Coding Associate (CCA) examination. Graduates of the HIMT degree program may transfer to The Ohio State University, the University of Cincinnati, or the University of Toledo for a Bachelor of Science degree, majoring in Health Information Management and Systems. Description of Students (2007-2010) Note: This information was obtained from CAHIIM program accreditation reports that are submitted annually and the website from CSCC Knowledge, Resources and Planning. Unduplicated Discipline Enrollment Profile: Approximately 54 students enrolled in the HIMT degree program annually and approximately 23 students enrolled in the Medical Coding Certificate program annually. Approximately 89 students enrolled in PRE-HIMT degree program annually and approximately 19 students enrolled in PREMedical Coding Certificate program annually. Program Related Student Profile: Approximately 40% of our students attend parttime. Number of Degrees Awarded: 32 Number of Certificates Awarded: 27 FTEs – Traditional and Distance Learning: Approximately 78% (traditional); Approximately 50% (distance). Note: HIMT 121 – Advanced Medical Terminology is 7 offered in the classroom as well as on the web and is a high enrollment course for the HIMT. Students from various programs take HIMT 121; thus, the higher percentage of traditional students as compared to web students. Graduate Survey Summary: Conducted annually for CAHIIM program accreditation report. Survey response rate of graduates has been 100% satisfaction. Transfer Data: Approximately 15-20% of degree students continue in four-year HIM programs. Retention Data: Approximately 5% attrition annually. Most of these students leave the program temporarily and eventually return to complete their studies in either the HIMT degree program or the Medical Coding Certificate program. Percent of Distance Learning: All courses are offered via the web with the exception of HIMT 292, 294, and 296. These courses are the hybrid professional practice experience courses that use the AHIMA Virtual Laboratory. Section 2: Review Resources With clinical practicum sites becoming more difficult to obtain each year, The HIMT degree program and the Medical Coding Certificate program have been using the American Health Information Management Association’s (AHIMA) Virtual Laboratory for the past two years to provide students with professional practice experience (PPE). To help bring experiential learning to the HIM academic experience, AHIMA developed the Virtual Laboratory—an Internet-based, practical, participative, HIM and health information technology (HIT) work environment. Students can access and experience state-of-the-art software like the master patient index (MPI), encoders, electronic document management systems (EDMS), transcription and speech recognition, and other applications they’ll regularly use in the working world. Over the past several quarters, we have been experiencing problems with the computers in the HIMT computer lab (UN 528). In extreme cases, it can take up to 30 minutes for the AHIMA Virtual Lab to load. Some students have taken to bringing lap tops to class just to get on a computer in a reasonable amount of time. We have requested to have the PCs in UN 528 replaced since the slow response time of the computers impedes effective us of class time. We have been told by the folks in IT that our computers are currently the oldest computers on campus; we have been informed by IT that roughly 1,000 PCs are slated for replacement this year and that UN 528 will get new PCs this year. On-campus tutoring has been available over the past several years to students enrolled in the HIMT degree program and the Medical Coding Certificate program. Students who have taken advantage of the tutoring have stated that the personal sessions are extremely helpful and that the face-to-face tutoring helps them to feel more “connected” in the web courses. 8 Section 3: Validation of Program Outcomes A survey (external measure) was emailed to 24 central Ohio health information managers. Those surveyed work in the following settings: hospitals, mental health facility, cancer registry, student health center, health department, managed care organization, four-year academic HIM program, and a medical review company that audits providers and government agencies. Of the 24 surveys sent electronically, four surveys were returned (16.66% return rate). The HIMT Community Advisory Committee met on May 7, 2010 to review and approve the changes to the program outcomes for both the HIMT degree program and the Medical Coding Certificate program. The approved outcomes are noted below. Health Information Management Technology Upon completion of the associate degree in the Health Information Management Technology, the graduate will be able to: Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. Comment: This outcome will remain as stated. Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. Comment: This outcome will remain as stated. Maintain and compile health information using electronic applications and work processes. Comment: This outcome was revised. New outcome = Use electronic applications and work processes to manage health information. Apply legal principles, policies, regulations and standards for the control, use, and dissemination of health information. Comment: This outcome will remain as stated. Collect, compute, analyze, interpret and present statistical data related to health care services. Comment: This outcome was revised. New outcome = Apply statistical techniques in support of healthcare administrative, financial, and research activities. Abstract data from patient records for administrative, reimbursement, and research purposes. Comment: This outcome was added. Code, classify, and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval and statistical analysis. Comment: This outcome was revised. New outcome = Apply official coding principles in the assignment of diagnostic and procedural codes for the purpose of healthcare administrative, reimbursement, and research purposes. Review, abstract, retrieve, and compile health data for reimbursement, quality assessment, patient care research, clinical registries and other informational needs. Comment: This outcome was deleted. It is redundant as stated and is captured in other outcomes. 9 Apply principles of supervision and leadership and the tools used to effectively manage human resources. Comment: This outcome was revised. New outcome = Apply supervisory principles in managing human resources. Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA) Code of Ethics. Comment: This outcome will remain as stated. Medical Coding Certificate Upon completion of the Medical Coding Certificate, the student will be able to: Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. Comment: This outcome will remain as stated. Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. Comment: This outcome will remain as stated. Identify components of appropriate and adequate documentation of health care. Comment: This outcome will remain as stated. Abstract data from patient records for reimbursement, quality assessment, patient care research, clinical registries and other identified informational needs. Comment: This outcome was revised. New outcome = Abstract data from patient records for administrative, reimbursement, and research purposes. Code, classify and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval and statistical analysis. Comment: This outcome was revised. New outcome = Apply official coding principles in the assignment of diagnostic and procedural codes for the purpose of healthcare administrative, reimbursement, and research purposes. Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA) Code of Ethics. Abstract data from patient records for reimbursement, quality assessment, patient care research, clinical registries and other identified informational needs. Comment: This outcome will remain as stated. Section 4: Implications of Results and Specific Plans for Revision of Curriculum and/or Program Outcomes The newly revised program outcomes for both the HIMT degree program and the Medical Coding Certificate program will be reflected in the next update of the college catalog. The outcomes validation process helps guide us in what we do enhance the students’ learning experience. The process stimulates conversation which in turn serves to validate that we are teaching what we ought to be teaching. 10 PROGRAM ONE UPDATED AUGUST 2008 2009-2010 CATALOG Upon completion of the Associate of Applied Science Degree in Program Name the graduate will achieve competency in: GENERAL REQUIREMENTS ENGL 101 & ENGL 102 OR ENGL 111 ENGL 200 BASIC REQUIREMENTS COMM 105 OR COMM 110 SSCI 10x HUM 1xx BASIC BASIC BASIC ELECTIVES BASIC BASIC BASIC BASIC BASIC BASIC BASIC BASIC BASIC BASIC Program Outcome 1 Program Outcome 2 Program Outcome 3 Program Outcome 4 Program Outcome 5 Program Outcome 6 Program Outcome 7 GENERAL REQUIREMENTS Upon completion of the Program Name the graduate will achieve compentency in: Critical Thinking Effective Communication Community and Civic Responsibility Quantitative Literacy Scientific and Technlolgical Effectiveness Information Literacy ENGL 101 & ENGL 102 OR ENGL 111 ENGL 200 BASIC REQUIREMENTS COMM 105 OR COMM 110 SSCI 10x HUM 1xx BASIC BASIC BASIC ELECTIVES BASIC BASIC HIMT Degree Program (July 2010) 2010-2011 CATALOG Upon completion of the Associate of Applied Science Degree in HIMT the graduate will achieve competency in: Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. GENERAL REQUIREMENTS ENGL 101 & ENGL 102 OR ENGL 111 BASIC REQUIREMENTS ENGL 200 COMM 105 OR COMM 110 SSCI 10x HUM 1xx BIO 121 CIT 101 F BIO 122 CIT 102 MATH 102 CIT 233 F Use electronic applications and work processes to manage health information. Apply legal principles, policies, regulations and standards for the control, use, and dissemination of health information. Apply statistical techniques in support of healthcare administrative, financial, and research activities. Abstract data from patient records for administrative, reimbursement, and research purposes. Apply official coding principles in the assignment of diagnostic and procedural codes for the purpose of healthcare administrative, reimbursement, and research purposes. Apply supervisory principles in managing human resources. Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA) Code of Ethics. GENERAL REQUIREMENTS Upon completion of the HIMT the graduate will achieve compentency in: Critical Thinking Effective Communication Community and Civic Responsibility Quantitative Literacy Scientific and Technlolgical Effectiveness Information Literacy ENGL 101 & ENGL 102 OR ENGL 111 BASIC REQUIREMENTS ENGL 200 COMM 105 OR COMM 110 SSCI 10x HUM 1xx BIO 121 CIT 101 BIO 122 CIT 102 MATH 102 CIT 233 F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S S F/S F/S F/S F/S F/S F/S F/S F/S F F/S F/S F/S F/S F/S F F F/S F F F F/S F/S F/S F/S F F F/S F F F F/S F/S F/S F/S F/S F/S F/S S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S 12 HIMT Degree Program (July 2010) 2010-2011 CATALOG Upon completion of the Associate of Applied Science Degree in HIMT the graduate will achieve competency in: Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. GENERAL REQUIREMENTS ENGL 101 & ENGL 102 OR ENGL 111 BASIC REQUIREMENTS ENGL 200 COMM 105 OR COMM 110 SSCI 10x HUM 1xx BIO 121 CIT 101 F BIO 122 CIT 102 MATH 102 CIT 233 F Use electronic applications and work processes to manage health information. Apply legal principles, policies, regulations and standards for the control, use, and dissemination of health information. Apply statistical techniques in support of healthcare administrative, financial, and research activities. Abstract data from patient records for administrative, reimbursement, and research purposes. Apply official coding principles in the assignment of diagnostic and procedural codes for the purpose of healthcare administrative, reimbursement, and research purposes. Apply supervisory principles in managing human resources. Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA) Code of Ethics. GENERAL REQUIREMENTS BASIC REQUIREMENTS Upon completion of the HIMT the graduate will achieve compentency in: ENGL 101 & ENGL 102 OR ENGL 111 Critical Thinking F/ S F/S F/S Effective Communication F/ S F/S Community and Civic Responsibility F/ S Quantitative Literacy Scientific and Technlolgical Effectiveness Information Literacy SSCI 10x HUM 1xx BIO 121 CIT 101 BIO 122 CIT 102 MATH 102 CIT 233 F/S F/S F/S F/S F/S F/S F/S F/S F/S S F/S F/S F/S F/S F/S F/S F/S F F/S F/S F/S F/S F/S F F F/S F F F F/S F/S F/S F/S F F F/S F F F F/S F/S F/S F/S F/S F/ S F/S S F/S F/S F/S F/S F/S F/S F/S F/S ENGL 200 COMM 105 OR COMM 110 F/S F/S F/S F/S 13 Medical Coding Certificate Program (July 2010) 2010-2011 CATALOG Upon completion of the Medical Coding Certificate progran the student will achieve competency in: • Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. • Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. Identify components of appropriate and adequate documentation of health care. Abstract data from patient records for administrative, reimbursement, and research purposes. Apply official coding principles in the assignment of diagnostic and procedural codes for the purpose of healthcare administrative, reimbursement, and research purposes. Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA) Code of Ethics. Abstract data from patient records for reimbursement, quality assessment, patient care research, clinical registries and other identified informational needs. TECHNICAL REQUIREMENTS HIM T 135 HIM T 141 HIM T 256 HIM T 245 HIM T 255 F F F/S F/S BASIC AND GENERAL EDUCATION HIM T 113 HIM T 265 HIM T 275 HIM T 296 BI O 12 1 F/S F/S F/S F Critical Thinking Effective Communication Community and Civic Responsibility Quantitative Literacy Scientific and Technlolgical Effectiveness Information Literacy BI O 12 2 EN G 101 F/S F/S F F/S F/S F/S F/S F F/S F/S F/S F/S F/S F/S F S TECHNICAL REQUIREMENTS Upon completion of the Medical Coding Certificate program will be able to: CI T 10 1 BASIC AND GENERAL EDUCATION HIM T 135 HIM T 141 HIM T 256 HIM T 245 HIM T 255 HIM T 113 HIM T 265 HIM T 275 HIM T 296 BI O 12 1 CI T 10 1 BI O 12 2 EN G 101 F F F F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F F F/S F/S F/S F/S F F/S F F F F F F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F/S F F/S F/S F/S F/S 14 Health Information Management Technology Columbus State Community College Health Information Management Technology (Associate Degree) Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Maintain and compile health information using electronic applications and work processes. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ 15 Apply legal principles, policies, regulations, and standards for the control, use, and dissemination of health information. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Collect, compute, analyze, interpret, and present statistical data related to health care services. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Code, classify, and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval, and statistical analysis. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Review, abstract, retrieve, and compile health data for reimbursement, quality assessment, patient care research, clinical registers, and other informational needs. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ 16 Apply principles of supervision and leadership and the tools used to effectively manage human resources. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA Code of Ethics). ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ 17 MEDICAL CODING SPECIALIST CERTIFICATE PROGRAM Demonstrate knowledge of human anatomy, physiology, and pathophysiology, medical terminology, pharmacology and clinical data as it relates to the collection and use of health information. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Review health records for completeness and accuracy to determine appropriateness and adequacy of health care documentation. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Identify components of appropriate and adequate documentation of health care. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Code, classify, and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval and statistical analysis. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ 18 Abstract data from patient records for reimbursement, quality assessment, patient care research, clinical registries and other identified informational needs. ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Demonstrate ethical practices as outlined in the American Health Information Management Association (AHIMA Code of Ethics). ______Outcomes should remain as written. ______Delete outcome. No longer applicable. ______Not appropriate for me to evaluate this outcome. ______Revise outcome. (Refer to comments below.) Comments: _____________________________________________ _____________________________________________ _____________________________________________ Name __________________________________________ (Optional) _________________________________________ Job Title: _________________________________________ __________________________________________ Facility: __________________________________________ __________________________________________ Address: __________________________________________ __________________________________________ __________________________________________ Phone: __________________________________________ Fax: _________________________________________ Email: _________________________________________ Thank you for your time and input! 19 GRADUATE SURVEY Health Information Management Academic Program: City/State: This survey is designed to help the HIM program faculty determine the strengths and areas for improvement for our program. All data will be kept confidential and will be used for program evaluation purposes only. Please check () the category or categories that reflect(s) your status at the time of this survey: Employed (Circle either) Full-time OR Part-time Attending College toward another degree (Circle either) Full-time OR Part-time Other (please explain): INSTRUCTIONS: Consider each item separately and rate each item independently of all others. Circle the rating that indicates the extent to which you agree with each statement. Please do not skip any rating. If you do not know about a particular area, please circle N/A. 5 = Strongly Agree 4 = Generally Agree N/A = Not Applicable 3 = Neutral (acceptable) 2 = Generally Disagree 1 = Strongly Disagree A. KNOWLEDGE BASE (Cognitive Domain) THE PROGRAM: 1. Helped me acquire the knowledge necessary to function in my current job. 2. Prepared me to use sound judgment while functioning in my current job. 5 4 3 2 1 5 4 3 2 1 N/A 5 4 3 2 1 N/A N/A 3. Prepared me to be able to recommend appropriate procedures relevant to my job. 4. Enabled me to think critically, solve problems, and develop appropriate action steps. Comments: 20 B. PROFESSIONAL PRACTICE (CLINICAL) PROFICIENCY (Psychomotor Domain) THE PROGRAM: 1. Prepared me with the skills to perform as an HIM professional. 5 4 3 2 1 5 4 3 2 1 N/A 5 4 3 2 1 N/A 5 4 3 2 1 N/A N/A 2. My professional practice experiences were valuable in reinforcing my HIM skills. Comments: C. BEHAVIORAL SKILLS (Affective Domain) THE PROGRAM: 1. Prepared me to communicate effectively within my work setting. 2. Prepared me to conduct myself in an ethical and professional manner. 3. 4. Taught me to manage my time efficiently while functioning in my current job. 5 4 3 2 1 N/A Prepared me to work effectively as a team member. 5 4 3 2 1 N/A 5 4 3 2 1 Comments: D. OVERALL RATING: 1. Please rate and comment on the OVERALL quality of your preparation as an HIM professional. N/A Comments: 21 E. GENERAL INFORMATION (Check yes or no, or respond to the question in the space provided) 1. I have actively pursued attaining my RHIT or RHIA credential. YES NO 2. I am a member of AHIMA. YES NO . Comments: 3. Based on your work experience, please identify two or three strengths of the HIM program? 4. Based on your work experience, please make two or three suggestions to further strengthen the HIM program? 5. What qualities/skills were expected of you upon employment that was not included in the program? 6. Please provide comments and suggestions that would help to better prepare future graduates. BACKGROUND INFORMATION: Job Title: Employer: Name of Graduate: Today’s Date: Please return this questionnaire to the accredited program. Thank you for your responses 22