Home Sleep Testing AAST 2009
advertisement

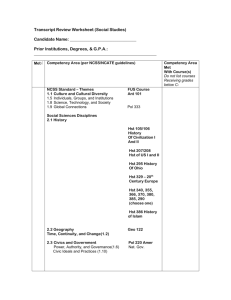
Home Study Focus Group – AAST Meeting June 2008 Michael Salemi, RPSGT I. Attendees will gain a comprehensive knowledge of the current technologies used in HST testing A. New Technologies 1. Pressure Transducers 2. RIP – respiratory inductive plethysmography a) “A plethysmograph is an instrument for measuring changes in volume within an organ or whole body (usually resulting from fluctuations in the amount of blood or air it contains)” Wikipedia b) Measures cross sectional area across the full circumference of the Thorax and Abdomen c) Most uses of RIP are “non calibrated” d) Calibrated RIP provides a SUM channel that can be used an alternative flow measure 3. PAT - peripheral arterial tonometry a) “make[s] use of autonomous nervous system changes which accompany disordered breathing during sleep. The peripheral arterial tonometry (PAT) determines the peripheral arterial vascular tone using a plethysmographic method on the finger”. b) IEMBS apos;04. 26th Annual International Conference of the IEEE Volume 2, Issue , 1-5 Sept. 2004 Page(s): 3856 - 3859 4. PTT – Pulse Transit Time a) PTT is the time taken by the arterial pressure wave to travel from the aortic valve to the periphery and is recorded as the time delay between the ECG R-wave and the arrival of the corresponding pulse wave at the finger. b) Smith et al. Thorax 1999;54:452-457 II. Attendees will learn ways to integrate HST into their diagnostic testing programs A. Historical: 1. Marvin Sackner & William Gruen a) 2. Respitrace Ancoli-Israel S, et al, J Gerontol. 1985 Jul;40(4):419-25 Laughton Miles a) Vitalog - Gyulay S, Sleep. 1987 Apr;10(2):130-42. b) Auto CPAP – (1991) Miles LE Sleep Research 1996; 25: 514. 3. Dan Cohen a) 4. Poly-G (1982) Ruggles K, et al Sleep Research 1986; 25: 526 Harley Shear - German Nino-Murcia a) TeleDiagnostics Vista (1987) III. Attendees will discuss the various uses of home testing as defended in AASM practice parameters as well as anecdotal uses of sleep testing organizations throughout the country. A. B. C. D. E. AASM Overview 1. Must be performed under the auspices of an AASM accredited comprehensive sleep medicine program 2. Only in conjunction with a comprehensive sleep evaluation by a board certified sleep specialist 3. Only for patients with a high probability of moderate to severe OSA 4. Not for patients with co-morbidities, other sleep disorders or for screening a) CHF b) COPD c) Hypoventilation Realities on The Street 1. Home studies are performed by many entities 2. Dentists 3. DME / HST Affiliates 4. National Organizations 5. Traditional Sleep Labs CCSD’s Protocol 1. Performing HST for >10 years 2. Screen out BMI >39 & <30 3. Screen out Co-morbidities 4. Screen in Pt’s with high probability of OSA 5. Witnessed Apnea 6. EDS 7. Loud Snoring 8. Neck >16” Preparing for the Future 1. Start a HST program in your lab 2. If you don’t someone else will! 3. Educate your community on the pro’s and con’s of HST 4. Make sure you are seen as the sleep experts in your community 5. Educate yourselves 6. Understand the technologies, costs, benefits in your communities What Do the Data Say? 1. Most “Pro” studies have been sponsored by the device mfg’s 2. 3. 4. 5. 6. 7. 8. 9. 10. Most “Con” studies have been conducted in traditional labs settings Extrapolating data across HST platforms is often difficult a) CMS Decision Memo CAG-00093R2 MedCAC expressed “There is no Gold Standard” a) Medicare Evidence Dev. and Coverage Advisory Committee 3-18-08 b) Clinical eval with PSG: strong moderate to high c) Clinical eval with Type 2 HST: strong moderate d) Clinical eval with Type 3 HST: moderate e) Clinical eval with Type 4 HST: less than moderate f) Clinical evaluation alone: less than moderate Arguments Pro a) Lower cost to patient and healthcare system b) More rapid expansion of testing capabilities c) More convenient for patients d) Addresses tech shortages and limited PSG beds Arguments Con a) Higher repeat rate than PSG b) Sensitive but not Specific c) finds frank OSA d) high # false negatives e) Patients still require in-lab titration f) High risk of user error (1) Chervin et al. Ann Intern Med.1999; 130: 496-505 Sensitivity and Specificity a) Bar et al. Chest 2003;123;695-703 n = 99 Patient Preference of HST a) Neill et al, Wellington School of Medicine and Health Sciences, (unpublished) (1) N = 30 (2) 50% preferred home PSG, (3) 27% preferred the Laboratory environment (4) 23% had no preference. (5) Preferred Home (a) Not having to travel (46%) (b) Sleeping in their own bed (80%). (6) Preferred laboratory (a) Presence of trained staff (25%) (b) No family distractions (63%). The most uncomfortable sensor was the nasal cannula in both groups Patient Preference of HST a) Lloberes et al. Eur Respir J 18 (3): 530. (1) N = 35 (2) 53% preferred home (3) 28% in hospital (4) 19% showed no preference IV. Attendees will discuss the various methodologies using Auto-titrating PAP devices to compliment their diagnostic testing programs A. O.Marrone et al. Sleep Medicine, Volume 5, Issue 3, Pages 247-251 1. Preference between Auto vs Fixed CPAP 2. N = 22 3. Four preferred fixed CPAP 4. Four expressed no preference 5. Fourteen preferred autoCPAP. B. Nolan et al. Sleep. 2007 Feb 1;30(2):189-94 1. APAP vs Fixed CPAP a) No differences in polysomnographic variables or ESS b) Mean APAP pressure levels were significantly lower than CPAP (6.3 +/1.4 vs 8.1 +/- 1.7 cm H2O, p < .001). c) Pt compliance was similar with both treatments d) Pt’s requiring higher fixed pressure (> or = 8cm H2O) preferred APAP e) Pt’s requiring lower pressure (< 8 cm H2O) preferred CPAP C. All things being equal – how do you… 1. Deal with mask leakage? 2. Change masks during the study? 3. Deal with pt anxiety? 4. Titrate to arousals? D. In CMS commentary period - Only 32 of 680 expressed an interest in the trial use of CPAP without a sleep study test. V. Attendees will discuss the current regulations from CMS regarding HST and its use to qualify patients for OSA therapy A. B. Reimbursement 1. CMS NDC 240-4 Effective August 2008 2. Most private carriers have paid for HST for years 3. CMS drafts and approves National Coverage Determinations – NDC 4. CMS outsources to Medicare Administrative Contractors (MAC’s) that focus on four areas: a) Customer service b) Operational excellence c) Innovation and technology d) Financial management Local Coverage Determinations 1. A/B Mac’s approve Dx reimbursement 2. D-Mac’s approve Tx reimbursement 3. DMAC LCD takes precedent C. CMS National Coverage Determination 1. CMS NCD 240.4 Effective 8-4-08 a) The AHI and/or RDI may be measured by polysomnography (PSG) in a facility-based sleep study laboratory, or b) Type II (HST) monitor, a Type III HST monitor, or c) Type IV HST monitor measuring at least 3 channels. (1) “For the purposes of this NCD, a respiratory disturbance is defined in the context of the sleep test technology of interest and does not require direct measurement of airflow. (2) Local contractors will, as needed, determine, based on their review of the published, peer-reviewed medical literature, the equivalent test result criteria corresponding to the required AHI or RDI for Type IV devices measuring 3 or more channels that do not measure AHI or RDI directly”. D. A/B MAC 1. Pays for Diagnostic & MD Services 2. Trailblazers - Texas a) G0398: Home Sleep Testing, Type II portable monitor; minimum 7 channels - $150.00 - $100 is recognized for the Professional Component - $50 is recognized for the Technical Component b) G0399: Home Sleep Testing, Type III portable monitor; minimum 4 channels - $125.00 - $85 is recognized for the Professional Component - $35 is recognized for the Technical Component G0400: Home Sleep Testing, Type IV portable monitor; minimum 3 channels $100.00 - $70 is recognized for the Professional Component - $30 is recognized for the Technical Component 3. Performance of home sleep testing is limited to FDA cleared devices 4. Adequate patient instruction and support to assure successful completion of the studies. 5. Can be provided by accredited sleep centers as well as Independent Diagnostic Testing Facilities and other entities that can demonstrate use of FDA approved devices, inspection of the devices, and the patient support activities required. E. The DMAC (Durable Medical Equipment Administrative Contractors) are responsible for providing coverage guidance on CPAP devices. 1. Determines if your patent gets therapy 2. Noridian LCD 9-18-08 a) Type II device – Monitors and records a minimum of seven (7) channels: EEG, EOG, EMG, ECG/heart rate, airflow, respiratory movement/effort and oxygen saturation; or, b) Type III device – Monitors and records a minimum of four (4) channels: respiratory movement/effort, airflow, ECG/heart rate and oxygen saturation; or, c) Type IV device – Monitors and records a minimum of three (3) channels that allow direct calculation of an AHI or RDI as defined above. (1) Devices that record channels that do not allow direct calculation of an AHI or RDI may be considered as acceptable alternatives if there is substantive clinical evidence in the published peer-reviewed medical literature that demonstrates that the results accurately and reliably correspond to an AHI or RDI. This determination will be made on a device by device basis. (2) Currently there is no device that indirectly measures AHI or RDI that meets this criterion. 3. November 1, 2008, all beneficiaries who undergo an HST must, receive instruction on how to properly apply a portable sleep monitoring device. a) Instruction must be provided by the entity conducting the HST and may not be performed by DME b) Patient instruction may be accomplished by either: (1) Face-to-face demonstration of the portable sleep monitoring device’s application and use; or, (2) Video or telephonic instruction, with 24 hour availability of qualified personnel to answer questions or troubleshoot issues with the device. c) To qualify for PAP on or after November 1, 2008, all HSTs must be interp’ed by a physician who holds either: (1) American Board of Sleep Medicine (ABSM); or, (2) Sleep Board from American Board of Medical Specialties (ABMS); or (3) Completed residency or fellowship training by an ABMS member board and has completed all the requirements for subspecialty certification in sleep medicine except the examination itself and only until the time of reporting of the first examination for which the physician is eligible; or (4) Active staff membership of a sleep center accredited by the American Academy of Sleep Medicine (AASM) or The Joint Commission – JCAHO 4. Same will apply for PSG’s after January 2010 5. No aspect of an HST, including but not limited to delivery and/or pickup of the device, may be performed by a DME supplier. a) This prohibition does not extend to the results of studies conducted by hospitals certified to do such tests.