Diagnostic Imaging - Logan Class of December 2013
advertisement

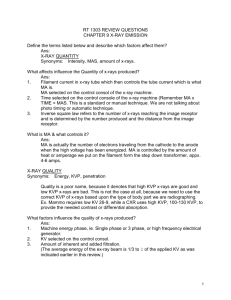
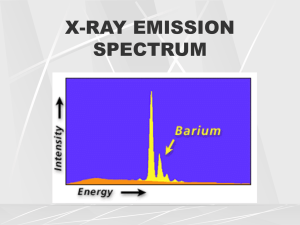
Diagnostic Imaging 9-11-02 Who gets x-rayed? Those who need it; show clinical indications – a crooked spine isn’t necessarily a clinical indication. The risks are small to cause cancer with ionizing radiation. X-rays are good at showing advanced tumors, infections, big fractures, dislocated bones and joints. Since the bones are not the same in all people, viewing subluxations on x-ray isn’t necessarily important – i.e. asymmetrical C-1 TP, bent spinous, etc. Our profession has a problem with poor quality x-rays due to low volume. Medicare says, as a doctor, we can’t send patients to a separate facility that we have any interest in. It would be smarter to go in with a few other Drs and keep the x-ray technician busy all day. It also keeps the machine in better working order. Chiropractors get sued for misdiagnosis on x-rays due to film quality and the fact that DCs aren’t radiologists – misdiagnosis is usually cancer. We reviewed atomic theory. Atom is the smallest unit of an element, central nucleus with protons (+), neutrons (no charge), almost equal in number, surrounded by electrons. Bohr’s atomic model. Lose an electron, becomes +, it is therefore ionized. This happens in the tube and inside the patient during the time of exposure. A molecule – two or more atoms bound together by electrostatic and electromagnetic forces. It is the simplest structural unit that displays the characteristic physical and chemical properties of a compound. X-ray can create radicals that are electron scavengers. Electron binding energy – the work required to remove an atomic electron to an infinitely remote position from its orbit. The strength of attachment of an electron to the nucleus. Tungsten – Wolfrum was the original name, hence “W” on the periodic scale. Used in diagnostic x-rays. Gamma rays are stronger and more damaging. The x-rays necessary to do a mammogram are molybdenum (lower energy). Computer over-reads are picking up about 10% more cancer cases than the 80-90% found on mammograms. Fingers and toes (KVP 50-150) – photons from Tungsten is used. Radioactivity is never involved in x-rays. Radioactivity – some atoms contain excess energy. These atoms are excited with an unstable nucleus. To become stable the nucleus spontaneously emits particles and energy. This doesn’t happen in x-rays. Once the “beep” in the x-ray room happens, it’s OK to step from behind the barrier – this is about the speed of light (186,000 miles/second). Radioactive – Uranium and Plutonium – have half-lives. Bones scans are radioactive – within 24 hours it’s gone – has short half-life. Types of ionizing radiation - Particulate (alpha and beta particles) – electromagnetic (x-rays and gamma rays). Most of this can come from the sun. People live at altitude get about 600 mR’s (milli Roentgens) per year compared to 300 mR on the coast. X-ray does about 15 mR per P->A x-ray. ALARA (as low as reasonably achievable) – government policy – they feel you are more at risk if you live at higher levels. Alpha particles – basal cell carcinoma – can’t penetrate a piece of paper. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 1 of 16 Beta particles – can penetrate paper but not a thin piece of aluminum. Gamma rays – can get through paper and aluminum but can’t get through concrete. Government doesn’t care if the shield is lead, it just has to be effective, i.e. a 2-foot thick concrete wall would do it. Shielding depends on the circumstance (where our office is located, i.e. basement, third floor, etc.) Images.gsfc.nasa.gov/ems/waves3.html – website that the following information came off of. “Waves in the electromagnetic spectrum vary in size from very long radio waves the size of buildings to very short gamma rays smaller than the size of the nucleus of an atom. Did you know that electromagnetic waves can not only by described by their wavelength, but also by their energy and frequency? All three of these things are related to each other mathematically. This means that it is correct to talk about the energy of an X-ray or the wavelength of a microwave or the frequency of a radio wave.” All the waves have wavelength and frequency. “Photons” are referred to in he visible light to gamma rays – wavelengths used to refer to those below visible light. Roentgen, Wilhelm Conrad, Germany, 1895, discovered x-ray by accident. Diagnostic Imaging 9-12-02 Roentgen – discovered properties of x-ray by accident using a cathode ray tube. Others 10-12 years before had done it but didn’t appreciate what they had. His wife had to sit for 20 minutes to get the exposure done. X-ray Properties No appreciable mass No electrical charge Travels at the speed of light (or not at all) – even after they collide (except photoelectron x-ray) Can penetrate most matter (especially big metallic atoms – it has to be thick or like lead – a big molecule) Travel in a straight line until they interact with matter – then they can scatter (Lead can be dangerous but it has to be touched at lot over a long period of time) **Capable of making certain chemical compounds fluoresce **Capable of exposing photographic film **Can change biologic matter by ionization – changes in DNA, water in the body, etc. = damage Ca++ Tungstate – screen materials used in fluoroscopy (light from the screen produces the image – not the x-rays) – Edison discovered fluoresens worked best. CaW (Calcium Tungstate) was the best out of 2000 compounds they experimented with. Edison’s company became General Electric. Originally, x-rays were done on a screen and were moving – they were used to look at the heart, the GI system, any movement. In 1973, 3M discovered rare earth materials were 2 x more efficient than the CaW. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 2 of 16 MDs, like cardiac surgeons, like to watch their surgery on fluoroscopy. This can cause burns on the patient’s back and the tissue doesn’t regenerate (this is 5-10 minutes of exposure) Fluoroscopy of the spine is done in addition to normal x-ray so the patient gets a higher dose of radiation (fluoroscopy is twice the dose of the plain x-ray dose) Art Croft – whiplash researcher – It took 2 minutes of x-ray beam to do the full set of cervical motion studies. He copied them and sent them to ten radiologists - there was less than 50% agreement in what was happening - the interpretations were not consistent. Radiation is either electromagnetic or particulate. Alpha and beta particles are particulate; x-ray and gamma ray are electromagnetic. A short wavelength and high frequency I what gives x-rays the ability to penetrate material (60 kVp for gamma rays) X-Ray Production Electron-target interaction X-ray emission specrum Factors affecting x-ray emission He showed a picture of what is inside the tube housing – The tube housing is lined with lead. Inside is a glass tube – a fancy “light bulb” – a diode ($5,000 per light bulb) and it is vacuum-sealed. This is in a mineral oil bath that serves as a heat sink to dissipate the heat and offer electromagnetic protection. Older x-ray equipment used PCB oil – very dangerous – causes bone resorption of the distal phalanges. Lots of heat is produced where the x-rays come out of the tube – the heat is transferred down the anode to the oil. The useful portion of the x-ray beam comes out through a portion of the glass that is thinner so as to not impede the x-rays. A round wheel of tungsten (not pure) with a beveled edge (specific degree is 14) on the anode is a feature to look for when purchasing an x-ray machine. Electron-target interaction - mA controls electrical current to filament on cathode (cathode block) - prep button spins rotor and sends electricity to filament (rotating anode effectively increases the area the electrons bombard by a factor of 2*Pi*radius over a stationary anode (gives us cooler metal to work with – anode spins as long as you hold down the prep button) - resistance causes filament to heat up - electrons are “boiled off” filament (thermionic emission) @ 2000 degrees C. We use Tungsten because it has the highest melting point we know. - Space charge effect – tendency to limit more electron from escaping filament Filament and anode are made of Tungsten READ BOOK – this is where the mid-term and final questions come from. - - exposure switch is depressed (while you are holding the prep button) kVp is applied across the cathode/anode (90 kilivolts = kVp, 220 volts goes through transformer and steps up the voltage to 90,000 volts) – cathode becomes negative 90,000 volts and the anode becomes positive 90,000 volts. This changes depending on what you set on the controls – it can vary. The cathode pushes electrons away and the anode attracts them. (1/2 to ¾ inch space between the cathode and anode – the electrons travels and roughly ½ the speed of light) electrons are accelerated from cathode to anode “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 3 of 16 - - projectile electrons collide with anode 1 Ampere = 1 Coulomb/second = 6.3 x 10(18) electrons/second. At 100 mA it is 6.3 x 10 (17) electrons/second. In a .1 second exposure you would get 6.3 x 10 (16) electrons/second. Only about 1% of the electrons actually make the x-rays. line focus principle Diagnostic Imaging 9-18-02 Line Focus Principle Uses an angled (beveled) surface to disperse the heat, but a very effective focal spot. X-rays are produced (about 1%) and the rest of the electrons produce heat. Only about 5% of the 1% actually make the x-rays. The focal spot controls the clarity of the image. (Check out Figure 2-5 for display of where x-rays go) Anode heat: The majority of energy used (99%) results in heat Outer shell electrons of target material (Tungsten on anode wheel) are temporarily excited As they fall back into orbit they release energy as infrared radiation (heat) Heat is directly related to mAs and kVp (you set both of these) 100 mA @ 1 second @ 80 kv = 8000 HU (heat units) Heat units are calculated by multiplying kVp by mAs (single phase only. Multiply kVp x mAs by 1.41 for HF – high frequency) Figure 2-6 compares single phase to HF. Book says 1.35 (or something) – the new figure is 1.41 (efficiency factor) for HU in a single exposure. “Seasoning” procedure – a way of warming up the x-ray machine (anode) to keep it from cracking after being cold (air conditioning on all weekend). The new machines have safety switches so you can’t do an x-ray that will damage the anode. Page 35 has a figure (2-7) showing how long you need to wait in between shots to keep from overheating and maxing out the heat capacity of the anode. Full Spine x-rays take more heat capacity. Normal heat capacity is 150,000. It will cost about $800 more to get it jacked up to 400,000 to do the full spine x-ray. Anode Heel Effect – Page 36 in the book – Figure 2-8. Cathode side – 4 degrees = 103%, 8 degrees = 104%, 12 degrees = 105%; after 12 degrees it falls off again. On the anode side from the central ray – 4 degrees = 95%, 8 degrees = 85%, 12 degrees = 73%. The skinny part of the person should be on the anode side and the thicker part on the cathode side. Intensity variation is 32%. If the focal film distance (FFD) is longer, it minimizes these effects. Intensity of the beam is non-uniform in the long axis of the tube If the central ray = 100%, intensity progressively decreases toward the anode and increases then decreases toward the cathode Variation in intensity is approximately 30% (17” film @ 40” FFD) – Figure 2-8 Decreased at longer FFD Small vs. Large Focal Spot – the smaller the space he sharper the image. Large focal spot is less detailed. The central portion of the object on the film is called “umbra” and pen-umbra is the edges of the object. The large focal spot is used for those patients who will possibly move during the taking of the film (metally challenged, babies, patients with a tick, etc.) Second Hour “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 4 of 16 He went thru how we need to process film. He said we would go over it again in lab tomorrow. The class will be split into two groups for first hour and second hour – only come to the lab you are assigned – the other hour is independent study. Large focal point – 2mm x 2mm, Small focal point – 1 mm x 1mm Fractional focal point 1.5 and .6 (for large and small focal points). X-ray Production: Three things happen: Heat (already discussed) Bremsstrahlung radiation (every x-ray) Characteristic radiation (part of the time) Characteristic Radiation The radiation produced is characteristic for the anode material (Tungsten for x-ray, Molybdinum for mammograms) Depended on electron binding energies for the target material (69.6 keV for Tungsten – needs this amount of energy or more to remove the electrons) (kVp has to be greater than keV to produce an image) Projectile electron ionizes a K shell electron (comes from kVp that we dial set) (This is an inner shell electron) Electrons from higher orbits fill the “hole” – this creates the “photon” – if it drops in from an “L” shell, there isn’t much characteristic radiation – it has to come from the most outer shells The change in electron binding energies results in photons with that keV value. Bremsstrahlung Radiation Braking (slowing, decelerating) radiation Projectile electron (negative charge) comes under influence of the nucleus (electric Coulomb force) Projectile electron changes direction, variably – depends on the degree of deflection all the way up to the peak that we set (kVp) Change in direction causes Bremsstrahlung x-ray photon production (conservation of momentum) Bremsstrahlung – three electrons enter at different distances from the nucleus. Three photons exit at different directions, different wavelengths – Medical College of Wisconsin Alternating Electric Current – 1/120 second it’s up and 1/120 second it is down. US, Canada, Mexico are all on 110, Australia is on 220, Japan is on 330. See canned notes for pictures. A full sine wave cycle is 1/60 of a second – 60 Hertz (60 Hz). Top 30% of top sine wave is useful for x-ray. Rectified Waveform – see canned notes for picture. The electricity is “transformed” to 70,000 volts – the ripple factor – the variation in the peak x-ray energy during the exposure (in this example it is 100%). The peaks can be 60,000-100,000 volts when stepped up. Three Phase Electrical Waveform – see canned notes – the waves overlap. Ripple factor is 10% from peak to valley. 6kHz Medium Frequency Electrical Waveform (Figure 2-12) – three phase waves on single phase electricity. There is a calibration spike (1st spike) – delivers the ripple factor of 10%. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 5 of 16 100 kHz high Frequency Electrical Waveform (Fig 2-12) – controls the electricity across the tube to produce the ripple factor of about 1%. Driven by single phase electricity. Ripple Factor – Single Phase – 100% - least efficient producer of x-rays Three phase – 10% Medium frequency – 10% High Frequency – 1% - most efficient Graph of an unfiltered beam – canned notes for picture Spike on 1st picture is the characteristic x-ray spike – it has to have a kVp of 70 for a Tungsten xray. Everything under the curve except what is under the spike is Bremssrahlung radiation. An aluminum shield is in the equipment to absorb this radiation. This is the filter. Picture #2 – filter has been added – very few x-ray photons on either end of the scale. Low energy on left, and peak energy on right. Diagnostic Imaging 9-19-02 mAs = mA x time Changes in mA (quantity of photons, small changes make small changes on film) and kV (quality creates contrast – punch power – changes are much more evident) Decrease in kV – short scale – increase in contrast Increase in kV – long scale – decrease in contrast Diagnostic Imaging 9-25-02 For there to be a significant change in the density of the film there needs to be at least a 15% change in MAS (TIME) for each exposure. A 15% change in kVp shows significant change also (density is the average darkness of the whole film) – up makes it darker, down makes it lighter. (Foot – in jacket labeled time) A 50% reduction in MAS (time) makes it much lighter and a 50% increase in time (MAS) makes it much darker. We have to think in terms of percentages not actual time. KVp – 80 kVp and 12 MAS – a difference of 1 kVp isn’t going to make a big difference in the density. It takes at least a 4% change in kVp to see a density difference. It took a 50% reduction in MAS to do the same thing that a 15% reduction in kVp did. (Thoracic spine – in jacket labeled KV) MA – this is harder due to the way x-ray machines are wired. All the pictures were taken at the same time and the same kVp but the MA changed. 150 to 75 (50% reduction) and 150 to 200 (33% increase) – these are a lousy way to control the density of the film – the changes are too big – it’s better to control the density with time rather than the MA. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 6 of 16 Tomorrow in lab we will change 2 of the factors – the 15% rule – if kVp goes up 15% then MAS has to go down 50%, if it goes down 15% the MAS has to increase 100%. We will be looking at contrast rather than density. Graphs in the notes – all the area under the graph are the amount of photons produced – it creates the density. The net effect is to shift everything straight up (doubling the MA). KVp changes – graph the peak of the lower energy Bremsstrahlung photons shifts up and to the right – there’s more of them and they are stronger when the kVp is increased. Government requires that the manufacturers have an aluminum filter in the beam – to decrease the radiation dose add more aluminum between the tube and the ??? – the peak shifts to the right. Photon energy – 1 @ 10, 1 @ 8, etc. down to 2 = average energy is 6. With the thicker aluminum it flters out anything below 6, the average increases to 8 (do the math 10 + 8 + 6 = 24 /3 = 8) High frequency – mR = milliRoentgens per MAS - see graph in notes – single phase versus high frequency. Shorter times means fewer repeats of films due to the motion of the patient. High frequency = lower exposure times. Understand the principle (don’t have to do the figures) X-ray quantity The number of x-ray photons in an exposure beam. May be expressed and “quantity = output intensity = radiation exposure Measured in roentgens (R) or milliroentgens (mR) International community uses gray (Gy) and sievert (Sv) Gray is patient dose Sievert in occupational exposure (one gray to the patient is the same as one sievert to you) In diagnostic radiology 1 rad (patient exposure) radiation absorbed dose = 1 rem (occupational) radiation equivalent for man = 1 roentgen (exposure in air) The final measure is in terms of mR/mAs 70 kVp there is usually 3-6 mR/mAs Factors affecting x-ray quantity (area under the graph) mAs – quantity is directly proportional kVp – 15% rule (not directly proportional to mAs changes an increase in kVp by 15% must be balanced by a 50% reduction in mAs conversely a decrease in kVp by 15% must be balanced by a doubling of the mAs the result, in either case, are two films of equivalent average density but a change in contrast (difference in white and black on the film) – high contrast is black and white, low contrast is black and gray. Distance – inverse square law To maintain the density of the film, if the FFD (focal film distance) is increased 100% (e.g. 40” to 80”) you need to quadruple the mAs (to get the same darkening effect) Conversely, if you cut the FFD by 50% (e.g. 80” to 40”) you would need one fourth the mAs. If you increase the distance by 50% (e.g. 40” to 60”) you would double the mAs. (We are trying to maintain the number of photons per square inch) *****NEED TO KNOW THIS PROCESS***** I(1)/I(2) = (d2/d1)2 This was originally figured out with light “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 7 of 16 I1 = Intensity 1 D= distance Assume a technique at 40” produced an exposure dose of 300 mR. What would the exposure dose by if the tube was moved to 72” WITHOUT CHANGING the kVp or mAs? I1 = 300 mR (40”/72”)2 I1 = 300 mR (.56) 2 I1 = 300 mR (.31) I1 = 93 mR 93 x 3.25 (the amount in between 60 and 80, 40 to 60 = 2, 40 to 80 = 4, 40 to 72 = 3.25, the proportion of the dose). If the kVp or mAs isn’t changed but the distance is, the film will be lighter Assume a technique at 72” produced an exposure dose of 300 mR. What would the exposure dose be if the tube was moved to 40” WITHOUT CHANGING the kVp or mAs? It gets darker. I1 = 300 mR (72/40) 2 What about tube tilts? Do I need to adjust the tube’s position when using a 15 degree tube tilt at 40”? This AP lower cervical technique requires an exposure dose of 15 mR for a proper exposure. (1” for every 5 degrees) I1 = 15mR (40/43)2 I1 = 15 mR (0.93)2 I1 = 15 mR (0.87) I1 = 13 mR 14% decrease – this isn’t going to make any difference – anything above 15 degrees tube tilt will make a difference, otherwise is won’t. X-RAY QUALITY – power of the penetrating beam – kVp Refers to the penetrating power of the beam Hard vs. soft x-rays Hard x-rays have higher kV values Soft x-rays have lower kV values Measured by half value layer (HVL) The thickness of an absorbing material necessary to reduce the intensity to ½ of its original value. Factors affecting quality (of beam and hence the image) KVp (adequate to penetrate the body part) Filtration – types of filtration Inherent – what comes with the tube Added – gets rid of Brumsstralung radiation, improves quality of film, this is what the Government requires be added to Compensating – Nolan filters, clear light filters, filters part of the beam. If you stay within 15% of what Supertech recommends and you’ll be OK as far as kVp is concerned. Less contrast – ¼ sec, 300 MA, 75 MAS, 90 kVp is normal – if the patient has Parkinson’s you need to take the film faster. Go from 90 to 104-108 kVp – time goes to 1/8 second, lower MAS, it will have less contrast but a sharper image because there won’t be as much movement. Smaller focal spot = lower MA and longer time. We use 300 MA because it is a good balance between focal spot and contrast FIVE BASIC INTERACTIONS – only two are important “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 8 of 16 Classic scattering – not important to what we do Aka coherent or Thompson scattering; between low energy x-ray photon and an atom; photon changes direction without loss of energy; no ionization; most scatter forward; may contribute to film fogging Compton effect – WE NEED TO KNOW THIS – has to do with grids (this is our biggest problem) Between moderate energy x-ray photons and an outer shell electron Photon changes direction, loses energy, ionizes atom creating a Compton electron (creates damage) Scattered photon may ionize another atom (happens during the exposure – stops when the exposure stops) May cause backscatter (180 degrees) Adds to film fog (we use grids to protect from this) Increases with increasing kVp Arthur Holly Compton – general information, Born September 10, 1892; Nobel Laureate, Physics 1927; Director of Metalurgic Lab, Manhattan Project 19421945; Chancellor Washington University 1945-1953; Died of a heart attack March 15, 1962 (not radiation exposure) – not on test. Photoelectric effect – WE NEED TO KNOW THIS Between moderate energy x-ray photons and an inner shell electron Photon loses all of its energy, ionizes the atom creating a photoelectron Produces characteristic x-rays (secondary radiation) in the object being x-rayed Secondary x-rays behave like scattered x-rays (isotropic) – they go everywhere Pair production Occurs with x-ray energies >1.02 Mega electron volts (million electron votls – way above what we do) Photon intereacts with nuclear force field – emits a positron and an electron Photodisintegration Occurs with x-ray energies > 10 Mev Photon absorbed by the nucleus itself Nuvcleus then emits a nuclear fragment Diagnostic Imaging 10-02-02 We looked at images taken last week – changing kVp 15% and mAs – same density but penetrating power is different (causes a cange in contrast) Whiter = lower kVp; Grayer = higher kVp Increase kVp (15%) and cut mAs in half – decrease kVp 15% and increase mAs by 2. Here are 3 films – according to the 15% rule, which one taken with the lowest kVp? The one with the whitest whites? Choice of kVp settings – 50, 60, 70? Which one (of the three films) was taken with the lowest kVp according to the 15% rule? Contrast = kVp (inversely proportional), Density + mAs (double mAs, double kVp, makes it blacker, directly proportional). “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 9 of 16 DIFFERENTIAL ABSORPTION Compton scattered x-rays contribute no useful information (it’s bad) Adds radiographic density, results in film fog (hides detail – higher kVp – as kVp goes up there is more Compton scatter) Structures that absorb a great amount of x-ray are radiopaque (photoelectric interaction – the whitest things you see on the x-ray) – big atoms that the photons run into and give up all their energy Structures that allow x-rays to pass through are radiolucent (like air) The main difference is the atomic number of the structure (atomic number – protons + neutrons) – metals (like lead) are big atomic numbers and absorb the photons – photoelectric Generally less than 5% of x-rays that hit the patient reach the film. Less than half of those interact with the film to form an image. Therefore approximately 1% of the x-rays emitted from the tube (This info not on the test) Maximal differential absorption results from lower kVp values (photons either pass through the person, have Compton effects or photoelectric effects) But as kVp is lowered patient dose increases (high contrast – patient dose increases – lower energy photons – mAs has to increase) At lower energies (kVp) the percentage of photoelectric interactions increases (relative to Compton) – around 40kVp there is a crossover – TEST INFO********below 40 kVp the predominant x-ray photon interaction with matter is photoelectric (i.e. 60% photoelectric, 40% Compton). At 40 kVp it is 50-50. Above 40 kVp Compton is predominant (makes the whites less white – a layer of fog on top of the image) We use grids to deal with this. (80 kVp = 85% Compton, 15% photoelectric – he doesn’t know if these numbers are absolutely accurate but they are close and are being used as examples. 70 kVp = 83% Compton and 17% photoelectric) To image small differences in soft tissue (renal stone) use low kVp technique (for maximal differential absorption) – the smallest kidney stone can cause extreme pain – very difficult to see if it is the size of a grain of sand. You can “see” four things radiograpically:: Air – black – optical density is 4.0 (1 in 10,000 photons get through to the film) Fat – lighter color (dark shade of gray) – fascial planes Water – represented by muscle, blood vessels, etc. Metal – whitest things we see – i.e. fillings – optical density is .25 or so (it’s real low) The interaction of x-rays and tissue is directly proportional to the density (specific gravity) of the tissue (anything that has a large specific gravity will be whiter) Attenuation is the reduction in the number of x-rays as they penetrate matter. X-rays are attenuated exponentially. (only applies through a solid material – starts out with 10,000 photons into the first layer of the solid material, 100 in the second layer, 10 in the 3 rd layer, 1 in the fourth layer) “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 10 of 16 GRIDS Used where we x-ray bigger body parts (>12 cm******KNOW THIS) – most necks, average knee – anything bigger needs a grid Screens alone cannot adequately improve film contrast Selective filtration between the patient and film is ineffective Invented by Dr. Gustave Bucky, 1913 (picket fence like stuff done with lead – horizontal and vertical lead strips – improved quality of film but lines of the grid got in the way of fine pathologies. Hollis Potter improved the grid by removing the horizontal grids and said that moving the vertical grids during the exposure would obscure them and still provide the absorption of the Compton photons) (moving buckys cost about $500 – there are other options – stationary grids are better) Principle Function – Improve Film contrast Grids are made of: 1. Grid material, usually lead 2. Interspace material, may be plastic, aluminum, or fiber (usually aluminum) Note – fiber is hydroscopic resulting in uneven density on the resulting films and may cause the grip to warp Grid material is approximately 50 microns thick separated by interspace material approximately 350 microns thick Some primary beam will be eliminated by the grid material Grids remove between 80-95% of scatter emanating from the patient (Non-grid holders are about $200 – reduces radiation by about 1/3 – allow for this in our room drawings) See drawings in notes re: Primary Beam, Scatter, Interspace Material, Grid Material GRID RATIO The height of the strip divided by the interspace thickness Ratios vary from 6:1to 16:1 In General practice 12:1 is most desirable NOTE – the higher the grid ratio the greater the patient dose (the more it costs) The reason to use a grid is to improve film contrast – not radiation related The number of lead lines per unit measure (e.g. 85 lpi or 103 lpi – lines per inch aka lines per centimeteres – lpc) 85 lpi is designed to move – 103 or more are designed to be stationary Moving grids require fewer lines per inch Stationary grids must have the lines very close together so the lines become imperceptible on the resulting film “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 11 of 16 Picture of grid label – “Tube Side” should be facing the tube so the grid lines are oriented properly. Gives “per inch” information and the ratio (i.e. 12:1), focal range. TYPES OF GRIDS Linear or Parallel – designed to move Focused Crossed – eliminates tube tilts – one linear on top of the other turned 90 degrees GRID RECOMMENDATIONS: 12:1 (Dr. G likes a 10:1 ratio) 103 lead lines per inch Focused range from 40-72 inches Aluminum interspaced Appropriate size (physically) 18” x 18” if you will only perform sectional films 18” x 36” if you will perform scoliosis radiography PROBLEMS Grid cutoff Off level – grid pickoff Off center Off focus – Dr.s problem – move back further than focused for Upside down AIR GAP TECHNIQUE The part is intentionally or necessarily separated from the film Results in an increased object-film distance (shoulder gets in the way when you are trying to get a picture of the neck) This allows scatter to physically miss the receiver Scatter that does intercept the film is attenuated by the inverse square law. This method works best with kVp settings below 90 Due to the direction of the scatter produced To offset the magnification created by the increased OFD (Object film distance) a longer focal-film distance is used Air does not appreciably filter the beam BEAM RESTRICTING DEVICES (Collumnation) Two types of photons interact with the film to form image: those which don’t interact and Compton scatter x-rays Remnant x-rays – photons that exit patient and interact with the film ( what’s left after the beam has interacted with the patient) Collimation reduces patient dose by: Limiting the volume of tissue irradiated Secondarily reducing the amount of scatter (also reduces fogging) Failure to collimate is the greatest contributor to needless patient exposure ********KNOW THIS – Medicare laws says that it has to be collimated on three sides Diagnostic Imaging 10-9-02 “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 12 of 16 Anode heel effect from last week – Dr. G did the corrections – needed to check the view box for the optical density first and then adjust the tube (tilt and distance) for a proper effect. At 36” it is about 28 degrees divergence, perpendicular there is no anode heel effect, and at 72” it is about 12 degrees divergence. Inverse square log – 72” proper exposure (same kVp and mAs, same body part, etc.) it looks good, but at 40” it’s too dark. Then a 40” proper exposure (Shortest focal film distance – measure from edge of body to edge of body, the larger one is the 40”) – mAs was different than the 72”. Then did a 40” proper exposure, and then moved to 72” – the 72” was much lighter FFD (focal film distance) takes 3.24 times more mAs at a longer distance. Air, fat, water and metal density x-ray – very subtle in water and fat. Moving objects – spin top tool – designed to check the accuracy of timer exposures. Single phase – 120 “McDonald’s Arches” per second – each cycle is represented at one dot. A manual spin top timer is useless for a continuous output machine. He talk about arcs – I missed it. A synchronous timer – the length of the arc makes a difference – length of the arc compared to the time. LOOK AT THE X-RAYS – besides the x-rays, there will be Supertech questions (part A and B), anode, cathode, parts and pieces will all be on the test next week. BEAM RESTRICTING DEVICES Two types of photons intereact with the film to form image: those which don’t interact and CompTom scatter x-rays. (Last time?) Factors affecting scatter radiation: As kVp increases the relative number of Compton interactions increases. In general high (optimal) kVp technique is preferred to low kVp technique is preferred to low kVp technique due to patient dose considerations. Field size – as the area of the beam enlarges, scatter increases. Seen more on small film sizes. Film size 14X17 13X16 Area 238 208 % Reduction 13% 8X10 80 7X9 63 21% (i.e. a spot film – watch technique – it will change - the smaller it is the lighter it will be – mAs needs to increase 20-25% to maintain density) Patient thickness – the thicker the part the more scatter. Patient thickness is under your control. Deciding to perform lumber spine and abdominal films in the recumbent versus upright positions If you decide to use patient compression – (contraindication – elderly white male, smoker with history of inguinal hernia – aortic aneurysm waiting to happen) CONTROL OF SCATTER RADIATION Use beam restriction and grids Beam restriction: “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 13 of 16 Aperture diaphragm Cones or cylinders Variable aperture collimator Aperture diaphragms are generally not suitable for general practice Cones are used primarily by dentists General practice requires variable aperture collimator Variable aperture collimators (positive beam limitation) – can’t use a beam that is larger than the film. (Automatic collimation – comes to film size – can be made smaller but can’t be made bigger). We, as DCs, aren’t required by law to use the PBL, the automation isn’t necessary – as long as we collimate, this will continue – it saves us money. Off-focus radiation may be reduced by a first stage entrance shuttering device (picture of filament and electrons) – contributes about 25% of patient’s dose – shows images outside the primary beam (i.e. open mouth – get the ears in the film) Second stage collimator shutter leaves are made of lead (at least 3 mm thick), work in pairs, independently, yielding square or rectangular fields which compliment the film size being sued. Light localized by lamp and mirror Place rheostat on x-ray room lights Collimator bulbs are expensive, handle with tissue when installing or their life will be shortened and crack. (Re-align properly – can be very tricky – easier to have a professional come and do it) Lights must coincide with the x-ray beam. If your equipment is properly installed and maintained the resulting film will show evidence of FOUR SIDES of collimation Collimator adds about 1 mm of Aluminum filtration equivalent VIDEO TAPE – Kodak – how film came to be – tape was done in the 1960s. Interesting but didn’t need to take notes on it. INTENSIFYING SCREENS Screen Construction Protective coating Phosphor Layer Reflective layer Base Protective coating Closest to film Minimizes damage to screens from handling and dirt Reduces static electricity Phosphor Converts x-ray photon energy to light Formerly, calcium tungstate (Edison) Currently, rare earth mixtures – 3M discovered they are even better, produce twice as much light when exposed to the same amount of radiation. Screen phosphors should have: 1. a high atomic number 2. high conversion efficiency 3. light matched to film used 4. minimal afterglow Rare earth materials used for intensifying screens include: 1. gadolinium 2. lanthanum “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 14 of 16 3. yttrium (1 & 2 – proportions of each of these determines green or blue film) Reflective layer Light is produced isotropically Takes light produced y screen moving away from the film and directs it toward the film Increases the speed of the screen by doubling the number of photons reaching the film (All this decreases patient dosage) Base Provides mechanical support for phosphor layer Luminescence Light produced by the screen X-ray photon temporarily elevates an outer shell electron from its orbit This adds energy to the electron When the electron falls back into orbit the exvess energy is released in the form of light The wavelength of light produced is specific for the phosphor material Screens provide approximately 95% of the film’s exposure RADIOGRAPHIC FILM Emulsion is primarily silver halide crystals in gelatin (AgBr and AgI) May be coated on one or both sides of the film (called a duplitized film, one side is single emulsion film) – the image is superimposed on both sides of the film – gives us a sharper picture with duplitized. Mammography uses single emulsion, more detail. Emulsion speed is a function of grain diameter or surface area Flat (tabular grains) offer a larger cross section with more light gathering capability than conventional grains (KODAK T-Mat-G = t = tabular, G = half speed film (H is full speed)) Tabular grains are more tolerant t developer activity (more forgiving) Use the film that is spectrally matched to the light from the screen (don’t mix blue screen with green film, etc. – you have to use more radiation to get the same darkening effect) Rare earth screens manufactured by: Kodak give off green light (Lanex Fast – THIS ONE WE NEED TO KNOW FOR THE TEST) – we use Lanex Fine for extremity films For Kodak – use T-Mat-G or T-Mat-H (G film + Lanex Fast = 600 speed, H film + Lanex Fast = 1200 speed) – G is half speed, H is full speed CHAPTER 5 - Typical H & D Curve (Hurter and Driffield – they discovered this in the late 1800’s regarding photographic film) Optical density of 0 = perfectly clear, all light intensity is transmitted to the other side, Optical density of 4 = one photon in 10,000 gets through. “Step numbers” are gradiations of light exposure on the film. PAGE 87, 88-89 show graded steps – captions on the pictures are fair game for test material. (21 steps). Step #1 – no light exposure (blue dye adds a base density so #1 isn’t at –0- density = this is base + fog) Each increasing step is a doubling of the exposure – the “toe” area doesn’t darken very fast, then it goes fast until you get so dark that it levels off, Steps 18-21. KNOW THIS FROM THE BOOK!!!!!! Chart that compares TMG and TMH film – shows that at 1.25 optical density it would require 2X as much radiation to do an H film compared to a G film. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 15 of 16 TEST – CHAPTERS – Chapter 1, 2, 3, 5 – READ – even if he didn’t cover it in class, we are responsible for it for the test. Diagnostic Imaging 10-10-02 Turn on the machine, turn out the room lights, take your measurement with the direction of the central ray – be skin on skin – watch for curves i.e. the lordosis – don’t measure from the table up, just from their back up. Otherwise the film will be too dark. 80 kVp – 12.5 mAs, less radiation than 71 kVp at 15 mAs (which is the default the machine was set at). 300 mA - .04 for exposure time (100 mA we would use for a small focal point but some equipment allows a choice between large and small. For table x-ray – use 14X17 film, tall in the holder, flash where it won’t block the anatomy that you are trying to shoot, marker L or R, gray side up. When setting distance, set it on “cassette” – not “table” because the film is in the cassette, not lying on the table. Move the table and set it in the middle – tilt the tube toward both ends to make sure the light is in the middle. Collimate and center the cassette with the center ray. If you collimate from a 13 x 16 down to a 5 x 5 you will need to increase the mAs 15% for equal optical density. Medicare requires that you collimate a minimum of 3 sides. “Linda’s Notes” by Linda Hite – These notes are not guaranteed to be complete or without errors – they are meant to be a supplement to help you study. Page 16 of 16