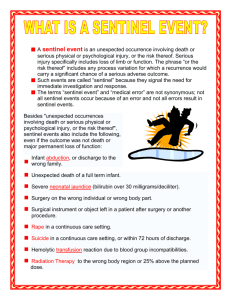
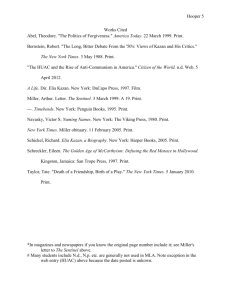
DHB summary of serious and sentinel events final
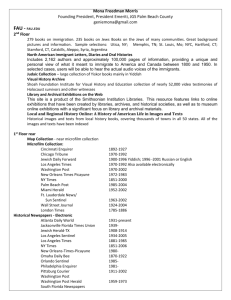
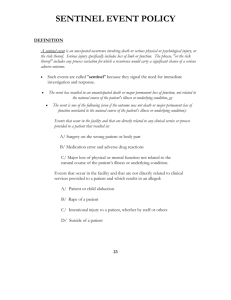
advertisement

DHB Summary of Serious and Sentinel Events Report 2009/10 Published in November 2010 by the Health Quality &Safety Commission Wellington, New Zealand This document is available on the Health Quality & Safety Commission website www.hqsc.govt.nz Northland District Health Board Codes used to classify events 1 2 3 4 Wrong patient, site or procedure Suicide of an inpatient Retained instruments or swabs Clinical management problem Plus sub-code: A B C D E F G 5 6 7 8 9 10 11 12 Diagnosis (including delayed and misdiagnosis) Treatment (including delayed and inadequate) Monitoring/observations (not performed and/or actioned) Procedure associated incident or complication Investigation (delayed, not ordered or actioned) Discharge and transfer Other Medication error Falls Blood transfusion reaction AWOL patient Physical assault on patient Delays in transfer Other Hospital acquired infection DHB Summary of Serious and Sentinel Event Report 2009/10 1 Northland District Health Board Northland Serious or sentinel Serious Event code 4B, 12 Description of event Review findings Recommendations/actions Follow-up Hospital acquired infection Infection caused possibly by infected luer site and inadequate pain control or femoral line exacerbating critical condition Unrecognised E-coli urinary infection Lab results not followed up in timely fashion for both urine sample and blood cultures Pain relief changed immediately prior to transfer, ineffective – resulting in delirium Documentation did not identify clinical risks and management plans, staff focused on crisis at hand Visual; record of luer sites to be included in intensive care unit (ICU) recording sheet Medical staff to review transfer form Protocols to be written regarding pain relief management prior to ward transfer Protocol to be written regarding investigation and identification of the delirious patient Review of patient controlled analgesia (PCA) guidelines Transfer sheet reviewed Patient controlled analgesia (PCA) guidelines reviewed Others in progress Serious 4C Unrecognised deterioration in patient, delaying treatment Prolonged period of instability Early warning score (EWS) process not followed – scores absent, incorrect Case review Education/training on EWS Escalation of medical contact if necessary Continue to progress with EWS identification and staff training Serious 5 Medication error – 10x the dose of insulin given, patient unresponsive – requiring emergency resuscitation Unclear prescribing of all medications Acute medical patient on surgical ward Education of staff in use of insulin and ranges of blood sugars Review of locality of high-need medical patients during overflow Staff educational sessions undertaken with nursing staff Serious 4B/C Failure to recognise excess digoxin given -patient transferred to CCU Patient transferred from regional hospital to base – same high dose medication continued, given twice in one day Full review under way DHB Summary of Serious and Sentinel Event Report 2009/10 2 Waitemata District Health Board Waitemata Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Serious 4C Delayed recognition of deteriorating condition Severe pneumonia. Delay in action on EWS once deteriorated Handover and referral to senior medical staff delayed Transferred to intensive care unit (ICU). Recovered following prolonged care and rehabilitation Staff assessment and response education reinforced using case review Clinical communication processes reviewed with the team Sentinel 4C Delayed recognition of deteriorating condition Significant tissue infection on admission Deteriorated over 16 hours with muscle damage and organ failure Condition critical and died despite treatment Staff assessment and response education reinforced using case review On-call clinical communication processes reviewed Serious 6 Inpatient fall resulting in dislocation of hip requiring surgery Recovering from elective revision of total hip joint replacement and slipped in shower Lowered to floor by assistant but hip dislocated Required re-operation Discharged after rehabilitation Manual handling education for junior staff Implement falls minimisation project initiatives Sentinel 4B Unexpected death following day surgery repair of large hernia Underwent day surgical repair of large hernia After discharge the next day, collapsed at home and died Found to have bowel obstruction as a postoperative complication Recognised potential complication discussed at case review Multidisciplinary pre-op clinic established to review patient health prior to surgery and plan discharge Increased emphases on discharge information for families on actions if unwell following discharge Serious 6 Inpatient fall resulting in head injury Under assessment in emergency department (ED). Climbed off end of trolley and hit head Small traumatic frontal and bilateral subarachnoid haemorrhage and overlying subdural haemorrhage identified Remained in hospital for monitoring and treatment. Discharged home Close monitoring of confused patients on narrow ED trolleys. Trolley kept in low position Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 3 Waitemata District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Serious 6 Inpatient fall resulting in fracture of ribs Under assessment in ED. Fell off trolley as cot side not in place Fractured six ribs Remained in hospital due to pain, breathing and treatment of internal bleeding. Long rehabilitation. Discharged home Close monitoring of elderly patients on narrow ED trolleys. Trolley kept in low position with cot sides up Sentinel 2 Suicide – inpatient Patient under observation but not actively suicidal Suicide completed Clinical emergency treatment unsuccessful Close observation procedures reviewed Review of environment undertaken to reduce chance of self harm Sentinel 6 Inpatient fall resulting in fracture of hip requiring surgery Fall unwitnessed while on ward Underwent surgery Delayed discharge due to prolonged rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Implement falls minimisation project initiatives Serious 6 Inpatient fall resulting in fracture of arm requiring surgery Fall unwitnessed on ward resulting in fracture of arm Delayed discharge after prolonged rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Implement falls minimisation project initiatives Serious 6 Inpatient fall resulting in fracture of hip requiring surgery Fall unwitnessed on ward resulting in fracture of femur Patient having difficulty with walker Discharged after prolonged rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Implement falls minimisation project initiatives Serious 6 Inpatient fall resulting in fracture of hip requiring surgery Fall unwitnessed on the ward resulting in fracture of femur requiring surgery Patient frail and unsteady due to previous surgery and was deconditioned due to long bed rest Discharged after prolonged rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Half-hourly rounding at night Implement falls minimisation project initiatives Serious 4G Shoulder injury during stroke patient transfer Patient with dense stroke had manual transfer rather than using sling hoist transfer as specified by physiotherapist Resulted in severe damage to left shoulder requiring intensive physiotherapy Stroke unit opened for dedicated team care Staff re-education on manual handling using hoists Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 4 Waitemata District Health Board Serious or sentinel Event code* (see codes below) Serious 5 Serious 4C Serious Description of event Review findings Recommendations/actions Medication administered not appropriate to need Woman experienced a haemorrhage after delivery Carboprost medication was administered intravenously resulting in cardiovascular emergency Recovered after treatment and monitoring Lead maternity carers (LMCs) and obstetricians reminded that carboprost only used in exceptional circumstances Clinical guidelines reviewed Delayed recognition of deteriorating condition Patient receiving treatment for severe acute inflammatory muscle disease Deteriorated over some hours Delay in action on EWS once deteriorated Required ICU treatment Recovered after rehabilitation Staff assessment and response education reinforced using case review 5 Medication error resulted in cardiac arrest Short acting cardiac medication changed to higher dose but slow release medication Administered more short acting rather than slow release Developed significant slow heart rhythm and low blood pressure Responded to emergency treatment Increase staff education on medication risks Increase clinical pharmacy monitoring and alerts in Pyxis system Serious 6 Inpatient fall resulting in fracture of hip requiring surgery Recovering from surgery for right neck of femur fracture Fell and required surgery to repair right neck of femur fracture Patient frail and unsteady due to previous surgery and rehabilitation Discharged after rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Implement falls minimisation project initiatives Serious 6 Inpatient fall resulting in prolonged hospitalisation fracture of neck vertebrae Unwitnessed fall and complained of sore neck Managed conservatively Discharged after rehabilitation Junior staff required to supervise mobilisation of frail elderly patients in unfamiliar environment Implement falls minimisation project initiatives Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 5 Auckland District Health Board Auckland Serious or sentinel Serious Serious Event code* (see codes below) Description of event 4A/C Neonatal seizures possibly as a result of undetected low oxygen levels at delivery Monitoring in labour difficult to interpret Provide education on low oxygen brain injury Long term outcome uncertain Lack of clear guidance regarding confirmatory diagnostic tests Specific guidelines for foetal scalp blood tests Incomplete handover Update handover and transfer documentation Adoption policy not followed Social work triage of new referrals Failure of social work triage, risk identification and alert processes Education of staff regarding social work alerts Completed Communication failures Update adoption policy Completed 11 Sentinel 4A/B/C Sentinel 4D Serious 5 Unauthorised removal of baby from hospital Review findings Recommendations/actions Follow-up All completed Established Delayed diagnosis and treatment of fatal meningococcal septicaemia Initial emphasis on viral rather than bacterial infection No re-review when triage time exceeded Insufficient vital sign recordings delayed aggressive treatment Air entered fluid tubing during brain X-ray, leading to a stroke Flush fluid ran out Use 1000 ml bag 1000 ml bags in use Manual systems to check the bag Investigate high pressure infusion pumps Infusion pumps being assessed Responsibility for checking fluid level not assigned Change site of infusion bags to more visible position Completed Bag not clearly visible to staff members Bag check responsibility of circulating nurse Completed No after-hours specialist advice on complex substance use Establish access to senior on-call advice Consultation strategy with alcohol and drug service Prescription unclear Assess competencies and provide training and support for practice improvement Medication competency assessment developed Baseline physical assessment not completed on admission Staff development in physical assessment Medical specialist nurse appointed Respiratory arrest due to excess prescribed sedative in combination with self administered methadone No long term harm DHB Summary of Serious and Sentinel Event Report 2009/10 6 Auckland District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Sentinel 2 Suicide after absconding from inpatient mental health unit Ran away from staff while on an escorted break outside the building Preventability uncertain Suicide risk not fully identified May have been improved by more culturally directed approach and advanced risk assessment Further development of cultural competent services Training in advanced risk assessment Serious 4A/B Delay in escalation of treatment for patient with respiratory deterioration Required ICU admission but no long term harm Emergency escalation process not followed Poor communication between staff members Further training on priority of medical emergency call system Strategies to improve handover and documentation Serious 11 Serious 4A/B Serious 1 Serious 4C/D Follow-up Implementation in progress Postoperative surgical patient Past history of suicide risk unknown to attempted suicide ward staff No long term harm Post-operative delirium inadequately treated “Watch” requirements unclear Delirium/psychosis clinical guideline Completed but yet to be disseminated Review of watch instructions every shift change Not yet implemented Delay in diagnosis and treatment of heart attack in a young woman, possibly worsening severity of heart damage Locum doctors failed to identify diagnostic heart tracing Competency for roles not confirmed Supervision inadequate More specific assessment and documentation competency for locums Incorrect sperm used for donor insemination Unused sperm container not discarded from centrifuge End of shift discard of all samples No pregnancy resulted Labelling not recognised as incorrect Two staff to check all stages of sperm preparation Grossly inadequate ventilation of an ICU patient during MRI scan Ventilator circuit incorrectly assembled in MRI room Dedicated MRI ventilator circuits to be set up in ICU prior to transfer Subsequent death was unrelated Significance of breathing monitor data not appreciated Add specific monitoring section to MRI training Implemented Implemented DHB Summary of Serious and Sentinel Event Report 2009/10 7 Auckland District Health Board Serious or sentinel Sentinel Event code* (see codes below) Description of event 4B/D Death following cardiac injury during dialysis catheter extraction Review findings Recommendations/actions Follow-up Inadequate multidisciplinary planning External review of service Completed No check of roles/risks/back-up prior to commencing Multidisciplinary forum for complex case planning In process No appropriate physical equipment/ facility available Extend “safety checklist” concept to interventional radiology In progress Business case for additional equipment In process Serious 3 Retained surgical swab after complex 14-hour procedure not identified until following day despite incorrect swab count being notified Swab not identified on initial postoperative X-ray in intensive care X-rays to be taken in operating room Operating surgeons to review any X-rays required for retained surgical items Serious 3 Retained surgical swab not identified for 5 days after operation Swab count was reported as being correct at the time of surgery Interruptions and distractions during the count processes Poor communication between the team members regarding the swabs placed inside the patient Sentinel 11 Mother accidentally fell asleep (in parent room) with baby causing fatal suffocation Bed/chair arrangements Limited opportunities for parental education No signs in room regarding safe sleeping practice Dedicated breastfeeding chairs Review parental information package Add “safe sleeping” signs All completed Serious 4A Delayed diagnosis of intra abdominal bleeding in woman on anticoagulant post caesarean section Initial misdiagnosis confounded by poor handover Introduction of clinical midwife advisor role Completed Early post-operative anticoagulation may not have been indicated Review guidelines/teaching for perioperative anticoagulation In draft Serious 5 Severe anaphylactic reaction to antibiotic with previously documented allergy No long term harm Recent admissions had not documented the allergies noted earlier No allergy alerts for patients in the electronic record Revise clinical alert system for patient allergies Long term project linking with national system Sentinel 1 Patient incorrectly received cardiac biopsy in addition to his scheduled procedure with serious complications Patient subsequently died Informal cardiac biopsy referral process Add cardiac biopsy to current referral form Completed Incorrect patient sticker for referral Review cardiology referral, consent and patient identification processes In process Inadequate patient information and consent process Consider electronic referral system Awaiting DHB-wide process DHB Summary of Serious and Sentinel Event Report 2009/10 8 Auckland District Health Board Serious or sentinel Event code* (see codes below) Description of event Sentinel 4E Delayed in follow-up of investigations of complications of pregnancy Foetal death before specialist appointment Sentinel 2 Suicide of community patient with daily visits Serious 4D Sentinel 4A/B Sentinel 4B Serious Serious Serious Oral medication given via intravenous line instead of via stomach/bowel tube No long term harm Review findings Recommendations/actions Referred non-urgently to clinic rather than hospital admission, possibly as a result of lack of role clarity Follow-up N/A Intravenous syringe used as bowel tube had intravenous connector Clear labelling of tubes Labelling process implemented Misunderstanding at nursing handover Implement comprehensive enteral tube medication system Partially implemented Improve access to previous care plans System in place Still under review N/A Pressure ulcer leading to multiple complications, eventually fatal High risk of pressure areas scored appropriately, but institution of preventative measures was delayed Delay in response to low blood pressure Treatment ineffective, patient died Preventability of death uncertain Emergency escalation process not followed 6 Inpatient fall causing fractured neck of femur requiring surgery Unwitnessed fall Non-English speaking patient 6 Inpatient fall causing fractured neck of femur requiring surgery Initial risk factors identified but an unwitnessed fall the previous day had not led to a documented change in mobility status Staff training Completed Falls risk assessment in every patient’s file Implemented Inpatient fall causing fractured right hip requiring surgery Witnessed fall Risk falls assessment within first 24 hours of admission Patient cognitive and behavioural factors Standardise abbreviations in clinical record Poor documentation and handover of risk factors Review scoring of falls risk assessment 6 Develop physiotherapy handover sheet DHB Summary of Serious and Sentinel Event Report 2009/10 9 Auckland District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Serious 6 Inpatient fall causing dislocated hip replacement requiring surgery Unwitnessed fall while walking to the bathroom Patient behavioural and cognitive factors Poor English – patient’s third language Documentation standards not met Review of documentation, care map and terminology review, handover sheet for physiotherapy, comprehensive nursing assessment that include falls assessment Serious 6 Inpatient fall causing fractured neck of femur requiring surgery Patient instructed to ring bell for assistance as required; however patient chose to toilet independently Nil Serious 6 Inpatient fall causing fractured neck of femur requiring surgery Nursing assessment did not incorporate all needs and requirements No formal physiotherapy handover sheet Improve documentation between allied health and nursing Ward to purchase cordless phone Serious 6 Inpatient fall causing fractured wrist requiring reduction and cast Patient mobilised to toilet unattended Serious 6 Inpatient fall causing fractured hip requiring surgery Confused patient on peritoneal dialysis accidentally dislodged tubing; slipped on wet floor A “watch” was used the previous evening but had been discontinued Serious 6 Inpatient fall causing fractured wrist requiring reduction and cast Patient tried to mobilise independently Follow-up Nil DHB Summary of Serious and Sentinel Event Report 2009/10 10 Counties Manukau District Health Board Counties Manukau Serious or sentinel Event code* (see codes below) Description of event Review findings Sentinel 4A Delay in receiving ultrasound scan contributed to delayed management of a complex problem and subsequent patient death No process in radiology to communicate possible delays for planned ultrasounds Lack of clarity between primary and secondary care re clinical responsibility for patient’s care Develop service specific process to track diagnostic requests Standardise outpatient clinic letters so that responsibility for patient care is clearly outlined In progress Sentinel 4B Delay in surgery due to lost follow up appointment at laser eye clinic leading to poor clinical outcome. Failure in referral processes in Ophthalmology. Ophthalmology to review: All laser overdue appointments Planned appointment process, Referral management, Scheduling based on priority, Appointment booking processes. Review of all outpatient processes in progress Serious 4D Nerve damage causing loss of use of arm following large excision to remove skin cancer Rare complication Consent process not explicit about potential risks associated with this surgery Consent processes to be reviewed to ensure risks associated with procedures are clearly outlined In progress Serious 4D Cotton fibres found under synthetic eye lenses requiring re-operation in three patients Two sources of fibres found: Cotton drying cloths used in sterile services unit (SSU) instead of usual air drying process Immediate cessation of using cotton cloths in drying process Develop guideline for processing ophthalmology instruments Develop intraoperative checks to inspect instruments prior to use Inform manufacturers Report to Medsafe New process for processing ophthalmology instruments meets best practice guidelines New rigid containers trialled and purchased for storage and processing of ophthalmology instruments Intraoperative checks have been included in the newly printed cataract pack Powerful magnifying glass has been installed in SSU for examination of fine ophthalmology instruments prior to packaging Medsafe incident report completed Product fault: fibres were found in cataract eye packs and also on the introducing cartridge from manufacturer that places the lens in the eye No documented procedure for the handling and processing of fine ophthalmology instruments Recommendations/actions Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 11 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4D Chest drain insertion contributed to collapse and sudden death in patient with severe lung disease Lack of senior medical officer (SMO) supervision of a high risk procedure done after hours in a severely compromised patient Lack of clear criteria for when chest drains should be inserted under image guidance Follow 2010 British Thoracic Society (BTS) guideline that states: Plueral procedures should not take place out of hours except in an emergency It is strongly recommended that all chest drains for fluid should be inserted under image guidance Completed Serious 4D Obstetric haemorrhage precipitated by forceps delivery requiring hysterectomy Lack of credentialing process for resident medical officers (RMOs) performing forceps deliveries Lack of awareness of massive transfusion protocol Establish formal credentialing process for registrars Alert the department to the massive transfusion protocol Completed Serious 4D Burns to buttock and perineum due to scalding from hot water Epidural for difficult labour Sensation had not returned to normal; patient placed in hot water bath to aid passing urine There is no guideline in place for the post natal care of a patient who has had an epidural during labour – this meant an unrecognised and unsafe procedure was used Communication to all DHB midwives and LMCs to stop procedure immediately Alert to be sent to national professional bodies recommending this practice cease immediately Orientation programme for midwives to review gaps in practice and the availability of Counties Manukau DHB obstetric guidelines Guideline to be drafted for the post natal care of women who have had epidurals Completed Serious 4G Laceration to abdominal area from protruding metal on commode chair. Patient required surgery. Faulty design of old commode chairs All old commode chairs identified and fixed Completed Sentinel 4G Patient with suspected heart attack given anti-clotting medication which resulted in spinal cord bleed and subsequent paraplegia Over-interpretation of tests led to patient being treated as having a heart attack and prescribed anticoagulants Nursing staff didn’t recognise that progressive leg weakness and numbness was a cause for urgent escalation Publicise other reasons for troponin rise among RMOs Review and update clinical pathway and preferred treatment guideline Increase awareness of adverse event profiles of anticoagulants Present case at nursing round to reinforce need to escalate care for any deteriorating patient In progress DHB Summary of Serious and Sentinel Event Report 2009/10 12 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4D Undiagnosed blood clot resulting in pulmonary embolus and subsequent death Three negative ultrasound tests contributed to the decision not to treat despite the high probability of a deep vein thrombosis (DVT) in high risk patient Regional DVT pathway team to develop pathway that takes into account the pretest probability Order form for DVT diagnostic ultrasound to include standardised risk factor identification Result of diagnostic ultrasound to refer to the pre-test probability Serious 4D Abdominal urinary catheter perforated bowel which required surgery Potential for complications not recognised as patient considered low risk and preprocedure investigations not done Patient’s signs and symptoms were subtle and masked by pre-existing conditions and therefore not recognised by staff Post procedure guidelines following a catheter insertion not formalised to support and guide staff with the care of a patient Urology service to review and update best practice guidelines for initial supra pubic catheter procedures (insertion and changes) Case presentation to wider health care team to raise awareness In progress Sentinel 4B Delay in identifying foetal distress during labour despite being on a baby monitoring machine Emergency caesarean section performed, but baby died No guideline for baby monitoring machine in antenatal care unit Baby monitoring machine alarm was switched off by automatic default, unbeknownst to the staff No staff member allocated to patient care during lengthy handover Baby monitoring machine guideline for antenatal care to be developed Review the model of care on maternity ward Implement a standardised communication process during handover All baby monitoring machines need to have functioning alarms All antenatal patients to be seen by a SMO within 24 hours of admission on the maternity ward Education of medical staff about standards of documentation Completed DHB Summary of Serious and Sentinel Event Report 2009/10 13 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 3 Retained endoscopic basket requiring second endoscopy to remove. Rare equipment failure with endoscopic basket. .Special surgical equipment to extract broken piece not readily available resulting in patient having to undergo second endoscopy. Company notified and MedSafe alert sent. This brand of equipment no longer being used. Process to be put in place to notify staff re location of special equipment. Completed Serious 5 Augmentin prescribed to patient with known allergy to penicillin Patient required additional treatment Centre for Adverse Reactions Monitoring (CARM) alert on electronic record not checked Medication safety pharmacist to ensure allergy information updated with general practitioner (GP) and CARM Revise allergy poster and disseminate organisation-wide Reminder to all medical teams to check for drug allergies Completed Serious 5 Following clot buster (urokinase) the patient’s blood-thinning medication dose was too low over 12-hour period resulting in long term loss of pulses in right leg There is no place to document blood results in urokinase protocol therefore heparin chart was used to document blood results and heparin changes Mismatch between urokinase blood thinning protocol (heparin) and standard hospital heparin chart. Patient given standard dose that was too low for condition New thrombolysis protocol form developed that allows a place for results to be charted so the standard heparin chart is not used – this form is started in radiology and documentation continues on same form Completed Serious 5 Insulin overdose causing severe low blood sugar levels Prescribing error – strength confused with dose when medications charted on admission Insulin not charted in main medication chart Medication reconciliation process not available over the weekend due to lack of pharmacy resource Hypoglycaemia not recognised as cause of depressed level of consciousness in diabetic patient Prescribing doctor to list medication in main medication chart Work with senior diabetes specialist team to review and reformat insulin chart so it reflects key alerts Lack of pharmacy resource to be referred to senior executive management team for discussion Clarify role of diabetes nurse In progress DHB Summary of Serious and Sentinel Event Report 2009/10 14 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Serious 5 Overdose of anti-clotting medication due to prescribing, dispensing and administration error Patient suffered severe bleed requiring several transfusions Medication reconciliation process not available over a public holiday due to lack of pharmacy resource Lack of familiarity with drug meant staff didn’t question unusual dose Case presentation to wider health care team to raise awareness Lack of pharmacy resource to be referred to senior executive management team for discussion Serious 6 Inpatient fall resulting in fractured wrist Watch not maintained for confused and unstable patient Serious 6 Inpatient fall resulting in fractured wrist Falls risk assessment not completed therefore falls prevention care package not implemented Serious 6 Inpatient fall resulting in fractured wrist Patient with high falls risk left unattended in toilet Limited staff available to respond to call bells Falls risk assessment to be completed for all patients within six hours of admission Appropriate falls prevention interventions to be implemented for high risk patients Patient safety falls work group is currently investigating contributing factors to falls with a view to implementing effective risk assessment and prevention strategies across the organisation Serious 6 Inpatient fall resulting in fractured wrist Contrary to patient’s usual practice, patient had mobilised independently without requesting assistance Serious 6 Inpatient fall resulting in fractured hip requiring surgery Fall prevention interventions not implemented for high risk falls patient Serious 6 Inpatient fall resulting in fractured hip requiring surgery High risk falls patient fell due to slippery floor – wearing hip protectors at the time Serious 6 Inpatient fall resulting in fractured hip requiring surgery Against advice, patient had mobilised independently and slipped on wet floor in bathroom Serious 6 Inpatient fall in bathroom resulting in fractured hip requiring surgery Lack of appropriately placed handrails in bathrooms in new patient block Serious 6 Inpatient fall resulting in pelvic fracture Deterioration in condition and falls prevention strategies not put in place Serious 6 Inpatient fall resulting in pelvic fracture Failure to implement falls reduction strategies when patient identified as high risk Falls risk assessment to be completed for all patients within six hours of admission Appropriate falls prevention interventions to be implemented for high risk patients Follow-up In progress Patient safety falls work group is currently investigating contributing factors to falls with a view to implementing effective risk assessment and prevention strategies across the organisation DHB Summary of Serious and Sentinel Event Report 2009/10 15 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 6 Inpatient fall resulting in fractured finger and upper cervical spine Failure to implement falls reduction strategies when patient identified at risk Cot sides left partially down Inadequate handover from rest home Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service Client not linked into usual clinical processes within DHB model of care, due to receiving interventions from clinical staff that were not based within usual team Lack of clarity around the process for selection of external supervisors and the mechanism for the external supervisors to link with the DHB clinical team for registrars engaged in psychotherapy with clients Unclear process for selection of appropriate cases for registrars to provide psychotherapy The usual clinical pathway process applies to all clients, irrespective of from whom or where they are receiving their interventions Regional training committee to have a regional process in place for supervisor selection and provision for the registrars college supervisor to link in with the DHB psychiatrists Regional training committee to clarify process and develop a guideline for registrars Actions completed Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service Inconsistent process for triage of referrals and allocation of a case manager Incomplete documentation of contacts with client and/or family Processes for triage and allocation for follow-up to be reviewed to ensure a clearly identified consistent approach to triage decision-making for routine or urgent follow-up All attempts to make contact with families to be documented in the client’s notes in the electronic clinical record. Contact numbers to be checked against other databases in patient management systems Actions under way Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service Lack of clarity around process Process for referral for cultural support to be clarified and made known to all teams Actions under way Cultural support referral and documentation of cultural interventions Cultural support staff to be trained to ensure all cultural contacts to be documented in the clinical notes Actions completed Delay in access to psychological intervention Review of prioritisation process for access to psychological services DHB Summary of Serious and Sentinel Event Report 2009/10 16 Counties Manukau District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service People who may require follow-up for existing or identified issues, and have agreed to private follow-up after declining public follow-up may not actively seek that follow-up Research protocols not followed Staff to look at options for maintaining contact to support the agreed engagement with the private sector An investigation and review of the research project to ensure agreed protocols are followed Actions under way Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service No findings which impacted on outcome N/A N/A Sentinel 2 Suicide of an outpatient known to mental health services within seven days of contact with this service Front line staff received notification of the client death via email request for a coroner’s report All requests for coroner’s reports to be directed to the service manager or team manager for follow-up with the staff members who have been involved in client care Actions completed GPs are not routinely being notified of the death of a client when this comes to the attention of the DHB mental health services Process to be put in place whereby the service manager or team manager for the team where the death has occurred, ensures telephonic or written notification is sent to the GP on DHB records Staff maintaining a hard copy form of co-ordinated care plan, thereby having no current plan in the electronic documentation system Clear directive that only one system will be used and all plans to be documented in the electronic documentation system Actions completed All contacts were not documented in the notes Staff to ensure that all client did not attends, phone calls and attempts to contact client are documented in the client’s notes Actions under way Lack of clarity around responsibility for monitoring and follow-up of mental state for clients attending groups when not under the team running the group Criteria for group attendance to be clarified to ensure that only clients who receive services from a specialist team may attend Actions completed The team providing after hours services were not familiar with local supports and DHB practices, impacting on the response in a crisis situation Robust system to be in place for the team providing after hours services to ensure staff have an orientation which includes client pathways to accessing services within DHB and information about local supports and DHB practices Actions under way Sentinel Sentinel 2 2 Suicide of an outpatient known to mental health services within seven days of contact with this service Suicide of an outpatient known to mental health services within seven days of contact with this service Recommendations/actions Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 17 Counties Manukau District Health Board Serious or sentinel Sentinel Sentinel Event code* (see codes below) 2 2 Description of event Suicide of an outpatient known to mental health services within seven days of contact with this service Suicide of an outpatient known to mental health services within seven days of contact with this service Review findings Recommendations/actions Follow-up Care plan held at the team providing after hours services did not reflect up-to-date information DHB staff to ensure that a current care plan is available to the team providing after hours services for those clients who are receiving dialectical behaviour therapy (DBT) treatment Actions completed A number of agencies were involved in providing care for the client; the opportunity for sharing of relevant information was missed All mental health staff ensure that they utilise the regional electronic record to review the clinical information of clients who are accessing services provided by all services involved in the client’s care Actions under way Capacity for people to receive long term psychological therapy is limited The capacity of health psychologists to provide follow-up after discharge from general hospital to be clarified for mental health staff Actions completed Community mental health centre staff were not notified of the client’s non-arrival at the crisis respite facility Agreement that crisis respite facilities are to advise the relevant clinical team if a client does not arrive at the expected time Actions completed The plan for transport to crisis respite changed and this was not communicated to community mental health centre staff Lack of clarity around the expectation for a face-to-face handover by crisis staff for clients entering a respite facility Despite the psychiatrist ensuring that mental health medications were dispensed blister packed and one week at a time, the family were able to fill a script for one month’s physical health medications and have these available in the house Agreement with non-government organisation (NGO) providers that any change to an agreed plan is to be communicated to the relevant clinicians within a timely fashion Clear directive to be given to crisis staff of the expected practice regarding the process of supporting a client into a community crisis respite facility DHB staff to notify the GP of those clients who are regarded as high risk to self/self harm and where there is a plan for weekly dispensing of medications Actions under way DHB Summary of Serious and Sentinel Event Report 2009/10 18 Waikato District Health Board Waikato Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Serious 6 Patient fall resulting in fractured hip Not formally reviewed Serious 6 Patient tripped on return from toilet and fractured hip Was being supervised at time Not formally reviewed Serious 6 Patient fall resulting in fractured hip Patient slipped getting out of bed Serious 6 Patient fall resulting in fractured hip Patient left unattended on commode – attempted to mobilise and fell Serious 6 Patient fall resulting in fractured hip Patent with multiple risk factors mobilised without assistance and fell Falls assessment was incomplete and falls risk was not accurately assessed Serious 6 Patient fall resulting in injury and dislocated hip Patient left unattended on commode – attempted to mobilise and fell Serious 6 Patient fall resulting in fractured pubic bone Patient fell on transfer from chair to bed Serious 6 Patient fall resulting in fractures to hand Patient with cognitive impairment mobilised without assistance Serious 6 Patient fell and fractured hip Review in progress Serious 6 Patient fell in bathroom and sustained fractured hip Review in progress Serious 6 Patient climbed over bed rails and fell – sustained fractured hip Review in progress Serious 6 Patient fell and dislocated hip Review to be completed by 30 October 2010 Serious 6 Patient had seizure and fell from trolley sustaining fractured right arm Review to be completed by 30 October 2010 Follow-up Falls minimisation project has been completed Falls minimisation committee established and meets monthly Falls focus group meet quarterly Trials and introductions of best practice multi-factorial, preventative interventions New falls procedure being developed Plan to introduce the validated Heindrich model of falls assessment and management – this will be developed in partnership with an international organisation and will involve the delivery of education, learning and training via 24/7 web-based programmes Staff education provided on managing patients with delirium and confusion Review to be completed by 30 October 2010 DHB Summary of Serious and Sentinel Event Report 2009/10 19 Waikato District Health Board Serious or sentinel Serious Event code* (see codes below) 11 Description of event Patient sustained fracture to foot whilst being transferred through door in wheelchair Review findings Recommendations/actions Follow-up The patient’s foot caught the doorframe as the attendant turned the wheelchair through a doorway that was angled into another corridor Implement process of ensuring staff understand how to transport patients safely in wheelchairs Completed There were delays in diagnostic intervention and pain management for patient Revise education for staff regarding appropriate assessment and pain management Completed Serious 4D Patient developed cellulites on hand following luer insertion. Patient required surgical intervention to drain abscess Review concluded staff followed correct process for insertion and was as per intravenous insertion protocol As a result of this review an additional learning was identified of staff to be reminded to ensure appropriate documentation of luer site is completed Completed Serious 12 Prolonged norovirus infection outbreak – involving six patients and 30 staff Confirmed norovirus outbreak Extensive infection control outbreak management plan in place Extensive outbreak management plan in place Extensive staff education and audit programmes in place Hand hygiene project in place Alcohol based hand rub in place throughout the organisation All actions completed and infection control practices ongoing Sentinel 4D Patient had cardiac surgery and developed post surgical complications – patient died Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Serious 4G Patient found lying across bed and in pain X-ray confirmed dislocated hip – taken to theatre for relocation No root cause identified As a result of the review additional learnings were identified including prompt pain relief management and reminder to staff of correct mode of assisting patients move with limb injuries Completed DHB Summary of Serious and Sentinel Event Report 2009/10 20 Waikato District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Guideline completed and implemented Significant change made to credentialing process of foetal monitoring education for practitioners Serious 4C Failure of recognition of an obstructed labour in a multiparous woman Issues related to transfer of woman under lead maternity carer care in labour from primary birthing facility to tertiary obstetric unit Urgent lower caesarean section required baby considered to be born stillborn; patient suffered a cardiac arrest and required active resuscitation Patient had significant haemorrhage and required a hysterectomy Patient has ongoing medical issues as result of event Revise handover processes ensuring appropriate information is provided The new transfer of care guideline replacing the outdated maternity handover and handback procedure is to be signed off and implemented as a matter of urgency; the completed document is to include that all women transferred from primary into secondary care shall have a prompt assessment including complete set of baseline observations taken on admission and this is to be documented in the clinical records Service reviewing foetal monitoring credentialing processes Sentinel 4B/C A baby suffered cerebral palsy potentially as a result of the labour and birth No root causes identified As a result of this review other learning’s were identified: Serious 12 Prolonged MRSA infection outbreak on ward involving 16 patients Cross transmission within ward – ward closed to admissions Ongoing education regarding foetal monitoring in labour – including electronic foetal monitoring Completed Improved communication between staff in rural areas and tertiary units whilst awaiting retrieval Completed Share learning’s of this event with staff Completed Extensive outbreak management plan in place Extensive staff education and audit programmes in place Hand hygiene project in place Alcohol based hand rub in place throughout the organisation All actions completed and infection control practices ongoing DHB Summary of Serious and Sentinel Event Report 2009/10 21 Waikato District Health Board Serious or sentinel Sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up 4B Baby presented with gastroenteritis and the correct clinical procedure/ pathways regarding the management of gastroenteritis not followed by staff Baby died at home following discharge from unit Failure to recognise and action the probable ongoing dehydration in part due to a secondary diagnosis distracting from the appropriate clinical management of gastroenteritis To review the current gastroenteritis guidelines that are available and develop and implement new protocol for the paediatric inpatient environment Change to management plan for such admissions Completed All children under one year to be weighed on admission and daily thereafter Completed Audits to take place to ensure compliance with new weighing regime Completed Process to be implemented to manage children/babies re-presenting to service within a short timeframe Completed Learnings from this event to be shared amongst staff Completed Serious 4D Patient suffered bladder harm as a result of indwelling catheter Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 4C/G Patient had procedure to remove self-ingested foreign object from stomach Patient condition deteriorated and this was not escalated in a timely manner Patient died from sepsis Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Serious 4B/G Patient not referred in a timely manner by lead maternity carer for review in early pregnancy Further delays occurred in service leading to slow actioning of the referral to appropriate clinic Patient went into premature labour Delayed referral by primary practitioner for obstetric specialist review To advise the Midwifery Council of the outcomes of this review Changes made to how referrals are processed within service Completed Delay within service actioning the received referral Detailed information provided to practitioners informing of the required information for referrals Procedure in draft format and due for completion Delay in recognising and acting on severity of deterioration of patient condition – patient died Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 4C DHB Summary of Serious and Sentinel Event Report 2009/10 22 Waikato District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4C Delay in recognising and acting on severity of deterioration of patient condition – patient died Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 4C Patient admitted following fall at home. Sustained fractured pelvis and skull from fall Patient was not managed as per required pathway and subsequently died Failure to use best practice to manage head injury patient: in particular a timely request for a head CT scan Locum medical staff working in ED without robust orientation Changes made to how orientation is provided to new staff working in areas Audit to ensure compliance with specific pathways Use information in education sessions to advise staff on how to manage such patients Senior medical staff to agree locum covers with managers In progress Serious 4A Patient presented to ED having sustained a fall at home – patient was discharged home and represented to ED days later where a fractured femur was diagnosed Other possible diagnoses were not considered and excluded before discharge Use learnings form this event in case review for staff education Discuss with all ED nurses at ED nurses’ meeting Particularly, discharge section of form not well completed Audit of triage forms including criteria of discharge and self-discharge, completed In progress Serious 4B/F/G Patient discharged to regional hospital and developed lifethreatening complications – patient re-admitted to Waikato Hospital and received ongoing care and treatment Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Serious 4B Patient admitted with stab wounds – undue delay meant optimal timing for safe surgical intervention was missed Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Serious 4D Patient arrested following epidural insertion – delay in perimortem caesarean section – mother admitted to intensive care unit and baby admitted to neonatal intensive care unit Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 DHB Summary of Serious and Sentinel Event Report 2009/10 23 Waikato District Health Board Serious or sentinel Event code* (see codes below) Description of event Serious 4C Patient transferred to ward from high dependency unit Patient’s condition deteriorated and was not escalated to medical staff in a timely way Sentinel 4B Sentinel Review findings Recommendations/actions Follow-up Failure to escalate the deteriorating patient to a medical officer to review in a timely manner RRS (Rapid Response System) adult deterioration detection chart is being trialled at present as of August 2010 throughout Waikato Hospital. This when rolled out organisationwide will give some framing and parameters for nursing staff to identify then escalate the adult deteriorating patient for review by medical officer Evaluation of trial has been completed Awaiting final report as at 30 September 2010 Patient admitted following road traffic accident Delays in management occurred. Patient died Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 4A Patient sent home from ED Returned two days post motor vehicle accident with multiple issues Required intensive care unit and surgical management. Patient died Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 12 Patient readmission with hospitalacquired pneumonia and MRSA. Patient died Review to be completed by November 2010 Mortality event Review to be completed by November 2010 Review to be completed by November 2010 Sentinel 4D Patient required surgery for fractured femur. Surgery delayed Following surgery, patient developed complications and condition deteriorated. Patient died Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Sentinel 4G Patient admitted for elective surgery Following surgery patient developed complications. Patient died Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Sentinel 4G Patient admitted with low blood pressure and tachycardia – found collapsed on floor. Patient died Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 DHB Summary of Serious and Sentinel Event Report 2009/10 24 Waikato District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4G Patient admitted with renal failure and later found deceased Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Sentinel 4G Patient admitted for cardiac surgery Complications developed following surgery. Patient died Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Review not completed – identified through newly established mortality review project June 2010 Sentinel 4B,12 Patient developed cellulites from intra-venous (IV) site and possibly sepsis. Patient died Review to be completed 30 November 2010 Mortality event Review to be completed 30 November 2010 Review to be completed 30 November 2010 Serious 5 Baby administered medication by a route that protocol had not been authorised for The failure to follow DHB policy regarding the development, approval and implementation in a change of practice probably contributed to the inappropriate administration of the medication The service needs to have a process regarding policy, protocols, procedures and guidelines (PPPG) that are required Key staff responsible should be identified and attend PPPG workshop Learnings from this event regarding the correct PPPG process should be shared with all staff through in-service education, staff meetings and other service forums Other learning identified as part of review process: an early warning scoring system may have alerted staff to have involved more senior medical staff sooner rather than administering the medication Serious 11 During an incident resulting in the use of physical restraint mental health service user sustained a fracture to arm Nil issues identified in restraint de-brief and review process Physical investigation of client’s injury revealed previously undiagnosed bone condition Service user’s treatment and risk management plans updated and amended to incorporate information on medical condition Completed Serious 8 Service user subject to a community treatment order was admitted voluntarily to the acute adult inpatient unit but left the unit without approved leave Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 DHB Summary of Serious and Sentinel Event Report 2009/10 25 Waikato District Health Board Serious or sentinel Sentinel Serious Event code* (see codes below) Description of event 2 Suicide of a service user receiving treatment in the community, within seven days contact with the service Reviewed Service user receiving treatment in the community self-harmed requiring assessment in ED Medically cleared without admission to hospital required No root cause identified Other learnings during the review identified the risk assessment and management plan had not included specific information on environmental risk factors Service users not to be accepted by provider without comprehensive risk assessment and management plans in place Completed Checklist to be developed to assist in identifying everyday items and substances which could be potentially harmful when someone is at risk of self harm Completed 11 Review findings Recommendations/actions Follow-up Completed NB Additional information not included to protect the family Sentinel 11 Sudden death of a service user subject to Mental Health (CAT) Act 1992 inpatient order Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 11 Sudden death of a service user receiving treatment in the community, within seven days contact with the service Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Sentinel 2 Sudden death of a service user receiving treatment in the community, within seven days contact with the service Review to be completed 30 October 2010 Review to be completed 30 October 2010 Review to be completed 30 October 2010 Sentinel 2 Suicide of a service user receiving treatment in the community, within seven days contact with the service Nil – no care issues identified Not applicable – review concluded no care issues Not applicable – review concluded any care issues Serious 3 Post operative wound infection secondary to retained product or six-week period – required readmission to hospital, intravenous antibiotics and two additional surgical procedures Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 Review to be completed by 30 October 2010 DHB Summary of Serious and Sentinel Event Report 2009/10 26 Bay of Plenty District Health Board Bay of Plenty Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4D Patient inhaled stomach contents when anaesthetic given, subsequently died A lack of communication led to nasogastric tube not being inserted prior to the patient being anaesthetised Lack of guidelines regarding decision making and escalation when a patient deteriorates in theatre after hours Ensure adequate communication between staff at handover and during the continuing care of the patient To be covered in the patient safety initiative – clinical communication Subject to coroner’s inquest Sentinel 2 Suicide of an outpatient known to mental health services within seven days of last contact with service A number of incidental findings were identified but no major system failures contributed to this event More attention to the inclusion of family members in consumers’ crisis plans Development of the integrated model of service Development of an escalation policy covering procedures to be followed in the event of repeated re-presentations with active self-harm suicidal ideation and plans Clinical nurse specialist appointed to advise and encourage strengthening standards of crisis work and clinical documentation Projects in progress to strengthen acute response and review options for crisis services Risk assessment project: new risk assessment forms and staff training occurring Sentinel 4A Misdiagnosis of strangulated hernia resulted in complications which led to patient death Internal review completed Multiple “distracting” elements to clinical history which resulted in a wrong working diagnosis Lump in groin was hernia and required surgery Heuristic, training – case presentation Serious 6 Inpatient fall resulting in a fractured ankle Person wearing jandals in wet conditions, surface of steps slippery Steps be replaced with grooved decking timber Complete Sentinel 2 Suicide of an outpatient known to mental health services within seven days of last contact with service Review in progress Nil to date Subject to coroner’s inquest Provisional findings: Failure to recognise the acuity and treat appropriately DHB Summary of Serious and Sentinel Event Report 2009/10 27 Bay of Plenty District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Sentinel 6 Inpatient fall sustained head injury and subsequently died Provisional findings: Death from injuries sustained by this fall may not have been preventable however there were delays in recognising deterioration in condition Falls plan of care was not updated when the patient moved to a new environment within the ward No co-ordinated plan of care was developed post fall No follow-up to unanswered pages requesting medical review and no escalation of the need for medical review Review of organisation-wide falls reduction programme Review processes to ensure staff are aware of and understand organisational policy and protocol Review the approach and processes of clinical handover Review on-call house officer workload capability at weekends That the current format and process of emergency doctor roster publication be reviewed Develop a protocol for non response to pages requesting assistance from medical staff Sentinel 2 Suicide of an outpatient known to mental health services within seven days of last contact with service Review in progress Nil to date Follow-up To be covered in the patient safety initiative – falls reduction Provisional findings: A number of incidental findings were identified but no major system failures contributed to this event DHB Summary of Serious and Sentinel Event Report 2009/10 28 Bay of Plenty District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Serious 6 Inpatient fall resulting in fractured hip Elderly confused patient took self to toilet unaided – falls risk assessment had been completed and risks identified Serious 6 Inpatient fall resulting in fractured ribs Elderly patient being assisted by staff to walk to a chair Serious 6 Inpatient fall resulting in a fractured arm Elderly confused patient Assessed as medium falls risk Going to toilet and slipped in own urine Safety watch discussed but not in place Serious 6 Inpatient fall resulting in a fractured hip Elderly patient, legs became weak while walking with gutter frame and being assisted by nurse Sentinel 6, 4C Inpatient fall and sustained head injury and died Elderly patient assessed as high falls risk being assisted up to toilet with mobility frame – sudden collapse hit head on floor and died three days later Unpreventable fall Serious 6 Inpatient fall resulting in a fractured arm Unwitnessed fall Falls risk assessment completed – moderate Recommendations/actions Follow-up Falls has been identified as one of the organisation’s top three patient safety priorities. A project is being scoped and progress will be monitored by the patient safety committee This will include a review of current organisation-wide falls reduction programme to ensure interventions and documentation is implemented and evaluated to effectively reduce the risk of harm falls to ensure it reflects patients current status Be more proactive with high falls risk ensure falls risk assessments are accurate Trial of low beds has commenced DHB Summary of Serious and Sentinel Event Report 2009/10 29 Lakes District Health Board Lakes Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 6 Unwitnessed fall in shower Falls risk assessment completer. Patient independent Patient was on blood thinning drugs to prevent clotting. This caused uncontrolled internal bleeding after fall Soap dispensers to be installed in all showers to reduce falls risk A falls professional advisory group has been established to implement initiatives that reduce falls A business case to purchase equipment to reduce falls Serious 6 Unwitnessed fall of an inpatient Unwitnessed fall – patient fell against uncovered heater resulting in injury Root cause analysis completed with recommendations to be implemented Business case for equipment to support patient safety, eg, low/low beds and sensor mattresses, heater protection Serious 4D Patient required bladder monitoring post operatively returned to theatre for surgery Failure to monitor and treat patient post-operatively led to complications Root cause analysis completed Nursing education on assessment, planning, intervention and evaluation of patient care Purchase of bladder scanning equipment Serious 4D Patient being infused with a chemotherapy drug. The intravenous site tissued causing a chemical burn and tendon damage which required plastic surgery and ongoing physiotherapy Staff had difficulty inserting the IV luer to deliver the drug. The IV luer could only be sited on one arm There was limited information available to support the clinical care of the patient after hours A protocol for difficult cannulation is being developed Written patient and medical information on complications of IV chemotherapy drugs being prepared Sentinel 2 Suicide of a mental health client within seven days of contact with the service Patient was able to use a previously unfilled prescription which meant they collected more medication than was indicated in the discharge process Discharge planning processes reviewed including risk assessments as part of discharge Process to be developed around patient’s personal medication supply when admitted to the inpatient unit DHB Summary of Serious and Sentinel Event Report 2009/10 30 Lakes District Health Board Serious or sentinel Event code* (see codes below) Serious 3 Serious 4G Description of event Review findings Recommendations/actions Retained surgical swab Investigation found inaccurate count was performed Case review completed Implementation of a theatre count document Use of separate instrument and swab packs Implemented new swabs that are X-ray detectable A more structured procedure for counting swabs is being trialled Deterioration of patient with inadequate handover on transfer of care Failure to monitor patient Incomplete handover of patient information Root cause analysis with recommendations completed Review of current policy and procedure Review of current processes for clinical handover of patients that supports safe transfer of care Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 31 Tairawhiti District Health Board Tairawhiti Serious or sentinel Event code* (see codes below) Sentinel 4F Serious 3 Serious 4D Description of event Review findings Recommendations/actions Follow-up Following transfer from ED patient arrested and died on arrival in ICU Inconsistent process for patients presenting to ED based on referral process, ie, GP referrals are seen by junior doctors and self-presenting patient are seen by ED medical staff Triage process failed to alert ED medical staff to unwell patient as GP referral ED dept very busy at time of presentation New medical staff unfamiliar with department and equipment Review referral pathways to clarify responsibility for admission, eg, GP referrals and selfpresenting patients Improve an orientation package with a common foundation for all personnel working in ED Consider one multidisciplinary guideline manual for ED to enable clear, concise information for all professional groups Implementation process under way In addition changes have been implemented regarding the roles and relationship between ED medical staff and the RMO team Retained equipment following insertion of central IV line – requiring transfer to tertiary service for procedure to remove Inconsistent knowledge and insertion practices Variation of lines available for use Product failure concern referred to Medsafe Review and standardise catheters and education on the insertion and management of these special IV lines Review and improve access to guidelines for the insertion and management of these IV lines Product review under way aligned with tertiary hospital Patient arrested when given anaesthetic for surgery Successful resuscitation During resuscitation potassium level found to be abnormal. Not identified prior to surgery – unclear if related to treatment, eg, bowel prep Audit under way to identify frequency of patient presenting to theatre with electrolyte imbalance that has not been previously identified Initial findings suggestive of imbalance resulting from prep To be finalised DHB Summary of Serious and Sentinel Event Report 2009/10 32 Taranaki District Health Board Taranaki Serious or sentinel Event code* (see codes below) Description of event Serious 11 An inpatient became un-rousable – patient was admitted to ICU overnight for antidepressant overdose “On leave” procedure to be strengthened On leave procedure reviewed and additional statement incorporated to reflect on-leave escort responsibilities and also client’s contract towards abstinence from unauthorised/non-prescribed medications Completed Serious 11 An inpatient disclosed that she had overdosed on antidepressant medication that then required treatment and monitoring in ICU for 48 hours Inconsistency around the level of service user “search” required The appropriate level of “search” required will be decided on a case by case basis. As a minimum this will include searching of the service user’s bag and clothing but will not at any stage involve intimate searches Completed Detailed risk assessment not provided at the time of transfer from one service to another Memo to be sent out to all staff, service-wide, to raise awareness about the importance of undertaking a detailed risk assessment, that the risk assessment is communicated on transfer from one service to another and that the appropriate level of search is undertaken Completed Patient was sent home from ED with an undiagnosed bleed on the brain Patient presented again after collapsing on arrival at home and was diagnosed appropriately and admitted but progressively deteriorated and died a few days later Lack of a robust formal referral process to ED that resulted in the original concern of a possible stroke not being highlighted to ED staff A formal process for referral of patients by staff into the emergency department be established Completed Focus on one diagnosis and lack of consideration of alternate diagnoses in spite of being provided with information Case discussed by ED staff at the mortality and morbidity meeting highlighting the focus on one diagnosis Completed A more robust process to ensure the appropriate senior doctor supervision of junior medical staff is required Expectations already in place with both senior and junior medical staff regarding supervision, however these are to be outlined in the orientation booklet Completed Review of the clinical record for the patient’s visit showed gaps in documentation including no documentation of the attending doctor discussing the patient with a senior doctor Implement a clear pathway for more junior medical staff to seek advice/guidance from a designated SMO Completed Sending the patient home Documentation standards highlighted for medical and nursing staff and audits of clinical content such as completion, date, time and signature to be monitored Completed and ongoing To be documented that patient has been discussed with SMO Completed Use “aid to identification of at risk elderly” assessment form when there are questions over the ability for an elderly person to cope at home – to be discussed with staff Completed Sentinel 4A Review findings Recommendations/actions Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 33 Taranaki District Health Board Serious or sentinel Serious Serious Serious Event code* (see codes below) Description of event 4A Patient presented with and is being treated for lung cancer that was visible on a chest X-ray taken in 2008 – the 2008 X-ray result was not reviewed at the time 4A 4A Review findings Recommendations/actions Follow-up Four areas of focus for recommendations following review: IT process issues radiology results management clinical training, and management of resources Review results management processes and obtain endorsement by clinical heads of department including: clearing the backlog of viewed but not “marked as viewed” results delegation to junior staff for results management training needs identified roll-out of digital radiology IT and key champions to monitor on a weekly basis Nearing completion A team has formed to evaluate and oversee implementation of the recommendations Monitoring and evaluation to be implemented once all other actions above complete Completed Patient presented with and is being treated for lung cancer that was visible on a pre surgery chest X-ray taken in 2008 but was not acted on at the time Failure to report the chest X-ray and publish the result on the DHB’s electronic patient management system Failure to send a copy of the report to the GP Failure to check the chest X-ray that had been ordered, nor to hand this over to the House Surgeon for the team Failure of staff that accessed the result for the other X-ray, taken at the same time, to not see that the chest X-ray had not been reported Three different junior medical staff cared for the patient, all covering for sick leave and crosscovering other teams See above recommendations and actions Completed Patient presented with and is being treated for lung cancer that was visible on a chest X-ray taken in 2009 but not acted on at the time No review of chest X-ray film while patient admitted Copy of chest X-ray report not sent to GP GP did not follow up on chest X-ray report as requested to do No follow-up of the chest X-ray report by medical team post discharge of patient Radiology has reviewed, discussed and have put in place a system that ensures all X-rays taken at the one radiology appointment are reported on, before the complete report can be sent for verification Medical management team leader to be made aware of incident and implications of covering junior medical staff Completed Pre-admission nurses to be informed of incident and confirm that a process is in place to check every diagnostic ordered from pre-admission clinic Completed Radiology now send out copies of all inpatient and outpatient radiology reports to GPs unless there is clear direction from the consultant or patient that this should not occur Completed GP involved will be diligent re follow-up of radiology reports if requested Completed Responsibility and accountability for ordering, reviewing, signing off “as read” and taking appropriate action in regard to diagnostic results to be clearly communicated and compliance monitored Progressing DHB Summary of Serious and Sentinel Event Report 2009/10 34 Taranaki District Health Board Serious or sentinel Serious Event code* (see codes below) Description of event 6 Inpatient fall resulting in a fractured pelvis Review findings Falls risk assessment process not repeated when the patient transferred to the ward Patient not specialled on the night of the fall – no reasons for this documented Verbal handover at the start of the shift did not give detail re patient’s restless state Recommendations/actions Follow-up Instruct staff to repeat the falls assessment as part of the transfer/admission process Ongoing Education followed by audit to ensure compliance Ongoing Document in clinical notes information related to specialling including discussions with the duty manager Ongoing Use available documentation, eg, staff deficit forms to accurately capture information/ contributing factors When there is no special available, a management plan needs to be formulated and documented in the clinical notes, eg, reassigning of work load (base a staff member in the room), consider relocating the patient to another area Ongoing DHB Summary of Serious and Sentinel Event Report 2009/10 35 Whanganui District Health Board Whanganui Serious or sentinel Event code* (see codes below) Sentinel 2 Serious 4A/B Description of event Review findings Recommendations/actions Follow-up Suicide of a community mental health patient, known to the service within seven days Patient transient and regularly did not attend appointments Key worker made a number of attempts to contact patient at several addresses All existing and new staff made aware of the “did not attend” policy Community mental health team established a risk register to record any clients of concern Clients on risk register are discussed at weekly multidisciplinary team meetings Incorrect referral process for surgical assessment of a neck lump resulted in delayed surgery Outpatient clinic letter was used as an internal referral, instead of the approved referral form, which is logged through patient scheduling referral centre Lack of clarity as to which specialty has primary responsibility for the assessment of neck lumps Consultants and scheduling staff advised that only internal referral forms would be accepted to be used Establishment of a neck lump guideline, in conjunction with departments of surgery and ear, nose and throat Developed DHB Summary of Serious and Sentinel Event Report 2009/10 36 Whanganui District Health Board Serious or sentinel Serious Event code* (see codes below) 6 Description of event Elderly patient, with a number of significant medical morbidities, fell while an inpatient, fracturing a hip – she died in the operating theatre during the corrective procedure Review findings Recommendations/actions Follow-up Patient was prescribed haloperidol for sedation that was higher than recommended for age and weight – this dose, along with other analgesia administered more than likely contributed to the fall Refresher sessions on best practice administration of analgesics and sedatives be implemented to all nursing staff Completed for existing staff, will be included in orientation programme for new staff; Canterbury Guidelines in all clinical areas Patient’s condition slowly deteriorated on the weekend before the fall but this information was not handed over to the relevant staff Doctors to use the Canterbury Guidelines for Common Medical Conditions and seek pharmacist advice when charting analgesic and sedation for frail, elderly patients In progress Medically ordered “special” was discontinued when patient appeared to settle A formal clinical handover policy/standard be developed and implemented with the underpinning principles of collaboration between professional groups and inclusion of patient and family Procedure completed Patient’s falls risk plan was not comprehensive, nor updated as her condition changed A procedure be developed with inbuilt decision support for ordering, ceasing specials and specifying the level of staff who should special a patient Updated falls injury prevention policy and standard be completed and implemented Completed Sentinel 2 Suicide of a community mental health patient known to the service within seven days Care plan and risk assessment not updated following discharge from inpatient unit Care plans and risk assessments are updated regularly Audits to be conducted to monitor compliance and feed back results to the treating team Serious 5 Neonate given incorrect dose of antibiotic Prescriber used an adult ICU reference, instead of the neonatal medication reference All staff instructed to use neonatal medication reference as the only resource Compliance monitored through incident reporting system Error detected several days later when neonate was being transferred back from another DHB Paediatric house surgeon orientation programme updated Compliance monitored through incident reporting system DHB Summary of Serious and Sentinel Event Report 2009/10 37 Whanganui District Health Board Serious or sentinel Sentinel Sentinel Sentinel Sentinel Event code* (see codes below) 4D 2 12, 6 2 Description of event Unexpected death of a patient undergoing plasma exchange, from overwhelming infection Review findings Recommendations/actions Follow-up No effective process for communicating urgent afterhours laboratory results for outpatients Process developed for communicating urgent after-hours results for outpatients Responsible clinician not identified on laboratory’s urgent fax notification form Plasma exchanges take place in a day unit and laboratory results are sent to this unit which is not always open Urgent fax notification laboratory template has been modified to identify treating clinician Location for plasma exchanges is being reviewed Audit three months post implementation Care provided was appropriate and responsive. There were clear risk assessments and treatment plans Nil Process developed to monitor crisis phone log An anonymous and vague call was left on the crisis team’s answer-phone. The call did not identify either the patient or the caller Establish a consistent response for the crisis team when they receive calls with insufficient information Fractured hip following fall in the rehabilitation unit Patient a recognised as a high falls risk Falls injury prevention care plan reviewed to ensure they reflect best practice Underwent surgical repair, hip wound became infected, patient died of sepsis three weeks later All aseptic procedures/ processes adhered to Nil No hospital-wide falls standard Whanganui DHB falls policy and standard be updated to reflect best practice Suicide of a community mental health patient, known to the service within seven days Patient seen regularly and compliant with treatment adhered to relapse and recovery plan at all times. No identified triggers or causes for concern Suicide of a community mental health patient, known to the service within seven days Completed and in the process of implementation Completed and in the process of implementation Falls care plan did not reflect best practice Nil DHB Summary of Serious and Sentinel Event Report 2009/10 38 Hawke’s Bay District Health Board Hawke’s Bay Serious or sentinel Serious Event code* (see codes below) 4D Serious* 1 Serious* 4B Sentinel 2 Serious 4B Sentinel 6 Description of event Review findings Recommendations/actions Throat injury following endoscopy procedure Undiagnosed and unsuspected pharyngeal pouch Frail patient with multiple co-morbidities Rare but recognised complication of endoscopy – patient required intensive care Review pre-operative assessment processes (determine whether the patient has any difficulty with swallowing. If positive, barium swallow to be undertaken) Internal audit Wrong site surgery Fusion of cervical spine 6–7 rather than cervical spine 5–6 Misinterpretation of X-rays on lateral views Perform multiple view X-rays to enable clear visualisation of anatomy Surgical audit in progress Intra-uterine infection (Group B Strep). Not sensitive to antibiotics given Transferred to tertiary care after successful resuscitation. Patient did not progress and subsequently died. Swabs taken two days prior to delivery not checked. Identify and communicate antenatal and social risk factors. Review systems to check laboratory results. Policy reviewed. Referral forms standardised. Communication pathway established between Laboratory Technicians and Lead Maternity Carers. Suicide of mental health outpatient within seven days of contact with service Good engagement with patient, family, psychiatrist and staff Recommendation from investigation related to administrative processes The processes do not contribute to or have the ability to change outcome Clinical leaders conduct regular file reviews both electronic and hard copy files. Results shared at meetings Undiagnosed brain aneurysm Failure to diagnose a cerebral aneurysm on MRI scans resulting in a delay in arranging treatment Establish a process to seek a second opinion (internal or external) where a high risk of a positive result is indicated Implemented Inpatient fall resulting in brain injury and death Frail, elderly patient with confusion Identified as a “falls risk” All reasonable steps were taken to manage and minimise the risk of suffering a fall Patient died in hospital five days later No recommendations Falls management project in progress Incidental findings: Documentation and filing did not meet health record standard requirements Follow-up External opinion obtained DHB Summary of Serious and Sentinel Event Report 2009/10 39 Hawke’s Bay District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Sentinel 2 Suicide of mental health outpatient within seven days of contact with service Self-presentation to crisis assessment and treatment team Clinical and risk assessment completed Management plan confirmed, no immediate safety risk identified Coronial investigation completed Care in accordance with best practice No recommendations from review or coronial inquiry Sentinel 2 Suicide of mental health outpatient within seven days of contact with service Expert advice and service provided by other DHBs High risk client. Care well documented Risk management plan in place Regularly assessed by key staff Coronial investigation completed. Injuries sustained intentionally selfinflicted Care review consistent with best practice No recommendations from review or coronial inquiry Sentinel 2 Suicide of mental health outpatient within seven days of contact with service Commenced on anti-depressants 14 days prior to death No evidence of comprehensive assessment to identify changing mental state or relevant crisis management or risk plans All staff to comply with health records standard and DHB documentation policies Review of alcohol and drug service Implement national competencies for mental health practitioners for the management of dual diagnosis Follow-up Terms of reference for audit of alcohol and drug files completed Audit scheduled In progress *Coding has been changed since initial publication. DHB Summary of Serious and Sentinel Event Report 2009/10 40 MidCentral District Health Board MidCentral Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4A Fracture of hip undiagnosed for several days resulting in additional days in hospital Lack of progress/improvement not recognised Standard orthopaedic physical examination Strengthen multidisciplinary team communication In progress Serious 4B Post partum haemorrhage resulting in blood transfusion and surgical procedure Delayed recognition of post partum haemorrhage due to lack of formal clinical handover Strengthen clinical handover procedure Review policy on student supervision In progress Sentinel 4B Delay in treatment potentially contributing to death The seriousness of the patient’s condition and deterioration not recognised early Adherence to completion of early warning score (EWS) in ED and regular audits Strengthen SMO supervision In progress Serious 5 Unusually high dose of medication administered over several days Medication prescribed incorrectly and not recognised for several days Continue implementation of medication reconciliation across organisation Develop an annual education plan for all clinical staff In progress Serious 8 Attempted to leave secure area in mental health for older people facility resulting in injury to leg with full recovery Inadequate risk assessment Refocus mental health risk assessment process Review and adapt physical environment In progress Sentinel 4C Delayed response to deterioration potentially contributing to death Placement options within a high dependency area or intensive care unit not readily available Review intensive care unit guidelines for admission Strengthen communication between critical care services In progress Serious 4B Delay in providing intravenous fluid hydration leading to transfer to intensive care unit Not managed in the specialty service relating to the patient’s diagnosis with consequence of delayed recognition of needs Strengthen process of oversight of patients who are located in other specialty services rather than the one that relates to their diagnosis Completed Sentinel 4B Baby born early Assessment of gestational age not completed potentially contributing to death of baby Inadequate nursing handover Limited knowledge on management of women in early labour in ED Strengthen nursing handover process Develop a clinical pathway for preterm labour and pregnancy loss In progress DHB Summary of Serious and Sentinel Event Report 2009/10 41 MidCentral District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 3 Retained swab following surgical procedure leading to further surgical procedure for removal of swab Count incorrect Review and reinforce swab counting policy Familiarisation sessions regarding policy and procedure for all staff Completed Serious 1 Intravenous line inserted in wrong patient. No health impact Formal identification of patient not undertaken Reinforce informed consent process Develop recording system for all acute referrals Standardise patient location terminology In progress Serious 5 Medication prescribed and administered despite allergy being noted Resulted in patient being monitored in high dependency area overnight Procedure on administration of medication not clear with regard to use of alert stickers Policy on abbreviations not adhered to Review medication administration procedure Provide update on use of abbreviations In progress Serious 6 Fall whilst an inpatient resulting in fracture of hip No recommendations Serious 6 Fall resulting in fracture of hip with increased days in hospital All patients had been appropriately assessed for risk of falls and all appropriate measures had been put in place for all patients Serious 6 Fall whilst an inpatient resulting in fracture of arm Serious 6 Fall whilst an inpatient resulting in fracture of wrist A falls risk pilot is in progress to determine a greater level of detail on contributing factors for falls. Based on the outcome of this pilot a falls prevention strategy will be developed Serious 6 Fall whilst an inpatient leading to fracture of arm Serious 6 Fall whilst an inpatient resulting in fracture of arm Serious 6 Fall whilst an inpatient resulting in fracture of hip DHB Summary of Serious and Sentinel Event Report 2009/10 42 Wairarapa District Health Board Wairarapa Serious or sentinel Event code* (see codes below) Description of event Review findings Serious 6 Inpatient fall resulting in fractured hip, requiring surgery Patient was documented as falls risk and precautions identified Serious 6 Inpatient fall resulting in fractured hip, requiring surgery Unanticipated fall, low falls risk Patient tripped Sentinel 2 Sentinel 2 Suicide of a community mental health patient within seven days of contact Root cause analysis (RCA) review was performed – no preventable factors found, although some opportunities for improvement were identified Recommendations/actions Follow-up No recommendations which would have prevented this incident as process had been followed however it was reviewed as part of the falls management group Both investigations identified the opportunity for improved primary/secondary/NGO mental health services communication and collaboration. Project under way to address this Internal investigations completed but still awaiting coronial decision DHB Summary of Serious and Sentinel Event Report 2009/10 43 Hutt Valley District Health Board Hutt Valley Serious or sentinel Serious Event code* (see codes below) 6 Description of event Inpatient fall resulting in fracture of upper arm Review findings On admission, the patient’s risk of falling was noted to be low The initial injury noted was a skin tear Recommendations/actions Follow-up Following the fall and injury, the patient’s falls risk assessment was upgraded to 15 minute observations and the patient was encouraged to seek assistance when mobilising We have reviewed the sloping floors in the bathrooms, ensuites and showers in the ward the patient was in and other wards with the same features. Our maintenance schedule now includes a plan to remove all existing slopes Project under way to ensure ongoing hospital-wide focus on falls prevention Serious 6 Inpatient fall resulting in fracture of hip Patient sustained a minor fall on the previous day. The patient’s falls risk assessment was reviewed, patient was encouraged to seek assistance when mobilising and the call bell was repositioned close to the patient Following the second fall, the patient’s falls risk assessment was upgraded from moderate to high and placed on 15 minute observations Project under way to ensure ongoing hospital-wide focus on falls prevention Sentinel 6 Inpatient fall resulting in fracture of thigh bone, requiring surgery Patient died 14 days later following a post-operative complication of pneumonia Inpatient fall resulting in fracture. High risk of falling identified on admission Fracture required surgery Surgery successfully completed Patient’s condition deteriorated post-operatively Patient died 14 days after the fall occurred Falls incidence and prevention is a standing agenda item at ward meetings A review of tasks involved in 15 minute patient checks is under way Project under way to ensure ongoing hospital wide focus on falls prevention Sentinel 5 Patient with history of stomach ulcer prescribed non-steroidal antiinflammatory drug Patient re-presented to ED with stomach ulcer bleed and subsequently died Patient was treated for the initial bleeding stomach ulcer, but developed further bleeding and later died Policy implemented in emergency department to ensure safe prescribing of non-steroidal antiinflammatory medications to elderly patients Education of clinical staff in the emergency department on the policy has occurred through the clinical head of department DHB Summary of Serious and Sentinel Event Report 2009/10 44 Hutt Valley District Health Board Serious or sentinel Serious Event code* (see codes below) 4E Description of event Endoscopy service cluster of patients with delayed diagnostic procedures: A group of patients referred for endoscopy have been booked for procedures outside national guidelines for waiting times Serious 4D/4B Patient’s heart damaged during insertion of chest drain Patient made full recovery Review findings Recommendations/actions Follow-up Internal reviews under way on individual cases and causes for this cluster as a whole; three patients identified to date with cancer diagnosis: Discrepancy found on Ministry of Health website with two sets of national guidelines for triage times. MoH notified of discrepancy. Hutt Valley DHB has now developed and implemented its own set of guidelines for triaging of patients Extensive review of endoscopy waiting list identified patients outside of wait times recommended by new guidelines. Additional capacity to provide procedures to patients found to be outside guidelines was commissioned by adding extra sessions within HVDHB endoscopy unit, contracting colonoscopy procedures to an external provider, and recruiting 0.5 full-time equivalent (FTE) additional endoscopy specialist All three patients have been directly contacted and an apology offered for the delay in being seen For Patient C an external review was undertaken and the results shared with the patient Monitoring of compliance with national guidelines ongoing Backlog fully cleared by 20 December 2009 Patient A: Following initial triage, the patient was to be seen within three months but was seen after 6½ months Diagnosed with cancer, currently undergoing treatment Patient B: Following initial triage, the patient was seen 26 days outside guidelines Diagnosed with cancer, and commenced palliative treatment (deceased) Patient C: Following initial triage the patient was to be seen within three months but was actually seen nine months later Diagnosed with cancer, currently undergoing treatment Enlarged heart size made the fluid look larger than it was X-ray was taken two weeks prior and no other imaging undertaken Exact location of drain not obvious from documentation Clinical review completed Recommendations: That a recent chest X-ray is undertaken prior to the procedure and is viewed prior to and during the procedure That advice is sought from the respiratory physician if clinically indicated That the informed consent process is clearly documented in the clinical record Attendance at teaching and training sessions for medical staff is recorded All recommendations communicated to medical staff as part of ongoing education following clinical review DHB Summary of Serious and Sentinel Event Report 2009/10 45 Hutt Valley District Health Board Serious or sentinel Serious Event code* (see codes below) 4B Description of event Health-care acquired pressure ulcer requiring surgery Review findings Clinical review complete Areas of concern raised: Ability of junior nursing staff to assess skin and general condition of complex patients on admission, and in the event of their health status changing Skin assessment tool did not reflect other complications Recommendations/actions Follow-up Recommendations: Junior nurses to be up-skilled in patient assessment process Visual skin assessment to be included in patient notes Service to develop guidelines with support from Pacific and Maori health units, and disability advisor for use when family/caregivers wish to be involved with care Action plan for service in place and all recommendations being progressed Serious 6 Inpatient fall resulting in fractured shoulder Patient presented to ED following a fall at home While in ED, patient tried to move from trolley to chair unassisted, and fell Staff members in ED have been reminded about the importance of increased monitoring of patients who attend ED with a history of falling Changes to the new facility currently under way will increase visibility of patients awaiting treatment Project under way to ensure ongoing hospital wide focus on falls prevention Serious 6 Inpatient fall resulting in fracture to pelvis The patient had been assessed as a moderate falls risk on admission. Inpatient fall occurred Falls risk was upgraded to high, which resulted in increased observation and monitoring of the patient for remainder of stay Education of staff on falls prevention strategies is ongoing Patients at risk of falling have a red flag placed outside their cubicle to alert staff Project under way to ensure ongoing hospital wide focus on falls prevention Serious 3 Retained swab following surgery Patient underwent further surgery to remove swab Contributing factors found to be: communication between staff; orientation of new staff to the procedure; unfamiliarity with theatre policies. Swab count policy to be reviewed and updated with recommendations from event review Surgical team brief undertaken before commencement of surgery to enhance team communication Updated the orientation programme to support new staff An additional scrub nurse in place to support new staff Action plan will continue to be updated and reviewed by clinical manager of operating theatre DHB Summary of Serious and Sentinel Event Report 2009/10 46 Capital & Coast District Health Board Capital & Coast Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 9 Assault by client on another client who required surgery as a result Both clients were reviewed by their treating teams and cared for in separate areas Review identified that a violence management team review may have assisted decision making and management plan development Review recommended the role of the violence management team be promoted within the service and clear staff guidance for notifying Police of inpatient assault events be made available Client issues resolved as above The role of the violence management team was publicised across the directorate and guidance provided to staff Action plan complete Sentinel 4C/E Recommended surveillance of a patient’s condition did not occur due to a breakdown of the recall system The patient re-presented with metastatic cancer some years later Review invited GP involvement Review identified the need for clarity regarding criteria and process for surveillance Review recommended instituting a service electronic recall system, clarification of responsibility for surveillance between specialist and GP on case by case basis and agreement of service guidelines to formalise assessment of a patient’s suitability for surveillance Meetings held with family and GP and report provided to both parties Paper-based surveillance system implemented to mitigate risk Action plan complete Sentinel 2 Suicide of community mental health client within seven working days of being seen Review invited input from family Review found that overall care met expected standards Review identified some aspects of care that could be improved that did not relate to the outcome and recommended that these be fed back to staff and that the issue of multiple copies of information in files be reviewed Report provided to family Feedback provided to staff and relevant audit added to schedule Risk register updated regarding multiple copies of information in files – in addition electronic health record enhancements currently being implemented will reduce reliance on hard copy documentation Action plan complete Sentinel 2 Suicide of community mental health client within seven working days of being seen Review invited input from the family The review team found that care prior to this presentation was of an adequate standard but considered that during the acute presentation only a limited assessment of risk occurred due to a number of factors Review recommended improvement of regular review processes for community mental health clients, suicide risk assessment and information for families where a member has died by suicide Report provided to family All actions are in progress, ie, review processes for community mental health clients are being improved, suicide risk assessment training for the crisis assessment and treatment team (CATT) staff is in progress and information for families is in development DHB Summary of Serious and Sentinel Event Report 2009/10 47 Capital & Coast District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4F Patient follow-up appointment for one month after hospital discharge did not occur Patient presented acutely unwell with advanced tumour some months later Review found that ordered followup did not occur due to a breakdown in follow-up booking process The review team were not able to identify the cause of the breakdown Review recommended provision of the report and an apology to the patient’s family and review of the process for followup and improvement and strengthening of the follow-up system Meeting held with family and report provided Electronic internal referral form implemented Work is in progress to develop a system for patients concerned about appointments to have a clear point of contact Sentinel 2 Suicide of community mental health client within seven working days of being seen Review report in development and almost complete Serious 4A/C/D Care plan timeframe exceeded during trial of labour after previous caesarean section Patient deteriorated Uterine rupture occurred Surgical repair required There was no adverse outcome for the baby Review found that the decision to proceed with a trial of labour was reasonable and care was appropriate based on clinical information available at the time Some staff had not been oriented to the relevant policies regarding care during trial of labour Review recommended review of policy for inconsistencies and staff orientation improvements Report provided to family Action plan reviewed and timeframes and responsibilities agreed Actions in progress Serious 4G Prolonged second stage labour Infant required neonatal intensive care admission for asphyxia Review found that while there was prolonged second stage of labour it was not possible to identify a specific cause of the asphyxia Review recommended clear communication of the plan after clinical review – using the ISBAR-identify, Situation, Background, Assessment, Request tool, provision of information and education of staff re monitoring in second stage labour and monitoring and recording of foetal heart rate Report provided to family The need for clear communication of the plan using the ISBAR tool has been reinforced Registrar orientation has been updated, a newsletter to raise staff awareness has been circulated and technical skills training updated action plan complete Serious 6 In-patient fall resulting in fractured hip – required surgery Review found the fall occurred without warning when relevant falls risk management strategies were in place including nursing staff supervision of patient The event did not occur as a result of a deficiency in systems or processes of care The review made no recommendations Report provided to family DHB Summary of Serious and Sentinel Event Report 2009/10 48 Capital & Coast District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 12 Bone marrow transplant patient developed sepsis Required intensive care unit admission. Patient deceased Review found that overall care provided to this patient was of a good standard and that an infection developed at the site where finger prick for blood glucose sampling had occurred Review identified that no guideline for monitoring blood glucose levels in neutropenic patients exists in New Zealand or internationally Review recommended development and implementation of guidelines for monitoring blood glucose levels in neutropenic patients Report provided to family, follow-up meeting with family scheduled Work is in progress on organisationwide and area-specific guidance related to blood glucose sampling practice Serious 4G Significant birth weight loss in newborn under care of primary midwifery team Infant readmitted due to seizures Review found overall care provided was good Shortfalls were identified in inhospital review of feeding, output and discharge check Weight assessment on home visit was not validated Review recommended improvement in midwife education, new policy and improved handover Report provided to family Quarterly study days implemented and ongoing, policies updated and new process for communication of neonatal paediatric checks implemented Action plan complete Sentinel 2 Death of client of mental health services in community Review team information gathering complete Review report in development Serious 4A/C Delayed recognition of maternal deterioration Mother required intensive care admission and care Baby delivered by caesarean section The mother recovered well There was no adverse outcome for the baby Review found that earlier use of the MEOWS-Modified Early Obstetric Warning Score tool would have highlighted maternal deterioration at an earlier stage but review was unable to quantify if this would have altered the course of events Recommendations include reintroducing the MEOWS tool, the ISBAR tool and the advanced monitoring chart to staff Report provided to family Action plan reviewed and timeframes and responsibilities agreed Actions in progress Sentinel 4D Patient deterioration subsequent to chest drain insertion and drainage of plueral effusion Patient required intensive care admission. Patient deceased Review found that risk factors were considered in the decision to undertake the procedure, that care was appropriate including when the patient deteriorated Recommendations include consideration of adoption of British Thoracic Society guidelines in relation to correction coagulation pre procedure and an incidental recommendation regarding consideration of ultrasound prior to plueral aspiration in non-urgent cases Meeting with family held Timeframes and responsibilities for action plan are in process of being confirmed DHB Summary of Serious and Sentinel Event Report 2009/10 49 Capital & Coast District Health Board Serious or sentinel Event code* (see codes below) Serious 6 Serious Description of event Review findings In-patient fall resulting in fractured hip. Surgery required Review found that comprehensive falls risk assessment was not completed 4G Post mortem and histology on miscarriage tissue remains was not able to be completed due to process failure Review report in development and almost complete Serious 4G Histology and the return to family of miscarriage tissue remains was not able to be completed due to process failure Review report in development and almost complete Sentinel 2 Suspected suicide of community mental health client within seven working days of being seen Review commencing – file review in progress Recommendations/actions Recommendations related to increasing equipment, education focus on staff falls awareness and administration process change Follow-up Additional equipment purchased and installed, staff education plan completed Patient falls risk assessment tool added to all patient files and ongoing audit implemented Action plan complete DHB Summary of Serious and Sentinel Event Report 2009/10 50 Nelson / Marlborough District Health Board Nelson / Marlborough Serious or sentinel Sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up 4A/C A patient presented to ED with severe pain and apparent vomiting She was HIV positive with diagnosed shingles She was discharged and returned to ED later that day when she was admitted. She died soon after admission The severity of disease was initially under-estimated and nursing observations were not taken as part of the triage process Due to language difficulties, the history was poorly communicated The patient left the department without discharge advice Patients presenting to ED should have a full set of observations performed as part of the triage process Implemented Improve ED triage nurse training Implemented ED staff should be reminded of the process to call interpreters and use of communication cards Implemented Ongoing staff education on the recognition of sepsis Implemented Install a sign reminding patients to check they have discharge advice before leaving the department Implementation commenced DHB Summary of Serious and Sentinel Event Report 2009/10 51 West Coast District Health Board West Coast Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 2 Suicide of an outpatient known to mental health within seven days of last contact with service Review and coroner’s inquest still ongoing Review and coroner’s inquest still ongoing N/a Sentinel 2 Suicide of an outpatient known to mental health within seven days of last contact with service Review and coroner’s inquest still ongoing Review and coroner’s inquest still ongoing N/a Serious 4A Long-stay patient complaining of right shoulder pain was found to have undiagnosed dislocation Review still ongoing Review still ongoing N/a Serious 6 Inpatient fall resulting in fracture All relevant West Coast DHB policy had been complied with by staff Consideration by staff of improved communication – has been actioned through implementation of ISBAR communication tool N/a DHB Summary of Serious and Sentinel Event Report 2009/10 52 Canterbury District Health Board Canterbury Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 2 Possible suicide of a mental health inpatient whilst absent without authorised leave Patient’s last contact with the service was within seven days Inadequate handover processes between outpatient and inpatient services Lack of workable plan to prevent unauthorised leave The development of formal structured handover systems Development of an effective operational system to prevent patients from leaving the hospital without authorisation Action complete Sentinel 2 Death of a mental health service patient on home leave Patient assessed as low risk and had on previous occasions been on home visits Introduction of a revised risk management protocol for inpatient home leave including the triggers for re-evaluation of risk, and supporting documentation and communication Action under way Serious 3 Retained surgical instrument in patient following surgery Root cause analysis review completed Report in draft stage Sentinel 4D/E Patient death following a series of bowel preparations for colonoscopy, which had been delayed due to the patient’s anticoagulant blood level being too high The treatment guidelines to reduce the patients anticoagulant blood level did not attain the desired result Variations in the way patient weight on admission and ongoing weights are recorded Ongoing bowel preparation resulted in unrecognised fluid imbalance Absence of consistent bowel preparation protocols Incomplete adoption of the early warning score (EWS) and associated management pathway Daily weight be included as part of standard fluid balance monitoring Reinforcement of assessment and management of fluid status for staff That the protocol for urgent reversal of anticoagulation be reviewed That the protocols for colonoscopy bowel preparation be updated That the EWS be recorded and pathways followed That the process for rebooking endoscopies be reviewed to address the risk of sequential cancellations Sentinel 4A Potentially avoidable lower limb disability (neurological) related to delayed diagnosis Root cause analysis under way Report awaited Sentinel 4A/E Death of a baby from extensive bowel tissue death precipitated in part by a strangulated hernia Root cause analysis under way Report awaited Serious 4A/E A lesion diagnosed as containing a cancer was not noted until several months after its removal Root cause analysis under way Report awaited Actions under way DHB Summary of Serious and Sentinel Event Report 2009/10 53 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Sentinel 4B Inpatient death following delayed cardiac surgery Root cause analysis review complete Report in final draft format Sentinel 4B Death of a patient with reduced immunity following a delay in antibiotic administration Inadequate processes for the recording of telephone referrals to ED and internal communication of this information Review of communication processes to be undertaken Serious 4B Extended illness of a patient with reduced immunity following a delay in antibiotic administration Root cause analysis under way Report awaited Sentinel 4B/C Death following delay in recognising the deteriorating patient Training needs in relation to the unstable patient Incomplete adoption of the EWS and associated management pathway Lack of formal handover processes That the EWS be recorded and pathways followed That the EWS be promoted and reinforced to all staff That the business case for additional surgical progressive care unit beds be progressed Training in relation to the recognition and management of the unstable patient Development of more formal structured handover systems Sentinel 4B/C/F Stroke following delay in achieving optimal anticoagulation Root cause analysis under way Report awaited Sentinel 4C Extended illness following delay in recognising the deteriorating patient Root cause analysis completed Report in final draft format Sentinel 4D Anaesthetic difficulties prior to an emergency caesarean Baby injured through lack of oxygen with expected moderate disability Root cause analysis under way Report awaited Serious 4D Post partum haemorrhage following a caesarean section necessitating further surgery and intensive care Root cause analysis indicated that this event could not have been anticipated No actions necessary Follow-up Actions under way DHB Summary of Serious and Sentinel Event Report 2009/10 54 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4D The tip of central venous catheter penetrated into the plueral space resulting in a volume of fluid infusing into the plueral cavity The patient required intensive care and later died No preventable causal factors identified Consideration be given to the development of a multi-disciplinary care plan for the management of Hickman lines and Infusaports/Portacaths Action under way Sentinel 4D Procedural related death of a patient undergoing a placement of an arterial stent Root cause analysis under way Report awaited Sentinel 4B/C Stillbirth following delay in transfer of mother to hospital during labour Variation in interpretation of intrapartum cardiotocography tracings and problems in separating maternal from foetal pulse Education for staff regarding the importance of distinguishing between maternal and foetal pulses Actions under way Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Lack of an explicit process for updating, managing and handing over ongoing risk Safety checks in the event of attempted self harm not undertaken The risk assessment and management process to include risk review and updates during treatment progress and handover practices Information regarding evaluation of patients who have attempted self-harm has been circulated to staff Actions under way Serious 11 Mental health inpatient self harmed whilst absent without leave Patient’s mental state required use of the Mental Health Act and locked unit status Communication failure between admitting team and hospital staff regarding risk status of patient Team involvement and risk assessment and management to be emphasised Handover to hospital staff should accurately reflect clinical conclusions The importance of joint risk assessment/ management between medical and nursing staff Actions complete DHB Summary of Serious and Sentinel Event Report 2009/10 55 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 11 Mental health patient upon discharge refused to leave the building and was removed by Police Patient later readmitted with injuries apparently sustained whilst being removed from the facility Diagnostic difficulties for treating teams Handover between teams was not complete Discharge planning was not clearly documented Rationale for seclusion use varied That clinical teams are reminded of the established complex case conference process in the assessment and management of consumers whose clinical state causes dilemma among a number of clinicians That clinical teams be reminded of the importance of comprehensive handovers between shifts and teams To develop a process to be followed after a case conference. Ensure discharge planning is included in the treatment plan and documentation meets set standards All staff adhere to the seclusion policy – seclusion events require monitoring, review and evaluation to inform best practice Actions complete Sentinel 4A/B/C Pregnant woman involved in motor vehicle accident Whilst in ED there was delay in managing the foetal distress. Still birth delivery Complexities in initiation and organisation of an emergency caesarean section from a department other than maternity Communication systems for contacting key health professionals Review of the process for emergency caesarean section when originating from a hospital department outside maternity Additional communication systems to contact staff in an emergency Nil Serious 11 Mental health inpatient gained access to the unit’s roof (single story building) and fell resulting in a fracture requiring surgical intervention A treatment plan review required Access to the roof required review Treatment team to review the current treatment plan with the patient Undertake a review of the building roofline to prevent future patient access Actions complete Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days No preventable causal factors identified No recommendations Nil Sentinel 12 Death of a patient following hospital acquired gastroenteritis (norovirus) causing aspiration pneumonia No preventable causal factors identified Continued programme to limit the risk of transfer of infection in facilities including a focus on hand hygiene Nil DHB Summary of Serious and Sentinel Event Report 2009/10 56 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Possible suicide of a mental health inpatient while on arranged leave Variation in staff interpretation of “no leave” status Alternatives to seclusion were not considered Variation in clinical review processes and inadequate documentation Clarification of what “no leave” status means has been provided to all staff Staff reminded of seclusion policy and the requirement to exhaust all alternatives prior to the use of seclusion Information arising from weekly multidisciplinary team clinical review is documented and entered directly onto the electronic record Actions complete 4B Anticoagulation may have contributed to a post trauma death There was no information about the patient’s participation in a study of a new anticoagulant drug in the patient management system Inability to contact the drug study co-coordinator That relevant information about research studies be placed on the patient information system The Multi-region’s Ethics Committee be advised of the findings of the event Actions under way Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Root cause analysis under way Root cause analysis report being finalised Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Root cause analysis under way Report awaited Sentinel 2 Possible suicide of mental health outpatient Patient’s last contact with the service was within seven days No preventable causal factors identified No recommendations Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days The risk assessment and management process was not systematically documented within a framework to inform a risk management plan Clinical documentation to be more robust, systematic and centralised with regard to risk planning and management Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Root cause analysis review under way Report awaited Sentinel 2 Sentinel Actions under way DHB Summary of Serious and Sentinel Event Report 2009/10 57 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Root cause analysis review under way Report awaited Sentinel 2 Possible suicide of a mental health outpatient Patient’s last contact with the service was within seven days Root cause analysis review under way Report awaited Serious 6 Inpatient fall resulting in a fractured pelvis Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall sustaining a dislocated hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured femur Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured femur Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured pelvis Serious 6 Inpatient fall resulting in a fractured pelvis Serious 6 Inpatient fall resulting in a dislocated hip The clinical board is providing a leadership role to progress work in falls management with the vision of having zero harm from falls. All falls are subject to a root cause analysis (RCA) review, the learnings from which contribute to the overall clinical board-led falls initiative. Key activities and initiatives in this area include those detailed below: A forum was held in May to bring key front line staff and leaders together. All the ideas raised have been captured in an action plan A fall event notification sticker has been designed to make falls more visible in the clinical record and reinforce the heightened “falls risk” of individual patients to staff Patient safety crosses and ward location maps are being used to display information regarding the number of falls in an area. This was undertaken to heighten the awareness of the impact of falls Patient safety walk rounds have commenced. These provide an opportunity for frontline staff to have conversations with clinical board members about their concerns, successes and ideas for improvement regarding patent safety A falls campaign is being run in Genr8 to help us share ideas on how we can achieve a goal of zero harm from falls. Genr8 is a website where anyone can lodge an idea and add comments and suggestions An intranet page has been established so that people can find out more about the clinical board-led patient falls initiative A model for the continued delivery of the Otago Exercise Programme (OEP) in the Canterbury region has been developed following the withdrawal in December 2009 of ACC funding. The Canterbury DHB (CDHB) has contracted with ACC accredited physiotherapists across Canterbury to provide an enhanced version of the OEP to the frail elderly in our region. CDHB will pay a co-payment to allow this physiotherapist-led service to be delivered in people’s homes for the next six months. The service remains free of charge to the frail elderly. The Canterbury clinical network has also funded an educational position for a physiotherapist to develop a comprehensive evidence-based falls prevention training programme available to all primary care physiotherapists Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip DHB Summary of Serious and Sentinel Event Report 2009/10 58 Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall displacing a previous fracture Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fracture Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Inpatient fall resulting in a fractured hip Serious 6 Outpatient fall resulting in a fractured hip Review findings Recommendations/actions Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 59 South Canterbury District Health Board South Canterbury Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4D Patient had the wrong size hip implant component inserted during surgery Further surgery required to replace incorrect hip implant Misinterpretation of the previous operation note by the surgeons performing the surgery Format of the operation note to be reviewed with implant components used to be clearly referenced Action plan developed and monitored Serious 6 Inpatient fall resulting in a fractured hip Fracture surgically repaired Patient fell while attempting to go to toilet Risk of falls was assessed appropriately as a low risk Serious 6 Inpatient fall resulting in a fractured hip Surgery not required but patient had a longer stay in hospital Patient slipped on wet floor while showering Assessed as not at risk of falling on admission Serious 6 Inpatient fall resulting in a fractured hip Fracture surgically repaired Patient fell while showering Patient independent with mobilising Fall prevention and management programme under development and due to be launched 20 September Programme includes: Revised falls risk assessment tool Action plan for patient identified as a falls risk Green wrist bands for identified patients Standardised symbol for patient status at a glance board Staff education on the new programme Serious 6 Inpatient fall resulting in a fractured ankle Sustained a fractured ankle Surgery not required but patient had a longer stay in hospital Patient found on floor, assumed to have fallen Falls risk assessment completed on admission Patient was assessed as being safe to sit in normal chair No indication as to what caused this fall Serious 6 Inpatient fall resulting in a fractured hip Fracture surgically repaired Patient fell while returning from toilet Patient admitted for assessment of reduced mobility, falls and confusion Falls risk assessment completed but no care plan or interventions in place Serious 6 Resident fall resulting in a fractured hip Fracture surgically repaired Dementia hospital level care resident fell while getting up from chair Falls assessment completed and assessed as high risk Restraint not considered appropriate so cared for by close staff observation DHB Summary of Serious and Sentinel Event Report 2009/10 60 South Canterbury District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Serious 6 Inpatient fall resulting in a fractured hip Fracture surgically repaired Patient fell returning from toilet Falls risk assessment completed No falls care plan in place aside from patient being nursed in a room close to the care station Serious 6 Inpatient fall resulting in a fractured hip Patient not suitable for surgery so treated with bed rest Patient admitted with a history of falls Falls care plan in place including use of appropriate aids Recommendations/actions Follow-up DHB Summary of Serious and Sentinel Event Report 2009/10 61 Otago District Health Board Otago Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 6 Inpatient fall resulting in a fractured wrist requiring treatment Patient attempted to mobilise independently without alerting staff to provide the necessary supervision The falls assessment tool may not have addressed the patient’s level of risk appropriately New falls prevention programme has been introduced with new strategies for staff education on the prevention of patient falls The falls prevention programme has been rolled out and audits continue to make improvements and monitor progress Sentinel 4D Patient death due to a rare complication following a biopsy procedure in the radiology department Although complete consent process was followed this was not documented accurately on the consent form In hindsight communication regarding treatment options could have been more comprehensive Those obtaining consent are to be vigilant in completing the documentation in full surrounding the consent process A fuller outline of the options, likely treatment course and outcome, be made available to the patient A new surgical consent form has since been developed Sentinel 4D Patient death due to severe respiratory failure and known difficult airway who needed emergency surgery, but who had decided against alternative management options for their airway No concern with care or management of patient and no problems with personnel, equipment or facilities Planning and preparation of the case was of a high standard No recommendations identified Not applicable Sentinel 2 Suicide of a community mental health client more than seven days since contact with the service Community teams documentation could have been more comprehensive Review systems supporting GP authority, particularly ensuring GP liaison and documentation is consistent with the treatment planning service provision framework including a six-monthly review Clinical documentation audits covering key aspects of patient care have been developed and continuous audit process implemented to ensure documentation meets national standards Sentinel 2 Suicide of a community mental health client more than seven days since contact with the service The community mental health team were not aware of the patient’s access to a firearm Lowering the threshold for face-toface contact to ensure it occurs in a timely manner That the DHB and mental health and intellectual disability (ID) service as a matter of routine enquire whether a consumer has access to a firearm That a review is conducted of the case manager role in facilitating face-to-face contact within seven days of discharge from an inpatient ward Education provided to community mental health teams relating to increase in risk associated with weapons Prompt has been included on the assessment form for staff to ask routinely if the consumer has access to weapons DHB Summary of Serious and Sentinel Event Report 2009/10 62 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 4D Patient death during therapeutic diagnostic procedure of the gall bladder/pancreas due to a rare complication A rare but recognised risk associated with this type of procedure Two audits of clinical practice completed Detailed surgical audit and a detailed endoscopy team audit completed Following the endoscopy audit the patient information sheet for this procedure has been revised Sentinel 2 Suicide of a community mental health client within seven days of contact with the service Final report in progress Serious 11 Patient self harm requiring surgical intervention General ward nursing staff unaware that once the patient was under the Mental Health Act that there would be mental health nursing resource made available Delays getting assistance due to internal telecommunication fault Education for ward staff about patients under the Mental Health Act and their responsibilities subsequent to this Communication to be widely circulated to all medical/surgical wards when psychiatric registrars are unavailable that the emergency psychiatric service should be contacted at this time Education provided and staff now aware of who to contact in this type of emergency Serious 6 Patient fall in an outpatient clinic resulting in fractured hip requiring surgery No recent falls prevention education for nursing staff in this outpatient area No signage to indicate patients with difficulties with mobilisation should use the high-legged chairs to make standing up a safer procedure Department will receive falls prevention programme education Evaluate waiting room and clinic areas to make sure access is optimised for those with decreased mobility Falls education has now been provided to the area and the waiting room has been changed to enhance mobility compromised patients safety Sentinel 2 Suicide of a community mental health client more than seven days since contact with the service This patient received a high standard of care Documentation issue in recording the patient’s therapeutic blood test and changes of care in the treatment plan Clinical staff be reminded (via line management) that the therapeutic blood test should be monitored and recorded according to guidelines Clinical staff be reminded to document all patient contact, changes in care, objectives, etc, in the clinical record, including termination of care planning in the treatment plan Medicines management audit developed to ensure medication optimally monitored Regular audit regime implemented DHB Summary of Serious and Sentinel Event Report 2009/10 63 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Patient stroke during catheterisation of an artery, diagnostic procedure A recognised complication of this kind of interventional procedure The patient required rehabilitation Review the pink form named “Day Surgery Vascular Consent and Preparation” with possibility of adding tick box “observations within parameters” or similar to indicate if the observations are within normal limits for the patient The Day Surgery Vascular Consent and Preparation form has been updated with the patient’s blood pressure having to be recorded in the examination section and a prompt in the medical checklist to escalate if the patient’s systolic blood pressure is greater than 200mgHg Serious 4D Serious 6 Inpatient fall associated with a subdural haematoma The patient was disorientated and moving independently without a walking frame or one-person assistance to mobilise safely and subsequently fell Regular offering of toilet and checking for assistance throughout night when patients are high falls risk and confused Regular re-orientation for the patient to the ward and environment Continued audit occur to ensure that the falls prevention programme is being utilised Strategies implemented to reduce falls as per the falls prevention guidelines Sentinel 2 Suicide of a community mental health client within seven days of contact with the service Documentation issues relating to clinical assessment and detailed recording of discussions involving risk related decisions in patient care All clinical assessments be typed for legibility and composed in such a manner that they provide useful, comprehensive and up-to-date patient information. (Typing of documents suggested as ideal, rather than compulsory) Where risk-related decision of patient care this is documented in the patient’s file Clinical documentation audits covering key aspects of patient care developed and continuous audit process implemented to ensure documentation meets national standards Sentinel 1 Wrong patient taken for procedure in day surgery, however patient underwent the correct surgical procedure The standard checking process for patient identification failed No adverse outcome for patient as they did receive the correct procedure A new “timeout” procedure checklist will be implemented in the day surgery unit. The checklist will be based on the World Health Organization surgical safety checklist Implement “timeout” procedure prior to all procedures in Otago DHB theatres including local anaesthetic procedures Require staff to undertake preoperative identity checks at the appropriate time as described in the theatre policies The timeout checklist and procedures are now fully functioning for all surgical procedures DHB Summary of Serious and Sentinel Event Report 2009/10 64 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 2 Suicide of a community mental health client within seven days of contact with the service There does not appear to be any evidence that this patient’s care was in any way deficient, and therefore there are no particular recommendations from this investigation No recommendations identified Not applicable Serious 8 High risk patient absent without official leave returned to ward with no adverse outcome Increase in supervision of high risk patients All staff should be aware of the potential of safety issues for patients and to regularly give updates when there are changes identified Information not provided to the patient on admission regarding expectations while being an inpatient No specific recording of patients leaving the ward Safety concerns regarding the patient were identified but no clear plan documented in relation to these concerns No process in place when to identify a patient as missing and elevate concerns to senior staff Identify patients who are at risk and document in notes clearly On admission all patients will be asked to inform staff if they are leaving the unit and will need to sign a register if leaving for more than 20 minutes All patients on admission are verbally informed of expectations regarding leaving the ward/unit. This is to be provided in the patient information handbook A ward log/book will be in place at reception for patients to record when they leave the ward All patients will have a completed risk assessment on admission and any safety concerns will be clearly stated The current missing consumer policy will be reviewed The new missing consumer policy and associated document education and feedback about the change has commenced Serious 4B Management of bleeding post delivery of baby Patient has since recovered Review required of supervision of resident medical staff Review of trainee supervision Education for staff regarding management of bleeding post delivery Education has been provided in the form of a staff study day on this topic Serious 6 Inpatient fall resulting in fractured hip requiring surgery There is not an area in the admission assessment document with cues to document the patient’s baseline mobility Patient was reviewed on the ward round by the medical team after the fall, however there is no documented medical ward round note Recommend update of patient nursing admission assessment document When following the post fall management protocol, medical staff document acknowledgement of fall or near miss fall in clinical record That continued audit occurs to ensure that the falls prevention programme is being utilised The falls prevention programme is now in progress with audits taking place with the aim to prevent falls and falls resulting in injury Changes to the assessment documentation have been completed DHB Summary of Serious and Sentinel Event Report 2009/10 65 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up One dose of radiation therapy administered to patient due to incorrect diagnosis A major cause of this incident was the incorrect interpretation of imaging results Follow-up with the patient continues Encourage the responsible clinical staff to jointly review and discuss the images with a radiologist (if the formal report of the investigation is not available) before proceeding to active treatment Encourage staff to gain backup/second opinions from colleagues in difficult clinical situations to apply accurate clinical judgement Ensure appropriate staffing and backup/support available when staff are absent Follow as accurately as possible recommended policies, in this case treating according to defined waiting time criteria Staff will ensure all possible steps have been taken to establish as definitively as possible the correct diagnosis before commencing therapy Sentinel 4A Serious 6 Patient fall resulting in head laceration Staff documented falls risk but no strategies to ameliorate or eliminate risk documented Whilst the admission relating to the falls had a falls risk assessment completed subsequent assessments missing It appears that there is a practice of having bedsides in place for all patients in this department Falls prevention programme will address documentation and will provide training for staff in falls prevention strategies Frequency and documentation of assessment part of falls prevention programme Bedsides will only be implemented if clinically indicated according to the falls prevention strategy Falls prevention programme is now in progress with audits taking place with the aim to prevent falls and falls resulting in injury Serious 6 Inpatient fall resulting in a fracture dislocation of shoulder requiring treatment The falls risk assessment tool did not identify this patient as a falls risk This will be followed up by falls prevention co-ordinator to amend the assessment tool The assessment tool has now been updated and further audits are occurring to ensure the amendments are appropriate DHB Summary of Serious and Sentinel Event Report 2009/10 66 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4D Intravenous cross contamination of morphine between two patients. After blood testing was completed, neither patient had any abnormalities detected in their results Pre-package morphine syringes mean there is one less opportunity for an error to occur as would potentially be the case if nurses were required to repeatedly manually drawing up morphine ampoules and dilute for administration Intravenous morphine administration Patient observations were not fully completed following morphine administration Blood and body fluid exposure from patient to patient although rare does not appear to have an established process on the Otago site on how to deal with this issue Open disclosure to both parties was undertaken Ward areas use 10 mg/10 ml premixed morphine syringes which is cost effective if more than one dose is able to be administered from the same syringe The intravenous manual is amended to allow wards to store named controlled drug syringes and reuse the labelled syringe for more than one drug administration The narcotic flow chart be updated A joint policy be formulated to cover this scenario between occupational health & safety and infection prevention and control regionally The IV narcotic administration flow chart has now been updated to include what observations are required pre and post administration Sentinel 2 Suicide of a community mental health client within seven days of contact with the service Final report in progress Serious 5 Medication error involving a syringe swap of intravenous fentanyl and intravenous insulin causing low blood sugar The error was identified as the patient was being closely monitored and the patient recovered once treated for low blood sugar Final report in progress DHB Summary of Serious and Sentinel Event Report 2009/10 67 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Sentinel 2 Suicide of a community mental health client within seven days of contact with the service The patient’s care was divided between two teams which appear to have had inconsistent communication/interaction with each other The difficulty communicating is increased by the practice of keeping records in different services or even in different folders in the charts The mental health service conduct a comprehensive review of the policy and guidelines governing the case manager role The community alcohol and drug service review its discharge practice The document working group reconsiders the desirability of separating psychology and progress notes in the comprehensive clinical file That the mental health service management and educators continue to promote the importance of family/whānau involvement The case manager role review is currently under way Educators are providing family involvement sessions and will continue to do this on a regular basis Serious 4B Patient burn from wheat bag Treatment given with no lasting harm for the patient Patient safety was compromised by the wheat bag that was brought in to the hospital by the patient Staff education and increase awareness of risk to patients Patient and visitor awareness of wheat bag ban in hospital New product be sourced as a safe replacement for patient comfort and warmth Ban the use of heated wheat bags for all patients Inform staff of the discontinuation of heated wheat bag use for patients Standardised signs be put on all microwaves advising they only be used for food/fluids Product evaluation committee introduce the new product in accordance with health and safety and infection control guidelines with education for staff on their use Wheat bag/heat pack/hot water bottle ban in place, reminder signs on all microwaves, and a safer alternative product is now available Sentinel 2 Suicide of a mental health Inpatient while on approved leave Final report in progress Serious 6 Inpatient fall resulting in a fractured shoulder and fractured pelvis Weekend cover for allied health is at minimal levels Falls risk assessment documentation was completed by nursing staff It is not clear if an early assessment by the physiotherapist would have prevented this fall as the assessment could not happen for two days Continue to refine the documentation of assessments and strategies with nursing staff, including strategies to compensate for lack of allied health availability DHB Summary of Serious and Sentinel Event Report 2009/10 68 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 11 Patient self harm requiring surgical intervention Opportunity arose for patient to harm self despite continuous observation Patient watch documentation requires review Review nurse education for patient watch processes Review of patient watch processes Ensure patient watch education is provided to staff The patient watch staff education has now been added to the staff orientation booklet Education sessions for staff have now been reintroduced Serious 4E Incorrect patient specimen collection during colonoscopy Assumption made that a doctor’s credentialing for colonoscopies in another New Zealand hospital was transferable to Dunedin Hospital Unit’s “best practice” for colonoscopies was not discussed Minimal working knowledge of the software programme used in the unit The unit’s nursing staff did not question doctor’s placing of four biopsies into the one jar even though this is not usual practice in the Dunedin unit Credential all locums who are contracted to work in Dunedin Hospital Inform and discuss the unit’s best practice guidelines to new staff Ensure and confirm that all locums are familiar with and able to confidently use the endoscopy software package Instruct the unit’s nursing staff to question any practices/other behaviour of locums which differ demonstrably from the usual Ongoing surveillance occurring with no harm currently evident Sentinel 2 Suicide of a community mental health client within seven days of contact with the service Final report in progress Serious 6 Inpatient fall resulting in a fractured hip requiring treatment Falls prevention care plan documentation for the patient was incomplete Near miss falls although documented were not reported via the incident system The patient had been in hospital thirteen days without having a fall; however this particular fall may have been preventable Identify an action plan to ensure appropriate education and systems are implemented to ensure the falls prevention care plan is completed to the expected standard Promote the use of incident reports for near misses Further education for staff re: near miss, the identification of and reporting of near misses Monthly audits and feedback occurring to ensure that the falls prevention programme is being utilised correctly DHB Summary of Serious and Sentinel Event Report 2009/10 69 Otago District Health Board Serious or sentinel Event code* (see codes below) Sentinel 4C Serious Description of event Review findings Recommendations/actions Follow-up Patient death post elective total knee joint replacement surgery Final report in progress 2 Suicide of a community mental health client more than seven days since contact with the service Final report in progress Serious 6 Inpatient fall resulting in a fractured hip requiring surgery Patient tripped while attempting to mobilise independently The bathrooms are relatively narrow and confined making it difficult for patients to manoeuvre with walking aids and other apparatus The new falls prevention programme has been in use now for 2½ months and in this case highlighted the potential hazard Recommend that this practice be reviewed, and alternative practices evaluated Seek the advice of the occupational therapy and/or physiotherapy departments to determine if there are smaller or more suitable mobilising aides available Continue the use of the falls prevention assessment tool with increased emphasis on both preventative measures and improving engagement with patients in participating with identified falls prevention measures Serious 6 Inpatient fall resulting in a fractured hip requiring surgery The patient had a falls risk assessment completed on admission but the required reassessments had not taken place Identifying clear responsibilities of staff in relation to updating the falls risk assessment within the timeframes outlined in the guideline information, including consideration of all factors which may affect the patients vulnerability to falling, eg, medications Completion of audit as commenced in ward, with results being utilised to develop an education update for all nursing staff in the area DHB Summary of Serious and Sentinel Event Report 2009/10 70 Otago District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Nursing and medical staff identify solutions for this specific work environment Consideration of formalised policy for requesting assistance Implement a double check for administration of all medications Implement the standard use of coloured medication labels Implement the use of extension tubing to ensure the three-way tap is not nearby the casing of the syringe driver Discard ceased medication immediately Recommendations are currently being implemented in this area with the potential for some of the recommendations to become organisation-wide policy No recommendations identified Continue the use of the falls prevention assessment tool with increased emphasis on both preventative measures and improving engagement with patients in participating with identified falls prevention measures Sentinel 5 Medication error, wrong drug infusion connected to a patient in intensive care resulting in decreasing consciousness Systems errors identified No formal process for nursing staff to request additional nursing aid for high acuity patients No formal double check process in this area when administering medications to patients Potential for medications to be mismatched between pump, syringe and tubing Inability for labelled syringe to be rotated so the labels are not obscured Ceased medications not discarded at the time of cessation resulting in potential for confusion Sentinel 2 Suicide of a mental health Inpatient while on approved leave Final report in progress Serious 6 Inpatient fall resulting in a fractured hip requiring treatment Patient was confused and mobilised independently without alerting staff Regular falls assessments had taken place which identified this patient as high risk All appropriate falls prevention strategies were implemented for this patient prior to the fall DHB Summary of Serious and Sentinel Event Report 2009/10 71 Southland District Health Board Southland Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 5, 6 Medication error and inpatient fall resulting in head injury Medication policy not followed, patient closely monitored following medication error but despite this fell Fall was not witnessed Night staff revised knowledge of medication policy and provided reflective statement for portfolio Education provided to staff on monitoring patients post fall, and importance of notifying families in a timely manner Falls project has been commenced Serious 6 Inpatient fall resulting in head injury Fall was not witnessed Patient not noted to be falls risk on admission Reassessment of falls risk not completed following improvement in condition Delay in notification to family Serious 6 Inpatient fall resulting in head injury Fall was not witnessed Neurological consult obtained, patient not for surgical intervention Family fully informed Falls alarm in-situ post fall until discharge Uneventful recovery, patient discharged Sentinel 4B Patient died during X-ray investigations following road traffic accident Patient sustained multiple fractures including pelvis and chest trauma Trauma protocol not well followed Team leader not assigned as per trauma protocol Team members unable to be clearly identified Handover between staff lacked co-ordination Absence of alarm relay system in department Trauma protocol to be reviewed Staff be supplied with a top garment that has designation monogrammed Handover of clinical care between senior medical staff from different specialties should be standardised to ensure continuity of care Consideration is given to the installation of a cardiac arrest alarm relay from radiology department to ED Recommendations in progress Serious 4A Delay in diagnosis Root cause analysis undertaken Patient receiving treatment Additional clinics held that resulted in reducing backlog Management plan in place to avoid future backlogs Awaiting final report DHB Summary of Serious and Sentinel Event Report 2009/10 72 Southland District Health Board Serious or sentinel Event code* (see codes below) Description of event Review findings Recommendations/actions Follow-up Serious 4D Booking error for radiological procedure Root cause analysis investigation being undertaken Patient underwent unnecessary bowel preparation resulting in adverse effects Patient recovered and discharged Awaiting outcome of investigation Awaiting outcome of investigation Sentinel 2 Suicide of community mental health patient within seven days Sudden death review completed – no recommendations made Event referred to coroner Support provided to family and staff Complete Sentinel 2 Suicide of community mental health patient within seven days Sudden death review completed – no recommendations made Event referred to Police and coroner Support provided to family and staff Complete Sentinel 2 Suspected suicide of community mental health client within seven days Sudden death review completed – no recommendations were made Event referred to coroner Support provided to client’s family Complete DHB Summary of Serious and Sentinel Event Report 2009/10 73