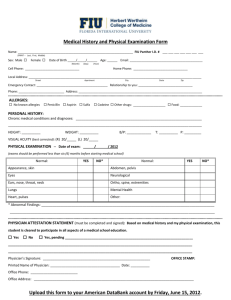
Medical Exam
advertisement
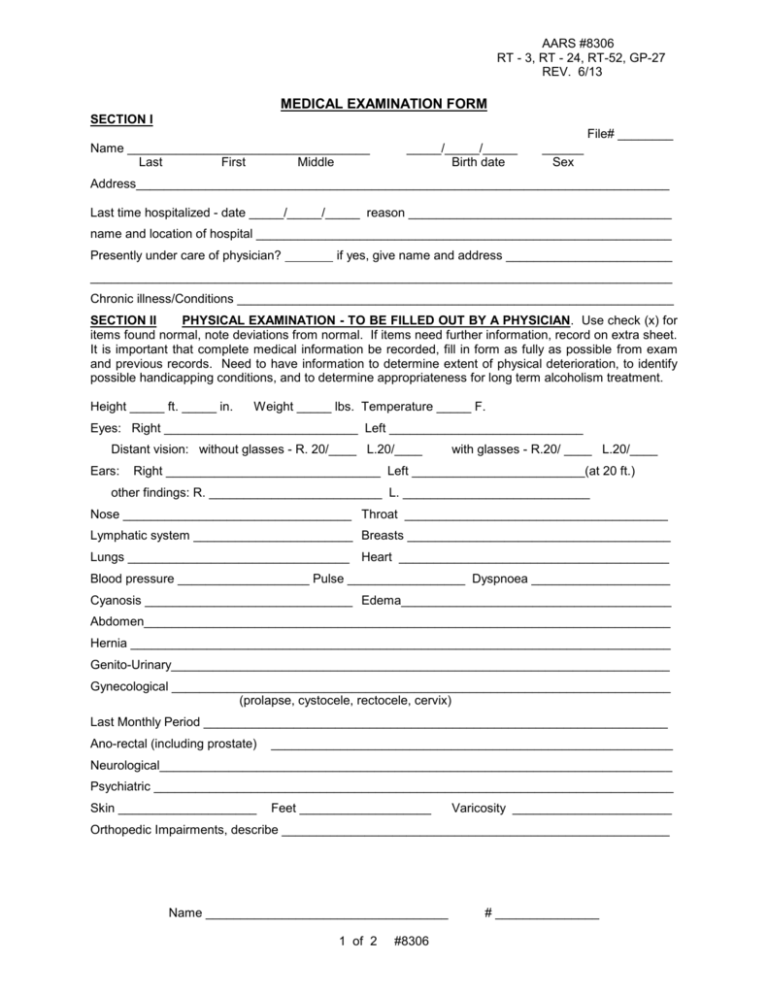
AARS #8306 RT - 3, RT - 24, RT-52, GP-27 REV. 6/13 MEDICAL EXAMINATION FORM SECTION I File# ________ Name ___________________________________ Last First Middle _____/_____/_____ Birth date ______ Sex Address_____________________________________________________________________________ Last time hospitalized - date _____/_____/_____ reason ______________________________________ name and location of hospital ____________________________________________________________ Presently under care of physician? if yes, give name and address ________________________ ____________________________________________________________________________________ Chronic illness/Conditions _______________________________________________________________ SECTION II PHYSICAL EXAMINATION - TO BE FILLED OUT BY A PHYSICIAN. Use check (x) for items found normal, note deviations from normal. If items need further information, record on extra sheet. It is important that complete medical information be recorded, fill in form as fully as possible from exam and previous records. Need to have information to determine extent of physical deterioration, to identify possible handicapping conditions, and to determine appropriateness for long term alcoholism treatment. Height _____ ft. _____ in. Weight _____ lbs. Temperature _____ F. Eyes: Right ____________________________ Left ____________________________ Distant vision: without glasses - R. 20/____ L.20/____ Ears: with glasses - R.20/ ____ L.20/____ Right _______________________________ Left _________________________(at 20 ft.) other findings: R. _________________________ L. ___________________________ Nose _________________________________ Throat ______________________________________ Lymphatic system _______________________ Breasts ______________________________________ Lungs ________________________________ Heart _______________________________________ Blood pressure ___________________ Pulse _________________ Dyspnoea ____________________ Cyanosis ______________________________ Edema_______________________________________ Abdomen____________________________________________________________________________ Hernia ______________________________________________________________________________ Genito-Urinary________________________________________________________________________ Gynecological ________________________________________________________________________ (prolapse, cystocele, rectocele, cervix) Last Monthly Period ___________________________________________________________________ Ano-rectal (including prostate) __________________________________________________________ Neurological__________________________________________________________________________ Psychiatric ___________________________________________________________________________ Skin ____________________ Feet ___________________ Varicosity _______________________ Orthopedic Impairments, describe ________________________________________________________ Name ___________________________________ 1 of 2 #8306 # _______________ Lab Tests (HTLV & HEPATITIS - OPTIONAL) HTLV Date: ___/___/___ Results __________________________________________ HEPATITIS Date: ___/___/___ serologic test for syphilis: Results __________________________________________ Date _____/_____/_____ Name of test _______________________ Result ____________________________________________________ Urinalysis: Date _____/_____/_____ Specific gravity ______________________________ Reaction _______________ Albumen _______________ Sugar ________________ Chest X-ray: Date _____/_____/_____ Results: ________ Hemoglobin: Date _____/_____/_____ TB-Skin Test: Date _____/_____/_____ Results: __________ Results: __________ Diphtheria/Tetanus Booster: Current immunization required date given: _____/_____/_____ RECOMMENDATIONS Is examination by a specialist advisable? if so, please specify specialty __________________________________________________________________________________ refraction X-ray of chest Hemoglobin Other diagnostic procedures or services (specify) ___________________________________________ Hospitalization (reasons and estimate duration) _____________________________________________ ___________________________________________________________________________________ Treatment (type and estimate duration) ____________________________________________________ ___________________________________________________________________________________ Re-examination or Re-evaluation, how soon _______________________________________________ SECTION III PHYSICIAN'S CONCLUSIONS AND COMMENTS PLEASE CHECK ALL ACTIVITIES CLIENT CAN DO perform daily hygienic routines dress unassisted lifting pulling control body eliminations feed self climbing walking communicate with others move about freely pushing standing please include other activities client should avoid or cannot do __________________________________ Does client exhibit any of the following: Psychosis or Psychoneurosis? explain (DSM IV) _____________________________________________ Current medications ____________________________________________________________________ History of Inhalant abuse, head injury? explain _______________________________________________ Potential danger to self or others? explain __________________________________________________ Suicidal?_____________________________________________________________________________ Communicable Disease? explain _________________________________________________________ Any special accommendations needed?____________________________________________________ Physician (print) _______________________________________ Date _____/_____/_____ Signature ____________________________________________ Address___________________________________________________________________ Name ___________________________________ 2 of 2 #8306 # _______________