Olga Sinicka. Genetic testing for hereditary breast and ovarian
advertisement

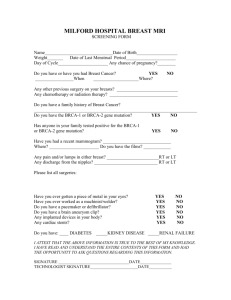
Biomedical Research and Study Centre University of Latvia Olga Sinicka GENETIC TESTING FOR HEREDITARY BREAST AND OVARIAN CANCER IN THE POPULATION OF LATVIA Summary of Academic Dissertation Supervisors: Dr.biol. Laima Tihomirova Biomedical Research and Study Centre, University of Latvia Dr.med. Aivars Stengrevics Latvian Oncology Center Reviewers: Prof. E. Grens Biomedical Research and Study Centre, University of Latvia Dr.med. Dz. Emzinsh Latvian Oncology Center Prof. A. Palotie Finnish Genome Center, University of Helsinki Riga, 2005 Actuality of the work Understanding of cancer as disease process, including its genetic, molecular and cellular basis is providing targets for prevention, detection, elimination and control interventions. At the beginning of 20th century the likelihood of an individual surviving cancer was very low. Today the 5 years survival rate is much higher and it is possible to improve it just by putting into practice all what is already known to be effective. Important factor affecting the outcome of disease is a time of diagnosis. Early detection of cancer as well as early warning of relapse and prediction of cancer risk are strategic priorities in fighting cancer. Genes affected in several hereditary cancer syndromes have been characterised and genetic testing for cancer predisposition has become an essential part of clinical management for families with inherited cancer syndromes. More than 20 different hereditary cancer syndromes have been defined now and attributed to germline mutations in various cancer-associated genes. Predictive DNA testing has been successfully applied by specialists of clinics to several inherited cancers - for example, retinoblastoma, polyposis coli, and multiple endocrine neoplasia type 2 (MEN-2). Family history is the most important risk factor of cancer and in cases when mutation in family is detected it is easy to discriminate those family members who have an elevated risk of disease. Breast cancer is the most frequent cancer in women (23% of all cancers) worldwide, with an estimated 1.15 million new cases in 2002 (Parkin, 2005). Breast cancer is the leading cancer site in Latvian women and ranks as the first highest cause of cancerrelated death, with an age-standardised morbidity 42.5 and age-standardised mortality 19.9 (to world age standard population) in 2001. More than 900 primary breast cancer patients were diagnosed annually during last years in Latvia, and about 23% of them before the age of 48 years. If breast cancer is detected early, the five-year survival rate exceeds 97%. On a worldwide basis, the total number of ovarian cancer cases has been estimated around 204,000 per year and the number of ovarian cancer-related deaths about 125,000 (Parkin et al., 2005). The 5-year survival rate for all stages of ovarian cancer is <40% (10% for Stage IV), with a possible 80-90% survival rate for Stage I. Nearly 300 women are diagnosed with ovarian cancer in Latvia annually and high mortality of women with ovarian cancer is associated with late diagnosis of disease (approximately 70% of them are diagnosed at stages III - IV). The discovery of breast and ovarian cancer susceptibility genes, BRCA1 (Miki et al. 1994) and BRCA2 (Wooster et al. 1995) facilitated detection of individuals predisposed to cancer. These tumor suppressor genes are involved in many important cellular processes, including DNA damage recognition, DNA repair, chromatin remodelling and control of transcription. Inactivating germline mutations in BRCAl and BRCA2 genes account for highly penetrant cancer predisposition, mostly limited to carcinomas of breast and ovaries. The estimated lifetime risk of breast cancer reaches 85% in BRCAl and BRCA2 carriers (Easton et al. 1995, Ford et al. 1998). The corresponding ovarian cancer risks are ~60% in BRCAl mutation carriers (Easton et al. 1995) and ~30% in BRCA2 mutation carriers (Ford et al. 1998). The characteristic features of hereditary cancer cases are earlier onset of disease and recurrence of cancer with high probability. The prevalence and spectrum of BRCAl and BRCA2 gene mutations has been characterised for different populations (Szabo and King, 1995; Liede and Narod, 2002) and the DNA testing for identification of individuals at elevated risk of cancer is widely used in clinics of all developed countries. Three recurrent mutations were identified in Ashkenazi Jewish population (Friedman et al., 1995), another recurrent mutation was identified in Icelandic population (Thorlacius et al., 1997). Similarly, the founder effects have been observed in Eastern European populations (Gayther et al. 1997, Csokay et al. 1999, Gorski et al. 2000; Oszurek et al. 2001). High prevalence of recurrent mutations facilitates the identification of the risk individuals. Screening procedures has been shown to reduce breast cancer mortality by approximately 35% (Vainio and Bianchini 2002), and even more in ovarian cancer patients. BRCAl and BRCA2 are high-penetrance genes. No additional high-penetrance susceptibility genes have been found presently to be involved in breast cancer. The remaining familial breast cancer risk could be explained by different genetic backgrounds due to the combination of low-penetrance genes (polygenic mechanism). In support of the polygenic model, a variant in the CHEK2 gene, 1100delC mutation, has been described as the first low-penetrance gene associated with familial breast cancer to confer a 2-fold increase in risk (Meijers-Heijboer et al., 2002) Different techniques for mutation detection (SSCP, HD, DHPLC, MLPA, direct sequencing) have been used in our study. The development of technologies to identify mutations and sequence variants in patient samples quickly, efficiently and inexpensively will play a crucial role in the future of medical genetics. The allelic heterogeneity of BRCA1 mutations serves as an example of the considerable technical challenge in developing diagnostic tests for all possible sequence variants in large genes. Aims of the study The aims of our study were: • to characterise the mutation spectrum of BRCA1/2 genes in breast and ovarian cancer patients and • to assess the criteria and possibilities for identification of women at elevated risk of breast/ovarian cancer in Latvia. For these reasons > the analysis of entire BRCA1 gene in breast and ovarian cancer patients, > the screening for BRCA1 recurrent mutations in different groups of individuals, > the analysis of entire BRCA2 gene, > the screening for large rearrangements in the BRCA1, > the screening for 1100delC mutation in CHEK2 gene have been carried out and the importance of this information for appropriate genetic counselling in Latvian population was assessed. Novelty of the work A role of different genetic factors known to be associated with risk of breast and ovarian cancer to date such as point mutations and large rearrangements in the BRCA1 gene, point mutations in the BRCA2 gene and 1100delC mutation in the CHEK2 gene has been assessed for the first time in Latvia. Screening for BRCA1 pathogenic mutations in series of breast and ovarian cancer patients and for two most prevalent mutations (5382insC and 4154delA) in different groups of cancer patients has been carried out. It allowed us to conclude that breast and ovarian cancer in Latvia are highly attributable to these two mutations and to specify groups of individuals with high risk of breast and ovarian cancer associated with BRCAl mutations. On the basis of these results it was possible to characterize criteria for genetic testing of hereditary breast and ovarian cancer and to optimize the policy of this testing in Latvian population. The results of this study are useful for genetic counselling and genetic testing for the identification of individuals at high risk of cancer in Latvia. Given current constraints on health-care resources, the results of our study indicate that screening for only two BRCAl mutations may have the strongest impact on health-care. Abbreviations BC - breast cancer Bilat - bilateral breast cancer C - cancer CC - colorectal cancer HD - heteroduplex analysis LuC - lung cancer OC - ovarian cancer PAAG - polyacrilamide gel PrC - prostate cancer RenC - renal cancer SSCP - single strand conformation polymorphism analysis F-SSCP - SSCP analysis using fluorescently labeled primers StC - stomach cancer UC - uterine cancer UV - unclassified variant Other abbreviations are explained in the text. Material and methods Breast and ovarian cancer patients. Breast and ovarian cancer patients were recruited at the Latvian Oncology Center (LOC) between the period of 1998 and 2004. The criteria for including patients in this study were the following: • agreement to participate in genetic testing, • diagnosis of breast cancer before the age of 48 years and of ovarian cancer before age of 55 years, independently on family history, • breast and/or ovarian cancer before 61 years and a positive family history (at least one first-degree relative affected with breast or ovarian cancer). The information about families was obtained by personal interview of patients. A total of 119 breast (Table 1) and 41 ovarian (Table 2) cancer patients were invited to participate in genetic testing for mutations of the entire BRCA1 gene. Two patients were twin sisters, all other patients were from unrelated families. The analysis of large rearrangements in BRCA1 gene was performed in 46 breast and ovarian cancer patients. The information concerning this group of patients is presented in Table 3. The analysis of the entire BRCA2 gene has been carried out in 42 BRCA1 mutation negative breast and ovarian cancer patients. The same patients were screened for the 1100delC mutation in the CHEK2 gene. The BRCA2 gene analysis, screening for the 1100delC mutation in the CHEK2 and the analysis of large rearrangements in the BRCA1 gene have been performed in the Department of Oncology and Surgical Sciences, Oncology Section, Azienda Ospedaliera, Padua, Italy (UICC ICRETT Fellowship: "Contribution of BRCA2 germline mutations to hereditary breast/ovarian cancer in Latvia", 2003). Screening for six pathogenic mutations in the BRCA1 gene has been carried out in series of breast and ovarian cancer patients (Table 4): 384 samples from breast and ovarian cancer patients have been screened for the 5382insC and the 4154delA mutations; 214 - forthe 300T>G mutation; 235 - for the 185delAG mutation; 81 - for the 3650delT mutation and 95 - for the 962del4 mutation. Of patients screened for the 5382insC and the 4154delA mutations 156 breast and all ovarian cancer patients were women who have donated blood for the Genome Database of the Latvian Population. The screening for the 3650delT and the 964del4 mutations have been performed only in DNA collected for the Genome Database of the Latvian Population. The information concerning personal and family history of cancer was obtained from questionnaires filled by patients. The screening for the 4154delA and the 5382insC mutations has been carried out as well in DNA from blood of 564 control DNA samples of cancer patients. Research ethics. An agreement to participate in the study including genetic analysis of entire BRCA1 gene was asked from all breast and ovarian cancer patients, and written consent was obtained. Data concerning patients who donated blood for the Genome Database of the Latvian Population were from questionnaires completed by the patients. The Science Council of the Biomedical Research and Study Centre approved the protocol of this study and appropriate research permission was obtained from the Central Ethics Committee of Latvia. DNA isolation. DNA was extracted from peripheral blood lymphocytes of breast and ovarian cancer patients according to standard non-enzymatic procedure using extraction with phenol or by standard non-enzymatic salting out procedure. BRCA1 mutation detection. Oligonucleotide PCR primers were used according to Friedman et al. (1994) and to sequences available in BIC database (http://research.nhgri.nih.gov/projects/bic). PCR reactions were carried out on a MJ Research PT100 thermocycler (USA) using reagent kits from Fermentas (Lithuania). Screening for mutations was carried out in the entire coding sequence of the BRCA1 gene and 5'- and 3'-flanking intronic sequences of each exon by SSCP and/or HD analysis. Screenings for the 4154delA, 300T>G, 3600delT, 1186A>G mutations were carried out by SSCP in PAAG. Screenings for the 185deiAG, I62A>G, 962del4 and partly for 5382insC mutations were carried out by HDA in PAAG with glycerol. The screening for the 5382insC mutation in exon 20 was carried out as well by the F-SSCP method and automated analysis of PCR-fragments using scanning on the ABI PRISM 310 sequencing device. Nucleotide alterations associated with SSCP/HDA variant bands were analysed by direct sequencing of corresponding DNA fragments on the ABI Prism 3100 automated DNA sequencing device. The screening for large rearrangements of the BRCA1 gene. BRCA1 genomic rearrangement analysis was performed by multiplex ligation-dependent probe amplification method (MLPA) using MLPA kit (MRC, Holland) with P002 mix probes for all BRCA1 exons. The analysis has been performed according to protocol provided by manufacturers. The separation and relative quantification of amplification products were performed by electrophoresis on the ABI PRISM 310 DNA Analyser and using Genescan 3.1 software (Applied Biosystems, USA). Haplotype analysis. Haplotype analysis has been performed for 46 carriers of 5382insC mutation and for 24 carriers of 4154delA mutation using three BRCA1 intragenic markers (Easton et al., 1994, Neuhausen et al., 1996) D17S1323, D17S1322, D17S855and BRCA1 flanking markers D17S1328, D17S1327 and BRCA1 90565. Primer sequences for these STR markers are from the Genome Data Base (GDB, http://gdbwww.gdb.org) with the exception of the BRCA1 90565, for which primers were used according to Liu and Barker (1999). The amplified products were mixed with formamide 95%, denatured, kept on ice, and loaded onto 7.5% urea/ 6% PAAG. Products were visualised after silver staining. The analysis of the entire BRCA2 gene and screening for the 1100delC mutation in the CHEK2 gene. Amplification reactions for all coding exons including flanking intronic sequences of BRCA2 gene (47different fragments - 200-700 bp) were performed using AmpliTaqGold® DNA Polymerase kit (Applied Biosystems, USA) on the PTC 200 (MJ Research Inc., USA) thermalcycler Primers for the amplification were used according to Wagner (1999) and the B1C database (http://research.nhgri.nih.gov/projects/bic). For amplification of CHEK2 exon 10 primers used were: F 5'-GCA AGT TCA ACA TTA TTC CCT TTT-3' and R 5'- ATC ACC TCC TAC CAG TCT GTG C-3\ Amplified fragments were analysed for mutations by DHPLC method (denaturing high performance liquid chromatography) using automated Transgenomic WAVE 3500 System. When variant profiles were identified DNA was reamplified. PCR products were analysed by sequencing on the ABI PRISM 310 DNA Analyser (Applied Biosystems, USA). Statistical analysis. Statistical analyses were performed with SISA software (http://home.clara.net/sisa/). 95 % confidence intervals were calculated using exact Binomial estimate. THE OVERVIEW OF RESULTS AND DISCUSSION I. THE CONTRIBUTION OF DIFFERENT GENETIC FACTORS TO HEREDITARY BREAST AND OVARIAN CANCER IN LATVIA We attempted to estimate a role of most important genetic factors associated with risk of breast and ovarian cancer (point mutations and large rearrangements in the BRCA1 gene, point mutations in the BRCA2 gene and the 1100delC mutation in the CHEK2 gene), in Latvian population. 1. The analysis of all coding and flanking intronic sequences of the BRCA1 gene in breast cancer patients Altogether 119 breast cancer patients (Table 1) have been involved in the analysis of the entire BRCA1 gene. Average age at diagnosis of patients analysed was 44.3 years. 87 of women tested were diagnosed before age of 48 years. Only 12 women had a strong family history of breast and/or ovarian cancer (with two or more cases). In spite of the relaxed criteria for DNA testing 24 carriers of deleterious mutations and 5 carriers of mutations with unclear clinical significance have been identified in this study. One of these carriers had a twin sister who was diagnosed with breast cancer simultaneously. The age at diagnosis of breast cancer for mutation carriers was between 22 and 60. Only two mutation carriers with late presentation of disease at 59 and 60 years (carriers of 5382insC) were detected in this group. Average age of diagnosis of breast cancer for BRCAl deleterious mutation carriers was 38.3 years. Table 1. Characteristics of breast cancer patients analysed for mutations in the entire BRCAl gene and results of this analysis Altogether seven different deleterious mutations: 185delAG, 300T>G, 962del4, 3650delT, 4154delA, IVS13+1G>A (4476+lG>A), 5382insC and three unclassified variants: 1186A>G, 4158A>G, 5002T>C have been detected in Latvian breast cancer patients. Only the 3650delT frameshift mutation in breast cancer patient diagnosed at 35 years of age and no cancer cases in her family is a novel, not registered in BIC database. Out of 24 mutation carriers identified 13 were found to have the 5382insC mutation, 6 the 4154delA, two - the 300T>G, and single carriers of three other deleterious mutations (3650delT, 185delAG, 962del4 and 4476+1G>A) were identified. Common polymorphisms such as: IVS8-57delT, IVS7-36C>T, 2430T>C (Leu>Leu), 3232A>G (Glu>Gly), 3667A>G (Lys>Arg), IVS18+66G>A, 4427T>C (Ser>Ser), 4956A>G (Ser>Gly), IVS16-92A>G, IVS16-68A>G and other were detected in this study. 2. The analysis of entire BRCA1 gene sequence in ovarian cancer patients 41 ovarian cancer patients (Table 2) were selected for the entire BRCA1 gene analysis. An average age at diagnosis was 40.1 years. 9 carriers of deleterious mutations were detected in this patient group. Only five of women tested had a strong family history of breast and/or ovarian cancer and two mutation carriers were detected in this group. A significant part of women tested (20 patients) had no family history of cancer, however in five of these patients BRCA1 mutations were detected. Table 2. Characteristics of ovarian cancer patients selected for the analysis of entire BRCA1 gene Three recurrent mutations detected previously in breast cancer patients were identified in ovarian cancer patients as well: the 5382insC in five, the 4154delA in three and the 300T>G in one women. The age of diagnosis of ovarian cancer for carriers of pathogenic mutations was between 28 and 61 years with average age of 44.8 years. The same common polymorphisms detected in breast cancer patients were detected in ovarian cancer patients as well. One carrier of a novel not registered in BIC, the 162A>G missense mutation, has been identified. The clinical effect of this mutation is unknown but a patient with the 162A>G mutation was diagnosed with ovarian cancer at an early age (20 years); she had no cancer in her family. Unclassified variant 1186A>G was detected by the analysis of the entire BRCA1 gene more frequently among ovarian cancer patients (four carriers) than among breast cancer patients (one carrier), especially in view of the significantly smaller set of patients with ovarian cancer involved in the analysis of the entire BRCA1 gene. Unclassified variant 5002T>C detected among breast cancer patients was not detected among ovarian cancer patients. Individuals with the 4158A>G missense mutation were identified among breast and among ovarian cancer patients as well. 3. The analysis of large rearrangements in the BRCA1 gene BRCA1-associated presentations of breast and ovarian cancer may be partly due to large genomic alterations in BRCA1 gene that cannot be detected by standard PCR-based mutation detection approaches. The frequency of BRCA1 rearrangements among all BRCA1 mutations may be different, depending on population. The highest frequency of BRCA1 rearrangements were found in Dutch breast cancer patients (36% of all BRCA1 mutations, Petrij-Bosch et al., 1997). In populations with detected BRCA1 large rearrangements their screening is an important step that should be systematically included in genetic testing. Complex rearrangements in the BRCA2 gene are less common. In order to estimate the contribution of large gene rearrangements to the BRCA1 mutation spectrum in Latvia we have analysed a series of breast and ovarian cancer patients, using the MLPA analysis (Fig. 1). The analysis has been carried out in 46 breast and ovarian cancer patients from Latvia (Table 3) analysed before and found negative for BRCA1 small genetic alterations (point mutations, small insertions and deletions). No large rearrangements in the BRCA1 gene were detected. Table 3. Characteristics of patients analysed for BRCA1 large rearrangements The results of MLPA analysis indicate that the role of large BRCA1 rearrangements may be not significant in the incidence of breast and ovarian cancer in Latvia. MLPA analysis of additional samples would be useful to draw more convincing conclusions. Figure 1. The comparing of two MLPA profiles: of Italian breast cancer patient with 3kb-deletion in the BRCA1 gene (red) (Montagna M. et al., 2003) and Latvian breast cancer patient without detected alterations (blue). 4. The analysis of entire BRCA2 gene All exonic and flanking intronic sequences of the BRCA2 gene have been carried out in the same set of breast/ovarian cancer patients (Table 3), excluding four patients (totally in DNA of 42 patients) by DHPLC (Figure 2). Figure 2. The comparing of two profiles; BRCA2 11K fragment, profile of patient No. 334-normal (pink) and 355 with polymorphism 4035T>C (blue). No deleterious mutations of BRCA2 gene were detected. The following mutations of unclear clinical significance and registered in BIC as unclassified variants were detected: 2014G>C (D596H), 4486G>T (D1420Y), 5972OT (T1915M), 6328OT (R2034C), 8377G>T (A2717S), 10323delCinsll-ter3369. Several common exonic polymorphic variants: 1342A>C (His>Asn), 4035T>C (Val>Val), 5427C>T (Ser>Ser), and five intronic polymorphisms: 8+56OT, TVS10-74T>C, IVS20+70A>G, IVS2166T>C, IVS24-113T>G were identified as well. Three intronic variants (IVS10-74T>C, IVS20+70A>G, IVS24-13T>G) are not registered at BIC, but the IVS10-74T>C is a common polymorphism in Italy as well. Altogether, 11 carriers of six different BRCA2 variants of unclear clinical significance were detected. One women with bilateral breast cancer diagnosed at age of 49 and with breast cancer in mother was a carrier of two unclassified variants (5972C >T and 8377G>T). Frameshift mutation 10323delCins11 leading to stop at codon 3369 in exon 27 was detected in one breast cancer patient. The effect of mutations in exon 27 of the BRCA2 gene is unknown but presently it is considered that mutations in distal exon 27 of the BRCA2 gene are not pathogenic (Narod, 2002). The mutation 10323delCinsll was detected in German population three times among 989 patients with breast or ovarian cancer (Meindl et al., 2002). The results of this study indicate that the contribution of BRCA2 gene mutations to hereditary breast and ovarian cancer in Latvia may be not significant. However, the analysis of more samples and segregation analysis in families would be useful. 5. Screening for the CHEK2*1100delC mutation Screening for protein truncating mutation 1100delC in the CHEK2 gene has been carried out in the same 42 breast and ovarian cancer patients analysed for entire BRCA2. This mutation has been detected in an early onset (35 years) breast cancer patient of Latvian ethnicity with strong family history of breast cancer (three cases in family: in sister, mother and mother's sister) (Figure 3). Figure 3. DHPLC profiles of normal sample (338), positive control and Latvian breast cancer patient with detected CHEK2* 1100delC mutation (149). This frameshift mutation causes premature termination at codon 381 and abrogates the kinase activity of the encoded CHEK2 protein. The 1100delC mutation is associated with 2-4-fold (Thompson and Easton, 2004) breast cancer risk. The range of cancers associated with mutations of the CHEK2 gene may include also prostate, colon, kidney and thyroid cancer (Dong X., 2003, Cybulski C. et al, 2004). The highest frequency of this mutation was reported in Finland (Vahteristo P., 2002). Limited relevance for CHEK2 mutations in familial breast cancer in several other populations (in Italy Caligo M.A., 2004, in Germany -Dufault M.R., 2004, Czech Republic - Kleibl Z. et al., 2005) was suggested. The results of our study carried out in 42 DNA samples demonstrated the presence of mutant allele in Latvian population that could contribute to breast cancer incidence in Latvia. II. MUTATION PROFILE IN LATVIAN BREAST AND OVARIAN CANCER PATIENTS The results of the DNA analysis carried out have demonstrated that breast and ovarian cancer syndromes in Latvian population are related mainly with BRCA1 pathogenic mutations. Mutations detected in the BRCA1 and BRCA2 genes are presented in Fig. 4. Figure 4. Genetic alterations detected in the BRCA1 and BRCA2 genes The analysis of entire BRCAl gene in breast and ovarian cancer patients allowed us to characterise the BRCAl mutation profile. This analysis indicates that breast and ovarian cancer in Latvia are highly attributable to two mutations - the 5282insC and the 4154delA. Apart from these two most prevalent frameshift mutations the analysis of the entire BRCAl gene resulted in detection of other pathogenic BRCAl mutations: one missense mutation with proved pathogenic effect (300T>G), three frameshift mutations (the 185delAG, the 962del4, the 3650delT) and one splice-site mutation (the 4476+lG>A). Three known missense mutations (the 1186A>G, the 4158A>G and 5002T>C) and one novel, not registered in BIC (the 162A>G) mutation, with unclear significance and several common polymorphisms were identified as well. Only two different pathogenic mutations were detected in patients of Russian ethnicity: the 5382insC (nine carriers), and a new frameshift mutation 3650delT (one carrier). The mutation profile in patients of Latvian ancestry was more heterogeneous, represented mainly by the founder mutations: the 5382insC - 39%, the 4154delA-35%, the 300T>G - 13%, the 185delAG, the 962del4 and the 4476+lG>A - 4% each. The BRCAl mutation spectrum in ovarian cancer patients differs from that in breast cancer patients insignificantly. Three pathogenic founder mutations (5382insC, 4154delA and 300T>G) detected in our studies of breast cancer patients were found as well in ovarian cancer patients. Mutation profile of breast cancer patients is presented by more different mutations, probably because of larger set of samples analysed. The analysis of other genetic factors predisposing to breast and ovarian cancer such as BRCA2 mutations (Figure 4), large rearrangements in the BRCAl gene, low-penetrance mutation 1100deI4 in the CHEK2 gene, showed insignificant role of these factors in breast and ovarian cancer incidence in Latvian population. Similar results were obtained in other populations with founder mutations in which non-founder BRCA mutations have been identified with a significantly lower frequency than would be expected (in Ashkenazi Jewish population - Kauff et al., 2002, and Polish population - Gorski et al., 2004). 1. BRCA 1 pathogenic mutations in breast and ovarian cancer patients in Latvia Most frequent mutation in Latvia, the 5382insC mutation is a frameshift mutation in exon 20 (Figures 5, 6), resulting in a stop-codon at 1829 in the important C-terminal BRCT domain. The BRCT domain is a very conservative domain necessary in the DNA repair and transcriptional activation. The mutation was observed in many populations, and the vast majority of carriers, including our carriers of 5382insC, share the same core haplotype (for intragenic markers). It is one of founder mutations in several populations: in Ashkenazi, Polish, Russian and Greek. 5382insC has been reported as well in individuals of Dutch, Hungarian, French, Germanic, Italian, British, Turkish, Canadian populations. This suggests that it is a relatively old mutation that has spread through migration. The mutation has been detected in individuals of Latvian as well of Russian (Slavic) ethnicity. Our results confirm the presence of a gradient from the East to the West in the prevalence of the 5382insC mutation with reducing frequency of this mutation from Russia to Latvia, Poland and Germany. Figure 5. Heteroduplex analysis of exon 20 in the BRCA1 gene. The 5382insC mutation(*). Figure 6. Confirmation of the 5382insC mutation by direct sequencing on the ABI PRISM 3100 automatic DNA analyser. Reverse primer was used in this case. The other mutation detected with the high frequency amongst breast and ovarian cancer patients in Latvian population is the 4154delA (Figures 7, 8), protein-truncating frameshift mutation located in exon 11. The 4154delA mutation leads to stop at codon 1365 in the region of SCD domains. The SCD are preferred sites for phosphorylation by ATM, CHK2 and ATR These kinases are activated in response to DNA damage and prevent cell division by phosphorilating of BRCA1 and p53 (Yoshida and Miki, 2004; Narod, 2004). Figure 7. The SSCP analysis of 3'- end of the BRCA1 gene. The 4154delA(*) and the 4158A>G (*) mutations Figure 8. Confirmation of 4154del and 4158A>G mutations by direct sequencing on ABBI3100 automatic DNA analyser (reverse primer was used in this case). The 4154delA mutation is characteristic for Eastern Europe and it was reported in Poland (Sobczak et al., 1997), Russia (Gayther et al., 1997), Western Belarus (Oszurek et al., 2001) and has been found out also in the USA, Canada (BIC), Finland (Sarantus L., 2001). In our study the 4154delA mutation was detected altogether in 33 breast and ovarian cancer patients, including data of screening for this mutation discussed in Chapter III (27 of them were Latvians). This probably is the highest proportion of this mutation detected to date in a single population. The haplotype analysis has been carried out for 24 carriers of the 4154delA mutation. The haplotype for intragenic makers was common for all carriers and most of carriers share the common haplotype also for BRCA1 flanking markers. The third recurrent in our population mutation is the mutation 300T>G (C61G) in exon 5 (Figure 9, 10). This missense mutation leads to substitution of cisteine to glycine at codon 61 in an important RING-finger domain of brcal protein and its strong pathogenic nature was proved unambiguously using segregation analysis and functional tests (Castilla et al. 1994, Brzovic et al.1998; Hashizume et al., 2001, etc.). Figure 9. SSCP analysis of BRCA1 exon 5. 300T>G mutation. Figure 10. Confirmation of the 300T>G mutation by direct sequencing on ABI3100 automatic analyser. The ligase activity of the RING domain and its importance in ubiquitination was shown. Mutations within the RING domain of BRCA1 could affect the interaction with other proteins such as BAP1, which is a Ub hydrolase, and BARD1, which also contains a RING finger. BARD1 acts with BRCA1 in double-strand break repair and ubiquitination. It was shown that BARD1 induces apoptosis by catalysing phosphorylation of p53 by DNA-damage response kinase (Feki A., 2005). In contrast to other Eastern European countries (Hungary, Poland, Czech Republic) and Germany the frequency of this mutation in Latvia is significantly lower. One of the founder mutations in Ashkenazi population, the 185delAG mutation, has been detected in two breast cancer patients of Latvian ethnicity. We have no strong data about ancestral origin of these patients and relation to Jewish ancestry can be not excluded unambigously. This mutation in exon 2 changes the reading frame of the mRNA and causes a premature termination codon at position 39. Suggestions about direct link between the 185delAG mutation and alterations in the caspase-mediated apoptotic pathway were reported recently (Johnson et al, 2004) The 962del4 mutation was detected in one patient which breast cancer diagnosed at the age of 36 and ovarian cancer at the age of 40 years. Patient had not family history of breast and ovarian cancer but reported colorectal and renal cancer cases in family. The 962del4 is a protein-truncating mutation at the 5'-end of the exon 11, with deletion of CTCA nucleotides resulting in stop at codon 297 The 962del4 mutation has been detected in German (Meindl et al., 2002), Austrian (Wagner et al., 1998), American (Janezic et al., 1999; BIC), Italian and Ashkenazi Jewish populations (BIC). Two novel, not registered in BIC mutations, unique each have been detected in this study: a new frameshift mutation 3650delT in exon 11 leading to a stop codon at 1209, and the missense mutation 162A>G leading to amino acid substitution - isoleucine to valine at codonl5 with unclear clinical effect. 4476+1G>A (IVS13+1G>A) mutation at splice acceptor site alters splicing of mRNA. It was detected in women of Latvian ethnicity diagnosed with breast cancer at age of 44 years. Her mother was affected by breast cancer as well. This mutation was detected before in USA. It is more prevalent among people of African American, Native American, and Latin American ethnicity and rare among women of Western European ethnicity. The BRCAl and BRCA2 analysis carried out in African American breast cancer patients revealed that this mutation is recurrent in this population and is one of two African American founder mutations (Pal et al., 2004). 2. The study of the possible role of two unclassified variants in the BRCAl (1186A>G and 4158A>G) in Latvian population Several lines of evidence derived from population based analyses and functional studies indicate that all mutations leading to premature termination of translation are associated with increased cancer susceptibility: However, missense mutations remain an important problem for risk assessment. The association of most alleles carrying missense mutations with cancer is unknown, creating significant problems for genetic counselling. One of missense mutation with proved pathogenic effect is the 300T>G mutation discussed above. Despite to the location of several missense mutations detected in our study in very important functional domains of the BRCAl or BRCA2 genes (for example, M1628T is located in the BRCT domain of BRCAl involved in the regulation of transcription and DNA repair; H372N is located in the histone acetyltransferase domain of BRCA2 involved in the modulation of the activity of many genes), the pathogenic effect of unclassified variants in the BRCA1 and BRCA2 genes detected in our study has not been proved till now. The attempts to clarify a role of two missense mutations detected in our study (1186A>G and 4158A>G) have been done. 1186A>G. This missense mutation 1186A>G results in amino acid substitution glutamine to arginine at codon 356 (Q356R). Studies of this mutation were carried out in several populations and controversial data about its role in cancer development were reported (Durocher et al., 1996, Janezic et al 1999; Dunning et al., 1997; Smith et al., 2001, etc). In accordance to several of studies reported (Janezic et al., 1999, Dunning et al., 1997) this mutation has been detected by the analysis of entire BRCA1 gene more frequently in ovarian cancer patients than in breast cancer patients (Chapter 2). We extended the analysis for this mutation in sets of breast and ovarian cancer patients, and in control group of clinically healthy individuals as well. The 1186A>G mutation was detected in all tested groups of individuals. Including data of entire gene analysis it was detected: in 13 out of 205 breast cancer patients (6.3%; 95% CI: 3.4-10.0%), in 10 out of 61 ovarian cancer patients (16.4%; 95% CI; 8.2-28.1%) and in 10 out of 54 controls (18.5%; 95% CI: 9.2-31.4%). The presence of RR homozygotes in all groups analysed shows that this allele is common in our population. The frequency of 356R amongst breast cancer patients is less than amongst ovarian cancer patients and healthy persons. It is in accordance to Dunning et al. (1997), suggesting that the 356R allele may be protective against breast cancer. More extensive analysis of the role of genetic factors in cancer ethiology would clarify this question. 4158A>G. Missense mutation of unclear clinical significance the 4158A>G (Figure 7, 8) results in substitution of arginine to glycine at codon 1347 (R1347G) in the region of SCD domains associated with cell cycle checkpoint control function of BRCA1. By the analysis of entire gene the 4158A>G was identified in two breast cancer patients and in one ovarian cancer patient, who was carrier of 5382insC mutation as well. Screening for the 4154delA pathogenic mutation (Chapter 111) carried out in different groups of individuals allowed to identify carriers of the 4158A>G variant as well. Including data of entire BRCA1 analysis the mutation was detected in breast cancer patients with less frequency (two carriers among 413 patients - 0.5%; 95% CI: 0.1-1.7%) than in ovarian cancer patients (two carriers among 132 patients - 1.5%; 95% CI: 0.2-5.4%) and in control group (11 carriers among 670 controls - 1.6%; 95% CI: 0.9-3.0%). Similar conclusions as for the 1186A>G mutation may be drawn from the screening for the 4158A>G mutation, indicating that no elevated cancer risk may be associated with this mutation. However, the ascertainment bias can not be excluded and for appropriate conclusions the analysis of additional samples and segregation in families would be useful. III. SCREENING FOR BRCA1 MUTATIONS 1. Screening for six pathogenic BRCA1 mutations in breast and ovarian cancer patients To clarify the prevalence of different pathogenic mutation in the population of Latvia breast and ovarian cancer patients were screened for six pathogenic mutations (Table 4) detected by the analysis of entire BRCAl gene. This screening resulted in detection of 39 more mutation carriers: 22 carriers of the 5382insC, 16 of the 4154delA, one carrier of the 300T>G and one carrier of the 185delAG. No carriers of the 300T>G mutation were detected among 159 breast cancer patients and only one carrier of the 300T>G mutation was detected among 55 ovarian cancer patients. Including data of the entire gene analysis we can conclude that altogether two carriers of the 300T>G mutation have been detected in breast cancer patients and two in ovarian cancer patients. One more breast cancer patient was identified with the 185delAG. Smaller sets of patients were analysed for 3650delT and 962del4 and no carriers of these mutations have been detected. The screening for BRCAl pathogenic mutations in breast and ovarian cancer patients supported the data of the entire BRCAl gene analysis: the importance of testing for two mutations (5382insC and 4154delA) and the low frequency of other pathogenic mutations. However, two other mutations (the 300T>G and the 185delAG) are recurrent in our population. BRCA1 mutations were detected with high frequency among young patients and more frequently in ovarian cancer patients than in breast cancer patients. Four mutation carriers have been detected among patients with late age at diagnosis, one of these patients (5382insC mutation carrier) didn't report cancer cases in family. Significant proportion of all mutation carriers identified by screening (38.5%, 95% CI: 23.4-55.4%) have no breast or ovarian cancer but have other cancers in family. Table 4. Results of screening for BRCA1 pathogenic mutations 2. Screening for the two most prevalent mutations in different groups of patients To estimate the prevalence of recurrent mutations among cancer patients in Latvia, to characterise cancer sites associated with prevalent mutations and to find out the criteria for genetic testing, DNA samples from peripheral blood lymphocytes of 376 cancer patients treated in the Latvian oncology center were screened for the two most prevalent BRCA1 mutations - the 5382insC and the 4154delA. Data about the age at diagnosis and cancer site, and the results of screening are presented in the Table 5. Nine mutation carriers (2.4%, 95% CI: 1.1 - 4.5%) were detected: four with the 4154delA mutation and five with the 5382insC mutation. Six of the mutation carriers were ovarian cancer patients, one also diagnosed with breast cancer eight years before, one man was diagnosed with prostate cancer at 72 years and one man was diagnosed with renal cancer at 62 years. Only one breast cancer patient carrying the 4154delA mutation (diagnosed at 67 years) was detected in this group. It should be noted that the average age at diagnosis of breast cancer in this group was 60.2 years and only 4 women diagnosed before 40 years of age were tested in this group. Taking into account the high proportion of ovarian cancer patients amongst carriers identified, we extended the study to screen control samples from patients with different gynaecological diagnosis. 216 DNA samples were screened for the two most prevalent mutations and 12 (5.6%; 95% CI: 2.9-9.5%) mutation carriers were detected: 6 carriers of the 4154delA and 6 carriers of the 5382insC mutation (Table 5). All mutation carriers detected were ovarian cancer patients (two of them with breast cancer before the ovarian cancer). Table 5. Screening for 5382insC and 4l54delA mutations in cancer patients High proportion of two BRCA1 mutations (5382insC and 4154delA) in Latvia. We observed a high proportion of the 5382insC and the 4154delA mutation carriers amongst breast and ovarian cancer patients in all our studies. Altogether, the 5382insC and the 4154delA have been identified in 39 breast and in 43 ovarian cancer patients. The results indicate that these mutations are an important factor in breast and even more in ovarian cancer aetiology in our population. The frequencies of two prevalent mutation carriers among ovarian cancer patients were similar in all patient groups tested: 19.5% (95% CI: 8.8-34.9 %) of two mutation carriers were identified by the analysis of entire BRCA1 gene in 41 patients, 22.0% (95% CI: 14.0-31.9 %) in 91 patients who have donated blood for Genome Database of Latvian population at 20.9% (95% CI: 12.9-31.0%) in 86 unselected ovarian cancer patients. Variation BRCA1 mutation frequencies was observed in different series of breast cancer patier analysed indicating on the necessity to extend the BRCA1 mutation screening patients with this cancer site to define the criteria for genetic testing more precisely. IV. RISK OF CANCER AT OTHER SITES FOR BRCA1 MUTATION CARRIERS To assess a possible risk of other cancers for patients and for healthy individuals relat to BRCA1 mutations we considered useful to perform the analysis of cancer history for mutation carriers and their relatives as well. 29 women with two cancer cases in the individual history of disease have been involved in BRCA1 mutation analysis and nine BRCA1 mutation carriers (31.0%; 95% CI: 15.350.8%) have been identified among these women (Table 6). Table 6. Patients with multiple cancer analysed for BRCA1 mutations The results of this analysis demonstrated that BRCA1 mutation carriers were affected secondarily by breast or ovarian cancer more often than by other cancers The presence of breast and ovarian cancers in the same patient is strong criterion for genetic testing. The high possibility of second cancer for BRCA1 mutation carriers points to different strategies for risk reduction, including surgery, first at all salpingo-oophorectomy. Significant portion of BRCA1 mutation carriers detected in our study had other cancer in families. 26.4% (95% CI: 16.7-38.1 %) of carriers had no breast/ovarian cancer in their families but only tumours localised at other sites, most frequently uterine , colorectal, and lung cancer as well (Fig. 11). Figure 11. Cancer sites reported in families of BRCA1 mutation carriers Other cancers were reported also: renal, prostate, stomach, melanoma, pancreatic, cervical, neuroblastoma and other (undisclosed). It is necessary to note that by the screening for two prevalent mutations in consecutive cancer patients two individuals (one prostate cancer patient and one renal cancer patient) both with the 5382insC mutation (Table 5) have been detected. This information is very important for risk assessment in patient and healthy relatives and can be useful for genetic counselling of families in which pathogenic mutations have been detected. It is important to take into consideration the risk of BRCA1- associated cancers for male (however, lower than breast and ovarian cancer risk for women). It has been suggested that ovarian cancer risk depends on the localisation of mutation in the BRCAl gene (Gayther et al. 1995). Several reports indicate that the risk of breast cancer is higher if the mutation is localised nearer to the 5'-end and in the 3'-end of the gene (Gayther et al., 1995; Risch et al., 2001). Mutations in the middle part of the gene localised between nucleotides 2401 and 4191 result in a higher proportion of ovarian cancer (Risch et al. 2001, Thompson et al. 2002). Deleterious mutations have been detected in our study in the whole coding sequence of the BRCAl gene and we cannot suggest that mutations in some of BRCAl regions are more related with breast or ovarian cancer. Large number of the 5382insC mutation has been detected among ovarian cancer patients (25 of 51 carriers of this mutation) and among 33 carriers of the 4154delA mutation 15 carriers were breast cancer patients. Our results indicate that at least the specific mutation 5382insC localised in the 3'-end of the gene may be associated with ovarian cancer and 4154delA localised in the middle part of BRCAl may be associated with breast cancer in high proportion of cases. Ovarian cancer appears to be an important site of disease in Latvian women carrying the 5382insC mutation, and this should be recognised in genetic counselling of mutation carriers V. THE CRITERIA AND POLICY FOR GENETIC TESTING OF HEREDITARY BREAST AND OVARIAN CANCER IN LATVIAN POPULATION There are different models that estimate the likelihood of detecting a BRCAl or BRCA2 mutation in a given family or individual. There are also a number of features indicating increased likelihood of carrying BRCA mutations worldwide: the presence in a family of cases of breast and/or ovarian cancer and at least one diagnosed at early age, breast and ovarian cancer in the same women, multifocal or bilateral breast cancer, male cancer cases, Ashkenazi Jewish (or other ethnicity characterised by founder mutations) ancestry. However, these models are based on general Caucasian population and these features can be variable between populations because of different genetic and environmental factors. Data obtained by the entire BRCA1 gene analysis (Tables 1, 2) and by screening for BRCA1 pathogenic mutations in breast and ovarian cancer patients (Table 4) demonstrate that large number of mutation carriers identified in our study, were patients with no cancer in family history (22.2%; 95% Cl: 13.3-33.5%). Only 19.4% (95% Cl: 11.1-30.5%) of mutation carriers detected had strong family history of breast/ovarian cancer. The identification of large number of mutation carriers with insignificant or no family history of cancer suggests that DNA testing policies limited only to families with a strong history of breast/ovarian cancer could miss a significant proportion of mutation carriers in the population of Latvia. 90.3% (95% Cl: 81.0-96.0 %) of mutation carriers detected in this study were early onset breast and ovarian cancer patients. Based on our data we can note that the major proportion of mutation carriers among ovarian cancer patients may be identified by the screening of women diagnosed before 65 years and among breast cancer patients before 50 years, respectively. We could conclude that the presence of other cancer in families of breast and ovarian cancer patients indicates with high likelihood on the possible segregation of BRCA1 mutation in the family. This should be considered as very important information for genetic counselling and an important criterion to offer BRCA1 testing in these families. The results of our study indicate that the screening for only two mutations (5382insC and 4154delA) allows an easy identification of majority of women with high risk of breast and ovarian cancer. CONCLUSIONS AND RECOMMENDATIONS The role of different genetic alterations (BRCA1 and BRCA2 gene mutations, large rearrangements in the BRCA1 gene, HOOdelC mutation in the CHEK2 gene) associated with hereditary breast and ovarian cancer have been assessed and the mutation spectrum of BRCA genes in breast and ovarian cancer patients from Latvia has been characterised. Results of our study demonstrated that hereditary breast and ovarian cancer in Latvian population are related mainly to pathogenic mutations in the BRCAl gene. - The analysis of entire BRCA1 gene in cancer patients different 160 breast and ovarian resulted in detection of 33 mutation carriers (seven deleterious mutations: 185delAG, 300T>G, 962del4, 3650delT, 4154delA, 5382insC, IVS13+1G>A and four unclassified variants: 162 A>G, 186A>G, 4158A>G, 5002T>C). No elevated risk of cancer can be associated with missense alterations (excluding 300T>G in the BRCA1 gene). - Two mutations were detected with high frequency in Latvian population: 5382insC and 4154delA (~80% of all mutations detected by the analysis of entire BRCA1 gene). These mutations were found in all cancer patient groups tested. - Deleterious mutations were not detected by the analysis of entire BRCA2 gene in 42 DNA samples, only missense mutations and polymorphisms were found (altogether 6 mutations with unknown clinical significance, 3 exonic and 5 intronic polymorphic variants). - Large rearrangements are not characteristic for the population of Latvia no rearrangements were found by MLPA analysis in 42 patient DNAs - The 1100delC mutation in the CHEK2 gene may have some effect to cancer incidence in Latvia (one carrier was detected among 42 patients). Significant number of mutation carriers identified allowed us to characterise the criteria for genetic testing of hereditary breast and ovarian cancer in the population of Latvia and to optimise the policy of this testing. - We could recommend as the first step for DNA analysis of hereditary breast and ovarian cancer in Latvia to perform the screening for 5382insC and 4154delA mutations. If these two mutations are not detected, the screening for two other recurrent mutations, 300T>G and 185delAG, can follow. In a patient with early onset of disease and strong family history of cancer and negative for recurrent mutations, the analysis of entire BRCA1 gene should be offered. - Results of our study showed that the early onset of breast or ovarian cancer in women of Latvian population indicates on high possibility of the BRCAl mutation carrier status and is an important criterion to involve the patient in genetic testing for hereditary disease regardless family history of cancer. Genetic testing offered only to women with strong family history of cancer can miss carriers and limit the identification of persons with elevated risk of disease. - For rapid, money-saving and effective identification of BRCAl mutation carriers in Latvia it would be useful to perform screening for two prevalent mutations in breast cancer patients before the age of 50 years and ovarian cancer patients before the age of 65 years regardless of family history of cancer. - Presentation of cancer in wide range of sites (not only breast and ovary, but also uterus, colon and rectum, lung, cervix, prostate, pancreas, kidney etc.) in family members of mutation carriers and the identification of BRCAl carriers among patients with other cancer sites is not only one of the criteria for genetic testing but important information for possible risk assessment for patients and their relatives. Publications: > Csokay,B., Tihomirova, L., Stengrevics, A., Sinicka, O., Olah, E. (1999) Strong founder effects in BRCA 1 mutation carrier breast cancer patients from Latvia. Human Mutation. Mutation in Brief # 258. Online.l4(l), p. 92. > 0. Sinicka. A. Stengrevics, J. Eglitis, D. Smite, Z. Shomsteine, L. Tihomirova. Ovarian cancer in Latvia is highly attributable to recurrent mutations in the BRCAl gene. Acta Universitatis Latviensis, Biology, 2004, Vol. 670, pp. 17-25. > Tikhomirova L., Sinicka P.. Smite D., Eglitis J., Hodgson S., Stengrevics A. High prevalence of two BRCAl mutations, 4154delA and 5382insC, in Latvia. Fam Cancer. 2005;4(2):77-84. Participation on the conferences and conference theses: 2002 - The 4th Milan Breast Cancer Conference, June 5-7, Milan, Italy 1. Sinicka O., Smite D.. Stengrevics A., Eglitis J.. Tihomirova L. Prevalence and spectrum of BRCA1 mutations in breast and ovarian cancer patients from Latvia. The 4 th Milan Breast Cancer Conference, Milan, Italy, June 5 th -7 th 2002, Abstracts book p .41. 2003 - The 5th Milan Breast Cancer Conference, June 11-13, Milan, Italy. 2. Sinicka., Smite D., Stengrevics A., Tihomirova L. BRCA1 gene mutations in Latvian breast cancer patients without family history of cancer. The 5th Milan Breast Cancer Conference, Milan, Italy, June 11 th - 13th, Abstracts, p. 37. 2004 - The 4th European Breast Cancer Conference, 16-20 March, Germany, Hamburg. 3. O. Sinicka, A. Stengrevics, D. Smite, J. Eglitis, L. Tihomirova. DNA diagnosis of hereditary breast and ovarian cancer in Latvia. The 4th European breast cancer conference, Hamburg, Germany, 16-20 March 2004, Abstract No. 168, European Journal of Cancer Supplements, European Journal of Cancer Supplements, Vol. 2, No.3, March 2004, p. 103. 4. Tihomirova L., Csokay B., Stengrevics A., Sinicka P., Kamerade R., Olah E. Hereditary breast cancer in Latvia: mutation analysis of the BRCA1 gene.Biomed 2: Familial Breast Cancer Demonstration Project Symposium "Familial Breast Cancer - The Problems and the Solutions? ", Deutsches Krebsforschungzentrum, Heidelberg, Germany, May 27th - 29th 1999. 5. L.Tihomirova, O.Sinicka, E.Olah. High frequency of BRCA1 mutations in patients with early onset breast cancer. 17th International Conference on Human Tumor Markers, Hong Kong, 2000, Taiwan. 6. Tihomirova L., Sinicka P., Smite D., Stengrevics A. Recurrent mutations of BRCA1 gene as diagnostic genetic markers of hereditary breast cancer in Latvian patients. 18 th International Conference on Human Tumor Markers 2001.Riga, Latvia. Abstr. Journal of Tumor Marker Oncology, 2001, Vol.16, No.2, 116-117. 7. A.Stengrevics, P.Sinicka, L. Tihomirova. BRCA1 gēna mutācijas krūts vēža slimniecēm Latvijā. Pasaules latviešu ārstu 4. kongress. 2001. Rīga. tēzes lp.l73 (in Latvian). 8. A.Stengrevics, P.Sinicka, D.Smite, L.Tihomirova. The epidemiology and clinical implications of BRCA1 mutations for breast and ovarian cancer in Latvia. The 3fh Baltic States Congress. Vilnius, Lithuania, May 2-4? 2002, Abstracts, p.203. 9. Tihomirova, L., Sinicka, P., Smite, D., Eglitis, J., Stengrevics, A. Genetic epidemiology of BRCA1 gene mutations in Latvia. The 3d Genetical Congress of Baltic States, Vilnius, Lithuania, October 10 th -12 th 2002, Programme and Book of Abstracts, p.48, 10. Tihomirova, P. Sinicka, D. Smite, J. Eglitis, A. Stengrevics. Characterization of BRCA1 gene mutation profile and frequencies in cancer patients and population of Latvia. BCLC and ICG-FBPC 14th General Meeting. Madrid, June 2nd-4 th , 2003, Abstract book. p. 90. 11. T.V. Nasedkina. O.E. Fedorova. O. Sinicka. L. Tihomirova, A.D. Mirzabekov. Analysis of mutations in the BRCA1 gene using gel-based microarrays. BCLC and ICG-FBOC 14th General Meeting, Madrid. June 2nd-4 th , 2003, Abstract book, p. 150. 12. Eglitis. L. Tihomirova. O. Sinicka. High incidence of mutations in BRCA1 in breast and ovarian cancer patients in Latvia. ECCP 12 - the European Cancer Conference, Copenhagen, Denmark. 2125 September 2003. Abstract 1044. Citation: European Journal of Cancer Supplements: Vol. 1, No. 5, September 2003. page S311.