Corticosteroids – An Overview - Wellington Intensive Care Unit
advertisement
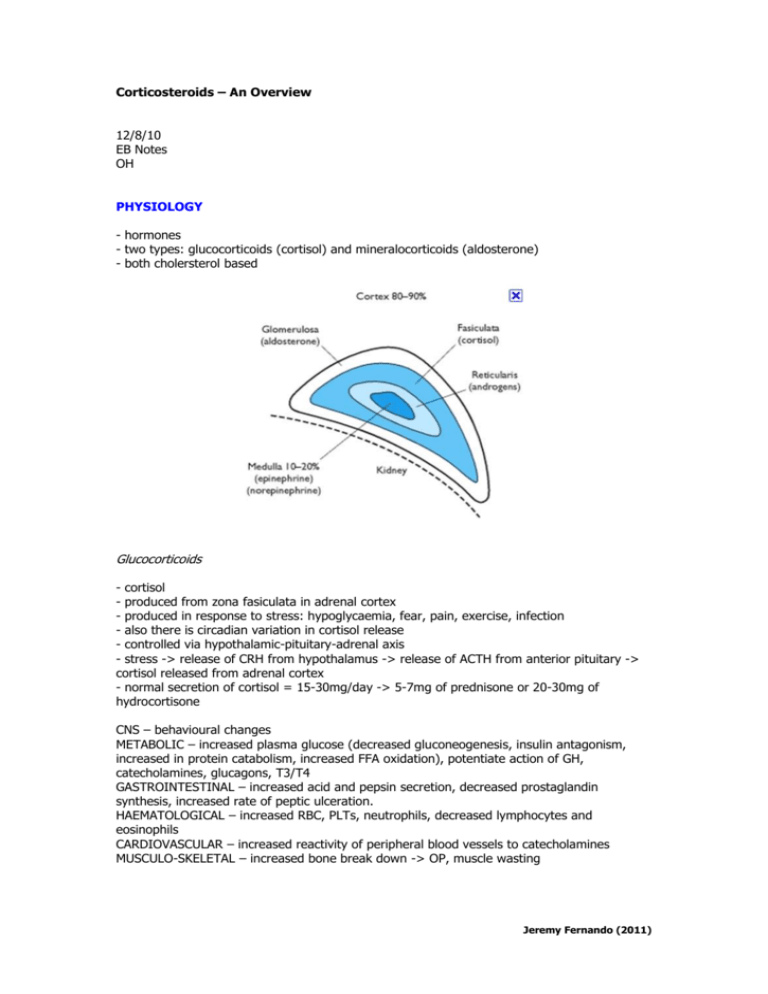
Corticosteroids – An Overview 12/8/10 EB Notes OH PHYSIOLOGY - hormones - two types: glucocorticoids (cortisol) and mineralocorticoids (aldosterone) - both cholersterol based Glucocorticoids - cortisol - produced from zona fasiculata in adrenal cortex - produced in response to stress: hypoglycaemia, fear, pain, exercise, infection - also there is circadian variation in cortisol release - controlled via hypothalamic-pituitary-adrenal axis - stress -> release of CRH from hypothalamus -> release of ACTH from anterior pituitary -> cortisol released from adrenal cortex - normal secretion of cortisol = 15-30mg/day -> 5-7mg of prednisone or 20-30mg of hydrocortisone CNS – behavioural changes METABOLIC – increased plasma glucose (decreased gluconeogenesis, insulin antagonism, increased in protein catabolism, increased FFA oxidation), potentiate action of GH, catecholamines, glucagons, T3/T4 GASTROINTESTINAL – increased acid and pepsin secretion, decreased prostaglandin synthesis, increased rate of peptic ulceration. HAEMATOLOGICAL – increased RBC, PLTs, neutrophils, decreased lymphocytes and eosinophils CARDIOVASCULAR – increased reactivity of peripheral blood vessels to catecholamines MUSCULO-SKELETAL – increased bone break down -> OP, muscle wasting Jeremy Fernando (2011) Mineralocorticoids - aldosterone produced in the zona glomerulosa daily output: 100-150mcg/day secreted in response to; Na+ deficiency -> elevated angiotensin II, elevated plasma K+ RENAL – 1. acts on collecting ducts -> increases production of the Na+/K+ ATPase in the basement membrane, increased Na+ and K+ channels in the apical membrane -> increase in Na+ reabsorption and K+ secretion -> ECF volume expansion. 2. increases excretion of H+ and NH4+ 3. increases Cl- reabsorption OTHER – increased Na+ reabsorption in sweat, salivary and distal colon glands. ADRENAL INSUFFICIENCY (AI) - types: primary, secondary and tertiary + acute/chronic Primary = Addison’s - destruction of > 90% of adrenal glands - rare - causes: autoimmune destruction, haemorrhage, tumour (breast and melanoma), infection (Tb, HIV, meningococcaemia, purpura fulminans) or inflammatory process - loss of mineralocorticoid and glucocorticoid activity Secondary - insufficient production of ACTH rare mineralocorticoid function intact causes: destruction or dysfunction of the pituitary Tertiary/Iatrogenic/Relative - suppression of HPA axis over time most common cause: administration of exogenous glucortiocoids mechanism: chronic ACTH suppression -> adrenal atrophy CONSEQUENCES Crisis Jeremy Fernando (2011) - concurrent illness, surgery, failure to take medications GI: abdominal pain, vomiting and diarrhoea CVS: dehydration, hypotension, refractory shock, poor response to inotropes/pressors fever confusion Chronic - GENERAL: weight loss, arthalgia, myalgia CNS: fatigue, anorexia, mood change CVS: postural hypotension, syncope, salt craving SKIN: pigmentation, vitiligo ELECTROLYTES: hypoglycaemia, hyponatraemia, hyperkalaemia, increased urea MANAGEMENT Diagnosis - plasma cortisol level < 80mmol/L - short synacthen test: 250mcg (normal response = cortisol > 525mmol/L) Treatment - fluid resuscitation - reversal of electrolyte abnormalities - high dose hydrocortisone (100mg IV Q6 hrly) Jeremy Fernando (2011) PERIOPERATIVE STEROID THERAPY - glucocorticoids introduced into clinical practice in 1949 - soon after there were two deaths from withheld steroids in perioperative period -> “stress doses” in the perioperative period. - for many years we overcooked these patients with large doses of steroids - new guidelines: - those on 5mg or less of prednisone OD -> don’t need supplementation minor operation -> normal dose + 25mg hydrocortisone in OT moderate operation -> normal dose + 25mg hydrocortisone Q6hourly for 24 hours high risk operation -> normal dose + 25mg hydrocortisone Q6 hours for 48-72 hours Prednisone 1mg = Hydrocortisone 4mg = Dexamethasone 0.15mg = Triamcinolone 0.8mg = Methylprednisolone 0.8mg = Betamethasone 0.15mg = SEVERE SEPSIS + SEPTIC SHOCK - basis: that patients with severe sepsis has relative adrenal insufficiency - difficult to diagnose because of the questionable validity of using plasma cortisol and the synacthen test. - benefit shown in meningitis - 1970’s + 1980’s – massive doses of steroid (30mg/kg) -> no survival benefit + increase in secondary infections Annane D, Sbille V, Charpentier C, et al: “Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock”. JAMA 2002; 288:862-871 - RCT in refractory septic shock - low dose hydrocortisone + fludrocortisone VS placebo - n = 300 -> non-responders to cosyntrophin test + given steroid -> significant decrease in mortality (P = 0.02) -> duration of vasopressor therapy shorter - problems: bad trial design, use of etomidate Sprung CL, Annane D, Keh D, et al: “CORTICUS Study Group: Hydrocortisone therapy for patients with septic shock.” N Engl J Med 2008; 358:111-124. - 2008 – CORTICUS - ANZICS - MRCT - low dose hydrocortisone vs placebo -> no survival benefit -> shock reversed more quickly -> more superinfections, hyperglycaemia, hypernatraema - weakness: patients were less sick than Annane’s study and was underpowered Jeremy Fernando (2011) The COIITSS Study Investigators (2010) “ Corticosteroid Treatment and Intensive Insulin Therapy for Septic Shock in Adults: A Randomized Control Trial” JAMA 303 (4):341-348 - septic shock: corticosteroids VS insulin therapy VS both improved outcomes +/mineralocorticoid - MRCT - inclusion criteria: adult, septic shock, MODS, hydrocortisone - exclusion criteria: no consent, moribund, pregnant, co-enrolement - primary end points = hospital mortality and 90 day mortality - secondary end points = 28, 90 and 180 day mortality, ventilator free days, ICU length of stay, hospital length of stay, hypoglycaemia, infectious complications, weakness - n = 509 - ITT analysis Intensive Insulin Group -> double hypoglycaemic rate -> no increase in mortality -> no difference in secondary outcomes -> no difference in synth-ACTH-en responders -> no difference in fludrocortisone patients Fludrocoritisone Results -> no increase in mortality -> no difference in inotropes -> excess superinfection rate -> don’t use in septic shock Criticisms - did not reach required recruitment levels - not blinded - tested multiple variables SUMMARY - steroids are not good in low risk patients with sepsis - most people with refractory shock receive low dose steroids - those in the middle – the literature is not clear ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS) - mortality = 40-60% - pathophysiology: excessive inflammation and vascular permeability with extravasation of plasma and leukocyte infiltration (fibroproliferative stage) -> steroids thought to reduce the extent of theses processes Meduri study (JAMA) - cross over trial -> reduction in lung injury score -> improved mortality Meduri study -> reduction in length of ICU stay Jeremy Fernando (2011) -> reduction in duration of IPPV Steinberg KP, Hudson LD, Goodman RB, et al: National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network: “Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome.” N Engl J Med 2006; 354:1671-1684. - n = 180 - MRCT - methylprednisolone for 14 days with taper VS placebo -> reduced shock symptoms -> reduced ventilator days -> improved pulmonary compliance -> increased mortality in patient who had had steroids > 14 days -> increased neuromuscular weakness -> NO improvement in survival - outcomes in trials have varied -> two recent systematic reviews have reached opposite conclusions! Agarwal R, Nath A, Aggarwal AN, Gupta D. “Do glucocorticoids decrease mortality in acute respiratory distress syndrome? A meta- analysis.” Respirology 2007;12:585-90. -> current evidence does not support the efficacy of steroids in ARDS Meduri G, Marik P, Chrousos G, Pastores S, Arlt W, Beishuizen A, et al. Steroid treatment in ARDS: a critical appraisal of the ARDS network trial and the recent literature. Intensive Care Med 2007 -> prolonged glucocorticoid treatment substantially and significantly improves meaningful patient-centered outcome variable and has a distinct survival benefit What about steroids for ARDS prophylaxis? - increase in ARDS and subsequent mortality (weak trend) SUMMARY - exact place of steroids in ARDS is unknown - further investigation required MENINGITIS van de Beek D, de Gans J, McIntyre P, et al: Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev 2007; 1 de Gans J, van de Beek D: European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators: Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347:1549-1556 - systematic reviews Jeremy Fernando (2011) - dexamethasone with first antibiotics in community acquired bacterial meningitis -> reduces mortality -> reduces severe hearing loss -> reduces neurological sequelae TBI Roberts I, Yates D, Sandercock P, et al: CRASH trial collaborators: Effect of intravenous corticosteroids on death within 14 days in 10,008 adults with clinically significant head injury (MRC CRASH trial): Randomised placebo-controlled trial. Lancet 2004; 364:1321-1328. Edwards P, Arango M, Balica L, et al: CRASH trial collaborators: Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injuryoutcomes at 6 months. Lancet 2005; 365:1957-1959. - 48 hours of IV steroids vs placebo -> increased mortality within 14 days -> increases mortality @ 6 months -> increased risk of severe disability ACUTE SPINAL CORD INJURY Bracken MB, Shepard MJ, Collins WF, et al: A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990; 322:1405-1411. - high dose methylprednisolone within 8 hours in injury -> evidence supported use Miller SM: Methylprednisolone in acute spinal cord injury: A tarnished standard. J Neurosurg Anesthesiol 2008; 20:140-142. George ER, Scholten PJ, Buechler CM: Failure of methylprednisolone to improve the outcome of spinal cord injury. Am Surg 1995; 61:659-663. Pointillart V, Petitjean ME, Wiart L: Pharmacotherapy of spinal cord injury during the acute phase. Spinal Cord 2000; 38:71-76. -> criticisms of NASCIS: study design flawed, statistical analysis flawed, conflicting evidence Bracken MB: Steroids for acute spinal cord injury. Cochrane Database Syst Rev 2002.CD001046 -> supports use of methylprednisolone Tsutsumi S, Ueta T, Shiba K, et al: Effects of the Second National Acute Spinal Cord Injury Study of high-dose methylprednisolone therapy on acute cervical spinal cord injury results in spinal injuries center. Spine 2006; 31:2992-2996. -> supports use of methylprednisolone Jeremy Fernando (2011) Leypold BG, Flanders AE, Schwartz ED, et al: The impact of methylprednisolone on lesion severity following spinal cord injury. Spine 2007; 32:373-378. -> patients who had methylprednisolone had significantly less intramedullary haemorrhage than those who were no treated. Eck JC, Nachtigall D, Humphreys SC, et al: Questionnaire survey of spine surgeons on the use of methylprednisolone for acute spinal cord injury. Spine 2006; 31:E250-253. - n = 305 spine surgeons -> 90% would initiate methylprednisolone especially within the 8 hour window -> reasons given: institutional protocol, medicolegal reasons -> only 24% used steroids because of a belief in improved outcomes! Summary - controversial issue - methylprednisolone may have role in neurological protection in early spinal cord injury - a well designed RCT’s is required SUMMARY OF PROVEN ROLES FOR STEROIDS Airway - croup - decreased post-extubation stridor in those at risk Breathing - anaphylaxis asthma COPD PJP pneumonia Nervous - bacterial meningitis myasthenic crises myxoedema coma decreases cerebral oedema associated with brain tumour Endocrine - Addison’s hypercalcaemia myxoedema coma hypothalamic-pituitary-adrenal insufficiency previous steroid use Jeremy Fernando (2011) Other - purpura fulminans fulminant vasculitis organ transplantation various malignancy (lymphoma) anti-emetic palliative care ACCEPTED BUT CONTROVERSIAL USES OF STEROIDS - severe sepsis with resistant shock - spinal injury - early ARDS CONTRAINDICATIONS TO USE OF STEROIDS - Cushings disease - traumatic brain injury - late ARDS (after 2 weeks) Jeremy Fernando (2011)