www
advertisement

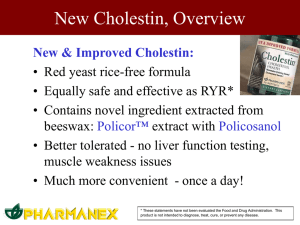
www.consumerlab.com Policosanol: clinical pharmacology and therapeutic significance of a new lipid-lowering agent. Gouni-Berthold I, Berthold HK. Medical Policlinic, University of Bonn, Bonn, Germany. berthold@unibonn.de BACKGROUND: Policosanol is a mixture of higher primary aliphatic alcohols isolated from sugar cane wax, whose main component is octacosanol. The mixture has been shown to lower cholesterol in animal models, healthy volunteers, and patients with type II hypercholesterolemia. METHODS: We reviewed the literature on placebo-controlled lipid-lowering studies using policosanol published in peer-reviewed journals as well as studies investigating its mechanism of action and its clinical pharmacology. RESULTS: At doses of 10 to 20 mg per day, policosanol lowers total cholesterol by 17% to 21% and low-density lipoprotein (LDL) cholesterol by 21% to 29% and raises high-density lipoprotein cholesterol by 8% to 15%. Because higher doses have not been tested up to now, it cannot be excluded that effectiveness may be even greater. Daily doses of 10 mg of policosanol have been shown to be equally effective in lowering total or LDL cholesterol as the same dose of simvastatin or pravastatin. Triglyceride levels are not influenced by policosanol. At dosages of up to 20 mg per day, policosanol is safe and well tolerated, as studies of >3 years of therapy indicate. There is evidence from in vitro studies that policosanol may inhibit hepatic cholesterol synthesis at a step before mevalonate generation, but direct inhibition of the hydroxy-methylglutaryl-coenzyme A reductase is unlikely. Animal studies suggest that LDL catabolism may be enhanced, possibly through receptormediated mechanisms, but the precise mechanism of action is not understood yet. Policosanol has additional beneficial properties such as effects on smooth muscle cell proliferation, platelet aggregation, and LDL peroxidation. Data on efficacy determined by clinical end points such as rates of cardiac events or cardiac mortality are lacking. CONCLUSIONS: Policosanol seems to be a very promising phytochemical alternative to classic lipid-lowering agents such as the statins and deserves further evaluation. Publication Types: Review Protective effect of policosanol on atherosclerotic plaque on aortas in monkeys. Noa M, Mas R. Center of Natural Products, National Center for Scientific Research, Havana City, Cuba. cpn@cnic.edu.cu BACKGROUND: Policosanol is a cholesterol-lowering drug isolated from sugar cane wax with concomitant antiplatelet effects. Previous studies have shown that policosanol prevents lipofundin-induced atherosclerotic lesions in rabbits and rats, including foam cell formation, as well as the development of foam cells in carrageenan-induced granulomas in rats. Policosanol also inhibits smooth muscle cells proliferation induced on rabbit cuffed artery and on forceps-induced arterial wall damage. Furthermore, policosanol administered long term lowered serum cholesterol and prevented the development of atherosclerotic lesions in Macaca arctoides monkeys. The present study was undertaken to determine whether policosanol could change some characteristic features of atherosclerotic lesions, such as macrophage number and immunohistochemical localization of apoA-1 and apoB in aortas of M. arctoides monkeys. METHODS: Fourteen adult male monkeys weighing 6-10 kg and receiving a low fat, protein-rich diet were randomly distributed in three groups: control group (six monkeys) and two other groups (four monkeys/group) treated with policosanol (2.5 and 25 mg/kg) for 54 weeks. Samples of arteries were examined by light microscopy. Monoclonal antibodies were used to evaluate the presence of macrophage, apoA-1 and apoB. RESULTS: Policosanol reduced the presence of macrophages and the occurrence of apoB, whereas increased apoA-1 localization in aortic atherosclerotic lesions compared with control monkeys. CONCLUSIONS: These results suggest the policosanol potential benefit on plaque composition and stability and could explain the protective effects of policosanol on atherosclerosis development. Effects of addition of policosanol to omega-3 fatty acid therapy on the lipid profile of patients with type II hypercholesterolaemia. Castano G, Fernandez L, Mas R, Illnait J, Gamez R, Mendoza S, Mesa M, Fernandez J. Surgical Medical Research Center, Havana City, Cuba. BACKGROUND: Policosanol is a mixture of higher aliphatic primary alcohols purified from sugar-cane wax. The mixture has cholesterol-lowering efficacy, its specific effects being to reduce serum total (TC) and low-density lipoprotein cholesterol (LDL-C), and to increase high-density lipoprotein cholesterol (HDL-C). The effects of policosanol on triglycerides (TG) are modest and inconsistent. Omega3 fatty acids (FA) from fish oil protect against coronary disease, mainly through antiarrhythmic and antiplatelet effects. Omega-3 FA also have lipid-modifying effects, mostly relating to TG reduction. Thus, potential benefits could be expected from combined therapy with omega-3 FA and policosanol. OBJECTIVE: To investigate whether combined therapy with omega-3 FA + policosanol offers benefits compared with omega-3 FA + placebo with respect to the lipid profile of patients with type II hypercholesterolaemia. METHODS: This randomised, double-blind study was conducted in 90 patients with type II hypercholesterolaemia. After 5 weeks on a cholesterol-lowering diet, patients were randomised to omega-3 FA + placebo, omega-3 FA + policosanol 5 mg/day or omega-3 FA + policosanol 10 mg/day for 8 weeks. Omega-3 FA was supplied as 1g capsules (two per day); placebo and policosanol were provided in tablet form. Physical signs and laboratory markers were assessed at baseline and after 4 and 8 weeks on therapy. Drug compliance and adverse experiences (AEs) were assessed at weeks 4 and 8. The primary efficacy variable was LDL-C reduction; other lipid profile markers were secondary variables. RESULTS: After 8 weeks, omega-3 FA + policosanol 5 and 10 mg/day, but not omega-3 FA + placebo, significantly reduced LDL-C by 21.1% and 24.4%, respectively (both p < 0.0001). Omega-3 FA + policosanol 5 mg/day also significantly lowered TC (12.7%; p < 0.01) and TG (13.6%; p < 0.05), and significantly increased HDL-C (+14.4%; p < 0.001). Omega-3 FA + policosanol 10 mg/day significantly decreased TC (15.3%; p < 0.001) and TG (14.7%; p < 0.01), and significantly increased HDL-C (+15.5%; p < 0.0001). Omega-3 FA + placebo significantly reduced TG (14.2%; p < 0.05) but had no significant effect on other lipid profile variables. The proportion of randomised patients in the omega-3 FA + policosanol 5 or 10 mg/day groups that achieved LDLC targets or reductions 15% was significantly greater than in the omega-3 FA + placebo group (p < 0.001). Combined therapy with omega-3 FA + policosanol 5 or 10 mg/day resulted in significantly greater changes in LDL-C, TC and HDL-C than treatment with omega-3 FA + placebo, but did not modify the TG response compared with the omega-3 FA + placebo group. Four patients (two in the omega-3 FA + placebo group and two in the omega-3 FA + policosanol 10 mg/day group) withdrew from the study; none of these withdrawals was due to AEs. Two patients reported mild AEs, namely nausea/headache (one in the omega-3 FA + placebo group) and heartburn (one in the omega-3 FA + policosanol 5 mg/day group). CONCLUSIONS: Policosanol 5 or 10 mg/day administered concomitantly with omega-3 FA 1 g/day improved LDL-C, TC and HDL-C, maintained the reduction in TG attributable to omega-3 FA monotherapy, and was well tolerated. Treatment with omega-3 FA + policosanol could be useful for regulating lipid profile in patients with type II hypercholesterolaemia, but further studies involving larger sample sizes are needed before definitive conclusions can be drawn. PMID: 16050054 [PubMed - in process] !!!!!!!!!!!!!!!!!!!!!!מחקר מעניין An ezetimibe-policosanol combination has the potential to be an OTC agent that could dramatically lower LDL cholesterol without side effects. McCarty MF. NutriGuard Research, 1051 Hermes Avenue, Encinitas, CA 92024, USA. mccarty@pantox.com Although many risk factors influence atherogenesis, LDL appears to play a primary role in this process. In prospective epidemiology, coronary risk increases as LDL cholesterol increases, throughout the entire range of concentrations encountered in healthy humans. Coronary risk is minimal in individuals and populations whose serum cholesterol remains quite low throughout life. Thus, practical strategies for achieving large reductions of LDL cholesterol in the general population could have a dramatic impact on coronary mortality rates. Dietary measures have limited potential in this regard; modest restriction of saturated fat has a rather trivial effect on LDL cholesterol, and the very-low-fat quasi-vegan diets that do have a notable effect in this regard currently have little appeal to the majority of the population. With respect to pharmacotherapy, most available hypolipidemic agents with reasonably potent activity entail side effects or compliance difficulties that would render their use too expensive or impractical for population-wide application. However, two agents may have great potential in this regard: policosanol and ezetimibe. The former, a mixture of long-chain alcohols derived from sugar cane wax, has effects on serum lipids comparable to those of statins, and may work by down-regulating expression of HMG-CoA reductase. However, unlike statins, policosanol appears to be devoid of side effects or risks. Ezetimibe is a newly approved drug that is a potent and highly specific inhibitor of an intestinal sterol permease; in daily doses as low as 10 mg, it suppresses intestinal absorption of cholesterol and decreases serum LDL cholesterol by approximately 18%. No side effects have been seen in clinical doses, and the fact that its hypolipidemic activity is additive to that of statins has generated considerable interest. Both policosanol and ezetimibe can be administered once daily. Future studies should determine whether policosanol, like statins, interacts additively with ezetimibe. If so, it may be feasible someday to produce a tablet combining policosanol and ezetimibe that could reduce LDL cholesterol by about 40%, without side effects, and that could be recommended to virtually anyone whose LDL cholesterol levels were not already ideal. Role of policosanols in the prevention and treatment of cardiovascular disease. Varady KA, Wang Y, Jones PJ. School of Dietetics and Human Nutrition, McGill University, Ste-Anne-de-Bellevue, Quebec, Canada. Policosanols are a mixture of aliphatic alcohols derived from purified sugar cane. When administered at 5 to 20 mg/day, policosanols have been shown to decrease the risk of atheroma formation by reducing platelet aggregation, endothelial damage, and foam cell formation in animals. Additionally, policosanols have been shown to lower total and low-density lipoprotein (LDL) cholesterol levels by 13 to 23% and 19 to 31%, respectively, while increasing high-density lipoprotein (HDL) cholesterol from 8 to 29%. Policosanols are thought to improve lipid profiles by reducing hepatic cholesterol biosynthesis while enhancing LDL clearance. When compared with statins, policosanols exhibit comparable cholesterol-lowering effects at much smaller doses. The mixture is well tolerated when administered to animals; however, a more precise safety profile is needed for humans. In summary, policosanols are a promising resource in the prevention and therapy of cardiovascular disease (CVD), but these results need to be confirmed in independent laboratories. A 6-Month Study on the Toxicity of High Doses of Policosanol Orally Administered to Sprague-Dawley Rats. Gamez R, Aleman CL, Mas R, Noa M, Rodeiro I, Garcia H, Hernandez C, Menendez R, Aguilar C. Center of Natural Products, National Center for Scientific Research, Cubanacan, Havana, Cuba. Policosanol is a cholesterol-lowering drug purified from sugar cane. Previous toxicological studies have not demonstrated any policosanol-related toxicity, even with long-term oral administration at 500 mg/kg, a dose 1,724 times larger than the maximal therapeutic dose (20 mg/day) recommended to date. The present study was undertaken to investigate the oral toxicity of policosanol administered for 6 months in doses up to 5,000 mg/kg to Sprague-Dawley rats. Animals were randomly distributed in five groups (15 animals per dose per sex): a control and four groups given oral policosanol (50, 500, 2,500, or 5,000 mg/kg). Eight treated rats (6 males, 2 females) died during the study, five of them (4 males, 1 female) from among those receiving the highest dose (5,000 mg/kg). According to necropsy, all deaths were related to gavage manipulation of higher doses. Although the differences were not significant, body weight gain and food consumption in the groups receiving 2,500 or 5,000 mg/kg tended to be lower than in the control group. Nevertheless, no drug-related toxicity symptoms were detected. Analysis of blood biochemistry, hematology, organ weight ratios, and histopathological findings did not show significant differences compared with controls, nor any tendency with the dose. Therefore, the present study did not show any new evidence of oral toxicity of policosanol, and the findings observed were a consequence of long-term administration by gastric gavage of the highly concentrated suspensions needed to reach the higher doses. It is concluded that policosanol chronically administered by the oral route is safe and that no drug-related toxicity was demonstrated. Efficacy of over-the-counter nutritional supplements. Davidson MH, Geohas CT. Department of Preventive Cardiology, Rush-Presbyterian-St. Luke's Medical Center, 1725 West Harrison Street, Suite 1159, Chicago, IL 60612, USA. mdavidson@protocare.com More than 100 million people in the United States report using nutritional supplements. Most people are under the impression that nutritional supplements offer health benefits and are closely regulated to ensure safety and efficacy. Unfortunately, the Dietary Supplement Health and Education Act of 1994 allows for the promotion of nutritional supplements without review by the United States Food and Drug Administration; therefore, it is important to evaluate the efficacy and safety of these supplements. There is strong scientific evidence supporting the use of plant sterols/stanols, omega-3 fatty acids, niacin, folate, vitamin B(6)/B(12), and tree nuts. There is potential evidence for the health benefits of soy protein, tea extracts, policosanol, guggulipids, coenzyme Q10, and L-arginine. There has been a lack of evidence for the health benefits of garlic and antioxidants. Comparison of the efficacy, safety and tolerability of original policosanol versus other mixtures of higher aliphatic primary alcohols in patients with type II hypercholesterolemia. Castano G, Fernandez L, Mas R, Illnait J, Fernandez J, Mesa M, Alvarez E, Lezcay M. Medical and Surgical Research Center, National Center for Scientific Research, Havana, Cuba. This randomized, double-blind study was undertaken to compare the efficacy and tolerability of policosanol and Octa-60 in patients with type II hypercholesterolemia. After 4 weeks on a diet, 110 patients were randomized to policosanol or Octa-60 5 mg tablets once a day for 5 weeks. The dose was then doubled to 10 mg/day for the next 5 weeks. Policosanol 5 and 10 mg/day significantly lowered low-density lipoproteincholesterol (LDL-C) (p<0.0001 and p<0.00001), the main efficacy variable, by 18.6% and 30.2%, while Octa-60 significantly reduced (p<0.05) LDL-C by 10.0% at study completion only. The frequency of policosanol patients reaching reductions of LDL-C > or = 15% after 5 mg/day (37/55; 67.3%) and 10 mg/day (47/55; 88.7%) was greater (p<0.01 and p<0.01) than in the Octa-60 group, which was 5/55 (9.1%) and 20/55 (36.4%). Likewise, the frequency of patients reaching LDL-C values of <3.4 mmol/l at study completion was greater (p<0.001) in the policosanol group (39/55, 70.9%) than in the Octa-60 group (6/55, 10.9%). Policosanol 5 and 10 mg/day significantly lowered (p<0.00001) total cholesterol (TC) (13.4% and 20.4%), LDL-C/high-density lipoprotein-cholesterol (HDL-C) (22.1% and 37.0%) and TC/HDL-C (17.2% and 28.2%). Octa-60 at 10 mg/day lowered (p<0.05) TC (8.7%), LDL-C/HDL-C (12.6%) and TC/HDL-C (9.4%). HDL-C was increased (p<0.001 and 0.0001) by policosanol 5 and 10 mg/day (5.6% and 12.5%) but was unchanged by Octa-60. In both groups, triglycerides remained unchanged. Both treatments were safe and well tolerated. Octa60, but not policosanol, significantly increased glucose and alanine aminotransferase, but individual values were within the normal range. Four patients (two from each group) discontinued the trial, but only one (in the Octa-60 group) did so because of an adverse event (AE) (skin rash). Overall, three patients (all from the Octa-60 group) reported AEs. In conclusion, original policosanol at 5 and 10 mg/day, but not Octa 60, was effective in patients with type II hypercholesterolemia. Thus, policosanol reached the efficacy criterion for LDL-C reduction in both steps, while Octa-60 failed to reach this goal. In addition, policosanol was better tolerated than Octa-60. Antiplatelet effects of policosanol (20 and 40 mg/day) in healthy volunteers and dyslipidaemic patients. Arruzazabala ML, Molina V, Mas R, Fernandez L, Carbajal D, Valdes S, Castano G. Center of Natural Products, National Center for Scientific Research Cubanacan, Havana City, Cuba. 1. The present study was undertaken to compare the effects of a higher dose of policosanol, a cholesterol-lowering drug, (40 mg/day) with the effects of 20 mg/day policosanol on platelet aggregation in healthy volunteers and type II hypercholesterolaemic patients. 2. Study subjects were randomized to receive, under double-blind conditions, placebo or policosanol (20 or 40 mg/day) for 30 days once a day. Blood sampling was performed at baseline and after 30 days on therapy. 3. Platelet aggregation was induced with three aggregating agents: arachidonic acid (AA), collagen and low doses of ADP. 4. Policosanol (20 and 40 mg/day) moderately yet significantly reduced platelet aggregation, but no differences were observed in the effects produced by either dose of policosanol. In healthy volunteers, policosanol at 20 and 40 mg/day inhibited aggregation induced by 2 mmol/L AA (28.2 and 24.9%, respectively), 1 micro g/mL collagen (21.1 and 20.2%) and 1 micro mol/L ADP (30.9 and 29.1%). Changes that occurred following the administration of placebo were not significant, although an upward trend for collagen- and ADP-induced aggregation occurred in normal and hypercholesterolaemic subjects, respectively, thus partially masking the effects of policosanol on these responses. 5. The antiplatelet effects of policosanol at 20 and 40 mg/day in hypercholesterolaemic patients were also similar, so that both doses inhibited aggregation induced by 1.5 mmol/L AA (20.1 and 33.0%, respectively), 0.5 micro g/mL collagen (22.7 and 21.1%) and 1 micro mol/L ADP (40.5 and 34.7%). 6. In addition, after 30 days of therapy, 20 and 40 mg/day policosanol significantly (P < 0.01) reduced low-density lipoprotein-cholesterol (15.9 and 17.0%, respectively) and total cholesterol (12.4 and 12.3%, respectively; P < 0.05), yet increased high-density lipoprotein-cholesterol values by 5% in both groups (P < 0.05). 7. Triglycerides were decreased compared with baseline, but not with respect to the placebo. 8. We conclude that the antiplatelet effects induced by 40 mg/day policosanol administered for 30 days to healthy volunteers and to hypercholesterolaemic patients were similar to the effects induced by 20 mg/day policosanol. Thus, no enhancement of the response was achieved with the use of a higher dose of policosanol in study patients. Publication Types: Pharmacotherapy for dyslipidaemia--current therapies and future agents. Bays H, Stein EA. L-MARC Research Center, 3288 Illinois Avenue, Louisville, KY 40213, USA. HBaysMD@aol.com Current lipid-altering agents that lower low density lipoprotein cholesterol (LDL-C) primarily through increased hepatic LDL receptor activity include statins, bile acid sequestrants/resins and cholesterol absorption inhibitors such as ezetimibe, plant stanols/sterols, polyphenols, as well as nutraceuticals such as oat bran, psyllium and soy proteins; those currently in development include newer statins, phytostanol analogues, squalene synthase inhibitors, bile acid transport inhibitors and SREBP cleavage-activating protein (SCAP) activating ligands. Other current agents that affect lipid metabolism include nicotinic acid (niacin), acipimox, high-dose fish oils, antioxidants and policosanol, whilst those in development include microsomal triglyceride transfer protein (MTP) inhibitors, acylcoenzyme A: cholesterol acyltransferase (ACAT) inhibitors, gemcabene, lifibrol, pantothenic acid analogues, nicotinic acid-receptor agonists, anti-inflammatory agents (such as Lp-PLA(2) antagonists and AGI1067) and functional oils. Current agents that affect nuclear receptors include PPAR-alpha and -gamma agonists, while in development are newer PPAR-alpha, -gamma and -delta agonists, as well as dual PPAR-alpha/gamma and 'pan' PPAR-alpha/gamma/delta agonists. Liver X receptor (LXR), farnesoid X receptor (FXR) and sterol-regulatory element binding protein (SREBP) are also nuclear receptor targets of investigational agents. Agents in development also may affect high density lipoprotein cholesterol (HDL-C) blood levels or flux and include cholesteryl ester transfer protein (CETP) inhibitors (such as torcetrapib), CETP vaccines, various HDL 'therapies' and upregulators of ATP-binding cassette transporter (ABC) A1, lecithin cholesterol acyltransferase (LCAT) and scavenger receptor class B Type 1 (SRB1), as well as synthetic apolipoprotein (Apo)E-related peptides. Fixed-dose combination lipid-altering drugs are currently available such as extended-release niacin/lovastatin, whilst atorvastatin/amlodipine, ezetimibe/simvastatin, atorvastatin/CETP inhibitor, statin/PPAR agonist, extendedrelease niacin/simvastatin and pravastatin/aspirin are under development. Finally, current and future lipid-altering drugs may include anti-obesity agents which could favourably affect lipid levels. --------------- Medical lipid-regulating therapy: current evidence, ongoing trials and future developments. Evans M, Roberts A, Davies S, Rees A. Department of Metabolic Medicine, Diabetes and Endocrinology, University of Wales College of Medicine, Cardiff, Wales. marc.evans2@ntlworld.com Coronary heart disease (CHD) is a major cause of morbidity and mortality worldwide. Elevated low density lipoprotein-cholesterol (LDL-C) and reduced high density lipoprotein-cholesterol (HDL-C) levels are well recognised CHD risk factors, with recent evidence supporting the benefits of intensive LDL-C reduction on CHD risk. Such observations suggest that the most recent National Cholesterol Education Program Adult Treatment Panel III guidelines, with LDL-C targets of 2.6 mmol/L, may result in under-treatment of a significant number of patients and form the basis for the proposed new joint European Societies treatment targets of 2 and 4 mmol/L, respectively, for LDL and total cholesterol. HMG-CoA reductase inhibitors (statins) reduce LDL-C by inhibiting the rate-limiting step in cholesterol biosynthesis and reduced CHD event rates in primary and secondary prevention trials. The magnitude of this effect is not fully accounted for by LDL-C reduction alone and may relate to effects on other lipid parameters such as HDL-C and apolipoproteins B and A-I, as well as additional anti-inflammatory effects. With increasing focus on the benefits of intensive cholesterol reduction new, more efficacious statins are being developed. Rosuvastatin is a potent, hydrophilic enantiomeric statin producing reductions in LDL-C of up to 55%, with about 80% of patients reaching European LDL-C treatment targets at the 10 mg/day dosage. The Heart Protection Study (HPS) demonstrated that LDL-C reduction to levels as low as 1.7 mmol/L was associated with significant clinical benefit in a wide range of high-risk individuals, including patients with type 2 diabetes mellitus, or peripheral and cerebrovascular disease, irrespective of baseline cholesterol levels, with no apparent lower threshold for LDLC with respect to risk. Various large endpoint trials, including Treating to New Targets (TNT) and Study of Effectiveness of Additional reductions in Cholesterol and Homocysteine (SEARCH) will attempt to further address the issue of optimal LDL-C reduction. At low LDL-C levels, HDL-C becomes an increasingly important risk factor and is the primary lipid abnormality in over half of CHD patients, with the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study set to assess the effect of raising HDL-C on cardiovascular events in patients with low HDL-C and LDL-C levels below 3 mmol/L. A variety of agents are being developed, which affect both LDL-C and HDL-C metabolism, including inhibitors of acyl-coenzyme Acholesterol acyl transferase, microsomal transfer protein and cholesterol ester transfer protein, as well as specific receptor agonists. Ezetimibe is a selective cholesterol absorption inhibitor, which produces reductions in LDL-C of up to 25 and 60% reduction in chylomicron cholesterol content with a 10 mg/day dosage. A 1 mmol/L reduction in LDL-C results in a 25% reduction in cardiovascular risk, independent of baseline LDL-C levels. Growing evidence supports the concept that lower is better for LDL-C and that increasing HDL-C represents an important therapeutic target. Furthermore, there is growing appreciation of the role of inflammation in atherogenesis. Consequently, increasing numbers of people should receive lipidregulating therapy with the development of newer agents offering potential mechanisms of optimising lipid profiles and thus risk reduction. In addition, the pleiotropic anti-inflammatory effects of lipid lowering therapy may provide further risk reduction. Consistency in efficacy and safety of ezetimibe coadministered with statins for treatment of hypercholesterolemia in women and men. Bennett S, Sager P, Lipka L, Melani L, Suresh R, Veltri E; Ezetimibe Study Group. Cardiology Associates, P.C., Washington, DC, USA. BACKGROUND: Women are often not treated as aggressively as men to control levels of low-density lipoprotein cholesterol (LDL-C), despite evidence that women and men realize comparable cardiovascular benefit from lipid-lowering therapy. Statins are the most effective drugs currently available for treating hypercholesterolemia. Despite the impressive cholesterol-lowering capacity of statins, however, many patients on statin therapy fail to reach established target levels of LDL-C. The cholesterol absorption inhibitor, ezetimibe, blocks the intestinal absorption of dietary and biliary cholesterol, a mechanism of action complementary to that of statins, which inhibit hepatic cholesterol synthesis. Ezetimibe coadministered with statins produces significant incremental reductions in LDL-C compared with statin monotherapy. METHODS: Four randomized, double-blind, placebo-controlled, balanced-parallel group trials compared the efficacy and safety of statin monotherapy (lovastatin or pravastatin 10, 20, or 40 mg; simvastatin or atorvastatin 10, 20, 40, or 80 mg) vs. ezetimibe 10 mg plus statin (as above). A gender subset analysis (women, n = 1065; men, n = 796) on data pooled across these four trials was carried out to determine whether ezetimibe plus statin for the treatment of hypercholesterolemia is equally efficacious in women and men. RESULTS: Compared with statin monotherapy, ezetimibe plus statin demonstrated greater efficacy in reducing blood levels of LDL-C, apolipoprotein B, and triglycerides and raising high-density lipoprotein cholesterol. The beneficial effects of ezetimibe were comparable in women and men. The safety profile of subjects receiving ezetimibe plus statin was similar to that of patients receiving statin monotherapy and similar between the two sexes. CONCLUSIONS: Ezetimibe plus statin was more effective than statin alone in improving the lipid profile of patients with hypercholesterolemia and was equally efficacious in women and men. Ezetimibe plus statin was well tolerated and had a favorable safety profile in both patient subgroups. Ezetimibe coadministered with statins, a dual inhibition treatment strategy that targets both cholesterol absorption and synthesis, is an effective therapeutic option for women with hypercholesterolemia. !!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!! Inhibition of cholesterol absorption by the combination of dietary plant sterols and ezetimibe: Effects on plasma lipid levels. Jakulj L, Trip MD, Sudhop T, von Bergmann K, Kastelein JJ, Vissers MN. The consumption of plant sterols as well as treatment with ezetimibe both reduce cholesterol absorption in the intestine. The mechanism of action of both treatment modalities is not similar and the consequences of combination treatment are unknown. Therefore, we performed a double-blind placebo controlled cross-over study for the plant sterol component with open-label ezetimibe treatment to determine the individual consequences of plant sterol intake and ezetimibe as well as their combined effects on safety and plasma lipid levels. Forty mildly hypercholesterolemic subjects were randomized to the following treatments for four weeks each: 10 mg/d ezetimibe in combination with 25 g/d of control spread; 10 mg/d ezetimibe in combination with 25 g/d of spread containing 2.0 g of plant sterols; 25 g/d of spread containing 2.0 g of plant sterols; and placebo treatment consisting of 25 g/d of control spread. Combination treatment of plant sterols and ezetimibe reduced LDL-C by 25.2% or 1.06 mmol/L (p<0.001) as compared to 4.7% or 0.23 mmol/L (p=0.006) by plant sterols and to 22.2% or 0.94 mmol/L (p<0.001) by ezetimibe monotherapy. LDL-C reduction conferred by the combination treatment did not differ significantly from ezetimibe monotherapy (-3.5% or -0.12 mmol/L; p=0.13). In addition, the ratio of the cholesterol precursor lathosterol to cholesterol increased with all treatments. The ratios of sitosterol and campesterol to cholesterol increased after plant sterol treatment, and decreased upon ezetimibe and combination therapy. No differences were observed for liver transaminases and creatine phosphokinase between treatments. Our results demonstrate that the combination of plant sterols and ezetimibe has no therapeutic benefit over ezetimibe monotherapy in subjects with mild hypercholesterolemia. בטיחות של אזטימיד וסטטינים יחד ולחוד A multicenter, randomized, double-blind, placebo-controlled, factorial design study to evaluate the lipid-altering efficacy and safety profile of the ezetimibe/simvastatin tablet compared with ezetimibe and simvastatin monotherapy in patients with primary hypercholesterolemia. Bays HE, Ose L, Fraser N, Tribble DL, Quinto K, Reyes R, Johnson-Levonas AO, Sapre A, Donahue SR; Ezetimibe Study Group. Louisville Metabolic and Atherosclerosis Research Center, 3288 Illinois Avenue, Louisville, KY 40213, USA. HBaysMD@aol.com OBJECTIVE: The purpose of this study was to evaluate the efficacy and safety profile of ezetimibe/simvastatin(EZE/SIMVA) combination tablet, relative to ezetimibe (EZE) and simvastatin (SIMVA) monotherapy, in patients with primary hypercholesterolemia. METHODS: This was a randomized, multicenter, doubleblind, placebo-controlled, factorial design study After a 6- to 8-week washout period and 4-week, single-blind, placebo run in, hypercholesterolemic patients (low-density lipoprotein cholesterol [LDL-C], 145-250 mg/dL; triglycerides [TG], < or =350 mg/dL) were randomized equally to 1 of 10 daily treatments for 12 weeks: EZE/SIMVA 10/10, 10/20, 10/40, or 10/80 mg; SIMVA 10, 20, 40, or 80 mg; EZE 10 mg; or placebo. The primary efficacy analysis was mean percent change from baseline in LDL-C to study end point Secondary end points included percent changes in other lipid variables and C-reactive protein [CRP]. RESULTS: There were 1528 patients randomized to treatment (792 women, 736 men); mean (SD) age ranged from 54.9 (112) years to 56.4 (10.6) years across pooled treatment groups. The treatment groups were well balanced for baseline demographics. Pooled EZE/SIMVA was associated with greater reductions in LDL-C than pooled SIMVA or EZE alone (P < 0.001). Depending on dose, EZE/SIMVA was associated with reductions in LDL-C of -44.8% to -602%, non-high-density lipoprotein cholesterol of -40.5% to -55.7%, and TG of -22.5% to -30.7%; high-density lipoprotein cholesterol increased by 5.5% to 9.8%. EZE/SIMVA was associated with greater reductions in CRP and remnant-like particle-cholesterol than SIMVA alone (P < 0.001). More patients receiving EZE/SIMVA versus SIMVA achieved LDL-C concentrations <100 mg/dL (78.6% vs 45.9%; P < 0.001). EZE/SIMVA was generally well tolerated, with a safety profile similar to SIMVA monotherapy There were no significant differences between EZE/SIMVA and SIMVA in the incidence of consecutive liver transaminase levels > or =3 times the upper limit of normal (ULN) (1 .5% for EZE/SIMVA and 1.1% for SIMVA; P = NS) or creature kinase levels > or =10 times ULN (0.0% for EZE/SIMVA and 02% for SIMVA; P = NS). CONCLUSION: The EZE/SIMVA tablet was a highly effective and well-tolerated LDL-C-lowering therapy in this study of patients with primary hypercholesterolemia.