8. Summary of the HIS assessment
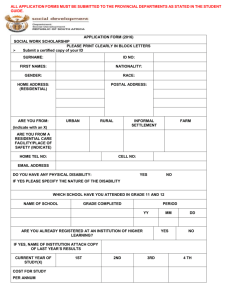
advertisement

Health Metrics Network Viet Nam Health Information System: Review and Assessment December, 2006 By Ministry of Health Coordinated by [Name and address of recipient institution] Dr.Duong Huy Lieu Director of Planning & Finance Department Ministry of Health Contact authors Nguyen Thi Tinh - Health Statistics Informatics Division, Planning & Finance Dept. MOH Hoang Thanh Huong - Health Statistics Informatics Division, Planning & Finance Dept. MOH Le Tran Ngoan - Hanoi Medical University Do Thi Phuong Lan - Health Statistics Informatics Division, Planning & Finance Dept. MOH Page 1 of 70 Acknowledgements This work was supported by the HMN and Ministry of Health of Viet Nam. The working group, under the direct supervision of the Health Information System Sterring Committee, Ministry of Health (MoH), organized two workshops assessing the HIS in the north and south respectively. Based on the assessment of these workshops, the Wowrking Group conducted in-depth interviews with sub-systems and the information systems of some concerned sectors and provinces. This was a quite comprehensive assessment of the components of the system using the tools of the HMN. The aim of the assessment is to deine strengths and weaknesses as well as difficulties and shortcomings to tailor solutions for consolidating and upgrading the HIS. Assuring data provided from the system will be evidence for the sterring, mnagement and policy making in order to effectively utilize resources invested in the health sector to successfully contribute to the completion of the strategic objective of health for all by 2015 and beyond. On behalf of the Sterring Committee of the HIS, the MoH would like to sincerely thank the HMN for financial support for the implementation of the Project: “Strengthening HIS”, including the assessment of the HIS. Our sincere thanks should also be extended to Dr. Churnrurtai Kanchanachitra, Dr. Waranya Teokul, consultants of HMN and Dr.Yok Ching Chong, health information consultant of WHO Regional Office for their active and useful technical support for this assessment. We should also extend our acknowledgements to the Ministry of Justice, National Committee on Population, Family and Child Affairs, General Statistics Office (GSO), various departments, institutes, national health programs and 3 provinces, namely: Khanh Hoa, Thai Nguyen and Nam Dinh for their valuable assistance and close coordiantion during the assessment process. The MoH hope to receive continued support from HMN, international experts and collaboration from various institutions from within and outside the health sector for the development and implementation of the strategy for developing the HIS of Vietnam. On behalf of the HMN Steering Committee Dr. Duong Huy Lieu Page 2 of 70 Table of contents 1. BACKGROUND ......................................................................................................................... 7 The central level ....................................................................................................................... 8 2. Context and resources ............................................................... Error! Bookmark not defined. 2.1. Policy and planning ............................................................ Error! Bookmark not defined. 2.2. HIS institutions, human resources and financing ............................................................... 14 2.2.1. Comprehensive health ifnormation system .................................................................. 14 2.2.3. Sub-sysems in national health programs...................................................................... 17 2.2.3. Communicable diseases surveillance system............................................................... 18 2.2.4. Information system in other sectors, ministries ........................................................... 18 2.2.5. Assessment of facilities, manpower and financial resource of HIS (See Table 1) ...... 18 2.3. HIS infrastructure (Table 1) ............................................................................................... 19 3. Essential Health Indicators ........................................................................................................ 21 4. Data sources .............................................................................................................................. 22 4.1. Census ................................................................................................................................. 22 4.2. Vital statistics ..................................................................................................................... 22 4.3. Population based survey ..................................................................................................... 24 4.4. Medical records (including disease surveillance systems) ................................................. 24 4.5. Professional service record ................................................................................................. 25 4.6. Administrative records ....................................................................................................... 25 4.6.1. Database/ infrastructure mapping ................................................................................ 25 4.6.2.Database on human resource ........................................................................................ 25 4.6.3. Information on finance and expenditures on health services ....................................... 26 4.6.4. Information on equipment............................................................................................ 26 5. Data management ...................................................................................................................... 29 5.1. GHSIS:................................................................................................................................ 29 5.2. EPI:. .................................................................................................................................... 30 5.3. Malaria control program ..................................................................................................... 31 5.4. Therapy related information sub-system: ........................................................................... 31 6. Information products ................................................................................................................. 33 6.1. Indicators on health status .................................................................................................. 35 6.1.1. Under-5 mortality rate.................................................................................................. 35 6.1.2. MMR ............................................................................................................................ 35 6.1.3. Adult mortality rate ...................................................................................................... 35 6.1.4. HIV prevalence ............................................................................................................ 36 6.1.5. Low weight under-5 children ....................................................................................... 36 6.2. Indicators of the health system ........................................................................................... 37 6.2.1. Outpatient treatment: metod of collection ................................................................... 37 6.2.2. Immunization for children < 12 years of age ............................................................... 37 6.2.3. Professionally attended deliveries ................................................................................ 38 6.2.4 Percentage of success in treating TB ............................................................................ 39 6.2.5 Percentage of children <59 months old sleeing in mosquito-nets ................................ 39 6.2.6. Government general expenditures on health per capita ............................................... 40 6.2.7. Private health expenditure per capita ........................................................................... 41 6.2.8. Distribution rate of health staff (total by professional category) ................................. 41 6.3. Indicators on risk factors ................................................................................................. 41 6.3.1. Smoking prevalence ..................................................................................................... 41 6.3.2. Percentage of condom use with high-risk sexual behaviours ...................................... 42 6.3.3. Percentage of households using improved water sources ............................................ 42 6.4. Supplementary indicators ................................................................................................... 43 6.4.1. IMR .............................................................................................................................. 43 6.4.2. Low-weight birth rate (<2500Gram) ........................................................................... 43 Page 3 of 70 6.4.3. Morbidity/mortality of 10 leading diseases ................................................................. 44 7. Information dissemination and utilization................................................................................. 44 7.1. Data analysis and use .......................................................................................................... 44 7.2. Policies and communication ............................................................................................... 45 7.3. Plans and setting priority .................................................................................................... 45 7.4. resource allocation .............................................................................................................. 45 7.5. Action performance ............................................................................................................ 45 8. Summary of the HIS assessment ............................................................................................... 46 8.1. Resources ............................................................................................................................ 46 8.2. Data soruces ........................................................................................................................ 47 8.3. Data management ............................................................................................................... 48 9. HIS orientation .......................................................................................................................... 50 9.1. Analysis of strenths, weaknesses, difficulties, challenges, opportunities of HIS ............... 50 9.2. Areas potentially developing HIS ....................................................................................... 51 9.3. Opportunities for donor coordination ................................................................................. 52 9.4. Identifying priorities for strengthening HIS ....................................................................... 52 Annex......................................................................................... Error! Bookmark not defined. Page 4 of 70 List of Tables Table 1 Overall results of HIS resources in Hanoi and Ho Chi Minh cities ................................. 20 Table 2 Results of indicators in Hanoi and Ho Chi Minh cities ................................................... 21 Table 3 Scores of data sources ...................................................................................................... 27 Table 4 Results of data sources ..................................................................................................... 28 Table 5 Results of data management............................................................................................. 32 Table 6 Information products of health status in Hanoi and Ho Chi Minh cities ......................... 34 Table 7 Overall scores in Hanoi and Ho Chi Minh cities ............................................................. 42 Table 8 Overall results in Hanoi and Ho Chi Minh cities ............................................................. 46 List of Figures Figure1: The organization structure of the Vietnam health sector bellow ..................................... 8 Figure 2: HMN framework ........................................................................................................... 11 Figure 3: Organizational structure of general health statistics information system ...................... 16 Figure 4: Flow of information ....................................................................................................... 29 Figure 5: Flow of therapy related information .............................................................................. 31 Figure 6: Overall health information system in Hanoi and Ho Chi Minh cities ........................... 47 Figure 7: Data sources in Hanoi and Ho Chi Minh cities ............................................................. 48 Figure 8 Information products in Hanoi and Ho Chi Minh cities ................................................. 48 Figure 9: Information products in Hanoi and Ho Chi Minh cities ................................................ 50 Page 5 of 70 Acronyms CBR CDR CHS DHB DHC DOTS EPI GGHE GHSIS GSO HDI HIS HIV HMN IARC IMR MMR MoF MOH PHS TB Crude Birth Rate Crude Death Rate Commune Health Station District Health Bureau District Health Center Direct Observation Treatment Strategy Extended Program of Immunization General Government Expenditure on Health General health statistical information system General Statistics Office Human Development Index Health Information System Human Immunodeficiency Virus Health Metrics Network International Agency for Research on Cancer Infant Mortality Rate Maternal Mortality Rate Ministry of Finance Ministry of Health Provincial Health Bureau Tuberculosis Page 6 of 70 1. BACKGROUND Vietnam is a developing country in Southeast Asia with a surface area of 332,600 sq. km, stretching along the 3,260 km easten coastline of the Indochinese Peninsula. The country, in the shape of the letter S, borders Laos and Cambodia to the West and China to the North. Approcimately 80% of Vietnam’s land is mountainous, highland and jungles; only 20% is flat land. Vietnam has 64 provinces and municipalities with 659 districts and equivalents and 10,732 communes. There are 8 different regions Vietnam is the second most populous nation in the Southeast Asia. According to the 2005 survey, Vietnam had a population of over 83 million, of whom men account for 49.15% and women 50.85%. The population growth rate is 1.33 %. The country has 54 different ethnic groups of which the Kinh represents 87% of the total; the rest are ethnic minorities living scattered all over the country. Estimated GDP per capita in 2004 was approximately 560 US Dollars and Government health budget per capital is approximately of 15USD. Sine 1945, the Leadership of Socialist Republic of Vietnam stressed hunman development in general and Health and Education in particular, consequently the literary rate in Vietnam over the past years always stood at a high levele of 93%. The health service provide network has been developed covering whole country from grassroots to higer level. 1.1. Health situation Sine transferring from a centralized, planned economy to a socialist-orientated market economy, the Vietnam’ economy has achieved high annual growth. The average GDP growth rate of each year was about 7% and the people’living condition of a majority of population has markedly improved. The reforms conducted in the past years have not only brought about economic growth but also consider ameliorated the Health status. The Vietnam’people health indicators are even better than those of other countries with the same level of income. According to the Health statistics yearbook of the Ministry of Health: the life expectancy was 71,3 in 2002, maternal mortality ratio was 80 per 100000 live births, infant mortality was 17.5 per 1000 liver birth, Under-five mortality rate was 27.55 Malnutrition rate among the under five was 25.2 in 2005. Vietnam’s human development indexes ranked 108 among 177 nations while its average per-capita income only stood at 124 out to 1779 Report of UNDP in 2004). The mortality and morbidity patterns have been major changes in Vietnam over the last two decades. Infection and parasitic diseases and malnutrition have the tendency of deceasing whilst non-communicable diseases and accidents/injuries have been on the rise. In 1976, communicable diseases were the cause of 53.06 % of all deaths; this rate was only 16.53 in 2005. Mortality from accidents/injuries/ poisonings which were 2.23% in 1976 decreased to 22.33% in 2005. Other non-communicable diseases such as cancers, diabetes, cardiovascular diseases and mental diseases are on the rise. Among the five leading causes of mortality, traffic accidents is the highest (26.7 per 100 000 inhabitants). The growing rate of road injuries has become alarming. Data from the National Traffic Safety Committee show that in the nearly 10 years, the mortality of road accidents went up 2.42 time in 2005 compared with 1995 . Thank to the vast public health network, the Health sector has effectively delivered health protective and curative services to people. The vertical National Health programs have brought about enormous results which have contributed substantially to the improvement of people’s health. 1.2.Health service provision network of Vietnam Page 7 of 70 Right after the foundation of the Democratic Republic of Vietnam had decided to develop human resources in which development of people’ health care and protection services provide were a high priority in the strategy for socio-economic development of country. The health network has being covered whole country with many defferent fields. The central level At the top, the Ministry of Health (MOH) is a Government agency exercising State management in the field of people’s health care, which include preventive medicine, consultation and treatment, rehabilitation, traditional medicine, pharmaceuticals, hazardous effects of cosmetics to human health, food hygiene and safety, and medical equipment and health facilities; State management; and representing State ownership and managed by MOH in accordance with the stipulations of law Provincial level: Provincial Health Services are technical agencies administered by the People’s Committee of provinces or centrally -run cities. They assist the Provincial People’s Committee in exercising the State management within the province in people’s health care, which includes preventive medicine, consultation and treatment, rehabilitation, traditional medicine and pharmaceuticals, hazardous effect of cosmetics to human health, food hygiene and safety, and medical equipment and health facilities, public services belonging to the health sector; and exercising a number of authority as delegated by Provincial People’s Committees in accordance with the stipulations of law. Provincial Health Services are administered by the Provincial People’s Committees in respect of its organization, staff and activities whilst its professional operations are subjected to the MOH’s guidance, instructions, supervision and inspection. District level District Health Centre are technical agencies administered by the People’s Committees of districts, precincts, provincial capitals or towns. They exercise State management in people’s health care and health promotion in the district. which includes preventive medicine, consultation and treatment, rehabilitation, traditional medicine and pharmaceuticals, hazardous effects of cosmetics to human health, food hygiene and safety, medical equipment and health facilities, exercising management over health centre at the communes, wards and/or district town; and executing a number of tasks and authority as devolved by the Provincial People’s committees and delegated by Provincial health Services. District People’s Committees in respect of its organization administer district Health Centre. staff and operations whilst its professional work is subjected to guidance and supervision from the Provincial Health Services. Commune level: Health Centre in communes are the primary health care units accessible to people. As part of the State health system, these health centres have the tasks of providing primary health care services, early detection of epidemic outbreaks, treating common diseases and attending normal deliveries. Other tasks include mobilization of community participation in family planning practices, hygiene and prophylactics and health promotion. The setting up, merger or dissolution of communal health centre. Wards or district towns will be decided by People’s Committees of Provinces or centrally- run cities if and when proposed by the people’s committees at communes, districts and the Director of the Provincial Health Services. Figure1: The organization structure of the Vietnam health sector bellow Page 8 of 70 ORGANISATIONAL CHART OF THE HEALTH SECTOR GOVERNMENT 1. Central level MINISTRY OF HEALTH Professional units under the Ministry - Curative: 30 hospitals with beds - Preventive: 17 institutes or centres - Quality Control: 5 instituties or centres - Training; 14 schools or colleges - Centre for health education and communication: 17 units - 14 Dept. & Administrations - The Cabinet - Inspectorate Provincial People’s Committees PROVINCIAL HEALTH SERVICE - Office - Inspectorate - Divisions 2. Provincial and municipal levels Professional units under the PHS - General & Specialised hospitals for curative care - Preventive Health Centres - Quality inspection and control - Training: middle level schools or colleges - Centre for health education and communication People Committees at dists DISTRICT HEALTH BUREAU 3. District level - District General Hospitals - Polyclinics People Committees at Communes 4. Communal level COMMUNAL HEALTH CENTRES - Head - Health workers Village Health Workers Notes: State Management Professional guidance Page 9 of 70 District Preventive Health Centres Recognizing the importance of information in management, steering and policy making, immediately aftr the establishment, the Government of Vietnam and leaders of the MoH paid attention to the development and strengthening of the HISS. The information statistic system has developed nationwide, closely linked to the health service provision network. Due to special characteristics of health care and protection for the people, the health service provision network incldues many other sectors such as curative care, preventive care, reproductive health care, pharmaceutical production and trading, training and rehabilitation etc. In order to exercise the strategic goal of the health sector and address issues geratly affecting health, the Government of Vietnam and internaitonal multi-lateral and bilateral organizations have made investment in the implementation of many national health programs such as tuberculosis (TB) control. Malaria control, goiter contron, leprosy control, extended program of immunization (EPI), reproductive health care, nutrition, mental health, Dengue fever control, food safety and hygiene .... Allt hese programs are under the management and supervision of various departments within the MoH, institutes, specialized hospitals: the TB control program under the management of the Hospital of TB and Lung Diseases; the malarial controlo program under the management of the Institute of Malaria, Parasitology and Insectology; the goiter control program under the management of the Endocrine Hospital; the leprosy control program under the management of the Dermatology Institute; the EPI and Dengue fever control program under the management of the Central Hygiene and Epidemiology Institute; the reproductive health care under the management of the Department of Reproductive Health; the malnutrition control program under the management of the Nutrition Institute; the mental health program under the management of the Central Mental Hospital; the food hygiene and safety program under the Vietnam Administration of Food Safety; the HIV/AIDS control program under the Vietnam Administration of HIV/AIDS. Recognizing the requiorement of management, evaluating progress and professional supervision of each program and area, each runs its own statistical information system (called sub-system). The activities of national health programs make significant contributions to improvement of health of people, but the integration of the collection and analysis of information across areas and national health programs still reveal many drawbacks that need further improvement. The aggregated data for health management, assessing health outcomes and effectiveness of the health sector and people’s health status is provided by the comprehensive statistical information system. Therefore, the health information is collected from the following systems: - General health statistical information system - Information sub-systems of various areas and national health programs. - Communicable diseases surveillance system. - Statistical information system of other sectors, ministries, such as GSO, NAtional Committee on Population, Family and Child Affairs, Ministry of Justice... Each information system and sub-system is accompanied by separate record and reporting forms and relatively independent activities. Despite the fact that many systems collect and process data at the same time, the requirement of information serving management, supervision and policy making has not been met. The MoH has made assessments to find out causes of drawbacks of health statistical information system, yet, they have only focused on every aspect of the system and within a very modest scope, for example: (1) Assessment of form system in 3 districts and selected national health programs under support of UNICEF in 2001; (2) Assessment of information need in 2 districts, 6 communes and Bac Giang provincial Health Bureau under financial support by WHO in 2005. These assessments do not fully reflect strengths, weaknesses, difficulties and shortcomings of the whole system. In April 2006, under the financial and technical support, the MoH collaborated with the GSO to convene an assessment and in-depth interview workshop. This was a comprehensive assessment of the health information system, from the inputs to outcomes. This assessment aimed to function as a basis for developing a strategy for health statistical information system development up to 2015 and 2020. Page 10 of 70 HEALTH INFORMATION SYSTEM ASSESSMENT The MoH used the HMN tool set for assessing 6 components of the HIS. Figure 2: HMN framework HMN Framework Health information system components & standards Roadmap for implementation Principles HIS Resources Indicators Process Data Sources Data Management Tools Information Products HMN Goal Increase availability, accessibility, quality and use of health information that is critical for decision making at country & global levels. Dissemination and use After being supported by the experts of HMN as regards training on use of the assessment tool set, the Working Group, under the direct supervision of the Steering Committee, organized two assessment workshops, one in the north and the other in the south, attended by 167 participants who were leaders and planning and statistical and information workers in various departments, institutes, national health programs, concerned ministries and sectors and 64 provinces nationwide. Every question in the tool set was explained in details by the Working Group so that the participants could understand and give scores. By the end of the first day of the workshop, the Working Group collected the fully completed questionnaire and then dealt with the results for the group discussions ont he next day. One day was set aside for discussion on every question according to the criteria set in the tool set of HMN. Based on the assessment results of the workshop, the Working Group and national experts, selected 3 provinces/municipalities, 12 institutions from within and outside the health sector for in-depth interviews. The assessment results were presented in each components of the HIS. Vietnam highly appreciates the HMN tool set and considers it as an important tool set for assessing the HIS. However, during the use of this set, some shortcomings have been found, for Page 11 of 70 instance, the contents of questions include too many aspects such as socio-economic status; age/gender; province/region/urban/rural; it is advisable to separate the public nad private aspects to facilitate the scoring. The score table is limited, thus it also affects the results of assessment. Page 12 of 70 2. Context and resources 2.1. Policy and planning In order to enhance effectiveness of the activities in the statistical sector in general and health statistical system in particular, the Govrenment of Vietnam has issued a series of policies related to the health statistical information system, for example: - Ordinance on Accounting – Statistics, dated 10/5/1988 of the State Council (presently Government); Circular instructing the execution of the Ordinance on Accounting – Statistics No. 555/TCKT-PPCĐ dated 13/9/1988 of the GSO. The Ordinance on Accounting – Statistics is the highest legal document on accounting and statistics which was enacted in Vietnam for the first time. This Ordinance was a legal ground for: (1) monitoring the implementation of the accounting and statistics mechanism by grassroots institutions and citizens in order to provide information timely and precisely to enhance economic and financial management of all institutions at all levels. (2) Exercising reforms and strengthening disiplines related to accounting and statistics. (3) Assuring professional independence right of the accounting and statistical workers in order to enhance objectiveness of data. - Decree No. 93/1999/NĐ-CP dated 7/9/1999 of the Government on exercising administrative punishments related to the statistical field, which was modified by Decree No.14/2005/NĐ-CP dated 4/2/2005 in order to increase responsibilities of various sectors at all levels and statistical workers for collecting, processing and providing information. Policies on statistical ifnormation are regularly modified to be in line with each reform period of the country. Specially, when the economy of Vietnam transforms to the market mechanism, some policies on statistics have been supplemented, for example: - Directive of the Prime Minister (PM) on strengthening and modernizing statistical work No. 28/1998/CT-TTG. This Directive requires the GSO and concerned minsitries and sectors to consolidate and upgrade their statistical system and promote the employment of the informatic technology in processing, storing and transforming information. - Statistical Law no. 04/2003/QH11 of the Term XI - National Assembly of the SR of Vietnam; Decree No. 40/2004/NĐ-CP dated 13/2/2004 of the Government detailing and instructing the execution of some articles in the Statistical Law. The Statistical Law elaborates the Ordinance on Accounting and Statistics, specifically as regards the applicable subjects; the HIS; statistical surveying and reporting; statistical information publication and use; statistical organization; State regulatory aspect of statistics; ...The Statistical Law was issued to enhance effectiveness of the statistical work and to assure true, objective, accurate, comprehensive and timely statistical information to serve State bodies in assessments, projections, strategy development, policy making, making socio-economic development plans and to meet the need for statistical information of various organizations and individuals as well as enhance regulatory effectiveness in the statistical field. - Decision No. 305/2005/QĐ-TTg dated 24/11/2005 by the PM on the issuance of the National Statistical Indicators System. This Decision specifies and assigns the task of collecting and calculating these indicators to various ministries and sectors to avoid overlaps. Based on the policies of the Government and the health sector, the MoH has issued a series of policies related to the health statistics, specifically as follows: - Decision by the Minister of Health on the publication of the record and booking forms developed in 1960s. This Decision was modified to be in line with each period in the history of the country, for instance: the Decision on the issuance of record forms was released in 1977 after the reunification of the country; Decision issued in 1992 was upon the need for information during the reform process; and Decision issued during 2001-2002 to respond to the situation of integration into the countries in the region and the world and the need for information in the industrialization and modernization process. Page 13 of 70 - Decision of the Minister of Health on the promulgation of the Health Statistics Regulation No. 379/2002/QĐ-BYT dated 8/2/2002. This Regulation acts as a legal ground for the collection and analysis of health statistical information and specifies functions, tasks and authorization of health facilities nationwide as regards recording and reporting; as well as enhances responsibilities of managers and workers involved in the health information system. - Decision No. 2553/2002/QĐ-BYT dated 4/7/2002 by the Minsiter of Health on the issuance of the list of essential health indicators. This Decision aims to uniform various concepts, methods of collection and calculation and to increase quality of data and enhance the use of data in analyses, assessments anf policy making. - Decisions by the Minsiter of Health on the publication of software for management, processing and storage of health data at the grassroots level and in hospitals in order to enhance the application of the information technology in the health sector, for example: Decision No. 1833/2002/QĐ-BYT dated 17/5/2002 on the issuance of the software on management of frassroots health system; Decision on the issuance of hospital statistic software ( Medisoft). - Decision by the Minister of Health on the enactment of regulation on reporting information on communicable diseases No. 4880/2002/QĐ-BYT, dated 6/12/2002 serving the control of communicable diseases. - Many other related legal documents. Some policies in the health statistics sector such as statistics regulation, Decision on the issuance of the list of essential health indicators, Decision on the issuance of record forms and others will also be modified to accord with the Statistical Law and National Statistics Indicators System issued by the end of 2005. Despite the fact that many policies related to the statistical system in general and health statistical system in particular have been promulgated, in the two assessment workshops, the part on policies and plans only met 54.16% (See Table 13). The cause was elicited during the discussions and in-depth interviews. According to results from discussions and interviews, the above policies do not cover all aspects and components of the HIS. For instance, some policies have been issued but not exercised in reality, partly because they lack solutions and conditions for implementation, regulation on human and financial resources for implementing them. The communication and advocacy of implementing these policies were not regularly and widely exercised. The policies of the HIS did not specify the collection, processing and implementation of the reporting mechanism in private health facilities, thus some health statistical indicators did not fully reflect the activities of the health sector and the people’s health status; there was no comprehensive strategy for development of the HIS in accordance with the copmponents in the HMN Framework. The GSO and MoH were not set up a coordination mechanism during the collection and sharing of information. The MoH, despite the establishment of the Steering Committee on the HIS, lacked resources for activities. It was recommended by the participants that in the coming time, the MoH and GSO should review existing documents and further develop policies based on the Statistical Law and the HMN Framework, especially develop a strategic plan on developing the HIS up to 2015 and 2020. 2.2. HIS institutions, human resources and financing Situation As presented earlier, the HIS includes a general health statistics information system and sub-systems under various departments, national health programs, communicable diseases control system… and the information systems under concerned minsitries and sectors. 2.2.1. Comprehensive health ifnormation system The network of the general health statistics information system is set up from the commune to the district, provincial and central levels. At the central level Page 14 of 70 The general health statistics information system is under the direct operation of the division of health information and staistics within the Department of Planning and Finance – MoH – with the following functions and duties: - Developing and uniformedly managing health statistical indicators, methods of collection, recording of data, operating procedures, regulation on provision and use of data, uniformed statistical forms system in the entire sector. - Synthesizing and analyzing statistical data on an annual, every-5-years and every-10years basis. - Compiling and publishing annual Health Statistical Yearbooks and other statistical documents. Being the only institution who provides health statistical data for publication nationally and internationally by the Minsiter of Health. - Developing policies and strategies aiming to strengthen and develop the health information sector. - Providing profesisonal guidance for the subsidiaries of the MoH, local health network, health institutions under other ministries and sectors. Organizing and managing surveys and assessments on the activities of the health sector as well as the factors related to people’s health status. - Developing and applying information technology achievements in processing, storing and transmitting information. - Implementing the reporting mechanism to the concerned Government bodies. At the provincial level On average, each provincial Health Bureau has 1 or 2 statistical and information workers who are members of the planning department with the following functions and duties: - Organizing the collection and processing of information on health activities and health status of the people in the entire province. - Providing health statistical – information guides to health institutions within the province. - Exercising the reporting mechanism of the MoH and local bodies such as People’s Committee, provincial statistics department. At the district level In 2006, in implementing Decree No. 01/NĐ-CP dated03/01/1998 of the Government on the "local health organizational structure"; Decree No. 171/2004/NĐ-CP specifying the organizational structure of profesisonal bodies under the provincial and municipal People’s Committees; Decree No. 172/2004/NĐ-CP dated 29/9/2004 of the Government specifying the organizational structure of profesisonal bodies under the district People’s Committees and JointCircular No. 11/2005/TTLT-BYT-BNV dated 12/4/2005 of the MoH and Ministry of Home Affairs instructing functions, duties and organizational structure of professional bodies assisting the People’s Committee in regulatory aspect at the local level, the health sector rearranged the organizational structure at the district level. Compared with the previous structure, the health information network, especially that at the district level, has felt significant change. Instead of only one district health center (DHC) taking management over all health aspects within the province, now there are 3 institutions: district health bureau (DHB), district hospital and district preventive health care center with 3 different functions. The DHB is udner the direct management umbrella of the district People’s Committee and responsible for the regulatory aspect in the health sector within the district and holds the management of commune health stations (CHS). The district hospital and preventive health care center take indirect responsibility for providing technical supervision and guide to the commune level, reporting to the DHB and is under the direct management umbrella of the provincial Health Bureau. The DHB is in charge of guiding health institutions in the district and CHSs to collect and record the forms and write reports to submit to the provincial Health Bureau and People’s Committee. Page 15 of 70 By the end of the first quarter, 2006, more than 35 provinces/municipalities nationwide had implemented Decrees No. 171, 172. However, some difficulties arose during the in-depth interviews in 3 provinces who had implemented these decrees, as follows: Skillful statistical workers were assigned other work. The district statistical department has a function of taking regulatory role in the entire district, but because it was just set up, there was shortage of manpower (1-3 workers/department), shortage of worker in charge of statistical and rpeorting work. The receipt of reports was separated into 3, thus the CHS had to send copies of reports to many institutions within the district (to the DHB, district preventive health care center and commune People’s Committee ...). From a State regulatory perspective, the DHB is in charge of collecting all health data in the district, but due to the fact that most of the statistical and information workers in most DHB worked on a part-time basis in this field, they could not address all information on health activities in the district. There was shortate of facilities and equipment for the informaiton system. In many districts, there was no computer, printer... therefore, the processing and analysis of data and reporting at the DHB encountered difficulties, affecting significantly the whole information system. At the commune level: The CHS is reponsible for recording information after each contact to patients for provision of health services; collecting information on health status of the community through the village health network; synthesizing data on health services provision and health status of the people in the commune to report to the DHB, commune People’s Committee and district preventive health care center. At the village level: Village health workers are responsible for conduting health education and communication and collecting essential information related to the community as regards their births, deaths, communicable diseases, accidents and injuries and environment to report to the CHS. Figure 3: Organizational structure of general health statistics information system The General Health Statistics Information System MOH HSID, Planning & Finance Dept. NHI & Vertical health programs Central hospitals Other central health facilities PHB The planning bureau Provicial hospitals P. Preventive health center Page 16 of 70 Reproductive health center District health bureau Other provicial health facilities 2.2.3. Sub-sysems in national health programs As presented earlier, the general health statistics informaiton system has a duty of collecting and synthesizying essential data and essential indicators for policy making and making sector development plans. Therefore, this system could not fully respond to the need for information for the management and operation of the activities in all areas and national health programs, thus these programs had their own sub-systems of health information. The information in these programs was also collected from the commune to the district, provincial and central levels, for example: - Reproductive Health Information Sub-system (RHIS) is under the coordination of the Department of Reproductive Health. In the CHSl, midwives are in charge of reporting the provision of reproductive health care services to the reproductive health division at the district preventive health care center. The district preventive health care center is in charge of collecting reports submitted by CHSs to submit to the provincial reproductive health center (PRHC). The PRHC is in charge of collecting reports from district preventive health care centers to submit to the Department of Reproductive Health in the MoH. Likewise, the malaria control, safe community programs, EPI, malnutrition control program…. undertake the same mechanism. - The information subsystem of the curative care sector is under the coordination of the Therapy Department, MoH. Presently, there are two statistical and information workers at the Department. ON average, each hospital has a statistical worker. Small hospitals such as those at the district and township level, the statistical worker also has to do some other jobs. As regulated by the Therapy Department, all hospitals from the district to the central levels must report data directly to the Department and the provincial health Bureau at the same time for synthesis of reports to be submitted to the Department of Planning and Finance of the MoH (GHSIS). In the curative care area, there is lack of information from general and specialized clinics and CHSs. Due to the fact that there is no decentralization of collecting data on hospital activities to provincial Health Bureaus, the Therapy Department curently can only collect information from around one-third – half of the existing hospitals. Data on curative care, morbidity and mortality is presently collected from the GHSIS. - Information Subsystem of the TB control program is under the coordination of the Central Hospital of TB and Lung Diseases. The head of the division of technical supervision is in charge of the information system and there are 2 full-time information workers. + In the south, it is assigned to Phạm Ngọc Thạch hospital with one statistical worker in charge of collecting and processing information on TB control in southern provinces to submit to the program. + At the provincial level: The center for social diseases control has a part-time statistical worker, in charge of collecting information on TB control in the whole province and reporting to the program and provincial Health Brueau. + At the district level: at the district preventive health care center there is a part-time statistical worker who is in charge of collecting information on TB control activities in the district to submit to the center for social diseases control. + The CHS is in charge of managing and dispensing medicines to TB patients in the commune according to the treatment protocol of the upper level. + Patient related data and treatment results are collected from the district level onwards - Some other information sub-systems also have the same organizational structure as that in the TB control program such as HIV/AIDS control, leprosy ciontrol, mental health programs... Page 17 of 70 2.2.3. Communicable diseases surveillance system The central Institute of Hygiene and Epidemiology and regional epidemiology subinstitutes are in charge of directing the system of surveillance and prevention of some dangerous communicable diseases (26). Information serving the surveillance and reporting is collected from the commune level, combined with the surveillance of the district preventive health care center, provincial preventive health care center, the central Institute of Hygiene and Epidemiology and regional epidemiology sub-institutes. The central Institute of Hygiene and Epidemiology and regional epidemiology subinstitutes have statistical workers. The provincial and district preventive health care centers also have part-time statistical workers. Statistical workers of the Central Institute of Hygiene and Epidemiology and regional epidemiology sub-institutes, in collaboration with the provincial Health Bureau, guide statistical worker at the provincial preventive health care center to record into forms, collect data on the morbidity/mortality due to communicable diseases in the province to report to the Vietnam Administrative of Preventive Health, MoH. At the provincial level: the statistical workers of the provincial preventive health care center and ealth Bureau are in charge of guiding the statistical workers of the district preventive health care center to record into forms, to collect data from districts in the province and to add hospital-based data on the morbidity and mortality due to communicable diseases at the central and sectoral hospitals located in the province to submit to the regional epidemiology subinstitutes and the provincial Health Bureau. At the district level: like the provincial level, the statistical workers at the district preventive health care center and the DHB are in charge of guiding the commune level to record into forms. The district preventive health care center is in charge of collecting data on morbidity and mortality due to communicable diseases in the commune and adding the same data based on the services provided in clinics and communicable diseases department of the district hospital to submit to the provincial preventive health care center and DHB. At the commune lvel, information on diseases and epidemics is collected from medical records (A1/YTCS). There are two types of reporting form: weekly and monthly, which are used uniformedly nationwide. When an epidemic occurs, health facilities are required to report urgently to the upper level by telephone, telegraph or fax. Weekly report form: specify the number of affected people in the epidemic outbreak in a week, including data reported urgently as well as the morbidity of other diseases in a week to submit to the upper level. Monthly report form: the CHS should collect data on morbidity and mortality of each communicable disease (26) from the medical record (A1/YTCS and A6/YTCS) to submit to the district preventive health care center. 2.2.4. Information system in other sectors, ministries The State statistical information system at the central level is coordinated by the GSO. At the provincial level, there is a provincial statistical department. At the district level, the statistical division is located in the district People’s Committee and at the commune level the People’s Committee has a statistical worker. The manpower in the State statistical system from the district to the central levels is under the management of and salaried by the GSO. Information on population, births, deaths, socio-economic situation, environment is mainly collected through this system. 2.2.5. Assessment of facilities, manpower and financial resource of HIS (See Table 1) As assessed at the workshop, the statistical information network covers the whole country and closely linked to the health service provision network wit systematic activities. The statistical workers at the national level are those trained in epidemiology, statistics, population Page 18 of 70 and information... The MoH has developed and issued tools and guidelines on data collection and processing for all levels and health facilities. Some softwares have been designed and functioned such as the report processing one, hospital statistics software, CBM..., However, human and financial resources for the HIS are limited (55.5%), of which the investment in this area in southern provinces is higher (59%). Limited financial resource for the HIS was analyzed in group discussions and in-depth interviews. Presently, the manpower in the statistical sector is in shortage. Only the departments in the MoH, institutes, central hospitals, provincial health Bureaus, provincial hospitals have full-time statistical workers. Other health facilities at the provincial, district and commune levels and national health programs mostly have part-time ones who have to do other jobs such as planning, administration, accounting or health service provision etc. The manpower in this field in health facilities is unstable, partly due to the typically poorer incentives compared with the workers at the same qualification level but working in other fields; partly because they have to do other jobs; moreover, their knowledge of using statistical data is limited. As regards financial resources for the health statistical information system and subsystems, all participants highlighted that in the annual budgetary allocation plan at all levels, including the central one, there is no budget line for health statistical information. Salary of statistical information workers are included in the total salary fund of each institution. Against financial constraints in the HIS, in the , past years the system has received financial support from WHO. On average, in each two-year period, the support valued around 150,000 USD for hiring consultants, organizing workshops and training courses. Some national health programs financially supported by international multilateral or bilateral organizationshave also set aside a modest amount of money for procuring equipment for the statistical work of the programs at the central and provincial levels and for priting forms related to the activities of the programs. Most of the provinces and districts without such financial support have to rely on the government budget share or the fund raised from hospital user fees, health insurance or other services. The government budget allocated to health activities is significantly different between levels and provinces. The MoF allocates budget for the central health institutions through the MoH. The local health budget is allocated by the provincial Bureau of Finance. After receiving budget from the provincial Bureau of Finance, the provincial Health Bureau is responsible forfurther allocating it to provincial health facilities, district hospitals, polyclinics, district preventive health care centers. The budget of the DHB, CHS and village health workers is allocated by the district People’s Committee. Due to limited government budget share allocated to the health sector (around USD 15/capita/year), health institutions typically give priority to profesisonal activities and thus the investment in the statistical information work is very modest and not regular, especially in poor provicnes and disadvantaged areas. 2.3. HIS infrastructure (Table 1) In recent years, the Government has paid special attention to the procurement of equipment for transmitting information and calculation. Currently, 100% CHSs in delta and midland provinces and 80 - 85 % CHSs in mountainous provinces have telephone. This facilitates the reporting of the diseases and community health problems. Statistical information dividions under the MoH, provincial Health Bureau and institutes, central and provincial hospitals are equipped with computers, internet... The education and communication network develops and covers the entire country. The list of public health facilities is regularly updated and reporting forms are provided to health facilities. As assessed at the two workshops, the infrastructure of the HIS meets 63%. However, it was also commented that the application of the information technology in the health sector is stagnant compared with other sectors in the whole country. Presently, in many district health facilities and some provincial ones, statistical workers still have to share computers with others such as planning, accounting, adminsitration etc. Most CHSs and DHBs do not have computers. Many departments in the district and provincial hospitals, and even central ones, do not have a computer. The capacity of using computer by Page 19 of 70 many workers in the health sector in general and statistical workers in particular is limited, thus the employment of some software is difficult. This is one of the causes explaning why Vietnam still do not have a database for each level and are not able to collect data on diseases by age/gender. The relliability and timeliness of data are not good. There is no regulation on forms for reporting by private health facilities and. Some current indicators published by the MoH are based on the data collected from public health facilities (no availability of information fromt he private health systsem) thus they do not fully reflect the activities of the health sector and people’s health status. The following is the assessments from the two worshops: Table 1 Overall results of HIS resources in Hanoi and Ho Chi Minh cities Summary of Result Maximum Score % Total A Policy and Planning 24 12 51% B HIS institutions, human resources and financing 27 15 55% C HIS Infrastructure 18 11 63% Overall Results 69 38 56% Hanoi city A Policy and Planning 24 12 49% B HIS institutions, human resources and financing 27 14 53% C HIS Infrastructure 18 10 57% Overall Results 69 36 53% Ho Chi Minh city A Policy and Planning 24 14 57% B HIS institutions, human resources and financing 27 16 59% C HIS Infrastructure 18 13 74% Overall Results 69 43 62% Based on the ersults from the two workshops and comments from group discussions and in-deoth interviews, it is shown that resources for the health statistical information system is in shortage (56%). Only infrastructure is recognized to achieve the standard of HMN (63%) . Results of Resources Summary Result Policy and Planning Present but not adequate HIS institutions, human resources and financing Present but not adequate Page 20 of 70 HIS Infrastructure Adequate Overall Present but not adequate 3. Essential Health Indicators In 2002, the MoH developed and issued a health insicator set, including 121 indicators for the national level, 97 for the grassroots level (commune and district) grouped into 4 categories: health related indicators such as population, socio-economic situation, environment; input indicators; performance and output indicators; impact indicators (health status) (see table below): Essential health indicators in Viet Nam Indicator category Number of indicators Central and province level District& communal level Population, socio-economic and environment 10 9 Input indicators 16 6 Performance and Output indicators 86 79 Impact indicators 9 3 Total 121 97 As assessed by the workshops, this set of indicators already includes all indicators assessing sectoral performance and MDG related to national health. Compared with the assessment standards of the HMN, the participants agreed that this set was up to standard (66%). Table 2 Results of indicators in Hanoi and Ho Chi Minh cities Summary of Result Maximum Score % Total of workshops 15 10 66% Hanoi city 15 10 66% Ho Chi Minh city 15 10 66% However, in group discussions and in-depth interviews, the participants reflected that this set of indicators did not introduce data collection method associated with every indicator. There was no written assignment and coordination documents between various ministries and sectors and across various institutions within the health sector, thus it resulted in the situation that some indicator was collected by no one while many others were repeatedly collected and calculated by many, causing overlaps, waste and shortage of information. Some indicators could not be collected though periodic reports but were still included in the forms, thus they complicated the reporting system. This problem was caused by shortage of finance for conducting surveys for collecting and calculating some indicators that cannot be collected through periodic reports, for instance, MMR, IMR, injury prevalence, disability or activities in private health facilities... Page 21 of 70 4. Data sources 4.1. Census Census is one of the three main sources for collecting population statistics: (i) census; (ii) selected sample survey (iii) periodic reports based on population registers (administrative records). The census in 1979 was the first one conducted nationwide. In Vietnam census is carried out every 10 years. The latest was carried out in 1999. According to the Statistics Law approved by the National Assembly in 2003, which took effect on 1/1/2004, the subsequent one will be carried out in 2009. Data from the censuses provide comprehensive and detailed data on quantity, distribution, structure, distribution by age group and demographic change in certain periods of time. Capacity and practice assessed by surveys are quite good (72%). Recent censuses have received support from international organizations. The census in 1979 was financially and technically supported by the UNFPA. The census in 1989 received technical support and equipment (computers), software. The workers involved in censuses were provided with knowledge of population, statistics and experiences of conducting a census, the design, guidelines, forms, logistics achieved international standards. However, generally these censuses met 54-55% and the integration and utilization rate of results was low (45%), followed by contents (50%) and data dissemination (53-54%). The reason was that they did not collect causes of deaths; the integration was poor for collecting information on disability, perinatal mortality rate, MMR… Results of the censuses were not widely disseminated (only in workshops, meeting at the central level and print-outs to concerned ministries and sectors) thus it was not convenient for data exploration and use. Crude data was not available for community’s access. Population projections as related to age, gender were available for the national and provincial levels, not for the district, commune and village ones. The accuracy of projections was not reliable, thus the use of these projection in planning and health service provision was limited. Census is conducted every 10 years, thus it coulod not meet the regular need of the users. Therefore, the GSO carry out additional surveys on demographic change and family planning on an annual basis. The demographic change survey is relatively simple. The sample selection is randomized and stratified based on the samples of the latest census. In each province, 6,000 households are selected. Surveyors are statistical workers at te provincial and district levels. The Department of Population and Labour of the GSO is the focal point to process and analyze results. Information from censues and demographic change surveys includes: population present by 1/4 every year; demographic change; family planning performance and births/deaths by urban/rural areas and men/women. No information related to deaths, especially causes of deaths, are not available. Especially, data from demographic change and family planning surveys only represents the provincial level, thus the utilization is limited. Demographic and health surveys, emigration surveys etc. are only conducted when financial support is available. 4.2. Vital statistics In Vietnam 4 existing systems can be a base for collecting population-related data: (i) Permanent residence registration system in the public security sector; (ii) birth, death and marriage registration system at the Ministry of Justice; (iii) Population surveillance system of the population, family and child affairs sector; and (iv) primary vital record system of the health sector. * Permanent residence registration system in the public security sector: each household should have a residence book to record all the family members by: full name, date of birth, occupation, place of work. This system aims to identify the residential status of citizens, assure political security and social order and safety. Information on demographic change such as births/deaths and migration Page 22 of 70 (immigration and emigration) is not frequently updated, especially deathc cases and causes of deaths, thus ifnormation on demographic characteristics cannot be collected from this system. * birth, death and marriage registration system at the Ministry of Justice According to Decree No. 83/1998/NĐ-CP of the Government the commune People’s Committee is responsible for the registration of births, deaths, marriages, divorces... and record the information into the birth, death, marriage, divorce registration record (Article 11) IN accordance with Decree No. 83-CP, within 30 days from birth, the parents or the child’s relatives or responsible people should register the child’s birth. In remote and mountainous areas, it is 60 days (Article 18). The births of children who die 24 hours after birth must also be registered (Article 20). When a family member dies at home or when receiving a death notification, the family members of the dead person must register the death. If the dead person has no relative, the landlord or responsible person in his office or organization should take this responsibility. In urban areas, the duration of death registration is 48 hours from death. In rural and mountainous areas, it should not exceed 15 dayes (Article 28). Children die 24 hours after birth must have both birth and death registration (Article 29). Based on the birth, death, mariage and divorce registration record, it is possible to explore all events related to the permanent citizens in the commune. The Working group conducted interviews with the Ministry of Justice on the birth and death registration and it was reported that 94% children had birth registration (quite high compared with other countries in the region). Delayed birth registration is common, especially in remote and mountainous areas, thus it is impossible to use the data of this system for calculating the birth rate of the whole country and in each region. Likewise, death registration only met 50% and typically delayed. Causes of deaths are hardly collected from this system. Therefore, this system is impossible to provide full and timely data for calculating birth rate and death rate due to the delayed and insufficient registration. Moreover, children who can live less than 24 hours after birth are not included in this system, thus the total number of live births and mortality do not reflect these cases. * Household record system of the population, family and child affairs sector. The primary recording mechanism on population, family and child affairs is reflected in the Household Record of the population collaborator, issued in conjunction with Decision No. 03/2005/QĐ-DSGĐTE dated 29/7/2005 of the Minister – head of the National Committee on Population, Family and Child Affairs. Primary information collected by the collaborators is recorded into the household record and will be a base for making reports on population, family and child affairs. The household record is the primary record of the the HMIS and basic document of the statistics garner on populatyion, family and child affairs. Based on the Household Record of the collaborators, it is potential to explore information on demographic characteristics related to the permanent citizens (as regards gender, age, ethnicity, educational level, professional qualification…) as well as demographic changes (birth, death, marriage, divorce, migration of all permanent residents in the commune. However, in group discussions, it was commented that this system focused mainly on birth and family planning and the updating information in many places was not done frequently. It could not provide causes of deaths, especially perinatal mortality, thus the data of this system cannot meet requirement of various ministries and sectors. * Vital record system of the health sector In order to ovrecome shortcomings of the vital register systems in the above sectors and to provide regular information for managers at all levels, the MoH has developed a system of forms for collecting and recording information on births and deaths, undertaken by the GHSIS. At the commune level, the CHS has two record books for births and deaths: birth record (A4/YTCS) and death record (A6/YTCS). As regulated by the MoH, data related to all births, Page 23 of 70 regardless of place of birth (i.e. at home, health facility etc.), in the commune should be collected and recorded into the birth registration record book by commune health workers in collaboration with village health workers. Likewise, all deaths in the commune should also be recorded into the death record book. The information in these two books reflect the total number of births and mortality, delivery situation, place of birth, number of births by mother’s age, weight and gender of the newborns. Especially, they include information on age, gender, occupation and causes of every death case. As evaluated by Hanoi medical University on causes of deaths, this is a more reliable information source compared with the sources from the above sectors. Information from these two books plays an improtant role in the research and direction of the sector activities. When making general assessment of the population management and birth/death registration, the participants reflected that it was gragmented, duplicated and ununiformed. The data collected is contradictory, causing waste and do not meet needs of the information users. The monitoring and exploration of data do not meet the need for policy making, planning the development of various sectors and ministries. 4.3. Population based survey During 2001 -2002, the MoH, under the financial support by SIDA, conducted a National Health Survey. This was the first survey of the health sector to collect information on the utilization of essential healthcare services such as family planning, antenatal care, immunization and measuring the prevalence of some non-communicable diseases/prioritized health problems such as disability rate, prevalence of mental health problems, hypertension etc. and leading risk factors such as smoking, drinking alcohol, environmental sanitation, nutrition... The sample size covered 36.000 households. The sampling method is randomized and stratified based on the sample design of the census in 1999. As assessed at the two workshops, the national health survey achieved 53%. This was the first national health survey, thus it received technical support from many international consultants for design, questionnaire development, software development and guidelines (including training for surveyors) and logistics. The surveyors of this survey was experienced one who had participated in many surveys in the State statistical system and staff members of medical univresities qualified in epidemology, thus their practice and capacity achieved 71%. However, the contents only achieved achieved 49%, especially the integration and utilization rate was low (43%). As reflected by many participants in group discussions, the contents of the survey did not cover essential information such as causes of deaths, MMR and IMR. Most of the indicators collected from this survey represented the retional and national levels. Due to small sample size, the morbidity of some non-communicable diseases and prioritized health problems at the provincial and district levels was not measured. The data on diseases was categorized by urban/rural areas other than by age/gender. The results of the survey was not dissemined widely, thus it was not convenient for the exploration and utilization of data. 4.4. Medical records (including disease surveillance systems) Despite the fact that the assessment achieved 57%, but in group discussions and in-depth interviews, most of the participants reflected that the surveillance system of communicable diseases had been established and strengthened. The activities of the system made significant contribution to the control and prevention of dangerous diseases and information provision. Important health problems such as causes of morbidity, mortality and disability are accompanied by strategies and plans on expanding the coverage, for instance, National Strategy for Accident and Injury Prevention; national strategy for preventing some social diseases such as TB, leprosy, mental health problems, goiter etc. Decision No. 1812/QĐ-BYT dated 23/5/2005 on the issuance of the procedure for addressing avian flu (H5N1). Around 90% of the health workers making primary diagnoses correctly defined the diseases that should be notified. Around > 95 % of weekly and monthly monitoring reports were submittted tot he district level in time and >90% of monthly monitoring reports were submitted to the provincial level in time. The ICD X was Page 24 of 70 employed for reporting hospital discharged cases. More than 75% of epidemic outbreaks at the regional or national levels were primarily detected at the district level. From the above analysis, the capacity and practice of setting up medical record related to disease surveillance achieved 65%. The information collected from medical records and the disease surveillance system met the standards of HMN. However, the participants were also concerned that the mapping of risks in public health system, risk population groups and resources was not exercised due to shortage of financial and human resources. Surveillance data disseminated and feedbacked through weekly, monthly or quarterly bulletins did not reach the district level. There was lack of integration of disease surveillance reporting into national health programs, thus health workers, especially commune ones, have to shoulder a heavy burden of reports and records. 4.5. Professional service record As assessed by the workshops, professional service records achieved 51,5%. The cause of such result was commented in group discussions and in-depth interviews in 3 selected provinces and 10 central institutions, specifically: The record and form system was set up and issued for the public health system at all levels. This system can also be used in the private health sector, but there is no regulation on that, thus information on the practice of private health facilities is absent. This system mainly focuses on quantity other than quality of health service provision. Information on quality of health services is collected though surveys and national health survey. The information system in each district used to have a full-time statistical worker, but they only attend 3 – 5-day training courses. Since the end of 2005, the new organizational structure have come into being, thus currently in district health facilities, including the DHB under the district People’s Comitteethực, statistical workers have to do many other jobs. Only those in hospitals employing medisoft, hospital management software receive short-term training which is typically integrated into other programs or workshops. The feedback to the lower level is limited, only related to some communicable diseases and important diseases such as HIV/AIDS, leprosy, TB, mental health problem, malaria, vaccinated diseases... The staff members in charge of management and analysis of health activiries at the provincial and central levels use the findings of the national health survey, research studies, censuses and demographic change surveys for evaluating value of data based on the health service record, but it is not regular. Data collected from ehalth service records is used for calculating the coverage of essential health services such as delivery rate attended by professionals, rate of pregnant women receiving 3 or more antenatal contacts, child immunization rate, morbidity and mortality classified by ICDX v.v... 4.6. Administrative records 4.6.1. Database/ infrastructure mapping Many participants and interviewees, by analyzing the database and mapping infrastructure, said that currently only regulation on recording and reporting for the public health system is available and there is no national assignment table for public and private health facilities. Each health facility has not been assigned a unique code allowing the connection between ehalth facilities. The global positioning satellite (GPS) has only been piloted in 2 provinces, 3 districts in wach under the fupport by the HMN. Thus, the database and infrastructure mapping achieved only 32%. 4.6.2.Database on human resource The database on the human resource was more appreciated than the infrastructure mapping and achieved around 58%. According to most participants, at the national level there is a database on human resource classified by professional capacity of public ehalth facilities. The number of health workers graduating annually could only be collected from medical universities Page 25 of 70 and colleges under the management of the health sector. Those graduating from the schools under the management of the Minsitry of Education and Training (MoET) or private ones were not updated. IT was recommended that the MoH should collaborate with the MoET to collect full data on the medical and pahrmaceutical graduates and the existing number students in the whole country on an annual basis, especially the post-graduates trained abroad. At the national, provincial and district levels, there are workers to update and maintain the database on the human resource. The latest update and publication was 1 year agogo. 4.6.3. Information on finance and expenditures on health services As assessed at the two workshops, financial information achieved 57%. Tools for collecting financial information have been improved significantly so far. The record system including record books and forms on public financing management has been significantly enhanced, facilitating the analysis and assessment of expenditures.. All public health facilities use a uniformed system issued by the MoF for management and monitoring of health expenditures by source and budget items. However, the collection of information on health financing in the whole sector still encounters certain difficulties and reveals shortcomings. Data is delayed, not sufficient, not reliable and there is lack of information on the activities under the management of other sectors. The cause of the problem is that the financial management is not put in a sectoral system. The MoH is responsible for allocating and managing the finance of the MoH and healt institutions at the central level. At the local level, the provincial Finance Bureau is responsible for allocating finance to the health institutions at the provincial and district levels through the provincial Health Bureau. The recurrent budget of the CHS and village health workers and the DHB is allocated and managed by the district People’s Committee. The budget of the health institutions under other ministries and sectors is under the management of the superior sector. Grant or loan based projects are also udner the management of provinces. Due to many coordinators, the development of a regulation for coordination of the collection, reporting and sharing financial information between institutions and levels as well as between donors is not issued. In order to deal with the above difficulties, in recent years, under the support by WHO, the MoH has set up national health accounts (NHA). The result is that it provides relatively complete information on health expenditures..... However, it can only provide information to the regional and national levels and no information of the provincial and district level and on some major diseases is available. The results of the NHA is not widely disseminated, mainly in workshops and meetings at the central level. Financial information from NHA typically goes behind the need of using information (estimates of expenditures can only be provided after more than 2 years). Thus the utilization of the results of NHA as evidence for allocating budget and financing planning in the health sector is limited. As reagrds capacity for developing NHA, it was commented that the MoH still need external technical and financial support. Many participants also recommended that NHA should be developed regularly, not only at the national, but also at provincial and district levels and related to some other major diseases such as TB, malaria, HIV/AIDS etc. and this task should be assigned to the Health Information Division under the Department of Planning and Finance for implementation. 4.6.4. Information on equipment Such information was most highly appreciated by the participants, approximately 60%: information on facility inventory: at least twices a year (on 1/7 and 31/12). Human resource and logistic management skills related to emdical devices and materials are trained and experienced.The reporting is undertaken on an annual basis as regards fixed assets and on a Page 26 of 70 quarterly basis as regards medical consumables. The reporting system as regards emdical consumables is integrated, but not completed. The check of data at the central and provincial levels is rarely done. Below is the results from analysis and scoringat the two workshops organized in hanoi and Ho Chi Minh City respectively. Table 3 Scores of data sources Contents Capacity & practices Dissemination Integration & use Total Census 48% 72% 53% 45% 55% Vital statistics 54% 56% 59% 62% 58% Population-based surveys 52% 71% 49% 43% 54% Health and disease records (incl. disease surveillance sys.) 55% 65% 45% 56% 55% Health service records 35% 43% 65% 59% 50% Administrative records 56% 54% 36% 46% 48% Data Platform infrastructure and health services 32% human resources 58% financing of health services 57% equipment, supplies and commodities 60% Hanoi city Census 50% 73% 54% 41% 54% Vital statistics 59% 57% 59% 63% 60% Population-based surveys 54% 71% 51% 42% 54% Health and disease records (incl. disease surveillance sys.) 53% 61% 35% 51% 50% Health service records 31% 40% 62% 57% 48% Administrative records 54% 54% 36% 47% 48% infrastructure and health services 31% human resources 57% financing of health services 57% Page 27 of 70 equipment, supplies and commodities 59% Ho Chi Minh city Census 44% 71% 53% 51% 55% Vital statistics 43% 53% 59% 59% 54% Population-based surveys 47% 73% 45% 44% 52% Health and disease records (incl. disease surveillance sys.) 58% 73% 64% 64% 65% Health service records 43% 47% 69% 61% 55% Administrative records 58% 54% 36% 46% 49% infrastructure and health services 36% human resources 59% financing of health services 56% equipment, supplies and commodities 60% Table 4 Results of data sources Data Source Census Vital statistics Contents Present but not adequate Present but not adequate Capacity & Practices Integration and use Total Hanoi city Present but not Adequate adequate Present but not Present but not adequate adequate Present but not adequate Present but not adequate Present but not adequate Present but not adequate Dissemination Population-based surveys Present but not adequate Adequate Present but not adequate Present but not adequate Present but not adequate Health and disease records (incl. disease surveillance sys.) Present but not adequate Adequate Adequate Adequate Adequate Health service records Present but not adequate Present but not adequate Adequate Adequate Present but not adequate Administrative records Present but not adequate Present but not adequate Not adequate Present but not adequate Present but not adequate Ho Chi Minh city Census Present but not adequate Adequate Present but not adequate Present but not adequate Present but not adequate Vital statistics Present but not adequate Present but not adequate Present but not adequate Present but not adequate Present but not adequate Population-based surveys Present but not adequate Adequate Present but not adequate Present but not adequate Present but not adequate Health and disease records (incl. disease Present but not adequate Adequate Adequate Adequate Adequate Page 28 of 70 surveillance sys.) Health service records Present but not adequate Present but not adequate Adequate Adequate Present but not adequate Administrative records Present but not adequate Present but not adequate Not adequate Present but not adequate Present but not adequate Analysis of contents and capacity by HMN framework Highly adequate content 3 C C D D Adequate content 2 C C D D Not adequate content 1 B B A A Extremely not adequate content 0 C C A A 0 1 2 Extremely not adequate capacity Not adequate capacity Adequate capacity 3 Highly adequate ca pacity As assessed above, all the contents of all data sources have not met the standards of the HMN, especially service records were not complete and put in part B. As reagrds capacity, only the census, population-based surveys and medical records (including the disease surveillance system) is put in part A. 5. Data management The data flows of the GHSIS and most sub-systems in various departments, institutes and national health programs follow the vertical system from the commune to the district, provincial and central levels. 5.1. GHSIS: This system is responsible for collecting and synthesizing all health activities and health status of the people by level (currently 4): Figure 4: Flow of information GSO Flow of information MOH Health Statistics & Informatics Division Other Departments Institutes & National vertical programs Provincia l GSO Provincial Health Service Page 29 of 70 Central Hospital, P.hospital, other branch, Private sector Provincial Preventive Medicine, MHC/FP.... * Commune level (head of CHS): based on the information recorded into the 9 primary record books issued according to Decision No. 2554/2002/QĐ-BYT and information on births, deaths cololected by village health workers, the CHS should aggregate reports and submit to the DHB. This report should include 7 tables (see attached forms). * District level: In DHBs whose organizational structure is not stable: the stastistical worker of the Bureau should be responsible for collecting and synthesizing data on the performance of CHSs and submit it to the provincial ehalth Bureau and People’s Committee. After stabilizing the organization, the DHB should collect information on activities in the whole district, including district hospital, district preventive health care center, polyclinics and all CHSs. Information on population and economic status in the district should be collected and compared with the data of the DHB. The report submitted to the provincial health Bureau by the DHB includes 15 tables (See attached forms) * Provincial level, provincial ehalth brueau (Division of Planning and Statistics): in provinces where the DHB is not set up or it does not have sufficient manpower, the statistical worker of the provincial health Bureau is responsible for collecting and synthesizing data on health activities in the entire province, including: reports of health institutions at the provincial level, district preventive health care center, district hospital, polyclinics and DHB. After stabilising the organization at the district level, and when the DHB has sufficient manpower for statistical work, the DHB is responsible for synthesizing information from district hospitals to submit to the provincial Health Bureau. Associated information such as socio-economic and population information in the province is collected and compared with the data collected by the provincial statistics office. The report should be submitted to te provincial People’s Committee and the MoH by the provincial health Bureau (Division of Health Information within the Department of Planning and Finance) should include 16 tables (See attached table). * Central level, MoH (Division of Health Information within the Department of Planning and Finance) is responsible for collecting and synthesizing reports on health activities in 64 provinces, from departments, institutes, national health programs and information on population, socio-economic status and environment collected by the GSO;m calculating and analyzing the implementation of the strategic goals of the health sector, publishing health statistical documents such as Health Statisics Yearbook, summarizing other statistical documents and reporting to the concerned Governemnt bodies (See above chart and flow of information). The information sub-system of the departments, institutes and national health programs is also organized by level. Below is the introduction of some information sub-systems of various departments, institutes and national health programs: 5.2. EPI:. * Commune level: The CHS bases on the information in their immunization book (A2./YTCS ) to synthesize data and submit top the district preventive health care center and DHB. Page 30 of 70 * The district preventive health care center synthesizes reports submitted by CHSs to submit to the provincial preventive health care center. * The provincial preventive health care center synthesizes reports of the district preventive health care centers to submit to the EPI at the central level and provincial Health Bureau (Division of Planning and Statistics). 5.3. Malaria control program * Commune level: the CHS has a book for monitorign malaria patients (A7/YTCS) and malaria parasitological testing sheets (using in communes where microscopes are available). The head of the CHS is responsible for reporting the malaria control performance on a monthly and quarter;y basis to submit to the the district preventive health care center. * District level: the district preventive health care center keeps record books of malaria parasitological testing; malaria parasitological testing sheets; malaria surveying forms (used for the district levels onwards). The district preventive health care center should collect and synthesize reports on a monthly and quarterly basis from CHSs and add data on malaria treatment reported by district hospitals to the the provincial preventive health care center (malaria control center). * Provincial level: The provincial malaria control center synthesizes monthly and quarterly reports from the the district preventive health care center and supplements data on malaria treatment in provincial hospitals reported to the regional Sub-institute of Malaria, Parasitology and Insectology and provincial health Bureau (Division of Planning and Statistics. * Other sectors: each health center under other sectors and ministries has the same reporting forms as those in the district preventive health care center should monthly and quarterly collect and synthesize data on malaria control in the district to report to the central Institute of Malaria, Parasitology and Insectology and provincial Health Bureau. The central Institute of Malaria, Parasitology and Insectology synthesizes data from subinstitutes and sectors and ministries to submit to the Vietnam Administrative of Preventive Health and Department of Planning and Finance – MoH. The reporting forms are uniformed from the commune to the central levels. 5.4. Therapy related information sub-system: In hospitals, forms for recording primary information include patient medical records, laboratory testing sheets, books for recording activities of various departments issued in accordance with Decision No. 4069/2001/QĐ-BYT dated 28/9/2001 by the Minister of Health. On average, in each hospital there is one statistical worker in the general planning division. In some big hospitals there are 1 – 2 statistical workers in charge of collecting patient medical records and reports from all departments and reporting to the Therapy Department – MoH. Figure 5: Flow of therapy related information Minister of Health HIS – Dept. of Planning and Finance Therapy Dept. Page 31 of 70 Provincial Health Bureau Central hospital Information on curative care of the Therapy Department is mainly used for professional direction, thus it is not necessary to collect information in all therapeutic facilities. Due to the absence of decentralization, annually the Therapy Department can only collect information from around 300 – 400 oput of more than 1000 hospitals. Information on curative care, morbidity and mortality is still collected through the GHSIS. Analyzing management guidelines, many participants reflected that: (1) the general statistical system and information sub-systems have compiled guidelines for collecting, analyzing and presenting data. These guidelines had been disseminated to the commune level, but the disemination was not regular, thus it was difficult fo new staff members to access to it, especially recently the organizational structure has changed, thus most statistical workers at the DHB have not had access to them. The database of the central and provincial leveld was poor. The storage of data is mainly in CDs, books or PCs. The cause of this problem was that there was no regulation on developing a database for the central and local levels. The results of research studies and surveys were not centrally stored in the general statistical institution of the MoH. Currently, there is only information of the first national health survey conducted during 2000-2001. The application of information technology in the health sector in general and in the statistical and information sector in particular is limited, causing difficulties in processing, transmitting and storing as well as exploring information. (2) Guidelines defining variables and their use for calculating indicators have been developed, but definitions and technical specifications are not comprehensive. The dissemination and communication of the definitions are not widely done. Some provinces financially supported by international organizations have organized training to the comune level. (3) Codes for identifying health institutions in the database are only available for provincial, district and commune administrative institutions, thus it is impossible to link various data sources to each other. Table 5 Results of data management Summary of Result Maximum Score % Total 15 9 57% Hanoi city 15 8 55% Ho Chi Minh city 15 9 61% According to the scores given at the above workshop, the data management of the HIS only achieved 57%, which was not up to the standard of the HMN. Page 32 of 70 6. Information products The GHSIS and sub-systems have produced many information products serving the analysis, assessment, development of action plans and policy making in the sector and in each area and program. The health information division within the Department of Planning and Finance of the MoH compiles and publishes the Health Statistics Yearbook and many otherdocuments such as assessment reports, summarized data ..., of which the Helath Statistics Yearbook is highly appreciated. It is very valuable for analysis and comparison of results from the activities across various provinces, regions in the whole country and between Vietnam and other countries in the region and in the world. Contents of the Health Statistics Yearbook: - Data serving the assessment of the implementation of the strategic goals of the health sector and DMG including: Life expectancy; IMR; under-5 mortality rate; under-5 malnutritionl rate; low-weight births (<2500gram); MMR; child full immunization rate; percentage of communes covered by doctor, birth attendant or midwife; drug expenditure per capita; elimination os some diseases such as polio, infant tetanus, leprosy... - Data of the indicators related to health activities and health status such as population growth rate, population density, GDP per capita, proportion of health budget in the gross products and total budget expenditures, utilization rate of clean water and sanitary facilities. - Data on demographic characteristics for calculating indicators reflecting impacts of health activities such as average population nationwide and in each province by gender, urban/rura areas; population structure by gender/age; crude birth rate; total fertility rate; crude death rate and IMR by province and ecological region. - Data reflecting investments in the health sector: * Government budget share allocated to the health sector ove time and by province; expenditures of public health facilities by income source; composition of expenditure sources for the health sector; health expenditure structure by areas. * Data on the enrollment and performance of the health insurance system over time; * Patient beds by technical level and type of facility: hospital, clinic, CHS, nursing and rehabilitation... * Health manpower by professional qualification. Information on pharmaceutical institutions, production, trading and drug expenditure per capita; data on devices and equipment by type of equipment such as CT Scanner, X- ray apparatus, ultrasonic device, endoscopic device by province. - Information on health activities includes: * Curative care activities such as number of contacts, outpatient and inpatient contacts, average number of treatment days, paraclinical activities. This information is categorized by region and province. * Data on child health care and reproductive health care: includes (1) child health care by province and performance results such as immunization, nutrition, morbidity and mortality of vaccinable diseases; (2) reproductive health care by province, including data reflecting antenatal, natal and postnatal care; gynaecological care and family planning; abortion and morbidity/mortality of obstetric complications. * Data reflecting the prevention and control of some major diseases such as TB, leprosy, dermatological diseases, malaria, HIV/AIDS, mental health problems, goiter, in terms of incidence, managed prevalence and treated prevalence, mortality… by region and province. - Information reflecting impacts of health activities: * Morbidity and mortality of 26 communicable diseases and important diseases over time serving the research of disease trend. Page 33 of 70 * Data on hospital-based morbidity and mortality according to ICD-X for analyzing 10 leading causes of morbidity/mortality; trend of 3 major disease groups: communicable diseases; non-communicable diseases; accidents and poisoning... - Data on the issues greatly affecting health such as morbidity/mortality of traffic accidents over time by province. - IN addition to the information reflecting health status and results from activities of the health sector, the Health Statistics Yearbook also includes information from some countries in the region and the world, facilitating the analisys, assessment and comparison. Analysis of indicators on health status according to HMN framework The results from the two workshops are presented in Table 8 Table 6 Information products of health status in Hanoi and Ho Chi Minh cities Marking Indicators Elements for assessing selected indicators Health status Mortality Morbidity Overall Health system Indicators Risk factors Overall health indicators indicators quality Data collection method 64% 66% 65% 58% 51% 59% Timeliness 78% 89% 83% 64% 61% 69% Periodicity 72% 76% 74% 61% 56% 64% Consistency/ completeness 59% 69% 64% 60% 47% 59% Representativeness/ appropriateness 66% 61% 64% 59% 42% 57% Disaggregation 59% 70% 64% 54% 51% 56% Estimation method/transparency 65% 65% 44% Overall assessment of results 66% 72% 68% 57% 51% 60% 66% 77% 71% 58% 66% 63% 87% 75% 66% 60% Hanoi city 64% 82% 73% 62% 63% 57% 63% 60% 58% 59% 51% 60% 54% 46% 43% 58% 68% 63% 57% 57% 61% 57% 65% 69% 65% 57% 70% 67% Ho Chi Minh city 53% 42% 56% 52% 51% 56% 51% 59% 60% 80% 73% 63% 67% 72% 92% 79% 75% 63% 66% 86% 76% 69% 65% 59% 66% 64% 63% 60% 51% 62% 59% 48% 39% 59% 71% 67% 62% 57% 55% 80% 68% 71% 63% 80% 72% 54% 47% 59% 49% 55% 67% 63% Data collection method Timeliness Periodicity Consistency/ completeness Representativeness/ appropriateness Disaggregation Estimation method/transparency Overall assessment of results Elements for assessing selected indicators Data collection method Timeliness Periodicity Consistency/ completeness Representativeness/ appropriateness Disaggregation Estimation method/transparency Overall assessment of results 75% 56% 51% In group discussions and in-depth interviews related to each indicator, the participants provided the following comments based on the HMN framework: Page 34 of 70 6.1. Indicators on health status 6.1.1. Under-5 mortality rate The indicator on uner-5 child mortality rate is collected by routine reports based on the death records at the commune level (A6/YTCS). Some sample surveys were conducted to assess such mortality rate such as UNICEF-supported MICS, 5-year demographic and health surveys. However, the sample size of these surveys is small and is not representative Based on the above analysis, the participants reflected that quality of data on child mortality rate was not reliable.Estimates from surveys and records were delayed (typically 2 years). Child death cases were not categorized by demographic characteristics (age/gender), socio-economic situaiton (parents’ income, occupation, educational level), urban/rural areas. This data is only available at the central level. 6.1.2. MMR Currently, it is very difficult for managers to select data on MMR for use because the sources are not uniformed, for instance: First source: routine reports (administration reports). The CHS based on the death recorded data at the commune level to report to the DHB. Then, the DHB synthesizes the data on mortality submitted by te commune level to submit to the provincial Health Bureau. The provincial Health Bureau then synthesizes data on MMR in all health facilities nationwide. The data in 2002 was 91/100,000 live births and in 2005 it was around 80/100,00 live births Second source: MICS supported by UNICEF in 2000. This survey used the Sisterhood method with technical support of international experts. The MMR was 95/100,000 live births. Thus, the data from routine reports and MICS was relatively uniformed. Third source: maternal mortality survey carried out in 2000-2001 under support of WHO. This survey was conducted in 7 provinces. The MMR was 130/100,000 live births, which was significantly higher than that according to the MICS and routine report system. Comments in group discussions and in-depth interviews: the results from the maternal mortality survey (the third source) were not reliable. Many participants were concerned that the sample size was too small and the sample distrituion was not even across regions, thus it could not represent the whole country. The survey focused more on remote, mountainous, disadvantaged and poor provinces. According to the survey, the MMR in mountainous, disadvantaged and poor provinces was far higher than that in delta provinces, for instance: Cao Bằng: 441/100,000 live births; Đắc lắc: 178; Quảng Ngãi: 199; Quảng Trị: 162, while it was very low in deltal provinces, around 45-46/100,000 live births. Most of the population of Vietnam concentrates in delta provicnes and large cities (around 80%), thus the above sample selection method generated high MMR. The participants were also concerned that it was costly to conduct a material mortality survey because it can only be reliable when the sample size is large enough. In order to deal with the problem, they recommended to establish a maternal mortality surveillance system based on the routine reporting system and setting up sentinels representing the whole country for updating and synthesizing data on maternal and child mortality rates. Similar to the under-5 mortality rate, surveys and routine reports could not analyze the maternal mortality by age, educational level, economic status and urban/rural area. 6.1.3. Adult mortality rate The data is directly collected from censuses and annual demographic change surveys. Estimated data is published < 1 years from the collection point. Thus, in the past 10 years, data had been published 10 times. The data on general mortality is collected by the only Department of Population and Labour of the GSO, thus it has assured unfirmity over time. Like the data on MMR and child mortality rate, as regards adult mortality rate, only crude death rate (CDR) was calculated nationwide and on a provincial basis, other than by demographic characteristics such as population, socio-economic status and administrative areas. Page 35 of 70 6.1.4. HIV prevalence Against the increased transmission of HIV/AIDS, the Government of Vietnam has inacted a strategy for HIV/AIDS control up to 2010 and 2020. In order to evaluate the implementation of strategic objectives, the HIV/AIDS control program implemented by the Vietnam Administration of HIV/AIDS Control, MoH, has carried out many activities, including collection and processing data on morbidity/mortality of HIV/AIDS. The data collection method in recent years has been employed through focused HIV surveys, integrated surveillance of serum and behaviours, HIV drug resistance surveillance, STI focused surveillance. Surveillance is a process of continuously and systematically collecting data aiming to estimate seriousness of the HIV epidemic, description of distribution and transmission of HI; surveillance of risk behavioural change. Sentinel surveyllance is carried out on an annual basis by the provincial and district preventive health care centers. The Central Institute of Hygiene and Epidemiology and sub-institutes as well as the Dermatology Institute are responsible for collecting and synthesizind data to submit to the Vietnam Adminsitration of HIV/AIDS Control MoH. Data on HIV/AIDS prevalence is published every month and year. HIV/AIDS cases are confirmed after carrying out tests and are collected in a system, thus the data assures uniformity over time. Data on HIV/AIDS prevalence is analyzed by region and some age groups such as <13, 13-19, 20-29, 30-39, 40-49, and >50 years of age, without socio-economic situation, occupation or educational level analysis. The collection and synthesis of data based on the cases detected and diagnozed by health facilities as currently done cause duplication as patients typically conceal their personal information such as name, age, address when visiting health facilities. Thus, the same patient but visiting many health facilities can be recognized as different ones. To address this problem, the HIV/AIDS control program is setting up a software for updating information on HIV cases from the community. 6.1.5. Low weight under-5 children The collection and processing of data on low-weight malnutrition of under-5 children are undertaken by the national malnutrition control program within the National Institute of Nutrition. Data of the program is derived from 3 sources: - Routine report system. Nutrition collaborators in communes are responsible for weighing under-5 children on a monthly basis and recording the data into record books; then data on low-weight children is synthesized and submitted to the district preventive health care center. The distrct level then synthesizes reports from the communes to submit to the provincial preventive healt care center and the provincial preventive health care center reports to the National Malnutrition Control Program. - Malnutrition surveillance system: this system came into being in 1998. the National Malnutrition Control Program is in charge of the surveillance of maternal and uunder-5 malnutrition on an annual basis. For surveillance, 1500 children are selected in each province. Information collected from this system includes low-weight malnutrition rate (weight/age); stunting rate (height/age); wasting (weight/height); permanent energy deficiency among mothers; percentage of fully breastfed children and percentage of children taking vitamin A. - Special surveys: nutrition general survey every 10 years; general survey on vitaminA; general survey on anaemia every 5 years; surveys in research studies... The population-based surveillance and survey system. The time of publishing estimates on nutrition situation against income in the commune surveillance system is 15 days after each quarter; the annual surveillance systsem: 2 moths after the reporting period. Special surveys: 6 months to less than 2 years. Thus, the reporting cycle should achieve standard of the HMN. According to the scores in the workshops, information on health status achieved 68% and the uniformity and sufficiency of information on mortality were not up to standard (Table 6). Page 36 of 70 6.2. Indicators of the health system 6.2.1. Outpatient treatment: metod of collection - Routine report system Information on curative care such as: number of contacts; inpatient, outpatient treatment contacts; number of treatment days and paraclinical activities is collected mainly based on the routine report system in public health facilities. Information on treatment activities in each health facility in recent years has felt significant improvement. The reporting period is every 3 months, 6 months, 9 months and every year. The period of time from the collection to the national publication is around 2.5 months, meeting the standard of the HMN. However, the data synthesized at each level is not reliabloe because of the absence of data from the private health system and health facilities under other sectors. - Sample survey Surveys to private health facilities and those under other ministries and sectors to collect data on curative care activities have not been conducted. In order to deal with the problem, the NHS and VLSS introduced a module on consultation, inpatient and outpatient treatment in the questionnaire for households interviews. The results of these surveys provides percentage of consultation, including inpatient anad outpatient care; health expenditure per capita on inpatient, outpatient treatment. The data of the surveys was published around >1 year ago (VLSS 2004). These data were categorized by demographic characteristics such as gender/age; economic status; 5 income quintiles; occupation; educational level of the patient; ecological region; urban and rural area. However, the interviews with the heads of households focused on curative care situation during the past 12 months, so many could not recall all contacts and expenditure incurred by every family member, especially under-5 children. Moreover, the sample size was small, thus there was no uniformity between the results of the survey and routine reports. Some important indicators on curative care were not collected such as number of treatment days, treatment duration related to eahc diseases and paraclinical activities... 6.2.2. Immunization for children < 12 years of age The information system on infant immunization is collected from two major sources: routine report system and surveys - Routine report system (administrative statistics) The collection of data on infant immunization against 7 diseases (leprosy, pertussis, diphtheria, tetanus, polio, measles, and herpatitis B) is undertaken by the EPI in collaboration with the GHSIS. Primary records of the EPI, at the commune level (CHS) include codes for monitoring infant immunization (A2.1/YTCS). The list of infants who need immunization is recorded into the book. Each oral/intravenous immunization is marked in the equivalent column. After every month, the commune health workers based on the synthesized data on immunization to report to the district preventive health care center and DHB. The district preventive health care center synthesizes the data from communes to submit to the provincial preventive health care center. The provincial preventive health care center synthesizes and submit to the EPI at the central level and provincial Health Bureau. The denominator (number of infants who need immunization based on the number of births in the birth registration book (A4/YTCS) of the CHS and is added the migrants as all deliveries in the commune must be recorded in to the A4 book. The results of immunization over time not only greatly afects the reduction of morbidity and mortality of dangerous child diseases, but also greatly affect mothers’ awareness. Most Vietnamese mothers consider vacinnation for their children as a benefit. Data on morbidity/mortality of preventable diseases is collected through the communicable diseases surveillance system, thus it is relatively sufficient and uniformed. This data is published every year. - Immunization survey Page 37 of 70 The survey of immunization and measles prevalence is integrated into the household survey of MICS and VNHS 2001-2002. The MICS is conducted every 5 years. The first MICS was carried out in 2000-2001 with support by UNICEand the second at the end of 2006. Results are not available. As assessed by the first MICS and VNHS, the child immunization rate was around >70%, lower than the percentage in the routine report system. The cause of such difference is that the surveys only focused on household interviews, thus many heads of households did not recall the type of vaccines and number of immunizations their children had been taken. Approximately 2/3 of the households did not keep the immunization sheet, thus the surveyors could not collect precisely information on immunization from households. Therefore, the data on immunization published currently is mainly derived from the administrative reporting system. The period of time for immunization data publication is every 3 months, 6 months, 9 months and 12 months. Information on morbidity/mortality of vaccinable diseases is reported through the communicable diseases surveillance system. As regards measles, any case in the community is reported to the CHS and the CHS then reports to the district preventive health care center for definition. Measles cases in the community and those treated in health facilities are recorded into the system of records and forms. This data is published monthly. In case of serious epidemics, it is reported weekly, even every hour. Thus, this reporting cycle achieves the standard of the HMN (5 years/5 times). 6.2.3. Professionally attended deliveries One of the strengths of the health sector of Vietnam is the public health service provision network with the even coverage nationwide. Presently, 100% communes have a CHS, approximately 70% CHS have a doctor, more than 90% of CHS has midwives or obstetric and paediatric assistant doctor, approximately 90% villages have village health workers. Most of the deliveries in the rural area are at CHSs and only complicated ones are referred to the upper levels. The system of delivery information surveillance is integrated into the general information system and reproductive health surveillance sub-system. The CHS has a birth surveillance record (A4/YTCS). As specified under Decision No. 2554/2002/QĐ-BYT of the MoH, all deliveries in the commune, regardless of places of birth (at home, hospitals at upper levels or others) must be recorded into the birth surveillance record. The contents of this book include 28 columns for recording information, including information on the birth attendant’s professional qualification (seen attached form). In order to collect sufficient information for the book, the CHS hold monthly meetings with village health workers to supplement the deliveries outside the CHS. Information in this book not only serves the reporting to the upper levels, but also serves the CHS in preparing for child care activities such as provision of VitaminA, immunization, nutrition monitoring… Quarterly, the CHS report the situation of the commune, including the deliveries without professional attendance. The report on antenatal, natal and post-natal care is submited to the reproductive health care division within the district preventive health care center and DHB to report to the provincial reproductive health care center. The provincial reproductive health care center then submits the report to the department of Preventive Health (reproductive health care program). The provincial health Bureau synthesizes the data submited by the DHB to compared with the data of the provincial reproductive health care center and submits to the health information division within the Department of Planning and Finance – MoH (GHSIS). In the past 5 years, 2 surveys have been conducted, collecting information on deliveries,: demogtaphic and health survey 2002 and VNHS 2001-2002, but these two surveys showed slightly different results. According to the demographic and health survey, the percentage of deliveries professionally attended was 85% (page 109) while the corresponding figure in the VNSH was 82.4% ( page 26, on coverage of public health programs). This difference is subject to different sample sizes. The demographic and health survey included 1321 deliveries during 3 years prior to the survey but it was 11,159 during 5 years prior to the survey in the VNHS. The data collected from the routine report system is published every year. In the past 10 years, such Page 38 of 70 data has been published for 10 times (once a year). There is slight difference between data from routine report system and surveys (90 % against 82.4% - 85%). The coverage of survey data is very modest while the data collected from the administrative reporting system covers around >90% deliveries. Such data in the administrative reporting system is not categoried by age, socio-economic status, occupation and educational level of the mothers. 6.2.4 Percentage of success in treating TB Information on TB control and treatment is collected by the TB information sub-system under the TB control program in the Central Hospital of TB and Lung Diseases. The tool for collecting such information is printed and provided to all health facilities nationwide. The information collected by this sub-system includes: Total number of TB patients nationwide and in each province, including lung TB: ÀFB(+) pincidence, ÀFB (+) relapse, AFB(-) and non-lung TB. Indicators for assesing the program: Detected incidence of TB AFB(+) incidence/100.000 inhabitants Percentage of cured AFB(+) Death rate during treatment Any patient detected TB at the central and provincial levels, after treament, is referred to the district preventive health care center for monitoring. The Center then reports the CHS the new detected case to record into the TB patietn surveillance book (A9/YTCS). According to the treatment protocol of the upper levels, the CHS dispenses medicines to the TB patietn free of charge. After the treatment course finishes, the patient is referred tot he upper levels for testing to confirm the treatment results. Ifnormation on success of TB treatment according to DOTS method is collected from the district preventive health care center. The provincial social diseases control center or TB hospital synthesizes data from district preventive health care centers and supplements data on patients treated at provincial TB hospital to submit to the Central Hospital of TB and Lung Diseases (central TB control program). Most of the data is published on an annual basis. In the past 5 years, this data has been calculated 5 times. The data on success in treating TB since 1995 is fully uniformed. The coverage of the recent data is based on more than 90% DOTS reports from the local level to the national TB control program. However, such data is only categorized by region, province and drug resistance situation other than by gender/age, socio-economic status such as occupation, educational level, urban/rural distribution and HIV. 6.2.5 Percentage of children <59 months old sleeping in mosquito-nets The malaria control information subsystem is coordinated by the National Malaria Control Program under the Central Institute of Malaria, Parasitology and Insectology. The system of forms includes primary records and reporting forms. The tools for collecting information of the program are uniformed with the tools of the GHSIS. At the commune level there is A7/YTCS book used for recording all malaria cases and suspected cases in the commune for management to prevent transmission and treatment at the grassroots level. The cases detected at the upper levels (district and provincial or central levels) are also recorded into this book for management and drug dispensing. The reforting forms are uniformed from the commune to the provincial levels in order to avoid overlaps during the synthesis of data on morbidity/mortality of malaria. It is regulated by the MoH that the report of the commune level should only synthesizes the morbidity and mortality detected by the CHS. The district preventive health care center synthesizes the morbidity and morality from the reports of the communes supplemented by the cases detected and treated in district health facilities to submit to the provincial preventive health care center. The provincial preventive health care center synthesizes data from districts and adds the cases detected and treated in provincial health facilities to submit to the Sub-institute of Malaria, Parasitology and Insectology and provincial Health Bureau. The Page 39 of 70 Sub-institutes synthesize data from provinces and the data from central hospitals to submit to the national malaria control program. The information collected and synthesized by the malaria control program includes population in malaria region; total number of malaria patients; mortality due to malaria; prevalence among under-5 children, 5-14 age group; number of pregnant women incurring malaria; total number of tested blood smears; percentage of blood smears containing parasites and types of parasites; total number of malaria patients treated; protected population. 6.2.6. Government general expenditures on health per capita As presented earlier in the section on information o finance and health expenditures, in item F on administrative records, the financial distribution and management in the health sector is not according to the sectoral system. The MoH only manages the finance for the central institutions; the provincial Bureau of Finance allocates and manages expenditures at the local level. However, due to the need for information for assessments of performance and making investment strategic plans, the MoH still collects and synthesizes data on finance on an annual basis, including average health expenditure per capita from the Government buidget. Health budge includes Government budget share for the health sector every year, grants and loans, health insurance, user fees. - Collection method: 2: *Adminsitrative reports * Data compiled using the NHA method. - Timeliness: * Data from adminsitrative reports: duration between the collection and publication: 6 months. * Data from NHA: duration between the collection and publication: more than 2 years. - Data synthesis cycle: * Collecting and synthesizing and publishing data according to the administrative report system is undertaken every year. * The collection,. Synthesis and publication of data by the NHA: every two years. - Consistency betwween compoents, indicators and time of the above two data sources is not good. The data according to the administrative repotrs is typically lower than the over, for example: In 2002, Government budget expenditure on health: According to administrative reports: VND 8 286 billion According to NHA VND 11 428 billion In 2003, Government budget expenditure on health: According to administrative reports: VND 10 181 billion According to NHA: VND 13 873 billion The causes of the difference between the two sources were also commented upon by the participants as follows: Firstly, the administrative reports do not synthesize all the data from institutions, for example data on health expenditure under the management of other ministries and sectors. Secondly, many localities cannot synthesize all the amount from grants and loans, especially funding from donors for e.g. training and study tours abroad, hiring local and external consultants, procurement of equipment.... Thirdly, some localities (institutions) do not fully report the income from user fees spent on activities. Data of the components in the above two sources are national and provincial ones. Page 40 of 70 Data collected from administrative reports can be classified into: expenditure on health from Government budget, grants and loans, user fees, health insurance, administration, training and expenditure by central and provincial levels, while the NHA categorizes into all components. The data of the NHA is tested, checked and compared with the data from other surveys such as VLSS and data reported by the MoF. 6.2.7. Private health expenditure per capita - Data collection method: household survey and routine reports of health facilities for setting up NHA. - Interval between collection and publicatio: >2 years - Repetition: every 2 years. Data is estimated from annual NHA for all components. - NHA is the unique source which collects data on private health expenditure, thus it assures consistency between components of indicators and time. - Components in NHA represent all components such as household expenditure, private health insurance, NGO, enterprises... Private health expenditure is classified by province, district due to the modest household sample size. Around 50% of data from NHA is checked. 6.2.8. Distribution rate of health staff (total by professional category) Data on the distribution of human resoruces in te health sector includes the total and by profesisonal qualification, thus it does not assure reliability because the data collected and published by the health sector only reflect the public health system under the management of the MoH; data from health facilities in other sectors is not sufficient and there is absence of data from private ehalth facilities. The MoH, MoLISA as well as GSO have not conducted any survey on the manpower in the health sector. The information division of the Department of Planning and Finance has recommended a general survey on the manpower in the public health facilities (permanent and contracted) and in private health facilities, but it has not been conducted due to absence of finance. Therefore, in group discussions and in-depth interviews, the participants only commented on the manpower in te public system. - The method of collecting data on manpower in the public health system based on the administrative records from the commune to the central levels is not tested by any survey. - The existing data on manpower is from the public health system and the interval between the collection and publication is 2 months. - Data on manpower in the ehalth sector nationwide is published every year: 5 times in 5 years. - Because there is only signle source of data (routine reports) synthesized by the GHSIS in combination with the health staff organizational ssytem, thus variables, definitions and classification is consistent over time. - The categorization of manpwer in the health sector is by highest qualification such as doctor of medicine or pharmacy; master; medical doctor; university pharmacist;.... - Data is not categorized by gender/age, urban/rural distribution; public/private sectors etc... 6.3. Indicators on risk factors 6.3.1. Smoking prevalence The data collection method is based on theVLSS 1992-1993 and 1997-1998; VNHS 2001-2002. However, in recent years, the tobacco control program has carried out some studies on smoking in Vietnam, but only focusing on certain groups such as students, military force, cancer pateints, women of Raglai ethnic minority, thus the data cannot be sued for calculating the prevalence int he whole country. Data published recently are derived from the VNHS. The data was collected and published 4 years ago. Page 41 of 70 In te past 10 years, data on smoking has been published twice: VLSS 1997-1998and VNHS 2001-2002. Due to difference in terms of time and sample sizes, there is some difference in terms of data. The coverage of data is relatively optimal nationwide sampling. 6.3.2. Percentage of condom use with high-risk sexual behaviours Data on the use of condoms in the high risk groups was collected by two methods (1) administrative reports of the institutions distributed condoms and (2) household inteviews and interviews with high risk people. Routine data is reported every year on the quantity distributed and number of risk people. The first survey on use of condoms was carried out in 2000-2001 and the second in 2005-2006. Thus, such survey is conducted every 5 years. The survey in 20002001 was carried out in 5 provinces with high prevalence of HIV/AIDS: Hà nội, Hải phòng, HCMC, Đà nẵng and Cần thơ. Data fromt he survey in 2005-2006 is being processed. The results of the surveys were derived from questionnaires using for households, high-risk groups such as sex workers, restaurants, hotels, lorry drivers. Most of the data was published 5 years ago. The data from surveys and service statistics is not highly consistent because service statistics mainly base on the quantity of distributed condoms, thus it cannot fully reflect the number of risk people using condoms, while data from interviews includes those people buy themseves or the quantity distributed but not used. Information on condom use is classified by province and risk group other than by demographic characteristics. 6.3.3. Percentage of households using improved water sources The collection of data on use of water is according to 2 methods: administrative reports and household surveys. Administrative reports are not routine and do not assure reliability, thus the published data currently is mainly based on the VLSS and VNHS. VLSS is carried out every 2 years with 45,900 households (approximately 10.000 househods more than the number in the VNHS 2001-2002. data of 2004 is available (2 years ago). In the past 5 years, data on water use has been published 3 times. There is not consistency between sources of data, for example, in the VLSS 2002, the percentage of households using running water in delta provinces was 33% while it was 20.8% in the VNHS 2001-2002. Likewise, the utilization rate of drilled hole water in delta provinces according to VLSS was 57.6% while it was 28.5% in the VNHS. The cause of such inconsistency is subject to the different sampling methods applied and sample sizes. Furthermore, though the two surveys were conducted in the same year, but in the interval between the two, disaster occurred such as typhoon, flooding, tsunami... results of the surveys would definitely be different from each other. The sampling method of the VLSS is randomized based on the sample design in the cencus 1999. Data on the use of advanced water sources is classified by demographic characteristics: men/women; socio-economic situation: income, major households production or trading; by ecological region, but not by province and educational level of the heads of households. Table 7 Overall scores in Hanoi and Ho Chi Minh cities Indicator Health status Health system Indicators Risk factors indicators Overall health indicators quality Chung 68% 57% 51% 60% Hanoi city 67% 56% 51% 59% Page 42 of 70 Ho Chi Minh city 72% 59% 51% 63% Based on the above analysis and as assessed at the two workshops on information products, only the indicators on health statuswere up to standard: 68%, while other idicator groups did not meet the standard, especially indicators on risk factors: 51%. 6.4. Supplementary indicators 6.4.1. IMR The data collection method is based on routine reports adn demographic change and family planning surveys. - In the reoutine reporting system, data is collected at the commune level. As regulated by the MoH, all deaths in teh commune must be recorded into the A6/YTCS book. This book is kept by the CHS. The CHS holds a meeting with village health workers ocne a month to collect information on mortality in the commune within the monthn and record it into the book (see attached form). By the end of the year, the workers of the CHS synthesize IMR and classified it by deaths during < 7, <28 days and <12 months according to Form 1: “ Population, birth and death report” to submit to the DHB; the DHB synthesizes the data from the CHSs in the district according to form 2/BCTKH and submit to the provincial Health Bureau (Department of Planing); te provincial Health Bureau synthesizes data from districts in the province according to form 2BCTKT to submit to the MoH (Division of Health Information, Department of Planning and Finance). Data on mortality is processed by the GHSIS. The routine reporting system on mortality was highly appreciated in surveys on mortality due to accidents and injuries and cancers. However, in remote and mountainous provinces and the communes without village health workers, it is difficult to collect information on mortality and causes. - Demographic change and family plannig survey Demographic change and family plannig survey is carried out at 0:00 on 1st April every year with approximately 1,600,000 people. The sampling method is the stratified combined with randomized one. Around 26,000 people are surveyed in each province/municipality. Data on child mortality is published every year. The latest data published was in 2005. In the past 10 years, such data has been collected and published for 10 times (annually). Data on child mortality is consistent over time in each source. However, there is some inconsistency between sources (routine reports and surveys). The mortality rate in routine reports is typically lower that that in surveys. The cause is that some provinces, districts and communes do not collect and record information on mortality adequately, especially those in disadvantaged areas, in localities where staff rotation is frequently done and in commnes where there are not sufficient village health workers. The demographic change survey has too small sample size. 6.4.2. Low-weight birth rate (<2500Gram) Data on < 2500 gram children is collected fromt he routine reports from the commune to the district, provincial and central levels. No survey on <2500gram newborns has been conducted. Most CHSs are equipped with infant weight. As regulated by the MOH any newborn must be weighed and the data recorded into the existing form. The CHS has a Delivery book (A4/YTCS): like recording data on mortality, all deliveries in the commune must be recorded intot his book regardless of places of delivery. In order to have sufficient data on deliveries at the commune level the workers of the CHS should collaborate with village ehalth workers to collect information. Based on the delivery book, the CHS synthesizes data on the weighed newborns, including those <2500gram and submit to the DHB according to form 3. The DHB synthesizes data from CHSs according to form 9/BCTKH and submit to the provincial ehalth Bureau. The provincial Health Bureau synthesizes data according to form 10BCTKT and submit to the MoH. As regards low-weight births, in group discussions, the participants reflected taht the percentage of < 2500 gram newborns published by the MoH in 2005 was low (5.1%). The cause was that the weighing of newborns is not up to stanbdard in many facilities. Pregnant women Page 43 of 70 with risk of complication are typically referred to upper levels for deliveries. Typically, the percentage of low-weight births at the upper level is higher than that at the lower one, but it is not reported to the commune level for synthesis. The participants also recommended to establish a Sentinel Delivery surveillance system No. A4/YTCS and A6/YTCS as if these two data are proerply recorded, detailed information on birth/death, especially <2500gram newborns classified according to mother’s age, occupation, tiem of delivery, antenatal care situation... Collecting data on low-weight births by survey is very costly and sometimes mothers do not recall their children’s weight when born. 6.4.3. Morbidity/mortality of 10 leading diseases The data collection for calculating this indicator is based on routine reports. Information on the 10 leading diseases with highest morbidity/mortality is derived from district or upper hospitals because only tese health facilities aer capable of giving accurate diagnoses. Primary data is collected from the medical records of discharged and dead patients. In large hospitals, when a patient is discharged from hospital or dies, the doctor or administrative nurse of the department should base on the diagnosis to record the code of the disease according to ICD10. In small hospitals (district ones), medical records are referred to the department of general planning and the hospital statistical worker is responsible for recording the code. After being coded, medical records are entered into the computer for synthesis according to form 15/BCTKH at the district level and form 16/BCTKT at the provincial level. The list of diseases includes 312 diseases divided into 21 chapters. The data on morbidity and mortality in district hospitals is submitted to the provincial Health Bureau and the provincial Health Bureau synthesizes data from district, provincial and central hospitals in the province to submit to the MOH. The MoH synthesizes data from provincial health Bureaus and selects 10 leading diseases with highest morbidity/mortality. Data on morbidity/mortality of 10 leading diseases is published annually and the latest publication was in 2005. Because of the signle soruce, there is consitency in terms of timw. Data covers around 90% provinces nationwide. However, it is not classified by age/gender; rural/urban distribution... althouth this information is recorded quite sufficiently in the medical records. The cause is was the employment of information technology in data management and processing in many hospitals is limited. Although Medioft is available for processing data, due to limited informatic skill and finance for the hospital stastistical system, it has not been commonly used. Analyzing the above data on morbidity and mortality, many participants and interviewees reflected that such data does not fully reflect the disease and mortality pattern sue to: (1) lack of data from private hospitals and hospitals under other sectors, especially those in the military and public security sectors which provide services to general population, (2) statistics on morbidity and mortality for selecting 10 leading diseases with highest morbidity and mortality only includes inpatient cases, (3) hospital-based mortality is very low compared to reality because in many serious cases patients die at home... 7. Information dissemination and utilization 7.1. Data analysis and use Analysis of data is poor, not only at the grassroots level, but also at the central one. Central ehalth institutions annually collect, process and publish data on health activities and health status. Figures are widely used to present information in statistical publications and at health facilities. The aim of using graphs and charts is for rapid assessment and recognizing disease trend and capacity of providing services at health facilities The graphs typically used in health facilities and publications inlcude diseases over time, morbidity/mortality of some dangerous diseases, including malaria, Dengue fever, TB, HIV/AIDS... but in-depth analysis for planning and policy making is limited. Data and indicators of the HIS are not widely diseminated and transmitted on mass media, greatly affecting the exploration and use of information. Page 44 of 70 The participantes, based on the above analysis, evaluated that data analysis and use only acheived 58%, far from standard of the HMN (see table below) 7.2. Policies and communication The GHSIS synthesizes improtant information on performance of the health sector and people’s health status from surveys and information sub-systems. This information is diseminated through books/documents and reports, but the analysis is poor. Under-5 mortality rate, MMR, vaccination rate against 7 dangesources diseases for children and HIV prevalence are recognized by politicians, central and provincial managers. HIV prevalence and child vaccination rate are routinely transmitted on mass media. Ppolicy makers often use information of the HIS for policy development. However, it is not widely used because of the suspected reliability of some indicators on causes of deaths. The workshops evaluated that the HIS achieved HMN standard, but not high: 67%. 7.3. Plans and setting priority All indicators in the seential indicator set include short-term (one year) ones reflecting the implementation of plans in all areas in the health sector: curative care, reproductive health care, child health care, social diseases control and only the indicators reflecting impacts of health activities on health promotion and improvement serve the assessment of the implementation of the obkectives stated in demium-term and long-term plans, including: life expectancy, IMR and under-5 mortality rate; child malnutrition, MMR, polico elimination, infant tetanus elimination, leprosy and disease pattern... Data of the HIS is sued for analysis, assessment and selection of priorities, butt he pl;anning is not fully based on prioritized issues but on the bduget allocated, for instance, budgetting plan: as presented earlier, localm budget is allocated by te provincial Finance Bureau, thus the same prioritized issue can be allocated different budget due to different allocations of financial resources between localities. Poor provinces can identify priorities, but cannot make action plans due to poor financial resources. Most district health workers use data collected and processed by the district level for analyzing and assessing health service provision in the district without comparison with other districts in the province and natioanl standards because the MoH does not have a feedback system. Thus, planning and priority identification only achieved 63% . 7.4. Resource allocation Some indicators published through the ifnormation system such as data on newly detected diseases, Avian flue (H5N1), SARS and diseases greatly affecting health are supported by the government budget through national health programs. Information of the HIS is widely used by provincial and district health workers in their planning, but support from local budget based on information is limited because the local budget for health is limited compared with need for ehalth services provision. Information of the HIS is routinely used in enhancing equity in health care.The use of information is 55%, far from standard. 7.5. Action performance He participants agreed that health information had been used by managers at all levels in their management, planning and monitoring the health service provision. For example, at the commune level, the CHS bases on information in the immunization A2.1/YTCS book to identify how many children should be vaccinated subsequently and what vaccines should be used so that they can make their immunization plan: estimating vassines, immunization devices, assignment of tacks, ... Likewise, health workers base on the information in the antenatal care book Page 45 of 70 A3/YTCS to know how many aill deliver, who will be provided with service... so as to make plan to assign tasks to the staff in the CHS, prepare tools and medicines... Information on risk factors is used systematically to widely disseminate in mass media and to risk groups.The use of information in management, planning and and monitoring of service provision was most highly appreciated: 70%. Below is assessment at the two workshops Summary Result Maximum Score A Analysis and Use of Information 18 11 B Policy and Advocacy 12 8 C Planning & Priority Setting 9 6 D Resource allocation 12 7 E Implementation/action 9 6 60 37 TOTAL % 58 % 67 % 63 % 55 % 70 % 62 % General assessment of information disemination and use: 62% compared with HMN standards, but the analysis and use of data and resource allocation are not up to standard. 8. Summary of the HIS assessment The assessment and scores in the two workshops and groups discussions as well as indepth interviews are generally consistent. In the 6 areas, two related to the health statistical information system: indicators; publication and use of data achieved the HMN standards (See Table 8): In the data publication and use, section A on “ data analysis and use” and section D on “information-based resource allocation” are not up to standard. The remaining 3 areas including resources, data sources and data management are not up to standard. 8.1. Resources The participants fully agreed with the scores given to the infrastructure, which achieved the standards. The section on policy does not coveraspects of the HIS and some should be revised and refined to be in line with the socio-economic development in the present context, especially developing HIS development strategy up to 2015 and 2020. Resources invested in the information system is limited and not regular; statistical workers are in shortage and instability, especially at the grassroots level. General assessment is presented in Table and the figure below. Table 8 Overall results in Hanoi and Ho Chi Minh cities Overall HIS Dissemination & use Information products Data management Data sources 62% 60% 57% 53% Page 46 of 70 Hanoi city 60% 59% 55% 52% Ho Chi Minh city 66% 63% 61% 55% Indicators Resources Data Sources Administrative records Health service records Health & diseases records Population-based surveys Vital statistics Census Information Products Estimation method / transparency Disaggregation Representativeness / appropriateness Consistency / completeness Periodicity Timeliness Data collection method Quality of Health Information Overall health indicators quality Risk factors Health system Health status - morbidity Health status - mortality 66% 56% 66% 52% 65% 62% 48% 50% 55% 54% 58% 55% 48% 48% 50% 54% 60% 54% 49% 55% 65% 52% 54% 55% 56% 56% 57% 59% 64% 69% 59% 51% 56% 57% 57% 63% 68% 58% 67% 55% 57% 62% 67% 71% 59% 60% 51% 57% 72% 66% 59% 51% 56% 70% 65% 63% 51% 59% 75% 68% Figure 6: Overall health information system in Hanoi and Ho Chi Minh cities Return to Menu Resources Indicators Data sources Data management Information products Dissemination & use Not functional 0% 10% Present but not adequate Not adequate at all 20% 30% 40% 50% 60% Adequate 70% Highly adequate 80% 90% 100% 8.2. Data sources According to assessments and in-depth interviews, capacity for conducting censuses, population-baed surveys such as NHS, demographic change surveys, demographic and health surveys... and emdicalr ecords, including communicable disease surveillance system, is up to Page 47 of 70 standard. Censuses and population-based surveys are acrried out by the State statistical system. Censuses started in 1960 and on a 10-year basis; thus so far, 5 – 6 censuses have been conducted. Demographic and health surveys are also conducted on a 5-year basis. Additionally, those surveys were financially and technically supported by international organizations, thus the State statistical system currently has experienced surveyors and managers. Medical records, including surveillance records are quite good (see assessment of emdical records in section D, part III). Contents of data sources, data publication, integration and use are not up to standard. Data is not widely disseminated, mainly via bookis or workshops and meetings at the central level. There is lack of coordination, assignment of tacks amd ifnormation sharing between sectors and even thiwinth the health sector, causing overlaps in information collection and processing. Figure 7: Data sources in Hanoi and Ho Chi Minh cities Return to Menu Census Vital statistics Population-based surveys Health & diseases records Health service records Administrative records Not functional 0% 10% Not adequate at all 20% 30% 40% Present but not adequate 50% 60% Adequate 70% Highly adequate 80% 90% 100% 8.3. Data management According to the participants, currently at all levels, including the central one, database hardly exists. Data from various levels are mainly those processed and stored in books, paper reports and PC, causing difficulties in the exploration and use of these data. The cause is that the appliaction of the information technology in health facilities in general and in the HIS in particular is poor; identify code for health facilities is not set up to facilitate the combination of databases from various sources. The HIS and sub-systems do not have a good software for data management and processing, thus databases do not have crude data and individual information for analysis of the phenomenon according to various aspects such as demographic characteristics, scio-economic situation and administrative areas. Figure 8 Information products in Hanoi and Ho Chi Minh cities Page 48 of 70 Return to Menu Data collection method Timeliness Periodicity Consistency / completeness Representativeness / appropriateness Disaggregation Estimation method / transparency Not functional 0% 10% 20% Not adequate at all 30% Present but not adequate 40% Page 49 of 70 50% 60% Adequate 70% Highly adequate 80% 90% 100% 8.4. Assessment of information products The srores in group discussions and in-depth interviews were not fully consistent, for instance, according to the scores on information products, data on morbidity and mortality was up to wtandard. But according to the comments by many participants reflected that these scores were not completely accurate as: (1) data on adult mortality was collected from annual demographic change surveys and censuses conducted by the GSO and cannot be compared with other sources. According to the GSO in the census in 1999, the fertility and mortality rate in Vietnam were very low, especially in urban areas, thus the data on births and deaths collected from the 20,000 people was modest and could not assure reliability for estimated of fertility, deaths, (2) MMR and under-5 mortality rate were not consistent between sources (3) surveys for collecting information on under-5 mortality and MMR were also not representative. Figure 9: Information products in Hanoi and Ho Chi Minh cities Return to Menu Selected Indicators & Results Health status - mortality Health status - morbidity Health system Risk factors Overall health indicators quality Not functional 0% 10% Not adequate at all Present but not adequate 20% 30% 40% 50% 60% Adequate 70% Highly adequate 80% 90% 100% 9. HIS orientation 9.1. Analysis of strenths, weaknesses, difficulties, challenges, opportunities of HIS - Strengths In the past years, health statistics and information sector has gained many improvements. The ifnormation has gradually been refined, closely linked to the health service provision network. The indicator and form systems have been set up and provided to all levels. Statistics have been widely used and been an important base doe analysis, assessment and coordination of health care protection and care activities. The contents of the indicator system, colelction and processing methods have gradually reached the international standards. However some shortcomings still need solutions. - Shortcomingsi Agaionst the increasing need for information in the context of promoted cooperation and integration into the region and the world, health information system has revealed weaknesses: Page 50 of 70 - Too many indicators, forms but lack synchronism, which burdens the grassroots health sysetm. Some importnt indicators have not been collected and provided regularly nan not reliable such as MMR, IMR, morbidity and mortality rate, especially causes of deaths by age/gender, sconio-economic situation and administrative areas. There is lack of information from private health facilities thus many indicators could not fully reflect health status and ehalth activities. Statistics have not been processed, stored and transmitted by modern communication facilities, causing difficulties for exploration and use of data. Database at various levels is too poor, even at the central level. Opportunities for strengthening HIS - The statistical system in general and the HIS has been paid special attention to by the Government and leaders of the MOH. Many policies related to statistics and information have been issued (see section 2.1): finance for the statistical information system has been significantly improved. Most censuses, national health survys and some research studies of various sectors and ministries have received financial and technical support from multilateral and bilateral organizations. The routine reporting system in the health sector and other sectors has been supported, but not signitifant; however it also encourages the promotion of the statistical work. Stastical workers in the State statistical system and statistical workers in the health sector at the central level and in some provinces of the GHSIS and information sub-systems are experienced in developing, implementing and operating the system. Health information is used as evidence for plan development and policy making. Challenges to the HIS In addition to opportunities and achievements gained, the HIS still has en cope with many challenges , for example: - Globalization is a rapid process, especially information technology development to improve global information and it requires the HIS to apply these advances and strenths in enhancing its capacity. - Professional qualification and basic knowledge of informatics of health facilities atthe provincial, district and commune levels is limited and unstable, especially most statistical workers due to changed organizational structure. - Financing for the statistical system is poornand not regular. Thus it is impossible to carry out surveys to collect information that cannot be collected though routine reports or check data of routine reports. Finance for procurement of equipment for calculation and capacity enhancement for statistical workers is limited. Most of statistical workers at the provincial and district levels have to share computers with otherr. Many departments and wards in provincial and district hospitals, even at the central level,do not have a computer. Some softwares have been set up but not developed and widely used due to limited finance. - Some policies have been issued but not widely disseminated and they do not cover all aspects of the HIS. There is insufficuiency of necessary conditions for implementation. There is lack of documents regulating the coordination, assignment and information sharing between ministries, sectors and national health programs. No strategy for developing the HIS is available. - Knowledge of data use in analyses, assessments, projections, planning and resource allocation is liomited, thus it does not encourage the responsible people and investment in the HIS. 9.2. Areas potentially developing HIS - AS analyzed by the participants and according to field surveys of Hanoi Medical University, Hanoi School of Public Health and safe Community Program, and cancer prevention program, the form system for collecting causes f deaths developed by the GHSIS is quite good. This system can provide information on causes of deaths by Page 51 of 70 - - demographical characteristics, socio-economic status, administrative areas. This is important information that cannot be collected in the system of the Misnitry of Justice, the system of the National Committee on Population and Family Affairsand even censuses, demographic change surveys and NHS (See section on analysis of birth and mortality above) The participants also recommended to develop sentinel death cause surveillance based on the system of forms on mortality, especially the A6/YTCS book and strengthen training, monitoring the recording at the commune level. The moH, under the support of the WHO has twice set up NHS, thus they are experienced indeveloping documents, forms, surveying, information collection and processing related to health expenditure. Information from the NHA reflects all expenditure items from various sources, both public and private. Therefore, it is immportant to maintain NHA in the coming years and expand it to the provinces and districts and some major diseases such as TB, malaria... In 2001-2002, the MoH, for the first time, conducted a NHS under financial and technical support of SIDA though the WB. Information fromt he NHS is highly appreciated and makes significant contribution to the improvement of database. BAsed on this survey, the MoH has gained experiences to carry out other similar surveys. It was recommended by the participants that such survey should be conducted every 5 years to collect detailed information for comparison and assessment of results and effectiveness of various areas, national health programs in a more objective manner. 9.3. Opportunities for donor coordination BY anaylyzing strenths and weaknesses, opportunities and challenges, the MoH has selected priorities to enhance the HIS (See section 9.4). The MoH would like to recommend that donors should base on their capacity and areas of their concerns to support the HIS. To avoid overlaps, donor support for the HIS or sub-systems should go through the health information division within the Department of Planning and Finance – MoH. WHO will be the technical donor for strengthening and developing the HIS. 9.4. Identifying priorities for strengthening HIS In the group dicsussions in the two workshops, the participants agreed to set some priorities for strengthening the HIS as follows: - Developing a srtategy for HIS development up 2015 and 2020. Based on the objectives of the strategy, developing annual, 5-year and 10-year action plans. Calculating need for necessary resources for implementing activities. - Refining and supplementing policies on statistical and information work to be in line with the context of the sector, in the short-term: (1) regulation on statistical reporting and tools for data collection and processing at private health facilities; (2) Regulation on coordination, assignment of collection, processign and sharing information between ministries, sectors, national health programs in order to minimize duplication and overburden to health facilities. - Developing database for integrating data, including data frm all sources at the central and provincal levels to serve timely the need for analysis, assessment and policy making. Setting up identity codes for health facilities and administrative units to facilitate the connection of databases from various sources. - At the workshops, it was emphasized that one of the important information items that Vietnam currently cannot collect and provide is causes of deaths by gender/age, occupation/educaitonal level,a dministrative area (urban/rural area and regional/provincial level). This is very important information for evaluating socio-economic development and impacts of health activities on health promotion. In order to gain such information IT WAS SUGGESTED to set up a sentinel Death Cause Surveillance System which shall be under the implementation and coordination of the MoH as only health workers can precisely diagnoze causes of deaths. Page 52 of 70 - In the coming time it is required to conduct surveys at private ehalth facilities to gain essential primary information such as facility, patient bedss, human resource.. serving the distribution of health service provision network and planning the training and developing the network of information collection and processing as well as setting up identify codes for public and private health facilities nationwide. - Enhancing capacity for managers, planners and statistical workers as regards use of data in making projections, anlysis, assessment and planning as well as resource allocation. - Developing and refining the indicator and form systems to be in line with the national health indicator system, statistical law and need for information in the context of industrialization and integration into the region and the world. - Promoting the employment of informationt echnology in processing, storing and transmititng information; primarily providing essential informatic and statistical knowledge for statistical workers at all levels, soft ware for hospital management, processing reports, TB, leprosy, malaria, HI patient management etc... - Fostering the dissemination of data on health activities and health status of the community as well as the country through statistical publications such as books, CDs, summaries, pamphlets, booklets websites and other media. - NHS should be conducted every 5 years. The first one was carried out in 2001-2002, thus the second should be conducted in 2007 to be a ground for comparison, assessment and collection of many important information items. (The attached Annex shows the scores, assessment structure, list of essential health indicators of the health sector and greassroots level and tools for collecting information of the GHSIS). Hanoi, 31/12/2006 Page 53 of 70 Annex 1: HMn Assessment tool : scoring See the Excel-file attached. Page 54 of 70 Annex 2: How was the HIS Assessment Organized? --Summary Report 1. Name of country: Viet Nam 2. Members of the stakeholder group (please list all organizations that participated in the planning and execution of the assessment including producers, users and sources of finance for health information) Steering Committee of Working group Project “Strengthening Health Information System” Leader of MOH 1. Dr. Nguyen Thi Xuyen - Vice Minister -Director of Committee Dept of Planning and Finance, MOH 2. Dr. Duong Huy Lieu, Director - Deputy 1. Mrs.Nguyen Thi Tinh- contact Director of Committee person for HMN Secretariat 2. Dr. Hoang Thanh Huong- contact person for HMN Secretariat Dept of Thearapy, MOH 3. Dr Ly Ngoc Kinh, Director, Dept of Treatment, MOH General Dept of Preventive Medicine, MOH 3. Dr.Ha Thai Son 4. Dr. Pham Hung 4. Dr Nguyen Van Binh, Vice Director Dept of Reproductive Health, MOH 5. Dr. Nguyen Dinh Loan, Director 5. Dr. Duong Thi Hai Ngoc Population and labour Dept., GSO 6. Mr. Dong Ba Huong, Director 6. Nguyen Huu Ba Dept of Social Environmental Affairs, GSO 7. Mr. Nguyen Phong, Director National Institute of Malariology, Parasitological and Entomology 7. Nguyen Thi Loan 8. Pham Anh Tuan 8. Dr Le Khanh Thuan, Director National Institute of Nutrition 9. Dr Nguyen Cong Khan, Director National institute of Hygiene & Epidemiology 10. Dr.Phan Hoai Duong 11. Dr.Vu Dinh Thiem Page 55 of 70 11. Dr Nguyen Tran Hien, Director, National Hospital of Tuberculosis and Respiratory Disease 12. Dr Dinh Ngoc Sy, Director, 12. Dr. Mai Tuyet Nhung Cabinet, MOH 13. Dr. Do Han, chief of Cabinet Dept. of Science and Training 14. Dr. Truong Viet Dung, Director Vietnam Drug Administration 15. Dr. Cao Minh Quang, Director Dept. of Medical Equipment & Construction 16. Mr. Nguyen Van Tinh, Director 17. Which unit or units took the lead in organizing the assessment? (e.g. "Central Statistics Office" or "M&E unit of the Ministry of Health", etc…) Ministry of Health, Health Statistics & Informatics Division of Dept. of Financial & Planning 18. Please describe briefly how the assessment was organized. How many separate meetings were held? Include meetings for planning the assessment as well as meeting for carrying out the assessment. This includes how many meetings of the full stakeholder group? This includes how many meetings of smaller worker group? * Desk review of HMN protocol and assessment tool, translate HIS assessment tool into vietnamese from May to Aug. 2006. * Training Workshop of Trainers: + Duration time: 02 days , 17-18 August 2006 + Trainers is three International Experts from HMN + Trainees: a HMN working group, participants from Hanoi Medical University. + Contents of Workshop: . Presentation on introduction to HMN framework and tools by International consultant . Guidance on making assessment final reports - International consultants . Practice - working group with computer of HMN assessment tools . Discuss on how to organize and facilitate the synthesis, writing up and presentation of the findings; preparations for development of a comprehensive strategic plan; * Revise and adjust some questionaires of the HIS assessment appropriate to Vietnam’s conditions * Two workshops were organized in Hanoi (Aug. 23-24, 1006) and Ho Chi Minh city (Sep. 7-8, 2006). a. Participants were Provincial Health Officers of the Department of Planning and Session of Health statistics. Participant number was 176 who attended the two workshops. Page 56 of 70 Workshop in Hanoi city for participants from 31 provinces and cities in the North as well as from the Ministry of Health, General Statistics Office, WHO were participated. Workshop in Ho Chi Minh city for participants from 31 provinces and cities in the South. b. Scheduled program: each Workshop was conducted for full two days. In the first day, participants have reviewed and completed the designed questionnaire made by HMN. In the second day, group discussions on the results of assessment. c. Data input was made. d. Make the final report on HIS assessment. 2. Meetings of smaller working groups -- Were subsets of items assessed by smaller working groups? YES or NO If yes, in the space below, indicate the number and types of participants (for example, "program managers" or "central statistics office and other statisticians and demographers" or "donors"), the number of items they assessed and the approximate number of hours that they met to assess these items We designed a questionnaires based on six components of HMN tool. This questionnaire was used in smaller working groups. We invited the leader, manager, planner and statistician of units as follow: + Committee of Population, Family & Child + Ministry of Justice + Departments belong to MOH: Department of Organization and Personnel, Dept. of Reproductive Health, Dept. of Thearapy, Dept. of Planning & Finance… + National vertical Programs: Tuberculosis Program, HIV/AIDS, National Institute of Nutrition, National Institute of Malaria… The contents of meeting: + Introduce the purpose of HIS assessment + Review and discussion on current HIS of sub- system + Collect recommendation in order to improving HIS 3. What role, if any was played by a national or international consultant? A working group who are from GSO, Hanoi Medical university, departments belong to the Ministry of Health, National vertical Programs was invited to introduce HMN and the goal of HMN assessment in Viet Nam. One national consultant from Hanoi Medical University has been closely participated during HMN assessment in Hanoi and Ho Chi Minh cities as well as in three provinces. 4. Was a national consensus conference organized to conclude the assessment and review the findings? YES NO If YES, please list all the organizations that were represented and indicate the number of participants. Now we will prepare to conduct the Workshop dissemination on the main findings of the HIS assessment in Vietnam 5. Briefly describe any modifications that were made to the assessment tool. Also note if the tool was translated. No modifications were made to the assessment tool. Page 57 of 70 The assessment tool has been translated into Vietnamese and used by all participants during workshop in both Hanoi and Ho Chi Minh cities. 6. List the item# of any items that were omitted from the assessment because they were judged to be inappropriate. No 7. List the item# of any items that were not well understood. Please offer any suggestions for clarifying the meaning of specific items. No 8. Describe any special problems you had with organizing the assessment 9. Has the final report on the assessment been completed? YES 10. How much time was required to complete the assessment process -- from the first planning meeting until the concluding meeting, how many weeks elapsed? The first plan was made in August 17-18, 2006. The first workshop was conducted in Hanoi city in August 23-24, 2006. The second workshop was conducted in Ho Chi Minh city in September 7-8, 2006. The indept-interviews was conducted from september to December 2006 11. Please offer any further comments or recommendations on how to improve the assessment tool or how to organize a successful assessment (use a separate sheet of paper if necessary) Vietnam highly appreciates the HMN tool set and considers it as an important tool set for assessing the HIS. However, during the use of this set, some shortcomings have been found: + The contents of questions include too many aspects such as socio-economic status; age/gender; province/region/urban/rural; it is advisable to separate the public and private aspects to facilitate the scoring. + The score table is limited, thus it also affects the results of assessment. To organize a successful assessment: should be combined between using HMN tool and dept- interview and discussion to find the shortcoming and solutions . Page 58 of 70 Annex 3 List of essential health indicators Issued under Decision No. 2553 /2002QD-BYT dated June 4 th 2002 by the Ministry of health I Population, socio-economic situation and environment 1 Population growth rate (%o) 2 Natural population growth rate (%) 3 Crude birth rate (%o) 4 Crude death rate (%o) 5 Total fertility rate ( Number of children) 6 Percentage of population by age and sex group (%) 7 Gross domestic product per capita (000VND) 8 Literacy rate by sex (%) In which: Male (%) Female (%) 9 Percentage of population using safe water (%) In which: Urban (%) Rural (%) 10 Percentage of population using hygienic toilet (%) In which: Urban (%) Rural (%) II Input indicators 11 Percentage of Government Health budget in GDP (%) 12 Percentage of Government Health budget in expenditure of state budget (%) 13 Health budget per capita (1000VND) 14 Proportion of health Expenditure by each field (preventive, curative, training, management) (%) 15 Number of beds per 10000 inhabitants 16 Number of Medical doctors per 10000 inhabitants 17 Number of pharmacists per 10000 inhabitance 18 Number of nurses per 10000 inhabitants 19 Number of dentist per 10000 inhabitants 20 Percentage of communes having CHS 21 Percentage of commune having Medical doctors 22 Percentage of commune having midwives or pediatrics; obstetrics assistant Page 59 of 70 23 Percentage of hospitals having basic equipment in four departments ( image diagnosis, laboratory, intensive care, operating theatre) 24 Percentage of commune with adequacy of essential drugs 25 Percentage of village having Health worker Of which: Percentage of village having trained health worker Percentage of village having trained health worker at least elementary medical attainment 26 Drug expenditure per capita (1000VND) III Performance and Output indicators Nutrition indicators 27 Average protein intake per capita (%) 28 Average calorie intake per capita (Kcal) 29 Weight malnutrition rate of children < 5 years of age (%) 30 Height malnutrition rate of children < 5 years of age (%) 31 Weight/ height malnutrition rate of children < 5 years of age (%) 32 Percentage of low birth weight (%) 33 Adults Body mass index (BMI) Treatment activities 34 Average number of contacts per capita (times/year) 35 Percentage of insured contacts 36 Number of in-patients per 1000 inhabitants 37 Percentage of insured in-patient among total in-patients 38 Number of out- patients per 1000 inhabitants 39 Average length of hospitalization per inpatient (days) 40 Average length of hospitalization per discharge inpatient (days) 41 Bed occupancy rate (%) 42 Bed rotation (Number of inpatients/ bed/ year) 43 Percentage of operations among of inpatients 44 Percentage of simple operations among of inpatients Reproductive health and Family planning 45 Percentage of women age from 15 to 35 vaccinated with TT 2 46 Percentage of pregnant women vaccinated with TT 2 47 Percentage of pregnant women with at least 1 antenatal care contact 48 Percentage of women with 3 antenatal care contacts 49 Percentage of deliveries in health facilities Page 60 of 70 50 Percentage of deliveries attended by trained health worker 51 Percentage of mothers who received post-natal care Of which: postnatal care during the first week after delivery 52 Percentage of pregnant women <19 years of age 53 Contraceptive prevalence rate (%) 54 Method specific contraceptive rate ( IUD; Pill; condom; sterilization, ... %) 55 Contraceptive complication rate (%) 56 Menstrual regulation and voluntary abortion ratio (%) 57 Spontaneous abortion ratio (%) 58 Morbidity and mortality ratio of obstetric complication ( %o) 59 Infertility rate (%) 60 Percentage of women received gynecological examination 61 Percentage of women received gynecological treated Child health care 62 Percentage of children< 1 year old fully vaccinated 63 Percentage of children < 1 year of age vaccinated against Tuberculosis (BCG) 64 Percentage of children<1yers. vaccinated against Pertussis, Tetanus; Diphtheria 65 Percentage of children < 1 year of age vaccinated against Polio 66 Percentage of children < 1 year of age vaccinated against Measles 67 Percentage of children 1-5 years vaccinated against encephalitis 68 Percentage of children <1 year vaccinated against Hepatitis 69 Percentage of children 3-5 year vaccinated against Typhoid 70 Percentage of children 2-5 year vaccinated against Cholera 71 Morbidity and mortality rate of 6 vaccine preventable diseases of children (%o) 72 Morbidity and mortality rate of Neonatal Tetanus ( per 1000 live births) 73 Average number of diarrhea episodes among children <5 years ( Times/child) 74 Percentage of diarrhea cases of children treated with ORS 75 Mortality rate from diarrhea of children < 5 years of age (per 100000 children ) 76 Average number of ARI episodes among children <5 years of age (Times/ child) 77 Mortality rate from ARI of children < 5 years of age (per 100000 children ) 78 Percentage of ARI cases of children without pneumonia treated by antibiotics 79 Percentage of Pneumonia of children < 5 years of age correctly treated 80 Percentage of serious pneumonia of children < 5 years of age transferred 81 Percentage of children <36 months of age provided vitamin A 82 Percentage of children <2 years of age using Growth chart 83 Percentage of children form 2 to 5 years of age using Growth chart Page 61 of 70 Social diseases control 84 Prevalence rate of Leprosy (per 10000inhabitants) 85 Incidence rate of Leprosy (per 100000inhabitants) 86 Proportion of new leprosy cases with degree 2 and over of disability (%) 87 Morbidity and mortality rate of Tuberculosis (per 100000inhabitants) 88 Notification rate of Tuberculosis (per 100000 inhabitants) 89 Rate of patients recovered from AFP+ 90 Incidence of AFB+ pulmonary TB (per 100000inhabitants) 91 Mortality rate in Tuberculosis treatment 92 Mortality and mortality rate due to malaria (100000 Inhabitants) 93 Malaria protected population rate (%) 94 Malaria treatment rate (%) Of which: Malaria cure rate (%) , Treatment for malaria prevention 95 Percentage of blood smears positive with parasite (%) 96 Number of malaria outbreaks 97 Malaria mobility, mortality rate of children <15 years of age (per 100,000) 98 Malaria mortality, mortality rate of pregnant women (100,000 pregnant women) 99 Percentage of household use iodized salt 100 Median urinary iodine level 101 Prevalence of goiter in school- age children (%) 102 Number of new HIV/AIDS (persons) 103 Cumulative number of HIV/AIDS (persons) 104 Number of death due to AIDS (persons) 105 Proportion of congenital syphilis of newborn (%) 106 Proportion of gonorrhea of eyes in newborn (%) 107 Proportion of Epilepsy (per 100000 inhabitants) 108 Proportion of Schizophrenia (per 100000 inhabitants) 109 Proportion of disabled persons (%o) 110 Percentage of disabled persons 15 are affiliated (%) 111 Percentage of disabled children <15 years of age are attended school (%) 112 Number of food poisoning outbreaks IV Impact indicators 113 Morbidity, mortality rate of communicable, important diseases (per100,000 inhabitants) 114 Ten leading causes of morbidity and mortality in hospitals (per 100,000 inhabitants) 115 Proportion of Disease chapter or group in hospital (%) Page 62 of 70 116 Under 5 years old mortality rate 117 Infant mortality rate ( per 1000 live births) 118 Perinatal mortality rate (per 1000 live births) 119 Maternal mortality ratio (per 100000 live births) 120 Life expectancy at birth (years) Of which: Male (years) Female (years) 121 Human development index Total of indicators: 121 Minister of Health Signed Page 63 of 70 List of basic district indicators Issued in decision no. 2553 /2002QĐ-BYT dated June 4th of 2002 of the Ministry of Health I Population, socio-economic and environment indicators 1 Population growth rate (%o) 2 Natural population growth rate (%) 3 Crude birth rate (%o) 4 Crude death rate (%o) 5 Literacy rate by sex (%) Of which: Male (%) Female (%) 6 Percentage of population using safe water (%) Of which: Urban (%) Rural (%) 7 Percentage of population using hygienic toilet (%) Of which: Urban (%) Rural (%) 8 Percentage of households practicing appropriate waste treatment 9 Percentage of households practicing appropriate animal waste treatment II Input indicators 10 Health budget per capita (1000VND) 11 Percentage of communes having CHS 12 Percentage of village having Health worker Of which: Percentage of village having trained health worker Percentage of village having at least elementary health workers medical attainment 13 Percentage of commune having Medical doctors 14 Percentage of commune having midwives or pediatrics; obstetrics assistant 15 Percentage of commune with adequacy of essential drugs III Performance and Output indicators Nutrition indicators 16 Weight malnutrition rate of children < 5 years of age (%) 17 Percentage of low birth weight (< 2500gram) Health education 18 Percentage of health workers of CHS and Villages are trained on basis health Education skills (%) Page 64 of 70 19 Number of times of Health education broadcasting on the commune media system (Times/commune/year) 20 Number of times of Health education is to be integrated in content of community’s meetings (times/commune/year) 21 Percentage of households understand the essential knowledge on Health care practice Practice Treatment activities 22 Average number of consultations per capita (times/year) 23 Percentage of patients being given appreciate diagnose and treatment at CHS 24 Percentage of patients being given treatment with traditional medicine or combined Therapies 25 Number of in-patients per 1000 inhabitants 26 Number of out- patients per 1000 inhabitants 27 Average length of hospitalization per inpatient (days) 28 Average length of hospitalization per discharge inpatient (days) 29 Bed occupancy rate (%) 30 Bed rotation (Number of inpatients/ bed/ year) 31 Percentage of operations among of inpatients 32 Percentage of simple operations among of inpatients Reproductive health and Family planning 33 Percentage of women age from 15 to 35 vaccinated with TT 2 34 Percentage of pregnant women vaccinated with TT 2 35 Percentage of pregnant women with at least 1 antenatal care 36 Percentage of women with 3 antenatal cares during pregnancy 37 Percentage of deliveries attended by trained health worker 38 Percentage of deliveries in health facilities 39 Percentage of mothers who received post-natal care Of which: postnatal care during the first week after delivery (%) 40 Percentage of pregnant women <19 years of age 41 Contraceptive prevalence rate (%) 42 Method specific contraceptive rate (IUD; Pill; condom; sterilization, ... %) 43 Contraceptive complication rate (%) 44 Menstrual regulation and voluntary abortion ratio (per 100 live births) 45 Percentage of women received gynecological examination 46 Percentage of women received gynecological treated Page 65 of 70 Child health care 47 Percentage of children < 1 year of age vaccinated against Tuberculosis (BCG) 48 Percentage of children<1yers vaccinated against Pertussis, Tetanus; Diphtheria 49 Percentage of children < 1 year of age vaccinated against Polio 50 Percentage of children < 1 year of age vaccinated against Measles 51 Percentage of children< 1 year old fully vaccinated 52 Percentage of children 1-5 years vaccinated against encephalitis 53 Percentage of children <1 year vaccinated against Hepatitis 54 Percentage of children 3-5 year vaccinated against Typhoid 55 Percentage of children 2-5 year vaccinated against Cholera 56 Morbidity and mortality rate of 6 vaccine preventable diseases of children (%o) 57 Morbidity and mortality rate of Neonatal Tetanus (per 1000 live births) 58 Average number of diarrhea episodes among children <5 years of age (Times/child) 59 Percentage of diarrhea cases of children treated with ORS 60 Mortality rate from diarrhea of children < 5 years of age (per 100000 children) 61 Average number of ARI episodes among children <5 years of age (Times/ child) 62 Percentage of ARI cases of children without pneumonia treated by antibiotics 63 Percentage of Pneumonia of children < 5 years of age correctly treated 64 Percentage of serious pneumonia of children < 5 years of age transferred 65 Percentage of children <36 months of age provided vitamin A 66 Percentage of children <2 years of age using Growth chart 67 Percentage of children form 2 to 5 years of age using Growth chart 68 Percentage of pupils having annual health examination Of which: The pupils at kindergarten (%) The pupils at primary and secondary school 69 Percentage of pupils at primary and secondary school given dental care services 70 Percentage of pupils given examinations to be sent to his/her family (%) Social diseases control 71 Prevalence rate of Leprosy (per 10000 inhabitants) 72 Incidence rate of Leprosy (per 100000 inhabitants) 73 Morbidity and mortality rate of Tuberculosis (per 100000 inhabitants) 74 Notification rate of Tuberculosis (per 100000 inhabitants) 75 Incidence of AFB+ pulmonary TB (per 100000 inhabitants) 76 Rate of patients recovered from AFP+ 77 Mortality and mortality rate due to malaria (100000 Inhabitants) 78 Malaria protected population rate (%) Page 66 of 70 79 Malaria treatment rate (%) Of which: Malaria cure rate (%) Treatment for malaria prevention (%) 80 Percentage of blood smears positive with parasite (%) 81 Number of malaria outbreaks 82 Malaria mobility, mortality rate of children <15 years of age (per 100000) 83 Malaria mortality, mortality rate of pregnant women (100 000 preg. women) 84 Percentage of household use Iodized salt (%) 85 Number of new HIV/AIDS (persons) 86 Cumulative number of HIV/AIDS (persons) 87 Number of death due to AIDS (persons) 88 Proportion of Epilepsy (per 100000 inhabitants) 89 Proportion of Schizophrenia (per 100000 inhabitants) 90 Proportion of disabled persons being registered (%o) 91 Percentage of disabled persons given consultations and rehabilitation 92 Percentage of invalids 15 are affiliated 93 Percentage of children <15 years of age are attended school 94 Number of food poisoning outbreaks IV Impact indicators 95 Morbidity, mortality rate of communicable, important diseases (per 100000 inhab.) 96 Ten leading causes of morbidity & mortality in district hospital (per 100000inhab.) 97 Proportion of Disease chapter or group in hospital (% of each group of ICDX) Total of indicators: 97 Note: Morbidity, mortality of communicable, important diseases include the cases and deaths of dengue fever and food poisoning. Minister of Health Signed Page 67 of 70 Register, Report form System at all level (See Excel-file attached) 1. At Communal health center (CHC) 1.1. Primary registers: + Consultation register A1/YTCS + Immunization register A2/YTCS This register includes 2 registers A2.1 and A2.2 to monitor the immunization situation of women and children. + Prenatal care register A3/YTCS + Delivery register A4/YTCS + Family planning register A5/YTCS + Mortality register A6/YTCS + Malaria control register - A7/YTCS + Tuberculosis register - A8/YTCS + Mental register - A9/YTCS + Leprosy management card. 1.2. The report forms of CHC: 7 forms - Monthly report: Form 6 (Bcx6): 28 communicable diseases and serious diseases in which communicable diseases: 24 - Quaterly report, every 6 month, every 9 month + Form 2 (Bcx2) - health budget + Form 3 ( Bcx3) - children health care + Form 4 (Bcx4) - matermal health care and family planning consultation - treatment activity + Form 5 (Bcx5) - consultation and treatment activities + Form 6 ( Bcx6) - preventive activities + Form 7 (Bcx7) - communicable and important diseases - Yearly report + Form 1 (Bcx1) - Population and birth and death information, commune health staff, establishment and equiments 2. At District level - Form 1- BCT: population, administration unit and CHC facilities - Form 2- BCT: birth and death statistics Page 68 of 70 - Form 3- BCT: health finance at the district - Form 4- BCT: health finance at the district - Form 5- BCT: health facilities and beds - Form 6- BCT: health manpower at the local facilities - Form 7- BCT: Pharmacy production and bussiness - Form 8- BCT: health equipment of district - Form 9- BCT: child health care - Form 10- BCT: maternal health care - Form 11- BCT: family planning - Form 12- BCT: curative care and treatment - Form 13- BCT: preventive care - Form 14- BCT: communicable diseases - Form 15- BCT: morbidity and mortality in hospital 3. At Provincial level - Form 1- BCT: population, administration unit and CHC facilities - Form 2- BCT: birth and death statistics - Form 3- BCT: health finance at the province - Form 4- BCT: health finance at the province - Form 5- BCT: health facilities and beds - Form 6- BCT: health manpower at the local facilities - Form 7- BCT: health worker training in the local - Form 8- BCT: health equipment of province - Form 9- BCT: child health care - Form 10- BCT: maternal health care - Form 11- BCT: family planning - Form 12- BCT: curative care and treatment - Form 13- BCT: preventive care - Form 14- BCT: communicable diseases - Form 15- BCT: morbidity and mortality in hospital Page 69 of 70 Health statistical regulation Page 70 of 70