Curriculum Block The Behavioral Changes and Disorders

Study Guide Behavior Changes and Disorders
TABLE OF CONTENTS
Table of Contens
The Seven General Core Competencies
Page
1
2
Planner team & Lecturers
Facilitators
3
5
Time Table (Regular Class)
Time Table (English Class)
6
7
12 Important Informations
Student’s Project
Meeting of the students’ representative
Assessment Method
Learning Programs
Basic Clinical Skill
Curriculum Mapping
References
57
64
65
12
14
14
15
Udayana University Faculty of Medicine, DME 1
Study Guide Behavior Changes and Disorders
The Seven General Core Competencies
1. Patient Care
Demonstrate capability to provide comprehensive patient care that is compassionate, appropriate, and effective for the management of health problems, promotion of health and prevention of disease in the primary health care settings.
2. Medical Knowledge Base
Mastery of a core medical knowledge which includes the biomedical sciences, behavioral sciences, epidemiology and statistics, clinical sciences, the social aspect of medicine and the principles of medical ethics
3. Clinical skill
Demonstrate capability to effectively apply clinical skills and interpret the findings in the investigation of the patients
4. Communication
Demonstrate capability to communicate effectively and interpersonally to establish rapport with the patient, family, community at large, and professional associates, that results in effective information exchange, the creation of a therapeutically and ethically sound relationship
5. Information Management
Demonstrate capability to manager information which includes information access, retrieval, interpretation, appraisal, and application to patience’s specific problem, and maintaining records of his or her proactive for analysis and improvement
6. Professionalism
Demonstrate a commitment to carrying out professional responsibilities and to personal probity, adherence to ethical principles, sensitivity to a diverse patient population and commitment to carrying out continual self-evaluation of his or her professional standard and competence
7. Community-based and health system-based practice
Demonstrate awareness and responsiveness to larger context and system of health care, and ability to effectively use system resource for optimal patient care.
Udayana University Faculty of Medicine, DME 2
Study Guide Behavior Changes and Disorders
Members Planning Group
No
1
NAME
Dr dr Cokorda Bagus Jaya Lesmana, SpKJ (K)
(Head)
2 dr Anak Ayu Sri Wahyuni, SpKJ (Secretary)
3 dr Luh Nyoman Alit Aryani, SpKJ
4 dr Wayan Westa, SpKJ (K)
No
5 Dr dr Ida Bagus Fajar Manuaba, SpOG, MARS
Lectures
NAME
1 Dr dr Cokorda Bagus Jaya Lesmana, SpKJ (K)
2 dr Wayan Westa, SpKJ (K)
3 dr Anak Ayu Sri Wahyuni, SpKJ
4 dr I Gusti Ayu Endah Arjana, Sp.KJ (K)
5 dr Lely Setiawati, Sp.KJ (K)
6 dr Ida Ayu Kusuma Wardani, SpKJ, MARS
7 dr Ni Ketut Putri Ariani, SpKJ
8 dr Ni Ketut Sri Diniari, SpKJ
9 dr Luh Nyoman Alit Aryani, SpKJ
10 dr I Gusti Ayu Indah Ardani, SpKJ
11 Dr dr Anak Agung Ayu Putri Laksmidewi Sp.S(K)
12 Dr dr Ida Bagus Fajar Manuaba, SpOG, MARS
13 dr Yenni Kandarini, SpPD
14 dr I Gusti Ayu Artini, M.Sc
15 DR. Ni Made Swasti Wulanyani, S.Psi., M.Erg., Psi
DEPARTMENT
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Obgyn
PHONE
0816295779
0361 7814010
085737717244
081999200900
081558101719
DEPARTMENT
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Psychiatry
Neurology
Obgyn
Internal Medicine
Pharmacology
Psychology
PHONE
0816295779
081999200900
0361 7814010
08123916842
08174709797
08123813831
08123806397
081338748051
085737717244
08123926522
0811388818
081558101719
08123805344
08123650481
08123764595
Udayana University Faculty of Medicine, DME 3
Study Guide Behavior Changes and Disorders
Curriculum Block The Behavioral Changes and Disorders
Aims:
1. Comprehend professional competence and ensure the highest quality care to those with mental illness
2. Comprehend the psychodynamic and psycho pathological process of the behavior disorders
3. Diagnose and manage patient with mental illness
4. Diagnose and manage patient with behavioral problems related with medical condition
5. Educate patient and their family, and community about behavior changes and disorders
Learning Outcomes:
Awareness of lifestyle as a risk factor of behavior changes and psychiatric disorders and the importance of early treatment and proper management and prevention
Recognizance of the new paradigm of medical practice: beyond bio-psycho-sociocultural model
Define medical and allied sciences, health prevention and health promotion in the relationship between medical competencies and the contributions of medical and allied sciences, professional skills and attitudes to the prevention and treatment of behavioral disorders.
Curriculum Contents:
1. Demonstrate ability to diagnose, manage and refer patient with problems in developmental stage of personality
2. Demonstrate ability to diagnose, manage and refer patient with psych-organic syndromes and disorders.
3. Demonstrate ability to diagnose, manage and refer patient with psychosis symptoms.
4. Demonstrate ability to diagnose, manage and refer patient with bipolar disorders
5. Demonstrate ability to diagnose, manage and refer patient with anxiety disorders
6. Demonstrate ability to diagnose, manage and refer patient with somatoform disorders.
7. Demonstrate ability to diagnose, manage and refer patient with sexual disorders
8. Demonstrate ability to diagnose, manage and refer patient with insomnia symptoms
9. Demonstrate ability to explain psycho pharmacology
10. Demonstrate ability to diagnose, manage and refer patient with self harm and suicidal behavior
11. Demonstrate ability to diagnose, manage and refer patient with problem related to child abuse or neglected
12.
Demonstrate ability to promote healing process in psychiatric patients
Udayana University Faculty of Medicine, DME 4
Study Guide Behavior Changes and Disorders
Class A
No Name
1 dr. I Gede Budhi Setiawan,
Sp.B(K)Onk
2 dr. Made Dharmadi , MPH
3 dr. Juli Sumadi, Sp.PA
4 dr. Reni Widiastuti
5 dr. Dewi Sutriani Mahalini , Sp.A
6 dr. Dewa Ayu Mas Shintya Dewi,
Sp.An
7 dr. Nyoman Astika, Sp.PD-Kger-
FINASIM
8 dr. Desak Ketut Indrasari Utami,
Sp.S
9 dr. Ayu Setyorini Mestika
Mayangsari, M.Sc,Sp.A
10 dr. Ni Luh Putu Eka Diarthini,
S.Ked
11 dr. Anak Agung Gde Yuda
Asmara, Sp.OT
12 dr. Agus Roy Rusly Hariantana
Hamid, Sp.BP
Class B
No Name
Facilitators
Group
1 dr. Pande Kurniari, Sp.PD
2 dr Ni Wayan Sucindra Dewi
3 dr Ni Nyoman Metriani Nesa,
M.Sc.,Sp.A
4 dr Ni Made Susilawathi, Sp.S
5 dr. Ariesanti Tri Handayani ,
Sp.M
6 dr I Gusti Agung Gede Utara
Hartawan, Sp.An
7 dr. Putu Yuliandari, S.Ked
8 dr. I G.A. Indah Ardani, Sp.KJ
9 dr. I Wyn Subawa, Sp.OT
10 dr. Ida Ayu Dewi Wiryanthini, M
Biomed
11 Dr.dr. Dyah Pradnyaparamita
Duarsa, M.Si
12 dr. Ida Bagus Sutha, Sp.P
B8
B9
B10
B11
B12
B5
B6
B7
B1
B2
B3
B4
A6
A7
A8
A9
A10
Group
A1
A2
A3
A4
A5
Dept
Surgery
Public Health
Anatomy
Pathology
Pharmacology
Pediatric
Anasthesi
Interna
Neurology
A11
A12
Pediatric
Parasitology
Orthopaedi
Surgery
Phone
08123923956
08123804985
082237407778
08174742501
08123641466
085238514999
08123974128
0811385099
081353286780
081353077733
081337870347
08123511673
Venue
(3 rd floor)
3 nd floor:
R.3.01
3 nd floor:
R.3.02
3 nd floor:
R.3.03
3 nd floor:
R.3.04
3 nd floor:
R.3.05
3 nd floor:
R.3.06
3 nd floor:
R.3.07
3 nd floor:
R.3.08
3 nd floor:
R.3.20
3 nd floor:
R.3.21
3 nd floor:
R.3.22
3 nd floor:
R.3.23
Dept
Interna
Pharmacology
Pediatric
Neurology
Opthalmology
Anasthesi
Microbiology
Psychiatry
Orthopaedi
Biochemistry
Public Health
Pulmonology
Phone
082147176796
08113935700
081337072141
08124690137
0818375611
08123868126
089685415625
08123926522
081337096388
081239990399
081835777
081916708565/
08123990362
Venue
(3 rd floor)
3 nd floor:
R.3.01
3 nd floor:
R.3.02
3 nd floor:
R.3.03
3 nd floor:
R.3.04
3 nd floor:
R.3.05
3 nd floor:
R.3.06
3 nd floor:
R.3.07
3 nd floor:
R.3.08
3 nd floor:
R.3.20
3 nd floor:
R.3.21
3 nd floor:
R.3.22
3 nd floor:
R.3.23
Udayana University Faculty of Medicine, DME 5
Study Guide Behavior Changes and Disorders
Time Table
Regular Class
Day/
Date
Time
1
Friday
8 May
2015
2
Monday
11 May
2015
3
Tuesday
12 May
2015
4
Wed
13 May
2015
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 09.30
09.30 – 12.00
12.00 – 14.00
14.00 – 15.00
Activity
Lecture 1: Introduction to
Behavior Changes and Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 2: Mental Status
Examination and Assessment
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 3: Psychological Test
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 4: Neurobehavioral approach to Behavior Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
5
Monday
18 May
2015
6
Tuesday
19 May
2015
7
Wed
20 May
2015
8
Thursday
21 May
2015
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
Lecture 5: Prenatal Psychobiology
(Case of Baby Blues)
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 6: Behavior Changes Due to a General Medical Condition
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 7: Delirium and Dementia
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 8 : General Approaches to
Substance Abuse
Independent learning
Group Discussion
Break and student project
Plenary session
Venue
Class room
Discussion room
Class room
Conveyer
Dr Sri Wahyuni
Dr Sri Wahyuni
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Sr Diniari
Dr Sri Diniari
DR Wulanyani
DR Wulanyani
DR Dr Laksmi
DR Dr Laksmi
DR Dr IB Fajar
DR Dr IB Fajar
Dr Yenni
Dr Yenni
Dr Endah
Dr Endah
Class room
Discussion room
Class room
Dr Westa
Dr Westa
Udayana University Faculty of Medicine, DME 6
9
Friday
22 May
2015
10
Monday
25 May
2015
11
Tuesday
26 May
2015
12
Wed
27 May
2015
13
Thursday
28 May
2015
14
Friday
29 May
2015
15
Monday
1 June
2015
16
Wed
3 June
2015
17
Thursday
4 June
2015
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
Lecture 9 : Primary & Secondary
Insomnia
Independent learning
Group Discussion
Break and student project
Plenary session
Lecturer 10: Schizophrenia &
Other Psychoses
Independent learning
Group Discussion
Break and student project
Plenary session
Lecturer 11: Delusional &
Schizoaffective Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 12: Bipolar Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 13: Panic Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 14: Somatoform
Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 15: Generalized Anxiety &
Obsessive-Compulsive Disorder
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 16: PTSD
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 17: Sexual Disorders
Independent learning
Group Discussion
Break and student project
Plenary session
Study Guide Behavior Changes and Disorders
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Alit Aryani
Dr Alit Aryani
DR Dr Cok Bagus
DR Dr Cok Bagus
Dr Sri Diniari
Dr Sri Diniari
Dr Lely
Dr Lely
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Indah
Dr Indah
Dr Indah
Dr Indah
Class room
Discussion room
Class room
Dr Putri
Dr Putri
Class room
Discussion room
Class room
Class room
Discussion room
Class room
DR Dr Cok Bagus
DR Dr Cok Bagus
Dr Westa
Dr Westa
Udayana University Faculty of Medicine, DME 7
Study Guide Behavior Changes and Disorders
18
Friday
5 June
2015
19
Monday
8 June
2015
20
Tuesday
9 June
2015
21
Wed
10 June
2015
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 09.00
09.00 – 10.30
10.30 – 12.00
12.00 – 14.00
14.00 – 15.00
08.00 – 15.00
Lecture 18: Psycho-Pharmacology
Independent learning
Group Discussion
Break and student project
Plenary session
Lecture 19: Self Harm & Suicide
Independent learning
Group Discussion
Break and student project
Plenary session
SP Group A1, A2, A3
Lecture 20: Child Abuse &
Neglected
Independent learning
Group Discussion
Break and student project
Plenary session
SP Group A4, A5, A6
Clinical Skill: Introduction to
Psychiatric Interview
Independent learning
Group Discussion
Break and student project
Plenary session
SP Group A7, A8, A9, A10
Clinical Skill: Interview with
Anxiety Disorders Patients
Class room
Discussion room
Class room
22
Thursday
11 June
2015
23
Friday
12 June
2015
24
Monday
15 June
2015
25
Tuesday
16 June
2015
Wed
17 June
2015
26
Thursday
18 June
2015
08.00 – 15.00 Clinical Skill: Interview with
Depression Disorders Patients
08.00 – 15.00 Clinical Skill: Interview with
Somatoform Disorders Patients
08.00 – 15.00 Clinical Skill: Interview with
Bipolar Disorders Patients
Skill Lab
Skill Lab
Skill Lab
Skill Lab
Pre-evaluation Break
Examination
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Artini
Dr Artini
Dr Dayu
Dr Dayu
Dr Sri Wahyuni
Dr Sri Wahyuni
Dr Sri Wahyuni
Dr Sri Wahyuni
Team Psychiatry
Team Psychiatry
Team Psychiatry
Team Psychiatry
Udayana University Faculty of Medicine, DME 8
Study Guide Behavior Changes and Disorders
English Class
Day/
Date
Time
1
Friday
8 May
2015
2
Monday
11 May
2015
3
Tuesday
12 May
2015
4
Wed
13 May
2015
5
Monday
18 May
2015
6
Tuesday
19 May
2015
7
Wed
20 May
2015
8
Thursday
21 May
2015
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
Activity
Lecture 1: Introduction to Behavior
Changes and Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 2: Mental Status
Examination and Assessment
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 3: Psychological Test
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 4: Neurobehavioral approach to Behavior Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 5: Prenatal Psychobiology
(Case of Baby Blues)
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 6: Behavior Changes Due to a General Medical Condition
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 7: Delirium and Dementia
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 8 : General Approaches to
Substance Abuse
Student project & break
Independent learning
Group Discussion
Plenary session
Venue Conveyer
Class room
Discussion room
Class room
Dr Sri Wahyuni
Dr Sri Wahyuni
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Sr Diniari
Dr Sri Diniari
DR Wulanyani
DR Wulanyani
DR Dr Laksmi
DR Dr Laksmi
DR Dr IB Fajar
DR Dr IB Fajar
Dr Yenni
Dr Yenni
Dr Endah
Dr Endah
Dr Westa
Dr Westa
Udayana University Faculty of Medicine, DME 9
Study Guide Behavior Changes and Disorders
15
Monday
1 June
2015
16
Wed
3 June
2015
9
Friday
22 May
2015
10
Monday
25 May
2015
11
Tuesday
26 May
2015
12
Wed
27 May
2015
13
Thursday
28 May
2015
14
Friday
29 May
2015
17
Thursday
4 June
2015
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
Lecture 9 : Primary & Secondary
Insomnia
Student project & break
Independent learning
Group Discussion
Plenary session
Lecturer 10: Schizophrenia & Other
Psychosis
Student project & break
Independent learning
Group Discussion
Plenary session
Lecturer 11: Delusional &
Schizoaffective Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 12: Bipolar Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 13: Panic Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 14: Somatoform Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 15: Generalized Anxiety &
Obsessive-Compulsive Disorder
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 16: PTSD
Student project & break
Independent learning
Group Discussion
Plenary session
Lecture 17: Sexual Disorders
Student project & break
Independent learning
Group Discussion
Plenary session
Class room
Discussion room
Class room
Dr Alit Aryani
Dr Alit Aryani
Class room
Discussion room
Class room
DR Dr Cok Bagus
DR Dr Cok Bagus
Class room
Discussion room
Class room
Dr Sri Diniari
Dr Sri Diniari
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Lely
Dr Lely
Dr Indah
Dr Indah
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Indah
Dr Indah
Dr Putri
Dr Putri
DR Dr Cok Bagus
DR Dr Cok Bagus
Dr Westa
Dr Westa
Udayana University Faculty of Medicine, DME 10
Study Guide Behavior Changes and Disorders
18
Friday
5 June
2015
19
Monday
8 June
2015
20
Tuesday
9 June
2015
21
Wed
10 June
2015
22
Thursday
11 June
2015
23
Friday
12 June
2015
24
Monday
15 June
2015
25
Tuesday
16 June
2015
Wed
17 June
2015
26
Thursday
18 June
2015
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
08.00 – 11.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 10.00
10.00 – 12.00
12.00 – 13.30
13.30 – 15.00
15.00 – 16.00
09.00 – 16.00
Lecture 18: Psycho-Pharmacology
Student project & break
Independent learning
Group Discussion
Plenary session
SP Group B10, B9, B8
Lecture 19: Self-Harm & Suicide
Student project & break
Independent learning
Group Discussion
Plenary session
SP Group B7, B6, B5
Lecture 20: Child Abuse &
Neglected
Student project & break
Independent learning
Group Discussion
Plenary session
SP Group B4, B3, B2, B1
Clinical Skill: Introduction to
Psychiatric Interview
Break
Independent learning
Group Discussion
Plenary session
Clinical Skill: Interview with Anxiety
Disorders Patients
09.00 – 16.00 Clinical Skill: Interview with
Depression Disorders Patients
09.00 – 16.00 Clinical Skill: Interview with
Somatoform Disorders Patients
09.00 – 16.00 Clinical Skill: Interview with Bipolar
Disorders Patients
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Class room
Discussion room
Class room
Dr Artini
Dr Artini
Dr Dayu
Dr Dayu
Dr Sri Wahyuni
Dr Sri Wahyuni
Class room
Discussion room
Class room
Dr Sri Wahyuni
Dr Sri Wahyuni
Examination
Skill Lab
Skill Lab
Skill Lab
Skill Lab
Pre-evaluation Break
Psychiatric Team
Psychiatric Team
Psychiatric Team
Psychiatric Team
Udayana University Faculty of Medicine, DME 11
Study Guide Behavior Changes and Disorders
Student’s Project
Every student requires finding a scientific journal based on the topic of their groups and create a review paper as a group project. The journal has to be from year 2013 to recent years. It has to be present in a report format by week 4 th to the facilitator and present in the plenary session.
No Topic Group
1 Paranoid Personality Disorder
2 Schizoid Personality Disorder
3 Schizotypal Personality Disorder
4 Antisocial Personality Disorder
5 Borderline Personality Disorder
6 Histrionic Personality Disorder
7 Narcissistic Personality Disorder
8 Avoidant Personality Disorder
9 Dependent Personality Disorder
10 Obsessive –Compulsive Personality Disorder
Report Format
Cover
Preface
Table of Content a. Introduction b. Content c. Discusion
A1, B10
A2, B9
A3, B8
A4, B7
A5, B6
A6, B5
A7, B4
A8, B3
A9, B2
A10, B1 d. Summary
Space
Font
: 1,5 Space
: Times New Roman 12
Minimum Page: 15
The student ’s project is present starting by the 18 th day of the meeting on the plenary meeting. The results will be review by the block planning group for final mark.
Udayana University Faculty of Medicine, DME 12
Study Guide Behavior Changes and Disorders
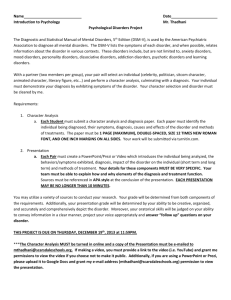
Student Project Assessment Form
Faculty of Medicine, Udayana University
Blok : Behavior Changes and Disorders
Name/NIM :
Facilitator
Title
:
:
Time Table of Consultation
Point of Discussion Week Date
Title 1
Tutor Sign
Translation of Journal 2
Discussion and
Summary of Journal
3
Final Report
Assessment
A. Paper structure
B. Content
C. Discussion
Total Point
Denpasar,
Facilitator
4
:
:
:
:
6
6
6
7
7
7
(A+B+C)/4
8
8
8
9
9
9
10
10
10
= __________
Udayana University Faculty of Medicine, DME 13
Study Guide Behavior Changes and Disorders
Meeting of Student Representatives and Facilitators
Meeting of student representatives and facilitators will be held on the second Friday of the block period if necessary .
This meeting will be organized by the planners and attended by lecturers, students group representatives and all facilitators. Meeting with the student representatives will take place at 09.00 until 10.00 am and meeting with the facilitators at
10.00 until 11.00 am . The purpose of the meeting is to evaluate the teaching learning process of the Block. Feedbacks and suggestions are welcome for improvement of the
Block educational programs.
~ ASSESSMENT METHOD ~
Assessment will be carried out on the 26 th day of the block period. The test will consist of
100 questions with 100 minutes provided for working. The assessment will be held at the same time for both Regular Class and English Class. The passing score requirement is
70 . More detailed information or any changes that may be needed will be acknowledged at least two days before the assessment.
Udayana University Faculty of Medicine, DME 14
Study Guide Behavior Changes and Disorders
Modul
1
Introduction to Behavior and Disorders
dr Anak Ayu Sri Wahyuni, SpKJ
AIMS:
Emphasizes clinical psychiatry and its development in Indonesia and in the world
Describe Mental Health Act in Indonesia, Manual of Indonesian Mental Disorders and multi axial diagnosis
LEARNING OUTCOMES:
Describe how to:
1. Emphasizes clinical psychiatry
2. Describe history of psychiatry
3. Understand the manual of Indonesian Mental Disorders
4. Use multi axial Diagnosis
CURRICULUM CONTENTS:
1. Psychiatric definition
2. Negative stigma of mental disorders
3. Development of psychiatric intervention
4. Diagnosis formulation
5. Global Assessment Function Scale
ABSTRACTS
The purpose of this lecture is to give general information about all of the subjects that will be given in this Block. It also creates awareness on how importance the subjects in the medical education and future medical profession.
This is an exciting time in the field of psychiatry. Scientificprogress has expanded the diagnostic and therapeutic capabilities of psychiatry at the same time that psychiatry has begun to play a larger role in the delivery of care to a wider population, both in mental health and in primary care settings. Psychiatry at the end of the 20th century plays an important role among the medical specialties.
The physician –patient relationship provides the framework for quality psychiatric practice. The skilled clinician must acquire a breadth and depth of knowledge and skills in the conduct of the clinical interaction with the patient. To succeed in this relationship, the psychiatristmust have an understanding of normal developmental processes across the life cycle (physiological, psychological, and social) and how these processes are manifested in behavior and mental functions. The psychiatrist must also be expert in the identification and evaluation of the signs and symptoms of abnormal behavior and mental processes and be able to classify them among the defined clinical syndromes that constitute the psychiatric nosology.
To arrive at a meaningful clinical assessment, one must understand the etiology and pathophysiology of the illness along with the contributions of the patient’s individual environmental and sociocultural experiences. Furthermore, the psychiatrist must have a command of the range of therapeutic options for any given condition, including comparative benefits and risks, andmustweigh the special factors that can influence the course of treatment such as medical comorbidity and constitutional, sociocultural, and situational factors.
Udayana University Faculty of Medicine, DME 15
Study Guide Behavior Changes and Disorders
Psychiatry today, the transformation of our field has gained increasing momentum.
Our understanding of the microstructure and function of the brain, and of the genetic controls of the brain reveals ever more amazing information which has already begun to transform clinical practice and psychiatric education. Further, the changes in the ways we have access to information have led to dramatic improvement of accessibility to our growing knowledge base. Yet, the clinical core of our discipline remains the imperative to integrate the best of our humanistic traditions with our cutting-edge scientific advances. With all the revising and restructuring though, our approach continues to emphasize an integrative biopsychosocial philosophy in both understanding psychopathology and providing treatment. And, as always, we hold to the view that the context of our understanding and intervention remains the therapeutic alliance we develop and maintain with our patients.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. Psychiatric definition
2. Negative stigma of mental disorders
3. Development of psychiatric intervention
4. Diagnosis formulation
5. Global Assessment Function Scale
SCENARIO
Since the 1980s, new technologies and fundamental new insights have transformed the biological sciences and most areas of medicine. The completion of the Human Genome
Project in 2002 provided a map of all of the genes of the human species. The soon-to-becompleted human haplotype map will provide a guide to individual variation of all of these genes. Along with genomics, neuroscience has become one of the most exciting areas of contemporary research. Recent discoveries have transformed the understanding of the brain, demonstrating how neurogenesis continues throughout adulthood, mapping the dynamic nature of cortical connectivity that can change in response to stimulation, and identifying some of the categorical rules by which information is processed in the brain. By any measure, recent decades have been revolutionary for the understanding of the human genome and how the brain functions, two areas of science fundamental to psychiatry. Yet, during this same period, clinical psychiatry has remained relatively unchanged.
Learning Task
1. Explain about psychiatric diagnostic terst
2. What are the major disorders in behavioral changes?
3. Discuss about genomic and neuroimaging progress in how clinicians diagnose or treat the patients with mental disorders
4. Explain about the latest finding in DNA for major disorders in behavioral changes
SCENARIO 2:
A psychiatric consultant was asked to see a 48-year-old man on a coronary care unit for chest pain deemed “functional” by the cardiologist who had asked the patient if his chest pain was “crushing.” The patient said no. A variety of other routine tests were also negative.
The psychiatrist asked the patient to describe his pain. He said, “It’s like a truck sitting on my chest, squeezing it down.” The psychiatrist promptly recommended additional tests that confirmed the diagnosis of myocardial infarction. The cardiologist may have been tempted to label the patient a “bad historian”.
Learning Task
1. Expalin about the key skill in psychiatry?
2. What are the different between listening and hearing?
3. What are the trends in psychiatric care?
Udayana University Faculty of Medicine, DME 16
Study Guide Behavior Changes and Disorders
4. Explain about the most important tool for healing?
5. How do you act as a primary care doctor to create a process of destigmatization?
Self Assessment
1. How to do a good anamnesis for a patient and his family?
2. Can the drug given by cardiologist and by psychiatrist be given simultaneously?
3. Try to assess using Multi Axial diagnosis (Axis I, II, III, IV and V)?
4. What is the main priority in handling the case above?
5. We recognize there is still a negative stigma about mental illness in society. How to overcome this?
Udayana University Faculty of Medicine, DME 17
Study Guide Behavior Changes and Disorders
Modul
2
Mental Status Examination and Assessment
dr Ni Ketut Sri Diniari, SpKJ
AIMS:
Know mental status examination, and multiaxial diagnostic
LEARNING OUTCOME:
Can describe the:
1. Mental status examination
2. The diagnostic classification system used in psychiatry
3. Multiaksial diagnostic
CURRCIULUM CONTENS:
1. Mental status examination
2. Sign and symptom in mental status examination
3. The diagnostic classification system used in psychiatry
4. Multiaksial diagnostic
ABSTRACTS:
Establishing rapport and a good therapeutic alliance with patients is critical to both their diagnosis and their treatment. The psychiatric assessment is different from a medical or surgical assessment in that: (1).The history taking is often longer and is aimed at understanding psychological poblems that develop in patients, each with a unique background and social environment; (2). A mental status examination is performed; and (3).
The assessment can in itself therapeutic.
The mental status examination comprises the sum total of the physician’s observations of the patient at the time of the interview. Of note is that this examination can change from hour to hour, whereas the patient’s history remains stable. The mental status examination includ es impressions of the patient’s general appearance, speech, mood, affect, thought process, thought content, sensorium, cognition, impuls control, insight, and judgment.. Even a mute or uncooperative patient reveals a large amount of clinical information during the mental status examination.
A diagnosis is made by careful evaluation of the database, analysis of the information, assessment of the risk factors, and development of a list of possibilities (the differential diagnosis). There are two main categorical classification system diagnostic in psychiatry: ICD-10 and DSM-IV. In Indonesia, we use PPDGJ-III (Pedoman Penggolongan dan Diagnosis Gangguan Jiwa-III) that uses a referral from DSM-IV. DSM-IV uses a multiaxial diagnostic with five axis. Axis I: includes all mental disorder that can be the focus of clinical attention such as schizophrenia, major depression, etc. Axis II: personality disorders and mental retardation. Axis III: physical disorders and other general medical conditions. Axis IV: includes any social or environmental problems that contribute to the mental condition. Axis V consists of a score from 0 to 100, obtained from a global assessment of functioning (GAF) sale.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. How to establishing raport ( therapeutic alliance)
2. The procedure of psyciatric interview and mental status examination
3. Sign and symptom in mental status examination
4. Able to make diagnostic multiaksial
Udayana University Faculty of Medicine, DME 18
Study Guide Behavior Changes and Disorders
SCENARIO
A 30-year-old married woman suffers from chronic low mood and lack of enjoyment of life.
She is highly dependent on her husband for practical and emotional support, although she frequently flies into rages at him, feeling that he is cold and uncaring. She has had a series of secretarial jobs which she begins enthusiastically, but soon comes to feel that her employers are highly critical and belittling, whereupon she resigns. Her friendships are limited to people with whom she can have very special, exclusive relationships. She deals poorly with change or loss, which frequently triggers episodes of acute dysfunction. When a friend is not sufficiently available to her, she feels betrayed and worthless, her mood plummets, she becomes lethargic, has eating binges, and is unable to work or pursue her usual routine for up to weeks at a time.
Learning task a. Does the patient have a psychiatric disorders? b. How severe is the illness? c. What is the diagnosis? d. What is the patient base line level of functioning? e. What the environment, biological and psychological factors contribute to the disorders?
SCENARIO 2
A 26-year-old man presented to the emergency department seeking a safe haven from “the mob.” He was convinced that he was being set up to be killed, as evidenced by the sequence of license plate numbers of the cars that had passed him on the way to work. He had initially gone to a police station, which had referred him to the hospital.
Learning task a. Please try to identifying the symptoms of the patient above! b. How to make first oriented intervention as psychiatric interview in the patient above? c. How to make therapeutic alliance with the patient above?
Self Assessment
1. Can you explain the signs and symptoms of psychotic disorders?
2. Can you explain the signs and symptoms of depression disorder?
3. Can you explain the signs and symptoms of anxiety disorder?
4. If a patient listening to the sounds in the ear there are people who threatened him, but other people do not hear, what is the name of this symptom?
5. What is put in the axis of the underlying psychosocial stressors problem of mental disorder?
Udayana University Faculty of Medicine, DME 19
Study Guide Behavior Changes and Disorders
Modul
3
Psychological Testing
DR. Ni Made Swasti Wulanyani, S.Psi., M.Erg., Psi
•
•
AIMS:
• To understand some of the fundamental principles underlying psychological testing
To understand types of psychological testing that patients needed
To acquaint with some of the important ethical issues relating to psychological testin.
LEARNING OUTCOMES:
Student will know how to describe:
1. the application of psychological testing
2. types of settings are assessments conducted
3. appropriate psychological testing for patients problems
CURRICULUM CONTENTS:
1. Psychological testing definition
2. The function of psychological testing
3. Assessment Setting
4. Types of psychological testing
5. Standardization
6. Ethics to conduct and report
ABSTRACTS:
The purpose of this lecture is to give general knowledge about psychological testing that could use to have complete information about human behavior. After learning this topic, students could analyze the needed of psychological approach of patients and chose the appropriate types of tests. Ethical issues also build understanding about the legal procedure to conduct psychological test, so that the result will keep valid.
SELF DIRECTED LEARNING:
Basic knowledge that must be known:
1. Psychological testing definition
2. The function of psychological testing
3. Assessment Setting
4. Types of psychological testing
5. Standardization
6. Ethics to conduct and report
SCENARIO:
An employee gets a promotion to a higher position in another unit in the company. A month later, the employee becomes ill, showed decreased in performance and withdrawn from social relationship
Learning Task: Please discuss!
1. Any psychological tests that can be given and the reason!
SCENARIO
A young boy has just become student in a Vocational High School (Sekolah Menengah
Kejuruan). At the end of the first semester, he got very bad marks, whereas he has shown good academic achievement while attending junior high school (SMP) before. He was frequently absent because of illness. No responses come from the parents although the
Udayana University Faculty of Medicine, DME 20
Study Guide Behavior Changes and Disorders school has sent an invitation letter to discuss their son’s problems. The boy is often punished at school because of bullying his friends.
Learning Task
What is the likelihood that the child experienced?
What would you do?
SCENARIO
A child cannot write even though she is in 3rd grade of elementary school now. When she was a toddler, she was not able to mimic the circle and other simple images.
Learning Task
Explain your suspicions to this case and what would you do?
SCENARIO
A unit at Education al institution, named “Berjaya”, provides psychological testing services for many settings such as educational, business, counseling. Most of unit member are not psychologists. Most of them are school counselor. They use computerized method for scoring.
Learning Task
Explain your analysis about ethical issues that must be consider by the unit or institution
Self Assessments:
Explain each of the following terms:
1. assessment
2. Intelligence test
3. Diagnostic
4. accommodation
5. Test user
6. Test developer
7. Test taker
8. Standardized test
9. Confidentiality
10. Responsibility or psychological tester
Udayana University Faculty of Medicine, DME 21
Study Guide Behavior Changes and Disorders
Modul
4
Neurobehavioral approach to Behavior Disorders
Dr dr Anak Agung Ayu Putri Laksmidewi Sp.S(K)
AIMS:
Student will be expected to know and understand the neurological basis of behavior, memory, and cognition, the impact of neurological damage and disease upon behavior disorders.
LEARNING OUTCOMES:
Student will be able to describe:
1. How neurobehavior theories develop
2. Approaches to neurobehavior
3. Types of psychological phenomena in patients with brain disease
CURRICULUM CONTENTS:
1. What is neurobehavior
2. Introduction Approaches to neurobehavior
3. Focal neurobehavioral syndromes
ABSTRACTS:
The nervous system is anatomically and functionally divided into central and peripheral subsystems. The central nervous system (CNS) includes the brain and spinal cord, and
CNS dysfunction can be subdivided into two general categories, neurobehavioral and motor/sensory. Neurobehavioral difficulties involve two primary categories: cognitive decline, including memory problems and dementia; and neuropsychiatric disorders, including neurasthenia (a collection of symptoms including difficulty concentrating, headache, insomnia, and fatigue), depression, posttraumatic stress disorder (PTSD), and suicide. Other CNS problems can be associated with motor difficulties, characterized by problems such as weakness, tremors, involuntary movements, incoordination, and gait/walking abnormalities. These are usually associated with subcortical or cerebellar system dysfunction. The anatomic elements of the peripheral nervous system (PNS) include the spinal rootlets that exit the spinal cord, the brachial and lumbar plexus, and the peripheral nerves that innervate the muscles of the body. PNS dysfunctions, involving either the somatic nerves or the autonomic system, are known as neuropathies.
Neurologic dysfunction can be further classified as either global or focal. For example, in neurobehavioral disorders, global dysfunction can involve altered levels of consciousness or agitated behavior, whereas focal changes give rise to isolated signs of cortical dysfunction such as aphasia or apraxia.
SELF DIRECTED LEARNING:
Students need to explore more theories of neurobehavior:
1. Neurobehavior approach to behavior disorders
2. Research in neurobehavior
3. Laboratory investigation in neurobehavior
SCENARIO:
A 20 years old woman complains of behavior disorder. From herrelatives, this woman do not want to communicate each other from 2 weeks ago. She also didn’t want to take a bath, do not want to eat and to make and interaction between her peer groups nor her realtives.
Regarding to her father, this patient often talk by her self, and often complain of hearing
Udayana University Faculty of Medicine, DME 22
Study Guide Behavior Changes and Disorders voices that only heard by herself. No previous evidence of fever or head injury before the onset of those features.
Learning task:
1. What is the properly list of question that need to be asked from the patient and her relatives?
2. What is the etiology of this case in general?
3. Please explain the neurophatogenesis of this case!
Case 2:
A 52-year-old female is admitted to a medical ward with an acute exacerbation of Crohn’s disease, requiring high-dose steroids and intensive emergency treatment. After a few days, however, she accuses the nurses on the ward of stealing her money and believes that one of the male nurses assaulted her during the night. However, once her steroids are stopped, she starts to settle and no longer voices any bizarre ideations..
Learning task:
1. What is the properly list of question that need to be asked from the patient and her relatives?
2. What is the differential diagnosis of this patient?
3. Please explain the neurophatogenesis from each of the differential diagnosis that has been mentioned above!
Case 3:
A 68-year-old male is admitted under the medical team for dehydration after refusing to eat or drink. His wife reports that he has been preoccupied with the belief that he has a brain tumour and has lost pleasure in everything. He has lost 12 kg in weight and spends most of his day in bed. He reports that he can smell rotting bodies and believes that he has committed a sinful crime because he has heard voices calling him a paedophile. He feels ashamed of himself.
Learning task:
1. What is the properly list of question that need to be asked from the patient and her relatives?
2. What is the proper psychotherapy planned for this patient?
Case 4:
A 40 years old man comes to private service with difficulty to fall a sleep since 5 days ago.
He usually abruptly wake up on midnight while sleeping, hence he didn’t feel well while waking up on the following morning.
Learning task:
1. What is the properly list of question that need to be asked from the patient and her relatives?
2. What kind of questionnaire proper to be applied to assess type of sleeping disorder in this patient?
Udayana University Faculty of Medicine, DME 23
Study Guide Behavior Changes and Disorders
Modul
5
Prenatal Psychobiology (Case of Baby Blues)
Dr dr Ida Bagus Fajar Manuaba, SpOG, MARS
AIMS:
Describe the clinical management of baby blues (Anamnesis, History taking, Mental State
Examination, Diagnosis, and Therapy).
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of baby blues and postpartum depression
3. Mental state examination of baby blues and postpartum depression
4. Diagnosis formulation
5. Modality of treatment of baby blues and postpartum depression
ABSTRACTS
Prenatal psychology is an interdisciplinary study of the foundations of health in body, mind, emotions and in enduring response patterns to life. It explores the psychological and psychophysiological effects and implications of the earliest experiences of the individual, before birth ("prenatal"), as well as during and immediately after childbirth ("perinatal") on the health and learning ability of the individual and on their relationships. As a broad field it has developed a variety of curative and preventive interventions for the unborn, at childbirth, for the newborn, infants and adults who are adversely affected by early prenatal and perinatal dysfunction and trauma. Some of these methods have not been without significant controversy, for example homebirth in the West and in earlier days, LSD psychotherapy for resolving birth trauma.
The relevance of birth experiences has been recognized since the early days of modern psychology. Although Sigmund Freud touched on the idea briefly before rejecting it in favor of the Oedipus complex, one of his disciples Otto Rank became convinced of the importance of birth trauma in causing anxiety neuroses. Rank developed a process of psychoanalysis based on birth experiences, and authored his seminal work, 'The Trauma of
Birth'. Freud's initial agreement and then later volte-face caused a rift between them, which relegated the study of birth trauma to the fringes of psychology. The transcendental and human aspects of awareness documented from the beginning of life became the core thread in this holonomic holographic model.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing the earliest experiences of the individual, before birth
("prenatal"), as well as during and immediately after childbirth ("perinatal").
2. Formulating diagnosis for baby blues and postpartum depression.
3. Management of baby blues and postpartum depression.
Udayana University Faculty of Medicine, DME 24
Study Guide Behavior Changes and Disorders
1.
2.
3.
4.
5.
SCENARIO
Mary is a 32-year-old married nurse with a history of panic attacks that have been well controlled for years. She presents 3 months postpartum, following a difficult pregnancy complicated by severe hyperemesis gravidarum and dysphoria in addition to traumatic delivery with a third-degree perineal tear. Mary now complains of crying spells, decreased appetite, insomnia, and obsessive worry over the baby’s health. She feels isolated from her husband, who is overwhelmed by her emotional needs and tends to retreat to work.
Learning Task:
What are the diagnostic features of this patient?
How long is the onset of illness on this kind of patient?
What is the diagnosed according to DSM-V?
Make a systematic screening for the risk factors in addition to current symptoms
Explain the differential diagnosis of the above case?
6.
7.
8.
3.
What therapy should be given?
What is the difference between baby blues and postpartum depression?
When reviewing the prognosis for people with baby blues, what kind of onset, gender, and duration suggest a more favorable outcome?
9. Discuss about the possibility when people like above case never get any treatment!
10. Discuss about any prevention work that possible for the relapse of the above case!
Self-Assessment:
1.
2.
Explain the understanding of reality testing for baby blues!
Explain the difference between baby blues, postpartum depression with Postpartum
Psychosis!
Explain one of the most widely used instruments to assess for postpartum
4.
5. depressive symptomatology is the Edinburgh Postnatal Depression Scale (EPDS)!
Read the book title The Secret Life of the Unborn Child.
Fiind current research on Welcoming Consciousness
Udayana University Faculty of Medicine, DME 25
Study Guide Behavior Changes and Disorders
Modul
6
Behavior Changes Due to a General Medical Condition
dr. Yenni Kandarini, SpPD
AIMS:
Describe the clinical management of Behavior Changes Due to a General Medical Condition
(Anamnesis, History taking, Mental State Examination, Diagnosis, and Therapy).
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of Behavior Changes Due to a
General Medical Condition
3. Mental state examination of Behavior Changes Due to a General Medical Condition
4. Diagnosis formulation
5. Modality of treatment of Behavior Changes Due to a General Medical Condition
ABSTRACTS
Psychiatric disorders are frequently under- and overdiagnosed in the medically ill for a number of reasons. First, psychiatric symptoms are similar to those of medical illness. As a result, it may be problematic to determine whether such symptoms are manifestations of a physical disease or a comorbid psychiatric disorder. For example, a false-positive diagnosis of depression may occur when fatigue, anorexia, and weight loss caused by amedical illness are mistakenly attributed to depression, and a false-negative diagnosis when depression’s vegetative symptoms are misattributed to the medical illness. A variety of approaches have been proposed to diminish the effect of medical symptoms confounding the diagnosis of depression. In an “exclusive” and “etiologic” approach, symptoms that are judged by the clinician to be etiologically related to a general medical condition are excluded from the diagnostic criteria for major depressive disorder (MDD). However, how to determine which symptoms are due to a medical illness, and which are due to depression, is unclear. In a “substitutive” approach, symptoms most likely confused with medical illness, such as fatigue and weight loss, are substituted with symptoms that are more likely to be affective in origin, such as irritability and social withdrawal. Such substitution eliminates the need to distinguish symptoms of medical illness from those of depression, but it also excludes some somatic symptoms that are core manifestations of depression. Furthermore, valid criteria to determine which symptoms should be substituted have not been established. An “inclusive” approach applies the unmodified
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of treatment to Behavior Changes Due to a General Medical condition
2. Formulating diagnosis for Behavior Changes Due to a General Medical Condition.
3. Management of Behavior Changes Due to a General Medical Condition.
Udayana University Faculty of Medicine, DME 26
Study Guide Behavior Changes and Disorders
Modul
7
Delirium and Dementia
dr. I Gusti Ayu Endah Arjana, Sp.KJ (K)
AIMS:
Describe the clinical management of delirium syndromes dementia (History, General
Medical and Neurologic Examination, Mental Status examination, Laboratory Studies,
Imaging, and Other Diagnostic Tests, Diagnostic criteria, Management)
LEARNING OUTCOMES:
Describe how to:
1. Definition and Diagnostic Features
2.
3.
Common Associated Features
Predisposing Factors
4.
5.
Selected Causes of Delirium and Dementia
Management: general Principles (Behavioral Interventions, Pharmacologic
Interventions, physical restraints)
CURRICULUM CONTENTS:
1. History taking of delirium and dementia
2.
3.
4.
5.
Physical examination of delirium and dementia
Mental examination of delirium and dementia
Investigation routine
Management (four main principles of management)
ABSTRACTS
Delirium is characterized by acute generalized psychological dysfunction that usually fluctuation in degree. Clinical features of delirium, prodromal symptoms include: perplexity, agitation, hypersensitivity to light and sound.
A stereotyped response of the brain to a variety of insults is very commonly seen in hospital inpatients. It is a clinical syndrome of fluctuating global cognitive impairment associated with behavioural abnormalities. Like other acute organ failures it is more common in those with chronic impairment of that organ.
The clinical management of delirium consists of how to make a proper diagnosis through good anamnesis, physical and mental examination, aetiologi, management four main principles.
SELF DIRECTING LEARNING
Basic knowledge that must be know:
1. The prosedure of delirium and dementia diagnosis
2.
3.
SCENARIO
Management of delirium and dementia
Assessment of delirium and dementia.
A 64-year-old woman admitted to the medical ward with an acute exacerbation of chronic obstructive pulmonary disease. She lived alone following the death of her husband 3 years earlier. Her normal medication was low-dose prednisolone, bronchodilators in inhalers, antihypertensives and ranitidine which were all continued. She was hypoxic on admission and treated with oxygen therapy. All her blood tests were normal apart from a raised Creactive protein. On the chest radiograph, there was a right basilar shadow and she was started on ciprofloxacin for a presumed infection.
After 3 days, Mrs A became progressively depressed, inhibited and non-compliant with therapy and routine interventions. She was assessed and referred to a psychiatrist for
Udayana University Faculty of Medicine, DME 27
Study Guide Behavior Changes and Disorders
‘depression impairing co-operation and compliance’. On mental status examination she appeared extremely inhibited and apathetic with decreased reaction to stimuli. She had a reduced ability to maintain attention, shortterm memory impairment and mild perception disturbances. There was a history of sleep/wake disturbance from the nursing notes.
According to her son, she had no cognitive problems before her admission.
Learning Task:
1. From the story above, what need to be asking to the patient?
2. Make the physical and mental examination of this patient.
3. What is the differential diagnosis of this patient?
4. What is the planning diagnosis, that you suggest?
5. What the treatment of this patient?
SCENARIO
A 73-year-old female presents with increasing confusion, lethargy, and disorientation. On examination, she is obese and has a distinctive deep voice. Her pulse is 40 and blood pressure is 110/72. She complains of constipation.
Learning Task:
1. From the story above, what need to be asking to the patient?
2. Make the physical and mental examination of this patient.
3. What is the differential diagnosis of this patient?
4. What is the planning diagnosis, that you suggest?
5. What the treatment of this patient?
SCENARIO
A 72-year-old male has been experiencing attacks of confusion, memory problems, and visual hallucinations over the last year. Each episode lasts for a few weeks and he is fine between these episodes; however, with subsequent episodes, his condition seems to be getting worse. His medical history shows blood pressure of 150/101 and he has had transient ischaemic attacks in the past. On examination there is an upgoing plantar.
Learning Task:
1. From the story above, what need to be asking to the patient?
2. Make the physical and mental examination of this patient.
3. What is the differential diagnosis of this patient?
4. What is the planning diagnosis, that you suggest?
5. What the treatment of this patient?
Self assessment;
1. How to do a good anamnesis in delirium and dementia cases?
2. How to do a good Mental and Physical examination?
3. What is the laboratory findings that need to be checked in delirium and dementia cases.
4. What is the etiology of delirium and dementia cases in general.
5. What is management of delirium and dementia cases.
Udayana University Faculty of Medicine, DME 28
Study Guide Behavior Changes and Disorders
Modul
8
General Approaches to Substance Abuse
dr. Wayan Westa, SpKJ (K)
AIMS:
Emphasizing on understanding the effects of substance abuse on physical health, mental, social
Understanding the follow-up of treatment of individuals with intoxication and withdrawal
LEARNING OUTCOMES:
1. Understand psychodynamic substance abuse problems
2. Understand the types of drugs in general
3. Understanding the symptoms of individuals with object withdrawal of drug poisoning
4. Understand the initial handling of the state of withdrawal, substance intoxication is then able to make a referral
CURRICULUM CONTENTS:
1. The definition of substance abuse, tolerance, dependence, craving
2. Understand the role of genetic, family roles, psycho-social stress associated with substance abuse
3. Understanding of the symptoms of the individual in a state of withdrawal and intoxication from drugs
4. Being able to make a diagnosis and early treatment and refer the individual to a state of withdrawal or drug intoxication
ABSTRACTS
Drug abuse or Narcotics, Alcohol, Psychotropic and Other Addictive Substances today continues to increase, and the alarming situation. Drug abuse is not only the case for those who are classified as unemployed but has been extended to adolescents with status as students, civil servants, officials, law enforcement and so on. This problem can not be separated from the influence of globalization, information technology, and faster transportation.
The flurry of parents, at least the time to pay attention, affection for the children, as well as family life is not harmonious, promiscuity outside and easy to obtain substances / drugs, especially narcotics would plunge the individual to a substance abuse problem and continues to dependence. Once the individual involved substance abuse dependency became very difficult to be normal again. The study says that only 10% of individuals dependence can be restored to normal. In undergoing the process of this dependence individual will feel the pain and suffering at the time of experience: the state of withdrawal, intoxication, craving or they are undergoing legal proceedings and sent to prison. A general practitioner should be able to provide aid / early treatment to individuals with a state of withdrawal, drug toxicity and referring to the hospital. Besides general practitioners are expected to provide outreach to the community about the dangers of drugs so that people can avoid drug abuse.
SELF DIRECTING LEARNING
Basic knowledge that must be know:
1. Understand psychodynamic substance abuse
2. Understand the types of drugs in general
3. Understanding the symptoms of the individual to the state of withdrawal, drug substance intoxication
4. Handle the initial handling of state withdrawal of drug substance intoxication and was able to make a referral
Udayana University Faculty of Medicine, DME 29
Study Guide Behavior Changes and Disorders
SCENARIO
A man aged 25 years unemployment driven by his friend to the hospital with complaints; fever, snot and tears, pain throughout the body, the hair on the body seemed to stand, also appears there is a pimple like the cold. This patient also complained of nausea and want to vomit. On physical examination found blood pressure 130/80, rather rapid respiration, pulse
96x / min, body temperature 37,80C. Medriasis pupils, reflex + / +. In the interview the patient obtained have been using substances / drugs, beginning with suction means further by means of a syringe. Patients taking these substances last was two days ago.
LEARNING TASK
1. In the above situation is the patient? Explain!
2. The substance / drug if the patient used before?
3. Describe how the psychodynamic process so people above fall into substance abuse and addiction / drug!
4. As a general practitioner, what treatment is given?
5. What are the dangers of injecting drug use?
6. What our efforts together so that drug abuse can be reduced?
SCENARIO 2
A man aged 40 years, a large body of high body tattooed, work as a guard café. Came to the hospital escorted by his friend and guarded by police, handcuffed her hands as it can go berserk and fight with visitors café. After soothed then conducted an interview, explaining that drinking ALCOHOL patients have long done and once in a while to get drunk. In times of strife and fighting in th e café, before he admitted taking ALCOHOL. Furthermore, he felt himself strong, selfconfidence increased, bold, look like smallish café visitors so easily defeated. When it peaked emotional, touchy, angry that a fight. Physical examination was normal. Physical illness previously denied.
LEARNING TASK
1. Under no circumstances does the male cases mentioned above? Explain!
2. What are consumed by men of the above? Explain!
3. Individuals who are used to the routine of drinking MIRAS suddenly stop taking
MIRAS what happens? What was the symptoms?
4. What are the dangers of alcoholic liquor to the physical condition, or mental?
Explain!
5. There is argued that the use of alcoholic beverages (MIRAS) is more dangerous than smoking heroin (heroin). Why? Explain!
6. As a general practitioner what actions and help you when dealing with cases of alcohol withdrawal?
SELF ASSESSMENT
1. Explain what is included drug / drug!
2. Any Drug / Drug including stimulants and sedatives which euphoria?
3. Explain the notion of amphetamine psychosis, Delerium Tremens (DT's), Psychosis
Korchakoff!
4. Why is the use of injectable opiate more dangerous than the opiates suction?
5. The method of treatment in opiate withdrawal, how wide? Explain!
6. Individuals with an overdose of heroin what treatment? Explain!
Udayana University Faculty of Medicine, DME 30
Study Guide Behavior Changes and Disorders
Modul
9
Primary & Secondary Insomnia
dr. Luh Nyoman Alit Aryani, SpKJ
AIMS:
Describe the clinical management of Primary and Secondary Insomnia (Definition, Etiology,
Risk Factor, Diagnose and Management)
LEARNING OUTCOMES:
Describe how to:
1. Understand the Classification of sleep disorder
2. Explain the Symptoms and Signs of insomnia and hypersomnia
3. Asses the Diagnostic of insomnia and hypersomnia
4. Give treatment for sleep disorder
CURRICULUM CONTENTS:
1. Understand the Classification of sleep disorder
2. Explain the Symptoms and Signs of insomnia and hypersomnia
3. Asses the Diagnostic of insomnia and hypersomnia
4. Give treatment for sleep disorder
ABSTRACTS
Sleep is a universal behavior that has been demonstrated in evey animal species study, from insects to mamalia. An earlier theory of sleep was that the excitatory areas of the upper brain stem, the reticular activating system, simply fatiqued during the waking day and became inactive as a result. Circadian rhythms are biological process that occur repeatedly on approximately a twenty-four-hour cycle. Lack of sleep can lead to the inability concentration, memory complaints and deficit in neuropsychological testing. Although several classification for sleep disorder exist, the Diagnostic and Statistical Manual of
Mental Disorder (DSM-IV) and the International Classification of Sleep Disorder, second edition (ICSD 2) are the most widely used. The DSM IV-TR classification is complaint based, it divides sleep disorders into primary and secondary sleep disorders based on clinical diagnostic criteria and presumed etiology.
The definition of Primary Sleep Disorder as those not cause by another mental disorder, a physical condition, or a substance but rather a caused by an abnormal sleep wake mechanism and often by conditioning. DSM-IV-TR divides primary sleep disorders into: Dyssomnias (disorders of quantity or timing of sleep) and Parasomnias (abnormal behaviors during sleep or the transition between sleep and wakefulness). The primary complaint of insomnia is difficulty in going to sleep. After a comprehensive history, the patient receives a detailed physical examination. Once a diagnosis has been confirmed, patients are offered approriate treatment (nonpharmacologic and pharmacologic).
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The physiology of sleep
2. Classification of sleep disorder
3. Symptom and sign of insomnia and hypersomnia
4. Clinical diagnostic of insomnia and hypersomnia
5. Management of sleep disorder
Udayana University Faculty of Medicine, DME 31
Study Guide Behavior Changes and Disorders
SCENARIO
Case 1
A 45 years old man, single, had 5 year history of fatique and sleepiness in the daytime. He started to sleep at 10.00 PM, and he woke up at 6.00 AM. He had oversleep almost every day. After having lunch he would routinely fell a sleep at the computer. He was free from mental or physical condition. When interviewd the patient was friendly, informative and self assured. He denied depressed mood or loss of interest or pleasure. He was in good health and jogged 4-5 miles daily. He lived with his wife and youngest son. He enjoyed socializing with his families.
Learning Task 1:
1. What is the most likely diagnosis?
2. From the story above, what need to be asking to the patient?
3. What is the therapy for the disorder?
Case 2
A 28 –year old woman came to psychiatric clinic. She said that she was difficult to sleep for
2 months. It lead inability concentration and fatique in his working. The physical examination was within normal limit.
Learning Task 2 :
1. What are the differential diagnosis?
2. What are the other symptom and medical history we have to find to asses the diagnostic?
3. What are the medications recommended for the patient?
4. What are the other treatment you recomend?
Case 3
A 27 years old woman was referred with symptoms of difficulty falling a sleep, shallow sleep
(easily wake up), dream a lot, early rise, fatique after waking up. When interviewing psychiatric patients complain of a very sad, hopeless against the problems that it faces. This complaint accompanied by loss of interest and fatigue, and has been going on for 2 months.
Free from physical condition and substance use.
Learning Task 3
1. What is the diagnosis of the disorder?
2. What are the baseline assesment must be done ?
3. What are the patient s symptoms point preferentally to the diagnosis?
4. What are the medications recommended for the patient?
Self Assesment :
1. How to do a good anamnesa in sleep disoerder?
2. What is the classification of sleep disorder and how to get the differential diagnosis ?
3. What are the management of sleep disorder?
Udayana University Faculty of Medicine, DME 32
Study Guide Behavior Changes and Disorders
Modul
10
Schizophrenia & Other Psychosis
Dr dr Cokorda Bagus Jaya Lesmana, SpKJ (K)
AIMS:
Describe the clinical management of Schizophrenia & Other Psychosis (Anamnesis, History taking, Mental State Examination, Diagnosis, and Therapy).
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of Schizophrenia & Other
Psychosis
3. Mental state examination of Schizophrenia & Other Psychosis
4. Diagnosis formulation
5. Modality of treatment of Schizophrenia & Other Psychosis
ABSTRACTS
Schizophrenia is a clinical syndrome of variable, but profoundly disruptive, psychopathology that involves cognition, emotion, perception, and other aspects of behavior. The expression of these manifestations varies across patients and over time, but the effect of the illness is always severe and is usually long-lasting.
Schizophrenia is a leading worldwide public health problem that exacts enormous personal and economic costs. Schizophrenia affects just less than 1 percent of the world's population. If schizophrenia spectrum disorders are included in the prevalence estimates, then the number of affected individuals increases to approximately 5 percent. The concept of schizophrenia spectrum disorders is derived from observations of psychopathological manifestations in the biological relatives of patients with schizophrenia. Diagnoses (and approximate lifetime prevalence rates [percent of population]) for these disorders are schizoid personality disorder (fractional percentage), schizotypal personality disorder (1 to 4 percent), schizoaffective psychosis (<1 percent), and delusional disorder (fractional percentage). The relationship of these disorders to schizophrenia in the general population is unclear, but in family pedigree studies, the presence of a proband with schizophrenia significantly increases the prevalence of these disorders among biological relatives.
Cognitive impairments and primary negative symptoms are largely responsible for the poor functional outcome and low quality of life of most persons with schizophrenia. Will new molecular targets result in the first efficacious treatments for these illness components?
What knowledge of etiopathophysiology is required to discover primary and secondary prevention interventions? Will the multiple genes involved in risk so overlap with affective and other disorders that current classification of diseases will be invalidated? Will the many common and small contributors to risk and the many and varied pathophysiological results require a new disease paradigm? The complexity of this most distinctively human disease syndrome, however, assures that the conquest of schizophrenia will be one of medicine's most difficult challenges.
Udayana University Faculty of Medicine, DME 33
Study Guide Behavior Changes and Disorders
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing Schizophrenia & Other Psychosis
2. Formulating diagnosis for Schizophrenia & Other Psychosis
3. Management of Schizophrenia & Other Psychosis
SCENARIO
A 30-year-old female is brought to hospital as she has been violent and hostile to her neighbours. According to the patient, her grandfather was a successful writer and she acquired his fortunes recently. However, she believes that her neighbours have found out about it and claims that she has heard them talking about stealing her money.
Learning Task:
1. What are the diagnostic features of this patient?
2. How long is the onset of illness on this kind of patient?
3. What is the diagnosed according to DSM V?
4. Explain the differential diagnosis of the above case?
5. What therapy should be given?
6. What is the difference between positive and negative symptoms of schizophrenia?
7. When reviewing the prognosis for people with schizophrenia, what kind of onset, gender, and duration suggest a more favorable outcome?
8. Discuss about the possibility when people like above case never get any treatment!
9. Discuss about any prevention work that possible for the relapse of the above case!
SCENARIO 2
An 18-year-old male is brought to hospital by his parents because they have noticed that he has been acting strangely recently. His parents say that the patient has just ‘lost it’ since failing his final examinations. The patient was noted to be giggling to himself, spending almost all his time in his room, and making unusual gestures with his hands. In addition, his speech has been incomprehensible and his parents cannot make any sense of it.
Learning Task:
1. What are the diagnostic features of this patient?
2. In relation to personality development what would be the cause for the occurrence of this disorder?
3. What is the diagnosed according to DSM-IV TR?
4. Explain the differential diagnosis of the above case?
5. What therapy should be given?
6. Discuss about the possibility when people like above case never get any treatment!
7. Discuss about any prevention work that possible for the relapse of the above case!
Self-Assessment:
1. What is the definition of suspicion, hallucinations, raptus, and abulia?
2. Explain the understanding of reality testing for psychosis!
3. Explain the difference between schizophrenia with organic mental disorders!
4. Explain the terms flat affect, inappropriate, inadequate!
5. Explain about developmental model of schizophrenia
6. Explain about early detection and intervention for schizophrenia
Udayana University Faculty of Medicine, DME 34
Study Guide Behavior Changes and Disorders
Modul
11
Delusional & Schizoafective Disorders
dr. Ni Ketut Sri Diniari, SpKJ
AIMS:
Describe Delusional disorder and schizoafective disorder, and its management.
LEARNING OUTCOME:
Can describe the:
1. Interview, mental status examination, diagnostic, and management delusional disorder.
2. Interview, mental status examination, diagnostic, and management schizoafective disorder.
CURRCIULUM CONTENS:
1. Psychiatric interview and mental status examination
2. Diagnostic in PPDGJ-III, ICD-X and DSM-5
3. Management of Delusional disorder and schizoafektif disorder
ABSTRACTS:
The DSM-5 criteria, delutional disorder and Schizoafectif disorder are a part of schizophrenia spectrum and other psychotic disorders. Delutional disorder is made when a person exhibits nonbizarre delutions of the last 1 month’s duration that cannot be attributed to other psychiatric disorders. They usually have to do with phenomena that, although not real, are nonetheless possible. Treatment use of antipsychotic, and individual supportive psychotherapy as well as family therapy.
Schizoafectif disorder has feature of both schizophrenia and mood disorders. An uninterrupted period of illness during which there is a mayor mood episode (major depressive or manic) concurrent with criterion A of schizophrenia. There are two type i.e:
Schizoafectif disorder, Bipolar type and Schizoafectif disorder, Depressive type. Treatment are included combination antipsychotic with mood stabilizer, and psychosocial treatment
(family terapy, social skill training, cogitive rehabilitation).
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1.
Able to make diagnostic and management Delusional disorder
2.
Able to make diagnostic and management schizoafective disorder
SCENARIO
A 23-year-old male believes that his life and the world are coming to an end after having lost his job. He has stopped looking after himself and has not eaten in 3 days as he believes that his body organs are decaying.
Learning task
1. What is the most likely diagnosis?
2. What are sign/ symptom dominant in this case?
3. What is the differential diagnosis of this patient?
4. How to management this disorder?
SCENARIO
A 26-year-old female has been living on the streets for the last week because she knows that a famous actor is planning a vendetta to kill her. She feels unsafe wherever she goes as she feels that she is constantly under threats of an attack.
Udayana University Faculty of Medicine, DME 35
Study Guide Behavior Changes and Disorders
Learning task
1. What is the most likely diagnosis for this patient?
2. What are sign/ symptom dominant in this case?
3. What is the differential diagnosis of this patient?
4. How to management this disorder?
Scenario
A 27-year-old male with no previous psychiatric history is brought to hospital by his family.
His parents noticed that he has been ‘high’ for the last few months, and that his behaviour has become increasingly erratic. He was also noted to have strange beliefs, such as the world being flat and the government trying to prevent this fact from being disclosed. He even stated that he has a radio-transmitting device implanted in his head which allowed him to pick up the signals sent from space. His elated mood and strange beliefs continued for a year.
Learning task
1. What is the most likely diagnosis for this patient?
2. What are sign/ symptom dominant in this case?
3. What is the differential diagnosis of this patient?
4. How to management this disorder?
Self Assessment
1. How to diagnose delusional and schizoaffective disorder?
2. How the characteristics of delusion in delusional and schizoaffective disorders?
3. How to distinguish delusions in schizophrenia and delusional disorders?
4. How to diagnoses schizoafective disorder?
5. what is the differences between schizoafective disorder with bipolar disorder?
6. what the management delutional disorder?
7. what the management schizoafective disorder?
Udayana University Faculty of Medicine, DME 36
Study Guide Behavior Changes and Disorders
Modul
12
Bipolar Disorders
dr Lely Setyawati, SpKJ (K)
AIMS:
Describe Bipolar Disorder and the clinical management of bipolar disorders
LEARNING OUTCOMES:
Describe how to:
1. Symptom and Sign of Bipolar disorders
2. Psychodinamic of Bipolar disorders
3. Diagnosis of Bipolar disorders
4. Therapy of Bipolar disorders
CURRICULUM CONTENTS:
1. History taking of Bipolar disorders
2. Observation and psychiatric interview of Bipolar disorders
3. Modality of treatment of Bipolar disorders
ABSTRACTS
The field of psychiatry has considered Major Depression and Bipolar Disorder to be two separate disorders, particularly in the last 20 years. The possibility that Bipolar Disorder is actually a more severe expression of major depression has been reconsidered recently, however. Many patients given a diagnosis of a Major Depressive Disorder reveal, on careful examination, past episodes of manic or hypomanic behavior that have gone undetected.
Many authorities see considerable continuity between recurrent depressive and bipolar disorders. This has led to widespread discussion and debate about the bipolar spectrum, which incorporates classic bipolar disorder, bipolar II, and recurrent depressions.
The Old Testament story of King Saul describes a depressive syndrome, as does the story of Ajax's suicide in Homer's Iliad. About 400 BC, Hippocrates used the terms mania and melancholia to describe mental disturbances. Mood is a pervasive and sustained feeling tone that is experienced internally and that influences a person's behavior and perception of the world. Affect is the external expression of mood. Mood can be normal, elevated, or depressed. Healthy persons experience a wide range of moods and have an equally large repertoire of affective expressions; they feel in control of their moods and affects.
Mood disorders are a group of clinical conditions characterized by a loss of that sense of control and a subjective experience of great distress. Patients with elevated mood demonstrate expansiveness, flight of ideas, decreased sleep, and grandiose ideas. Patients with depressed mood experience a loss of energy and interest, feelings of guilt, difficulty in concentrating, loss of appetite, and thoughts of death or suicide. Other signs and symptoms of mood disorders include change in activity level, cognitive abilities, speech, and vegetative functions (e.g., sleep, appetite, sexual activity, and other biological rhythms). These disorders virtually always result in impaired interpersonal, social, and occupational functioning.
Patients afflicted with only major depressive episodes are said to have major depressive disorder or unipolar depression. Patients with both manic and depressive episodes or patients with manic episodes alone are said to have bipolar disorder. The terms unipolar mania and pure mania are sometimes used for patients who are bipolar, but who do not have depressive episodes.
Three additional categories of mood disorders are hypomania, cyclothymia, and dysthymia. Hypomania is an episode of manic symptoms that does not meet the full text revision of the fourth edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-
Udayana University Faculty of Medicine, DME 37
Study Guide Behavior Changes and Disorders
IV-TR) criteria for manic episode. Cyclothymia and dysthymia are defined by DSM-IV-TR as disorders that represent less severe forms of bipolar disorder and major depression, respectively.
According to DSM-IV-TR, a major depressive disorder occurs without a history of a manic, mixed, or hypomanic episode. A major depressive episode must last at least 2 weeks, and typically a person with a diagnosis of a major depressive episode also experiences at least four symptoms from a list that includes changes in appetite and weight, changes in sleep and activity, lack of energy, feelings of guilt, problems thinking and making decisions, and recurring thoughts of death or suicide.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing bipolar disorders
2. Formulating diagnosis for bipolar disorders
3. Management of bipolar disorders
1.
2.
3.
4.
5.
SCENARIO
A 25-year-old male is taken to hospital by the police as he was found screaming on the streets. He had been trying to light himself with a lighter, claiming that he was invincible and had the power to fix all evil in the world. His speech was highly pressured and he complains that his thoughts are going out of control. According to hospital records, he had been admitted to hospital three times in the last year for similar episodes..
Learning task:
1. What is the most likely diagnosis?
2. What is the most likely etiology?
3. What is the baseline assesment must be done?
4. What is the patient’s symptoms point preferentally to the diagnosis?
5. What is the first line medications recommended for the patient?
6. What are the other symptoms of bipolar disorder depressive type?
7. Why is Isabel diagnosed as having bipolar I instead of bipolar II disorder?
SCENARIO
A 28-year-old female presents to the clinic complaining of low mood. She describes her m ood as ‘depressing’ and is unable to do anything. Because of her low mood, she has not eaten for 3 days. She mentions that a year ago, she was feeling on top of the world and went through periods when she did not have to sleep. On that occasion, she was admitted to hospital because her parents thought that she was going ‘out of control’.
Learning task
1. What is the most likely diagnosis for this patient?
2. What are sign/ symptom dominant in this case?
3. What is the differential diagnosis of this patient?
4. How to management this disorder?
Self Assessment:
Please describe Depressive Disorder according to ICD-10/PPDGJ-3.
What are the diagnosis differential of MDD? Please describe each of them.
Is there any relationship between Bipolar Disorder and Suicide?
What is the different between Bipolar I disorder and Bipolar II disorder
Individuals with major mood disorders are at an increased risk of having one or more additional comorbid Axis I disorders. Please describe the comorbidity of Bipolar
Disorder.
Udayana University Faculty of Medicine, DME 38
Study Guide Behavior Changes and Disorders
Modul
13
Panic Disorders
dr I Gusti Ayu Indah Ardani, SpKJ
AIMS:
Describe Panic Disorder and the clinical management of panic disorders
LEARNING OUTCOMES:
Describe how to:
1. Symptom and Sign of panic disorders
2. Psychodinamic of panic disorders
3. Diagnosis of panic disorders
4. Therapy of panic disorders
CURRICULUM CONTENTS:
1. History taking of panic disorders
2. Observation and psychiatric interview of panic disorders
3. Modality of treatment of panic disorders
ABSTRACTS
The essential feature are recurrent attacks of severe anxiety which are not restricted to any particular situation or set of circumstances, and which are therefore unpredictable. As in other anxiety disorders, the dominant symptoms vary from person to person, but sudden onset of palpitations, chest pain, choking sensations, dizziness, and feelings of unreality
(depersonalization or derealization ) are common. There is also, almost invariably, a secondary fear of dying, losing control, or going mad.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing panic disorders
2. Formulating diagnosis for panic disorders
3. Management of panic disorders
SCENARIO
Mrs K was a 35 year-old woman who initially presented for treatment at yhe medical emergency department at a large university- based medical center. She reported that while sitting at her desk at her job, she had suddenly experienced difficulty breathing, dizziness, tachycardia, shakiness, and felling of terror that she was going to die of a heart attack. A colleague drove her to the emergency department, where she received a full medical evaluation, including ECG and routine blood work, which revealed no sign of cardiovascular, pulmonary and other illness. She was subsequently referred for pshychiatric evaluation, where she revealed that she had experienced two additional episodes over the past month, once when driving from work and once when eating breakfast. However she had no presented for medical treatment because the symptoms had resolved relatively quickly each time, and she worried that if she went to the hospital without ongoing symptoms, “people would think “I’m crazy”. Mrs K reluctantly took the phone number of local psychiatrist but did not call until she experienced a fourth episode of a similar nature.
Learning Task
1. What should the doctor do for the first time towards the patient?
2. Explain the sign and symptoms of the above patient!
3. What is the multiaxial diagonosis?
Udayana University Faculty of Medicine, DME 39
Study Guide Behavior Changes and Disorders
4. How is the holistic treatment for the patient above?
Self Assessment
1. First time checking out a case of panic disorder, what therapeutic atmosphere should be given to the patient?.
2. Explain on making good environment for patient recovery!
3. Explain the basic personality for patient with panic disorders!
4. Explain the role of neurotransmitter in panic disorder!
5. Antianxiety often lead to dependency, as a doctor what is your wise opinion in using this medication?
6. Explain the psychodynamic of panic disorder!
Udayana University Faculty of Medicine, DME 40
Study Guide Behavior Changes and Disorders
Modul
14
Somatoform Disorders
dr I Gusti Ayu Indah Ardani, SpKJ
AIMS:
Describe the brief history, general phenomenology, general etiologies and treatment principal of somatoform disorders (Anamnesis, History taking, Mental State Examination,
Diagnosis, and Therapy).
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of somatoform disorders
3. Mental state examination of somatoform disorders
4. Diagnosis formulation
5. Modality of treatment of somatoform disorders
ABSTRACTS
There are seven somatoform disorders in the revised fourth edition of the Diagnostic and
Statistical Manual of Mental Disorders (DSM-IV-TR), two of which are subsyndromal or nonspecific disorders. This nosology overlaps with the tenth edition of the International
Statistical Classification of Diseases and Related Health Problems (ICD-10) classification, yet there are important differences that are apparent from the criteria. The DSM-IV-TR has conversion disorder and body dysmorphic disorder in its classification, whereas the ICD-10 does not, but instead specifies somatoform autonomic dysfunction and other somatoform disorders.
Characteristic of somatoform disorders are three enduring clinical features: (1) somatic complaints that suggest major medical maladies yet have no associated serious and demonstrable peripheral organs disorder, (2) psychological factors and conflicts that seem important in initiating, exacerbating, and maintaining the disturbances; and (3) symptoms or magnified health corncerns that are not under the patient’s conscious control.and laboratory
Because of their intense bodily perceptions, restricted level of physical functioning, and morbid beliefs, these patients have become convinced they harbor serious physical problem. Moreover, their symptoms are not willfully controlled. Whatever their faults and problems, these patients are not malingerers. Yet their physicians physical imfirmity other than the patients vigorous and sincere complaints. Patients with somatoform disorder are convinced that their suffering comes from some type of presumably undetected and untreated bodily derangement.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The psychological conflict in somatoform disorders
Udayana University Faculty of Medicine, DME 41
Study Guide Behavior Changes and Disorders
2. Formulating diagnosis for somatoform disorders
3. Management of somatoform disorders
4. Basic personality in somatoform disorders
SCENARIO
Mrs A, 38 year-old had complained of nervourness since childhood. She also said she was sickly since her youth, with a succession of physical problems that doctor often indicated were caused by her nerves or depression. She however, believed that she had a physical problem that had not yet been uncovered by the doctors. Besides nervousness, she had chest pain and had been told by variety of medical consultants that she had a nervous heart. She also consulted doctors for abdominal pain and had been told she has a spstic colon. She had seen chiropractors and osteopaths for backaches, for pains in extremities, and for anesthesia of her finger tips.
Three months previously, she was vomiting and had chest pain and abdominal pain, and she was admitted to a hospital for hysterectomy. Since the hysterectomy, she had had repeated anxiety attack, fainting spells that she claimed were associated with unconsciousness, vomiting, food intolerance, weakness, and fatique. She had been hospitalized several times for medical workups for vomiting, colitis, vomiting of blood, and chest pain. She had had a surgical procedure for an abscess of the throat. She said she felt depressed but thougth that it was all because her “hormones were not straightened out”.
She was still looking for medical explanation for her physical and physchological problems.
Learning Task
1. What is the most likely diagnosis for this patient?
2. What are sign/ symptom dominant in this case?
3. What is the differential diagnosis of this patient?
4. How to management this disorder?
Self Assessmant
1. How to distinguish somatization disorder with hipochondriac?
2. What is the primary choice for the treatment of somatoform disorders? please explain!
3. Explain the psychodynamic of somatoform disorder
4. Explain the differential diagnosis of somatoform disorder
Udayana University Faculty of Medicine, DME 42
Study Guide Behavior Changes and Disorders
Modul
15
Generalized Anxiety & Obsessive Compulsive Disorder
dr. Ni Ketut Putri Ariani, SpKJ
AIMS:
Describe the clinical management of generalized anxiety & obsessive compulsive disorders
(Anamnesis, History taking, Mental State Examination, Diagnosis, and Therapy)
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of generalized anxiety & obsessive compulsive disorders
3. Mental state examination of generalized anxiety & obsessive compulsive disorders
4. Diagnosis formulation
5. Modality of treatment of generalized anxiety & obsessive compulsive disorders
ABSTRACTS
Anxiety disorders, in general, are the most common form of mental illness in the USA.
Generalized Anxiety Disorders (GAD) is one of the most common anxiety disorders, with a lifetime prevalence of 5.1% in the adult US population. GAD typically occurs before the age of 40, runs a chronic, fluctuating course, and affects women twice as often as men. Despite historic controversy to the contrary, numerous studies have demonstrated that GAD is a distinct illness, which occurs at a significant rate with serious consequences. Additionally,
GAD has been found to confer disability at approximately the same level as depression and other chronic medical illnesses.
Pharmacological, cognitive-behavioral, and psychodynamic approaches have all proved useful in combating GAD. Most of patients should expect substantial relief from their symptoms in a relatively brief period. Hence, clinicians in psychiatry and other specialties must make the proper GAD diagnosis rapidly and initiate treatment.
GAD-associated genetic factors are completely shared with depression, while environmental determinants seem to be distinct. This notion is consistent with recent models of emotional disorders that view anxiety and mood disorders as sharing common vulnerabilities but differing on dimensions including, for instance, focus of attention or psychosocial liability.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing generalized anxiety & mixed anxiety-depression disorders
2. Formulating diagnosis for generalized anxiety & mixed anxiety-depression disorders
3. Management of generalized anxiety & mixed anxiety-depression disorders
Udayana University Faculty of Medicine, DME 43
Study Guide Behavior Changes and Disorders
SCENARIO
A 32-year-old single mother of two children is seeking professional help for her longstanding feelings of anxiety. Despite the fact that her life is relatively stable in terms of financial and interpersonal matters, she worries most of the time that she will develop financial problems, that her children will become ill, and that the political situation in the country will make life for her and he children more difficult. Although she tries to dismiss these concerns as excessive, she finds it virtually impossible to control her worrying. Most of the time, she feels uncomfortable and tense, and sometimes her tension become so extreme that she begins to tremble and sweat. She finds it difficult to sleep at night. During the day she is restless, keyed up, and tense. She has consulted a variety of medical specialist, each of whom has been unable to diagnose a physical problem.
Learning task:
1. What is the diagnosis of the presenting case?
2. How is the case of formulation?
3. What is the treatment plan?
4. What is the outcome or prognosis of the case?
SCENARIO 2
A 42-year-old seller woman, often complain of headache since last month. She also often feels nausea and appetite-less. She had consulted to a doctor many times who finally suggest her to visit a psychiatrist. She feels sad because her husband was hospitalized by stroke disease and she has financial problem. She worried that her husband will not recovery, and cannot pay for her children’s school. She feels uncomfortable and tense.
Leaning task:
1. What is the diagnosis of the presenting case?
2. How is the case of formulation?
3. What is the treatment plan?
4. What is the outcome or prognosis of the case?
Self assessment
1. What are the diagnostic features of GAD?
2. What are the diagnostic features of mixed anxiety-depression disorders?
3. Explain the treatment principles in GAD
4. Explain the treatment principle in mixed anxiety-depression disorders
5. Explain about the biopsychosocial aspects of GAD
6. Explain about the biopsychosocial aspects of mixed anxiety-depression disorders
ABSTRACTS
Obsessions and compulsions are the essential features of OCD. An individual must exhibit either obsessions or compulsions to meet DSM-IV-TR criteria. DSM-IV-TR recognizes obsessions as “persistent ideas, thoughts, impulses, or images that are experienced as intrusive and inappropriate,” causing distress. Obsessions provoke anxiety, which accounts for the categorization of OCD as an anxiety disorder. However, they must be differentiated from excessive worries about real-life problems and associated with efforts to either ignore or suppress the obsessions. Typical obsessions associated with OCD include thoughts about contamination (“my hands are dirty”) or doubts (“I forgot to turn off the stove”).
Obsessions and compulsions must cause an individual marked distress, consume at least 1 hour per day, or interfere with functioning to be considered above the diagnostic threshold. During at least some point in the illness, adult patients must recognize symptoms of OCD as unreasonable, although there is great variability in the degree to which this is true, both across individuals and in a given individual over time. For example, early in the
Udayana University Faculty of Medicine, DME 44
Study Guide Behavior Changes and Disorders course of the disorder, patients may recognize their hand washing as excessive or irrational, but, over a number of years, this recognition may no longer exist.
The clinical management of Trichotillomania and Obsessive Compulsive Disorders
Consist of how to make a proper diagnosis through good anamnesis, physical examination, psychometric examination and give the patient proper treatment with medical and psychotherapy modality.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of Trichotillomania and Obsessive Compulsive Disorders Diagnosis
2. Management of Trichotillomania and Obsessive Compulsive Disorders
3. Psychometric Examination of Trichotillomania and Obsessive Compulsive Disorders
SCENARIO
A 13 year old girl came to psychiatric clinic accompanied by her mother with main complain repetitive hair pulling that result in significant hair loss. There is an increasing level of tension immediately before hair pulling. There is a sensation of pleasure during hair pulling the pulling is not explained by a general medical condition or other mental disorder.
Significant distress of in social occupational or other areas of functioning is as a result of the pulling. Physical examination is a normal.
Learning Task
1. From the story above, what need to be asking to the patient?
2. Please explain the psychodynamic from this case!
3. What is the differential diagnosis of this patient?
4. What is the planning diagnosis that you suggest?
5. What treatment you give please explain it?
SCENARIO 2:
A 6-year-old male complains of feeling sick with stomach ache during school days and refuses to go to school. He cries if his mother attempts to leave him under any circumstance. He finds it difficult to go to bed without his mother being by his side and frequently gets up at night to check on her. When questioned about this, he says that he is worried that something terrible will happen to her and that he will never see her again.
These symptoms have developed since his parents divorced 6 months ago.
Learning Task
1. From the story above, what need to be asking to the patient?
2. Please explain the psychodynamic for this patient!
3. What is the differential diagnosis of this patient?
4. What is the planning diagnosis that you suggest?
5. What is the planning treatment that you give?
Self Assessment
1. How to do a good anamnesis in Obsessive-Compulsive Disorders case?
2. What is the psychometric test you make to the patient?
3. Explain the etiology of Obsessive-Compulsive Disorders!
4. Is the Obsessive-Compulsive Disorders ego dystonic? Please explain!
Udayana University Faculty of Medicine, DME 45
Study Guide Behavior Changes and Disorders
Modul
16
Post Traumatic Stress Disorder (PTSD)
Dr dr Cokorda Bagus Jaya Lesmana, SpKJ (K)
AIMS:
Describe the clinical management of PTSD (Anamnesis, History taking, Mental State
Examination, Diagnosis, and Therapy)
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis
2. History taking
3. Examine mental state
4. Diagnosis
5. Therapy (pharmacotherapy, psychotherapy)
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of PTSD
3. Mental state examination PTSD
4. Diagnosis formulation
5. Modality of treatment of PTSD
ABSTRACTS
Posttraumatic stress disorder is classified as an anxiety disorder in the DSM IV; the characteristic symptoms are not present before exposure to the violently traumatic event. In the typical case, the individual with PTSD persistently avoids all thoughts and emotions, and discussion of the stressor event and may experience amnesia for it. However, the event is commonly relived by the individual through intrusive, recurrent recollections, flashbacks, and nightmares. The characteristic symptoms are considered acute if lasting less than three months, and chronic if persisting three months or more, and with delayed onset if the symptoms first occur after six months or some years later. PTSD is distinct from the briefer acute stress disorder, and can cause clinical impairment in significant areas of functioning.
In PTSD, the individual develops symptoms in three domains: reexperiencing the trauma, avoiding stimuli associated with the trauma, and experiencing symptoms of increased autonomic arousal, such as an enhanced startle. Flashbacks, in which the individual may act and feel as if the trauma were recurring, represent the classic form of reexperiencing. Other forms of reexperiencing include distressing recollections or dreams and either physiological or psychological stress reactions when exposed to stimuli that are linked to the trauma. An individual must exhibit at least one reexperiencing symptom to meet criteria for PTSD. Symptoms of avoidance associated with PTSD include efforts to avoid thoughts or activities related to the trauma, anhedonia, reduced capacity to remember events related to the trauma, blunted affect, feelings of detachment or derealization, and a sense of a foreshortened future. An individual must exhibit at least three such symptoms.
Symptoms of increased arousal include insomnia, irritability, hypervigilance, and exaggerated startle. An individual must exhibit at least two such symptoms.
Because individuals often exhibit complex biological and behavioral responses to extreme trauma, the clinician must identify other medical and psychiatric conditions in the traumatized patient. The clinician must always evaluate whether neurological etiologies
Udayana University Faculty of Medicine, DME 46
Study Guide Behavior Changes and Disorders underlie trauma-related symptoms, particularly after traumatic events that involve physical injury. Traumatized patients also can develop mood disorders, including dysthymia and major depression, as well as other anxiety disorders, such as generalized anxiety disorder or panic disorder, and substance use disorders. Finally, recent research suggests that some psychiatric features of posttraumatic syndromes can relate to a patient's state before the trauma. For example, patients with premorbid anxiety or affective syndromes may be more likely to develop posttraumatic symptoms than individuals who are free of mental illness before the trauma. As a result, the clinician should consider the premorbid mental state of the traumatized.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of PTSD
2. Management of PTSD
3. Psychometric Examination of PTSD
SCENARIO
Mr. F. sought treatment for symptoms that he developed in the wake of an automobile accident that had occurred approximately 6 weeks before his psychiatric evaluation. While driving to work on a mid-January morning, Mr. F. lost control of his car on an icy road. His car swerved out of control into oncoming traffic, collided with another car, and then hit a nearby pedestrian. Mr. F. was trapped in his car for 3 hours while rescue workers cut through the car door. After referral, Mr. F. reported frequent intrusive thoughts about the accident, including nightmares of the event and recurrent intrusive visions of his car slamming into the pedestrian. He reported that he had altered his driving route to work to avoid the scene of the accident and that he found himself switching the TV channel whenever a commercial for snow tires appeared. Mr. F. described frequent difficulty falling asleep, poor concentration, and an increased focus on his environment, particularly when he was driving.
Leaning task:
1. What is the diagnosis of the presenting case?
2. How is the case of formulation?
3. What is the treatment plan?
4. What is the outcome or prognosis of the case?
SCENARIO 2:
Trevor was sexually abused as a child by a family relative. Although he was about to get married and had thoughts about planning a family, he still felt haunted by childhood events.
He was worried that the events from his past would affect his ability to bond with his children and affect their relationship.
Leaning task:
1. What is the diagnosis of the presenting case?
2. How is the case of formulation?
3. What is the treatment plan?
4. What is the outcome or prognosis of the case?
SCENARIO 3:
Max is a boy nearly four years of age who lived with his family in Battery Park City, across the street from the World Trade Center. Prior to 9/11, he had already experienced numerous traumatic events including surgeries for a chronic condition and hospitalization for a minor burn. In December 2001 Max saw his pediatrician for the first time in several months and
Udayana University Faculty of Medicine, DME 47
Study Guide Behavior Changes and Disorders presented with vomiting and poor appetite. Max had an overall positive score on PSC-17 and a positive score for internalizing problems. Since 9/11, Max has reverted to wearing diapers at night, wearing his shoes all the time, has become increasingly introverted and stopped wanting to go to school, although he enjoyed going to school in the past. Over time, pediatric visits grew more frequent as Max continued to experience stomachaches and difficulty breathing despite normal physical exams.
Learning task:
1. What is the role of family in this case?
2. What is the role of primary care physician in this case?
3. How do you formulate the intervention? Do you need to referall the patient?
4. What is the prognosis of this patient?
Self assessment
1. What are the diagnostic features of PTSD?
2. Explain the treatment principles in PTSD
3. Explain about the biopsychosocial aspects of PTSD
4. Explain the epidemiology of PTSD
5. Explain the differential diagnosis of PTSD
Udayana University Faculty of Medicine, DME 48
Study Guide Behavior Changes and Disorders
Modul
17
Sexual Disorders
dr Wayan Westa, SpKJ (K)
AIMS
Emphasizing on the understanding of sexual perversion relation to physical and mental health
Understanding the follow-up of sexual perversion good behavior of the offender and victim
LEARNING OUT COMES
1. Understand the notion of sexual deviance
2. Understand the psychodynamics of sexual deviation
3. Understand the types of sexual deviance
4. Understanding of the bad influence of sexual deviation, both physically and mentally on the victim
5. Understand the initial handling of the victim and the offender is then able to make a referral
CURRICULUM CONTENTS
1. Understand the definition of sexual deviance
2. Understand the role of genetics, upbringing of parents and psychosocial status were associated with the occurrence of sexual deviance
3. Understand the influence of bad behavior on the victim's sexual deviation, both physically and mentally
4. Being able to make a diagnosis of sexual deviations
5. Able to provide initial treatment to the perpetrator and the victim then make referrals
ABSTRACT
Cases of sexual deviation tendency of the number continues to rise. This problem can not be separated from the role of print media or television broadcast the news. Sexual deviance is a condition that deviate in the direction and sexual style. Sexual normal when an adult male sexual desire in a partner of the opposite sex peers. One example of sexual perversion an adult male sexual arousal to children only. Incidence of sexual deviance is not independent of the genetic role parenting parents during child development from birth through adolescence. Babies born has been equipped with instinct. Sexual instinct called libido associated with pleasure, at the beginning of enjoyment of the lips / mouth so the baby feel good when sucking the breast and nipple (oral phase), then taste the pleasure of moving into the rectum (anal phase), new last focused in genital organs (phase phallic).
When parenting parents, especially the mother goes well then psychosexual development can work well. However, if the phase of sexual development have problems, then comes the sexual perversion in adulthood.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. Understand the notion of sexual deviance or paraphilia
2. Understand the psychodynamics and sexual deviation
3. Understand the types of sexual deviance
4. Understand the characteristics of the individual potential to become a pedophile
5. Understand the bad influence, both physically and mentally on victims of pedophile behavior
6. Able to perform initial therapy and refer victims
Udayana University Faculty of Medicine, DME 49
Study Guide Behavior Changes and Disorders
SCENARIO
A man aged 50 years foreign nationals were on vacation in Bali staying at one of the hotels in Kuta. He often tours to Bali east in town Amlapura, sightings are very polite and generous attitude and love children so quickly accepted by the public. Children gathered to play given gifts of clothes, money, etc. But the uproar ensued because one of the kids that show strange behavior such as moody, did not venture out. After being asked by the child's parents that she had to serve the sexual appetite through the rectum (sodomy) by these men.
Learning Task
1. Sexual Deviations what happened to these men?
2. Explain the psychodynamics of pedophilia!
3. What are the adverse effects of physical and mental side of the victim?
4. What is the initial treatment can be given to victims of the above? What to do next?
5. Efforts to what can be done by the people and government so that such cases can be reduced or eliminated?
SCENARIO 2:
A man 30 years old unmarried farmer discovered by his neighbors were having sexual intercourse with his pet calf. The incident was reported to the village headman. Finally the meeting was to resolve this problem.
Learning Task
1. What is the diagnosis conclusion of the above behaviors?
2. Explain the instinct theory of progress toward normal sexual libido!
3. What do we know of the Oedipus phase - Complex?
4. Explain the notion of: voyeurism, transexualisme, fetishism!
5. The above case is a sexual perversion, do you think another diagnosis?
Self Assesment
1. Describe examples of sexual perversion!
2. Sexual Deviations which adversely affect the heaviest?
3. What do you know about GUY and LESBIAN?
4. What is a homosexual sintonik ego and ego-dystonic homosexuality?
5. In your opinion, how do the case of sexual deviance is not increasing in number?
Explain
Udayana University Faculty of Medicine, DME 50
Study Guide Behavior Changes and Disorders
Modul
18
Psycho-Pharmacology
dr. I Gusti Ayu Artini, M.Sc
AIMS:
1. Describe the rationale drugs can be used for anxiety, insomnia, depression and
Psychotic disorders.
2. Describe the pharmacokinetic and pharmacodynamic aspect of drugs used for
Psychiatric disorders.
LEARNING OUTCOMES:
Describe how:
1. The pharmacokinetic and pharmacodynamic aspect of drugs used for psychiatric disorders including sedative-hypnotic, antidepresssant, and antipsychotic drugs.
2. To apply the basic concepts and principles of drugs used for insomniaExamine mental state
CURRICULUM CONTENTS:
1. The pharmacokinetic and pharmacodynamic aspect of sedative-hypnotic drugs a. Benzodiazepines b. Barbiturates c. Misellaneous agents
2. The pharmacokinetic and pharmacodynamic aspect of antidepressant drugs a. Tricyclic antidepressant b. Heterocyclic antidepressant c. Selective Serotonin Reuptake Inhibitor (SSRI) d. Monoamine Oxidase Inhibitor (MAOI)
3. The pharmacokinetic and pharmacodynamic aspect of antipsychotic drugs a. Classic drugs (Phenothiazine, Thioxanthene, Butyrophenone) b. Atypical drugs (Olanzapine, clozapine, risperidone etc.)
ABSTRACTS
Drugs used to treat psychiatric disorders are generally known as psychotropic or psychotherapeutic drugs. Psychotherapeutic drugs used to treat mental illness include sedative-hypnotic, antidepressant and antipsychotic (neuroleptic) drugs.
There are three classes of sedative-hypnotic drugs: benzodiazepines, barbiturates and miscellaneous agents. Benzodiazepines and barbiturates exert their action by facilitating (potentiating) the inhibitory action of GABA, therefore increasing the frequency or duration of GABA-mediated chloride ion channel opening. The use of sedative-hypnotic drugs may cause many adverse effects including dependence, tolerans, CNS depression, cardiovascular and respiratory depression.
Most antidepressant exert their actions by inhibiting the metabolism or reuptake of monoamine neurotransmitter particularly norepinephrine (NE) and/or serotonin (5HT). There are four classes of antidepressant: tricyclic antidepressant (TCA), heterocyclic antidepressant, selective serotonin reuptake inhibitor (SSRI), and monoamine oxidase inhibitor (MAOI). Serotonin syndrome and hypertension crisis are the severe toxic effects of antidepressant should aware to.
Antipsychotic drugs are thought to act by inhibiting or blocking the release of dopamine in the brain, therefore will supress the symptoms of certain psychotic disorders.
Antipsychotic drug is classified into two group of drugs: classic drugs (including phenothiazine, thioxanthenes and butyrophenones) and atypical drugs (clozapine, olanzapine, loxapine, risperidone etc.). The most significant adverse reaction associated
Udayana University Faculty of Medicine, DME 51
Study Guide Behavior Changes and Disorders with the antipsychotic drugs is the extrapyramidal effect that commonly manifests as
Parkinson-like symptoms, akathisia, and dystonia.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The cycle of neurotransmitter in the synaps
2. The role of neurotransmitter involved in psychiatric disorders
3. The mechanism of action for sedative-hypnotic, antidepressant and antipsychotic drugs
4. The pharmacokinetic and pharmacodynamic aspect of sedative-hypnotic, antidepressant and antipsychotic drugs
5. Drug interaction related to sedative-hypnotic, antidepressant and antipsychotic drugs
SCENARIO
A 23-year-old male with no previous psychiatric history presents to hospital complaining that his neighbours have been plotting an attack on him. He also mentions that he can hear his neighbours discussing his actions and appearances all the time. He is suspicious all the time and believes that he is under surveillance by hidden cameras. The doctor prescribes this medication, but warns the patient of possible drowsiness and obesity.
Learning Task
1. What drugs can be used for patient above? Describe the mechanism of action for
2.
3. the drug.
Based on the scenario above, what condition possibly happened to this patient?
What are other adverse effects of sedative-hypnotic drugs should aware to?
SCENARIO 2
A 45-year-old male patient with a psychotic illness has been unsettled on the ward with increasing signs of agitation. His treatment is currently under review as he had developed
3.
4.
5.
6.
7. neuroleptic malignant syndrome following the use of atypical antipsychotics. He has an argument with a fellow patient and following this, starts screaming and breaking the ward windows. The team decides to treat this acute episode using an intramuscular combination of a short-acting benzodiazepine and this medication.
Learning Task
1. What drug can be given to manage patient’s disease?
2.
3.
4.
How is the mechanism of action of that drug?
What are the adverse effects possibly happened regarding the use of that drug?
If there were signs of hallucination and/or delusion found on the patient, what drug should be given? How is the mechanism of action? What are the adverse effects commonly occur regarding the use of that drug?
SELF ASSESSMENT
1.
2.
Mention classification of sedative-hypnotic drugs
How did benzodiazepine and barbiturate exert their action?
List adverse effect of sedative-hypnotic drugs
Mention classification of antidepressant drugs
How is the mechanism of action of each class of antidepressant drugs?
List adverse effect of sedative-hypnotic drugs
Mention classification of antipsychotic drugs
8.
9.
How is the mechanism of action of each class of antipsychotic drugs?
List adverse effect of antipsychotic drugs
Udayana University Faculty of Medicine, DME 52
Study Guide Behavior Changes and Disorders
Modul
19
Self Harm & Suicide
dr. Ida Ayu Kusuma Wardani, SpKJ, MARS
AIMS:
Describe the management of disorders mood, thought, and behavior at a time of crisis. Self harm and suicide one part of the emergency psychiatry
LEARNING OUTCOMES:
Describe how to:
1. Diagnosis
2. Risk factors
3. Pathophysiology
4. Treatment of suicide risk
CURRICULUM CONTENS:
1. Epidemiology
2. Psychiatric and medical risk factors
3. Familial and genetic
4. Pathophysiology
5. Treatment
ABSTRACTS
Emergency psychiatry refers to the management of disorders of mood, thought, and behavior at a time of crisis. It entails assessment, development of a differential diagnosis of psychiatric and other medical causes of presenting symptoms, and diagnostic specific pharmacotherapy, medical and surgical therapy, and psychotherapy. Psychiatric emergencies are oft en particularly disturbing because they do not just involve the body’s reactions to an acute disease state, as much as actions directed against the self.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. People very distress and change behavior, unsure what to do or not to do
2. Management of psychiatric emergency care
3. Treatment self harm & suicide
SCENARIO
A 23-year-old male was found cutting his arms and thighs with a knife. He claims that there are bugs crawling underneath his skin and that he is trying to get rid of them. On examination, he is tachycardic with prominent dilatation of pupils and nasal ulceration. He appears sexually disinhibited, restless, and excited.
Learning Task:
1. From the story above, why do act self-harm?
2. What are the methods of self-harm?
3. Please explain pathophysiology?
4. What is the diagnosis?
5. What is the holistic treatment?
SCENARIO
A 20-year-old female presents to hospital having lacerated her forearm. She claims that she had a major argument with her boyfriend and did it so that her boyfriend would worry and not break up with her. According to her, all her relationships in the past have been ‘intense like this’. On examination, there are multiple healed laceration scars on both arms.
Udayana University Faculty of Medicine, DME 53
Study Guide Behavior Changes and Disorders
Learning Task:
1. Explain the psychodynamic of self-harm?
2. What are the methods of self-harm?
3. Please explain pathophysiology?
4. What is the diagnosis?
5. What is the holistic treatment?
SELF ASSESSMENT
1. What is a defense mechanism used by the patient?
2. Which factors are associated with self harm and suicide?
3. What is the relationship between self-harm and suicide with mental disorders?
4. How to prevent self-harm and suicide?
Udayana University Faculty of Medicine, DME 54
Study Guide Behavior Changes and Disorders
Modul
20
Child Abuse & Neglected
dr Anak Ayu Sri Wahyuni, SpKJ
AIMS:
Describe evaluation, management, and treatment of child abuse
LEARNING OUTCOMES:
Describe how to:
1. Anamnesis child with child abuse
2. History taking of child abuse
3. Examine mental state of child with child abuse
4. Diagnosis child abuse
5. Therapy (pharmacotherapy, psychotherapy) child abuse
CURRICULUM CONTENTS:
1. Anamnesis child abuse
2. History taking (fundamental four and secret seven) of child abuse
3. Mental state examination of child abuse
4. Diagnosis formulation of child abuse
5. Modality of treatment of child abuse
ABSTRACTS
Abuse and neglect cases can be some of the most disturbing and heartwrenching eperiences in child and adolescent psychiatry, sometimes evoking horror and a wish to rescue the victim immediately. Therefore it is important to keep a sense of perspective on how good the evidence is that abuse is indeed happening, and to have a sympathetic team for emotional support to stop one becoming overwhelmed by, or cut off from, what is seen.
Within the broad definition of child maltreatment, five subtypes are distinguished – these are physical abuse; sexual abuse; neglect and negligent treatment; emotional abuse and exploitation. Compiling lists of general or culturally relative risks is a necessary first step toward assessing the interaction of risk and protective circumstances in each family, community and culture. However, theories that propose single factors or combinations of risk factors as invariably leading directly to child abuse will stigmatize families which fall within the profile and lead to missed cases of child abuse, which do not fit the profile. In families where child abuse does exist, they may be more likely to hide the abuse as it now carries a public condemnation. In families where it is not present, stigmatization may translate into marginalization of the family.
Preventing the abuse of children in settings other than the family (such as schools, hospitals, psychiatric institutions and prisons), and by persons other than caregivers (such as members of the clergy, the police and teachers) is also an important area of work, but one which is likely to require very different strategies to those which have proven effective in preventing intra-familial child maltreatment.
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing child abuse
2. Formulating diagnosis for child abuse
3. Management of child abuse
Udayana University Faculty of Medicine, DME 55
Study Guide Behavior Changes and Disorders
SCENARIO
Financially comfortable parents lived in a pleasant, clean house in a nice neighborhood, but they had no friends. Their four teenagers never had visitors. One day, the oldest girl, 17 years of age, went to the police and told them that she had a baby at home and that her own father was the father of the baby. The girl said that her father had been having sexual relations with her for more than 4 years and that he was now doing the same with her younger sisters. The mother admitted knowing about the situation for years, but she had not reported it to the authorities for fear of losing her husband.
Learning task:
1. Explain the definition of abuse and neglection in children
2. Describe the impacts of abuse and neglected children
3. Explain the symptoms of psychiatric disorders caused by abuse and neglect of children
4. Explain the strategy of therapy for children who are abused and neglected
5. Explain how to refer patient with abuse and neglect
6. Explain Diagnosis physically abuse children according DSM V
7. Explain Clinical features emotional abuse children
8. Explain Clinical features neglected children
9. Explain Evaluation process child who have been sexually abuse
10. Explain the prevention child abuse in families and community
11. Explain the treatment that can be provided to children that have been physically abuse
Self Assesment
1. Explain about child maltreatment
2. Explain about interpersonal violence
3. Explain about psychopathology of revictimization
4. Explain about the psychological symptoms of an abused child
Udayana University Faculty of Medicine, DME 56
Study Guide Behavior Changes and Disorders
Modul
BASIC CLINICAL SKILL
INTRODUCTION
AIMS:
Perform ability to collect specific, detailed information about topics constitute the psychiatric evaluation. Acquiring the database of information for the interviewer to make diagnoses on five axes and develop a treatment plan acceptable to the patient.
LEARNING OUTCOMES:
Able how to:
1. Warm-up and Chief Complaint
2. Make the Diagnostic Decision Loop
3. Make history and Database
4. Make diagnosing and Feedback
5. Make treatment Plan and Prognosis
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven)
3. Mental state examination
4. Healing formulation
5. Modality Treatment
ABSTRACTS
Psychiatric interviewing is a special form of human communication. The interviewer asks the patient to disclose complaints, share problems, and reveal suffering. According to the difficulties that the patient experiences with this request, the interviewer shifts the focus between disorder-centered and patient-centered interviewing. Disorder-centered interviewing is based on a descriptive, atheoretical model of psychiatric disorders called the medical model, which is the official model supported by the American Psychiatric
Association (APA) and the World Health Organization (WHO) codified in DSM-IV-TR (2000) and the International Classification of Diseases (ICD-10). This framework views psychiatric disorders as similar to medical disorders, using criteria for diagnosis as identifiable clusters of occurrences from a restricted menu of symptoms, signs, and behaviors that cause morbidity and mortality.
In contrast, patient-centered interviewing is based on the introspective model, which emphasizes the individuality of the patient's experience. This model attends to the intrapsychic battle of conflicts. It is sensitive to the patient's educational, emotional, intellectual, and social background, the personality, and the individual symptom constellations tracing their arrival to individual circumstances and the individual's unique response (cognitive-behavioral model).
SELF DIRECTING LEARNING
Basic knowledge that must be known:
1. The procedure of interviewing psychiatric disorders
2. Formulating mental status for psychiatric diagnosis
3. Management of psychiatric disorders
Udayana University Faculty of Medicine, DME 57
Study Guide Behavior Changes and Disorders
Modul
BASIC CLINICAL SKILL
INTERVIEW ANXIETY PATIENTS
AIMS:
Perform ability to collect specific, detailed information about topics constitute the anxiety patients evaluation. Acquiring the database of information for the interviewer to make diagnoses on five axes and develop a treatment plan acceptable to the patient.
LEARNING OUTCOMES:
Able how to:
1. Warm-up and Chief Complaint
2. Make the Diagnostic Decision Loop
3. Make history and Database
4. Make diagnosing and Feedback
5. Make treatment Plan and Prognosis
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of anxiety patients
3. Mental state examination of anxiety patients
4. Healing formulation of anxiety patients
5. Modality Treatment of anxiety patients
ABSTRACTS
Anxiety disorders are the most prevalent mental disorders in the general population.
Approximately one in four adults in the U.S. population has an anxiety disorder at some point in his or her life. Similar to adults, anxiety disorders are the most common mental disorder in children and adolescents. However, the rates of specific childhood anxiety disorders suggest the importance of brain development in the phenotypic expression of anxiety proneness. This is reflected by the findings of prospective community-based investigations revealing differential peak periods of onset of specific anxiety disorders: separation anxiety disorder and specific phobias in middle childhood, overanxious disorder in late childhood, social anxiety disorder in middle adolescence, panic disorder in late adolescence, generalized anxiety disorder in young adulthood and obsessive-compulsive disorder (OCD) in early adulthood. Gender differences in rates appear by 6 years of age when girls are significantly more likely to have an anxiety disorder than boys.
Psychodynamic psychiatrist views anxiety as a marker of underlying psychological conflicts to be explored and resolved and a psychiatric symptom that defines the diagnostic class of anxiety disorders. Although the term anxiety has been applied to diverse phenomena in the psychoanalytical, learning-based, and neurobiological literature, in the clinical psychopathological literature, it is used to refer to the presence of fear or apprehension that is out of proportion to the context of the life situation. Hence, extreme fear or apprehension can be considered clinical anxiety if it is developmentally inappropriate
(i.e., fear of separation in a 12-year-old child) or inappropriate to an individual's life circumstances (i.e., a successful banker worrying about supporting his or her family). Since the 1970s, clinical research has led to a progressive refinement of the nosology for clinical anxiety disorders. Although these disorders were broadly conceptualized in the early 20th century, narrower definitions have arisen, partially stimulated by Donald Klein's observations on pharmacological distinctions between panic and nonpanic anxiety.
Udayana University Faculty of Medicine, DME 58
Study Guide Behavior Changes and Disorders
Modul
BASIC CLINICAL SKILL
INTERVIEW DEPRESSIVE PATIENTS
AIMS:
Perform ability to collect specific, detailed information about topics constitute the depressive patients evaluation. Acquiring the database of information for the interviewer to make diagnoses on five axes and develop a treatment plan acceptable to the patient.
LEARNING OUTCOMES:
Able how to:
1. Warm-up and Chief Complaint
2. Make the Diagnostic Decision Loop
3. Make history and Database
4. Make diagnosing and Feedback
5. Make treatment Plan and Prognosis
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of depressive patients
3. Mental state examination of depressive patients
4. Healing formulation of depressive patients
5. Modality Treatment of depressive patients
ABSTRACTS
Severely depressed patients may also have difficulty concentrating, thinking clearly, and speaking spontaneously. The intensity of mood disturbance can seem all-consuming and may well lead to distortions in thinking and perception. Some depressed patients have psychotic symptoms in addition to cognitive difficulties. The psychiatrist evaluating a depressed patient may need to be more forceful and directive than usual. It sometimes seems that the examiner must provide all the emotional and intellectual energy for both participants. Although depressed patients should not be badgered, long silences are seldom useful, and the examiner may need to repeat questions more than once. Ruminative patients —for example, those who continually repeat how worthless or guilty they are—need to be interrupted and redirected.
All patients must be asked about suicidal thoughts; however, depressed patients may need to be questioned more fully. A thorough assessment of suicide potential addresses intent, plans, means, and perceived consequences, as well as history of attempts and family history of suicide. Many patients mention their thoughts of suicide spontaneously. If not, the examiner can begin with a somewhat general question, such as
“Do you ever have thoughts of hurting yourself?” or “Does it ever seem that life Isn't worth living?” These questions can then be followed up with more specific questions. The examiner must feel comfortable enough to ask simple, straightforward, noneuphemistic questions. Asking about suicide does not increase the risk. The psychiatrist is not raising a topic that the patient has not already contemplated. Specific, detailed questions are essential for prevention.
Udayana University Faculty of Medicine, DME 59
Study Guide Behavior Changes and Disorders
Modul
BASIC CLINICAL SKILL
INTERVIEW SOMATOFORM PATIENTS
AIMS:
Perform ability to collect specific, detailed information about topics constitute the somatoform patients evaluation. Acquiring the database of information for the interviewer to make diagnoses on five axes and develop a treatment plan acceptable to the patient.
LEARNING OUTCOMES:
Able how to:
1. Warm-up and Chief Complaint
2. Make the Diagnostic Decision Loop
3. Make history and Database
4. Make diagnosing and Feedback
5. Make treatment Plan and Prognosis
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of somatoform patients
3. Mental state examination of somatoform patients
4. Healing formulation of somatoform patients
5. Modality Treatment of somatoform patients
ABSTRACTS
Some patients experience and describe emotional distress in terms of physical symptoms.
This is certainly true for the group of somatoform disorders, but it also occurs in some mood and anxiety disorders and adjustment disorders and as a component of personality style or personality disorder. Somatizing patients pose a number of difficulties for the consulting and the treating psychiatrist. They are often referred by an internist or primary care physician, and the referral itself may be experienced as dismissive. Somatizing patients may be reluctant to engage in self-reflection and psychological exploration. Moreover, somatic distress without physical findings can lead to diagnostic uncertainty, which, in turn, makes treatment less certain. Antidepressant or anxiolytic medications may be helpful, but side effects are often less tolerable to individuals who are already highly attuned to small changes in body sensations.
Many somatizing patients live with the fear that their symptoms are not taken seriously and the parallel fear that something medically serious may be overlooked.
Psychiatrists' main task in dealing with these patients is to acknowledge the suffering conveyed by the symptoms without necessarily accepting the patient's explanation for the symptoms. Clinicians should be curious about not only the nature of the physical complaints, but also the impact of those complaints on the patient's life (e.g., “It must be very difficult to keep on working with such severe headaches,” or “It sounds as though your illness has crowded everything else out of your life.”).
It is essential that somatizing patients feel that their physical complaints are not being dismissed. Rather than limiting the scope of inquiry to psychological issues, the psychiatrist wants to expand discussion to include all aspects of the patient's well-being, emotional health, and physical health. Many patients become more willing to discuss personal issues, such as job-related stress or relationship difficulties, when they believe the
Udayana University Faculty of Medicine, DME 60
Study Guide Behavior Changes and Disorders psychiatrist will not automatically assume that those issues are the cause of physical symptoms. It is often helpful for the physician to propose a purely pragmatic approach —one that stresses a willingness to use whatever works to relieve the patient's suffering without causing harm. At times, this may include nonstandard approaches, such as meditation, yoga, or acupuncture, in addition to psychotherapy.
Udayana University Faculty of Medicine, DME 61
Study Guide Behavior Changes and Disorders
Modul
BASIC CLINICAL SKILL
INTERVIEW BIPOLAR DISORDERS PATIENTS
AIMS:
Perform ability to collect specific, detailed information about topics constitute the bipolar disorders patients evaluation. Acquiring the database of information for the interviewer to make diagnoses on five axes and develop a treatment plan acceptable to the patient.
LEARNING OUTCOMES:
Able how to:
1. Warm-up and Chief Complaint
2. Make the Diagnostic Decision Loop
3. Make history and Database
4. Make diagnosing and Feedback
5. Make treatment Plan and Prognosis
CURRICULUM CONTENTS:
1. Anamnesis
2. History taking (fundamental four and secret seven) of bipolar disorders patients
3. Mental state examination of bipolar disorders patients
4. Healing formulation of bipolar disorders patients
5. Modality Treatment of bipolar disorders patients
ABSTRACTS
Bipolar disorders (previously called manic-depressive psychosis) consist of at least one hypomanic, manic, or mixed episode. Mixed episodes represent a simultaneous mixture of depressive and manic or hypomanic manifestations. Although a minority of patients experience only manic episodes, most bipolar disorder patients experience episodes of both polarity. Manias predominate in men, depression and mixed states in women. The bipolar disorders were classically described as psychotic mood disorders with both manic and major depressive episodes (now termed bipolar I disorder), but recent clinical studies have shown the existence of a spectrum of ambulatory depressive states that alternate with milder, short-lived periods of hypomania rather than full-blown mania (bipolar II disorder).
Bipolar II disorder, which is not always easily discernible from recurrent major depressive disorder, illustrates the need for more research to elucidate the relation between bipolar disorder and major depressive disorder.
The past decade has seen major paradigm shifts in the treatment of bipolar disorder —acute to maintenance treatment, focus on the illness rather than episodes, and a focus on “functional recovery” rather than mere “syndromal recovery.” These three shifts form the core principles in the long-term management of bipolar illness. They have occurred because of a realization of 1) the chronic nature of the illness, interspersed by “crises” involving acute episodes of mania, depression, and mixed states that are similar to the hypertensive crises seen in hypertension; and because of 2) a lag in improvement of sociooccupational functioning among patients despite symptomatic recovery. Maintenance treatment of bipolar disorder is best accomplished with an approach that combines pharmacological and psychosocial interventions. Pharmacotherapy involves using medications that, alone or in combination, prevent the occurrence of new episodes; facilitate socio-occupational functioning by minimizing the number and intensity of interepisode symp
Udayana University Faculty of Medicine, DME 62
Study Guide Behavior Changes and Disorders toms; and are devoid of intolerable side effects, thus facilitating long-term compliance with the medication regimen. Remission of symptoms and more importantly “functional recovery”—the primary goals of treatment—are attainable despite the complex and chronic nature of bipolar disorder.
STEM QUESTIONS
Euphoria Stem Question
1. Some people have periods lasting several days when they feel much more excited and full of energy than usual. Their minds go too fast. They talk a lot. They are very restless or unable to sit still and they sometimes do things that are unusual for them, such as driving too fast or spending too much money.
Have you ever had a period like this lasting several days or longer?
If this question is endorsed, the next question (the irritability stem question) is skipped and the respondent goes directly to the Criterion B screening question
Irritability Stem Question
2. Have you ever had a period lasting several days or longer when most of the time you were so irritable or grouchy that you either started arguments, shouted at people or hit people?
Criterion B Screening Question
3. People who have episodes like this often have changes in their thinking and behavior at the same time, like being more talkative, needing very little sleep, being very restless, going on buying sprees, and behaving in many ways they would normally think inappropriate.
Did you ever have any of these changes during your episodes of being excited and full of energy or very irritable or grouchy?
Criterion B Symptom Questions
Think of an episode when you had the largest number of changes like these at the same time. During that episode, which of the following changes did you experience?
1. Were you so irritable that you started arguments, shouted at people, or hit people?
This first symptom question is asked only if the euphoria stem question (#1 above) is endorsed
2. Did you become so restless or fidgety that you paced up and down or couldn’t stand still?
3. Did you do anything else that wasn’t usual for you—like talking about things you would normally keep private, or acting in ways that you would usually find embarrassing?
4. Did you try to do things that were impossible to do, like taking on large amounts of work?
5. Did you constantly keep changing your plans or activities?
6. Did you find it hard to keep your mind on what you were doing?
7. Did your thoughts seem to jump from one thing to another or race through your head so fast you couldn’t keep track of them?
8. Did you sleep far less than usual and still not get tired or sleepy?
9. Did you spend so much more money than usual that it caused you to have financial trouble?
Udayana University Faculty of Medicine, DME 63
Study Guide Behavior Changes and Disorders
Smstr
10
9
8
7
6
5
4
3
2
1
~ CURRICULUM MAP ~
Program or curriculum blocks
Senior Clerkship
Senior Clerkship
Senior clerkship
Medical
Emergency
(3 weeks)
BCS (1 weeks)
The Respiratory
System and
Disorders
(4 weeks)
BCS (1 weeks)
Elective Study II
(1 weeks)
Special Topic:
-Travel medicine
(2 weeks)
The Cardiovascular
System and
Disorders
(4 weeks)
BCS (1 weeks)
Alimentary
& hepato- biliary systems
& disorders
(4 Weeks)
BCS (1 weeks)
Elective Study III
(6 weeks)
The Urinary System and Disorders
(3 weeks)
BCS (1 weeks)
The Endocrine
System, Metabolism and Disorders
(4 weeks)
BCS (1 weeks)
Clinic Orientation
(Clerkship)
(6 weeks)
Musculoskeletal Neuroscience system & connective and neurological tissue disorders
(4 weeks)
BCS (1 weeks) disorders
(4 weeks)
BCS (1 weeks)
Hematologic system & disor- ders & clinical oncology
(4 weeks)
BCS (1 weeks)
Immune system & disorders
(2 weeks)
BCS(1 weeks)
Medical
Professionalism
(2 weeks)
BCS (1 weeks)
Studium
Generale and
Humaniora
(3 weeks)
Evidence-based
Medical Practice
(2 weeks)
Medical communication
(3 weeks)
BCS (1 weeks)
Behavior Change and disorders
(4 weeks)
BCS(1 weeks)
Infection
& infectious diseases
(5 weeks)
BCS (1 weeks)
Health System-based
Practice
(3 weeks)
BCS (1 weeks)
The cell as bioche- mical machinery
(3 weeks)
BCS(1 weeks)
Growth
& development
(4 weeks)
BCS: (1 weeks)
Pendidikan Pancasila & Kewarganegaraan (3 weeks)
The Reproductive
System and Disorders
(3 weeks)
BCS (1 weeks)
Clinical Nutrition and
Disorders
(2 weeks)
BCS (1 weeks)
Special Topic :
- Palliative medicine
-Compleme ntary &
Alternative
Medicine
- Forensic
(3 weeks)
The Visual system & disorders
(2 weeks)
BCS
(1 weeks)
The skin & hearing system
& disorders
(3 weeks)
BCS(1 weeks)
Community-based practice
(4 weeks)
Special Topic
- - Ergonomi
- - Geriatri
(2 weeks)
Elective
Study II
(1 weeks)
Elective
Study I
(2 weeks)
Udayana University Faculty of Medicine, DME 64
Study Guide Behavior Changes and Disorders
References
1. Psychiatry. 4 th ed. John Wiley & Sons, 2015.
2. Katzung: Basic and Clinical Pharmacology, 13 th ed. McGrawHill’s. 2015
3. Neurosciences-From Molecule to Behavior: A University Textbook. Springer Spektrum,
2013
4. Diagnostic and statistical manual of disorders, 5 th ed, Arlington: American Psychiatric
Association, 2013.
5. Child and adolescent psychiatry. 3 rd ed. John Wiley & Sons, 2012
6. Textbook of Clinical Neuropsychiatry, 3 rd ed, Taylor & Francis Group, 2012
7. Abnormal Psychology. 6 th ed. McGrawHill’s, 2010
8. The American Psychiatric Publishing Textbook of Forensic Psychiatry. 2 nd ed. American
Psychiatry Pub. 2010
9. Principles of social psychiatry. 2 nd ed. John Wiley & Sons, 2010
10. Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10 th ed. Lippincott Williams & Wilkins. 2007.
11. Diagnostic Criteria from DSM IV-TR. 1 st ed. Washington: American Psychiatric
Association. 2000
12. Catatan Ilmu Kedokteran Jiwa. Edisi VI. Surabaya: Airlangga University Press. 1994.
13. ICD-10 Classification Or Mental and Behavioural Disorders. 1 st ed. Edinburgh;
Churchill Livingstone.1994
14.
Pedoman Penggolongan dan Diagnosis Gangguan Jiwa di Indonesia III. Edisi I. Jakarta:
Departemen Kesehatan. 1993
Udayana University Faculty of Medicine, DME 65