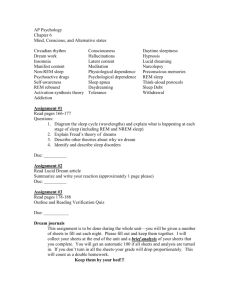
Stages of sleep (Updated 10
advertisement

Quick and Dirty Summary of Sleep (as much as Dean Beebe could fit on a page in 10/2004) Stages of Sleep Sleep staging is done via an overnight sleep study or polysomnogram (PSG) that includes, at a minimum, EEG, an electrooculogram (looking at eye movement), and an electromyelogram (looking at skeletal muscle movement, usually on chin). Most PSGs have additional leads to examine limb movement and respiration. There are 4 non-REM stages, plus REM: Wake: On EEG, predominantly low amplitude, relatively fast alpha activity (8-13 waves/sec) during relaxation or mixed alpha and beta activity (>13 waves/sec) accompanied by fast eye activity during vigilant/alert wakefulness. NREM: Very light sleep. EEG slows down, but remains low amplitude. Theta waves appear (medium amplitude, 4-7 waves/sec). Stage 1 is usually brief, and is a transition between wakefulness and Stage 2. Stage 2 NREM: Light sleep. EEG continues to show predominantly theta activity, with the introduction of K-complexes (left picture) and brief bursts of beta activity called sleep spindles (right picture). Stage 3 NREM: Deepening sleep. EEG showing increasing high amplitude, low frequency delta waves (< 4 waves/sec). Stages 3 and 4 are often called slow wave sleep. Stage 3 is usually brief, and is a transition between 2 & 4. Stage 4 NREM: Deep sleep. Delta waves predominate. Parasomnias (sleepwalking, night terrors) occur in Stage 3 or 4. REM: Rapid eye movement sleep, sometimes called “paradoxical sleep” because the EEG looks like wakefulness (quick, mixed frequency, low amplitude) but the person is asleep. Can be distinguished from wakefulness by evidence of rapid eye movements and very low skeletal muscle tone. Most dreaming (and nightmares) occur during REM. Other info about sleep stages: An Example of the Sleep Stages of a 12-year-old Muscle tone & activity is greatest in wakefulness, declines in stages 1-4, and lowest during REM With age, slow-wave and REM sleep diminishes, leaving mostly light sleep In a healthy young adult, slow-wave sleep occurs mostly during the first ½ of the night, REM mostly during the second ½. Most of sleep is spent in stage 2 (about 50%), REM (about 25%), or Stage 4 (about 10-15%). Important points for neuropsychologists: Adequate sleep quantity and quality are essential for daytime functioning, with the most marked effects of poor sleep seen in sustained attention/vigilance, coordination, and emotion regulation. There can also be effects on memory retrieval and aspects of executive functioning (EF). Sleep generation and regulation is dependent on a broad system that includes the brainstem through the diencephalon and limbic system. Any neurological condition or injury that affects a portion of this system can impact sleep. Dementing conditions are often accompanied by sleep disturbances, as is Parkinson’s Disease. Many psychotropic meds can affect sleep. If sleep is a complaint, consider whether meds are contributing. Sleep is particularly important in the epilepsies, as sleep deprivation can promote seizures, and seizures can occur during sleep (in some cases, sleep is the time they occur most). The sleep-wake cycle is influenced by two processes: (1) time spent awake relative to time recently spent asleep, and (2) the circadian rhythm…for example, core body temp is usually lowest at 2-4 am, highest in late afternoon. There are over 80 different sleep disorders. Two of the most important to know as a neuropsychologist are: o Narcolepsy: Misalignment of the various aspects of sleep. For example, aspects of REM can intrude into wakefulness during cataplexy (sudden loss of muscle tone during wakefulness, often when excited) or occur right around sleep onset or offset (hypnagogic and hypnopompic hallucinations, sleep paralysis in which person is awake but unable to move). There is also excessive daytime sleepiness, which is treated with stimulants. o Obstructive Sleep Apnea: Repetitive obstruction and/or collapse of the airway during sleep, especially seen during REM sleep, conventionally defined as occurring > 10 times/hour in adults or >5 times/hour in children. Results in frequent brief arousals and intermittent hypoxia, daytime sleepiness, poor daytime vigilance, motor uncoordination, depression, and ADHD symptoms in young kids. May cause memory and EF deficits, too. THE FINE PRINT: Caveat emptor! These study materials have helped many people who have successfully completed the ABCN board certification process, but there is no guarantee that they will work for you. The notes’ authors, web site host, and everyone else involved in the creation and distribution of these study notes make no promises as to the complete accuracy of the material, and invite you to suggest changes.