NURSING CARE PREPARATION
advertisement
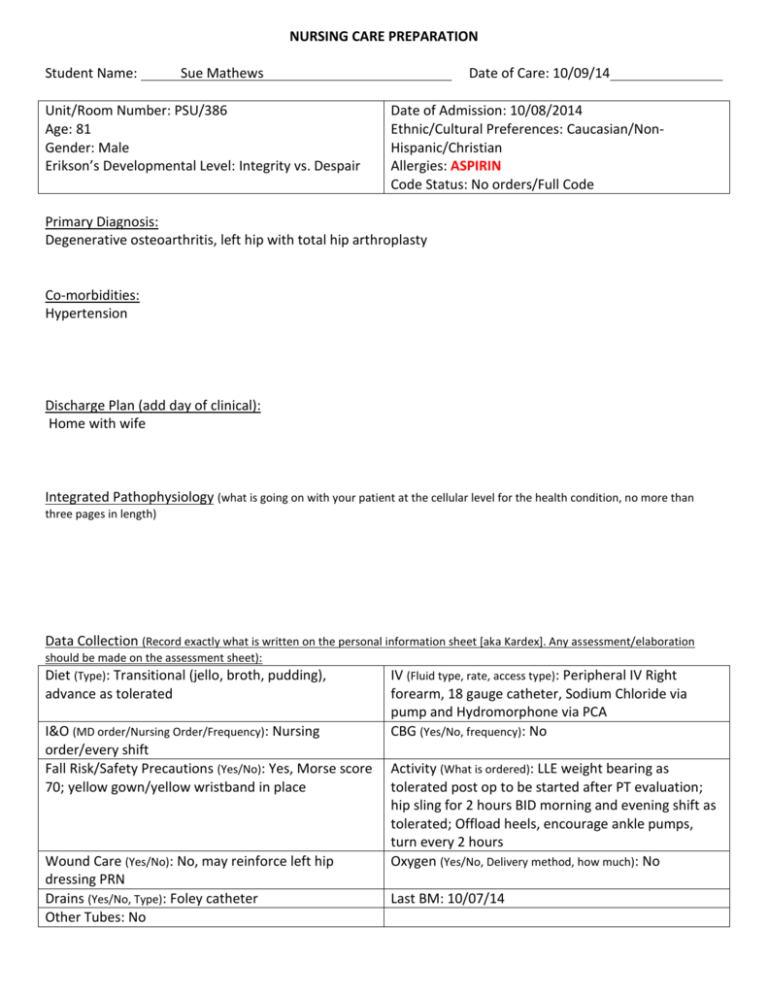
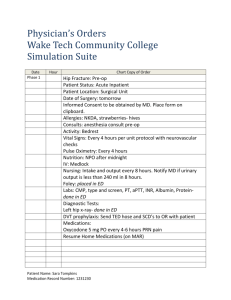
NURSING CARE PREPARATION Student Name: Sue Mathews Unit/Room Number: PSU/386 Age: 81 Gender: Male Erikson’s Developmental Level: Integrity vs. Despair Date of Care: 10/09/14 Date of Admission: 10/08/2014 Ethnic/Cultural Preferences: Caucasian/NonHispanic/Christian Allergies: ASPIRIN Code Status: No orders/Full Code Primary Diagnosis: Degenerative osteoarthritis, left hip with total hip arthroplasty Co-morbidities: Hypertension Discharge Plan (add day of clinical): Home with wife Integrated Pathophysiology (what is going on with your patient at the cellular level for the health condition, no more than three pages in length) Data Collection (Record exactly what is written on the personal information sheet [aka Kardex]. Any assessment/elaboration should be made on the assessment sheet): Diet (Type): Transitional (jello, broth, pudding), advance as tolerated I&O (MD order/Nursing Order/Frequency): Nursing order/every shift Fall Risk/Safety Precautions (Yes/No): Yes, Morse score 70; yellow gown/yellow wristband in place Wound Care (Yes/No): No, may reinforce left hip dressing PRN Drains (Yes/No, Type): Foley catheter Other Tubes: No IV (Fluid type, rate, access type): Peripheral IV Right forearm, 18 gauge catheter, Sodium Chloride via pump and Hydromorphone via PCA CBG (Yes/No, frequency): No Activity (What is ordered): LLE weight bearing as tolerated post op to be started after PT evaluation; hip sling for 2 hours BID morning and evening shift as tolerated; Offload heels, encourage ankle pumps, turn every 2 hours Oxygen (Yes/No, Delivery method, how much): No Last BM: 10/07/14 ASSESSMENTS (Include Subjective & Objective Data) Integumentary: skin is warm, dry, tan no clubbing or discoloration of nails, nail bed pale; oral mucosa is pink, moist, without lesions or tenderness; dressing of the incision was found to have shadowing but was not increasing or coming through Head and Neck: neck is soft without lumps, lesions, or bruising hair distribution even; facial features symmetrical Ear/Nose/Throat: facial movement is symmetrical and expressions appropriate without drooping of mouth, eyes, or eyelids; nares are patent with no reported tenderness; no drainage, redness, or irritation noted Sclera white with minimal appearance of blood vessels; conjunctiva pink and moist Thorax/Lungs: Lungs clear in all lobes; skin is warm, smooth, dry respirations regular in depth Cardiac: no JVD; capillary refill less than 3 seconds; pedal pulses equal palpable and strong; radial pulses consistent with apical pulse regularly irregular rhythm; S1, S2 noted Musculoskeletal: BLE 2-3 BUE 4 able to lift feet against resistance, and push against resistance; decreased muscle tone noted bilateral lower extremities; no loss of balance noted on ambulation with front wheeled walker; no decrease in length of lower or upper extremities Genitourinary: urine yellow clear, with no foul odor, without discomfort on urination (catheter D/C’d early 10/9/14 prior to beginning of shift) Gastrointestinal: Bowel sounds in all 4 quadrants, no distention or tenderness noted; no discoloration; umbilicus midline; patient reports passing flatus; last BM 10/7/14; abdomen is soft warm Other (Include vital signs, weight): Ht: 74 inches Wt: 82 kg BP: 148/72 P: 96 SpO2: 95% R: 18 T: 100.3 F Pain: 5/10 Neurological: A&O x 3; answers appropriately; cranial nerves intact; jaw movement intact; affect appropriate; patient cooperative; no anxiety noted CURRENT MEDICATIONS List ALL regularly scheduled and prn medications scheduled on your client. (Due morning of clinical) Generic & Trade Name Classification Dose/Route/ Rate if IV Onset/Peak Intended Action/Therapeutic use. Why is this client taking med? Adverse reactions (1 major side effect) Nursing Implications for this client. (No more than one) Rivaroxaban (Xarelto) Anticoagulant; Antithrombotic; Selective Factor XA inhibitor 10 mg/1 tab PO; start on 10/09/14 09:00 P: 2-4 H VTE Prophylaxis Monitor VS closely for S/Sx of bleeding/internal hemorrhage (epidural, intracranial) such as significant drop in BP or H&H Terazosin (Hytrin) Alpha-Adrenergic Receptor Antagonist; Antihypertensive Bile Acid; Gallstone Solubilizing agent Stimulant Laxative 2mg/1 cap PO QHS; start 10/08/14 21:00 P: 1-2 H Hypertension Bleeding complications (especially after surgery and spinal anesthesia) Syncope 300 mg/1 cap PO BID; start 10/08/14 21:00 8.6/50 2 tab PO BID; start on 10/08/14 20:00 P: 1-3 H Gallstone Prevention Peptic Ulcer O: 6-10 H May take up to 24 H Bowel regulation Excessive fluid loss Monitor BP prior to administration for effectiveness; teach patient regarding postural drop in BP; monitor position changes for safety Monitor for onset of GI distress/bleeding (nausea, severe pain, dark stools) Maintain fluid balance and hold if watery diarrhea develops Ursodiol (Actigal) Senna/ Docusate (Senokot-S) Metoprolol Succinate- XL (Toprol Metoprolol Succinate-XL) Cardioselective Beta-adrenergic antagonist antihypertensive 100 mg/1 tab PO QPM P: 1.5 H Hypertension Shortness of breath, bradycardia Do not give if HR less than 50, and/or SBP less than 90; Notify physician Monitor for respiratory distress Acetaminoph en IV Non-narcotic analgesic 100mL IV Q 6 H for 3 doses; MAX 4 GM IV per day; start 10/08/14 18:00; NO OTHER Acetaminophen while on IV P: 0.5-2 H Pain Hepatotoxicity with chronic use Monitor for abdominal pain, diarrhea, elevation of ALT, AST Acetaminophen Cefazolin/D5 W Duplex 1gm (Ancef/D5W Duplex 1 gm) 1st Generation Cephalosporin antibiotic Ascorbic Acid (Vitamin C) Vitamin supplement Multivitamin (Theragran) 50 mL IV Q 8 H for 2 doses start 8 H after Operative dose; must be complete within 24 hours 1000mg/2 tab PO daily 18:00; start on 10/08/14 18:00 P: 5 min IV Prophylactic against infection peri-operatively Renal insufficiency Monitor for onset of severe diarrhea associated with colitis/monitor renal output and BUN Readily absorbed PO Dysuria Monitor for salicylate toxicity- Ascorbic acid may decrease elimination of salicylates and can also reduce effect of anticoagulant Multivitamin 1 tab PO daily 18:00 Unknown Increases protective mechanism of immune systemsupporting healing Vitamin supplement Vitamin/mineral overload/ overdose Finasteride (Proscar) Antiandrogen; 5= Alpha reductase inhibitor 5mg/1 tab PO daily O: 3-6 H Benign prostatic hypertrophy Postural hypotension Saline Flush (Sodium Chloride Flush) FS-Dextrose 5%-Lactated Ringers 1052 ml bag FS-Sodium Chloride 0.9% 541 ml bag Saline Flush 2 mL IV Q shift flush with 2-5ml ; saline lock when PO tolerated IV @ 125mL/hour over 8.5 H N/A IV patency Redness/ irritation N/A Fluid loss replacement and maintenance Fluid volume excess Monitor for signs of hypervitaminosisexcessive itching, dry skin, nausea, vomiting, hives, sore mouth, foul taste, skin discoloration, flushing Monitor position changes and ambulation for signs of hypotensiondizziness, increased pulse, sweating, balance Flush IV line every shift and as needed before and after accessing IV; monitor for signs of irritation, blockage, infiltration Monitor I/O, weight, and signs of fluid excess ( constant irritated cough, dyspnea, vein engorgement) IV @ 22mL/hour over 24.5 H TKO with PCA if no other maintenance IV N/A Fluid loss replacement and maintenance Fluid volume excess Isotonic Crystalloid Fluid Isotonic Crystalloid fluid Monitor I/O, weight, and signs of fluid excess ( constant irritated cough, dyspnea, vein engorgement) fluid is running Mupirocin 2% Ointmentnasal (Bactroban 2% ointmentnasal) Magnesium Hydroxide (Milk of Magnesia) Pseudomonic acid antibiotic 1 gm nasal bid for 4 days Not systemically absorbed Infection Contact dermatitis Hold drug and notify physician if dermatitis or pus production increases Saline Cathartic; antacid 30 ml PO daily PRN constipation, if no BM by End of Post op day 3, start on 10/11/14 1 enema rectal daily PRN constipation if MOM ineffective and no BM by end of Post op day 3 1 suppository rectal daily PRN constipation if MOM ineffective O: 3-6 H Constipation Bradycardia Unknown Constipation Abdominal pain Monitor for Hypermagnesemia (profound thirst, flushing, sedation, confusion, depressed deep tendon reflexes, hypotension, depressed respirations) Assess bowel sounds prior to administration- do no use if obstructed O: 15-60 min Constipation Cramping O: 2 min Reversal of narcotic depression (sedation, respiratory depression, hypotension) Tachycardia, Hypertension Phosphates enema (Fleet enema) Stimulant Saline laxative Bisacodyl (Dulcolax, Bisac-Evac) Stimulant laxative Naloxone 1mg/1ml (Narcan 1mg/ml) Opiate antagonist narcotic 0.1 mg dose IV titrate PRN unable to arouse/resp rate; dilute Naloxone 2mg/2ml w/8ml NS to yield 10ml *conc: 0.2mg/ml* give 0.1mg Q 2-3 min until resp rate greater than 8 or Ensure adequate fluid intake 6-8 glasses/day unless fluid restriction; antacids will cause early dissolution of enteric coating- resulting in increased abdominal cramping (teach) Watch patient closely as some opiates may have longer duration of action than Naloxone’s; watch for changes in respiration Oxycodone immediate release (Roxicodone Immediate release) Ondansetron (Zofran) Opiate Analgesic Antiemetic Metaxalone (Skelaxin) arousable; may repeat x 3 per 24 hour; monitor Q 15 min for at least 2 hours 5 mg/1 tab PO Q 4 H PRN pain for 1 day; STOP order after 24 hours O: 10-15 min Pain management Respiratory depression Monitor response closely for pain relief; do not give if respirations less than 12; have Narcan readily available 4mg/2ml IV Q 4 H PRN P: 1-1.5 H Nausea Diarrhea, sedation Give over 2-3 minutes IV; monitor tachycardia Skeletal muscle relaxant 800 mg/1 tab PO Q 8 H PRN O: 3 H Muscle Spasm Anaphylaxis Hydromorph one/NS 0.2mg/ml Narcotic analgesic (opiate agonist) O: 15 min Pain management Respiratory depression Zolpidem (Ambien) Anxiolytic; sedative hypnotic, nonbenzodiazepine Anesthetic; antianxiety; sedative-hypnotic short acting PCA; Demand: 0.2 mg every 10 min; limit: 3mg/4 HRS; Loading dose= 0.2 mg IV PRN Pain for 4 days; May increase PCA dose by 0.1 mg every 30 minutes up to max dose of 0.4mg per injection 5mg/1 tab PO HS PRN for 7 days Monitor for allergic reaction ( rash around chest and neck, SOB, itching, tachycardia) Document # of mg infused every shift; monitor baseline respiratory rate; hold if respiratory rate less than 12; watch for signs of miosis (abnormal constriction of pupils) O: 7-27 min Insomnia Confusion/falls O: 1-5 min IV Preoperative sedation/anxiety Tachypnea Midazolam (Versed) 1mg/1ml IV x 2 PRN Preop- may repeat 1mg dose one time PRN Give directly before sleep to avoid impaired cognition/risk for falls; assess for vision changes and report to provider if present Monitor injection site continuously for signs of extravasation; monitor respirations for changes in rhythm depth, effort, as well as signs of benzodiazepine Oxycodone/ APAP Opiate analgesic Oxycodone/ APAP Opiate analgesic Acetaminoph en (Tylenol) Non-narcotic analgesic continued confusion 5/325 1 tab PO Q 4 H x 1 day Delay start x 24 HR while on Acetaminophen IV. Around the clock. Change to PRN Post op day 2 Start on 10/09/2014 10/325 1 tab PO Q 4H for 1 day, delay start while on Acetaminophen IV. Around the clock until post op day 2, then PRN Start on 10/09/14 14:00 650 2 tab PO Q 4H for 1 day, delay start while on Acetaminophen IV around the clock post op day 2, then PRN Start on 10/09/14 14:00 O: 10-15 min Pain Level 4-6 Sedation Monitor/assist with ambulation; monitor respiratory status frequently; monitor pain level/ relief; assess for bowel elimination O: 10-15 min Pain Level 7-10 Sedation Monitor/assist with ambulation; monitor respiratory status frequently; monitor pain level/ relief; assess for bowel elimination P: 0.5-2 H Pain Level 1-3 Hepatotoxicity with chronic use Monitor for abdominal pain, diarrhea, elevation of ALT, AST DIAGNOSTIC TESTING Include pertinent labs [ABGs, INRs, cultures, etc] & other diagnostic reports [X-rays, CT, MRI, U/S, etc.] NOTE: Adult values indicated. If client is newborn or elder, normal value range may be different. Date Lab Test Normal Values 10/09/14 Sodium 135 – 145 mEq/L Potassium 3.5 – 5.0 mEq/L Chloride 97-107 mEq/L Co2 23-29 mEq/L Glucose 75 – 110 mg/dL BUN 8-21 mg/dL Creatinine 0.5 – 1.2 mg/dL Uric Acid Plasma 4.4-7.6 mg/dL Calcium 8.2-10.2 mg/dL Phosphorus 2.5-4.5 mg/dL Total Bilirubin 0.3-1.2 mg/dL Total Protein 6.0-8.0 gm/dL Albumin 3.4-4.8gm/dL Cholesterol <200-240 mg/dL Alk Phos 25-142 IU/L SGOT or AST 10 – 48 IU/L LDH 70-185 IU/L CPK 38-174 IU/L WBC 4.5 – 11.0 RBC 10/09/14 HGB 10/09/14 HCT male: 43-49% female: 38-44% MCV 85-95 fL MCH 28 – 32 Pg MCHC 33-35 g/dL RDW 11.6-14.8% Platelet 150-450 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 Patient Values/ Date of care Interpretation as related to Pathophysiology –cite reference & pg # male: 4.7-5.14 x 10 female: 4.2-4.87 x 10 male: 12.6-17.4 g/dL female: 11.7-16.1 g/dL DIAGNOSTIC TESTING Date 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 UA Interpretation as related to Pathophysiology –cite reference & pg # N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A Normal Range Results Interpretation as related to Pathophysiology –cite reference & pg # N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A Color/Appearance pH Spec Gravity Protein Glucose Ketones Blood Date Other (PT, PTT, INR, ABG’s, Cultures, etc) 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 10/09/14 Date Results Normal Range N/A N/A N/A N/A N/A N/A N/A N/A Radiology 10/08/14 X-Rays 10/09/14 Scans 10/09/14 EKG-12 lead 10/09/14 Telemetry Results Interpretation as related to Pathophysiology –cite reference & pg # Hip 1 view left Well aligned unipolar left hip prosthesis without suspicious lytic or sclerotic bone lesions; soft tissue swelling and surgical staples consistent with immediate postoperative status N/A N/A N/A N/A N/A N/A DAR NURSING PROGRESS NOTE Include the same note that was written in the client record for the priority nursing diagnostic statement. Include the date/time/signature. 10/9/14 17:05 Grimacing, guarding, moaning with movement, increased irritability. Rates pain at 7 on 0-10 pain scale. Administered oxycodone/apap 10/325 per pain scale (see MAK). Able to swallow PO medication without incident, Pt reports no further needs at this time, call light in reach, door closed per patient request 10/9/14 17:34 Pt reports pain at 2-3 on 0-10 pain scale, verbalizes satisfaction with pain control, medication effectiveness documented (see MAK), no further needs reported, call light on bed, PCA pump control on bed; door closed per patient request PATIENT CARE PLAN Patient Information: 81 y.o. male; degenerative osteoarthritis; hypertension; benign prostatic hypertrophy Nursing Diagnosis should include Nanda Nursing Diagnostic statement, related to (R/T), as evidenced by (AEB). Problem #1 Acute Pain R/T loss of integrity of bone and surrounding structures due to surgical procedure AEB patient reports pain using pain scale, demonstrates protective gestures during positioning, and sleep disruption Desired Outcome: Patient will report that pain is well-controlled at a level that is acceptable for the patient and demonstrate improved sleep pattern, and a decrease in guarding or protective behavior during positioning and patient care Nursing Interventions Client Response to Intervention 1. Assess pain and comfort level frequently to ensure 1.Pt verbalized understanding of teaching and effectiveness of therapy- teach regarding the regarding pain management, discussed his importance of round the clock management concerns regarding “getting hooked” postoperatively to maintain better control of pain 2. Provide pillows and blankets to position patient comfortably and correctly to avoid hip flexion, rotation, or dislocation, while alternating weight in bed. Utilize the help of NT to ensure fluid movement of the patient and minimize discomfort 2.Pt was refusing wedge at beginning of shift and continued to refuse wedge throughout shift, he declines hip sling, and was able to reposition self in bed, alternating weight. 3. Administer pain medications as ordered- before pain level is unacceptable for patient and assess within 15-20 min after administration to ensure adequate relief is achieved- contact physician as soon as possible if pain is not adequately controlled 3.Pt verbalized needs for pain control on when I entered room; patient was able to report adequate control on reassessment Evaluation (evaluate goal & interventions, what worked/what didn’t, what would you adapt if needed): Maintained adequate control of pain as this was his priority issue, although his pain increased throughout the shift due to the patient’s increasing independence and refusal to call for help in getting in and out of bed or ambulating around the room; I think in the future in this type of intervention, I will just continue with teaching, emphasizing importance of exercising limitations but it is also important that the patient be able to have his independence as he wishes; he verbalized understanding the risks for falls, incisional dehiscence, and trauma; I could be more “aggressive” with teaching and it may help to have another nurse with me just to help emphasize importance to the patient, but not make them feel patronized Problem #2 Risk for Injury R/T decreased mobility, invasive procedure, and decreased perfusion AEB immobilization of left leg/hip, limited activity, and inability to reposition independently in bed Desired Outcome: Patient will demonstrate adequate perfusion of tissues, be free from development of infection or further impairment of the skin AEB intact skin (not including surgical site), will maintain clean dry dressing over incision Nursing Interventions Client Response to Intervention 1. Assess and monitor patient’s skin especially on the 1.Patient was able to reposition self but allowed back and heels at least every 2 hours with SN to assess heels each time pain/safety positioning checks/rounding were done 2. Continue to monitor circulation of all extremities, sensation, and movement- watch for signs of swelling, irritation, redness, or pain; ensure asceptic technique with all patient care especially of catheter and IV site 2.IV remained intact, noted slight elevation of skin proximal to the sorbaview dressing of the IV and increased blood from insertion around IV cannula; patient reported no pain, warm, or irritation, and none noted on all aspects of the forearm, hand and up the arm 3. Assess V.S. at least every 4 hours; teach patient the 3.Continued to teach incentive spirometry use; importance of incentive spirometry every 2 hours to patient reports “yes I have been using it so you prevent respiratory infection can put that in your report” Evaluation: A full skin audit was difficult to do given the independent nature of the patient and refusal for some care or assistance. Patient was very modest and it was very important to respect that and also report to the oncoming NOC nurse to protect patient’s rights; I was able to assess his back intermittently as well as the back of his legs; VS were assessed, and increasing amounts of teaching done; continued to monitor positioning, movement, and any factors of friction or pressure against the skin. Mainly though his risk for injury continues to be an issue regarding refusal for assistance. Problem #3 Potential complication of surgery: joint dislocation or displacement of prosthesis, infection, and venous thromboembolism Desired Outcome: Patient will not have dislocation or displacement of prosthesis , infection, or VTE throughout hospital admission Nursing Interventions Client Response to Intervention 1.Keep left leg slightly abducted; assess for pain and 1.Patient refused use of hip sling or wedge extremity shortening- report immediately if noted 2. Monitor appearance of dressing, note any changes in appearance, odor, swelling, or increased signs of inflammation of surrounding skin and tissue; monitor patient’s temperature, LOC, and vital signs at least every 4 hours ( or more if changes are noted) 2.shadowing noted; no odor noted; Temperature increased over shift. Reported to primary nurse and also NOC Nurse; LOC remained A&O x3; patient reported no concerns outside of pain 3.Apply sequential compression devices, teach the patient regarding the importance and encourage heel pumps; teach leg exercises as indicated by orders or PT (patient was to be evaluated 10/09/14 ~07:00 by PT, will address orders at beginning of shift); administer anticoagulant medication as prescribed- teach regarding importance and 3.SCDS used, teaching done, patient was cooperative with teaching; continually offered fluids and discussed heel pumps with patient; patient nodded with appropriate eye contact; refused to demonstrate heel pumps signs of adverse effects; encourage fluid intake Evaluation: patient was receptive to teaching, tolerating SN continued attempts at demonstration and return demonstration; again, with this patient just continued teaching and perhaps in his home environment, after he has had time to reduce ongoing pain to his tolerable level of 4 or less, he would be more interactive with teaching