Blood 1 - biologyonline.us
advertisement

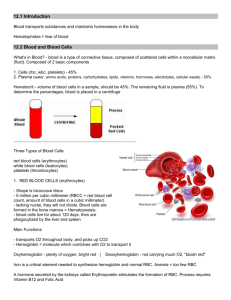
A&P 1 Blood Part 1 COMPOSITION OF BLOOD 1) fluid plasma 2) whole cells RBC, WBC 3) cell fragments platelets FUNCTIONS OF BLOOD 1) to transport 2) to regulate 3) to protect TRANSPORT food oxygen wastes hormones enzymes REGULATE pH buffers body temperature water content of cells PROTECT clotting mechanisms immune system factors FORMED ELEMENTS OF BLOOD 45% of blood cells, platelets 1) red blood cells (erythrocytes) “RBC” 2) white blood cells (leukocytes) “WBC” 3) platelets (thrombocytes) PLASMA 55% of blood fluid portion of blood 90% water, 10% solutes solutes are mostly proteins includes wastes, vitamins and nutrients BLOOD VOLUME 154 lbs= 1.5 gal of blood 8% of the total body weight blood volume varies age body type sex HEMATOCRIT describes the volume % of RBC in whole blood (PCV)- packed cell volume avg 45% hematocrit 45 ml/100 ml RBC 55 ml/100 ml plasma decreased RBC numbers= anemia elevated RBC numbers= polycythemia individuals living in high altitude blood viscosity rises elevating BP and contributing to thrombosis and hemorrhage FORMED ELEMENTS WBC, platelets account for less than 1% of the total blood volume RBC account for over 95% of the formed elements in blood RED BLOOD CELLS erythrocytes lack a nucleus, ribosomes, and mitochondria RBC perform anaerobic respiration biconcave disks shape gives a large surface area relative to its volume cumulative surface area of all RBC in the body is larger than a football field for exchange of respiratory gases able to change shape without injury primary component is a red pigment hemoglobin (1/3 of cell volume) RBC counts Male -- 5.5 million / mm3 Female -- 4.8 million / mm3 SICKLE CELL ANEMIA hereditary condition caused by formation of abnormal hemoglobin distorts the shape of RBC when blood oxygen levels are low FUNCTION OF RBC 1) transport oxygen 2) transport carbon dioxide both dependent on hemoglobin HEMOGLOBIN protein red pigment contains iron compound able to combine with oxygen to form oxyhemoglobin combines with carbon dioxide to form carbaminohemoglobin HEMOGLOBIN LEVELS 100 ml blood ===> 12-16 g hemoglobin less than 10 g/ 100 ml of hemoglobin is diagnosed as anemia CO2 TRANSPORT enzyme in RBC (carbonic anhydrase) catalyzes a reaction that joins CO2 and water CO2 + H2O ===> HCO3 (carbonic acid) carbonic acid dissolved in water forms bicarbonate ions ( HCO3-) bicarbonate ion diffuses out of the RBC and serves to transport CO 2 in the blood plasma bicarbonate ions are also important in maintaining normal blood pH levels FORMATION OF RBC erythropoiesis (hemopoieses) form in red bone marrow from hemocytoblasts nucleated stem cells maturation process requires about 4 days every minute 100 million RBC are formed if blood oxygen levels reaching the tissues is decreased the rate of RBC production increases tissue oxygen levels influence the rate of RBC production ERYTHROPOIETIN hormone which stimulates bone marrow to accelerate RBC production produced by the liver athletes have been known to use erythropoietin to improve performance RBC CLUMPING Note the clumping of red blood cells, typical of stress, health problems or fatigue Magnetic treatments???? RETICULOCYTE COUNT used to measure rate of erythropoiesis 0.5 % -1.5% of RBC are reticulocytes (newly formed RBC) counts less than 0.5% or higher than 1.5% indicate slowdown or acceleration of RBC production DESTRUCTION OF RBC life span of RBC averages 105-120 days macrophage cells in the liver and spleen phagocytose aged, abnormal or fragmented RBC breakdown causes release of amino acids, iron and pigments (bilirubin) into the bloodstream bilirubin is removed from the bloodstream by the liver liver excretes bilirubin into the intestine as bile amino acids are recycled in protein synthesis WHITE BLOOD CELLS leukocytes lack hemoglobin contain nucleus and all other cell organelles classified according to presence of granules and staining of cytoplasm Granulocytes Agranulocytes GRANULOCYTES 1) neutrophils 2) eosinophils 3) basophils AGRANULOCYTES 1) lymphocytes 2) monocytes NEUTROPHILS granules stain a light purple cytoplasm appears course nuclei has 2-6 lobes “polys” 65% of total WBC count highly mobile, active phagocytes able to migrate out of blood vessels into tissues (diapedesis) contain powerful lysosomes which destroy bacteria damaged cells release chemicals which attract neutrophils (positive chemotaxis) ex: interleukin(macrophage), histamine(basophil), CRP(liver), C3a, C5a(complement) EOSINOPHILS large, numerous cytoplasmic granules nuclei has 2 lobes 2%-5% of total WBC count very numerous in lining of respiratory and digestive tract weak phagocytes capable of ingesting inflammatory chemicals and proteins associated with antigen-antibody reactions help to protect against parasitic worms and allergic reactions BASOPHILS large, sparse cytoplasmic granules least numerous of WBC 0.5%-1% of total leukocyte count motile, capable of diapedesis, non- phagocytic play a major role in allergic responses contain histamine (inflammatory) contain heparin (anticoagulant) LYMPHOCYTES smallest of WBC large spherical nuclei 25% of WBC count T- cells attack directly mature and reside in the Thymus gland B- cells produce antibodies are released directly to the blood from the Bone marrow MONOCYTES largest WBC dark, kidney bean shaped nuclei mobile, highly phagocytic engulf large bacterial organisms and viral infected cells WHITE BLOOD CELL NUMBERS 1 cubic mm= 5000-9000 leukocytes clinical significance is given to a numbers or percentage change in WBC numbers acute appendicitis neutrophil numbers increase DIFFERENTIAL COUNT % count of WBC leukopenia== decreased WBC numbers leukocytosis== increased WBC numbers NEUTROPHIL (66%) HIGH infection burn stress inflammation LOW radiation vitamin B12 deficiency system lupus EOSINOPHIL(3%) HIGH allergic reaction parasitic infection autoimmune disease LOW stress Cushing’s disease BASOPHIL (1%) HIGH leukemia cancer LOW pregnancy ovulation stress LYMPHOCYTE (24%) HIGH viral infection immune disease LOW prolonged illness high steroid levels MONOCYTE (6%) HIGH viral, fungal infections TB LOW rarely occurs FORMATION OF WHITE BLOOD CELLS most WBC originate in red bone marrow many lymphocytes and monocytes are derived from lymphatic tissue WBC LIFESPAN most live only a few hours or days some lymphocytes may live for many years (10 years or more) WBC PHYSIOLOGY combat pathogens 1) phagocytosis 2) immune responses neutrophils and macrophages are active in phagocytosis ingest bacteria most leukocytes possess the ability to squeeze through the minute spaces of the capillary walls (diapedisis) PHAGOCYTES several chemicals attract phagocytes inflamed tissues toxins produced by microbes kinins from damaged tissue colony stimulating factors (CSF) NEUTROPHIL PHYSIOLOGY neutrophils respond to tissue destruction by bacteria quickest release destructive chemicals after phagocytosis RELEASED LEUKOCYTE CHEMICALS 1) lysozyme 2) defensins proteins which poke holes in microbe membranes 3) oxidants O2H2O2 ( hydrogen peroxide ) OCl- ( bleach ) MONOCYTE PHYSIOLOGY monocytes take longer to reach infection site arrive in larger numbers & destroy more microbes upon arrival they enlarge and differentiate into wandering macrophages clean up cell debris and microbes EOSINOPHIL PHYSIOLOGY eosinophils arrive and release histaminase which counteracts effects of histamine in allergic reactions phagocytize antigen-antibody complexes high counts indicate a parasitic worm infection or an allergic condition BASOPHIL PHYSIOLOGY arrive and develop into mast cells release heparin, histamine, serotonin intensify inflammatory reaction LYMPHOCYTE PHYSIOLOGY major combatants in immune responses B-cells and T-cells substances which initiate an immune response are called antigens B-CELLS B-cells develop into plasma cells in response to antigen presence plasma cells produce antibodies specific atibodies will bind to specific antigens creating antigen-antibody complexes antibodies “cover” the antigen inactivating them T-CELLS Killer T-cells (cytotoxic T-cells) destroy foreign invaders directly virus, fungi. cancer, transplanted cells, some bacteria Helper T-cells assist B-cells and killer T-cells LEUKEMIA malignant disease of blood forming tissue uncontrolled production and accumulation of immature leukocytes anemia and bleeding problems occur due to crowding out of normal bone marrow cells preventing normal production of RBC and platelets cause of death can be from internal hemorrhaging or from uncontrolled infection due to lack of mature leukocytes abnormal accumulations can be reduced by radiation or chemotherapy which destroys the abnormal bone marrow BONE MARROW TRANSPLANT bone marrow containing WBC are aspirated from the red bone marrow of the hip injected into the vein of the recipient injected cells “reseed” the unhealthy bone marrow MONONUCLEOSIS contagious disease affecting lymphoid tissue throughout the body caused by “Epstein-Barr virus” (EBV) and occurs mainly in young adults and children (mostly females) most commonly enters the body through intimate oral contact infects and multiplies in B-lymphocytes B-cells enlarge and become abnormal in appearance (look like monocytes) elevated WBC count with high number of lymphocytes PLATELETS also called thrombocytes small, colorless, irregular shaped fragments of larger cells about 20%-25% of the size of WBC and RBC 250,000 per mm3 FORMATION AND LIFE SPAN OF PLATELETS formed in red bone marrow, lungs and spleen fragments of larger cells called megakaryocytes life span of about 9 days FUNCTIONS OF PLATELETS promote blood clotting important factors in agglutination, adhesiveness, aggregation aged platelets are removed by liver macrophages END BLOOD PART 1