Blood - Dr. Victor Arai
advertisement

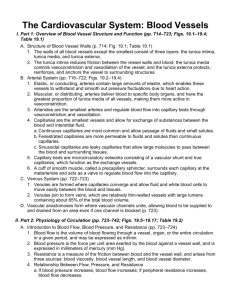
Chap 17 Objectives Overview: Blood Composition and Functions 1. Describe the components of blood and their relative proportions. Define the blood hematocrit. 2. List the physical characteristics of blood. Indicate the normal volumes for males and females. 3. Discuss the functions of blood. Blood Plasma 4. Define blood plasma and list the components and their functions. Formed Elements 5. Indicate the formed elements of the blood, their structure, function, and development. 6. Explain the fate and destruction of erythrocytes. 7. Examine the disorders of too many and too few of each type of formed element. Hemostasis 8. Define hemostasis. 9. Identify the events of platelet plug formation. 10. List the events of the coagulation phase of hemostasis. Differentiate between the intrinsic and extrinsic pathways of prothrombin formation. 11. Explain the mechanism and function of clot retraction and tissue repair. 12. Discuss the factors that limit clot formation. Transfusion and Blood Replacement 13. List the reasons for transfusion of whole blood, plasma, and blood volume expanders. 14. Discuss the basis for human blood groups. Identify what factor determines each blood group. 15. Explain the results of a transfusion reaction, and how blood typing is used to avoid such a problem. Diagnostic Blood Tests 16. Indicate how the various types of diagnostic blood tests are used. Developmental Aspects of Blood 17. List the structures involved in formation of fetal blood. I. Overview: Blood Composition and Functions (pp. 645–646) A. Components (p. 645–646; Fig. 17.1) 1. Blood is a specialized connective tissue consisting of living cells, called formed elements, suspended in a nonliving fluid matrix, blood plasma. 2. Blood that has been centrifuged separates into three layers: erythrocytes, the buffy coat, and plasma. 3. The blood hematocrit represents the percentage of erythrocytes in whole blood. B. Physical Characteristics and Volume (p. 646) 1. Blood is a slightly basic (pH 5 7.35–7.45) fluid that has a higher density and viscosity than water, due to the presence of formed elements. 2. Normal blood volume in males is 5–6 liters, and 4–5 liters for females. C. Functions (p. 646) II. 1. Blood is the medium for delivery of oxygen and nutrients, removal of metabolic wastes to elimination sites, and distribution of hormones. 2. Blood aids in regulating body temperature, body fluid pH, and fluid volume within fluid compartments. 3. Blood protects against excessive blood loss through the clotting mechanism, and from infection through the immune system. Blood Plasma (pp. 646–647; Table 17.1) A. Blood plasma consists of mostly water (90%), and solutes including nutrients, gases, hormones, wastes, products of cell activity, ions, and proteins. B. Plasma proteins account for 8% of plasma solutes, mostly albumin, which function as carriers. III. Formed Elements (pp. 647–661; Figs. 17.2–17.12; Table 17.2) A. Erythrocytes (pp. 647–654; Figs. 17.3–17.8) 1. Erythrocytes, or red blood cells, are small cells that are biconcave in shape. They lack nuclei and most organelles, and contain mostly hemoglobin. a. Hemoglobin is an oxygen-binding pigment that is responsible for the transport of most of the oxygen in the blood. b. Hemoglobin is made up of the protein globin bound to the red heme pigment. 2. Production of Erythrocytes a. Hematopoiesis, or blood cell formation, occurs in the red bone marrow. b. Erythropoiesis, the formation of erythrocytes, begins when a myeloid stem cell is transformed to a proerythroblast, which develops into mature erythrocytes. c. Erythrocyte production is controlled by the hormone erythropoietin. d. Dietary requirements for erythrocyte formation include iron, vitamin B 12 and folic acid, as well as proteins, lipids, and carbohydrates. e. Blood cells have a short life span due to the lack of nuclei and organelles; destruction of dead or dying blood cells is accomplished by macrophages. 3. Erythrocyte Disorders a. Anemias are characterized by a deficiency in RBCs. b. Polycythemia is characterized by an abnormal excess of RBCs. B. Leukocytes (pp. 654–660; Figs. 17.9–17.11) 1. Leukocytes, or white blood cells, are the only formed elements that are complete cells and make up less than 1% of total blood volume. 2. Leukocytes are critical to our defense against disease. 3. Granulocytes are a main group of leukocytes characterized as large cells with lobed nuclei and visibly staining granules; all are phagocytic. a. Neutrophils are the most numerous type of leukocyte. They are chemically attracted to sites of inflammation and are active phagocytes. b. Eosinophils are relatively uncommon and attack parasitic worms. c. Basophils are the least numerous leukocyte and release histamine to promote inflammation. 4. Agranulocytes are a main group of lymphocytes that lack visibly staining granules. a. T lymphocytes directly attack viral-infected and tumor cells; B lymphocytes produce antibody cells. b. Monocytes become macrophages and activate T lymphocytes. 5. Production and Life Span of Leukocytes a. Leukopoiesis, the formation of white blood cells, is regulated by the production of interleukins and colony-stimulating factors (CSF). b. Leukopoiesis involves differentiation of hemocytoblasts along two pathways: lymphoid and myeloid stem cells. 6. Leukocyte Disorders a. Leukopenia is an abnormally low white blood cell count. b. Leukemias are clones of a single white blood cell that remain unspecialized and divide out of control. c. Infectious mononucleosis is a disease caused by the Epstein-Barr virus. C. Platelets (pp. 660–661; Fig. 17.12) IV. 1. Platelets are not complete cells, but fragments of large cells called megakaryocytes. 2. Platelets are critical to the clotting process, forming the temporary seal when a blood vessel breaks. 3. Formation of platelets involves repeated mitoses of megakaryocytes without cytokinesis. Hemostasis (pp. 661–667; Figs. 17.13–17.14; Table 17.3) A. A break in a blood vessel stimulates hemostasis, a fast, localized response to reduce blood loss through clotting. B. Vascular spasms are the immediate vasoconstriction response to blood vessel injury. C. Platelet Plug Formation (p. 662; Fig. 17.13) 1. When endothelium is damaged, platelets become sticky and spiky, adhering to each other and the damaged vessel wall. 2. Once attached, other platelets are atracted to the site of injury, activating a positive feedback loop for clot formation. D. Coagulation, or blood clotting, is a multi-step process in which blood is transformed from a liquid to a gel (pp. 662–664; Figs. 17.13–17.14). 1. Factors that promote clotting are called clotting factors, or procoagulants; those that inhibit clot formation are called anticoagulants. 2. The clotting process involves: formation of prothrombin activator, conversion of prothrombin to thrombin, and the formation of fibrin mesh from fibrinogen in the plasma. E. Clot Retraction and Repair (p. 664) F. 1. Clot retraction is a process in which the contractile proteins within platelets contract and pull on neighboring fibrin strands, squeezing plasma from the clot and pulling damaged tissue edges together. 2. Repair is stimulated by platelet-derived growth factor (PDGF). Fibrinolysis removes unneeded clots through the action of the fibrin-digesting enzyme plasmin. G. Factors Limiting Clot Growth or Formation (pp. 664–665) 1. Rapidly moving blood disseminates clotting factors before they can initiate a clotting cascade. 2. Thrombin that is not bound to fibrin is inactivated by antithrombin III and protein C, as well as heparin. H. Disorders of Hemostasis (pp. 665–667) 1. Thromboembolytic disorders result from conditions that cause undesirable clotting, such as roughening of vessel endothelium, slow-flowing blood, or blood stasis. 2. Bleeding disorders arise from abnormalities that prevent normal clot formation, such as a deficiency in circulating platelets, lack of synthesis of procoagulants, or hemophilia. V. Transfusion and Blood Replacement (pp. 667–670; Fig. 17.15; Table 17.4) A. Transfusion of whole blood is routine when blood loss is substantial, or when treating thrombocytopenia (pp. 668–670; Fig. 17.15; Table 17.4). 1. Humans have different blood types based on specific antigens on RBC membranes. 2. ABO blood groups are based on the presence or absence of two types of agglutinogens. 3. Preformed antibodies (agglutinins) are present in blood plasma and do not match the individual’s blood. The Rh factor is a group of RBC antigens that are either present in Rh1 blood, or absent in Rh2 blood. 4. 5. A transfusion reaction occurs if the infused donor blood type is attacked by the recipient’s blood plasma agglutinins, resulting in agglutination and hemolysis of the donor cells. B. Plasma and blood volume expanders are given in cases of extremely low blood volume. VI. Diagnostic Blood Tests (p. 671) A. Changes in some of the visual properties of blood can signal diseases such as anemia, heart disease, and diabetes. B. Differential white blood cell counts are used to detect differences in relative amounts of specific blood cell types. C. Prothrombin time, which measures the amount of prothrombin in the blood, and platelet counts evaluate the status of the hemostasis system. D. SMAC, SMA12–60, and complete blood count (CBC) give comprehensive values of the condition of the blood. Chap 18 Objectives Heart Anatomy 1. Describe the size, location, and orientation of the heart. 2. Identify structures of the pericardium. 3. Define the endocardium, myocardium, and epicardium. 4. Compare the function of the atria and the ventricles, and describe the difference between the function of the right and left ventricles. 5. Discuss the need for coronary circulation, and name the vessels that play a role in it. 6. Indicate the function and location of the atrioventricular valves and semilunar valves. Properties of Cardiac Muscle Fibers 7. Describe the microscopic anatomy and control of cardiac muscle cells, and compare to skeletal muscle cells. 8. Name the energetic requirements of cardiac muscle and how these requirements are met. Heart Physiology 9. Describe the structures and activities of the intrinsic conduction system. 10. Draw a typical ECG. Label and define the three phases. 11. Discuss the cardiac cycle in terms of relative pressure in each set of chambers. 12. Explain the normal heart sounds and how the sounds relate to closure of specific valves and systole or diastole of the ventricles. 13. Define cardiac output, stroke volume, and heart rate. Calculate cardiac output and cardiac reserve. 14. List the factors that affect stroke volume of the heart. 15. Describe the effects of the divisions of the autonomic nervous system on the heart. Developmental Aspects of the Heart 16. Describe the events of development of the heart from two separate tubes to a fin-ished structure. 17. Explain age-related changes that occur in the heart. Discuss possible changes in heart function due to these changes. I. Heart Anatomy (pp. 676–687; Figs. 18.1–18.10) A. Size, Location, and Orientation (p. 676; Fig. 18.1) 1. The heart is the size of a fist and weighs 250–300 grams. 2. The heart is found in mediastinum and two-thirds lies left of the midsternal line. 3. The base is directed toward the right shoulder and the apex points toward the left hip. B. Coverings of the Heart (p. 676; Fig. 18.2) 1. The heart is enclosed in a doubled-walled sac called the pericardium. 2. Deep to pericardium is the serous pericardium. 3. The parietal pericardium lines the inside of the pericardium. 4. The visceral pericardium, or epicardium, covers the surface of the heart. C. Layers of the Heart Wall (pp. 676–678; Fig. 18.3) 1. The myocardium is composed mainly of cardiac muscle and forms the bulk of the heart. 2. The endocardium lines the chambers of the heart. D. Chambers and Associated Great Vessels (pp. 678-681; Fig. 18.4) 1. The right and left atria are the receiving chambers of the heart. 2. The right ventricle pumps blood into the pulmonary trunk; the left ventricle pumps blood into the aorta. E. Pathway of Blood Through the Heart (pp. 681–683; Fig. 18.5) 1. F. The right side of the heart pumps blood into the pulmonary circuit; the left side of the heart pumps blood into the systemic circuit. Coronary Circulation (pp. 683–684; Fig. 18.7) 1. The heart receives no nourishment from the blood as it passes through the chamber. 2. The coronary circulation provides the blood supply for the heart cells. 3. In a myocardial infarction, there is prolonged coronary blockage that leads to cell death. G. Heart Valves (pp. 684–687; Figs. 18.8–18.10) 1. The tricuspid and bicuspid valves prevent backflow into the atria when the ventricles contract. 2. When the heart is relaxed the AV valves are open, and when the heart contracts the AV valves close. 3. The aortic and pulmonary semilunar valves are found in the major arteries leaving the heart. They prevent backflow of blood into the ventricles. 4. When the heart is relaxed the semilunar valves are closed, and when the heart contracts the semilunar valves are open. II. Properties of Cardiac Muscle Fibers (pp. 687–690; Figs. 18.11–18.12 ) A. Microscopic Anatomy (pp. 687–688; Fig. 18.11) 1. Cardiac muscle is striated and contraction occurs via the sliding filament mechanism. 2. The cells are short, fat, branched, and interconnected by intercalated discs. B. Mechanism and Events of Contraction (pp. 688–690; Fig. 18.12) 1. Some cardiac muscle cells are self-excitable. 2. The heart contracts as unit or not at all. 3. The heart’s absolute refractory period is longer than a skeletal muscle’s, preventing tetanic contractions. C. Energy Requirements (p. 690) 1. The heart relies exclusively on aerobic respiration for its energy demands. 2. Cardiac muscle is capable of switching nutrient pathways to use whatever nutrient supply is available. III. Heart Physiology (pp. 690–703; Figs. 18.13–18.23) A. Electrical Events (pp. 690–695; Figs. 18.13–18.18) 1. Intrinsic conduction system is made up of specialized cardiac cells that initiate and distribute impulses, ensuring that the heart depolarizes in an orderly fashion. 2. The autorhythmic cells have an unstable resting potential, called pacemaker potentials, that continuously depolarizes. 3. Impulses pass through the autorhythmic cardiac cells in the following order: sinoatrial node, atrioventricular node, atrioventricular bundle, right and left bundle branches, and Purkinje fibers. 4. The autonomic nervous system modifies the heartbeat: the sympathetic center increases rate and depth of the heartbeat, and the parasympathetic center slows the heartbeat. 5. An electrocardiograph monitors and amplifies the electrical signals of the heart and records it as an electrocardiogram (ECG). B. Heart Sounds (pp. 695–696; Fig. 18.19–18.20) 1. Normal a. The first heart sound, lub, corresponds to closure of the AV valves, and occurs during ventricular systole. b. The second heart sound, dup, corresponds to the closure of the semilunar valves, and occurs during ventricular diastole. 2. Abnormal a. Heart murmurs are extraneous heart sounds due to turbulent backflow of blood through a valve that does not close tightly. C. Mechanical Events: The Cardiac Cycle (pp. 696–698; Fig. 18.19) 1. Systole is the contractile phase of the cardiac cycle and diastole is the relaxation phase of the cardiac cycle. 2. Cardiac Cycle a. Ventricular Filling: Mid-to-Late Diastole b. Ventricular Systole c. Isovolumetric Relaxation: Early Diastole D. Cardiac Output (pp. 698–703; Figs. 18.21–18.23) 1. Cardiac output is defined as the amount of blood pumped out of a ventricle per beat, and is calculated as the product of stroke volume and heart rate. 2. Regulation of Stroke Volume a. Preload: the Frank-Starling law of the heart states that the critical factor controlling stroke volume is the degree of stretch of cardiac muscle cells immediately before they contract. b. Contractility: contractile strength increases if there is an increase in cytoplasmic calcium ion concentration. c. Afterload: ventricular pressure that must be overcome before blood can be ejected from the heart. 3. Regulation of Heart Rate a. Sympathetic stimulation of pacemaker cells increases heart rate and contractility, while parasympathetic inhibition of cardiac pacemaker cells decreases heart rate. b. Epinephrine, thyroxine, and calcium influence heart rate. c. Age, gender, exercise, and body temperature all influence heart rate. 4. Homeostatic Imbalance of Cardiac Output a. Congestive heart failure occurs when the pumping efficiency of the heart is so low that blood circulation cannot meet tissue needs. b. Pulmonary congestion occurs when one side of the heart fails, resulting in pulmonary edema. IV. Developmental Aspects of the Heart (pp. 703, 706–707; Figs. 18.24–18.25) A. Embryological Development (pp. 703–706; Figs. 18.24–18.25) 1. The heart begins as a pair of endothelial tubes that fuse to make a single heart tube with four bulges representing the four chambers. 2. The foramen ovale is an opening in the interatrial septum that allows blood returning to the pulmonary circuit to be directed into the atrium of the systemic circuit. 3. The ductus arteriosus is a vessel extending between the pulmonary trunk to the aortic arch that allows blood in the pulmonary trunk to be shunted to the aorta. B. Aging Aspects of the Heart (pp. 706–707) 1. Sclerosis and thickening of the valve flaps occurs over time, in response to constant pressure of the blood against the valve flaps. 2. Decline in cardiac reserve occurs due to a decline in efficiency of sympathetic stimulation. 3. Fibrosis of cardiac muscle may occur in the nodes of the intrinsic conduction system, resulting in arrhythmias. 4. Atherosclerosis is the gradual deposit of fatty plaques in the walls of the systemic vessels. Chap 19 Objectives PART 1: OVERVIEW OF BLOOD VESSEL STRUCTURE AND FUNCTION 1. Define the direction of flow and oxygenation state of blood in arteries and veins. 2. Describe the structural arrangement and composition of the layers of blood vessels. 3. State the function of each type of blood vessel. 4. List the types of capillary endothelium and the functional applications of each. 5. Explain the pathway of blood flow through capillary beds, and the role of precapillary sphincters. PART 2: PHYSIOLOGY OF CIRCULATION 6. Define blood flow, blood pressure, and resistance, and describe the factors that affect each. 7. State the relationship between flow, pressure, and resistance. 8. Discuss systemic blood pressure in terms of pressure gradients and characteristics in each type of vessel. 9. Define systolic and diastolic pressure, pulse pressure, and mean arterial pressure. 10. Explain the mechanisms used to regulate blood pressure. 11. Define hypertension and hypotension, and identify contributing factors. 12. Explain how blood flow is regulated by the body. 13. Identify the types and causes of circula-tory shock. PART 3: CIRCULATORY PATHWAYS: BLOOD VESSELS OF THE BODY 14. List the major blood vessels of the body and the areas and organs they serve. 15. Describe the major differences between arteries and veins. Developmental Aspects of Blood Vessels 16. Explain how the vascular system develops during fetal development. 17. Discuss special structural adaptations of the fetal circulation. 18. Identify the changes that occur in the vascular system as a consequence of age. I. Part 1: Overview of Blood Vessel Structure and Function (pp. 712–721; Figs. 19.1–19.4; Table 19.1) A. Structure of Blood Vessel Walls (pp. 712–713; Fig. 19.1; Table 19.1) 1. The walls of all blood vessels except the smallest consist of three layers: the tunica interna, tunica media, and tunica externa. 2. The tunica interna reduces friction between the vessel walls and blood; the tunica media controls vasoconstriction and vasodilation of the vessel; and the tunica externa protects, reinforces, and anchors the vessel to surrounding structures. B. Arterial System (pp. 713–720; Figs. 19.2–19.4) 1. Elastic, or conducting, arteries contain large amounts of elastin, which enables these vessels to withstand and smooth out pressure fluctuations due to heart action. 2. Muscular, or distributing, arteries deliver blood to specific body organs, and have the greatest proportion of tunica media of all vessels, making them more active in vasoconstriction. 3. Arterioles are the smallest arteries and regulate blood flow into capillary beds through vasoconstriction and vasodilation. 4. Capillaries are the smallest vessels and allow for exchange of substances between the blood and interstitial fluid. a. Continuous capillaries are most common and allow passage of fluids and small solutes. b. Fenestrated capillaries are more permeable to fluids and solutes than continuous capillaries. c. Sinusoidal capillaries are leaky capillaries that allow large molecules to pass between the blood and surrounding tissues. 5. Capillary beds are microcirculatory networks consisting of a vascular shunt and true capillaries, which function as the exchange vessels. 6. A cuff of smooth muscle, called a precapillary sphincter, surrounds each capillary at the metarteriole and acts as a valve to regulate blood flow into the capillary. C. Venous System (pp. 720–721) 1. Venules are formed where capillaries converge and allow fluid and white blood cells to move easily between the blood and tissues. 2. Venules join to form veins, which are relatively thin-walled vessels with large lumens containing about 65% of the total blood volume. D. Vascular anastomoses form where vascular channels unite, allowing blood to be supplied to and drained from an area even if one channel is blocked (p. 721). II. Part 2: Physiology of Circulation (pp. 721–740; Figs. 19.5– 19.16; Table 19.2) A. Introduction to Blood Flow, Blood Pressure, and Resistance (pp. 721–722) 1. Blood flow is the volume of blood flowing through a vessel, organ, or the entire circulation in a given period, and may be expressed as ml/min. 2. Blood pressure is the force per unit area exerted by the blood against a vessel wall, and is expressed in millimeters of mercury (mm Hg). 3. Resistance is a measure of the friction between blood and the vessel wall, and arises from three sources: blood viscosity, blood vessel length, and blood vessel diameter. 4. Relationship Between Flow, Pressure, and Resistance a. If blood pressure increases, blood flow increases; if peripheral resistance increases, blood flow decreases. b. Peripheral resistance is the most important factor influencing local blood flow, because vasoconstriction or vasodilation can dramatically alter local blood flow, while systemic blood pressure remains unchanged. B. Systemic Blood Pressure (pp. 722–724; Figs. 19.5–19.6) 1. The pumping action of the heart generates blood flow; pressure results when blood flow is opposed by resistance. 2. Systemic blood pressure is highest in the aorta, and declines throughout the pathway until it reaches 0 mm Hg in the right atrium. 3. Arterial blood pressure reflects how much the arteries close to the heart can be stretched (compliance, or distensibility), and the volume forced into them at a given time. a. When the left ventricle contracts, blood is forced into the aorta, producing a peak in pressure called systolic pressure (120 mm Hg). b. Diastolic pressure occurs when blood is prevented from flowing back into the ventricles by the closed semilunar valve, and the aorta recoils (70–80 mm Hg). c. The difference between diastolic and systolic pressure is called the pulse presssure. d. The mean arterial pressure (MAP) represents the pressure that propels blood to the tissues. 4. Capillary blood pressure is low, ranging from 40–20 mm Hg, which protects the capillaries from rupture, but is still adequate to ensure exchange between blood and tissues. 5. Venous blood pressure changes very little during the cardiac cycle, and is low, reflecting cumulative effects of peripheral resistance. C. Maintaining Blood Pressure (pp. 724–732; Figs. 19.7–19.12; Table 19.2) 1. Blood pressure varies directly with changes in blood volume and cardiac output, which are determined primarily by venous return and neural and hormonal controls. 2. Short-term neural controls of peripheral resistance alter blood distribution to meet specific tissue demands, and maintain adequate MAP by altering blood vessel diameter. a. The vasomotor center is a cluster of sympathetic neurons in the medulla that controls changes in the diameter of blood vessels. b. Baroreceptors detect stretch and send impulses to the vasomotor center, inhibiting its activity and promoting vasodilation of arterioles and veins. c. Chemoreceptors detect a rise in carbon dioxide levels of the blood, and stimulate the cardioacceleratory and vasomotor centers, which increases cardiac output and vasoconstriction. d. The cortex and hypothalamus can modify arterial pressure by signaling the medullary centers. 3. Chemical controls influence blood pressure by acting on vascular smooth muscle or the vasomotor center. a. Norepinephrine and epinephrine promote an increase in cardiac output and generalized vasoconstriction. b. Atrial natriuretic peptide acts as a vasodilator and an antagonist to aldosterone, resulting in a drop in blood volume. c. Antidiuretic hormone promotes vasoconstriction and water conservation by the kidneys, resulting in an increase in blood volume. d. Angiotensin II acts as a vasoconstrictor, as well as promoting the release of aldosterone and antidiuretic hormone. e. Endothelium-derived factors promote vasoconstriction, and are released in response to low blood flow. f. Nitric oxide is produced in response to high blood flow or other signaling molecules, and promotes systemic and localized vasodilation. g. Inflammatory chemicals, such as histamine, prostacyclin, and kinins, are potent vasodilators. h. Alcohol inhibits antidiuretic hormone release and the vasomotor center, resulting in vasodilation. 4. Long-Term Mechanisms a. The direct renal mechanism counteracts an increase in blood pressure by altering blood volume, which increases the rate of kidney filtration. b. The indirect renal mechanism is the renin-angiotensin mechanism, which counteracts a decline in arterial blood pressure by causing systemic vasoconstriction. 5. Monitoring circulatory efficiency is accomplished by measuring pulse and blood pressure; these values together with respiratory rate and body temperature are called vital signs. a. A pulse is generated by the alternating stretch and recoil of elastic arteries during each cardiac cycle. b. Systemic blood pressure is measured indirectly using the ascultatory method, which relies on the use of a blood pressure cuff to alternately stop and reopen blood flow into the brachial artery of the arm. 6. Alterations in blood pressure may result in hypotension (low blood pressure) or transient or persistent hypertension (high blood pressure). D. Blood Flow Through Body Tissues: Tissue Perfusion (pp. 732–739; Figs. 19.13–19.16) 1. Tissue perfusion is involved in delivery of oxygen and nutrients to, and removal of wastes from, tissue cells; gas exchange in the lungs; absorption of nutrients from the digestive tract; and urine formation in the kidneys. 2. Velocity or speed of blood flow changes as it passes through the systemic circulation; it is fastest in the aorta, and declines in velocity as vessel diameter decreases. 3. Autoregulation: Local Regulation of Blood Flow a. Autoregulation is the automatic adjustment of blood flow to each tissue in proportion to its needs, and is controlled intrinsically by modifying the diameter of local arterioles. b. Metabolic controls of autoregulation are most strongly stimulated by a shortage of oxygen at the tissues. c. Myogenic control involves the localized response of vascular smooth muscle to passive stretch. d. Long-term autoregulation develops over weeks or months, and involves an increase in the size of existing blood vessels and an increase in the number of vessels in a specific area, a process called angiogenesis. 4. Blood Flow in Special Areas a. Blood flow to skeletal muscles varies with level of activity and fiber type. b. Muscular autoregulation occurs almost entirely in response to decreased oxygen concentrations. c. Cerebral blood flow is tightly regulated to meet neuronal needs, since neurons cannot tolerate periods of ischemia, and increased blood carbon dioxide causes marked vasodilation. d. In the skin, local autoregulatory events control oxygen and nutrient delivery to the cells, while neural mechanisms control the body temperature regulation function. e. Autoregulatory controls of blood flow to the lungs are the opposite of what happens in most tissues: low pulmonary oxygen causes vasoconstriction, while higher oxygen causes vasodilation. f. Movement of blood through the coronary circulation of the heart is influenced by aortic pressure and the pumping of the ventricles. 5. Blood Flow Through Capillaries and Capillary Dynamics a. Vasomotion, the slow, intermittent flow of blood through the capillaries, reflects the action of the precapillary sphincters in response to local autoregulatory controls. b. Capillary exchange of nutrients, gases, and metabolic wastes occurs between the blood and interstitial space through diffusion. c. Hydrostatic pressure (HP) is the force of a fluid against a membrane. d. Colloid osmotic pressure (OP), the force opposing hydrostatic pressure, is created by the presence of large, nondiffusible molecules that are prevented from moving through the capillary membrane. e. Fluids will leave the capillaries if net HP exceeds net OP, but fluids will enter the capillaries if net OP exceeds net HP. 6. Circulatory shock is any condition in which blood volume is inadequate and cannot circulate normally, resulting in blood flow that cannot meet the needs of a tissue. a. Hypovolemic shock results from a large-scale loss of blood, and may be characterized by an elevated heart rate and intense vasoconstriction. b. Vascular shock is characterized by a normal blood volume, but extreme vasodilation, often related to a loss of vasomotor tone, resulting in poor circulation and a rapid drop in blood pressure. c. Transient vascular shock is due to prolonged exposure to heat, such as while sunbathing, resulting in vasodilation of cutaneous blood vessels. d. Cardiogenic shock occurs when the heart is too inefficient to sustain normal blood flow, and is usually related to myocardial damage, such as repeated myocardial infarcts. III. Part 3: Circulatory Pathways: Blood Vessels of the Body (pp. 740, 744–766; Figs. 19.17–19.28; Tables 19.3–19.12) A. Two distinct pathways travel to and from the heart: pulmonary circulation runs from the heart to the lungs and back to the heart; systemic circulation runs to all parts of the body before returning to the heart. (pp. 740, 744–746; Tables 19.3–19.4) B. There are some important differences between arteries and veins. 1. There is one terminal systemic artery, the aorta, but two terminal systemic veins: the superior and inferior vena cava. 2. Arteries run deep and are well protected, but veins are both deep, which run parallel to the arteries, and superficial, which run just beneath the skin. 3. Arterial pathways tend to be clear, but there are often many interconnections in venous pathways, making them difficult to follow. 4. There are at least two areas where venous drainage does not parallel the arterial supply: the dural sinuses draining the brain, and the hepatic portal system draining from the digestive organs to the liver before entering the main systemic circulation. C. Four paired arteries supply the head and neck. (pp. 748–749; Figs. 19.17–19.20; Table 19.5) D. The upper limbs are supplied entirely by arteries arising from the subclavian arteries. (pp. 750– 751; Fig. 19.21; Table 19.6) E. The arterial supply to the abdomen arises from the aorta. (pp. 752–755; Figs. 19.22–19.23; Table 19.7) F. The internal iliac arteries serve mostly the pelvic region; the external iliacs supply blood to the lower limb and abdominal wall. (pp. 756–757; Fig. 19.23; Table 19.8) G. The venae cavae are the major tributaries of the venous circulation. (pp. 758–759; Fig. 19.24; Table 19.9) H. Blood drained from the head and neck is collected by three pairs of veins. (pp. 760–761; Fig. 19.25; Table 19.10) I. The deep veins of the upper limbs follow the paths of the companion arteries. (pp. 762–763; Fig. 19.26; Table 19.11) J. Blood draining from the abdominopelvic viscera and abdominal walls is returned to the heart by the inferior vena cava. (pp. 764–765; Fig. 19.27; Table 19.12) K. Most deep veins of the lower limb have the same names as the arteries they accompany. (p. 766; Fig. 19.28; Table 19.13) IV. Developmental Aspects of the Blood Vessels (pp. 740–741) A. The vascular endothelium is formed by mesodermal cells that collect throughout the embryo in blood islands, which give rise to extensions that form rudimentary vascular tubes. B. By the fourth week of development, the rudimentary heart and vessels are circulating blood. C. Fetal vascular modifications include shunts to bypass fetal lungs (the foramen ovale and ductus arteriosus), the ductus venosus that bypasses the liver, and the umbilical arteries and veins, which carry blood to and from the placenta. D. At birth, the fetal shunts and bypasses close and become occluded. E. Congenital vascular problems are rare, but the incidence of vascular disease increases with age, leading to varicose veins, tingling in fingers and toes, and muscle cramping. F. Atherosclerosis begins in youth, but rarely causes problems until old age. G. Blood pressure changes with age: the arterial pressure of infants is about 90/55, but rises steadily during childhood to an average 120/80, and finally increases to 150/90 in old age.