Polycythemia Vera
advertisement
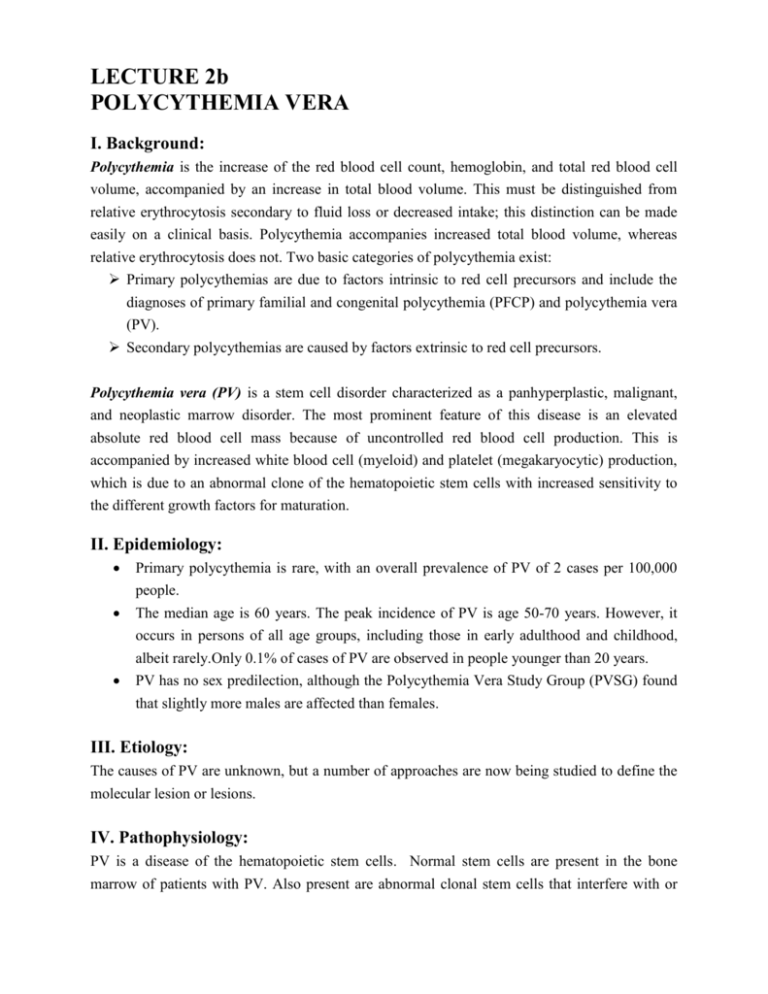
LECTURE 2b POLYCYTHEMIA VERA I. Background: Polycythemia is the increase of the red blood cell count, hemoglobin, and total red blood cell volume, accompanied by an increase in total blood volume. This must be distinguished from relative erythrocytosis secondary to fluid loss or decreased intake; this distinction can be made easily on a clinical basis. Polycythemia accompanies increased total blood volume, whereas relative erythrocytosis does not. Two basic categories of polycythemia exist: Primary polycythemias are due to factors intrinsic to red cell precursors and include the diagnoses of primary familial and congenital polycythemia (PFCP) and polycythemia vera (PV). Secondary polycythemias are caused by factors extrinsic to red cell precursors. Polycythemia vera (PV) is a stem cell disorder characterized as a panhyperplastic, malignant, and neoplastic marrow disorder. The most prominent feature of this disease is an elevated absolute red blood cell mass because of uncontrolled red blood cell production. This is accompanied by increased white blood cell (myeloid) and platelet (megakaryocytic) production, which is due to an abnormal clone of the hematopoietic stem cells with increased sensitivity to the different growth factors for maturation. II. Epidemiology: Primary polycythemia is rare, with an overall prevalence of PV of 2 cases per 100,000 people. The median age is 60 years. The peak incidence of PV is age 50-70 years. However, it occurs in persons of all age groups, including those in early adulthood and childhood, albeit rarely.Only 0.1% of cases of PV are observed in people younger than 20 years. PV has no sex predilection, although the Polycythemia Vera Study Group (PVSG) found that slightly more males are affected than females. III. Etiology: The causes of PV are unknown, but a number of approaches are now being studied to define the molecular lesion or lesions. IV. Pathophysiology: PV is a disease of the hematopoietic stem cells. Normal stem cells are present in the bone marrow of patients with PV. Also present are abnormal clonal stem cells that interfere with or suppress normal stem cell growth and maturation. Evidence indicates that the etiology of panmyelosis is unregulated neoplastic proliferation. Progenitors of the blood cells in these patients display abnormal responses (increased sensibility) to growth factors such as EPO, IL3 or GM-CSF (explaining their spontaneous growth), suggesting the presence of a defect in a signaling pathway common to different growth factors. Different observations suggest an additional decrease in cellular apoptosis ensuring them a longer survival. Recently it was emphasized a mutation in the gene coding the tyrosine kinase JAK2 (V617F) to nearly 100% of patients with PV. This mutation trains spontaneous activation of this kinase. Mutation has been emphasized too in patients with essential thrombocythemia and those with bone marrow fibrosis and myeloid metaplasia of the spleen (primary myelofibrosis). This discovery started to change diagnostic and therapeutic approach in these chroni myeloproliferative disease. Thromboses and bleeding are frequent in persons with PV and myeloproliferative disease (MPD), and they result from the disruption of hemostatic mechanisms because of an increased level of red blood cells and an elevation of the platelet count. Recent findings indicate the additional roles of tissue factor and polymorphonuclear leukocytes in clotting, the platelet surface as a contributor to phospholipid-dependent coagulation reactions, and the entity of microparticles. Tissue factor is also synthesized by blood leukocytes, the level of which is increased in persons with MPD, which can contribute to thrombosis. Hyperhomocystinemia is a risk factor for thrombosis and is also widely prevalent in patients with MPD (35% in controls, 56% in persons with PV). Acquired von Willebrand syndrome is an established cause of bleeding in persons with MPD, accounting for approximately 12-15% of all patients with this syndrome. This condition is largely related to the absorption of von Willebrand factor onto the platelets; reducing the platelet count should alleviate the bleeding and the syndrome. V. Clinic V.1. History: Symptoms are often insidious in onset. They are often related to blood hyperviscosity secondary to a marked increase in the cellular elements of blood, which impairs microcirculation. Symptoms are related to hyperviscosity, sludging of blood flow, and thromboses, which lead to poor oxygen delivery and symptoms that include headache, dizziness, vertigo, tinnitus, visual disturbances, angina pectoris, or intermittent claudications. Bleeding complications (1%) include epistaxis, gum bleeding, ecchymoses, and GI bleeding. Thrombotic complications (1%) include venous thrombosis or thromboembolism and an increased prevalence of stroke and other arterial thromboses. Abdominal pain due to peptic ulcer disease is present because PV is associated with increased histamine levels and gastric acidity or possible Budd-Chiari syndrome (hepatic portal vein thrombosis) or mesenteric vein thrombosis. Splenomegaly, when present, can cause early satiety because of (1) gastric filling being impaired by the enlarged spleen or, rarely, (2) symptoms of splenic infarction. Weight loss may result from early satiety or from the increased myeloproliferative activity of the abnormal clone. Pruritus results from increased histamine levels released from increased basophils and mast cells and can be exacerbated by a warm bath or shower. This occurs in up to 40% of patients. V.2. Physical: Physical findings are due to manifestations of the myeloproliferative process and excess of the cellular elements of blood. The following symptoms are due to the manifestations of myeloproliferative disorders with extramedullary hematopoiesis: Splenomegaly - Present in 75% of patients at the time of diagnosis Hepatomegaly - Present in approximately 30% of patients with PV Erythrosis is characteristic of PV and results from the marked increase in total red blood cell mass. This manifests in the face, palms, nailbeds, mucosa, and conjunctiva. Hypertension is common in patients with PV. The red blood cell mass should differentiate PV from Gaisbock syndrome, which is hypertension and pseudopolycythemia (ie, high hemoglobin levels due to low plasma volume). VI. Investigations VI.1. Lab Studies: CBC : Erythrocytosis - red blood cell counts, hemoglobin and hematocrit values are elevated. Leucocytosis - > 12,000/mm3 occurs in approximately 60% of patients. It is mainly composed of neutrophils with a left shift and a few immature cells. Mild basophilia occurs in 60% of patients. Thrombocytosis - to 400.000 - 800.000/mm3 in approximately 50% of patients. Morphologic abnormalities in platelets include macrothrombocytes and granule-deficient platelets. Abnormal platelet function (as measured by platelet aggregation tests with epinephrine, adenosine diphosphate, or collagen) may be demonstrated, but bleeding time may be normal. Bone marrow studies are not necessary to establish the diagnosis, but the finding of hypercellularity and hyperplasia of the erythroid, granulocytic, and megakaryocytic cell lines or myelofibrosis supports the diagnosis of a myeloproliferative process. Iron stores are decreased or absent because of the increased red blood cell mass, and macrophages may be masked in the myeloid hyperplasia that is present. Fibrosis is increased and detected early by silver stains for reticulin. Cytogenetics of the bone marrow cells show a clonal abnormality in 30% of patients who are not treated and in 50% of patients who are treated with alkylating or myelosuppressive agents. o These chromosomal abnormalities include deletions of the long arm of chromosome 5 or 20 (5q-, 20q-) and trisomy 8 (+8) or 9 (+9). o Leukemic transformation is usually associated with multiple or complex abnormalities. Routine coagulation test results are normal, with a high turnover rate for fibrinogen. Chemistry Vitamin B-12 levels are elevated to more than 900 pg/mL in approximately 30% of patients, and 75% of patients show an elevation in the unbound vitamin B-12 binding capacity greater than 2200 pg/mL. This is because of increased transcobalamin-III, a binding protein found in white blood cells, and reflects the total white blood cell counts in the peripheral blood and bone marrow. Hyperuricemia occurs in 40% of patients and reflects the high turnover rate of bone marrow cells releasing DNA metabolites. Pseudohyperkalemia The release of potassium into the serum caused by the increased number of platelets during in vitro coagulation may cause a in the serum, while the true plasma potassium level in vivo is actually within the reference range, as shown by measuring plasma levels and the lack of ECG changes. The leukocyte alkaline phosphatase (LAP) score is elevated (>100 U/L) in 70% of patients. VI.2. Imaging Studies: An enlarged spleen is often palpable and does not require any imaging studies. In some patients with posteriorly enlarged spleens or in those who are obese, ultrasonography or CT scanning may be able to detect an enlargement missed during the physical examination. VI.3. Other Tests: Direct measurement of the red blood cell mass should show an increase with a normal or slightly decreased plasma volume. Red cell mass is greater than 36 mL/kg in men and greater than 32 mL/kg in women. RBCs often have anisocytosis, basophilic stippling, and polychromatophilia. However, patients with hemoglobin concentrations of at least 20 g/dL or hematocrit values of at least 60% in males and 56% in females always have an elevated red blood cell mass. The serum Epo level should be decreased in nearly all patients with PV and no recent hemorrhage. This distinguishes polycythemia from secondary causes of polycythemia in which the serum Epo level is generally within the reference range or is elevated. Measuring arterial oxygen saturation (SaO2) and carboxyhemoglobin (COHB) levels is important to rule out hypoxia as a secondary cause for erythrocytosis. A value of SaO2 below 92% indicates a causal relationship with erythrocytosis Measuring spontaneous growth of erythroid progenitors in cultures (burst-forming unit, erythroid) in the absence of Epo is a very sensitive test for PV or familial erythrocytosis but is not routinely available for clinical use. The hemoglobin-oxygen dissociation curve may be useful in a rare condition to detect a congenital hemoglobinopathy with increased oxygen affinity. This can occur in families. VII. Diagnosis Diagnostic criteria set by the PVSG (Polycythemia vera stoudy group) are as follows: Category A 1. Total red blood cell mass - In males, greater than or equal to 36 mL/kg; in females, greater than or equal to 32 mL/kg 2. Arterial oxygen saturation greater than or equal to 92% 3. Splenomegaly Category B 1. Thrombocytosis with platelet count greater than 400,000/mm3 2. Leukocytosis with a white blood cell count greater than 12,000/mm3 3. Increased leukocyte alkaline phosphatase greater than 100 U/L 4. Serum vitamin B-12 concentration greater than 900 pg/mL or binding capacity greater than 2200 pg/mL Diagnosis is established with A1 plus A2 plus A3 or A1 plus A2 plus any 2 criteria from category B The current diagnostic criteria for polycythemia vera is now based on the World Health Organization (WHO) criteria for polycythemia vera* 2008 , which includes the following: Major criteria o Hgb > 18.5g/dl (♂) or 16.5g/dl (♀) or Hgb or Hct > 99% or Hgb > 17g/dl (♂) or 15 g/dl (♀) and a documented increase of 2 g/dl or RBC mass > 25% of mean normal o Presence of a JAK2 V617F or similar mutation Minor criteria o Bone marrow trilineage expansion o Subnormal EPO level o Endogenous erytyhroid colony growth *A diagnosis of PV is made by two major or first major and two minor criteria. VIII. Complications: PV is a chronic disease, and its natural history of 1.5-3 years of median survival in the absence of therapy has been extended to at least 10-20 years because of new therapeutic tools. The complications found in polycythemia are related to 2 primary factors. The first includes complications related to hyperviscosity. The second relates to bone marrow–related complications. Untreated, the median survival time for these patients is 18 months. However, if patients are treated, survival is greatly extended, up to 10-15 years with phlebotomy alone. The major causes of morbidity and mortality are as follows: Thrombosis has been reported in 15-60% of patients, depending on the control of their disease. It is the major cause of death in 10-40% of patients. Venous and arterial thromboses have resulted in pulmonary emboli, renal failure from renal vein or artery thrombosis, intestinal ischemia from mesenteric vein thromboses, or peripheral arterial emboli. Hemorrhagic complications occur in 15-35% of patients and lead to death in 6-30% of these patients. Bleeding is usually the consequence of vascular compromise resulting from ischemic changes from thrombosis or hyperviscosity. Peptic ulcer disease is reported to be associated with PV at a 3- to 5-fold higher rate than that of the general population. This has been attributed to increased histamine serum levels. Myelofibrosis and pancytopenia occur in 3-10% of patients, usually late in the disease, which is considered the spent phase of PV. In these patients, infections and bleeding complications may be the most serious health threats, and red blood cell transfusions may be required to maintain adequate red blood cell counts and to improve fatigue and other anemia-related symptoms. Acute leukemia or a myelodysplastic syndrome develops in 1.5% of patients treated with phlebotomy alone. The transformation risks increase to 13.5% within 5 years with treatment using chlorambucil and 10.2% within 6-10 years in patients treated with 32P. At 15 years, the transformation risk for HU is 5.9%, which, although not statistically significant, is a worrisome trend. The causes of death in adults are as follows: Thrombosis/thromboembolism (30-40%) Acute myelogenous leukemia (19%) Other malignancies (15%) Hemorrhage (2-10%) Myelofibrosis/myeloid metaplasia (4%) Other (25%) XI. Medical Care: The goals of therapy are to maximize survival while minimizing the complications of therapy as well as of the disease itself. Another objective of therapy is to control the myeloproliferative activity of PV. Evidence of an increase in white blood cells and/or platelets and organomegaly indicate uncontrolled myeloproliferative activity that requires a myelosuppressive agent. Phlebotomy and myelosuppressive chemotherapy are the cornerstones of therapy and have produced a median survival time of 9-14 years after the beginning of treatment. The goal of phlebotomy is to maintain normal red cell mass and blood volume, with a target hematocrit of 45%. The mean survival time of adult patients treated solely with phlebotomy is 13.9 years; however, a high risk of thromboembolic complications exists. In the past, patients have been treated with chlorambucil and other alkylating agents such as pipobroman and busulfan. However, these patients exhibited the highest rates of secondary malignancy including acute leukemia, lymphocytic lymphomas, and skin and gastrointestinal carcinomas. The rates of malignancy appear lower with busulfan than with the other alkylating agents. Currently, these agents are rarely used. Patients treated with phosphorus-32 (32P) tolerate treatment well and have prolonged periods of remission. However, these patients also exhibit increased rates of acute leukemias (10-15%). The mean survival time with 32P treatment is 10.9 years. IX.1. Phlebotomy or bloodletting - has been the mainstay of therapy for this disease process for a long time. The object is to remove excess cellular elements, mainly red blood cells, to improve the circulation of blood by lowering the blood viscosity. Patients with hematocrit values of less than 70% may be bled twice a week to reduce the hematocrit to the range of 40%. Patients with severe plethora who have altered mentation or associated vascular compromise can be bled more vigorously, with daily removal of 500 mL of whole blood. Elderly patients with some cardiovascular compromise or cerebral vascular complications should have the volume replaced with saline solution after each procedure to avoid postural hypotension. Strategy : Because phlebotomy is the most efficient method of lowering the hemoglobin and hematocrit levels to the reference range, all new patients are initially phlebotomized to decrease the risk of complications. The presence of elevated platelet counts that may be exacerbated by the phlebotomy is an indication to use myelosuppressive agents to avoid thrombotic or hemorrhagic complications. Once the patient's hemoglobin and hematocrit values are reduced to within the reference range (ie, <45%), implement a maintenance program either by inducing iron deficiency by continuous phlebotomies (frequency of the procedure depends on the rate of reaccumulation of red blood cells) or using a myelosuppressive agent. The choice depends on the risks of secondary leukemias and the rate of thrombosis or bleeding. Patients must be cautioned to not take iron supplements. IX.2. Hydroxyurea - has been the mainstay therapy for PV after the PVSG results indicated it is an effective agent for myelosuppression; however, concerns have been raised regarding longterm risks for leukemic transformation. In the PVSG trial, HU therapy reduced the risk of thrombosis compared with phlebotomy alone. IX.3. Anagrelide (Agrylin) - is a cyclic adenosine monophosphate phosphodiesterase inhibitor that prevents platelet aggregation and inhibits megakaryocyte maturation, thereby decreasing platelet counts. The total response rate for controlling platelet counts with anagrelide is greater than 70% in patients with MPDs (ie, PV, ET). Long-term treatment with anagrelide in 3660 patients with PV or ET, with a maximum follow-up of 7 years, was efficacious and safe with respect to leukemic transformation. To date, this agent does not appear to increase the risk of acute leukemia in patients with ET and PV over time. IX.4. Interferon alfa - has been demonstrated in small anecdotal studies to possibly be useful in patients who have relapsed or progressed into AMM or large hepatosplenomegaly. However, only low doses are tolerated and significant adverse effects from long-term use may limit its usefulness. IX.5. 32P determines an increase the risk of leukemic transformation from 1-2% to 11%. May be appropriate for patients intolerant of medications or for elderly patients. Single injection may control hemoglobin and platelet count for a year or more. Alternative nonleukemogenic agents are needed for these patients. o Therapy with low-dose aspirin in patients with thrombocytosis suppresses thromboxane biosynthesis by platelets, which is increased in PV and ET. IX.6. General principles in the management of PV include the following: Tailor therapy to suit the clinical needs of the patient. Consider the status of the formed elements of the blood, bone marrow, and organomegaly. Normalize red blood cell mass with phlebotomy as rapidly as clinically possible (250-500 mL every other day). Patients who are elderly or cardiovascularly compromised should be phlebotomized cautiously and smaller amounts should be removed. Suppress myeloproliferative activity with chemotherapy (HU) in all patients older than 50 years. In general, 32P should be reserved for patients older than 80 years or patients with comorbid conditions in whom life expectancy is less than 5-10 years and the convenience of 32P dosing outweighs the substantial risks of developing acute leukemia 5-15 years after 32 P administration. Patients with thrombotic tendencies or those who develop thrombocytosis following phlebotomy should be treated with marrow suppression. Consider anagrelide in younger patients (aged 50-70 y). Maintain blood values at reference range levels by regular examination and treatment. Avoid overtreatment and toxicity by careful and judicious use of chemotherapy and radiation. Supplemental phlebotomy is preferred over excess marrow suppression. Treat hyperuricemia with allopurinol (100-300 mg/d) until remission has been attained. For acute gouty attacks, colchicine or other anti-inflammatory agents are indicated X. Further Outpatient Care: Thrombosis in PV is substantially more frequent in patients treated with phlebotomy alone without myelosuppression. This risk is believed to be related to thrombocytosis, which was not observed in the study. Platelet numbers alone are not likely to be the primary factor responsible for the increased risk of thrombosis; the presence of abnormal platelets is more likely. The initial PVSG study using antiplatelet drugs also used aspirin at 300 mg 3 times a day plus dipyridamole at 75 mg 3 times a day. This showed an increase in the incidence of hemorrhage. Lower doses of aspirin have been suggested to be more effective without increasing bleeding complications, although this has not yet been demonstrated in a prospective randomized trial. A syndrome specific to PV and other myeloproliferative syndromes is termed erythromelalgia, and it is associated with an increased risk of thrombosis. The symptoms are burning pain in the feet, hands, and digits, sometimes associated with pallor, erythema, or cyanosis of the distal portions of the extremities. Occasionally, it may progress to frank gangrene. In some instances, this is treated with aspirin (50-300 mg/d) and dipyridamole (75 mg orally 3 times a day). Myelosuppressive therapy plus phlebotomies, with the intent of normalizing the erythrocyte and platelet counts, also decreases or eliminates these symptoms. Proven thrombotic complications warrant the use of long-term anticoagulation with warfarin. SECONDARY POLYCYTHEMIA Secondary polycythemia is defined as an absolute increase in red blood cell mass caused by enhanced stimulation of red blood cell production. In contrast, polycythemia vera is characterized by bone marrow with an inherent increased proliferative activity. Enhanced erythroid stimulation results from the following: Causes: I. Acquired polycythemia due to a physiologic response to generalized or localized tissue hypoxia A. Generalized inadequate tissue oxygenation or hypoxia can be due to the following: Decreased ambient oxygen concentration, as occurs in people living at high altitudes, can result in compensatory erythrocytosis as a physiologic response to tissue hypoxia. Chronic obstructive pulmonary disease is commonly due to a large amount of ventilation in poor gas exchange units (high ventilation-to-perfusion ratios). Alveolar hypoventilation can result from periodic breathing and oxygen desaturation (sleep apnea) or morbid obesity (pickwickian syndrome). Cardiovascular diseases associated with a right-to-left shunt (arteriovenous malformations) can result in venous blood mixing in the arterial system and delivering low oxygen levels to tissues. Hemoglobin abnormalities associated with high oxygen affinity and congenital defects can lead to oxidized or met-hemoglobin. These conditions are usually familial. Exposure to carbon monoxide by smoking or working in automobile tunnels results in an acquired condition. Carboxyhemoglobin has a strong affinity for oxygen. B. Impaired perfusion of the kidneys, which may lead to stimulation of erythropoietin [EPO] production, is usually due to local renal hypoxia in the absence of systemic hypoxia. Conditions include the following: arteriosclerotic narrowing of the renal arteries, aneurysms affecting the aorta and renal vessels can lead to kidney infarction and hypoxia, focal glomerulonephritis. II. Inappropriate stimulation of EPO production Benign renal lesions, such as hydronephrosis and cysts, can stimulate EPO production, possibly due to compromised renal blood flow by compressive or vasoconstrictive mechanisms. Malignant and benign tumors that secrete EPO have been observed in patients with renal carcinomas, cerebellar hemangioblastomas, adrenal carcinomas, adrenal adenomas, hepatomas, and uterine leiomyomas. Blood doping is an illegal practice. Illicit use of androgenic steroids to build muscles and strength can also increase red blood cell mass by stimulating endogenous serum EPO levels. Congenital causes of high EPO levels are as follows: Hemoglobin mutants associated with tight binding to oxygen and a failure to deliver oxygen in the venous blood can cause high EPO levels. A von Hippel-Lindau gene mutation results in polycythemia by altering the von Hippel-Lindau protein, which plays an important role in hypoxia sensing. Chuvash polycythemia is caused by an autosomal recessive gene mutation on the von Hippel-Lindau gene, which results the upregulation of the HIF1-alpha target gene and causes elevations in EPO levels. Low EPO-dependent polycythemias o These are called primary familial and congenital polycythemias. o The EPO receptor mutation results in a gain of function, and patients have normal-to-high hematocrit values and low EPO levels. o These conditions can be acquired from (1) insulinlike growth factor-1, a wellknown stimulator of erythropoiesis, and (2) cobalt toxicity, which can induce erythropoiesis.