File
advertisement

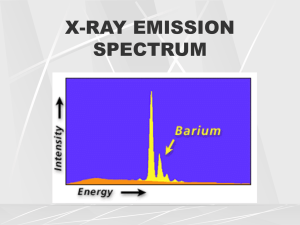
Radiographic Equipment Supertech TCF (Total Correction Factor) -control / generator cabinet -tube / collimator / stationary table / upright receiver -focal film distance indicators / turnstile for loaded cassettes / Nolan filters -positioning aids / lead apron and gloves / Nongrid cassette holder / darkroom -film flasher / Kodak ID camera / Konica SRX 301 processor -developer and fixer tanks / film storage 1) 2) 3) 4) choose a body part enter the appropriate TCF turn the supertech over select kVp, mA, time -it takes into account all of the variables involved: * X-ray generating system (single phase vs. high frequency) * film / screen speed (100,400/800, 600/1200) * grid ratio (non grid, 8:1, 10:1, 12:1) * focal film distance changes (40” or 72”) * processing variables (temperature, chemical concentration) How to establish your TCF? -work backwards from an existing good radiograph -use the penetrometer Working backwards from an existing good radiograph -from the exposure log find the part size (21 cm lumbar spine , AP) -you cannot set the TCF at this point -turn the Supertech over -find the time and mA (or mAs used) -line up the kVp next to that mAs value -turn the Supertech over again and there is your TCF for that exposure Making changes -focal film distance / grid ratio / body habitus / casts Calculate TCF at 72”, nongrid -TCF at 40 was calculated as -4 -from 40 to 72 add 3 ½ -going from 10:1 grid to nongrid subtract 3 ½ -the new TCF is -4 * the inverse square law change is balanced by removing the 10:1 grid from the beam 15% rule is built in -Supertech permits you to use kVp changes other than 15% to change contrast -there is a lower limit to kVp -must be enough to penetrate the body part How to account for children -children under the age of 12 have less calcium in their bones, compared to adults -use the red boxes (30% decrease in mAs for children) Change TCF for non normal patient -for patients with a muscular body habitus add a MINIMUM of +1 -for patient with a diminished bone density subtract a MINIMUM of -1 Exposure through casts -for plaster casts (if still wet, add +3 / if dry, add +2) -for fiber glass casts no adjustment is required New X-ray machine with programmed techniques -these programs often only anticipate one film / screen combination at a fixed FFD -you can use the Supertech to adjust the programmed technique for your circumstance Use the penetrometer -expose the penetrometer to 60kVp and 3.3 mAs at each mA station for high frequency generators (100 mA at 0.033 sec) (200 mA at 0.015 sec) (300 mA at 0.01 sec) -process the film -use the master film to determine TCF (the penetrometer image should be virtiually identical at each mA station) TCF test / Master film -bad test, 200 mA out of calibration (find unique correction factor) X-ray machine inventor -Wilhelm Conrad Roentgen (first X-ray taken of his wife Bertha’s hand = 1895) Properties of X-rays -no mass / no electrical charge -no travel at the speed of light / can penetrate most matter -travel in a straight line until they interact with matter -capable of making certain chemical compounds fluoresce -capable of exposing photographic film -can change biologic matter by ionization -radiation is either electromagnetic or particulate (alpha and beta are particulate) (x and gamma are electromagnetic) -part of the electromagnetic spectrum (ave wavelength = 10 to the power of -9 cm) (ave frequency = 10 to the power of 19 hertz) (ave energy = 60,000 electron volts) Electromagnetic Spectrum Gamma ray - X ray - UV rays - infrared rays - radar - FM - TV - short wave (~400 nm) (~700 nm) X-ray production (1) electron-target interaction (2) X-ray emission spectrum (3) factors affecting x-ray emission X-ray tube -an x-ray tube is a diode (anode + cathode) X-ray production (electron –target interaction) X-ray production -mA controls electrical current to filament on cathode (cathode block) -prep button spins rotor and sends electricity to filament (rotating anode effectively increases the area the electrons bombard by a factor of 2 * pi * radius over a stationary anode) -resistance causes filament to heat up -electrons are “boiled off” filament (thermionic emission) at 2000 Celsius -space charge effect = tendency to limit more electrons from escaping from the filament -exposure switch is depressed -kVp is applied across the cathode / anode (at 90 kVp, cathode is -45 kV, anode is +45 kV) -electrons are accelerated from cathode to anode, aka projectile electrons -the projectile electrons collide with anode (1A = 1C / s = 6.3 x 10 power of 18 electrons / sec ) at 100 mA , 6.3 x 10 ^ 17 -line focus principle -press / hold Prep button (heats filament, spins anode) -simultaneously press / hold expose button (must hold both buttons for the required time of exposure) -listen for the beep -release both buttons -if you release either / both buttons prior to the set time, you may see an error message (e.g. HYFOB) Line focus principle (figure 9-17) How anode angle affects focal spot size Target angle (10 / 12 / 14 / 16) vs. 40” and 72” Anode heat -the majority of energy used (99%) results in heat -outer shell electrons of target material are temporarily excited -as they fall back into orbit they release energy as infrared radiation (heat) -heat is directly related to mAs and kVp (heat units are calculated by multiplying kVp by mAs ) = single phase only for HF (x 1.4) (heat capacity determined by anode thickness and diameter) (150kHU standard upgrade to 400kHU) Thermal shock -extreme anode heating that results in damage (fracture) -to avoid anode damage, use the prescribed seasoning procedure prior to the first exposure of the day (example): lowest mA on large focal spot (80 / 90 / 100 / 110 kVp at 0.1 sec) 20 seconds between exposure Electric power P = IV -power (watts) is equal to current (amp) times electrical potential (volts) -if an x-ray exposure requires 70 kVp and 100 mA, how much power is required? (70 kVp x 100 mA = 7 kW) -25 kW tubes are standard, consider upgrading to 40 kW for bigger patients (90 kVp x 300 mA = 27 kW) = won’t work with a 25 kW tube! Anode heel effect -intensity of the beam is non-uniform in the long axis of the tube -if the central ray = 100%, intensity progressively decreases toward the anode and increases then decreases toward the cathode -variation in intensity ~ 30% (17” film at 40” FFD) figure 9-20 -decreased at longer FFD Beam Angle vs. FFD (focal field distance) Small vs. Large focal spot -talking about lesser or greater beam divergence (40” / 60” / 72”) -1 to 2 mm usual / 0.6 to 1.5 mm better -larger focal spot = bigger triangle Focal spot blur (aka Penumbra) (figure 10-28) Characteristic radiation Bremsstrahlung radiation -the radiation produced is characteristic for the anode material -depended on electron binding energies for the target material -projectile electron ionizes a K shell electron -electrons from higher orbits fill the “hole” -the change in electron binding energies results in photons with that keV value -braking (slowing, decelerating) radiation -projectile electron (negative charge) comes under influence of the nucleus (electric Coulomb force) -projectile electron changes direction, variably -change in direction causes bremsstrahlung x-ray photon production (conservation of momentum) -three electrons enter at different distances from the nucleus -three photons exit at different directions, different wavelengths About electrical waveform -alternating electrical current -single phase, full wave rectified waveform -three phase electrical waveform -6 kHz medium frequency electrical waveform (figure 2.12) -100 kHz high frequency electrical waveform (figure 2.12) Ripple factor -single phase = 100 % -medium frequency = 10% X-ray production (unfiltered beam) X-ray production -three phase = 10% -high frequency = 1% (1) x-ray emission spectrum . filtered beam, kVp > 70 (2) change in milliamperage, kVp > 70 (3) change in tube potential (4) effect of filtration, kVp > 70 mR per mAs (high frequency, 80 kVp, 200 mA, 0.5 s) = 790 mR X-ray quantity -the number of x-ray photons in an exposure beam -quantity = output intensity = radiation exposure - measured in roentgens ® or milliroentgens (mR) Measuring radiation -international community uses gray (Gy) and sievert (Sv) (gray is patient dose, one gray = 100 rads) (sievert is occupational exposure, one sievert = 100 rems) -1R is a measure of the amount of radiation needed to produce a number of ion pairs when air is x-rayed (2.08 x 10 to power of 8 ion pairs in a cubic cm of air) -in diagnostic x-ray 1R = 1 rem = 1 rad -the final measure is mR / mAs -at 70 kVp there is ~ 3 to 6 mR / mAs Factors affecting x-ray quantity (mAs): -quantity of x-ray photons is directly proportional -if the mAs is doubled, film density doubles (much darker) -if the mAs is halved, film density is halved (much lighter) (look at the back of supertech) (kPv): about 15% rule -an increase in kVp by 15% must be balanced by a 50% reduction in mAs (long scale of contrast, many shades of gray) -conversely a decrease in kVp by 15% must be balanced by a doubling of mAs (short scale of contrast: black / white) -the result, in either case, are two films of equivalent average density but a change in contrast kVp and patient dose Comparing doses -the average dose of full-field digital mammography at 1.52 mGy is less than that of screen – film mammography at 1.76 mGy, according to reports from FDA -an AP full spine on a patient measuring 23 cm requires ~125 mR ESE -a PA chest requires 15 mR ESE Inverse square law -to maintain the density of the film, if the FFD is increased 100% (40” to 80”) you need to quadruple the mAs to keep photon / in^2 the same -conversely, if you cut the FFD by 50% (80” to 40”) you would need one fourth the mAs to keep photon / in^2 the same and to create films of equal density -if you increase the distance by 50% (40” to 60”) you would double the mAs to keep photon / in^2 the same and to create films of equal density -build into supertech Q) Assume a technique at 40” produced an exposure dose of 300 mR. What would the exposure dose be if the tube was moved to 72” without changing the kVp or mAs? Q) Assume a technique at 72” produced an exposure dose of 300 mR. What would the exposure dose be if the tube was moved to 40” without changing the kVp or mAs? Q) Do I need to adjust the tube’s position when using a 15 degree tube tilt at 40”? This is AP lower cervical technique requires an exposure dose of 15 mR for a proper exposure? Q) How tube tilts lengthen the central ray? Q) How intensity falls off as FFD increases? Tube tilts and Keystoning X-ray quality -refers to the penetrating power of the beam -hard vs. soft x-rays (hard x-rays have higher kV values) (soft x-ray s have lower kV values) -measured by half value layer (HVL) (the thickness of an absorbing material necessary to reduce the intensity to ½ of its original value) (HVL increases with absorber thickness) -beam hardening with filtration (photons exiting tube = ave is 60) (photons exiting tube after additional filtration = ave is 80) -a uniform absorber, exponential absorption and half value layer (HVL) Factors affecting quality -kVp -filtration (type: inherent / added / compensating) -higher kVp, more total filtration required Filters (sectional filters): Nolan filters / Clear lead filters / Sportelli wedge filters -paraspinal filter -AP full spine: paraspinal filter to protect lungs insert to the level of the diaphragm (bottom of breast) add filter to protect cervical and upper thoracic region from overexposure also protects thyroid from unnecessary radiation note: no filter over upper cervical region -cervicothracic filter Five basic interactions -classic scattering -Compton effect -photoelectric effect -pair production -photodisintegration Classical scattering -aka coherent or Thompson scattering -between low energy x-ray photon and an atom -photon changes direction without loss of energy -no ionization -most scatter forward -may contribute to film fogging Compton effect -between moderate energy x-ray photons and an outer shell electron -photon changes direction, loses energy, ionizes atom creating a Compton electron -scattered photon may ionize another atom -may cause backscatter (180) -adds to film fog -increases with increasing kVp Electron binding energies, outer shell -calcium (M shell 25.4 eV) -hydrogen (K shell 13.6 eV) Arther Holly Compton Photoelectric effect -between moderate energy x-ray photons and an inner shell electron -photon loses all of its energy, ionizes the atom creating a photoelectron -produces characteristic x-rays (secondary radiation) in the object being x-rayed -secondary x-rays behave like scattered x-rays -the photoelectric effect has the highest probability with lower energy photons and atoms having a high atomic numbers Electron binding energies, inner shell -calcium (4038.5 eV) -phosphorus (2145.5 eV) Pair production -occurs with x-ray energies > 1.02 Mev -photon interacts with nuclear force field (emits a position and an electron) Photodisintegration -occurs with x-ray energies >10 Mev -photon absorbed by the nucleus itself -nucleus then emits a nuclear fragment Differential absorption -Compton scattered x-rays contribute no useful information -adds radiographic density, results in film fog -structures that absorb a great amount of x-ray are radiopaque (they appear whiter or lighter gray) -structures that allow x-rays to pass through are radiolucent (they appear black or darker) -the main difference is the atomic number of the structure Absorption of x-ray photons -the amount of absorption also depends on the number of electrons in the absorber (i.e., the atomic number) -the number of x-rays absorbed per centimeter of a material is proportional to the cube of the material’s atomic number -hence high atomic number materials like barium and iodine make good contrast agents and very high atomic number materials like lead provide maximum protection Differential absorption -generally less than 5% of x-rays that hit the patient reach the film -less than half of those interact with the film to form an image -therefore approximately 1% of the x-rays emitted from the tube make the image -at lower energies (kVp) the percentage of photoelectric interactions increases (relative to Compton) -to image small differences in soft tissue (renal stone) use low kVp technique (for maximal differential absorption) -you can “see” four things radiographically: (air: lungs, intestine / fat: fatty tumors / water:muscle, organs / metal: bones) -the interaction of x-rays and tissue is proportional to the density (specific gravity) of the tissue -attenuation is the reduction in the number of x-rays as they penetrate matter, x-rays are attenuated exponentially Compton vs. Photoelectric Grids -intensifying screens alone cannot adequately improve film contrast -selective filtration between the patient and film is ineffective -invented by Dr.Gustave Bucky, 1913 Why we call them Grids (1) a system of high tension cables by which electrical powers distributed throughout a region (2) a network of horizontal and vertical lines that provide coordinates for locating point on an image (3) an electrode placed between the cathode and anode of a vacuum tube to control the flow of electrons through the tube (4) a cooking utensil of parallel metal bars; used to grill fish or meat Principle function (improve film contrast) -grids are made of (1) grid material, usually lead (2) interspace material, may be plastic, aluminum, or fiber -note = fiber is hygroscopic resulting in uneven density on the resulting films and may cause the grid to wrap -grid material is approximately 50 microns thick separated by interspace material approximately 350 microns thick (some primary beam will be eliminated by the grid material) -grids remove between 80 to 95% of scatter emanating from the patent (depends on grid ratio) = 8:1 removes 80%, 16:1 removes 95% of the scatter Grid ratio -the height of the strip divided by the interspace thickness -ratios vary from 6:1 to 16:1 -in general practice 12:1 is most desirable -the higher the grid ratio the greater the patient dose Grid frequency -the number of lead lines per unit measure (e.g. 85 lpi or 103 lpi) -moving grids require fewer lines per inch -stationary grids must have the lines very close together so the lines become imperceptible on the resulting film Types of Grid -linear or parallel -focused -crossed Grid recommendations -12:1 ratio -103 lead lines per inch -focused from 40 to 72 inches -aluminum interspaced -appropriate size = 18” by 18” if you will only perform sectional films 18” by 36” if you will perform scoliosis radiography Problems (Grid cutoff) -off level -off center -off focus -upside-down Beam restricting devices -remnant x-ray = photons that exit patient and interact with the film -two types of photons interact with the film to form image: those which don’t interact with the patient and Compton scatter x-rays -collimation reduces patient dose by: -limiting the volume of tissue irradiated -secondarily reducing the amount of scatter (also reduces fogging) -failure to collimate is the greatest contributor to needless patient exposure Factors affecting scatter radiation How beam size affects scatter (part size): the more tissue in the path of the beam, the more scatter radiation there will be (e.g. morbidly obese patients) (field size): as the area of the beam enlarges, scatter increases the effect is seen more on smaller film / beamsizes (kVp): as kVp increases the relative number of Compton interactions increases in general high (optimal) kVp technique is preferred to low kVp technique due to patient dose considerations Round vs. Rectilinear collimation -the area of a 14 x 17 film is 238 square inches -the area of a circular beam, radius 11 inches, is 380 square inches -the are of a circular beam, radius 7 inches, is 154 square inches Beam restricting devices -patient thickness = the thicker the part the more scatter created -patient thickness is under your control -deciding to perform lumbar spine and abdominal films in the recumbent versus upright positions -if you decide to use patient compression -compression of the part increases image contrast Control of Scatter Radiation -use beam restriction and grid -beam restriction = aperture diaphragm cones or cylinders variable aperture collimator -light represents the size of the x-ray beam -aperture diaphragms are generally not suitable for general practice -cones are used primarily by dentists -general practice requires variable aperture collimator -variable aperture collimators (positive beam limitation) -off-focus radiation may be reduced by a first stage entrance shuttering device (accounts for approximately 25% of the patient’s dose) -second stage collimator shutter leaves are made of lead (at least 3mm thick), work in pairs, independently, yielding square or rectangular fields which compliment the film size being used -light localization by lamp and mirror -place rheostaton x-ray room lights -collimator bulbs are expensive, handle with tissue when installing -light must coincide with the x-ray beam Off-focus radiation -some electrons fly out of the stream, others hit the focal spot and rebound (bounce) but are pulled back toward the positive anode Control of Scatter Radiation -if you equipment is properly installed, aligned, and maintained the resulting film will show evidence of four sides of collimation -collimator adds about 1 mm of Aluminum filtration equivalent Air gap technique -the part is intentionally or necessarily separated from the film (results in an increased object film distance) -this allows scatter to physically miss the receiver -scatter that does intercept the film is attenuated by the inverse square law -this method works best with kVp settings below 90 (due to the direction of the scatter produced) -to offset the magnification created by the increased OFD a longer focalfilm distance is used -air does not appreciably filter the beam