Chapter 53 IA
advertisement

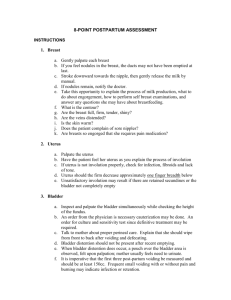
Chapter 53 Postpartum Care Instructional Approaches Approach: Maternal Physiologic Changes Review the maternal physiologic changes that occur during the postpartum period. Have students discuss assessments that are needed at this time. DISCUSSION/LECTURE The reproductive system is affected during the postpartum period. Involution is the return of the reproductive organs, especially the uterus, to their prepregnancy size and condition. Muscle fiber contraction, catabolism, and regeneration are completed in approximately 6 weeks. The fundus rises to the umbilicus and stays there for about 24 hours. The fundus descends about 1 cm, or one finger breadth, each day and descends in the pelvis and cannot be palpated abdominally after 10 days. Lochia, the uterine/vaginal discharge after delivery, is initially bright red, then changes to pink or pinkish brown, and finally to a yellowish-white color. It has a musty odor but should not have a foul odor. Foul odor may be a sign of infection. Lochia rubra lasts 3 days and is mostly blood that is bright red. Lochia serosa begins at approximately 4 days and is a pink to pinkish-brown color. After 10 days, lochia alba begins and the discharge becomes a yellowish-white color and may last 6 weeks. The cervix regains its shape and is closed by the end of 2 weeks, but the opening is more like a slit than a circle. It takes 6 weeks for the vagina to complete involution and regain its contour, but it will never regain its prepregnancy shape. The reduced level of estrogen may cause dyspareunia, or painful intercourse. The perineum may be bruised and have edema. Lacerations and episiotomies are classified according to the tissues involved. First degree is skin and mucous membrane; second degree is skin, mucous membrane, and muscle; third degree is skin, mucous membrane, muscle, and rectal sphincter; and fourth degree is skin, mucous membrane, muscle, rectal sphincter, and rectal mucosa. The endocrine system is also involved during the postpartum period. Levels of hormones fall rapidly, causing a reversal of the diabetogenic effect of pregnancy. The client’s glucose level must be closely monitored. Oxytocin causes breast milk to be produced and the let-down reflex to occur. Many women experience a tingling or burning feeling in the breasts when the milk is “let down.” In nonbreastfeeding mothers, ovulation recurs as early as 27 days after childbirth. Most nonbreastfeeding mothers resume menstruation within 3 months. The average time for ovulation to recur in breastfeeding mothers is 190 days after childbirth. Approximately 25 percent of breastfeeding mothers will ovulate before menstruating. Therefore, breastfeeding is not a reliable form of birth control. The breasts change during the postpartum period. Colostrum is produced during the last few weeks of pregnancy and is high in antibodies and protein. Engorgement of the breasts occurs at day three or four. If the breasts are not emptied, the engorgement will spontaneously disappear and discomfort will decrease in 24 to 48 hours. If the client never begins breastfeeding, or stops, lactation ceases within one week. The gastrointestinal system is also involved during this period. Most new mothers are hungry and thirsty. The client may have difficulty in having a bowel movement so should be monitored closely. The cardiovascular system is affected during the postpartum period. In a vaginal birth, blood loss averages 500 mL, while a cesarean birth causes an average blood loss of 1,000 mL. The new mother’s temperature may rise to 100.4 degrees during the first 24 hours because of dehydration. It should go back to normal within 24 hours but may rise again when milk production begins. The client’s pulse should not exceed 100 beats per minute. Periods of bradycardia may occur. The client’s pulse returns to her prepregnancy rate by 8 weeks after childbirth. Respirations will return to normal by 6 to 8 weeks, and there may be an increase in blood pressure that lasts about 4 days. Orthostatic hypotension may occur. Cardiac output remains elevated for at least 48 hours and eventually returns to prepregnancy levels at about 24 weeks. Excess plasma volume is eliminated by both diuresis and diaphoresis. The client’s white blood cell count increases to 20,000 or even 30,000 during the first 10 to 12 days as protection against invading organisms. Both the hemoglobin and hematocrit rise by the seventh day, unless excessive blood loss occurs. There is an increased risk for clots because of increased levels of clotting factors. Clients who have varicose veins, a cesarean birth, or a history of thrombophlebitis are at greater risk for thrombus formation. The urinary system is also affected. It is not uncommon for the client to have a urinary output of 3,000 mL per day for the first 2 to 3 days. Trauma and edema may result in difficulty in voiding. Bladder distention is common, especially in clients who have had regional anesthesia. Postpartum hemorrhage and urinary tract infection are two complications related to urinary retention and bladder overdistension. A full bladder displaces the uterus and causes excessive bleeding. Adequate emptying of the bladder helps the bladder regain its tone in 5 to 7 days after the birth. The musculoskeletal system is affected during the postpartum period. As relaxin decreases, the ligaments and cartilage begin to revert to their prepregnancy positions. Hip and joint pain is common. They stabilize by 6 to 8 weeks. It usually takes 6 weeks for the client’s abdominal muscles to return to the prepregnancy state. The integumentary system is involved as areas of hyperpigmentation from pregnancy begin to lighten in color. Some striae may still be visible. In some women, the linea nigra and nipple areola remain dark. Spider angiomas and palmar erythema usually fade. The neurological system is affected as well. If the client has had regional anesthesia, headache may be caused by a leakage of cerebrospinal fluid. The headache is more severe when the client sits or stands, and is relieved when she lies down. If the client experiences blurred vision, photophobia, and abdominal pain with a headache, it may indicate that she is developing pregnancy-induced hypertension. Approach: Maternal Psychosocial Changes Compare the symptoms of postpartum blues and postpartum psychosis. Have students identify why it is critical to identify psychosis early in the postpartum period. DISCUSSION/LECTURE Postpartum blues is a mild, transient condition of emotional lability and crying for no apparent reason that affects up to 80 percent of new mothers. It lasts up to 2 weeks. It is self-limiting, and the client may experience fatigue, anxiety, restlessness, headache, disappointment, and sadness. Postpartum psychosis is more severe and is characterized by delusions and thoughts of self-harm or infant harm. Symptoms, which usually begin within 2 to 3 weeks after birth, include fatigue, restlessness, insomnia, crying, labile emotions, inability to move, irrational statements, incoherence, confusion, and obsessive concerns about the infant’s health. Postpartum psychosis is a psychiatric emergency. Five percent of mothers commit suicide and four percent commit infanticide. Approach: Postpartum Assessment Divide the students into six groups and have each group use the acronym BUBBLE while describing the nursing assessments needed during the postpartum period. Saturate perineal pads with different amounts of food coloring to simulate bloody drainage. Have students assess each pad for the amount of drainage. DISCUSSION/LECTURE The acronym BUBBLE represents elements that should be assessed during the postpartum period: breasts, uterus, bladder, bowel, lochia, and episiotomy. Note the size and shape of the client’s breasts, including any abnormalities or reddened areas. Palpate the breasts for softness, firmness, engorgement, warmth, or tenderness. Check the nipples for cracks, fissures, soreness, or inversion. Palpate the uterus to find the fundus. Note the size, consistency, and placement of the uterus. It should be the size of a grapefruit, firm, and in the midline. It should descend approximately one finger breadth each day. Instructions should be given to the mother. Palpate the bladder to assess for distention and position. A distended bladder may cause hemorrhage. If the bladder is off to the side or the fundus is higher than usual, it is distended. Keep I&O for the first 24 hours. Inspect the bowel for distention and auscultate for bowel sounds. Inspect the anus and episiotomy. Encourage the mother to drink extra fluids, to eat a well-balanced diet with increased fiber, and to ambulate frequently. Assess lochia for color, amount, odor, and presence of clots. A few small clots are normal. Large clots and a foul odor should be reported to the physician. Assess the episiotomy while the client is in the Sims position. The upper buttocks are raised very gently. The anal area can be assessed for hemorrhoids at the same time. Assess the episiotomy for redness, ecchymosis, edema, discharge, and approximation of suture line. Approach: Cesarean Birth Have students discuss the differences and similarities in assessment when caring for a mother who has had a cesarean birth rather than a vaginal birth. DISCUSSION/LECTURE In addition to the assessments already discussed, postoperative assessments are needed. Inspect the incision for intactness and any bleeding or discharge. Assess the incision for redness, heat, pain, or edema, and the suture line for approximation. Assess respirations frequently, because narcotics depress the respiratory center. Respiratory rate and depth should be assessed every 15 minutes for the first hour, every 30 minutes for the next 4 to 5 hours, and every hour for the remainder of the first 24 hours. Breath sounds are auscultated and coughing, breathing, and use of incentive spirometer must also be assessed. Assess the abdomen for softness or distention. Bowel sounds should be auscultated until peristalsis returns and the client passes flatus. Assess the flow rate and site of intravenous fluids. Assess the amount of urine and monitor the Foley catheter. Pain medication is usually required for 24 to 48 hours after delivery. Student Learning Activities 1. Divide the students into groups and have them research the most common complications that occur in the postpartum period. Have them present the information to the class. Assessments, nursing interventions, and medical–surgical management in the text should be discussed. In addition, students should find statistics on the Internet and share causes and prevention of complications in class. 2. Fill balloons with various amounts of water and cover them with a gown. Have students assess for a boggy uterus or full bladder. Have them demonstrate the appropriate nursing interventions while verbalizing nursing rationale. 3. Classroom discussion tool: Have students review the case study and use the questions as a basis for discussion. Resources Albright, A. (1993). Postpartum depression: An overview. Journal of Counseling Development, 71(3), 316. Green, S. E., & Adams, W. M. (1993). Chronic psychiatric illness and pregnancy: Nursing implications. Journal of Perinatal, Neonatal Nursing, 7(3), 7–18. Johnson & Johnson. (1996). Compendium of postpartum care. Skillman, NJ: Johnson & Johnson Consumer Products. Luegenbiehl, D., Brophym G., Artigue, G., Phillips, K., & Flack, R. (1990). Standardized assessment of blood loss. The American Journal of Maternal/Child Nursing, 15(4), 241–244. Web Activities 1. Association of Women’s Health, Obstetric and Neonatal Nurses: www.awhonn.org. 2. Search the Web for information about postpartum depression and postpartum psychosis. Would this information be appropriate for or helpful to clients? What organizations are available to help clients? 3. What information is available on the Internet about the various complications that can affect a client during the postpartum period? Suggested Responses to the Case Study Jeff and Meli Lahoti had their third child, a second son, yesterday. The baby weighed 8 lbs, 10 oz, the largest of their three children. The labor lasted 5 hours. An episiotomy was performed this time but had not been for the previous births. Meli is having problems walking to the bathroom and says she feels faint and dizzy when she stands up. She talks constantly about the pain from the episiotomy. A bruised, edematous area is noted beside the episiotomy. Analgesics provide little relief. Plans were to breastfeed this infant as she had the first two. Today she does not want to feed the baby because she “hurts too much.” The following questions will guide your development of a nursing care plan for this case study. 1. What assessments should be made? Vital signs, fundus, lochia, episiotomy 2. Identify three nursing diagnoses for Meli. Nursing Diagnosis 1: Deficient Fluid Volume, Risk for, related to excessive loss through abnormal route as evidenced by bruised, edematous area next to episiotomy Nursing Diagnosis 2: Pain, related to physical injury as evidenced by client expression of discomfort Nursing Diagnosis 3: Breastfeeding, Interrupted, related to maternal pain as evidenced by Meli’s statement that she “hurts too much” 3. Identify planning/goals for Meli. Meli will maintain adequate fluid volume. Meli will experience less pain. Meli will return to breastfeeding her infant. 4. List nursing interventions to help Meli meet the goals. A1. Notify CNM/physician about bruised, edematous area next to episiotomy. A2. Monitor fundus, lochia, and episiotomy. A3. Apply ice pack to episiotomy/bruised area for 20 minutes; wait at least 10 minutes before reapplying the ice pack. A4. Assist Meli with perineal care. A5. Monitor vital signs for indication of infection or shock. A6. Keep CNM/physician informed of assessments and Meli’s response to care. B1. Ask Meli to rate pain, on a scale of 0 to 10 (0 = no pain, 10 = worst pain). B2. Administer analgesic as ordered. B3. Monitor episiotomy and bruised area. B4. Implement new orders from CNM/physician. C1. Administer analgesic 30 minutes before expected feeding time. C2. Assist Meli to the bathroom. C3. Help Meli get comfortable in bed, and assist her with infant during breastfeeding. 5. How can the effectiveness of this plan be evaluated? By the degree to which each goal has been met. Answers to the Review Questions 1. The nurse observes passive and dependent behaviors displayed by a postpartum client. According to Reva Rubin, the client is in the: a. taking-in phase. 2. A client has excessive vaginal bleeding after delivery. The assessment reveals a soft, boggy uterus located above the level of the umbilicus and displaced to the right side. The first action of the nurse should be to: c. initiate measures that encourage voiding. 3. A new mother tells the nurse that she is afraid of her baby and that she doubts that she will be able to love the baby. The most appropriate action for the nurse would be to: c. encourage the client to talk about her feelings. 4. A client has excessive vaginal bleeding following the birth. The nurse should suspect a cervical or vaginal tear if client assessment reveals: b. a hard, contracted uterus. 5. A client wants to know when she can begin breastfeeding and is anxious for her milk to start. The best response of the nurse would be: c. “We encourage you to breastfeed as soon as you wish. Your milk will probably ‘come in’ in about 3 days.”


![Title: [S4- poster] A longitudinal study of postpartum depression](http://s3.studylib.net/store/data/008396555_1-6c02377a087cf9a182a8798d6fbda024-300x300.png)