Preinstallb - MidWest Clinicians' Network
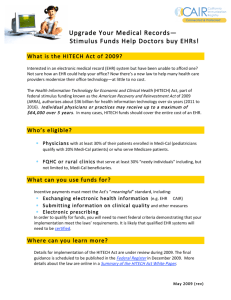
advertisement

Pre-Install Table of Contents EHR Implementation Checklist 2 Electronic Health Record Implementation in Physician Offices: Critical Success Factors 4 EHR Implementation Team 9 EHR Implementation Team Role and Responsibility Matrix 10 EHR Goal Setting 11 Transition Readiness Assessment 13 Issues Log 16 Computer Knowledge Evaluation Tool for Physician Staff 20 Staff Meeting Skills and Agenda Template 21 Huddles 23 Scanning and Back loading Tips 25 Workflow Assessment Guide 27 Processes 34 Return on Investment 36 EHR Implementation Checklist Task Date Complete___ � Establishment of Project Team Physician champion(s) Project manager Additional practice/department champions Subject matter experts ___________ � Development of Project Plan Scope document Implementation schedule/timeline Roles and responsibilities Change management process Issue tracking and management process ___________ � Communication ___________ Setup regularly scheduled meeting with vendor implementation staff Provide staff regular updates Post implementation timeline in break room and mark overall progress Utilize newsletters, email, etc. to address specific topics or issues � Mapping of Critical Practice Workflows ___________ Identify problem areas and bottlenecks Re-map practice workflows based on incorporation of EHR into them � Handling of Existing Data Identify key information and documents that need to be in system Develop plan for entering them into system Develop plan for handling new, outside documents and information ___________ � Training ___________ Assess PC and keyboarding skills of staff Establish plan for developing staff’s PC and keyboarding skills Have vendor conduct general overview of system for all staff prior to formal training Conduct multi hands-on, task oriented sessions tailored to staff responsibilities Identify “super users” and ensure they receive additional training sessions Allow staff on-the-job learning time to familiarize themselves with system Develop appropriate education material, such as cheat sheets, quick reference cards, diagrams of new workflows Pre-Install 2 of 38 EHR Implementation Checklist continued Task Date Complete___ � System Testing ___________ Conduct unit testing (i.e., single module) Conduct integration testing (i.e., interaction between two or more modules) Conduct interface testing (i.e., interaction between systems) Conduct system stress or load testing Ensure testing plans cover different scenarios and situations � Contingency Planning ___________ Develop disaster recovery plan Test ability to restore system from backups prior to go-live Ensure system backup plan in place and running Arrange for regularly scheduled pick up and off-site storage of backups � Go-Live Planning ___________ Determine amount physicians’ schedules will be reduced (if any) Determine rollout approach: Incremental vs. ‘big bang’ All physicians vs. physician champions All practice locations vs. select ones Allow time during day for providers to “catch up” Mid-morning and mid-afternoon buffers, or Extra minutes per visit Ensure sufficient resources available to support staff and physicians Make sure staff and physicians know who they can go to for assistance Inform third parties and other vendors, e.g., labs, transcription, etc. of go-live date so they’re prepared to provide additional support Plan for what to do if things go really wrong Identify situations or points where go-live needs to be stopped Decide what to do if that happens, e.g., go back to paper processes Schedule midday “huddle” to evaluate progress Schedule end-of-day debrief to identify and address issues Bring food, patience, and sense of humor Plan to celebrate Pre-Install 3 of 38 Electronic Health Record Implementation in Physician Offices: Critical Success Factors Overview Evidence suggests that implementation and adoption of electronic health records (EHRs) in the physician office has the potential to improve quality of care , as well as provide a positive return on investment (ROI) for the physician practice. Although “successful implementation” may be crudely defined as improved quality of care measures and a positive return on investment, a review of the literature on health information technology (IT) project implementation suggests that successful EHR implementation should be understood in a much more complex framework. i ii Implementation refers to the process of introducing an EHR into a physician office. “[T]he effort of designing, implementing, and using an information system involves numerous considerations and a series of processes that change the organization, the people and the information system involved” iii. “Successful” implementation of an electronic health record in the physician office involves application of technical, project management, and organizational skills, and embodies much more than mere installation of appropriate hardware and software. As Wager et al succinctly states, Technical success alone does not ensure the EMR will be accepted and used by physicians…[T]he success of EMR implementation and utilization depends on the integration of the system into an often complex organizational setting. iv Additional research supports this conclusion. In a case study of five community-based practices, all of which implemented the same EHR system, the authors found that the same EHR in comparable settings was viewed very differently. They conclude that within the practices analyzed, “perceived success or failure of the EMR system appeared to be related to organizational factors that were present before or during system implementation”. v Literature describing implementation of EHRs into physician offices emphasizes the importance of broader organizational context and the effects that EHR introduction has on office workflow and culture. Given the importance of these factors in the implementation process, evaluation of medical informatics projects is increasingly taking into account the “social, organizational, political, and other non-technical factors surrounding an information systems project”. In a report titled “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience”, Keshavjee et al state, “[i]nitial success of EMR implementation is largely dependant on managing the stress of the major change in the practice” and depends on a “perception that sufficient value is gained from the change to justify the costs” i Proper planning, training, and organizational mobilization are critical success factors to EHR implementation. vi vi EHR Implementation: Phases and Benchmarks of Successful Implementation As the framework below reflects, a large proportion of the effort associated with implementation should occur before the actual system is installed. Critical to project success is the up-front investment of time and energy. To illustrate this, in an eight-phase IT project framework outlined by Worthley in his textbook, Managing Information in Healthcare, “system installation” is the seventh step in the process. The majority of the implementation process precedes installation, and involves problem identification, system design, and testing. viii ix Various implementation and IT project management processes have been put forth in the literature. The outline below highlights dominant themes and factors identified with successful EHR implementation, but is not intended to serve as a comprehensive “checklist” or sequential timeline to successful implementation. Rather, it is intended as a broad framework to identify many of the key broad and widely cited critical success factors for EHR implementation. It is broken down into three major phases: PrePre-Install 4 of 38 Electronic Health Record Implementation in Physician Offices: Critical Success Factors Installation, Installation, and Post-Implementation. As the literature suggests, the majority of critical success factors fall into the “preinstallation” phase. Pre-Installation Identify Physician Champion In a study of solo/small physician practices in California, the authors state, “identify an EMR Champion- or don’t implement”x. The importance of strong physician leadership is underscored in the literature. The literature broadly emphasizes the importance of a physician champion to drive HER implementation. The following characteristics are associated with this lead: o Formal or informal authority to lead change: A well-respected leader who is “powerful enough to make things happen”. xi o Commitment to EHR implementation and ability to sell benefits to other physicians and office staff. To be successful, physicians and office staff must “buy-in” to the project.xii This leader must be careful to set realistic expectations.xiii Prepare Organization for Change Change management is critical to successful EHR implementation. Prior to implementing and installing an EHR, a leader must prepare the organization for change by identifying core values, understating broader organizational context and stakeholder concerns, understanding end-user needs, creating a vision for change, and being sensitive and responsive to organizational stress resulting from change.xiv Identify Strategic Objectives A critical element in preparing an organization for the change that will result from implementation of an informatics project is “identifying key core values and focusing efforts on those.” xv Clarifying areas for practice improvement in quality and efficiency helps to focus IT solutions on these areas.xvi o Strategic alignment of IT investments with the practice’s clinical and business strategies is one important critical success factor for organizations that wish to assess the ROI of IT investments.xvii Gain Support of Organizational Leadership/Secure Management Commitment The importance of organizational support is one of the most dominant factors associated with successful implementation of EHR. Support from management and/or senior leadership helps ensure adequate resource commitment, critical to successful implementation. xviii Such resources are “needed to build an infrastructure to support the system and its users over time” and include not only up-front investment in hardware and software, but also time and staff allocation. xix In one study of EMR implementation in an ambulatory care setting, the authors found an association between perceived usefulness of an EMR and organizational support. The authors explain, “By providing strong support for the redesign effort, management can communicate its commitment to the EMR investment”.xx Involve Multiple Stakeholders Involve the entire staff including upper management and administrative staff in implementation and training activities. Being able to meet the needs of conflicting stakeholders, including physicians, nurses, office staff and administrators, as well as vendors and patients requires a strong project manager who can ascertain broad needs, build support, and effectively negotiate solutions. xxi Good Project Management Establish project infrastructure (i.e. project team, including project manager, physician champion) to support proper planning and ongoing support of the project. xxii Pre-Install 5 of 38 Electronic Health Record Implementation in Physician Offices: Critical Success Factors Consider Workflow Redesign • “To be successful, health informatics systems need to support- or at least not be in conflict with the organizational structures of the organization in which the systems are implemented.” • In one case study of EHR implementation in a solo pediatric practice, one critical success factor identified was the minimal amount of “reengineering” that occurred in re-designing workflow: automated processes reflected, and sometimes simplified the physician’s manual workflow. xxiii Conduct Research • The process of choosing software is “an important time to learn about the strengths and weaknesses of the EMR, the vendor who is selling it and the type of support that is likely to be required for the EMR product” • Site visits and speaking to experts helps establish realistic expectations for physicians looking to implement systems. xxiv xxv Offer Hands-On Training and Testing of Software • Hands-on training, geared at appropriate computer skill levels is critical. “Hands-on training with a software demonstration program, or a simulated demonstration model should occur early and often, and be tailored to the needs and work schedules of the physicians.” xxvi Installation “Go Live” Go live date should be “boring” because all staff has had experience testing and using software. - Application/installation of hardware/software: Computer hardware should be selected and ordered well before installation. Staff should already be familiar with the hardware from training activities Cable high volume work areas and exam rooms xxvii xxviii Post-Installation Ongoing EMR Quality Improvement and Management One EHR Implementation methodology suggests that after the EHR software is installed, the ongoing management should be “handed over” to an office support team. As software, technology and medicine change, practices will continually have to adapt. Building flexible systems and continuous improvement of management processes are among the critical issues to consider in analyzing the success of health informatics projects xxix xxx Ensure Ongoing IT Support: Vendor and/or In-House Vendor support: The importance of proper technical support cannot be understated. Various authors cite the importance of vendor support On-site technical support: It is important to have on-site support to make adjustments to the system, and address technical issues that arise. In one literature review, the authors report many successful implementation efforts involve physician “super-users” who assist in training of others. “Super-users are those physicians who rapidly become expert users such that other physicians can call upon them for assistance.” Customizing EMR: Some reports suggest that the ability to customize an EHR to physician and practice needs is related to the success of EHR implementation . However, opinions in the literature regarding the importance of EHR customization are mixed. In a literature review of best practices in EHR implementation, Keshavjee et al found the ability to customize software was cited in the literature much less frequently than many other critical success factors. “Many authors neglected to mention whether their software was customizable, xxxi xxxii xxxiii Pre-Install 6 of 38 Electronic Health Record Implementation in Physician Offices: Critical Success Factors whether they did any customization work or whether they thought customization of EMR software was important to achieve success in their implementation” “Most implementers mentioned that special problem-solving teams involving technical people, trainers, nurses and physicians were an important tool to help achieve course corrections when problems start arising after ‘go-live’. Problems were considered inevitable and having dedicated staff to help users resolve their problems and achieve productivity goals is an important tool for implementers as they computerize practices.” xxxiv xxxv System Evaluation: Have Objectives Been Met? Evaluation of the EMR implementation provides opportunity to assess adoption and ascertain whether new problems have arisen. xxxvi Miller, R. H. and Sim I. Physicians’ Use Of Electronic Medical Records: Barriers And Solutions. Health Aff, 2004; 23(2): 116-126. K, Metzger J. Achieving tangible benefits in small physician practices. First Consulting Group. Oakland, CA: California Healthcare Foundation. September 2002. Available at: http://www.chcf.org/documents/ihealth/AchievingITBenefits.pdf. iii Kaplan B. “Addressing Organizational Issues into the Evaluation of Medical Systems.” J Am Med Inform Assoc 1997; 4(2):94-101. iv Wager K et al. Impact of an Electronic Medical Record System on Community-Based Primary Care Practices. J AM Board Fam Pract 2000; 13(5): 333-348 v Wager K et al. Impact of an Electronic Medical Record System on Community-Based Primary Care Practices. J AM Board Fam Pract 2000; 13(5): 333-348 vi Kaplan B. “Addressing Organizational Issues into the Evaluation of Medical Systems.” J Am Med Inform Assoc 1997; 4(2):94-101. vii Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. Available at: http://www.competestudy.com/Successful_Computerization_in_Small_Primary_Care_Practises.pdf viii Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. ix Worthley JA. Managing Information in Healthcare: Concepts and Cases. Chicago, IL: Health Administration Press; 2000. x Miller, R., Sim, I., and Newman, J. (2003). Electronic medical records: Lessons from small physician practices. California HealthCare Foundation. Available at: http://www.chcf.org/print.cfm?itemID=21521. Accessed on: 6/3/2004. xi Wager 2000, Disastrous; Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xii Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xiii Casey A, Drazen E, Metzger J, Patrino K. “Eleven Critical Success Factors for Implementing Electronic Medical Records.” Available online at: http://www.medicalogic.com/emr/user_experience/eleven_factors.html ; Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xiv Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xv Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xvi Worthley JA. Managing Information in Healthcare: Concepts and Cases. Chicago, IL: Health Administration Press; 2000. ; MacDonald K, Metzger J. Achieving tangible benefits in small physician practices. First Consulting Group. Oakland, CA: California Healthcare Foundation. xvii Arlotto P. Pam Arlotto, Healthcare IT Strategist, Shares Insight on the ROI Process and IT J Helathc Inf Mgmt Fall 2003 17(4) 18-19. i ii MacDonald xviii xix Wager K et al. Impact of an Electronic Medical Record System on Community-Based Primary Care Practices. J AM Board Fam Pract 2000; 13(5): 333-348 xx Dansky KH, Gamm LD, Vasey JJ, Barsukiewicz CK. Electronic medical records: are physicians ready? J Healthc Manag. 1999 NovDec;44(6):440-54; discussion 454-5. xxi Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xxii Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. Available at: http://www.competestudy.com/Successful_Computerization_in_Small_Primary_Care_Practises.pdf xxiii Cooper J “Organization, Management, Implementation and Value of EHR Implementation in a Solo Pediatric Practice”. J Healthc Inf Manag 2004; 18(3), 51-55. xxiv Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report Online. xxv Casey A, Drazen E, Metzger J, Patrino K. “Eleven Critical Success Factors for Implementing Electronic Medical Records.” Available online at: http://www.medicalogic.com/emr/user_experience/eleven_factors.html xxvi Dansky KH, Gamm LD, Vasey JJ, Barsukiewicz CK. Electronic medical records: are physicians ready? J Healthc Manag. 1999 NovDec;44(6):440-54; discussion 454-5. xxvii Casey A, Drazen E, Metzger J, Patrino K. “Eleven Critical Success Factors for Implementing Electronic Medical Records.” Available online at: http://www.medicalogic.com/emr/user_experience/eleven_factors.html xxviii Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001 xxix Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. xxx Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: Springer-Verlag. 1995. xxxiCasey A, Drazen E, Metzger J, Patrino K. “Eleven Critical Success Factors for Implementing Electronic Medical Records.” Available Pre-Install 7 of 38 Electronic Health Record Implementation in Physician Offices: Critical Success Factors online at: http://www.medicalogic.com/emr/user_experience/eleven_factors.html ; Cooper J “Organization, Management, Implementation and Value of EHR Implementation in a Solo Pediatric Practice”. J Healthc Inf Manag 2004; 18(3), 51-55. xxxii Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. xxxiiiCasey A, Drazen E, Metzger J, Patrino K. “Eleven Critical Success Factors for Implementing Electronic Medical Records.” Available online at: http://www.medicalogic.com/emr/user_experience/eleven_factors.html;Cooper J “Organization, Management, Implementation and Value of EHR Implementation in a Solo Pediatric Practice”. J Healthc Inf Manag 2004; 18(3), 51-55. xxxiv Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. xxxv Keshavjee K, Troyan S, Langton K, et al “Successful Computerization in Small Primary Care Practices: A Report on Three Years of Implementation Experience” Canada: COMPETE, 2001. Report online. xxxvi Worthley JA; Lorenzi N, Riley RT. Organizational Aspects of Health Informatics: Managing Technological Change. New York: SpringerVerlag. 1995. Pre-Install 8 of 38 EHR Implementation Team Selecting the right people for your EHR implementation team is a critical step in a successful implementation. In general, members of your team should be enthusiastic, well respected, and forward thinking. Team members should bring to the project differing perspectives on how the EHR will be used and provide a wide array of skills and knowledge. The size of your practice will determine the size of your implementation team. For smaller practices, one person may be managing several of the areas of responsibility listed below. Physician Champion An EHR implementation should not begin without a physician champion. The role of the physician champion is to act as a liaison between the physicians in the group and the implementation team. The physician champion acts as a point of reference for how things are done from a clinical perspective and how physicians need the EHR application to function. The physician champion is responsible for keeping the physicians up to date on the progress of the EHR and for maintaining physician “buy-in” to the project. Project Manager The project manager is responsible for keeping the project moving. In most implementations, there is a vendor counterpart to this position. The project manager is responsible for monitoring the work plan to ensure that the project is on schedule; maintaining a list of vendor and practice issues that need to be resolved; scheduling implementation-related events, such as hardware deliveries and live dates; and delegating tasks to the other members of the implementation team. In a small practice setting, the project manager is usually responsible for communicating updates to the rest of the practice. EHR Builder This person is responsible for building and customizing any EHR application areas such as templates, drop-down boxes and pick lists. This person will know more about how the EHR functions than any other person in the practice. This person may also have regular communication with the EHR vendor. Application Trainer Depending on the size and needs of the practice, an application trainer may be necessary. This person would be responsible for training new practice staff on the EHR application. This person may also assist with building tasks. Registration User Liaison This team member is responsible for providing input into the registration process. This person will become the EHR super user for the registration area. Billing User Liaison This team member is responsible for providing input into the billing process. This person will become the EHR super user for the billing area. Medical Records User Liaison This team member is responsible for providing input into the medical records process. This person will become the EHR super user for the medical records area. Technical Support This team member is responsible for the daily maintenance of the EHR servers, including running backups and applying upgrades to the system. This person should receive training from the vendor on recommended server maintenance. This person may also assist with developing and maintaining interfaces. Pre-Install 9 of 38 EHR Implementation Team – Role & Responsibility Matrix Role Physician Champion Project Manager EHR Builder Application Trainer Registration User Liaison Billing User Liaison Medical Records User Liaison Technical Support Responsibility Person Assigned Acts as a liaison between physicians in the group and the implementation team. Provides point of reference from a clinical perspective, including how physicians need EHR to function. Keep other physicians up to date on progress and maintain “buy in”. Day-to-day ownership of project, monitor workplan to keep project on schedule, track issues for resolution, schedule implementation related events, communicate the project’s progress to remainder of staff Building and customizing of any EHR application areas: templates, drop-down boxes, pick lists. Person with most knowledge about EHR’s functions. Training of new staff on EHR, assist EHR Builder Provide input on registration process. Become a super user for registration area. Provide input on billing process. Become a super user for the billing area. Provide input on the medical records process. Become a super user for medical records area. Daily maintenance of EHR servers, run backups and applying system upgrades*. Assist with developing and maintaining interfaces. (*not applicable for ASP model approach) Other: Pre-Install 10 of 38 Comments EHR Goal Setting The purpose of this tool is to help you define your goals for quality improvement and to help you target which features of the EHR will be critical to your quality improvement efforts. If you can define your goals, you can define your needs. If you can define your needs, you can select an EHR system that will meet your needs. Getting Started: Start with a workflow analysis and identify the bottlenecks and inefficiencies that exist today. Decide which bottlenecks and inefficiencies you want to improve and assign them a priority. It doesn’t matter so much where you start—as long as you start somewhere. In setting priorities, you may want to consider the following: In what areas is our performance far from ideal? What improvements do we think our patients will notice most? Where do we think we can be successful in making change? What groups of clinicians and staff should we involve in each item, and what is their readiness for change? Goal Definition: Set clear, measurable goals for what can be done to improve the existing conditions. You may want to state some of your goals in a patient focused manner—such as decreasing the time patients wait for prescription refills or increasing the number of patients who receive preventative health reminders. Tell your patients about these goals. Let them know that you are trying to make their experience in your office better. Have some fun with goal setting. Involve everyone in the office by asking for creative suggestions on ways to eliminate inefficiency. Action Plan: For each goal, define a plan of action for achieving the goal. What specific steps do you need to take to reach your goal? Measuring Success: Determine how you will measure the success of your action plan. Keep it simple! Don’t get hung up on statistics, sample size and complicating factors. Incorporate your baseline measurements from the workflow analysis. You’ll need something to compare your quality improvement efforts to. If you don’t meet your measurement for success the first time, re-evaluate, and try again. Quality improvement is a never-ending task. Pre-Install 11 of 38 EHR Goal Setting Examples: Goal: Action Plan: Measure of Success: Goal: Action Plan: Measure of Success: Goal: Action Plan: Measure of Success: Goal: Action Plan: Measure of Success: Decrease the number of pharmacy phone calls regarding prescriptions. Use the e-prescribing feature in the EHR to eliminate paper and handwritten prescriptions. Utilize the drug interaction checking feature of the EHR to guard against drug interactions. In two months, have an 85% reduction in pharmacy phone calls. Decrease transcription turnaround time and reduce transcription cost. Use clinical charting within the EHR to eliminate the need for transcription services. Within two months of EHR live, reduce the cost of transcription by 80%. Improve the quality of patient care for CAD patients. Use the EHR’s health maintenance tracking to monitor antiplatelet therapy. 95% of patients with CAD have been prescribed antiplatelet therapy. Decrease waiting room time for patients. Encourage patients to use the PC’s in the waiting room to update their demographics and insurance information. Within one month, 75% of patients wait no longer than 10 minutes in the waiting room. More sample goals to consider: • Improve patient access to the physician • Decrease the number of times the physician leaves the exam room during a visit • Increase the quantity/quality of patient education materials given to the patient • Decrease the number of calls to the lab for results/follow up • Increase the number of patients who receive reminders for age/sex appropriate preventative health measures. • Increase the number of patients who actually receive preventative health exams/procedures References: Building a Mind-Set of Service Excellence. Paul Plsek, MS. AAFP Family Practice Management, April 2002. Transition Readiness Assessment Organizational change can be smooth and straightforward or filled with setbacks and challenges. While you cannot plan for every eventuality, you can take steps to ensure that your organization is ready for change. To address potential problems, it is necessary to assess your group to determine where those problems may arise. This readiness assessment is intended to give you the data you need to locate and address areas of potential concern before they become problems during a time of transition. Taking this assessment You can take this assessment yourself to clarify your observations about the readiness of your organization to implement changes. For a wider view of the organization, it is recommended that you have a number of people from across the organization fill out the survey. The more people who fill out the survey, the better gauge you will have of your organization’s readiness for change. Encourage honesty in answering. This should be a reflection of how the organization currently is, not a reflection of an ideal. Other uses While this tool is primarily designed to reflect strengths and weaknesses in the organization prior to change, it can also assess the climate of group before and after a change. Often, it is a good idea to reassess at some point after a change has been made in order to show that the change has been an improvement. It can also be useful to gauge whether different levels in the organization are operating under the same assumptions about openness and performance. If managers and staff are not on the same page, there is more likely to be resistance to any efforts at making changes. Evaluating the Results To evaluate the results of the survey, average the total scores of all the people who filled out the survey. This will give you an overall picture of whether your organization is ready for change. Next, add the scores for each question individually so you can average the answers for each one. This will allow you to pinpoint your organization’s strengths and the problems that need to be addressed to promote smooth transitions. It is helpful to have the aggregate answers to show, in an impersonal way, areas that need to be addressed. Leadership and trust are potentially divisive issues, so it can be helpful to be able to address them in a nonconfrontational manner. Pre-Install 13 of 38 Transition Readiness Assessment Choose one: ___ I am filling out this assessment for the organization as a whole. ___ I am filling it out for a particular site, department, or other part of our organization. Which one? And answer this: The change for which I am assessing our transition readiness is as follows: Answer each question with the following numbers: 4 = The statement is definitely true or accurate. 3 = The statement is largely (though maybe not completely) accurate or true. 2 = The statement is only partly true or accurate. 1 = This is only occasionally (but not very often) true. 0 = The statement is utterly false. 1. _ _ Most people think that the change in question is a necessary one. 2. _ _ Most people agree that — given the situation — the change represents the best way of dealing with it. 3. _ _ The organization's leaders have shown that they are committed to the change. 4. _ _ In general, the middle managers are behind the change. 5. _ _ So are the supervisors or first-line managers. 6. _ _ The details of the change are being communicated to those who will be affected quickly as it is practical to do so. 7. _ _ There are effective ways for employees to feed back their concerns and questions about the change. 8. __ And those concerns and questions have, thus far, been responded to in a pretty Pre-Install 14 of 38 as honest and timely way. 9. _ There aren't a lot of old scars or unresolved issues around here. 10. _ _ The organization has a history of handling change pretty well. 11. _ _ The organization's leadership has a history of doing what it says it will do. 12. _ _ . . . and of saying what it is going to do before it does it. 13. _ _ I think if this is what the leadership wants to do, they can pull it off successfully. 14 _ _ Decisions generally get made in a timely fashion around here. 15. _ _ When people get new roles or tasks, they can usually count on getting the training and coaching that they needed to do them. 16. _ _ When faced with new and challenging situations, the organization forgets turf-issues and gets problems solved. 17. _ _ It is safe to take an "intelligent" risk in this organization; failure in a good cause or for a good reason isn't punished. 18. _ _ There is a pretty widely understood vision of what the organization is seeking to become and to accomplish. 19. _ _ While the higher-ranking people obviously get paid more, we feel like we're all in this thing together. 20. _ _ People's commitment to their work here is as high as it was a year ago. 21. _ _ Although the pace and extent of change around here is great, it is also workable. 22. _ _ Management generally practices what it preaches. 23. ___ There is basically no argument about what the organization's problems are around here. 24. _ _ The organization's leadership generally shows an awareness of and concern for how change will affect the rest of us. 25. _ _ People generally understand how things will be different when the change is finished. _____ TOTAL SCORE Pre-Install 15 of 38 Issues Log Describe Issue Internal issue External/Vendor Date Issue Communicated Pre-Install 16 of 38 Date Resolved Issues Log Describe Issue Internal issue External/Vendor Date Issue Communicated Pre-Install 17 of 38 Date Resolved Issues Log Describe Issue Internal issue External/Vendor Date Issue Communicated Pre-Install 18 of 38 Date Resolved Issues Log Describe Issue Internal issue External/Vendor Date Issue Communicated Pre-Install 19 of 38 Date Resolved Computer Knowledge Evaluation Tool for Staff Technological Skill Functional Skills – I can/am able to: Use a computer mouse to point and click Use a computer keyboard File Management- I can/am able to: Create and rename a folder Move file(s) from one folder to another Save and delete a file Find a file using Windows explorer Zip and unzip a file Empty the recycle bin and retrieve a deleted file from the bin if necessary Operations – I can/am able to: Use the task and tool bars Right click the mouse to bring up special menus Access computer functions through the ‘start’ button Shut down the computer using the ‘start’ button Reboot using the ‘shutdown’ function on the start button Minimize, restore, and/or resize a program’s window Create a shortcut to a program to the desktop Printing Basics – I can/am able to: Set up a page in portrait or landscape form and use the header and footer function Use print preview and send a document to the printer Pause or delete a print job Change the printer from printer settings Set a default printer E-mail fundamentals – I can/am able to: Check mail, compose mail, and send a new message Send an attachment Set up mailboxes Forward mail to someone Set up an address book and send e-mail to more than one address simultaneously Word Processing Functions – I can/am able to: Create and save a new document Save a document to a different drive Save a document as a different file type Check spelling and grammar in a document Internet Use – I can/am able to: Use and change search engines and search using keywords Print the screen Save an image to file, download, and save a file Reload a page Yes Pre-Install 20 of 38 No Unsure Staff Meeting Skills and Agenda Template* Before your staff meeting: 1. Create and distribute an agenda with clear goals and outcomes 2. Assign meeting roles Meeting Roles Leader Recorder Timekeeper Facilitator Responsibilities Prepares agenda BEFORE the meeting, moves agenda, elicits participation Visual record for group, next actions list Verbally announces amount of time remaining and when time is up Helps to manage group process, to balance participation, to keep group focused on objectives During the staff meeting: 1. 2. 3. 4. 5. Clarify aim/goal: What we will get done? Review roles: Leader, Recorder, Timekeeper, Facilitator Review agenda Work through agenda items Review meeting record: review flipchart record, make changes/additions, and decide what to keep for meeting record 6. Plan next actions and next agenda: Who will do what offline and aim for next meeting? 7. Evaluate the meeting: What went well? What could be improved? After the staff meeting: 1. Follow-up on action items * From Improve Your Medical Care, Dartmouth Pre-Install 21 of 38 STAFF MEETING AGENDA Date/Time: Location: Meeting Aim/Goal: Attendees: Leader: Recorder: Facilitator: Timekeeper: TOPIC TOPIC LEAD Plan Next Action(s): Plan Aim/Goal and Agenda for next meeting: Evaluate/Process Check (How can we improve this meeting?): Pre-Install 22 of 38 TIME HUDDLES The idea of using quick huddles, as opposed to the standard one-hour meeting, arose from a need to speed up the work of improvement teams. Huddles enable teams to have frequent but short briefings so that they can stay informed, review work, make plans, and move ahead rapidly. Huddles have a number of benefits: They allow fuller participation of front-line staff and bedside caregivers, who often find it impossible to get away for the conventional hour-long improvement team meetings. They keep momentum going, as teams are able to meet more frequently. The enable Plan-Do-Study-Act (PDSA) cycles to proceed rapidly. Directions: 1. Discuss the huddle concept with the team and explain that huddles are a tool for speeding up improvement. Various people can present them at various times during the day in different department areas so that every employee on every shift has an opportunity to hear the daily huddle. 2. Agree on the time and place that huddles will occur. Beginning of day: review of the day, review coming week and next week Mid day review/ End of day review Frequency of daily review dependent on situation To keep huddle focused and short, no one should sit 3. Bring the team together in the place that is most convenient for the team members who have the least time available for meetings. 4. Have a clear set of objectives for every huddle. 5. Limit the duration of the huddle to 15 minutes or less. 6. Review the objectives of the huddle for that day, review the work done since the last huddle, act on the new information, and plan next steps. Gear the information so it is meaningful for the attendees. Recognize individual or team effort, illustrate company mission in motion, share a corporate fact, fact of the day, benefit or policy update, highlight employee information such as birthdays or anniversaries and end with a motivational quote of the day To ensure effective huddles, the following activities can be assigned by staff member Medical Assistants- Consider possible bottlenecks that may arise in the schedule (e.g., two high- needs patients scheduled back-to-back), set up procedures and request outstanding labs and reports, make sure needed forms are in charts, Cancel scheduled appointments for patients who have been hospitalized Nurse- Consider phone contacts or rescheduling appointments if providers have too many patients, look for potential patients who could have nurse visits, identify potential slots for double booking if needed Front Desk- Alert staff to chronic no shows, chronic late or disruptive patients, do chart prep: ensure enough blank progress notes, name of patient on all sheets; have new patient sign request for information if possible Provider- Review list of scheduled patients. Help Nurse and MA’s plan flow and anticipate patient needs, request needed lab, procedure and ED reports, let staff know of any potential for double booking, check for patients that always take a lot of time (patients with lots of co-morbidities, complaints, Pre-Install 23 of 38 HUDDLES elderly). 7. Huddle frequently, as often as daily, when many PDSA cycles are being tested and the team needs to share information frequently. Huddle Worksheet What can we proactively anticipate and plan for in our work day/week? At the beginning of the day, hold a review of the day, review of the coming week and review of next week. Frequency of daily review is dependent on the situation, but a mid-day review is also helpful. This worksheet can be modified to add more detail to the content and purpose of the huddles. Practice: ____________________________ Date: _____________________ Aim: Enable the practice to proactively anticipate and plan actions based on patient need and available resources, and contingency planning. Follow ups from Yesterday: Heads Up for Today: (include special patient needs, sick calls, staff flexibility, contingency plans) Review of Tomorrow and Proactive Planning: Scanning and Backloading Tips Pre-Install 24 of 38 Transitioning patient data from paper charts to the EHR is probably the most time consuming and resource intensive task on the EHR implementation workplan. Careful thought and consideration should be given to this process. Time spent planning the scanning and backloading process will be time well spent. Scanning refers to the process of electronically scanning your paper medical records into the EHR. Backloading refers to the process of manually entering information into sections of your EHR. Scanning is a quick process and many practices will be tempted to scan all documents from the paper chart into the EHR. Practices may feel that scanning everything is the “safe way” to proceed and thus they will avoid the possibility of not having a piece of information they need to offer patient care. Unfortunately, scanning every document into the EHR could end up being more of a hindrance than a help. Too many scanned documents will slow the providers down as they try to find information on the patient. Ask any provider in your practice, flipping through a paper chart for a lab result is a frustrating experience. You will want to be sure not to duplicate this frustration in the EHR. Depending on your EHR vendor, scanned documents may or may not be searchable and reportable so keep this in mind if you are planning to generate reports on specific data elements. Backloading information such as allergies, medication lists, and past medical history into specific sections of the EHR is a more resource intensive process but the end result is an organized, searchable, reportable record of the patient’s medical experience. Backloading of data can also be a good “hands-on” training exercise for the staff. As you begin to plan your scanning and backloading methodology, discuss the following questions/concepts with your implementation team: Which paper charts will be scanned? All charts? Just patients that have been seen in the past five years? Which parts of the charts will be scanned? Which parts will be manually backloaded into the EHR? If sections of the chart will be manually backloaded into the EHR, who will enter the information and when will they enter it? Who will scan the paper charts? Staff? Temps? A scanning service? In what order will the paper charts be scanned? (Newest to oldest? Based on appointment schedule?) How will scanned documents be indexed in the EHR? Will there be separate sections for referrals, office notes, and other documents? How will new documents that are received in the mail every day be handled? What type of scanner is needed? Is there enough physical space for a high volume scanner? Will scanned documents be searchable/reportable? Be sure to ask your EHR vendor. What will we do with the charts once they are scanned? Will we store them offsite? Shred them? Pre-Install 25 of 38 Scanning and Backloading Tips If paper charts are to be scanned, you may need to develop a paper to electronic transition plan so your staff will know where to look for a patient’s chart. For example, should they look on the shelf or in the computer for the patient’s chart? Other practices facing this decision have opted to manually backload an historical patient summary including the past medical history, medications, allergies, etc into the EHR. Only the most critical documents from the patient’s chart were scanned into the EHR. Charts were “prepped”—meaning that the historical patient summary was manually entered and the pertinent chart pages (current progress notes, advance directives, release of information, etc) were scanned into the chart—based on the patient appointment list. In anticipation of the EHR being live, the practice began prepping charts for the first two months of appointments after the EHR live date. Charts were then continuously pulled and prepped based on the appointment list until all charts were scanned. An electronic archive was created on a server separate from the EHR to electronically store the entire patient chart. The entire patient’s chart was scanned into the archive and will be kept for the time required by law. The physical paper chart was then shredded. The purpose of the electronic archive is to keep all patient records post-EHR live, in accordance with law, without having to maintain space for the paper charts or bear costs of offsite storage. Pre-Install 26 of 38 DOQ-IT Workflow Assessment Guide Clinic Name: ________________________________________________________ Hours of Operation Monday Tuesday Wednesday Thursday Hours of Operation Friday Saturday Sunday Practice Schedule: Provider Name Daily Schedule # Patients/day Accepting New Patients Pre-Install 27 of 38 DOQ-IT Workflow Assessment Guide List all office staff members and describe job responsibility: Name Job Responsibility Full/Part Time Pre-Install 28 of 38 DOQ-IT Workflow Assessment Guide Background Questions: Questions General Layout: Obtain copy of floor plan/evacuation route Details # Exam rooms: # Workstations: # Offices: Identify Project Leader Chart Confidentiality: Current policies related to security of PHI/chart storage/access to PHI Need for new P&P’s related to security/access to EMR P&P regarding storage of paper records, on and off site Current PC use by staff: Staff familiarity with Windows technology? Need for Windows training? Renovation Plans: Any plans for future construction, relocation, renovation of office? What is timeframe? Known Staff Changes: Any plans to add new staff? Are any existing staff expected to leave in near future? IT Support: What IT support is available? On-site or contracted? List name and contact information Remote Access: Will providers or other staff need access to system remotely? Any remote access in use currently? Exam Rooms/workstations: Will workstations be placed in exam rooms? Is additional furniture or mounting devices needed? Provide Windows Training CD Provide resource list Pre-Install 29 of 38 Questions Details DOQ-IT Workflow Assessment Guide Wireless Devices: Plans for a wireless network? Type of device? (Tablet PC’s, laptops or hand held devices) Scanning Technology: Does practice currently use scanning software to store pt information? If not, plans to implement? Capable of multiple documents? Workflow Overview: Process Patient registration process Overview New patient: Demographic form? Insurance verified-card copied? HIPPA form? New patient packet sent? Co-pay collected? Forms added to chart for MA? Picture of patient taken? How is arrival communicated? Existing patient: Update demographics? Update insurance-copy card? HIPPA form? Co-pay collected? Forms added to chart for MA? Appointment scheduling: % of appointments made by phone vs previous visit? Who makes appointments, % of same day appt, % of new patients/day or month? Allow walk ins? Hours for walk ins? Pre-Install 30 of 38 Process Triage and Clinical Phone calls: Include Rx renewal process Overview Automated phone system? Who handles? refills/questions? How handled? Process for returning pt calls # calls for MD directly Rx calls: Accept pt and pharmacy calls for P&P’s for handling requests? Standing protocols? DOQ-IT Workflow Assessment Guide Other phone calls: How are messages communicated to staff? Medical Records: When and by whom are charts pulled? Who files information in charts? What is filed in the chart? What’s done about missing charts? Regular appointment Same Day appointment Nurse visit Phone calls Incoming results Describe Pre-visit tasks: Include printing of fee slip, chart preparation, pre-vist appt confirmation Who does Reminder calls Billing: Including onsite billing vs billing services Keeping current PM software? Would consider new PM software? Pre-Install 31 of 38 Process MA/Nursing tasks: Related to patient visits Overview MA/Nurse: Nurse only: Room patient? What’s MD responsibility? VS, weight taken? Brief hx, meds reviewed? What is documented? Routine exams/set-ups? How is patient ready status communicated to MD? What happens with no-shows? Is there provider variation? Exam: Reviewing the chart? DOQ-IT Workflow Assessment Placing Guide orders Requesting MA assistance? Documenting visit? How is provider kept on schedule? Provider tasks: Related to patient visits Dictation/Transcription: How often is dictation done? How (digital vs tapes)? How are transcribed notes sent back? Any transcription done on-site? Laboratory: % of on-site vs outside lab use? Where drawn on site? % tests per lab? How are results reports received? How often? Correspondence: Review of messages Review of labs/results MA’s draw? Process for removing and returning pt to exam room? list outside labs: How are results communicated to patients? What happens if pt can’t be reached? What is the tracking process for labs/results? Is there a lab-specific printer/fax for results? Pre-Install 32 of 38 Process Overview Referrals: How are referrals ordered? Authorized? Scheduled? Tracked? Is there a referral coordinator? Any process for verifying pt completes referral? Patient Check-out: Describe process. When is visit documentation completed? -As visit concludes -Immediately after visit at workstation -Between visits, when MD has time -At the end of the day -Days/weeks later -Usually within _____ hours What happens to the chart? -Goes with pt to checkout -Goes to the MD office -Sits at a work area for MD to complete when time permits -Other: Is there variability among providers? Super-bill/Encounter form: -Who documents on super-bill? -Where does it go at end of visit? -How does it get there? -What are the steps until a bill is dropped? Coders -Do they have the information they need? DOQ-IT Workflow Assessment Guide -How do they get their questions answered? Who checks the patient out? How are follow up appointments made? Patient correspondence: Missed appointment calls/letters, etc. Forms and Letters Collect copies of all standard forms used: Fee slips, patient encounter forms, referral forms, nursing order forms, lab order forms, lab report forms, immunization records, etc. Also Pre-Install 33 of 38 obtain copies of any standard letters that are sent out, missed appointments, reminders, etc. Chart Review Review several charts from each provider and summarize how organized Is there an up-to-date face sheet with problem list, current medication and allergies? Are notes typically hand-written, transcribed, or completed forms? What is the volume of outside correspondence is chart? Do all providers use the same method to record notes? How are phone notes recorded in chart? Are there in-house procedures performed that are documented on forms? Do they use drawings or graphics as part of their chart documentation? Other? Pre-Install 34 of 38 Processes *Review, adapt, and distribute the Core and Supporting evaluation form to ALL Practice Staff. Be sure the list is accurate for your practice and then ask staff to evaluate the CURRENT state of these processes. Rate each process by putting a tall mark under the heading which most closely matches your understanding of the process. Also mark if the process is a source of patient complaints. Tally the results to give the Lead Team an idea as to where to begin to focus improvement from the staff perspective. *Steps for improvement: Explore improvements for each process based on the outcomes of this assessment tool. Each of the processes below should be flowcharted in its’ current state. Once you have flowcharted the current state of your processes and determined your chage idea use the PDSA Cycle Worksheet to run tests of change and to measure. Primary Care Practice Know Your Processes Core and Supporting Processes Processes Works Well Small Problem Real Problem Totally Broken Cannot Rate We’re Working On It Source of Patient Complaint Answering Phones Appointment System Messaging Scheduling Procedures Order Diagnostic Testing Reporting Diagnostic Test Results Prescription Renewal Making Referrals Pre-authorization for Services Billing/Coding Phone Advice Assignment of Patients to Your Practice Orientation of Patients to Your Practice New Patient Work-ups Minor Procedures Education for Patients/Families Prevention Assessment/Activities Chronic Disease Management Palliative Care Pre-Install 35 of 38 Pre-Install 36 of 38 Return on Investment (ROI) Return on Investment (ROI) analysis is one way to build a business case for implementing an EHR. The term means that decision makers evaluate the investment by comparing the magnitude and timing of expected gains to the investment costs. Simple ROI is the most frequently used form of ROI and is the most easily understood. With simple ROI, incremental benefits of the investment are divided by the cost of the investment. In other cases, the term refers to the cumulative cash flow results of an investment over time. Since so many different ROI metrics are commonplace and the term itself does not have a single, universally understood definition, it becomes important to be sure that decision makers define ROI the same way and that everyone understands the limits of the concept when used to support business decisions. When looking at ROI for an EHR implementation, the major categories of savings are cost reduction; revenue enhancement; improved administrative efficiency; and improved clinical efficiency, patient care and service. These categories mirror the promised benefits of the EHR, because ROI analysis is really nothing more than the process of confirming that the system is delivering its expected benefits. EHR Savings to Consider Cost Reduction Reduced transcription costs Reduced internal and external copying expenses Labor savings Malpractice insurance savings Lower paper chart and storage expense Reduced paper office supply costs (paper, chart materials, prescription pads, etc.) Revenue Enhancement Increase in health maintenance services Improved coding accuracy Increase in the number of visits per day Increase in the amount of revenue-generating space (if the medical records area is used for something else) Improved Administrative Efficiency Fewer chart pulls and less filing Universal access to charts Reduction in phone tag Improved intra-office communication Fewer call-backs from pharmacies Easier compliance with chart requests and chart audits Pre-Install 37 of 38 Return on Investment (ROI) Improved Clinical Efficiency, Patient Care and Service Higher quality documentation Built-in protocols and reminders Improved medication management More efficient signing of charts Patient callbacks and telephone triage Patient education and involvement Electronic clinical decision support For the ROI analysis, also consider the cost of implementing the EHR. Listed below are some of the costs of implementing an EHR. Software license fees Hardware costs and maintenance fees Vendor implementation fees Internal network upgrade expenses Software upgrade costs Vendor support costs Training costs Costs to scan/backload paper charts into the EHR Cost of employee overtime to implement system Cost of temps or others to help with implementation Temporary loss of revenue if you are planning on a reduced schedule during the live event Additional IT staff expense Resources: 1. SolutionMatrix.com 2. The Dollars and Sense of Electronic Medical Records: The bottom line case for an EMR. Practice Partner Forum. A publication of Physician Micro Systems, Inc. 1999. 3. The Electronic Physician: Guidelines for Implementing a Paperless Practice. Allscripts Healthcare Solutions. 2005. Pre-Install 38 of 38