Next one
advertisement
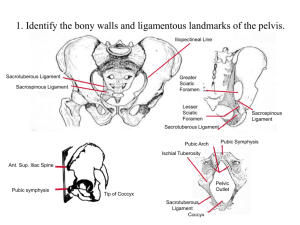
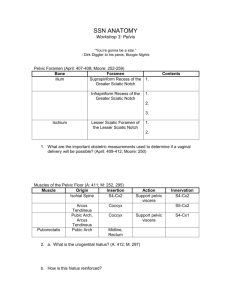
Week 24 LA – Pelvis walls, Prostate and Testicular examination : clinical implications Introduction The testicles and prostate are relatively common sites for malignancy ( at the opposite extremes of the period of male adulthood). Both a very good prognosis if picked up early. The pelvic walls and floor are very relevant to a number of clinical problems. Learning Objectives By the end of this session you should be able to: 1 2 3 4 5 6 Identify most parts of the pelvic girdle bones and sacrum on X-ray, as well as recognize obvious anomalies like fractures Outline and the sex differences between males and female pelvises, indicating these on the bones and describe their structure-function relationships. Understand the way to examine the testicles looking for testicular tumours – including the principle of comparing sides. Describe the function and weak points of the pelvic floor – how this relates to episiotomies during delivery. – Other clinical complications will be dealt with in the next session Outline the procedure of testicular examination Outline the procedure of rectal examination – in particular in relation to the prostate. Props. Pelvic Bones/Models – male and female, Pelvis X-rays, Male pelvic examination model. Volunteers : Two males, stripped down to the knees Session : (only joking above by the way) Students will divide themselves up into 3 groups and rotate, spending about 20 minutes in each case on one of the following stations. 1. Using the Pelvic bones a. briefly review the differences between the male and female pelvises – you should show 7 b. Identify the ligaments attaching the pelvic girdle to the axial skeleton and those involved in stabilizing it ( preventing rotation on the sacroiliac joint fulcrum). Indicate the passage of the sciatic and pudendal nerves from the sciatic foramina. c. draw on the blackboard, the levator ani muscle, indicate the slope of its fibres and of the muscle gutter (what is the reason for this). What is its nerve supply. 2. Using the 1st 5 X-rays, AP, oblique and and lateral views, identify the following parts of the pelvis ( Is the AP view likely a female or a male?) a. point of fusion of ilium, ischium and pubis bones b. pubic symphysis c. pubic crest d. iliac crest e. iliac fossa f. iliac tuberosity g. iliopectineal line h. pelvic brim i. pelvic outlet j. pelvic inlet k. sacroiliac joint l. greater sciatic notch m. lesser sciatic notch n. obturator foramen o. acetabulum p. anterior superior, inferior iliac spines q. posterior superior, inferior iliac spines r. ischial spines s. Ischial tuberosity t. Ischiopubic ramus u. Superior pubic ramus v. anterior sacral foramina w. lateral masses of sacrum or ala x. coccyx In the second set of 5 X-rays, identify the anomaly found in each film. 3. Using the examination model a. Examine the testes and identify which has some anomaly – a normal testes should feel somewhat rubbery – changes in shape, size, consistency and fluid accumulation around it should alert one to refer oneself for examination b. Perform a rectal examination and identify i. Coccyx ii. Prostate ( in all its forms) iii. What else would one expect to feel on a real person?