Document 8569217
advertisement

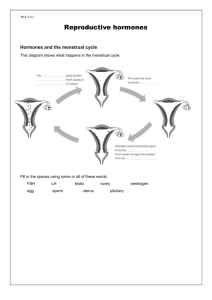
http://www.meddean.luc.edu/lumen/meded/Histo/frames/h_fram19.html Slide 27 – 31 Pancreas Testes 1: Low power view of the testis at the mediastinal region where the duct system leaves the organ. a = seminiferous tubules b = rete testis in mediastinum c = epididymis d = efferent ducts Note the thick collagenous connective tissue capsule (the tunica albuginea) surrounding the testis. Testes 2: Higher power of rete testis, the narrow cavernous channels lying in the dense connective tissue. You will notice a couple of thin-walled, blood-filled blood vessels also coursing in the same region. Sperm produced in the seminiferous tubules leave the testis by way of the rete, which ultimately converges on about twelve efferent ducts. Testes 3: Detail of rete testis, showing cavernous, irregular channels lined with a low epithelium. Testes 4: Low power view of seminiferous tubules. These tubules are very long and tightly coiled, so each one is cut many times in any given section of the testis. Blood vessels and interstitial cells of Leydig lie in the connective tissue stroma between the tubules. Testes 5: Seminiferous tubules of the testis. a = spermatogonia b = spermatocytes (probably primary because secondary spermatocytes go through their cell division so quickly that they are seldom seen in sections). The cells are largest at this stage. e = spermatids f = maturing sperm d = interstitial cells of Leydig (endocrine cells which secrete androgens). A small amount of smooth muscle around the tubule aids in moving differentiated sperm along the tubule and into the rete testis. Testes 6: Detail of wall of seminiferous tubule, showing stages of spermatogenesis. The large, vertically oriented nucleus at the base on the left belongs to a Sertoli cell; notice that sperm heads (somewhat out of focus) are clustered deep down near this nucleus. The horizontally flattened nuclei along the base of the tubule belong to spermatogonia, the continually multiplying, diploid germ cells. A few primary spermatocytes, with the dark, condensed chromosomes undergoing prophase of meiotic division, lie just above the spermatogonia. Above the spermatocytes are the round, relatively small, haploid spermatids, which would occupy the rest of the layers up toward the lumen. Testes 7: Drawing of stages in the differentiation of sperm directly from spermatids. This process is called spermiogenesis. A = a still-rounded spermatid, with an acrosomal body beginning to form in the region of the Golgi apparatus. At the opposite pole of the nucleus lie the centrioles, one of which begins to spin out a long cilium (or flagellum). B = an elongating spermatid, with an acrosomal cap now forming over the top of the nucleus. The flagellum is longer and the centrioles are oriented perpendicular to each other. The centriole related to the flagellum is comparable to the basal body of ordinary cilia. C = further development of the acrosomal cap and beginning pinching off of excess cytoplasm, thanks to the formation of a filamentous manchette, nuclear ring, and annulus. D = further condensing of the nuclear chromosomal material and separating off of the excess cytoplasm. Notice that the intercellular bridge connecting this spermatid to its neighbor is still intact. E = the cytoplasmic mitochondria have now collected along the proximal portion of the flagellum and are thus conserved (for energy purposes) when the residual cytoplasm is cast off. The flagellum has meanwhile developed a complex fibrous sheath which surrounds a central core of microtubules arranged in the nine plus two arrangement typical of cilia. Testes 8: Wall of seminiferous tubule. Along the base can be seen small dark nuclei of spermatogonia and large, pale, ovoid or triangular nuclei of Sertoli cells, each with a prominent nucleolus. Sperm heads are imbedded in folds of Sertoli cell membrane, rather deep within the tubule wall. Sperm tails are pointing toward the tubule lumen. Primary spermatocytes have large nuclei with the condensed chromosomes in prophase, near the base of the wall. The small, round nuclei toward the lumen belong to early spermatids. Pale pink cytoplasmic cast-offs from differentiating spermatids (becoming sperm) lie next to the lumen. Look again at the two Sertoli cells farthest to the left and notice how their cytoplasm meets near the base to form the basal and adluminal compartments on either side of the junction. Testes 9: Efferent ducts with their irregular epithelial border. These are the only portions of the male reproductive tract with motile cilia on the lining epithelium. Cilia help to move the sperm along toward the epididymis. Testes 10: Detail of efferent duct wall, a low pseudostratified columnar epithelium with some surrounding smooth muscle. The epithelium is ciliated. Sperm lie in the lumen. Testes 12: Epididymis with pseudostratified columnar epithelium with stereocilia. (Stereocilia are structurally like microvilli rather than like true cilia. They do not move.) Each cross-cut of tubule shows some surrounding smooth muscle cells. Notice how very regular this epithelium is in height, making an unusually smooth apical line near the lumen. This is characteristic of epididymis. Compare this with the "scalloped" edge of efferent ducts in the previous slides. Testes 13: Another view of epididymal wall, showing more clearly the basal and columnar cells of the pseudostratified epithelium. The stereocilia are long and pale (practically invisible here!). Circular smooth muscle in the outer wall is evident Testes 14: Distended epididymis packed with maturing sperm. They are already mature structurally but are only now acquiring the ability to move on their own. Testes 15: Ductus deferens with its proportionally small lumen and heavy muscular coat. The bulk of the smooth muscle is circular, but there is a thin inner longitudinal and a somewhat thicker outer longitudinal layer. Testes 16: Detail of epithelial lining of the ductus deferens. It is pseudostratified columnar with non-motile stereocilia. Ovary 1: Ovary with surface cuboidal epithelium. (Really a modified mesothelium.) Ovary 2: Cortex of ovary. A thick connective tissue capsule, the tunica albuginea underlies the surface epithelium. Somewhat deeper lie several small, primary (primordial) follicles. (All egg cells have reached the primary oocyte stage by birth and are held in this "suspended animation", in very early prophase, until such time as they may ovulate or undergo atresia.) Ovary 3: Primary follicles with one single layer of flat follicle cells surrounding an oocyte. Although an oocyte is a giant compared with its neighbors, this early stage is small for an oocyte, and the cell will grow considerably in size when it begins to mature, under the influence of FSH. The nucleus looks lightly granular, and the dark nucleolus is prominent. Cytoplasm is very pale. Note the "swirly" interstitial tissue of the ovarian stroma. Ovary 4: Early maturation stage of follicle with beginning proliferation of follicle cells around an enlarging oocyte. The nucleolus shows clearly inside the nucleus. As the oocyte enlarges, its chromosomes prepare further for the first meiotic division, which will occur at ovulation. Ovary 5: Further developed follicle a = with antrum beginning at arrows. The homogenous gray-blue line immediately surrounding the egg cell itself is the zona pellucida. b and c = primary follicles, containing oocytes which are still small. Ovary 6: A group of follicles in various stages of early development in the cortex of a rat ovary. Blood vessels of the ovarian medulla are seen in the center of the field. Development of follicles is regulated by FSH from the anterior pituitary. Ovary 7: Maturing follicle, so called because it contains a definite antrum (or fluid-filled space) and many layers of granulosa cells. The egg is still a primary oocyte and sits to one side of the follicle on a mound of cells called the egg hillock or cumulus oophorus. The cells closest to the oocyte will be expelled with it at ovulation as the corona radiata. Surrounding the granulosa cells of the follicle is the theca interna, a rather cellular and vascular connective tissue layer, which secretes estrogen. Outside of this is the theca externa a more fibrous connective tissue layer, not well defined here. Note that several follicles may start to develop in any one monthly cycle, but in the human only one will mature, unless there are to be multiple ovulations and therefore possible multiple births. All follicles that don't complete their maturation undergo atresia (i.e., degenerate). The egg dies, the granulosa layer breaks up, and the whole follicle collapses and undergoes fibrotic change. Ovary 8: Large ruptured follicle, just after ovulation. Arrow = stigma, the point of rupture where oocyte was expelled. The reduction division (or first meiotic division) takes place at the time of ovulation. a = granulosa cells that will now proliferate under the stimulus of pituitary LH and enlarge to become granulosa lutein cells, filling in the follicular cavity and becoming the major portion of the new corpus luteum. b = corpus albicans -- old scar of an earlier corpus luteum. Slide 1 Pituitary Macro view of the pituitary gland. This and the following pituitary slides are stained with Masson's trichome wherein nuclei and other basophilic structures (may include cytoplasm) are blue, collagen is green or blue, and cytoplasm (nonbasophilic) are red. Notice the lightlystained neurohypophysis and darker-stained adenohypophysis. Slide 2 Pituitary The anterior pituitary is to the upper right and the posterior pituitary is to the lower left. Small cystic spaces that mark the remnants of Rathke's pouch separate the two. Bar = 1mm Slide 3 Pituitary The small dark cells are a lymphocyte infiltrate into the intermediate lobe. There is a rich blood supply to the anterior lobe that supplies the hypothalamic releasing and inhibiting factors that regulate pituitary hormone secretion. Bar = 250 Microns Slide 4 Anterior Pituitary The anterior pituitary is composed of the stained-rich chromophils and the clear chromophobes. Of the chromophils, acidophils are red and basophils are blue. Bar = 1mm Slide 5 Anterior Pituitary Chromophobes (black arrow), Eosinophiles (red arrow), Basophiles (blue arrow). Also visible in this area are collagen (blue) and the red (yes, red) cells in the vasculature. Bar = 100 MM Slide 6 Posterior Pituitary The majority of the space is occupied by axons descended from the hypothalamus. It is thus not a true endocrine gland, but a specialization of the hypothalamus that maintains the blood brain barrier while still secreting hormones into the bloodstream by the axon endings. Bar = 250 Microns Slide 7 Posterior Pituitary Herring bodies (arrow) are the dilated hypothalamic nerve terminals from the hypothalamus from which the posterior pituitary actually releases ADH & Oxytocin. ADH and oxytocin are released from different Herring bodies reflecting their seperate cells of origin. Bar = 50 mm Slide 1 Thyroid The simple cuboidal epithelium lining the follicles produces the thyroglobulin which is stored in the colloid follicles. Later it is taken back up by these same cells, cleaved, and released as T3 & T4. Notice that the thyroid is the only gland to store its hormones extracellularly. Slide 2 Thyroid The C-cells secrete calcitonin which helps lower calcium levels. Recall that this hormone antagonizes the effect of PTH from the parathyroids. These C-cells are actually named for being "clear" (as in lighter staining). Notice that they are in the interstitium and do not normally touch the follicles. Bar = 50 Microns Slide 3 Thyroid Thyroglobulin (in the follicles) is a glycoprotein. The PAS stain reacts with the carbohydrate components of thyroglobulin and produces a deep red appearance. Bar = 250 Microns Slide 1 Parathyroid Cells of the parathyroid are often mistaken for lymphocytes. An actual lymphocytic infiltrate (arrow) stains darker. Notice the parathyroid cells are sometimes arranged in strings or lines. Bar = 250 Microns Slide 2 Parathyroid The string-like arrangement of the parathyroid cells on the right. The large, clear cells to the left are oxyphil cells whose function is unknown. They are found only in humans and increase with age. The intense eosinophelia in their cytoplasm reflects an abnormally high number of mitochondria in these cells. Bar = 50 Microns Slide 1 Adrenal Identify the three layer of the adrenal cortex from left to right: Zona Glomerulus, Zona Fasiculata, Zona Reticularis (mnemonic - GFR). Also notice the dark medulla and the surrounding capsule. Bar = 250 MM Slide 2 Adrenal Find the layers again and notice the rich blood supply. Bar = 250 Microns Slide 2KU Pancreas The pancreas, shown here stained with H&E, serves both endocrine and exocrine functions. The round islets of Langerhans are the endocrine portion and serve to identify pancreatic tissue. Bar = 250 Microns Slide 3KU Pancreas Islets are distinguished from the surrounding exocrine tissue by a continuous connective tissue capsule and an extensive microvascular that first bathes the center of the islet that is rich in B or beta (insulin) cells, and then the periphery where most of the A or alpha (glucagon) cells are located. Within the islet, the glucagon-secreting alpha cells stain red while the insulin-secreting beta cells stain blue. (Gomori Stain) Bar = 30 MM Slide 1 Pineal The pineal gland (in the brain) secretes melatonin, but its function in man is largely unknown. It is best identified by the distinctive dark globules known as brain sand that can be observed in the glands of older individuals. There are two principal cell types in the pineal; the pinealocyte that is a highly modified neuronal cell and that secretes melatonin, and glial cells. Bar = 250 Microns Slide 2 Pineal This is the brain sand of the same person after a grueling semester of Physiology. Obviously this is a digitally manipulated image, but do remember that this mineralization has no clinical manifestation. Bar = 250 Microns