Workbook - Skills for Care
advertisement

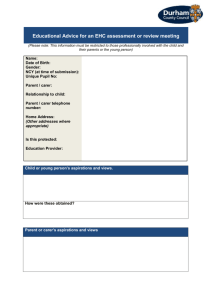
Enable rights and choices for individuals with dementia whilst minimising risks Dem 304 Name: Date: Assessor’s Name: Assessor’s Signature: Signature: Legislation to support and assist with rights and risks for people living with dementia Mental Capacity Act (2005) The mental capacity act was introduced in order to empower and protect people who may lack capacity to make some decisions for themselves. It makes it clear who can take decisions in which situations, and how they should go about this. It also allows people to plan ahead for a time when they may lack capacity. It covers major decisions about someone's property and affairs, healthcare treatment and where the person lives, as well as everyday decisions about personal care (such as what the person eats), where the person lacks capacity to make those decisions themselves. Key Principles There are five key principles in the Act: Every adult has the right to make his or her own decisions and must be assumed to have capacity to make them unless it is proved otherwise. A person must be given all practicable help before anyone treats them as not being able to make their own decisions. Just because an individual makes what might be seen as an unwise decision, they should not be treated as lacking capacity to make that decision. Anything done or any decision made on behalf of a person who lacks capacity must be done in their best interests. Anything done for or on behalf of a person who lacks capacity should be the least restrictive of their basic rights and freedoms. Understanding Safeguarding and Whistleblowing It is important that you are aware of the various policies and procedures so that you are working in a way which supports Your organisation’s s legal duty as a care provider, and your personal legal responsibility. As part of your induction you will need to understand the policies and procedures of the Trust in the following areas within the first 6 months. All policies and procedures are important, but these are the main areas that you will need to go through with your mentor/supervisor: You will need to be familiar with your Safeguarding Vulnerable Adults policy. The No Secrets guide for Alerters and Reporters also gives you vital information on abuse and what to do if you suspect abuse. Abuse can take many forms. You need to know about the main types of abuse. These are: Physical/sexual abuse Emotional/psychological abuse, including that related to age, race, gender, sexuality, culture or religion Financial abuse Institutional abuse Self-neglect Neglect by others. Abuse could happen in many settings. It could happen in care homes or nursing, homes, sheltered housing, day centres, people’s own homes and in the community generally. Nobody should have to tolerate abuse. However, some people may be more vulnerable to abuse than others. The reasons for this will vary from person to person. Some people may be more vulnerable to abuse due to issues within themselves such as physical or mental illness or learning difficulties. Some people may be more vulnerable to abuse because of the circumstances they live in; they may live alone or in poor housing, for example. Some people may be more vulnerable to abuse because of factors in the care environment they live in, such as low staffing levels Your responsibility Every employee who has contact with Vulnerable Adults has a responsibility to report concerns about abuse. Abuse can happen in any setting, and comes to light in different ways. Sometimes a service user may voice their concerns, but more often suspicions are raised by behaviour that can be observed. It may be reported by another person, such as another service user or carer. Whatever the source of the information it must be treated seriously, recorded and shared with an appropriate manager. If staff are unsure they should discuss concerns with their manager. Person-centred practice is a way of working with people who receive care services that discovers and acts on what is important to a person. It involves really listening to the person and other people who know them and planning what they need now and for the future. A person-centered care plan reflects what is important to the person. It supports staff by giving them the information they need to provide the care the person wants in the way that they want. It is important that we promote empowerment for people who use care services. In the past, people who used care services had often had little power over the decisions made about their care. People using care services can still feel as though all the power is with the staff who support them. People are empowered to make decisions if they are given time, support and information they can understand. The people we support can face risks in their daily life. It is important that people continue to do the activities they wish to. We can manage risks by supporting people to exercise choices and rights. Risks should be managed through risk assessments that recognise the balance between managing risk and enabling independence, choice and control. Risk assessments can help to prevent abuse occurring. Care Workers must also be familiar with the 5 principles of the Mental Capacity Act 2005 when supporting people to manage risks: Presume residents have capacity Support residents to make their own decisions Residents are allowed to make unwise decisions Make decisions for residents who lack capacity in their best interests Use the least restrictive option when making a decision for a resident who lacks capacity. Whistleblowing Members of staff should be able to raise questions about any area of concern regarding service or service delivery informally, during supervision or in staff meetings. In this way, practices can be modified and improved on an on-going basis and issues resolved long before they reach the "whistle blowing" stage. However, this policy and process must be followed if the concerns are serious and would appear to involve the physical, sexual, psychological or financial abuse of a service user or an employee or involves issues of neglect and acts of omission which impact on the service user or the employee in a negative manner. The service user comes first and issues in relation to their welfare will be treated seriously and sensitively. Managers will be expected to respond appropriately to protect the needs of the service user. Raymond’s Money – video case study The film portrays Raymond, a man in his 80s and recently diagnosed with dementia, and Wendy his paid care worker. The setting is Raymond's flat. Wendy visits daily to provide Raymond with practical support to manage at home. The context of the drama is whether Raymond has capacity to make a decision about spending 50 pounds on lottery tickets. 1. Does Raymond have capacity to ask Wendy to purchase the tickets? 2. Should Wendy be the one to purchase them? 3. What information might need to be shared or recorded with regard to this? 4. What monitoring might there need to be around this situation? 5. Think about the legislation covered earlier. How do you think this applies to Raymond’s situation? Risk Taking and Dementia Exercise Think about someone you work with who might sometimes make unwise decisions, or do things you consider risky • How could the identifying risks and impacts table and the Heat Map be used for people that you work with? • What role could you have in this? • Who else should be involved in identifying risks, and best interests decisions Confidentiality Confidentiality is the right of people who receive care to have personal, identifiable information kept private. Confidentiality is vital when working in care. The General Social Care Council Code of Practice for social care workers is clear that respecting confidentiality is a key part of the care worker's role. The Data Protection Act 1998 also requires organisations and their staff to keep information secure and confidential. You will have access to records about the people you support and personal information about them. You will also keep and store records about people. You will also at times need to discuss individual people with managers, colleagues and other professionals. Sometimes you may need to pass on information that might normally be considered to be confidential. This should not be done lightly but may be required by organisational policies or the law. Policies you need to be aware of in this regard include: Confidentiality policy The Safeguarding Adults policy The Whistle-blowing policy. You also need to be aware of your duty of care to the people you support. You may need to break confidentiality if there are issues of concern. You should explain to the person you are supporting and where ever possible, explain why and who you will be talking to. How would you deal with these concerns and complaints? 1. You arrive at a service users home for the first time and the service user says that the previous carer never used to turn up on time and was lazy. 2. A person that you visit regularly says that she is concerned that she is not getting everything that was agreed with her in her original care plan. 3. The wife of the person you visit says that she is unhappy with the amount of time it is taking ( that she is paying for) to help her husband to get washed and dressed in the morning. She believes it can be done quicker and continually asks you to not spend so long with her husband getting him to help with his care. 4. A service user complains that two cardigans have been ruined by care staff who have washed her clothes. Knowing how to recognise and handle complaints. It is important that people who are receiving a service are able to make complaints about that service without being labelled as ‘difficult’ or suffering any repercussions. Organisations providing health and social care should be transparent in relation to acknowledging where there are concerns or complaints about a service, and problems are resolved and not hidden. Staff should welcome justified complaints as they provide an opportunity to improve the quality of the service. Many of the people who receive services from care providers may well approach you with their concerns. It is important that you know how to respond. You will need to listen carefully and help them to communicate their concerns as accurately as possible. Assistive Technology to promote independent living Prompts and reminders These are devices that can act as memory prompts and reminders by providing visual, verbal or audible cues. Clocks and calendar clocks provide information about the day, date and time. Memo minders play a pre-recorded message when a person walks past to remind them to do something or not to go out during the night. Medication reminders and dispensers can help a person to remember when to take their tablets. Signs and notice boards can be used as reminders and to post messages. Talking Tins have been designed to help people who are visually or cognitively impaired to identify the contents of their tinned food. This could also be attached to other metal things in the house such as the fridge to record short messages/ reminders. This product comes in the form of a magnetic cap that sits on top of any sized steel tin. The cap allows you to record a voice message, which can then be played back at any time with the touch of a button. This striking clear visual kitchen timer takes some of the guesswork out of cooking and reminds you when the food is done which helps prevent burnt food or disasters in the kitchen. Simply twist the top half of the unit to gradually reveal an easy-to-read analogue dial, stopping when you reach the required number of minutes and seconds (up to 1hr). Release the bezel and the unit begins counting down, leaving you free to concentrate on other tasks. The graphic dial allows you to monitor progress at a glance, even from a distance, and when the time is up, a classic alarm bell sounds to attract your attention. The unit has a silky, soft-touch finish. No batteries required. Date and time These devices can help support people who have difficulties keeping track of the day or time. They range from large wall mounted clock calendars which show the day, date and time, to electronic calendars which digitally display the day, date and time of day e.g. ‘morning’, afternoon’, ‘evening’, or ‘night’. Item locator devices These are devices that can help locate commonly mislaid items in the home such as keys, wallets, glasses case etc. Medication reminders and dispensers These devices can help support people who have difficulties remembering to take their tablets. They range from simple flip lid pill boxes labelled with the day of the week and time of day, to automatic pill reminders and dispensers which give an audible and visual alert when it is time to take a tablet (the alert stops as soon as the tablet is tipped out). Telecare medication dispensers will also alert the carer or monitoring centre if the tablets are not taken out of the dispenser so that an appropriate response can be made. Voice recorders and memo minders These devices can help support people who have difficulties remembering to carry out tasks. Memo minders can record a short verbal message (usually up to 20 seconds) and be placed near a doorway or other suitable location. A passive infra-red motion detector will sense when the person walks past the device and the message will be played. Some also have a timer device that can be set e.g. to remind someone not to leave the house during the night. These devices may not be suitable for people who are hard of hearing. Signs, notices and other environmental aids These are simple visual devices that can act as memory prompts and range form signs or labels that can be placed on doors to notice boards and wipe boards for pinning or writing reminders and messages. In this category we also include other items that may be used in a setting to make it more "enabling" for people with dementia. Activity monitors These devices can be used to detect activity and inactivity. Passive infra-red (PIR) sensors can look for movement at pre-set times e.g. every 4 hours. If the person has not moved for this time an alarm will be sent to the carer or monitoring centre. Activity monitoring systems use wireless sensors around the home which send information on the daily activities of a person to a monitoring service for short term assessment purposes or to provide information to a carer. Alarm and pager units These devices are used to alert a carer or a community alarm monitoring centre to provide a response when a sensor is triggered. Some assistive technology devices will trigger a portable pager or bleeper that is carried by the carer within the same home. For people who are often on their own at home, telecare devices will trigger a table-top alarm unit which will automatically dial a carer outside the home or a 24 hour monitoring centre. Fall detectors These devices detect when a person who as been assessed as being at risk of falling is getting out of a bed or a chair or when they have had a fall. Pressure sensors or mats on the bed, chair or floor will send a signal to a portable receiver/pager to alert a carer that the person is getting up and about. Fall detectors are worn by the person and will trigger an alert to a carer if an impact is detected and/or the person remains in a lying position. Telecare fall detectors will also alert the monitoring centre so that an appropriate response can be made. Flood detectors and water temperature monitors These devices detect flooding and dangerously hot water. Flood detectors range from a simple plug that releases excess water if the taps have been left running in the bath or sink to prevent water overflowing, to wireless sensors that provide an audible alarm when they detect water rising above a certain level or when water is running onto the floor. Telecare flood detectors will also alert the carer or monitoring centre so that an appropriate response can be made. Water temperature monitors provide a visual or audible warning when water is dangerously hot. Gas, carbon monoxide, smoke and extreme temperature detectors These devices detect gas, carbon monoxide, smoke and extremes of temperature. Gas detectors provide a visual and audible alarm if a gas cooker or a gas fire is left unlit or there is a gas leak. In addition, some devices link to a cut off valve which will automatically cut off the gas supply. Carbon monoxide (CO) detectors provide a visual and audible alarm when dangerous CO emissions have been detected due to a blocked flu or fault in a fuel burning appliance. Smoke detectors provide an audible alarm when smoke is detected in the home. Extreme temperature monitor for excessively high and low temperatures and a rapid rate of rise in temperature. Telecare devices will also alert the carer or monitoring centre that the sensor has been triggered so that the emergency services can be called. Lighting These devices provide easy to use or automatic lighting in the home. Touch lamps are easy to use lamps which can be turned on by touching the base area. Automatic night lights range from lights that come on at dusk and switch themselves off at dawn, to lights that come on automatically when a person gets out of their bed or chair or opens a door during the night. Other safety and security devices These devices are used to improve general safety and security in the home. Devices include key-safes for use by authorised carers and other persons who may need to access the home if the person is unable to open the front door. "Wandering"/Safer walking technologies - to locate a person who may be lost There are a growing range of devices that fall under this heading. They vary greatly in design and how they may be used. For example a card may be carried by the person containing emergency contact details should the holder become lost or experience difficulties. New GPS (Global Positioning Satellite) technologies now enable devices (including mobile phones) to locate the precise position of the carrier. As with the application of all technologies, ethical issues, including best interests and consent, should be thoroughly considered. "Wandering"/Safer walking technologies - to alert when someone gets up or leaves These devices may trigger a sensor (door, bed, chair, floor) and notify another person (perhaps a carer in the same house or living elsewhere, or a monitoring centre) should a person open a door where a sensor is located or leave a designated area. As with the application of all technologies, ethical issues, including best interests and consent, should be thoroughly considered. Computer aids These include easy to see and use computer keyboards with large keys, magnifying screens and accessible computers and software. TV, Radio & Music These include easy to see and use TV remote controls, radios and music players, with simple large buttons to switch them on and off. Books, Photographs & Reminiscence materials These include specially designed books to be shared with people with dementia, talking photo albums which play a short message next to each photograph and a sample of other reminiscence materials that are available. Games These include talking games that can be played on the computer and electronic games and consoles. Dem 304 You will need to answer these questions following the training session in order for you to successfully complete the QCF unit Dem 304 enabling rights and choices for individuals whilst minimising risk. If you are unsure about how to answer any of the questions you should discuss this with the person who will be assessing you. 1 Explain the impact of key legislation that relates to fulfilment of rights and choices and the minimising of risk of harm for an individual with dementia 2. Think about two different service users that you work with who have dementia. Describe how the care plan for each person helps to maintain and promote the person’s rights and choices. How well do you think each care plan manages to do this. Is there anything that could be improved? 3. Explain how and when personal information may be shared with carers and others, taking into account the requirements of the Mental capacity act, safeguarding procedures, lasting power of attorney and your own service’s policies and procedures. 4. Briefly describe how the best interests of a person that you provide a service for have been considered when planning and delivering care and support. What role do you have to make sure that the person’s best interests in this situation are met and understood. 5. Describe a situation where you have helped a person with dementia to exercise their rights and choices even when a decision has not been deemed to be in their best interests. 6. Explain why it is important not to assume that an individual with dementia cannot make their own decisions 7. Describe how the ability of an individual with dementia to make decisions may fluctuate 8. Describe how a conflict of interest can be addressed between the carer and an individual with dementia whilst balancing rights, choices and risk 9. Describe how to ensure an individual with dementia, family and others feel able to complain without fear of retribution 10. Describe how to maintain privacy and dignity when providing personal support for intimate care to an individual with dementia Real work situations You will also need to complete all three of the following real work situations, to demonstrate that you are able to put your knowledge into practice for for you to successfully complete the QCF unit Dem 304 enabling rights and choices for individuals whilst minimising risk For each of the following statements you will need to describe how you have actually put these into practice in your work. You will also need to have each explanation signed by your manager, a senior colleague, or somebody actually involved in the situation you have described who can confirm that your account of the action you took is a true account. 1. Explain how you have involved family members and others in planning support that promotes the rights and choices of an individual with dementia and minimises risk of harm I am signing to say that I confirm that this is a true account of the actions taken by this care worker Signature of witness Relationship of witness to you 2. Explain how key physical aspects of the environment have helped you to show respect and dignity for an individual with dementia I am signing to say that I confirm that this is a true account of the actions taken by this care worker Signature of witness Relationship of witness to you 3. Demonstrate that key social aspects of the environment are enabling care workers to show respect and dignity for an individual with dementia I am signing to say that I confirm that this is a true account of the actions taken by this care worker Signature of witness Relationship of witness to you