approved
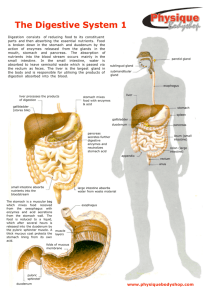
advertisement

Ministry of Health of Ukraine BUKOVINIAN STATE MEDICAL UNIVERSITY “APPROVED” on methodical meeting of the Department of Anatomy, Topographical anatomy and Operative Surgery “………”…………………….2008 р. (Protocol №……….) The chief of department professor ……………………….……Yu.T.Achtemiichuk “………”…………………….2008 р. METHODICAL GUIDELINES for the 2nd-year foreign students of English-spoken groups of the Medical Faculty (speciality “General medicine”) for independent work during the preparation to practical studies THE THEME OF STUDIES “Topographical anatomy of the organs of peritoneal cavity” MODULE I Topographical Anatomy and Operative Surgery of the Head, Neck, Thorax and Abdomen Semantic module 3 “Topographical Anatomy and Operative Surgery of the Abdomen” Chernivtsi – 2008 1. Actuality of theme: The topographical anatomy and operative surgery of the abdomen are very importance, because without the knowledge about peculiarities and variants of structure, form, location and mutual location of abdominal anatomical structures, their age-specific it is impossible to diagnose in a proper time and correctly and to prescribe a necessary treatment to the patient. Surgeons usually pay much attention to the topographo-anatomic basis of surgical operations on the abdomen. 2. Duration of studies: 2 working hours. 3. Objectives (concrete purposes): To know the definition of regions of the abdomen. To know classification of surgical operations on the abdomen. To know the topographical anatomy and operative surgery of the organs of the abdomenal cavity. 4. Basic knowledges, abilities, skills, that necessary for the study themes (interdisciplinary integration): The names of previous disciplines 1. Normal anatomy 2. Physiology 3. Biophysics The got skills To describe the structure and function of the different organs of the human body, to determine projectors and landmarks of the anatomical structures. To understand the basic physical principles of using medical equipment and instruments. 5. Advices to the student. 5.1. Table of contents of the theme: Esophagus (Abdominal Portion) The esophagus is a muscular, collapsible tube about 25 cm long that joins the pharynx to the stomach. The esophagus enters the abdomen through an opening in the right crus of the diaphragm. After a course of about 2 cm, it enters the stomach on its right side. The esophagus is related anteriorly to the posterior surface of the left lobe of the liver and posteriorly to the left crus of the diaphragm. The left and right vagi lie on its anterior and posterior surfaces, respectively. Blood Supply Arteries Branches from the left gastric artery. Veins These drain into the left gastric vein, a tributary of the portal vein. Lymph Drainage The lymph vessels follow the arteries into the left gastric nodes. Nerve Supply Anterior and posterior gastric nerves (vagi) and sympathetic branches of the thoracic part of the sympathetic trunk. Function The esophagus conducts food from the pharynx into the stomach. Wavelike contractions of the muscular coat, called peristalsis, propel the food onward. Gastroesophageal Sphincter No anatomic sphincter exists at the lower end of the esophagus. However, the circular layer of smooth muscle in this region serves as a physiologic sphincter. As the food descends through the esophagus, relaxation of the muscle at the lower end occurs ahead of the peristaltic wave so that the food enters the stomach. The tonic contraction of this sphincter prevents the stomach contents from regurgitating into the esophagus. Stomach Location and Description The stomach is the dilated portion of the alimentary canal. The stomach is situated in the upper part of the abdomen, extending from beneath the left costal margin region into the epigastric and umbilical regions. Much of the stomach lies under cover of the lower ribs. It is roughly J-shaped and has two openings, the cardiac and pyloric orifices; two curvatures, the greater and lesser curvatures; and two surfaces, an anterior and a posterior surface. The stomach is divided into the following parts: The fundus is dome-shaped and projects upward and to the left of the cardiac orifice. It is usually full of gas. The body extends from the level of the cardiac orifice to the level of the incisura angularis, a constant notch in the lower part of the lesser curvature. The pyloric antrum extends from the incisura angularis to the pylorus. The pylorus is the tubular part of the stomach. It has a thick muscular wall called the pyloric sphincter. The cavity of the pylorus is the pyloric canal. The lesser curvature forms the right border of the stomach and extends from the cardiac orifice to the pylorus. It is suspended from the liver by the lesser omentum. The greater curvature is much longer than the lesser curvature and extends from the left of the cardiac orifice, over the dome of the fundus, and along the left border of the stomach to the pylorus. The gastrosplenic omentum (ligament) extends from the upper part of the greater curvature to the spleen, and the greater omentum extends from the lower part of the greater curvature to the transverse colon. The cardiac orifice is where the esophagus enters the stomach. Although no anatomic sphincter can be demonstrated here, a physiologic mechanism exists that prevents regurgitation of stomach contents into the esophagus. The pyloric orifice is formed by the pyloric canal, which is about (2.5 cm) long. The circular muscle coat of the stomach is much thicker here and forms the anatomic and physiologic pyloric sphincter. The pylorus lies on the transpyloric plane, and its position can be recognized by a slight constriction on the surface of the stomach. The pyloric sphincter controls the rate of discharge of the stomach contents into the duodenum. The mucous membrane of the stomach is thick and vascular and is thrown into numerous folds, or rugae, that are mainly longitudinal in direction. The folds flatten out when the stomach is distended. The muscular wall of the stomach contains (1) longitudinal fibers, (2) circular fibers, and (3) oblique fibers. The longitudinal fibers are the most superficial and are most concentrated along the curvatures. The inner circular fibers encircle the body of the stomach and are greatly thickened at the pylorus to form the pyloric sphincter. Few circular fibers are found in the region of the fundus. The oblique fibers form the innermost muscle coat. They loop over the fundus and pass down along the anterior and posterior walls, running parallel with the lesser curvature. The peritoneum (visceral peritoneum) completely surrounds the stomach. It leaves the lesser curvature as the lesser omentum and the greater curvature as the gastrosplenic omentum and the greater omentum. Relations • Anteriorly: The anterior abdominal wall, the left costal margin, the left pleura and lung, the diaphragm, and the left lobe of the liver. • Posteriorly: The lesser sac, the diaphragm, the spleen, the left suprarenal gland, the upper part of the left kidney, the splenic artery, the pancreas, the transverse mesocolon, and the transverse colon. Blood Supply Arteries These are derived from the branches of the celiac artery. The left gastric artery arises from the celiac artery. It passes upward and to the left to reach the esophagus and then descends along the lesser curvature of the stomach. It supplies the lower third of the esophagus and the upper right part of the stomach. The right gastric artery arises from the hepatic artery at the upper border of the pylorus and runs to the left along the lesser curvature. It supplies the lower right part of the stomach. The short gastric arteries arise from the splenic artery at the hilum of the spleen and pass forward in the gastrosplenic omentum (ligament) to supply the fundus. The left gastroepiploic artery arises from the splenic artery at the hilum of the spleen and passes forward in the gastrosplenic omentum (ligament) to supply the stomach along the upper part of the greater curvature. The right gastroepiploic artery arises from the gastroduodenal branch of the hepatic artery. It passes to the left and supplies the stomach along the lower part of the greater curvature. Veins These drain into the portal circulation. The left and right gastric veins drain directly into the portal vein. The short gastric veins and the left gastroepiploic veins join the splenic vein. The right gastroepiploic vein joins the superior mesenteric vein. Lymph Drainage The lymph vessels follow the arteries into the left and right gastric nodes, the left and right gastroepiploic nodes, and the short gastric nodes. All lymph from the stomach eventually passes to the celiac nodes located around the root of the celiac artery on the posterior abdominal wall. Nerve Supply This includes sympathetic fibers derived from the celiac plexus and parasympathetic fibers from the right and left vagus nerves. The anterior vagal trunk, which is formed in the thorax mainly from the left vagus nerve, enters the abdomen on the anterior surface of the esophagus. The trunk, which may be single or multiple, then divides into branches that supply the anterior surface of the stomach. A large hepatic branch passes up to the liver, and from this a pyloric branch passes down to the pylorus. The posterior vagal trunk, which is formed in the thorax mainly from the right vagus nerve, enters the abdomen on the posterior surface of the esophagus. The trunk then divides into branches that supply mainly the posterior surface of the stomach. A large branch passes to the celiac and superior mesenteric plexuses and is distributed to the intestine as far as the splenic flexure and to the pancreas. The sympathetic innervation of the stomach carries a proportion of pain-transmitting nerve fibers, whereas the parasympathetic vagal fibers are secretomotor to the gastric glands and motor to the muscular wall of the stomach. The pyloric sphincter receives motor fibers from the sympathetic system and inhibitory fibers from the vagi. Small Intestine The small intestine is the longest part of the alimentary canal and extends from the pylorus of the stomach to the ileocecal junction. The greater part of digestion and food absorption takes place in the small intestine. It is divided into three parts: the duodenum, the jejunum, and the ileum. Duodenum Location and Description The duodenum is a C-shaped tube about 25 cm long that joins the stomach to the jejunum. It is important because it receives the openings of the bile and pancreatic ducts. The duodenum curves around the head of the pancreas. The first 3 cm of the duodenum resembles the stomach in that it is covered on its anterior and posterior surfaces with peritoneum and has the lesser omentum attached to its upper border and the greater omentum attached to its lower border; the lesser sac lies behind this short segment. The remainder of the duodenum is retroperitoneal, being only partially covered by peritoneum. Parts of the Duodenum The duodenum is situated in the epigastric and umbilical regions and for purposes of description is divided into four parts. First Part of the Duodenum The first part of the duodenum is 5 cm long and begins at the pylorus and runs upward and backward on the right side of the first lumbar vertebra. It thus lies on the transpyloric plane. Relations • Anteriorly: The quadrate lobe of the liver and the gallbladder. • Posteriorly: The lesser sac (first inch only), the gastroduodenal artery, the bile duct and portal vein, and the inferior vena cava. • Superiorly: The entrance into the lesser sac (the epiploic foramen). • Inferiorly: The head of the pancreas. Second Part of the Duodenum The second part of the duodenum is 8 cm long and runs vertically downward in front of the hilum of the right kidney on the right side of the second and third lumbar vertebrae. About halfway down its medial border, the bile duct and the main pancreatic duct pierce the duodenal wall. They unite to form the ampulla that opens on the summit of the major duodenal papilla. The accessory pancreatic duct, if present, opens into the duodenum a little higher up on the minor duodenal papilla. Relations • Anteriorly: The fundus of the gallbladder and the right lobe of the liver, the transverse colon, and the coils of the small intestine. • Posteriorly: The hilum of the right kidney and the right ureter. • Laterally: The ascending colon, the right colic flexure, and the right lobe of the liver. • Medially: The head of the pancreas, the bile duct, and the main pancreatic duct. Third Part of the Duodenum The third part of the duodenum is 8 cm long and runs horizontally to the left on the subcostal plane, passing in front of the vertebral column and following the lower margin of the head of the pancreas. Relations • Anteriorly: The root of the mesentery of the small intestine, the superior mesenteric vessels contained within it, and coils of jejunum. • Posteriorly: The right ureter, the right psoas muscle, the inferior vena cava, and the aorta. • Superiorly: The head of the pancreas. • Inferiorly: Coils of jejunum. Fourth Part of the Duodenum The fourth part of the duodenum is 5 cm long and runs upward and to the left to the duodenojejunal flexure. The flexure is held in position by a peritoneal fold, the ligament of Treitz, which is attached to the right crus of the diaphragm. Note the position of the duodenal recesses. Relations • Anteriorly: The beginning of the root of the mesentery and coils of jejunum. • Posteriorly: The left margin of the aorta and the medial border of the left psoas muscle. Mucous Membrane and Duodenal Papillae The mucous membrane of the duodenum is thick. In the first part of the duodenum it is smooth. In the remainder of the duodenum it is thrown into numerous circular folds called the plicae circulares. At the site where the bile duct and the main pancreatic duct pierce the medial wall of the second part is a small, rounded elevation called the major duodenal papilla. The accessory pancreatic duct, if present, opens into the duodenum on a smaller papilla about 2 cm above the major duodenal papilla. Blood Supply Arteries The upper half is supplied by the superior pancreaticoduodenal artery, a branch of the gastroduodenal artery. The lower half is supplied by the inferior pancreaticoduodenal artery, a branch of the superior mesenteric artery. Veins The superior pancreaticoduodenal vein drains into the portal vein; the inferior vein joins the superior mesenteric vein. Lymph Drainage The lymph vessels follow the arteries and drain (a) upward via pancreaticoduodenal nodes to the gastroduodenal nodes and then to the celiac nodes and (b) downward via pancreaticoduodenal nodes to the superior mesenteric nodes around the origin of the superior mesenteric artery. Nerve Supply The nerves are derived from sympathetic and parasympathetic (vagus) nerves from the celiac and superior mesenteric plexuses. Jejunum and lleum Location and Description The jejunum and ileum measure about 6 m long, the upper two-fifths of this length being the jejunum. Each has distinctive features, but there is a gradual change from one to the other. The jejunum begins at the duodenojejunal flexure, and the ileum ends at the ileocecal junction. The coils of jejunum and ileum are freely mobile and are attached to the posterior abdominal wall by a fan-shaped fold of peritoneum known as the mesentery of the small intestine. The long free edge of the fold encloses the mobile intestine. The short root of the fold is continuous with the parietal peritoneum on the posterior abdominal wall along a line that extends downward and to the right from the left side of the second lumbar vertebra to the region of the right sacroiliac joint. The root of the mesentery permits the entrance and exit of the branches of the superior mesenteric artery and vein, lymph vessels, and nerves into the space between the two layers of peritoneum forming the mesentery. In the living the jejunum can be distinguished from the ileum by the following features: 1. The jejunum lies coiled in the upper part of the peritoneal cavity below the left side of the transverse mesocolon; the ileum is in the lower part of the cavity and in the pelvis. 2. The jejunum is wider bored, thicker walled, and redder than the ileum. The jejunal wall feels thicker because the permanent infoldings of the mucous membrane, the plicae circulares, are larger, more numerous, and closely set in the jejunum, whereas in the upper part of the ileum they are smaller and more widely separated and in the lower part they are absent. 3. The jejunal mesentery is attached to the posterior abdominal wall above and to the left of the aorta, whereas the ileal mesentery is attached below and to the right of the aorta. 4. The jejunal mesenteric vessels form only one or two arcades, with long and infrequent branches passing to the intestinal wall. The ileum receives numerous short terminal vessels that arise from a series of three or four or even more arcades. 5. At the jejunal end of the mesentery, the fat is deposited near the root and is scanty near the intestinal wall. At the ileal end of the mesentery the fat is deposited throughout so that it extends from the root to the intestinal wall. 6. Aggregations of lymphoid tissue (Peyer's patches) are present in the mucous membrane of the lower ileum along the antimesenteric border. In the living these may be visible through the wall of the ileum from the outside. Blood Supply Arteries The arterial supply is from branches of the superior mesenteric artery. The intestinal branches arise from the left side of the artery and run in the mesentery to reach the gut. They anastomose with one another to form a series of arcades. The lowest part of the ileum is also supplied by the ileocolic artery. Veins The veins correspond to the branches of the superior mesenteric artery and drain into the superior mesenteric vein. Lymph Drainage The lymph vessels pass through many intermediate mesenteric nodes and finally reach the superior mesenteric nodes, which are situated around the origin of the superior mesenteric artery. Nerve Supply The nerves are derived from the sympathetic and parasympathetic (vagus) nerves from the superior mesenteric plexus. Large Intestine The large intestine extends from the ileum to the anus. It is divided into the cecum, appendix, ascending colon, transverse colon, descending colon, and sigmoid colon; the rectum and anal canal are considered in the sections on the pelvis and perineum. The primary function of the large intestine is the absorption of water and electrolytes and the storage of undigested material until it can be expelled from the body as feces. Cecum Location and Description The cecum is that part of the large intestine that lies below the level of the junction of the ileum with the large intestine. It is a blind-ended pouch that is situated in the right iliac fossa. It is about 6 cm long and is completely covered with peritoneum. It possesses a considerable amount of mobility, although it does not have a mesentery. Attached to its posteromedial surface is the appendix. The presence of peritoneal folds in the vicinity of the cecum creates the superior ileocecal, the inferior ileocecal, and the retrocecal recesses. As in the colon, the longitudinal muscle is restricted to three flat bands, the teniae coli, which converge on the base of the appendix and provide for it a complete longitudinal muscle coat. The cecum is often distended with gas and can then be palpated through the anterior abdominal wall in the living patient. The terminal part of the ileum enters the large intestine at the junction of the cecum with the ascending colon. The opening is provided with two folds, or lips, which form the so-called ileocecal valve (see below). The appendix communicates with the cavity of the cecum through an opening located below and behind the ileocecal opening. Relations • Anteriorly: Coils of small intestine, sometimes part of the greater omentum, and the anterior abdominal wall in the right iliac region. • Posteriorly: The psoas and the iliacus muscles, the femoral nerve, and the lateral cutaneous nerve of the thigh. The appendix is commonly found behind the cecum. • Medially: The appendix arises from the cecum on its medial side. Blood Supply Arteries Anterior and posterior cecal arteries form the ileocolic artery, a branch of the superior mesenteric artery. Veins The veins correspond to the arteries and drain into the superior mesenteric vein. Lymph Drainage The lymph vessels pass through several mesenteric nodes and finally reach the superior mesenteric nodes. Nerve Supply Branches from the sympathetic and parasympathetic (vagus) nerves form the superior mesenteric plexus. Ileocecal Valve A rudimentary structure, the ileocecal valve consists of two horizontal folds of mucous membrane that project around the orifice of the ileum. The valve plays little or no part in the prevention of reflux of cecal contents into the ileum. The circular muscle of the lower end of the ileum (called the ileocecal sphincter by physiologists) serves as a sphincter and controls the flow of contents from the ileum into the colon. The smooth muscle tone is reflexly increased when the cecum is distended; the hormone gastrin, which is produced by the stomach, causes relaxation of the muscle tone. Appendix Location and Description The appendix is a narrow, muscular tube containing a large amount of lymphoid tissue. It varies in length from 8-13 cm. The base is attached to the posteromedial surface of the cecum about 2.5 cm below the ileocecal junction. The remainder of the appendix is free. It has a complete peritoneal covering, which is attached to the lower layer of the mesentery of the small intestine by a short mesentery of its own, the mesoappendix. The mesoappendix contains the appendicular vessels and nerves. The appendix lies in the right iliac fossa, and in relation to the anterior abdominal wall its base is situated one-third of the way up the line joining the right anterior superior iliac spine to the umbilicus (McBurney's point). Inside the abdomen the base of the appendix is easily found by identifying the teniae coli of the cecum and tracing them to the base of the appendix, where they converge to form a continuous longitudinal muscle coat. Common Positions of the Tip of the Appendix The tip of the appendix is subject to a considerable range of movement and may be found in the following positions: (1)hanging down into the pelvis against the right pelvic wall, (2) coiled up behind the cecum, (3) projecting upward along the lateral side of the cecum, and (4) in front of or behind the terminal part of the ileum. The first and second positions are the commonest sites. Blood Supply Arteries The appendicular artery is a branch of the posterior cecal artery. It passes to the tip of the appendix in the mesoappendix. Veins The appendicular vein drains into the posterior cecal vein. Lymph Drainage The lymph vessels drain into one or two nodes lying in the mesoappendix and then eventually into the superior mesenteric nodes. Nerve Supply The nerves are derived from sympathetic and parasympathetic (vagus) nerves from the superior mesenteric plexus. Afferent nerve fibers concerned with the conduction of visceral pain from the appendix accompany the sympathetic nerves and enter the spinal cord at the level of the tenth thoracic segment. Ascending Colon Location and Description The ascending colon is about 13 cm long and lies in the right lower quadrant. It extends upward from the cecum to the inferior surface of the right lobe of the liver, where it turns to the left, forming the right colic flexure, and becomes continuous with the transverse colon. The peritoneum covers the front and the sides of the ascending colon, binding it to the posterior abdominal wall. Relations • Anteriorly: Coils of small intestine, the greater omenturn, and the anterior abdominal wall. • Posteriorly: The iliacus, the iliac crest, the quadratus lumborum, the origin of the transversus abdominis muscle, and the lower pole of the right kidney. The iliohypogastric and the ilioinguinal nerves cross behind it. Blood Supply Arteries The ileocolic and right colic branches of the superior mesenteric artery. Veins The veins correspond to the arteries and drain into the superior mesenteric vein. Lymph Drainage The lymph vessels drain into lymph nodes lying along the course of the colic blood vessels and ultimately reach the superior mesenteric nodes. Nerve Supply Sympathetic and parasympathetic (vagus) nerves from the superior mesenteric plexus. Transverse Colon Location and Description The transverse colon is about 38 cm long and extends across the abdomen, occupying the umbilical region. It begins at the right colic flexure below the right lobe of the liver and hangs downward, suspended by the transverse mesocolon from the pancreas. It then ascends to the left colic flexure below the spleen. The left colic flexure is higher than the right colic flexure and is suspended from the diaphragm by the phrenicocolic ligament. The transverse mesocolon, or mesentery of the transverse colon, suspends the transverse colon from the anterior border of the pancreas. The mesentery is attached to the superior border of the transverse colon, and the posterior layers of the greater omentum are attached to the inferior border. Because of the length of the transverse mesocolon, the position of the transverse colon is extremely variable and may sometimes reach down as far as the pelvis. Relations • Anteriorly: The greater omentum and the anterior abdominal wall (umbilical and hypogastric regions). • Posteriorly: The second part of the duodenum, the head of the pancreas, and the coils of the jejunum and ileum. Blood Supply Arteries The proximal two-thirds is supplied by the middle colic artery, a branch of the superior mesenteric artery. The distal third is supplied by the left colic artery, a branch of the inferior mesenteric artery. Veins The veins correspond to the arteries and drain into the superior and inferior mesenteric veins. Lymph Drainage The proximal two-thirds drains into the colic nodes and then into the superior mesenteric nodes; the distal third drains into the colic nodes and then into the inferior mesenteric nodes. Nerve Supply The proximal two-thirds is innervated by sympathetic and vagal nerves through the superior mesenteric plexus; the distal third is innervated by sympathetic and parasympathetic pelvic splanchnic nerves through the inferior mesenteric plexus. Descending Colon Location and Description The descending colon is about 25 cm long and lies in the left upper and lower quadrants. It extends downward from the left colic flexure, to the pelvic brim, where it becomes continuous with the sigmoid colon. The peritoneum covers the front and the sides and binds it to the posterior abdominal wall. Relations • Anteriorly: Coils of small intestine, the greater omentum, and the anterior abdominal wall. • Posteriorly: The lateral border of the left kidney, the origin of the transversus abdominis muscle, the quadratus lumborum, the iliac crest, the iliacus, and the left psoas. The iliohypogastric and the ilioinguinal nerves, the lateral cutaneous nerve of the thigh, and the femoral nerve also lie posteriorly. Blood Supply Arteries The left colic and the sigmoid branches of the inferior mesenteric artery. Veins The veins correspond to the arteries and drain into the inferior mesenteric vein. Lymph Drainage Colic lymph nodes and the inferior mesenteric nodes around the origin of the inferiorimesenteric artery. Nerve Supply Sympathetic and parasympathetic pelvic splanchnic nerves through the inferior mesenteric plexus. Differences between the Small and Large Intestine External Differences 1. The small intestine (with the exception of the duodenum) is mobile, whereas the ascending and descending parts of the colon are fixed. 2. The caliber of the full small intestine is normally smaller than that of the filled large intestine. 3. The small intestine (with the exception of the duodenum) has a mesentery that passes downward across the midline into the right iliac fossa. The longitudinal muscle of the small intestine forms a continuous layer around the gut. In the large intestine (with the exception of the appendix) the longitudinal muscle is collected into three bands, the teniae coli. The small intestine has no fatty tags attached to its wall. The large intestine has fatty tags, called the appendices epiploicae. The wall of the small intestine is smooth, whereas that of the large intestine is sacculated. Internal Differences 1. The mucous membrane of the small intestine has permanent folds, called plicae circulares, which are absent in the large intestine. 2. The mucous membrane of the small intestine has villi, which are absent in the large intestine. 3. Aggregations of lymphoid tissue called Peyer's patches are found in the mucous membrane of the small intestine; these are absent in the large intestine. Liver Location and Description The liver is the largest gland in the body and has a wide variety of functions. Three of its basic functions are (1) production and secretion of bile, which is passed into the intestinal tract; (2) involvement in many metabolic activities related to carbohydrate, fat, and protein metabolism; and (3) filtration of the blood, removing bacteria and other foreign particles that have gained entrance to the blood from the lumen of the intestine. The liver is soft and pliable and occupies the upper part of the abdominal cavity just beneath the diaphragm. The greater part of the liver is situated under cover of the right costal margin, and the right hemidiaphragm separates it from the pleura, lungs, pericardium, and heart. The liver extends to the left to reach the left hemidiaphragm. The convex upper surface of the liver is molded to the undersurface of the domes of the diaphragm. The posteroinferior, or visceral surface, is molded to adjacent viscera and is therefore irregular in shape; it lies in contact with the abdominal part of the esophagus, the stomach, the duodenum, the right colic flexure, the right kidney and suprarenal gland, and the gallbladder. The liver may be divided into a large right lobe and a small left lobe by the attachment of the peritoneum of the falciform ligament. The right lobe is further divided into a quadrate lobe and a caudate lobe by the presence of the gallbladder, the fissure for the ligamentum teres, the inferior vena cava, and the fissure for the ligamentum venosum. Experiments have shown that, in fact, the quadrate and caudate lobes are a functional part of the left lobe of the liver. Thus, the right and left branches of the hepatic artery and portal vein, and the right and left hepatic ducts, are distributed to the right lobe and the left lobe (plus quadrate plus caudate lobes), respectively. Apparently the two sides overlap very little. The porta hepatis, or hilum of the liver, is found on the posteroinferior surface and lies between the caudate and quadrate lobes (Fig. 5-33). The upper part of the free edge of the lesser omentum is attached to its margins. In it lie the right and left hepatic ducts, the right and left branches of the hepatic artery, the portal vein, and sympathetic and parasympathetic nerve fibers. A few hepatic lymph nodes lie here; they drain the liver and gallbladder and send their efferent vessels to the celiac lymph nodes. The liver is completely surrounded by a fibrous capsule but only partially covered by peritoneum. The liver is made up of liver lobules. The central vein of each lobule is a tributary of the hepatic veins. In the spaces between the lobules are the portal canals, which contain branches of the hepatic artery, portal vein, and a tributary of a bile duct (portal triad). The arterial and venous blood passes between the liver cells by means of sinusoids and drains into the central vein. Important Relations • Anteriorly: Diaphragm, right and left costal margins, right and left pleura and lower margins of both lungs, xiphoid process, and anterior abdominal wall in the subcostal angle. • Posteriorly: Diaphragm, right kidney, hepatic flexure of the colon, duodenum, gallbladder, inferior vena cava, and esophagus and fundus of the stomach. Peritoneal Ligaments of the Liver The falciform ligament, which is a two-layered fold of the peritoneum, ascends from the umbilicus to the liver. It has a sickle-shaped free margin that contains the ligamentum teres, the remains of the umbilical vein. The falciform ligament passes on to the anterior and then the superior surfaces of the liver and then splits into two layers. The right layer forms the upper layer of the coronary ligament; the left layer forms the upper layer of the left triangular ligament. The right extremity of the coronary ligament is known as the right triangular ligament of the liver. It should be noted that the peritoneal layers forming the coronary ligament are widely separated, leaving an area of liver devoid of peritoneum. Such an area is referred to as a "bare" area of the liver. The ligamentum teres passes into a fissure on the visceral surface of the liver and joins the left branch of the portal vein in the porta hepatis. The ligamentum venosum, a fibrous band that is the remains of the ductus venosus, is attached to the left branch of the portal vein and ascends in a fissure on the visceral surface of the liver to be attached above to the inferior vena cava. In the fetus, oxygenated blood is brought to the liver in the umbilical vein (ligamentum teres). The greater proportion of the blood bypasses the liver in the ductus venosus (ligamentum venosum) and joins the inferior vena cava. At birth, the umbilical vein and ductus venosus close and become fibrous cords. The lesser omentum arises from the edges of the porta hepatis and the fissure for the ligamentum venosum and passes down to the lesser curvature of the stomach. Blood Supply Arteries The hepatic artery, a branch of the celiac artery, divides into right and left terminal branches that enter the porta hepatis. Veins The portal vein divides into right and left terminal branches that enter the porta hepatis behind the arteries. The hepatic veins (three or more) emerge from the posterior surface of the liver and drain into the inferior vena cava. Blood Circulation Through the Liver The blood vessels conveying blood to the liver are the hepatic artery (30%) and portal vein (70%). The hepatic artery brings oxygenated blood to the liver, and the portal vein brings venous blood rich in the products of digestion, which have been absorbed from the gastrointestinal tract. The arterial and venous blood is conducted to the central vein of each liver lobule by the liver sinusoids. The central veins drain into the right and left hepatic veins, and these leave the posterior surface of the liver and open directly into the inferior vena cava. Lymph Drainage The liver produces a large amount of lymph - about onethird to one-half of all body lymph. The lymph vessels leave the liver and enter several lymph nodes in the porta hepatis. The efferent vessels pass to the celiac nodes. A few vessels pass from the bare area of the liver through the diaphragm to the posterior mediastinal lymph nodes. Nerve Supply Sympathetic and parasympathetic nerves form the celiac plexus. The anterior vagal trunk gives rise to a large hepatic branch, which passes directly to the liver. Bile Ducts of the Liver Bile is secreted by the liver cells, stored, and concentrated in the gallbladder; later it is delivered to the duodenum. The bile ducts of the liver consist of the right and left hepatic ducts, the common hepatic duct, the bile duct, the gallbladder, and the cystic duct. The smallest interlobular tributaries of the bile ducts are situated in the portal canals of the liver; they receive the bile canaliculi. The interlobular ducts join one another to form progressively larger ducts and, eventually, at the porta hepatis, form the right and left hepatic ducts. The right hepatic duct drains the right lobe of the liver and the left duct drains the left lobe, caudate lobe, and quadrate lobe. Hepatic Ducts The right and left hepatic ducts emerge from the right and left lobes of the liver in the porta hepatis. After a short course the hepatic ducts unite to form the common hepatic duct. The common hepatic duct is about 4 cm long and descends within the free margin of the lesser omentum. It is joined on the right side by the cystic duct from the gallbladder to form the bile duct. Bile Duct The bile duct (common bile duct) is about 8 cm long. In the first part of its course it lies in the right free margin of the lesser omentum in front of the opening into the lesser sac. Here it lies in front of the right margin of the portal vein and on the right of the hepatic artery. In the second part of its course it is situated behind the first part of the duodenum to the right of the gastroduodenal artery. In the third part of its course it lies in a groove on the posterior surface of the head of the pancreas. Here, the bile duct comes into contact with the main pancreatic duct. The bile duct ends below by piercing the medial wall of the second part of the duodenum about halfway down its length. It is usually joined by the main pancreatic duct, and together they open into a small ampulla in the duodenal wall, called the ampulla of Vater. The ampulla opens into the lumen of the duodenum by means of a small papilla, the major duodenal papilla. The terminal parts of both ducts and the ampulla are surrounded by circular muscle, known as the sphincter of Oddi. Occasionally, the bile and pancreatic ducts open separately into the duodenum. The common variations of this arrangement are shown diagrammatically in Figure 4- . Gallbladder Location and Description The gallbladder is a pear-shaped sac lying on the undersurface of the liver. It has a capacity of about 30 to 50 mL and stores bile, which it concentrates by absorbing water. For descriptive purposes the gallbladder is divided into the fundus, body, and neck. The fundus is rounded and usually projects below the inferior margin of the liver, where it comes in contact with the anterior abdominal wall at the level of the tip of the ninth right costal cartilage. The body lies in contact with the visceral surface of the liver and is directed upward, backward, and to the left. The neck becomes continuous with the cystic duct, which turns into the lesser omentum to join the right side of the common hepatic duct, to form the bile duct. The peritoneum completely surrounds the fundus of the gallbladder and binds the body and neck to the visceral surface of the liver. Relations • Anteriorly: The anterior abdominal wall and the inferior surface of the liver. • Posteriorly: The transverse colon and the first and second parts of the duodenum. Function The gallbladder serves as a reservoir for bile. It has the ability to concentrate the bile, and to aid this process the mucous membrane is thrown into permanent folds that unite with each other, giving the surface a honeycombed appearance. The columnar cells lining the surface also have numerous microvilli on their free surface. Bile is delivered to the duodenum as the result of contraction and partial emptying of the gallbladder. This mechanism is initiated by the entrance of fatty foods into the duodenum. The fat causes release of the hormone cholecystokinin from the mucous membrane of the duodenum; the hormone then enters the blood, causing the gallbladder to contract. At the same time the smooth muscle around the distal end of the bile duct and the ampulla is relaxed, thus allowing the passage of concentrated bile into the duodenum. The bile salts in the bile are important in emulsifying the fat in the intestine and in assisting with its digestion and absorption. Blood Supply Arteries Cystic artery, a branch of the right hepatic artery. Veins The cystic vein drains directly into the portal vein. Several very small arteries and veins also run between the liver and gallbladder. Lymph Drainage The lymph drains into a cystic lymph node situated near the neck of the gallbladder. From here the lymph vessels pass to the hepatic nodes along the course of the hepatic artery and then to the celiac nodes. Nerve Supply Sympathetic and parasympathetic vagal fibers form the celiac plexus. The gallbladder contracts in response to the hormone cholecystokinin, which is produced by the mucous membrane of the duodenum on the arrival of fatty food from the stomach. Cystic Duct The cystic duct is about 3.8 cm long and connects the neck of the gallbladder to the common hepatic duct to form the bile duct. It usually is somewhat S shaped and descends for a variable distance in the right free margin of the lesser omentum. The mucous membrane of the cystic duct is raised to form a spiral fold that is continuous with a similar fold in the neck of the gallbladder. The fold is commonly known as the "spiral valve." The function of the spiral valve is to keep the lumen constantly open. Pancreas Location and Description The pancreas is both an exocrine and an endocrine gland. The exocrine portion of the gland produces a secretion that contains enzymes capable of hydrolyzing proteins, fats, and carbohydrates. The endocrine portion of the gland, the islets of Langerhans, produces the hormones insulin and glucagon, which play a key role in carbohydrate metabolism. The pancreas is an elongated structure that lies in the epigastrium and the left upper quadrant. It is soft and lobulated and situated on the posterior abdominal wall behind the peritoneum. It crosses the transpyloric plane. The pancreas is divided into a head, neck, body, and tail (Fig. 4- ). The head of the pancreas is disc shaped and lies within the concavity of the duodenum. A part of the head extends to the left behind the superior mesenteric vessels and is called the uncinate process. The neck is the constricted portion of the pancreas and connects the head to the body. It lies in front of the beginning of the portal vein and the origin of the superior mesenteric artery from the aorta. The body runs upward and to the left across the midline. It is somewhat triangular in cross section. The tail passes forward in the splenicorenal ligament and comes in contact with the hilum of the spleen. Relations • Anteriorly: From right to left: the transverse colon and the attachment of the transverse mesocolon, the lesser sac, and the stomach. • Posteriorly: From right to left: the bile duct, the portal and splenic veins, the inferior vena cava, the aorta, the origin of the superior mesenteric artery, the left psoas muscle, the left suprarenal gland, the left kidney, and the hilum of the spleen. Pancreatic Ducts The main duct of the pancreas begins in the tail and runs the length of the gland, receiving numerous tributaries on the way. It opens into the second part of the duodenum at about its middle with the bile duct on the major duodenal papilla. Sometimes the main duct drains separately into the duodenum. The accessory duct of the pancreas, when present, drains the upper part of the head and then opens into the duodenum a short distance above the main duct on the minor duodenal papilla. The accessory duct frequently communicates with the main duct. Blood Supply Arteries The splenic and the superior and inferior pancreaticoduodenal arteries. Veins The corresponding veins drain into the portal system. Lymph Drainage Lymph nodes situated along the arteries that supply the gland. The efferent vessels ultimately drain into the celiac and superior mesenteric lymph nodes. Nerve Supply Sympathetic and parasympathetic (vagal) nerve fibers. Spleen Location and Description The spleen is reddish and is the largest single mass of lymphoid tissue in the body. It is oval shaped and has a notched anterior border. It lies just beneath the left half of the diaphragm close to the ninth, tenth, and eleventh ribs. The long axis lies along the shaft of the tenth rib, and its lower pole extends forward only as far as the midaxillary line and cannot be palpated on clinical examination. The spleen is surrounded by peritoneum, which passes from it at the hilum as the gastrosplenic omentum (ligament) to the greater curvature of the stomach (carrying the short gastric and left gastroepiploic vessels). The peritoneum also passes to the left kidney as the splenicorenal ligament (carrying the splenic vessels and the tail of the pancreas). Relations • Anteriorly: The stomach, the tail of the pancreas, and the left colic flexure. The left kidney lies along its medial border. • Posteriorly: The diaphragm; the left pleura (left costodiaphragmatic recess); the left lung; and the ninth, tenth, and eleventh ribs. Blood Supply Arteries Large splenic artery, which is the largest branch of the celiac artery. It has a tortuous course as it runs along the upper border of the pancreas. The splenic artery then divides into about six branches, which enter the spleen at the hilum. Veins The splenic vein leaves the hilum and runs behind the tail and the body of the pancreas. Behind the neck of the pancreas the splenic vein joins the superior mesenteric vein to form the portal vein. Lymph Drainage The lymph vessels emerge from the hilum and pass through a few lymph nodes along the course of the splenic artery and then drain into the celiac nodes. Nerve Supply The nerves accompany the splenic artery and are derived from the celiac plexus. Retroperitoneal Space The retroperitoneal space lies on the posterior abdominal wall behind the parietal peritoneum. It extends from the twelfth thoracic vertebra and the twelfth rib to the sacrum and the iliac crests below. The floor or posterior wall of the space is formed from medial to lateral by the psoas and quadratus lumborum muscles and the origin of the transversus abdominis muscle. Each of these muscles is covered on the anterior surface by a definite layer of fascia. In front of the fascial layers is a variable amount of fatty connective tissue that forms a bed for the suprarenal glands, the kidneys, the ascending and descending parts of the colon, and the duodenum. The retroperitoneal space also contains the ureters and the renal and gonadal blood vessels. 5.2. Theoretical questions to studies: 1. The topographical anatomy of the esophagus. 2. The topographical anatomy of the stomach. 3. The topographical anatomy of the duodenum. 4. The topographical anatomy of the jejunum. 5. The topographical anatomy of the ileum. 6. The topographical anatomy of the large intestine. 7. The topographical anatomy of the cecum. 8. The topographical anatomy of the appendix. 9. The topographical anatomy of the liver. 10.The topographical anatomy of the gallbladder. 11.The topographical anatomy of the bile ducts. 12.The topographical anatomy of the pancreas. 5.3. Materials for self-control: 1. The lesser omentum is incised close to its free edge, and the biliary tree is identified and freed by blunt dissection. The liquid contents of the gallbladder are aspirated with a syringe, the fundus incised, and the stones removed. The entire duct system is carefully probed for stones, one of which is found to be obstructing a duct. In view of the observation that the patient is not jaundiced, the most probable location of the obstruction is A the bile duct B the common hepatic duct C the cystic duct D within the duodenal papilla proximal to the juncture with the pancreatic duct E within the duodenal papilla distal to the juncture with the pancreatic duct 2. It is ascertained that an accessory right hepatic artery inadvertently had been torn. There is no choice but to ligate the accessory artery. The effect of this ligation most probably will be A ischemic necrosis of the quadrate lobe of the liver B ischemic necrosis of a discrete portion of the right lobe of the liver C no necrosis in any lobe because of the integrity of the hepatic portal vein D no necrosis in any lobe because of extrahepatic collateral blood supply E no necrosis in any lobe because of intrahepatic collateral blood supply 3. The biliary duct system is carefully dissected. The cystic artery and cystic duct both are identified, ligated, and divided, the duct at a point about an eighth of an inch from its juncture with the common hepatic duct. The gallbladder is then freed from the inferior surface of the liver by blunt dissection and removed. However, the operative field suddenly fills with arterial blood. In order to locate and ligate the bleeder, hemorrhage should be controlled by A ligating the common hepatic artery B ligating the proper hepatic artery distal to the origin of the right gastric and gastroduodenal arteries C ligating the left hepatic artery, especially if there are additional (aberrant) left hepatic arteries present D ligating the hepatic portal vein E temporarily compressing the hepatic pedicle 4. The subcostal incision, which parallels the costal margin anteriorly, is closed in layers. The patient is allowed up on her first postoperative day; on the third day the drain (which shows no bile leakage) is withdrawn, and on the tenth day the patient is discharged. As a result of the location and direction of the incision, one might expect healing to result in A loss of blood supply and necrosis of a portion of the rectus ab-dominis muscle B significant paralysis of a portion of the rectus abdominis muscle C minimal scarring D negligible possibility of subsequent abdominal herniation E none of the above 5. The crampy abdominal pain referred to the umbilical region and knowledge of peritoneal structure would lead the examining physician to suspect that the strangulated section of gut was most likely the A ascending colon B descending colon C small intestine D sigmoid colon E stomach 6. At surgery a loop of herniated gut appeared ischemic and was strangulated. While enlarging the hernial defect superiorly in the mid-line so that the loop of gut could be replaced into the abdominal cavity, profuse dark bleeding occurred. The source of the bleeding was not readily apparent, but the surgeon should have suspected that the origin was most likely due to severing the A inferior epigastric artery B dilated paraumbilical veins C superior epigastric artery D inferior mesenteric artery E veins of Retzius, which connect secondarily retroperitoneal structures to veins of the abdominal wall 7. In portal hypertension where blood flow through the liver is impeded, in addition to via the caput medusae, blood may return to the systemic circulation via all the following EXCEPT the A esophageal veins B inferior rectal veins C middle rectal veins D veins associated with the transverse colon E veins of Retzius associated with the descending colon 8. As standard prophylaxis, the small intestine was inspected unsuccessfully for the presence of an ileal diverticulum. All the following statements pertain to Meckel’s diverticulum EXCEPT A it is a remnant of the urachus B it is found on the antimesenteric side of the gut C it is located within 3 feet of the ileocecal valve D it is present in 3 percent of the population E it is usually lined by gastric mucosa 9. Next, the appendix was located and removed as prophylaxis. The vermiform appendix is best located by following the A B C D E anterior cecal artery descending branch of the right colic artery ileum to the ileocolic juncture posterior cecal artery teniae coli of the ascending colon 10. After the herniated segment of gut was placed into the abdominal cavity, its color changed from purple to pink, which indicated that the vasculature was functional. The small intestine normally receives significant collateral circulation from the A descending branch of the left colic artery B renal arteries C splenic artery D superior pancreaticoduodenal artery E none of the above 11. On manual exploration of the abdominal cavity, the liver was felt to be hard and nodular. This, in addition to the history of hematemesis, indicated that control of the portal hypertension was necessary. In a patient with cirrhosis of the liver, venous hypertension would be expected in A the hepatic vein B the renal vein C the short gastric veins D the suprarenal vein E none of the above 12. The incision was extended and the hepatic portal vein located. To relieve the portal hypertension, a side-to-side anastomosis was made between the portal vein and the inferior vena cava. The location of the inferior vena cava is A across the omental foramen from the portal vein B anterior and to the left of the portal vein C immediately to the right of the portal vein D posterior and to the right of the portal vein E none of the above 13. The lateral umbilical fold on each side is created by the underlying A falx inguinalis B inferior epigastric artery C lateral border of the rectus sheath D obliterated umbilical artery E urachus 14. A posteriorly perforating ulcer in the pyloric antrum of the stomach is most likely to produce initial localized peritonitis or abscess formation in the ‘ A greater sac B left subhepatic and hepatorenal spaces (pouch of Morison) C omental bursa D right subphrenic space E right subhepatic space 15. The lesser sac (omental bursa) is directly continuous with which of the following recesses or spaces? A Infracolic compartment B Left colic gutter C Left subphrenic recess D Right subphrenic space E Hepatorenal recess 16. A patient is diagnosed as having intestinal angina (thrombotic occlusion of the superior mesenteric artery near its origin). If significant collateral circulation is not present or fails to develop, all the following parts of the intestinal tract may become gangrenous EXCEPT the A ascending colon B appendix C descending colon D ileum E transverse colon 17. The myenteric plexus is characterized by all the following statements EXCEPT A it contains cell bodies of parasympathetic neurons B it contains enteric neurons C it contains neurons that regulate the enteric reflex D it innervates the glands of the mucosa E it is located between the layers of the muscularis externa 18. Mucosal necrosis of the rectum usually will not result from occlusion of the inferior mesenteric artery because A arterial supply to the rectum is from anastomotic connections from the superior mesenteric artery B arterial supply to the rectum is from the left colic artery with anastomoses at Sudeck’s point C the inferior mesenteric artery does not supply the rectum D a principal branch of the external iliac artery is a major supplier to the rectum E the middle rectal artery, a branch of the internal iliac artery, supplies the rectum 19. Pain associated with external hemorrhoids is mediated by A the hypogastric nerves to the lumbar splanchnic nerves B the pelvic splanchnic nerves (nervi erigentes) C the pudendal nerve D the sacral sympathetic chain E none of the above Literature 1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams & Wilkins, 2000. – 898 p. 2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and Technique. – Springer, 1995. – 674 p. 3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p. 4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical students. – Blackwell publishing, 2006. – 439 p.