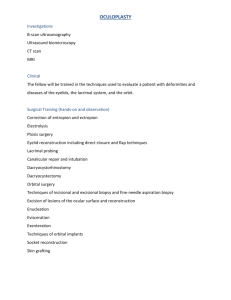
Eyelid Anatomy and Evaluation

Lip Teh
December 2005
Eyelid Anatomy and Evaluation
Embryology
eyelids develop from mesenchymal folds above and below the optic cup beginning during the 4 - 5 week
week 10 – eyelids make contact along their margin and temporarily fuse by desmosomes, thus isolating the eyes from amniotic fluid
begin to separate at 20 weeks
Failure of complete separation results clinically in varying degrees of ankyloblepharon
Levator develops late in the 3 rd
month
Initially, the levator and superior rectus are blended as one common muscle.
When the fetus reaches 60 mm in length, the levator muscle separates.
This unique two-stage embryogenesis may explain why the levator muscle is the eye muscle most prone to defects.
Anatomy
Lip Teh
December 2005
Eyelid skin
thinnest in human body (0.7mm), upper thicker than lower.
dense sweat glands
least sebaceous glands
Blood supply
marginal arcade - superior and inferior marginal palpebral arcades
peripheral arcade – at proximal end of tarsal plate
contibutors:
1.
superomedial - dorsal nasal artery, supraorbital artery, supratrochlea artery
2.
superolateral - frontal branch of superficial temporal artery
(Zygomaticoorbital – branch of middle temporal artery), lacrimal artery
3.
inferomedial - angular artery, infraorbital artery
4.
inferolateral - zygomaticofacial artery, transverse facial artery
Lip Teh
December 2005
Nerve supply
superomedial - supraorbital nerve, supratrochlea nerve, infratrochlea nerve
(V1)
superolateral – lacrimal (v1)
inferomedial - infraorbital nerve(v2), infratrochlea nerve
inferolateral - zygomaticofacial nerve (v2)
Lymphatics
preauricular nodes – upper lid, lateral canthus, lateral ½ of lower lid
submandibular nodes (via lymphatics of facial vein) – medial canthus, medial
½ lower lid layers
anterior lamellae - skin and orbicularis
middle lamellae - septum
posterior lamellae – tarsus, retractors and conjunctiva
Lip Teh
December 2005
Orbicularis oculi
palpebral (preseptal, pretarsal) and orbital parts
gentle blink - pretarsal and preseptal
hard blink –orbital part
Riolan's muscle - at lid margin, forms gray line
orbicularis oculi has a direct muscle attachment to the inferior orbital rim from the anterior lacrimal crest out to approximately the level of the medial corneoscleral limbus above the origin of the levator labii superioris. Lateral to this point, the attachment of the orbicularis to the rim is indirect through the orbicularis retaining ligament
Nerve suppy (on deep surface): o Superior - temporal and zygomatic branches o Inferior – segmental supply from buccal and zygomatic branches o Relevance is that subciliary skin/muscle flaps will not denervate the muscle
Lip Teh
December 2005
Orbicularis retaining ligament (orbito-malar ligament)PRS Sept 2002
bilaminar septum-like structure attaching the orbicularis oculi to the inferior orbital rim.
The attachment of the retaining ligament is broader and stronger inferolaterally than centrally.
Aging changes of the retaining ligament are associated with distension, elongation, and thinning.
Lip Teh
December 2005
ORL is negligible medially, increases to a maximum centrally, and then diminishes laterally. Its laxity creates a V-shaped deformity
Levator palpebrae
Lie deep to the preaponeurotic fat
55mm (40mm muscle), 10-15mm excursion
origin – lesser wing of sphenoid
changes direction from horizontal to vertical at Whitnall’s ligament ( superior to muscle)
insertion
anterior fibres – orbital septum/skin forming supratarsal fold
posterior fibres – anterior surface of tarsus 3-4mm below superior border
medial horn – posterior limb of medial canthal ligament
lateral horn – superior edge of lateral canthal ligament, dividing lacrimal gland into orbital and palpebral parts
Alternative theory (R Siegel)
Dynamic fusion between levator aponeurosis and septum with intervening fat (zipper or conjoint fascia). Eyelid folds at the superior end of the fusion
Take too much fat and the fusion point will move superiorly giving the impression of ptosis.
Lip Teh
December 2005
Mullers muscle
nonstriated smooth muscle (10mm long, 15mm wide)
2-3mm of excursion
inserts superior border of tarsal plate
nerve supply: sympathetic (T1) via internal carotid artery
Inferior Oblique muscle
originates on the orbital floor, 5.14 ± 1.21 mm posterior to the inferior orbital rim, on a line extending from the infraorbital foramen to 10 ± 0.9 mm medial to the supraorbital notch along the supramedial orbital rim.
Lip Teh
December 2005
Capsulopalpebral ligament
Condenses from Lockwood’s ligament (inferior oblique)
5mm length
Equivalent to levator for lower lid
Some fibres insert into dermis to contribute to lower eyelid crease
Deep to the fascia lies the inferior tarsal muscle, which is analogous to
Mueller's muscle.
Tarsus
firm, dense fibrous tissue, contains Meibomian glands
extends from lateral canthus to punctum
superior 30mm long, 1mm thick, 10mm wide
attachments – pretarsal obicularis, levator (anterior), Mullers(superior), conjunctiva (posterior), canthal tendons
inferior 25mm long, 1mm thick, 5mm wide
attachments – pretarsal obicularis, capsulopalpebral ligament, conjunctiva, canthal tendons
Medial canthal tendon
anterior limb – anterior lacrimal crest (anterior to lacrimal sac)
posterior limb – posterior lacrimal crest
vertical limb – directed superoposteriorly.
Unlike lateral tendon, this inserts strongly into bone (Sharpys fibers)
medial retinaculum – formed by
1.
deep head of pretarsal orbicularis
2.
medial horn of levator
3.
medial part of Lockwoods ligament
4.
medial rectus check ligaments
5.
orbital septum
6.
Whitnall’s ligament
Lip Teh
December 2005
Lateral canthal tendon
inserts into periosteum (not to bone) around Whitnalls tubercle (2mm deep to lateral orbital rim, 10mm below ZF suture)
has superficial and deep (or anterior and posterior), and superior and inferior,
attachments to the orbital rim
lateral retinaculum – formed by
1.
lateral canthal tendon
2.
preseptal and pretarsal orbicularis
3.
lateral horn of levator
4.
Lockwood’s ligament
5.
lateral check ligaments
lateral palpebral raphe lies superficial - joining the upper and lower preseptal orbicularis muscle
Septum orbitale
arcus marginalis is where periosteum meets the septum
Lip Teh
December 2005
Upper lid – inserts into levator aponeurosis 10-15mm above tarsus
Lower lid – insers into capsulopalpebral fascia 5mm below tarsus
Laterally, the septum is attached to the orbital margin, 1.5 mm in front of the
Whitnall’s tubercle attachment of the lateral canthal tendon. The Eisler fat pocket separates the lateral canthal tendon from the orbital septum. From there, the septum continues along the superior orbital rim at the arcus marginalis. Superomedially, the septum bridges the supraorbital groove, passes inferomedially anterior to the trochlea, and then follows the posterior lacrimal crest. As it runs down the posterior lacrimal crest, it lies anterior to the medial check ligament and posterior to the Horner muscle (and hence behind the lacrimal sac). The line of attachment crosses the lacrimal sac fascia to reach the anterior lacrimal crest at the level of the lacrimal tubercle. From there, it passes inferiorly down the anterior lacrimal crest and laterally along the inferior orbital rim. A few millimeters lateral to the zygomaticomaxillary suture, the attachment leaves the rim and lies several millimeters from it on the facial aspect of the zygomatic bone, thus forming the fat-filled premarginal recess of Eisler. The line of attachment then continues to again reach the lateral orbital rim just below the level of the Whitnall ligament.
Lip Teh
December 2005
The orbicularis muscle fibers, together with skin (anterior lamella) insert anteriorly on the outer edge of the lateral orbital rim. The tarsoligamentous sling
(posterior lamella) inserts as the lateral canthal tendon inside the lateral rim on the lateral orbital tubercle.
Postseptal/preaponerotic fat pads
acts as a cushion to the eyelid and divides the septum from the levator aponeurosis,
this fat remains relatively constant regardless of obesity or weight loss.
There is a greater amount of connective tissue and blood vessels in white fat
(medial compartments); the yellow fat (lateral) has a greater amount of carotenoids.
Lip Teh
December 2005
Upper eyelid: 2 fat pads
1.
long thin central fat pocket, preaponeurotic fat, yellow
2.
globular medial fat pad – derived from intraconal orbital fat, white
3.
Separated by superior oblique
4.
medial fat pad is associated with the infratrochlear nerve and the terminal branch of the ophthalmic artery
Lower eye lid 3 fat pads (nasal, middle, and temporal)
5.
The medial and central fat pads are separated by the inferior oblique proper
6.
Lateral fat pad sits in Eisler’s recess, separated by arcuate expansion of inferior oblique
Lacrimal glands
Basic secretors
1.
goblet cells(conjuctival, tarsal and limbal) – inner layer mucin
2.
accessory glands of Krause and Wolfring (fornices) - aqueous
3.
meibomian glands (tarsal plate) - oil
Reflex secretors – main lacrimal gland o Lateral horn of the levator palpebrae superioris divides the lacrimal gland into an orbital(66%) and a palpebral lobe (33%) o lateral palpebral lobe is prone to prolapse and may be visible externally. o Ducts from orbital lobe pass through palpebral lobe. which in turn empties into the superolateral conjunctival fornix via six to twelve tear ductules. Extirpation of palpebral lobe equals total excision of glands o
Pilosebaceous(sweat) glands of Zeiss and the apocrine glands of Moll are located anterior to the meibomian glands within the distal eyelid margin (at the cilia)
1.
infected meibomian gland leads to internal hordeolum
2.
infected Zeiss or Moll gland leads to external hordeolum
Tear = 3 layers
1.
Innermost – mucous layer from goblet cells. Thinnest layer (0.05
m thick)
2.
Middle – aqueous layer from Krause and Wolfring (7.0
m thick)
3.
Outermost – lipid layer from Meibomian-stabilise and reduce evaporation (0.11
m thick) – also reduces surface tension so tears don’t form doplets on cornea
Needs presence of intact neural system o Afferent fibres from the cornea (ophthalmic division of the trigeminal nerve, V1) synapse in the nucleus of the spinal tract of V. Within the brainstem, secondary axons from this nucleus synapse in the reticular formation. This initiates bilateral contact with the facial nerve (VII) motor nuclei which, in turn, innervate both orbicular muscles resulting in eyelid closure. o stimulation of the cornea gives rise to stimulation of the parasympathetic facial nerve fibres via the salivary nucleus through to the greater petrosal nerve. o From the pterygopalatine ganglion, the post-synaptic fibres follow the zygomatic nerve via the lacrimal nerve to the gland itself
Lip Teh
December 2005 o normal or basal tear flow is predominantly under sympathetic control by regulating the gland’s blood supply, whereas reflex tear secretion is under parasympathetic control as a result of trigeminal nerve stimulation.
Drainage system
1.
Evaporative 15%
2.
Canaliculi 85% (lower 80%, upper 20%)
3.
Punctum Lacrimale - Each is a small round or oval orifice (~0.3mm in diameter) at the summit of papillae lacrimalis, situated at the junction of the ciliary & lacrimal portion of lid margin medially. It is in line with the openings of tarsal glands.
4.
Each canaliculi has 2 mm vertical component and a 7-8 mm horizontal component
5.
Upper horizontal limb is directed medially & inferiorly while the lower limb is directed medially & superiorly, both piercing lacrimal fascia & unite (>90%) forming a small diverticulum ( sinus of Maier ) prior of entering lateral wall of lacrimal sac ~ 2.5 mm below its apex, at the level of the lower border of medial canthal tendon. Valve of
Rosenmuller within diverticulum prevents reflux.
6.
Lacrimal sac - 12-15mm in vertical length. Portion above entrance of common canaliculus is the fundus ~3-4mm in height & is normally compressed by the medial canthal tendon. Anterior ethmoidal sinus lies medially.
Lip Teh
December 2005
Lip Teh
December 2005
Tear composition
1.
proteins/enzymes a.
protein composition of the closed-eye tear(immediately upon waking) is significantly different from that of the open and reflex-eye tear. b.
protein constituents of human tears maintain the surface integrity of the cornea and conjunctiva, protect the eye from microbial invasion, maintain the stability of the tear film and also act as a lubricant between the eye and eyelids c.
Secretory IgA, lactoferrin, lipocalin(tear-specific prealbumin) and lysozyme d.
predominant proteins in reflex and open-eye tears are lactoferrin, lipocalin and lysozyme e.
closed-eye tear is characterised by an increase in sIgA, albumin and decrease in lactoferrin, lipocalin and lysozyme.
2.
electrolytes a.
297 mEq/l b.
Na 132 mmol/L, K 24 mmol/L, HCO2 32.8mmol/L, Ca
0.8 mmol/L, Mg 0.61 mmol/L
3.
Superior Transverse Ligament (Whitnall’s ligament)
extends from the lacrimal gland fossa to the trochlea
acts as a fulcrum to allow for the change in direction of the levator and as a
check ligament for the levator muscle
Lip Teh
December 2005
Inferior Suspensory Ligament (Lockwood’s ligament)
originates as a fibroelastic tissue from the inferior oblique muscle as two sheets.
Anteriorly these sheets fuse to form Lockwood’s ligament.
Anterior to Lockwood’s ligament is the capsulopalpebral fascia.
Preseptal Fat
Submuscular areolar tissue deep to the orbicularis oculi muscle.
The lid may be split into anterior and posterior portions through this potential plane, which is reached by division at the gray line of the lid margin.
In the upper lid, this plane is traversed by fibers of the levator aponeurosis, some of which pass through the orbicularis to attach to the skin to form the lid crease.
In the lower eyelid, this plane is traversed by fibers of the orbitomalar ligament.
Lip Teh
December 2005
Superior continuance in this submuscular plane arrives at the retro-orbicularis oculi fat (ROOF), which is best developed in the eyebrow region.
Suborbicularis oculi fat (SOOF) is found in the lower lid in a continuance of this plane. Ramirez believes that ptosis of SOOF forms the malar fat pad which is anterior to zygomaticus major and levator labii superioris
Evaluation
History
1) aesthetic concerns – wrinkles/forehead/eyelids/bulges
2) functional concerns – blocking vision
3) ocular history - dry eyes, contact lenses
4) systemic diseases – bleeding disorders, thyroid disease, myasthenia gravis
5) medications –aspirin
Surface assessment
1.
Brow position
Hairline 5-6cm
Midpupil to bottom of brow >23mm
With brow elevated, check eyes can still close—if not brow lift is limited
Get patient to close eyes in relaxed posture, then have patient open eyes—measure automatic brow elevation=compensated brow ptosis = this compensation will be lost if brow-only ptosis done
Close eyes and totally relax forehead—press thumbs against brow to obstruct elevation by frontalis—now open eyes—this is resting brow posture and position of brow if bleph-only procedure is performed
Lip Teh
December 2005
2.
Globe
Visual acuity
Visual fields especially with ptosis
Proptosis vs exopthalmos o Exopthalmos defined as protusion secondary to endocrine dysfunction and proptosis as due to nonendocrine causes
Shallow anterior chamber - glaucoma
Bells Phenomenon
Reflex between facial and oculomotor nuclei
Corneal reflex
Reflex between V
1
and Facial nerve
3.
Lid aesthetics
Palpebral fissure is 1/5 of facial width
intercanthal distance
28-32mm in female 32-34mm male (1/2 interpupillary distance)
hyperteloric vs telecanthus
Supratarsal crease (margin-crease distance)
results from a fusion of the levator aponeurosis, orbital septum, and fascia of the orbicularis oculi into the dermis.
8-10mm above lid margin in Caucasians males, 10-11 in females
Siegel believes that the height shoud be determined by the balance of levator vs orbicularis (zipper fascia). Slightly lower fold if levator is weak.
2-3mm in most Asians
Palpebral fissure distance 10-11mm
upper lid margin overlaps limbus 1-2mm (limbus usually 11mm)
lower lid crease
4-6mm below lid margin
margin touches limbus
lateral commissure more mobile and more acute angle
lateral canthus higher than medial (0-2mm male, 2-4mm female)
mongoloid if this exaggerated
reverse slant - Treacher Collins
Visible pretarsal skin 3-6mm
Factors determining amount of visualised pre-tarsal skin
1.
Posture of brow at rest—the lower the brow the more lid overhang
2.
Amount of skin redundancy
3.
Level at which levator aponeurosis joins septum—ie level of fold
4.
Lid fat—more fat=less pretarsal skin
Lip Teh
December 2005
The mean height of the eye fissure measured from the upper lid ( P s ) to lower lid ( P i ) margin at the midpupil was 10.8 ± 1.2 mm. The mean length of the eye fissure measured from medial to lateral canthus was
30.7. The mean inclination of the eye fissure was 4.1 degrees ± 2.2 degrees
4.
Eyelid Bags
Consider
1.
excess skin a.
loss of skin elasticity - leading to rhytides, color and texture changes, and festoon formation. The thin skin unveils underlying irregularities including orbicularis, orbital fat, and the tear trough.
2.
excess fat – orbital fat prolapse a.
upper lid – reduced pretarsal skin show or lower crease b.
lower lid – eyelid bags defined below by the junction of the septum at the orbital rim. fat compartments may be visualised c.
may also be due to SOOF or malar fat pads d.
Unlike oedema, orbital fat is ballotable .
3.
excess fluid a.
eyelid accumulates fluid preferentially in systemic edema or local edema such as facial allergy b.
worse after a salty meal or in the morning. c.
Purplish color d.
Limited inferiorly by the orbital rim because of the cutaneous ligaments, but it does not show the orbital compartmentalization of orbital fat.
4.
excess muscle a.
combines with loss of skin elasticity to contribute to dynamic and static rhytides b.
Festoons of hypotonic muscle are diagnosed by the squinch test , in which the patient tightly contracts the orbicularis and the fold disappears.
5.
tear trough depression a.
feature of eyelid and midface aging b.
more likely in those with maxillary hypoplasia c.
due to loss of subcutaneous fat with thinning of the skin over the orbital rim ligaments combined with cheek descent
Lip Teh
December 2005
5.
Lid ptosis
Elevated position of tarsal crease suggests levator dehiscence
Differentiate from pseudoptosis (excess skin)
ptosis measurements (in primary gaze)
Upper lid to limbus overlap
1.
1-2mm mild
2.
3 moderate
3.
>4mm severe
Marginal reflex distance -1 (light reflex to upper lid margin)
1.
>2.5mm normal
Marginal reflex distance -2 (light reflex to lower lid margin)
1.
>5mm normal
eyelid excursion (levator function)
1.
0-4mm poor (severe >4mm ptosis)
2.
5-7
3.
8-10
4.
>11 fair good mm
(3mm ptosis)
(1-2mm ptosis) excellent
6.
Lid support (lower lid)
Distraction test
pull lid away from globe
>7mm abnormal
Snap back test
pulls lid away and inferiorly and allow to retract
Grade 0 - normal lid that returns to position immediately on release
Grade I - approximately 2-3 sec
Grade II - 4-5 sec
Grade III - >5 sec but does return to position with blinking
Grade IV - never returns to position and continues to hang down in frank ectropion after the snap-back test
Cheek lift o Assess for cicatricial ectropion o If lid margin reaches level of upper limbus, no problem
Intraoperative (Codner)
Pull the incised lower lid laterally
Distance the lower lid stretches to the orbital rim represents the amount of redundancy.
<3mm overlap – canthopexy, otherwise canthoplasty
7.
Canthal laxity tests
Lateral canthal tendon
Pull lower lid medially away from lateral canthus and measure displacement of lateral canthal corner; the greater the distance the more the laxity
Grade 0 - <2mm (normal)
Grade I - 2-4 mm
Grade II - 4-6 mm
Grade III - > 6 mm
Grade IV - >6mm and does not return to baseline even after blinking
Lip Teh
December 2005
Medial canthal tendon
distract the lower lid laterally.
Grade 0 – <2mm (normal)
Grade I - 2 mm displacement
Grade II - 3 mm
Grade III - >3 mm
Grade IV - does not return to baseline
8.
Lacrimal apparatus
Look for
Prolapsed gland
Everted puncta
Canalicular test
involves injection of saline into the lower canaliculus through a lacrimal cannula. o If the saline comes out the upper canaliculus, the test is considered positive; ie, the ducts are patent at least as far as their union with each other or with the lacrimal sac.
Lip Teh
December 2005
Primary dye test
Checks for intranasal staining after 1 drop fluorescein application in the eye
If dye is seen, the test is said to be positive, meaning there is no obstruction in the lacrimal passages and the epiphora is due to hypersecretion.
Secondary dye test
Follows the primary test – saline is flushed via a lacrimal canula.
Staining in the nose implies a partial obstruction.
Slit lamp examination
Stains: Rose bengal stains not only dead and devitalized cells but also healthy cells that are protected inadequately by a mucin coating.
Fluorescein pools in epithelial erosions and stains exposed basement membrane.
Decreased tear meniscus
Increased debris in the tear film
Superficial punctate keratopathy
Tear film breakup time (BUT)
Looks at stability of the tear film
Measure the average time for the first small hole to appear in the tear film when the fluorescent stained cornea is viewed using a cobalt blue filter on a slit lamp
Abnormal if <10s
Schirmer test 1
Measures basal and reflex production
5x35mm Whatman no 41
5mm is placed on lateral third of lower lid
Left for 5mins
Normal is 15mm, abnormal <10mm, very abnormal <5 mm
Schirmer test 2 (perform if above is abnormal)
Measures basic secretion
Instill LA drops then dry with cotton tip applicator
Normal is 10mm, abnormal <5mm, <3mm is very abnormal.
Note: in ophthalmology literature, Schirmers 2 refers to a reflex secretion test o Perform by irritating the nasal mucosa with a cotton-tipped applicator prior to measuring tear production filter paper. Wetting <15 mm after 5 min is considered abnormal.
9.
Cheek aesthetics
malar hypoplasia – globe vector
relationship on lateral view between the anteriormost projection of the globe and the malar eminence.
Negative = angles posteriorly, indicates an absence of support for the lower lid.
Lip Teh
December 2005 the cheek mass should lie an average of 1.5 mm anterior to the cornea(positive vector)
superior sulcus deformity central/medial fullness – fatpad herniation lateral fullness – prolapse of lacrimal gland deepening – fat atrophy, orbital fracture, enucleation hypertrophy of orbicularis – patients who squint a lot
lower lid aging o orbital malar weakens – descend of malar fat pad o malar crescent – hollowing of infraorbital region and sagging cheek o increased distance between lower lid and check junction o nasolabial folds deepen
Tests for myasthenia gravis
edrophonium (Tensilon) test has remained the first-line test for diagnosis of
MG. The Tensilon test consists of injecting a small amount of the medication edrophonium intravenously. If the patient has MG the ocular muscle weakness, the ptosis, the general muscle weakness and/or nystagmus will improve dramatically for a short period of time.
acetylcholine receptor antibody titer (AChR Ab)
peek test – attempt to forcibly open closed eyes, fatigue results in one or both eyes opening, and the patient appears to “peek” at the examiner.
fatigue test - This consists of having the patient look at an object held up by the examiner in front of the patient. After a short period of time the eyelid(s) will droop in the person with ocular MG.
sleep test , which is based on the tendency for MG symptoms to improve following rest, may be especially useful in cases where a Tensilon test is technically difficult. This may be used in small children, patients with poor veins, or allergy or sensitivity to anticholinesterase drugs such as Tensilon.
morning/evening comparison test is similar in concept to the sleep test. The
Lip Teh
December 2005 patient is photographed, and the ptosis and ocular motility are compared at different times during the day. Old photographs are very helpful to determine how long the patient has drooping the of the upper eyelids.
ice test is a simple test for ocular MG in patients who have ptosis. A surgical glove filled with ice is held against the droopy eyelid for several minutes. In ocular myasthenia the patient can open his/her eyelid normally for a short period of time after the ice is removed.