10.25 Patient Safety - Royal College of Nursing
advertisement

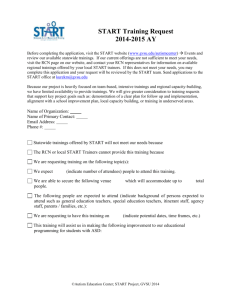
NPPC Meeting 23 June 2010 Agenda Item: 10/25 RCN Patient Safety Workstream 1. Purpose 1.1 To provide an overview of the RCN’s direction, workstream and deliverables on patient safety as a basis for endorsement and or revision by NPPC. Additionally, to identify gaps that needs to be addressed through task and finish groups. 2. Background 2.1 Patient Safety, along with clinical effectiveness and the patient experience is one of the three key components of quality in healthcare across the UK. High profile cases have served to focus, and to maintain attention on the role of safety in the provision of quality care underlining its importance. The President has championed patient safety at a European and U.K. level. The RCN is represented within national patient safety programmes and ongoing campaigns including the 1000 Lives plus in Wales, the Scottish Patient Safety alliance, the Patient Safety First campaign in England. Appendix 1 identifies the RCN links to external agencies. 2.2 The report from Mid-Staffordshire NHS Foundation Trust highlighted issues around organisational culture; the impact this can have on staffs’ ability to raise concerns effectively, and the effect it has on morale stating that the “lack of band seven nurses was a considerable risk that could result in poor standards of care” (CQC, 2009: 47) and that “there was a worrying deficit of senior nurses” (HCQ, 2009: 47). Furthermore the investigation revealed that “there had been little training and development of nurses…[and] the leadership of nurses had been poor” (CQC, 2009: 58). 2.3 Patient safety strategies in all four countries1 accentuate the link between quality, and productivity, together and emphasise the need to review, reorganise and evaluate ways of working and best use of resources so as to achieve increased outputs with better outcomes. 2.4 There is increasing interest across the UK in working locally to identify and address factors which may lead to the major failures in patient safety. However, the current economic climate raises serious concerns that any future change will be driven predominantly by the need to cut public sector spending which may have an adverse effect on nursing staff levels and skill mix leading to further potential compromises in the delivery of safe care to patients. 1 Department of Health (2006) Safety first: a report for patients, clinicians and healthcare managers. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_062848 Scottish Patient Safety Programme (2008) http://www.nhshealthquality.org/nhsqis/5191.html Welsh Assembly Government (2005) Designed for Life - a world class health service for Wales http://www.wales.nhs.uk/documents/designed-for-life-e.pdf Department of Health, Social Services and Public Safety (2006) The quality standards for health and social care http://www.skillsforhealth.org.uk/~/media/Resource-Library/PDF/qpi_quality_standards_for_health___social_care.ashx 1 NPPC Meeting 23 June 2010 Agenda Item: 10/25 RCN Background 2.5 2.6 The RCN argues that patient safety is embedded in all aspects of nursing practice and is an essential aspect of quality ( See NPPC June 2010 Quality Update linking quality to safety). . The RCN has had a clear and consistent voice on patient safety since the successful campaigns around needle stick injuries (2001; 2008); followed by the ‘Wipe it Out’ campaign (2005); and ‘Nutrition Now’ (2008).These campaigns, have been well received by members and parliamentarians alike, have provided a focal point for activity and key messages on infection prevention and patient safety in order to support both RCN members and patients in the delivery of safe care. 2.7 Work on safety culture and context has focused on the development and testing of The Safety Climate Assessment Tool (SCAT) which has been used with a number of acute and mental health organisations as well as residential homes to assess their safety climate. This tool, recently endorsed by European Union Network for Patient Safety2 provided baseline data pre and post workbased learning initiatives with practitioners in the RCN’s Derby Project and also evaluation of projects through RCN practice development and leadership programmes. 2.8. The public facing patient safety resource was launched last May. The website and the patient safety area on the Learning Zone have been viewed 8,428 and 9,166 times respectively between May 2009 and May 2010. 2.9. Recently the RCN has established a Quality, Standards and Innovation unit within the Learning & Development Institute to enable the co-ordination of all RCN activity around quality, standards and innovation around 8 workstreams monitored through the Quality Steering Group and in turn accountable to NPPC (Figure 1). 2 European Union Network for Patient Safety (2010) Use of patient safety culture instruments and recommendations. http://90plan.ovh.net/~extranetn/images/EUNetPaS_Publications/eunetpas-report-use-of-psci-and-recommandations-april-8-2010.pdf 2 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Figure 1: RCN Work Streams 1. Standards, guidelines & evidence 2. Measuring nursing quality 5. 6. Incentives and Board Reporting Accreditation 2.10 3. Implementing & Improving 4. Patient safety 7. Innovation in Practice 8. Integrated on-line resources The RCN’s quality and safety work is framed by UK-wide nursing practice principles, developed by the RCN and shortly to be launched across the UK, supported by all key UK stakeholders (Appendix 2). These principles make explicit what can be expected of nursing in any setting regardless of who the provider of care is. The principle specifically addressing patient safety is: “Nurses and nursing staff manage risk, are vigilant and help to keep everyone safe in the health care setting.” This principle provides the basis for developing key messages about patient safety and ways of measuring nursing care. 2.11. Following discussion at the previous NPPC a paper outlining current patient safety work being undertaken within the RCN was requested. The work of the patient safety workstream is now described with current challenges and areas for development identified. 3. Detail Patient safety workstream 3.1. The purpose and objectives of the workstream are outlined in Box 1. The workstream brings together all activity around patient safety consistent with the QSI unit’s role as a knowledge broker, bringing together key stakeholders across the UK with the expertise of members and staff to this end. This includes collating and appraising evidence around a small number of focused projects to support the RCN’s operational plan and strategic and policy priorities. There is also a key role in signposting resources for both members and staff. 3.2. The QSI unit provides an explicit public face and profile to the RCN’s quality and standards work including patient safety. However, to achieve its purpose 3 NPPC Meeting 23 June 2010 Agenda Item: 10/25 will require integrated working across many areas of the RCN so that the workstream can both benefit from and inform the work of others. Box 1 : Purpose & objectives of the Patient Safety Workstream Purpose To coordinate RCN-wide patient safety activity and intelligence so as to; support RCN members to provide safe care to patients enable the RCN to influence the patient safety context and policy Objectives: Help strengthen the nursing voice around patient safety so that patients receive safe care Develop relevant resources for nurses to implement and evaluate patient safety Gather and analyse data and intelligence around the safety context e.g. Raising Concerns, Raising Standards initiative 3.3. Specific projects planned for 2010-2011 bring together work undertaken by a number of RCN Departments and include an ongoing focus on cultural and contextual assessment; health care infections; nutrition; needle stick injuries; the measurement agenda around a number of practice focused projects and resources for members: Culture and Context: Evaluation and review of Safety Climate Assessment tool and its future MISSCARE Tool project brief being developed for approval by the Quality Steering Group (Appendix 3 describes the framework for this tool to illustrate how it could provide information around factors influencing patient safety outcomes). Development and rollout of a cascade system to the RCN’s Quality Improvement Network and RCN nursing forums to facilitate more effective feedback from members Campaigns: Wipe it Out: Health Care infection. The objective of the campaign, is currently undergoing a transitional period to enhance engagement and awareness of members and is the key focal point for communicating and gaining a greater awareness of issues that impact on the ability of staff to provide safe care. Needle stick campaign. A European Directive on the Prevention of Sharps injuries in the hospital and healthcare sector was published on 1st June 2010. Member states have three years to transpose this into national legislation. The Directive requires employers to carry out risk assessments and put measures in place to prevent injuries including the provision of safer needle devices and a ban on recapping. The RCN was a key player in the development of the European framework agreement 4 NPPC Meeting 23 June 2010 Agenda Item: 10/25 on sharps injuries (which led to the formation of the Directive) by providing both technical and negotiating expertise to the discussions. The RCN is working with key stakeholders to ensure transposition is effective. Nutrition Now Campaign; resources from this campaign are being placed on the RCNs website where they will continue to be updated. The RCN is currently working with the CQC to develop an observation tool for regulators to use in judging whether nutrition and hydration outcomes are being met. Measurement and Intelligence collection: Data gathering and intelligence around patient safety captured through the Raising Concerns Raising Standards database which builds on the analysis of Ombudsmen reports UK-wide. The measurement workstream includes a number of patient safety related projects being undertaken across the RCN, led by different teams e.g. the project promoting venous thromboembolism prophylaxis (Appendix 4). Integration and Implementation: Developing better integration of patient safety activity with activist support, the role of RCN Safety representatives; leadership and learning and development programmes; regional and country-wide activity, is being achieved through country-wide mapping against the QSI workstreams, and through the West Midlands Project led by Geraldine Cunningham and Tom Sandford. Resources for Members: RCN patient safety web pages launched at Congress 2009 Infection prevention and control website launched at Congress 2010 Patient safety stories to be launched summer 2010 Launch of a range of resources linked with quality and safety including staffing and skill mix during 2010-2011. 3.4 The patient safety workstream is closely linked to the measurement workstream which aims to co-ordinate, develop and refine a programme of measurement, data capture and audit in relation to nursing standards and patient safety, in collaboration with key internal and external stakeholders. 3.5 Inter-departmental collaboration is the basis for delivering all the quality and patient safety workstreams. RCN Safety Representatives are a key resource to patient safety work. Leadership of projects therefore varies according to the topic and focus, drawing on the RCN’s wealth of expertise. This can be illustrated in relation to: Infection prevention and control - led by Nursing Department and involving L&D Institute with the measurement agenda Pressure ulcers and tissue viability which is integrating a range of projects involving different departments -Nursing Department, Policy Unit and L&D Institute. Submission of evidence and representation on the advisory board to the Boorman review into health and wellbeing of the NHS workforce; leadership courses and competences. This involved Employment Relations Department and the L&D Institute. The final report made an implicit connection between patient safety and staff health and wellbeing. ERD ops plan around improving the nurses’ working environment 5 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Leadership and management - focusing on how executive nurses influence Trust Boards on quality and patient safety led by the Nursing Department and supported by the L&D Institute. 3.6 The RCN’s infection prevention network includes both members and nonmembers including those affiliated with external organisations. This provides informal but valuable opportunities for networking and collaboration on projects providing feedback from different perspectives. 3.7 The key nursing issues arising from this agenda relate to how the RCN can: 3.8 Other areas for development in patient safety activity relate to: 3.9 4. ensure that nursing is a key driver in maximising the relationship between the safety and the quality agenda maximise the nursing voice in future developments and decisions about patient safety support and develop nursing staff through the development, implementation and evaluation of a range of resources and tools aimed at learning around patient safety. support the role of executive, advanced and specialist nurses in improving the quality and safety of patient care strengthen the message that the quality and safety of patient care fundamentally requires agreed staffing levels and skill mix support members to identify and manage risk impact of nurse attitudes and behaviours in relation to safety; ways the RCN can actively involve patients and the public in determining the future patient safety and quality agenda; an emphasis in the Mid-Staffordshire investigation report around nurse’s lack of observation skills, low knowledge around ability to read cardiac monitors and failure to recognise deterioration further improving collaborative working between RCN Department’s on patient safety Developing a set of clear messages around patient safety Next steps relate to strengthening the patient safety workstream with a number of projects that address the areas for development identified above guided by NPPC’s discussion around this paper. Resources, costs and implications 4.1 The cost of co-ordinating the patient safety workstream and a number of small projects related to the RCNs operational plan is included in the L&D Institute budget. Other related projects feeding into the workstream are funded by other RCN departments or through the Forum bidding process. 5. Risks 6 NPPC Meeting 23 June 2010 Agenda Item: 10/25 5.1 Reputational risk may arise from the perception that the RCN is not actively pursuing an explicit programme of work about an issue of critical importance to the public, practitioners and policy makers. 6. Diversity 6.1 Diversity and equality issues are considered within projects and workstreams 7. UK-wide/Four country perspective 7.1 This work is UK wide and includes consideration of specific country specific perspectives as appropriate 8. Strategic plan 8.1 This workstream supports strategic objective 3.5 that the RCN “be recognised as a leading authority on the setting of professional standards and accreditation.” 9. Recommendations NPPC is asked to: Endorse the objectives and focus of the patient safety and related measurement workstreams Identify areas where a task and finish group needs to be established June 2010 Originators: Geraldine Cunningham; Kim Manley; Linda Watterson Input from: Geraldine Cunningham; Kim Manley; Rose Gallagher; Kim Sunley; Josie Irwin; Ross Scrivener; Martin Semple; Rita Devlin Clare Mayo. Linked information: June 2010 Quality Update to NPPC References Care Quality Commission (2009) Investigation into Mid-Staffordshire NHS Foundation Trust. London. CQC. 7 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Appendix 1 Person (alphabetical Order) Maura Buchanan Rita Devlin Ron Elvins Rose Gallagher Jenny Gordon Kim Manley Clare Mayo Mathew Rice/Dee Holbrook Martin Semple Sophie Staniszeweska Kim Sunley Linda Watterson Role in relation to patient safety External Links President National Patient Safety Forum Royal Colleges Northern Ireland Safety Forum RCN Northern Ireland Quality and Patient Link Representing & Influencing Link with RCN Safety Reps Learning and Development RCN Advisor Infection Control Links to Nursing Department Advisors Workstream lead: Standards, evidence and guidelines Quality and Standards Lead for RCN RCN Scotland Quality and Patient Link Enhancing Practice & Influencing- links to RCN Consultancy and leadership/quality programmes European network for Infection prevention and control NPSA Quality lead RCN Wales Strategic Alliance Warwick Patient Public Engagement Research Patient Safety ERD Lead Patient Safety and Measurement Workstreams 1000 Lives Plus campaign NICE, SIGN HQIP, CQC, Scottish Patient Safety Programme Scottish Patient Safety Alliance NPSA CQC 8 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Appendix 2 Eight principles of nursing practice The principles of nursing practice tell us what ALL people can expect from nursing practice, be they colleagues, patients, their families or carers. Nursing is provided by nursing staff, be they ward managers (in hospitals) or team members (in the community), specialist nurses, community nurses, health care assistants or student nurses. or, more simply... The principles of nursing practice describe what EVERYONE can expect from nursing. Stem statement: Nurses and nursing staff… Principle A - treat everyone in their care with dignity and humanity, understanding their individual needs, showing compassion and sensitivity, and caring in a way that respects all people equally. Principle B - take responsibility for the care they provide, answering for their own judgments and actions, and performing these in a way that is expected of them by patients, their families and carers, and required of them by their professional bodies and the law. Principle C - manage risk, are vigilant and help to keep everyone safe in the health care setting. Principle D - provide and promote care that is person centred, involving patients, users, their families and carers in decisions and helping them make informed choices about their treatment and care. Principle E - are pivotal communicators: they assess, record and report on treatment and care; they handle information sensitively and confidentially; they deal effectively with complaints; and they report conscientiously the things they are concerned about. Principle F - have up to date knowledge and skills, and use these with intelligence, insight and understanding according to the needs of each individual in their care. Principle G - work closely with their own team and other professionals, ensuring patients’ experience of care and treatment is seamless, of a high standard and has the best possible outcome. Principle H - lead by example, developing themselves and other staff, and influencing the way care is given in a manner that is open and responds to individual needs. 9 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Appendix 3 10 NPPC Meeting 23 June 2010 Agenda Item: 10/25 Appendix 4 11