乳房X光攝影影像判讀的標準化報告系統
advertisement

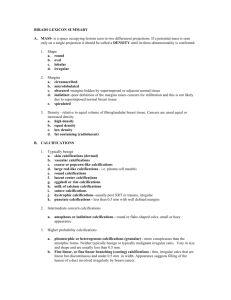
乳房 X 光攝影影像判讀的標準化報告系統 目的:為了避免錯誤解讀乳房攝影的檢查結果,使用標準化的報告格式、詞彙、 分類與建議處置,可讓臨床醫師充分瞭解報告內容與含意,做出適當的決策。此 外影像檢查不具專一性,良性與惡性腫瘤可出現相似的表徵,為了提高診斷率並 減少偽陽性對篩檢婦女的傷害,標準化報告系統可作為判讀醫師執行醫學評量的 基礎。 方法: 一、乳房 X 光攝影標準化報告格式。 1. 基本資料: 姓名、病歷號、年齡或出生年月日、檢查日期 2. 檢查名稱: 兩側或單側檢查、篩檢或診斷式乳房 X 光攝影 3. 報告內容: 是否比較舊片,乳腺緻密度分類(詳見二.),異常發現(有)(無), 建議使用統一的詞彙 (詳見三.) 4. 分類與建議處置: (詳見四.) 5. 判讀醫師: 姓名、專科醫師證書字號 二、乳腺緻密度(BREAST COMPOSITION) 1. The breast is almost entirely fat (<25% glandular). 2. There are scattered fibroglandular densities (approximately 25%-50% glandular). 3. The breast tissue is heterogeneously dense, which could obscure detection of small masses (approximately 51%-75% glandular). 4. The breast tissue is extremely dense. This may lower the sensitivity of mammography (>75% glandular). 三、報告內容所使用的統一詞彙。 A. MASSES A “MASS” is a space-occupying lesion seen in two different projections. If a potential mass is seen in only a single projection it should be called an “ASYMMETRY” until its three-dimensionality is confirmed. 1. SHAPE a. Round A mass that is spherical, ball-shaped, circular or globular in shape. b. Oval A mass that is elliptical or egg-shaped. c. Lobular A mass that has an undulating contour. d. Irregular The lesion’s shape cannot be characterized by any of the above. 2. MARGIN ( Modifies the shape of the mass ) a. Circumscribed (Well-Defined or Sharply-Defined) Margin The margin is sharply demarcated (at least 75% of the margin must be well defined, with the remainder no worse than obscured by overlying tissue, for a mass to qualify as “circumscribed“) with an abrupt transition between the lesion and the surrounding tissue. Without additional modifiers there is nothing to suggest infiltration. A mass, where any portion of the border is indistinct or spiculated should be classified on the basis of the latter. b. Microlobulated The short cycles of the margin produces small undulations. c. Obscured A margin that is hidden by superimposed or adjacent normal tissue. This is used when interpreting physician believes that the mass is circumscribed, but the margin is hidden. d. Indistinct (Ill-Defined) Margin The poor definition of the margin or any portion of the margin raises concern that there may be infiltration by the lesion and this appearance is not likely due to superimposed normal breast tissue. e. Spiculated Margin The lesion is characterized by lines radiating from the margin of a mass. 3. Density This is used to define the x-ray attenuation of the lesion relative to the expected attenuation of an equal volume of fiborglandular breast tissue. It is important that most breast cancers that form a visible mass are of equal or higher density than an equal volume of fibroglandular breast tissue. It is rare (although not impossible) for breast cancer to be lower in density. Breast cancers are never fat-containing (radiolucent) although they may trap fat. a. High-Density b. Equal Density (Isodense) c. Low Density, but not fat-containing d. Fat-Containing Radiolucent This includes all lesions containing fat such as an oil cyst, lipoma or galactocele as well as mixed lesions such as the hamartoma or fiboradenolipoma. Since specificity is lower than sensitivity, it is important to stress the benign nature of mammographic features when possible. A fat-containing mass will overwhelmingly represent a benign mass. B. CALCIFICATIONS Calcifications that can be identified as benign on mammography are typically larger, coarser, round with smooth margins and more easily seen than malignant calcifications. Calcifications associated with malignancy (and many benign calcifications as well) are usually very small and often require the use of a magnifying glass to be seen well. When a specific etiology cannot be given, a description of calcifications should include their morphology and distribution. Calcifications that are obviously benign need not always be reported. However, they should be reported if the interpreting physician is concerned that other observers might misinterpret them. When vascular calcifications are noted, especially in women under 50 years of age there are data to suggest potential risk of coronary artery disease (2-3). 1. Typically benign a. Skin Calcifications These are usually lucent-centered and often pathognomonic in their appearance. Skin calcifications are most commonly seen along the inframammary fold parasternally, axilla and areola. Unusual forms may be confirmed as skin deposits by performing mammographic views tangential to the overlying skin. b. Vascular Calcifications Parallel tracks, or linear calcifications that are clearly associated with tubular structures. c. Coarse or “Popcorn-like” Calcifications These are the classic large (>2-3 mm in diameter) calcifications produced by an involuting fibroadenoma. d. Large Rod-like Calcifications These benign calcifications associated with ductal ectasia may form solid or discontinuous smooth linear rods, usually ≥ 1 mm in diameter. They can have lucent centers if the calcium is in the wall of the duct and will generally be solid when secretions calcify in the lumen of ecstatic ducts. These follow a ductal distribution, radiating toward the nipple, and occasionally branching, and they are usually bilateral. Secretory calcifications are usually seen in women older than 60 years. e. Round Calcifications When multiple, they may vary in size. They can be considered benign when scattered. When small (< 1 mm), they frequently are formed in the acini of lobules. When smaller than 0.5 mm, the term “punctate” can be used. An isolated cluster of punctate calcifications may warrant close surveillance or even biopsy if new or ipsilateral to a cancer, though further study is warranted. f. Lucent-Centered Calcifications These are benign calcifications that a centimeter or more. These deposits are round or oval, with smooth surfaces and have a lucent center. The “wall” that is created is thicker than the “rim” or “eggshell” type of calcifications. lncluded are areas of fat necrosis and calcified debris in ducts. g. “Eggshell” or “Rim” Calcifications These are very thin benign calcifications that appear as calcium deposited on the surface of a sphere. These deposits are usually smaller than 1 mm in thickness when viewed on edge. Fat necrosis and calcifications in the wall of cysts are the most common “rim” calcifications. h. Milk of Calcium Calcifications This is a manifestation of sedimented calcifications in macro or microcysts. On the craniocaudal image they are often less evident and appear as fuzzy, round, amorphous deposits, while on the 90° lateral, they are more clearly defined, semilunar, crescent shaped, curvilinear (concave up) or linear defining the dependent portion of cysts. The most important feature of these calcifications is the apparent change in shape of the calcific particles on different mammographic projections (craniocaudal versus oblique or 90° lateral). i. Suture Calcifications These represent calcium deposited on suture material. They are typically linear or tubular in appearance and when present, knots are frequently visible. j. Dystrophic Calcifications These usually form in then irradiated breast or in the breast following trauma. Although irregular in shape, they are coarse and usually larger than 0.5 mm in size. They often have lucent centers. 2. Intermediate concern, suspicious calcifications a. Amorphous or Indistinct Calcifications These are sufficiently small or hazy in appearance that a more specific morphologic classification cannot be determined, Diffuse scattered amorphous calcifications can usually be dismissed as benign although baseline magnification views may be helpful. Amorphous calcifications in a clustered, regional, linear or segmental distribution may warrant biopsy. b. Coarse Heterogeneous Calcifications These are irregular, conspicuous calcifications that are generally larger than 0.5mm and tend to coalesce but are not the size of irregular dystrophic calcifications. They may be associated with malignancy but can be present in areas of fibrosis, fibroadenomas or trauma representing evolving dystrophic calcifications. 3. Higher probability malignancy a. Fine Pleomorphic Calcifications These are usually more conspicuous than the amorphic forms and are neither typically benign nor typically malignant irregular calcifications. They vary in sizes and shapes that are usually smaller than 0.5 mm in diameter. b. Fine Linear of Fine-Linear Branching Calcifications These are thin, linear or curvilinear irregular calcifications, which may be discontinuous and smaller than 0.5 mm in width. Their appearance suggests filling of the lumen of a duct involved irregularly by breast cancer. 4. Distribution modifiers These are used to describe the arrangement of calcifications in the breast. Multiple similar groups may be indicated in the report when there is more than one group of calcifications that are similar in morphology and distribution. a. Diffuse / Scattered These are calcifications that are distributed randomly throughout the breast. Punctate and amorphous calcifications in this distribution are usually benign and usually bilateral. b. Regional These are calcifications scattered in a large volume (> 2 cc) of breast tissue not conforming to a duct distribution. Since this distribution may involve most of a quadrant or more than a single quadrant, malignancy is less likely. However, evaluation must include element shape as well as distribution. c. Grouped or Clustered Should be used when at least five calcifications occupy a small volume (< 1 cc) of tissue. d. Linear Calcifications arrayed in a line. This distribution may elevate suspicion for malignancy as it suggests deposits in a duct. e. Segmental Calcifications in a segmental distribution are worrisome in that they suggest deposits in a duct or ducts and their branches raise the possibility of extensive or multifocal breast cancer in a lobe or segmental calcifications exist (e.g., secretory calcifications), the smooth, rod-like morphology and large size of individual calcifications can help distinguish benign calcification from finer, more irregular malignant calcifications. A segmental distribution may elevate suspicion for calcifications such as round (punctuate) or amorphous forms. C. ARCHITECTURAL DISTORTION The normal architecture is distorted with no definite mass visible. This includes thin lines or spiculations radiating from a point and focal retraction or distortion of the edge of the parenchyma. Architectural distortion can also be associated with a mass, asymmetry or calcifications. In the absence of appropriate history of trauma or surgery, architectural distortion is suspicious for malignancy or radial scar and biopsy is appropriate. D. SPECIAL CASES 1. Asymmetric tubular structure / solitary dilated duct This is a tubular or branching structure that that likely represents a dilated or otherwise enlarged duct. If unassociated with other suspicious clinical or mammographic findings, it is usually of minor significance. 2. Intramammary lymph node Intramammary lymph nodes are typically reniform or have a radiolucent notch due to fat at the hilum and are generally 1 cm or smaller in size. They may be larger than 1 cm and identified as normal when fat replacement is pronounced. They may be multiple, or marked fat replacement may cause a single lymph node to look like several rounded masses. This specific diagnosis is reserved for masses, usually in the lateral and upper portions of the breast, although they may occur anywhere in the breast. 3. Global asymmetry Asymmetric breast tissue is judged relative to the corresponding area in the contralateral breast and represents a greater volume of breast tissue over a significant portion of the breast. There is no mass, distorted architecture or associated suspicious calcifications. Global asymmetric breast tissue usually represents a normal variation, but may be significant when it corresponds to a palpable abnormality. 4. Focal asymmetry This is a finding that does not fit criteria of a mass. It is visible as a confined asymmetry with a similar shape on two views, but completely lacking borders and the conspicuity of a true mass. It could represent an island of normal breast tissue, particularly when there is interspersed fat, but its lack of specific benign characteristics may warrant further evaluation. E. ASSOCIATED FINDINGS Used with masses. Asymmetries, or calcifications or may stand alone as FINDINGS when no other abnormality is present. 1. Skin retraction The skin is pulled in abnormally. 2. Nipple retraction The nipple is pulled in or inverted. This is often bilateral and when stable and chronic in the absence of any other suspicious findings is not a sign of malignancy. 3. Skin thickening This may be focal or diffuse and larger than 2 mm. 4. Trabecular thickening This is a thickening of the fibrous septa of the breast. 5. Skin lesion Commented on when it projects over the breast in two views and may be mistaken for an intramammary lesion. These should be marked by the technologist with a radiopaque marker and recorded on patient worksheet. 6. Axillary adenopathy Enlarged (>2cm), non-fatty replaced axillary lymph nodes mat warrant comment, clinical correlation and additional evaluation if new. 7. Architectural distortion As an ASSOCIATED FINDING it can be used in conjunction with a finding to indicate that the normal tissue structure is distorted or retracted adjacent to the FINDINGS. 8. Calcifications As an ASSOCIATED FINDING, it can be used in conjunction with a FINDING to describe calcifications within or immediately adjacent to the finding. F. 描述病灶位置(location):如:外上象限(upper outer quadrant or UOQ);內 上象限(upper inner quadrant or UIQ);外下象限(lower outer quadrant or LOQ);內下象限(lower inner quadrant or LIQ),亦可使用鐘面描述病灶位 置如:三點鐘方向距離乳頭三公分。 四、分類與建議處置 Assessment Categories a. Mammography Assessment Is Complete Category 0 Need Additional Imaging Evaluation and/or Prior Mammograms For Comparison: Finding for which additional imaging evaluation is needed. This is almost always used in a screening situation. Under certain circumstances this category may be used after a full mammographic work-up. A recommendation for additional imaging evaluation may include, but is not limited to the use of spot compression, magnification, special mammographic views and ultrasound. Whenever possible, if the study is not negative and does not contain a typically benign finding, the current examination should be compared to previous studies. The radiologist should use judgment on how vigorously to attempt obtaining previous studies. Category 0 should only be used for old film comparison when such comparison is required to make a final assessment. b. Mammographic Assessment Is Complete-Final Categories Category 1 Negative: There is nothing to comment on. The breasts are symmetric and no masses, architectural distortion or suspicious calcifications are present. Category 2 Benign Finding(s): Like Category 1, this is a “normal” assessment, but here, the interpreter chooses to describe a benign finding in the mammography report. Involuting, calcified fibroadenomas, multiple secretory calcifications, fat-containing lesions such as oil cysts, lipomas, galactoceles and mixed-density hamartomas all have characteristically benign appearances, and may be labeled with confidence. The interpreter may also choose to describe intramammary lymph nodes, vascular calcifications, implants or architectural distortion clearly related to prior surgery while still concluding that there is no mammographic evidence of malignancy. Note that both Category 1 and Category 2 assessments indicate that there is no mammographic evidence of malignancy. The difference is that Category 2 should be used when describing one or more specific benign mammographic findings in the report, whereas Category 1 should be used when no such findings are described. Category 3 Probably Benign Finding-Initial Short-Interval Follow-Up Suggested: A finding placed in this category should have less than a 2% risk of malignancy. It is not expected to change over the follow-up interval, but the radiologist would prefer to establish its stability. There are several prospective clinical studies demonstrating the safety and efficacy of initial short-term follow-up for specific mammographic findings. Three specific findings are described as being probably benign (the noncalcified circumscribed solid mass, the focal asymmetry and the cluster of round﹝punctate﹞calcifications; the latter is anecdotally considered by some radiologists to be an absolutely benign feature). All the published studies emphasize the need to conduct a complete diagnostic imaging evaluation before making a probably benign (Category 3) assessment; hence it is inadvisable to render such an assessment when interpreting a screening examination. Also, all the published studies exclude palpable lesions, so the use of a probably benign assessment for a palpable lesion is not supported by scientific data. Finally, evidence from all the published studies indicate the need for probably benign findings increase in size or extent. While the vast majority of findings in this category will be managed with an initial short-term follow-up (6 months) examination followed by additional examinations until longer-term (2 years or longer) stability is demonstrated, there may be occasions where biopsy is done (patient wishes or clinical concerns). Category 4 Suspicious Abnormality-Biopsy Should Be Considered: This category is reserved for findings that do not have the classic appearance of malignancy but have a wide range of probability of malignancy that is greater than those in Category 3. Thus, most recommendations of breast interventional procedures will be placed within this category. By subdividing Category 4 into 4A, 4B and 4C as suggested in the guidance chapter, it is encouraged that relevant probabilities for malignancy be indicated within this category so the patient and her physician can make an informed decision on the ultimate course of action. Category 5 Highly Suggestive of Malignancy-Appropriate Action Should Be Taken:(Almost certainly malignant) These lesions have a high probability (≥95%) of being cancer. This category contains lesions for which one-stage surgical treatment could be considered without preliminary biopsy. However, current oncologic management may require percutaneous tissue sampling as, for example, when sentinel node imaging is included in surgical treatment or when neoadjuvant chemotherapy is administered at the outset. Category 6 Known Biopsy-Proven Malignancy-Appropriate Action Should Be Taken: This category is reserved for lesions identified on the imaging study with biopsy proof of malignancy prior to definitive therapy.