Foundation Handbook 2014 V1 - Surrey and Sussex Healthcare
advertisement

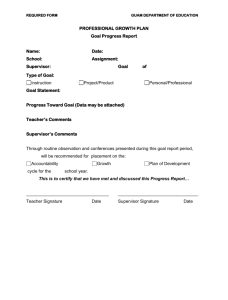
The Surrey and Sussex Foundation Training Programme Handbook In association with The Postgraduate Deanery for Kent, Surrey and Sussex A Guide for Trainees and Staff August 2014 Welcome to the Surrey and Sussex Foundation Training Programme. We hope you enjoy your time here. We have compiled this handbook to help orientate you at the start of the programme and guide you during your time here. This handbook contains useful information for staff and work colleagues who may come into contact with you (as a foundation programme trainee) during your time here This handbook has been divided into the following sections: Section The Foundation Training Programme Your Education E Learning Modules Your Educational Supervisor: their role Your Clinical Supervisor: their role Your Role Your Employment Steps to success in the foundation years If you need help… Key Contacts List of Appendices Page 2 7 8 10 10 11 12 13 14 15 16 There is a lot of information in this handbook. You should read it before your first day on the training programme and prepare any questions early on so that these can be addressed before you begin. If you have any other queries during your time at Surrey and Sussex, please do not hesitate to ask any member of the foundation training programme team (see section on Key Contacts) Again, we hope you enjoy your time at Surrey and Sussex. Dr Sarah Rafferty, Director of Medical Education Dr Sunil Zachariah-FY1 Programme Director Dr Hina Gandhi & Dr Sushil Niraula-FY2 Programme Directors Surrey and Sussex Foundation Training Programme Leads THE FOUNDATION TRAINING PROGRAMME Programme aims The Surrey and Sussex Foundation Training Programme (SASFTP) has been designed to provide comprehensive education and training for doctors in the early stages of their medical career. As a SASFTP trainee, you will be part of a structured programme which not only focuses on helping you gain the competences necessary to successfully complete the programme but also provides you with education and training tailored to your individual needs. The aims of the programme are to help you: Consolidate and develop your clinical skills, particularly in acute medicine so that you can identify and manage sick patients in whatever setting they present (including adult and paediatric settings). Embed modern professional attitudes and behaviours in every aspect of your clinical practice. Demonstrate your acquisition of these competences through our reliable and robust system of assessment and participate in annual ARCP process. Explore a range of career opportunities in different settings and in different areas of medicine. 2 Programme structure, trainee supervision and support The SASFTP consists of 30 F1 and 30 F2 individual foundation programmes. Each individual programme is made up of three 4-month placements in specialties offering a wide range of training experiences and opportunities (these are shown in appendix 1). During each 4 month placement you will be allocated a clinical supervisor who will monitor your progress during your placement. At the start of the programme, you will also be allocated an educational supervisor who will monitor your progress throughout the year. Further details regarding clinical and educational supervisors are contained later in this handbook. If you desire, you will also be assigned a mentor who will support you in a variety of ways. Your mentor may be someone who you want to discuss professional issues or issues that are troubling you. They may also advise you about issues such as your career or even act as a role model. If you are an F1 trainee, your mentor will be from the F2 year. If you are an F2 trainee, your mentor will be an SHO or Registrar from a speciality of your choice. You will be assigned a mentor within a few weeks of starting the programme. If you need further advice in regards to your career you can approach Trust career adviser. We also have Speciality Champions if you need any help or advice in regards to career advice in any speciality. As a part of Clinical Leadership role we encourage all the trainees to participate in a Leadership project. You should discuss this with you supervisor or the Trust Lead for clinical leadership, Miss Jean Arokiasamy. The learning portfolio As a foundation programme trainee, you will have an E-learning portfolio which must be kept up-to-date as a record of your training whilst on the programme. This is a key document and must be read prior to starting the foundation programme. Your learning portfolio contains a number of key documents. It is essential that you read these documents and familiarise yourself with the portfolio as a whole as this will help you plan your time here so that you successfully complete the programme which will then allow you to progress in your career. Please note that it is your responsibility to organise and update your portfolio and ensure that all appraisals and assessments are carried out and entered into this document. The assessment process Assessment is a key feature of the SASFTP. By assessing you at different intervals and by using a variety of assessment methods, your clinical and educational supervisors will gain a clear indication of your progress throughout the programme. The results of these assessments will also be considered when assessing whether you have completed the programme successfully. During the SASFTP, you will be assessed using the following supervised learning events (SLEs) descriptions: Team Assessment Behaviour (TAB) Direct Observation of Doctor-Patient Interaction: Mini Clinical Evaluation Exercise (mini-CEX) and Direct Observation of Procedural Skills (DOPS) Case-Based Discussion (CBD). Developing the Clinical Teacher F2 SLE Team Assessment Behaviour (TAB) This assessment method uses the views of a number of people with whom you have had contact to gauge your abilities, your strengths and your weaknesses. As a SASFTP trainee, you must nominate 8 ‘raters’ (who could be supervising consultants, GP principals, specialist registrars or experienced nursing or allied health professional (AHP) colleagues) who will then complete the necessary assessment forms, the results of which will then be collated and then fed back to you. You should complete two TABS during each foundation year, you should also complete yourself assessment. Direct Observation of Doctor-Patient Interaction Two methods have been devised to assess your interactions with patients: The Mini Clinical Evaluation Exercise (mini-CEX) and the Direct Observation of Procedural Skills (DOPS) 3 Mini Clinical Evaluation Exercise (mini-CEX) This assessment method involves an observer (who may be a consultant, GP principal or experienced SpR) observing your performance during a clinical encounter with a patient after which you will be given feedback on your performance. Each mini-CEX should represent a different clinical problem and should fall into one of the ‘acute care scenario’ conditions listed in appendix 2. It is your responsibility to choose the clinical encounter which you want observed, the timing of the encounter and who you want as your observer. Direct Observation of Procedural Skills (DOPS) This is an example of another assessment method where you will be observed during a clinical encounter, but in this instance, this will involve the performance of a practical procedure. Each DOPS should represent a different acute care skill (these are also listed in appendix 2) and again you should choose the time, the procedure to be observed and the observer for each encounter (observers may be consultants, GPs, SpRs, suitable nurses or allied health professionals. You should choose a different observer for each encounter). It has been agreed by the Executive Committee and cleared with the Deanery and Foundation School that all F1 and F2 trainees must undertake DOPS assessments in the following subjects within the first three months of them starting the Trust, i.e. by the end of October 2013. The subjects are: Blood culture (peripheral) IV Cannulation Urethral Catheterisation (male or female) Case Based Discussion (CBD) This assessment is based on a structured discussion which will take place between you and your clinical supervisor about a case which you have managed. This will allow your supervisor to assess your decision making and clinical reasoning skills. You should ensure that you take part in a minimum 6 CBDs per year. You will be expected to coordinate all of the above assessments yourself so that by the end of your foundation year you will have completed the required number and types of assessments. The information gained from these assessments will form the basis for your final or end of year review. As a foundation programme trainee, you have a key role in organising and carrying out the assessments which take place. A sample schedule for the timing of assessments in the foundation years is shown in appendix 2. You will be expected to have done 2 CbDs, 2 mini-CEX & 1 DOPS during your first four months to support your application for further training. Leadership Effective clinical leadership is essential for good patient care and leadership is now part of the curriculum for foundation as well as all core and higher specialty training. In response to this, STFS is piloting the addition of a formative, specific leadership skills assessment form to the foundation ePortfolio. This form - LEADER – Clinical Leadership for Work-based Assessment - is now available in the foundation ePortfolio. It can be found under ‘Forms > Work-Based Assessments > Add New Assessment’ within a trainee’s account (in the same way that you would access a CbD, DOPS or Mini-CEX) and can be ticketed by the trainee. A blank version of the form is available from ‘Home > Help > Blank Forms’. Please see below guidance for foundation doctors and for educational supervisors on completing this assessment which includes suggestions of leadership activities which foundation doctors could undertake. Quality Management Processes All Foundation trainees are expected to engage with quality management processes and any other activities that contribute to the quality improvement of training e.g. by completing the on-line GMC Trainee Survey and STFS training survey. 4 FY1- Core procedures What are core procedures? Core procedures are those 15 procedures set by the General Medical Council (GMC) for foundation year 1 (F1). The GMC requires demonstration of competence in all 15 procedures in order for provisionally registered doctors with a licence to practise to be eligible for full registration. Further information on this can be found via the GMC website: http://www.gmcuk.org/Outcomes_to_be_demonstrated_by_provisionally_registered_doctors_F1.pdf_26990221.pdf How does it work? It is a requirement that foundation doctors provide evidence that they can satisfactorily perform each of the 15 procedures at least once during F1. Satisfactory completion should be recorded within the e-portfolio. It is vital that patient confidentiality is maintained and patient identifiable details are not included when recording these procedures. The foundation doctor must record and should be able to competently perform and teach undergraduates the following 15 procedures: Venepuncture IV Cannulation Prepare and administer IV medication and injections and fluids Arterial puncture in an adult Blood culture (peripheral) IV infusion including the prescription of fluids IV infusion of blood and blood products Injection of local anaesthetic to skin Subcutaneous injection Intramuscular injection Perform and interpret an ECG Perform and interpret peak flow Urethral catheterisation (male) Urethral catheterisation (female) Airway care including simple adjuncts. What must foundation doctors demonstrate for satisfactory completion? There are both generic requirements and specific procedure requirements for each procedure. Employers will also typically have protocols for the safe performance of each procedure. The generic requirements are: introduce themselves check the patient’s identity confirm that the procedure is required explain the procedure to the patient (including possible complications and risks) and gain informed consent for the procedure (under direct supervision where appropriate) 5 take all necessary steps to reduce the risk of infection, including washing hands, wearing gloves and maintaining a sterile field if appropriate dispose of all equipment in the appropriate receptacles document the procedure in the notes; and arrange appropriate aftercare/monitoring. REMEMBER: it is vital that foundation doctors recognise the limits of their competence and seek advice and help where appropriate. Assessments Frequency E-portfolio Contemporaneous Core procedures Throughout F1 Team assessment of behaviour (TAB) Once in first placement in both F1 and F2, optional repetition Clinical supervisor end of placement report Once per placement Educational supervisor end of placement report Once per placement Educational Supervisor’s End of Year Report Once per year Completing the programme We hope that during your time on the SASFTP, you will use the varied training experiences and numerous educational opportunities available to you to ensure the successful completion of the programme. At the end of the programme, you should have gained a wide range of generic skills, and skills in the management of acutely ill patients which will then prepare you for your future career in either vocational training for General Practice or specialist training for Hospital Practice. If you successfully complete all parts of the foundation programme, you will receive the following: Certificate of Experience for PRHOs – This will be signed at the end of the F1 year by your University /Foundation School F2 Achievement of Competence Document (FACD) – This will be signed off at the end of F2 if you complete the F2 year satisfactorily as guided by ARCP process. Feedback We are always keen to receive feedback on the quality of the training and education we provide as this will help us to develop the SASFTP in the future. If you have any comments or suggestions relating to the SASFTP, please contact your educational supervisor. 6 BLOOD COMPETENCIES All FY1 and FY2 doctors joining the Trust need to be assessed as satisfactory on the following competencies in order to be involved in the process of blood transfusion o Obtaining and sending off a blood sample for G&S or X match o Receiving and administering blood products These competencies are valid for 3 years when they will need to be repeated and are transferable to other Trusts. The assessments are co-ordinated by Dr Fiona J Lamb (Fiona.lamb@sash.nhs.uk). Attend a lecture on blood transfusion which is usually incorporated in the Induction Day timetable. Alternatively it can be attended on one of the Trust’s education afternoons. Certificates of these competencies from other Trusts may be accepted after these have been presented for review to Dr Lamb. YOUR EDUCATION Education which is provided during the SASFTP is embedded in clinical practice. This means that the majority of education and training will take place whilst working in your clinical teams and providing clinical care for patients in Surrey and Sussex. Education and training in the clinical setting As a SASFTP trainee, you will be working in a multi-professional clinical team alongside other doctors, nurses and allied health professionals as well as other healthcare workers in providing clinical services for patients across Surrey and Sussex. Working within these teams, you will be able to closely observe other professionals at work and see them using both generic and acute care skills on a daily basis. The staff will also supervise you as your knowledge and skills develop. It is vital that you use the experience gained in these clinical settings to its maximum potential. Techniques which may help you gain the maximum educational benefit from seeing and treating patients include reflecting on your experiences at work and keeping a ‘reflective diary’. This can help you keep note of specific cases you see and incidents which take place which can then act as learning opportunities. It is also useful if you use your professional relationships with your colleagues to learn vital generic and acute care skills. Again this may be by observing your colleagues during their clinical practice or by asking colleagues about the principles which underpin their clinical practice. Using educational resources As well as the numerous training experiences and learning opportunities which you will be exposed to whilst working in your specific clinical teams, you will be able to supplement your learning by making use of a variety of educational resources at your disposal. These include courses run by the various organisations involved in the SASFTP. Details of these courses are available on the intranet sites of the various organisations. Examples of these are listed in appendix 3. Some of these courses are considered essential (or ‘statutory’ or ‘mandatory’). You should seriously consider attending these courses whilst on the SASFTP. Details of other courses and meetings (both internal and external) are available in the postgraduate education centres (PGEC) at East Surrey and on staff training and education noticeboards which you may find in individual departments when working in your 4-month placements. The PGEC also host regular clinical meetings, life support courses and teaching for vocational trainees which you may also attend (please see section on study leave on page 11). The East Surrey Hospital Medical Library is also an invaluable resource. It has a superb range of educational resources which you can access both in office hours and out of hours. These include a wide range of books and periodicals covering a wide range of subjects. The staffs in the medical library are extremely helpful and will help you access resources which are not available at either site through the system of interlibrary loans. East Surrey 7 Hospital Library also has a learning resource centre (with access to the internet and medical databases such as MEDLINE), audio-visual facilities and CD-ROM, a local historical collection and subscriptions to over 200 current journals. It is vital that you make use of these resources during your time here. You will be expected to have made excellent use of your educational time whilst on the programme. Your use of this time will be monitored and so you must keep a personal log of educational activities completed during each post. These will then be reviewed by your educational supervisor at your appraisal. The SASFTP formal educational programme in generic professional training The formal educational programme for foundation trainees has been designed to cover all aspects of good medical practice, patient safety and accountability through clinical governance. This programme starts with an induction which will help introduce you to some key aspects of patient care before starting work in your placement. FY2- Teaching will alternate between Tuesdays and Thursdays once a month from 8.30-5pm, FY1 Teaching -Tuesday lunchtimes from 12-1pm. Please note that these teaching sessions are compulsory. You must attend unless you are on annual, study, sick or special leave or if you have worked the night shift before the session or are due to work the night shift after. Attendance registers will be kept and will be reviewed by your educational supervisor. Provisional timetables are shown in appendix 4 and 5. Please inform your Foundation Programme administrator if you are unable to attend. A minimum of 70% attendance is required for sign off; there are a number of additional teaching opportunities available for you to attend, within each specialty. The sessions on this programme will not only be lecture based but will also give you the opportunity to put some of the principles of good medical practice into action using interactive group discussions and scenario based teaching. Please note, in addition to this formal programme, you will receive a specialty specific induction prior to each placement which will provide you with the basic knowledge and skills necessary to provide care for the patients you see during the placement. E-learning modules There are varieties of e-learning modules available on the internet for you to supplement your curriculum based teaching and learning opportunities, evidence of these modules should be recorded on your e-portfolio. You can access the e-LFH modules through the curriculum on your e-portfolio; the Programme Directors have produced the following lists of suggested modules- 1.1 FY1 Professionalism Behaviour in the workplace 2.2 2.5 Relationship and communication with patients Communication with patients Consent 3.0 Safety and clinical governance Safety and clinical governance 7.5 Good clinical care Safe prescribing 8.0 Recognition and management of the acutely ill patient Recognition and management of the acutely ill patient 8 1.1 FY2 Professionalism Behaviour in the workplace 01_09(Stress-Bullying) 11_20(Equality & Diversity: General Awareness) 11_21(Equality & Diversity: General Awareness Assessment) 2.5 Relationship and communication with patients Consent 11_03(Mental Capacity) 11_04(Mental Capacity Assessment) 3.2 Safety and clinical governance Quality & safety improvement 07_03(Quality and safety in the NHS) 4.0 Ethical and legal issues 11_06(DVLA) *This is not an exhaustive list, and you should complete the modules that you feel will benefit and supplement your training* Simulation All FY1 and FY2 trainees will be released from clinical duties to attend a mandatory Simulation training day. Community Placements-FY1 FY1-ITU 1 FY1 in ITU will be in a community palliative care posting (2 weeks posting) from September 16-27th, January 2031st and May 19-30th. During these 2 weeks posting the other ITU FY1 is not allowed to take leave. The second FY1 in ITU will be in community paediatrics posting (2 weeks posting) from September 30-Oct 11th, February 3-14th and June 2-13th. During these 2 weeks the other ITU FY1 will not be allowed leave. FY1-Vascular 1 FY1 in Vascular Surgery will be in community palliative care posting (2 weeks) from September 16-27, 2013 and January 20-31st 2014 and May 19-30th, 2014. During these 2 weeks the other FY1 in vascular surgery will not be allowed to take leave. The second FY1in Vascular surgery will be in community paediatrics posting from October 14-25th, 2013, February 17-28th, 2014 and June 16-27th, 2014. Respectively the other FY1 cannot take leave during that time. As a mandatory part of your foundation training you must register on the National Patient Safety Agency (NPSA) educational website (web address: http://www.npsa.nhs.uk/health/resources/ipsel). The educational material offered here is an integral part of the programme and will form part of your learning portfolio (please see section on study leave on page 11). As a foundation trainee, you will be expected to play an active role in your education. You will be expected to prepare presentations which may be case, teaching, audit or research presentations or clinical topic reviews and journal article reviews. This will help consolidate the learning which has taken place in the clinical setting and other settings. 9 YOUR EDUCATIONAL SUPERVISOR: THEIR ROLE At the beginning of your foundation training programme, you will be assigned an Educational Supervisor for the year. Your Educational Supervisor will conduct your appraisals throughout the year, will guide you during your time on the programme and will monitor your progress from an educational point of view. At your appraisal meetings, you will be able to discuss your strengths and your educational needs and your educational supervisor will be able to work with you to decide how you can best fulfil those needs and achieve your objectives. They will also discuss areas of concern with you so that potential difficulties or problems can be addressed early on during your year. To get the maximum benefit from your appraisals, you must ensure that your E-learning portfolio is up to date and includes all the necessary documentation required for your appraisal. Your educational supervisor may need access to your E-learning portfolio up to 2 weeks before your appraisal so that the contents of your portfolio can be reviewed and inform the appraisal process. If you have any comments or concerns about any aspect of your education whilst in the foundation programme, you should contact your educational supervisor as soon as possible. If you have any difficulties with your educational supervisor, you should contact your appropriate foundation programme director through the foundation programme administrator. YOUR CLINICAL SUPERVISOR: THEIR ROLE During your time on the foundation programme, you will rotate through three different specialties each year to gain experience in a variety of clinical settings. In each of these placements, you will be allocated a clinical supervisor. Your clinical supervisors will in most cases, be the consultant of the clinical team to which you are assigned. Their role will be to supervise you during your time in their specialty, monitor your work during your time there and advise you on any specialty specific areas relating to your post. They will also have a key role in performing your assessments whilst you are working in their clinical team. If you have any comments or concerns about your placement, you should contact your clinical supervisor as soon as possible. If you have any comments or concerns about your clinical supervisor, you should contact your educational supervisor (or the appropriate foundation programme director if your clinical supervisor is also your educational supervisor). 10 YOUR ROLE As a foundation programme trainee, it is essential that you play an active part in the programme and take an active role in your education – Remember; you will only get as much out of the foundation programme as you put in! Therefore you have a responsibility to ensure that you get as much out of your time in the programme as possible. To ensure that your time is as productive as possible you must: Meet with your educational supervisor and arrange your appraisals - It is important that you meet with educational supervisor (ideally within the first 2 weeks of starting your first placement) to discuss your educational needs and how you are going to achieve them. It is your responsibility to liaise with your educational supervisor to arrange a date and time for your appraisal. It is also your responsibility to ensure that all the necessary documentation has been completed /collated prior to your appraisal and that your educational supervisor has this well in advance of each meeting. In addition to completing your E-learning portfolio, please ensure that you have completed the self-appraisal tool in your E-learning portfolio. The information contained in these forms will be used as a basis for discussion during your appraisal. Take control of your education! – Of course we can’t force you to do this but we strongly believe that you should use your time on the SASFTP to the max! This will mean that you get the most out of it and will be more likely to complete the foundation programme successfully. We are keen for you to direct your own education and learning. Therefore, use the educational opportunities and resources available during your time here (It may not be available in your next job so, use it or lose it!). If there is something you really want to learn, speak to your educational supervisor and they will try and arrange something for you (If you don’t ask, you don’t get!). And lastly, we want you to play an active part in your own education. As we have said, you only get out what you put in! Coordinate your assessments well in advance – The assessments are a key component of the foundation programme as they will decide if you complete the programme successfully or not. It is your responsibility to arrange and coordinate these assessments. Make sure you do this well in advance and arrange these with your clinical supervisors as soon as possible. Remember, failure to complete all your assessments means that you will not successfully complete the programme. The following section contains a summary of what you need to do as a foundation trainee to ensure that you progress within the programme and increase your chances of successfully completing the programme. 11 YOUR EMPLOYMENT During your time here, you will be employed and paid by Surrey and Sussex Healthcare for the whole of your programme including the period in general practice. You will be paid on the pay scale according to your previous service, either in the UK or overseas, and will receive the banding for each leg of the rotation which is appropriate to the rota that you are on. Consequently your banding may change from one specialty to another. Annual leave You will be entitled to 5 weeks and 2 days annual leave per year and you must give at least 6 weeks’ notice of your proposed leave. Doctors on internal rotations are expected to take their holiday entitlement in each leg. As this affects mainly FY1 and FY2 trainees’, entitlement for each leg would be 9 days. If you wish to take more or to carry leave over to the next leg this must be agreed with the General Manager of the attachment concerned. Study leave If you are an F1 trainee, you will have protected generic professional training on Tuesday afternoons. You will also be given time to attend an Immediate Life Support (ILS) course and an Acute Life-threatening Events Recognition and Treatment (ALERT) course. If you are an F2 trainee, you are entitled to a study leave allowance of 30 days per year. Your attendance at the Tuesday/Thursday monthly generic professional training is automatically counted against this allowance. You may use the remaining days to gain focussed experience (‘taster’ experience) in specialties outside your placement specialty as long as this has been agreed with your educational supervisor. You may also use this time to attend courses or other activities to acquire generic knowledge or skills necessary for you to successfully complete the SASFTP which you cannot otherwise gain on the programme. However, F2 doctors should only be granted study leave for additional courses once the following have been attended or shown clear intention to do so: a) b) c) d) ALS required for F2. ALS is a requirement for F2 sign-off. Demonstration of regular attendance at internal training sessions (>70% attendance during working shifts, excluding night shifts) Intention to attend simulation training Booked a taster week, or have good reason not to require a taster. F2 trainees should not be given study leave for private study for preparation for examinations. F2 trainees’ study leave allowance is the same as CT or ST trainees, however according to Deanery recommendations we subtract a proportional amount for funding of generic training, this leaves a sum of up to a maximum of £500. Again you should plan attendance at such courses with your educational supervisor well in advance and submit a completed study leave application form at least 6 weeks prior to the leave being taken. Retrospective applications and applications for study leave at short notice will not be granted. If you have any queries concerning your terms of employment please contact the medical staffing office on ext 6624 12 STEPS TO SUCCESS IN THE FOUNDATION YEARS Attend SASFTP induction, FY1-July and FY2-7th August 2013. Meet foundation programme team, Collect relevant documentation including SASFTP handbook and learning portfolio Meet Clinical Supervisor for first placement and attend specialty specific induction (if appropriate) Read and prepare documents in learning portfolio and arrange to meet your educational supervisor within 2 weeks of starting your placement. Complete relevant self-assessment forms. Ensure your educational supervisor has your learning portfolio up to 2 weeks prior to induction appraisal along with completed forms and including relevant documentation Register on the National Patient Safety Agency (NPSA) educational website (web address: http://www.npsa.nhs.uk/health/resources/ipsel) Prior to first appraisal think about your strengths and educational needs and how you think you can achieve them. Think about accessing the various educational resources and educational opportunities on offer. Bring this information to your first appraisal Devise timetable /action plan for each of the educational objectives identified in your personal development plan and ensure that they are achieved by mid-point appraisal or before. Complete study leave forms at least 6 weeks prior to course if planning to attend SASFTP or external course Devise timetable of assessments for MSF, mini-CEX /DOPS and CBD and liaise with your clinical supervisor to coordinate these. Select ‘raters’ and ‘observers’. Ensure appropriate documentation forwarded to SASFTP administrator Ensure maximum educational value is gained from each placement. Consider keeping a reflective diary. Attend all formal educational sessions. Keep e-portfolio update and complete for ARCP process At end of each placement, meet with clinical supervisor to obtain Certificate of Satisfactory Service Arrange meeting with educational supervisor for mid-point appraisal (usually 6 months into foundation year) to review progress and discuss any issues Continue progress to meet all educational objectives, complete all relevant assessments, gain maximum educational value from placements and educational activities outside placements. Keep up-to-date log of all educational activities Arrange meeting with educational supervisor to ensure all educational objectives are met and satisfactory progress has been made throughout foundation year Obtain Certificate of Experience for PRHOs (FI) or F2 Achievement of Competence Document (FACD) (F2) if all of the above achieved SUCCESSFUL COMPLETION OF FOUNDATION YEAR 13 IF YOU NEED HELP… Some foundation programme trainees may find this period of training difficult. This can be due to a number of reasons which can involve issues outside work, personal health related issues and also issues related to ability to perform and take part in the programme. If you are starting to struggle, this may make you feel like not wanting to take part in the programme or any extra educational activities or you may start to feel that you don’t want to carry out some of the essential parts of the programme such as the assessments. Feeling like this may also make you focus less on your job and this in turn can lead to incidents and complaints which in the worst case, may adversely affect patients. It may be that other people notice these changes in you before you do (i.e. colleagues, mentors, clinical supervisors, educational supervisors). If you realise that you are starting to feel like this, ask for help early! Your work colleague, peers, mentors, clinical and educational supervisors are all there to support you during your time here. Your educational supervisor in particular has a role in providing support to you as a SASFTP trainee and should be able to provide a supportive environment in which you can discuss any difficulties or concerns. In addition we have the support of Jane Armstrong who is available to all for confidential and impartial pastoral support: p.armstrong@talk21.com Your supervisors may also contact you if you show signs of stress and difficulty. Again this may manifest itself by a worsening of your assessment results or attendance record or an increase in incidents relating to you or in sickness absence. They will be keen to provide an opportunity for you to discuss your progress and provide any assistance which may help you to manage better in the future. Remember, all staff are here to help you as a SASFTP trainee, the earlier staff knows about problems, the sooner they can help deal with them. So please contact them early 14 KEY CONTACTS Role SASFTP Administrator FY1 SASFTP Administrator FY2 Director of Medical Education SASFTP director SASFTP lead (FY1) SASFTP lead (FY2) PGEC South Thames Foundation School (STFS) Contact details Victoria Bates Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231722 Fax: 01737 231723 E-mail; victoria.bates@sash.nhs.uk Caroline Pusey (Kari) Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231722 Fax: 01737 231723 E-mail: caroline.pusey@sash.nhs.uk Dr Sarah Rafferty Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231722 Fax: 01737 231723 E-mail: sarah.rafferty@sash.nhs.uk Dr Sunil Zachariah Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231761 Fax: 01737 231723 E-mail: sunil.zachariah@sash.nhs.uk Dr Hina Gandhi & Dr Sushil Niraula Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231722. Fax: 01737 231723 E-mail: hina.gandhi@sash.nhs.uk Email: sushil.niraula@sash.nhs.uk Tina Suttle-Smith Surrey and Sussex Healthcare NHS Trust East Surrey Hospital, Canada Avenue, Redhill, Surrey RH1 5RH Telephone: 01737 231722 Fax: 01737 231723 E-mail: tina.suttle-smith@sash.nhs.uk Website: www.stfs.org.uk FY1: 0208 725 5041 FY2: 01273 523357 15 LIST OF APPENDICES Appendix Page Appendix 1: SASFTP Individual Foundation Programmes (IFPs) FY1 & FY2 17 Appendix 2: Acute care scenarios and acute care skills for mini-CEX and DOPS assessments and sample assessment schedule for F1 and F2 years 19 Appendix 3: SASFTP Courses 22 Appendix 4: SASFTP Formal education programme in generic Professional training (Foundation Year 1) 23 Appendix 5: SASFTP Formal education programme in generic Professional training (Foundation Year 2) 24 Appendix 6: Requirements for satisfactory completion of F1 25 Appendix 7: Requirements for satisfactory completion of F2 27 16 Appendix 1: SASFTP Individual Foundation Programmes (IFPs) - FOUNDATION YEAR 1 Foundation School (Year 1) Foundation School rotation Number SASH First Name No. Surname Educational Supervisor South Thames 14/KSS/RTP04/F1/001 ES01 Anneka Rudra South Thames 14/KSS/RTP04/F1/002 ES02 Robert Goldsby-West Niraula South Thames 14/KSS/RTP04/F1/003 ES03 Nicola Oldman Prajapati South Thames 14/KSS/RTP04/F1/004 ES04 Lorena Chavez Pino CampbellSmith South Thames 14/KSS/RTP04/F1/005 ES05 Shyamal Patel Thorning South Thames 14/KSS/RTP04/F1/006 ES06 James Buxton Ferrigan South Thames 14/KSS/RTP04/F1/007 ES07 Natalie Blundell Nadjafi South Thames 14/KSS/RTP04/F1/008 ES08 Katharine Brockett Zachariah South Thames 14/KSS/RTP04/F1/009 ES09 Dana Ali Mackenzie South Thames 14/KSS/RTP04/F1/010 ES10 James Horn Stenner South Thames 14/KSS/RTP04/F1/011 ES11 Inji Wissa Ibrahim Abousleiman South Thames 14/KSS/RTP04/F1/012 ES12 Emily Thomas Field Monkhouse 06/8/14 - 02/12/14 (Clinical Supervisor) 03/12/14 - 31/3/15 (Clinical Supervisor) Saha GIM/Cardio Cetti GIM/Chest Prajapati CoE Phongsathorn CoE Monkhouse Surgery-Upper GI Campbell-Smith Surgery-Lower GI Iqbal GIM/Cardio Zacharia Abousleiman CoE Phongsathorn CoE Swinn Urology Campbell-Smith Surgery-Lower GI Allen GIM/Cardio Cetti GIM/Chest Prajapati CoE Phongsathorn GIM/Endocrin Mackenzie South Thames 14/KSS/RTP04/F1/013 ES13 Peter De Souza Waheed South Thames 14/KSS/RTP04/F1/014 ES14 Liam Robinson Makadsi South Thames 14/KSS/RTP04/F1/015 ES15 John Melville Desikan South Thames 14/KSS/RTP04/F1/016 ES16 Shane Wilde Morgan South Thames 14/KSS/RTP04/F1/017 ES17 Ahkallya Kuganolipava Swinn South Thames 14/KSS/RTP04/F1/018 ES18 Timothy Bagnall Loosemore South Thames 14/KSS/RTP04/F1/019 ES19 Daniel Christopher Thorning South Thames 14/KSS/RTP04/F1/020 ES20 Hina Nayee Cetti South Thames 14/KSS/RTP04/F1/021 ES21 Kaveesh Dissanayake Davies South Thames 14/KSS/RTP04/F1/022 ES22 Hooria Cheema Niraula South Thames 14/KSS/RTP04/F1/023 ES23 Lucy Wharton Smith South Thames 14/KSS/RTP04/F1/024 ES24 Keshika Vishnuthevan Shattles South Thames 14/KSS/RTP04/F1/025 ES25 Isobel Spring Zachariah South Thames 14/KSS/RTP04/F1/026 ES26 Ketan Champaneri Acharya South Thames 14/KSS/RTP04/F1/027 ES27 Krishna Sivakumaran B Mearns South Thames 14/KSS/RTP04/F1/028 ES28 Keval Patel Clark GIM/Gastro Stenner GIM/Gastro Abousleiman CoE Phongsathorn CoE 01/4/15 - 04/8/15 (Clinical Supervisor) Monkhouse Surgery-Upper GI Campbell-Smith Surgery-Lower GI Saha GIM/Cardio Cetti GIM/Chest Abousleiman CoE Phongsathorn CoE Swinn Urology Loosemore/Waheed SurgeryCoE Vascular/Breast(3) Desikan Loosemore/Waheed SurgeryCritical Care(1) Vascular/Breast Morgan James Critical Care(2) Surgery-Upper GI Monkhouse Allen Surgery-Upper GI GIM/Cardio Loosemore/Waheed Field SurgeryGIM/Endocrin Vascular/Breast(3) Niraula Shattles AMU GIM/Rheum Loosemore/Waheed SurgeryVascular/Breast(4) Powell James CoE(Capel) Surgery-Upper GI Bray Smith Critical Care(1) Surgery-Lower GI Morton Aslam Critical Care(2) Surgery-Lower GI Swinn Zachariah Urology GIM/Endocrin Loosemore/Waheed Saha SurgeryGIM/Cardio Vascular/Breast(3) Loosemore/Waheed Mackenzie SurgeryGIM/Gastro Vascular/Breast(4) James Stenner Surgery-Upper GI GIM/Gastro Davies GIM/Rheum Makadsi GIM/Rheum Smith Surgery-Lower GI Aslam Surgery-Lower GI) James Surgery-Upper GI Acharya GIM/Chest B.Mearns AMU Clark GIM (Diab/Endo) Powell CoE(Capel) Niraula AMU Davies GIM/Rheum Shattles GIM/Rheum Acharya GIM/Chest Mearns AMU James Surgery-Upper GI Prajapati CoE Aslam Surgery-Lower GI Clark Makadsi GIM/Rheum Mackenzie GIM/Gastro Stenner GIM/Gastro Prajapati Phongsathorn CoE Niraula AMU Powell CoE ( Capel) Smith Surgery-Lower GI Aslam Surgery-Lower GI Morgan Critical Care(1) Sage Critical Care(2) B.Mearns AMU James Surgery-Upper GI Acharya GIM/Chest Aslam Surgery-Lower GI Clark Prajapati GIM ( Diab/Endo) CoE Aslam Prajapati South Thames 14/KSS/RTP04/F1/029 ES30 Abiola Fatimilehin Ahmed Diab/Endo Surgery-Lower GI CoE (1)1 FY1 in ITU will be in community palliative care posting (2 weeks posting) from 15th-26th September, 19th-30th January 2015, 18-29th May 2015. During these 2 weeks posting the other ITU FY1 is not allowed to take leave. (2)The second FY1 in ITU will be in Paediatrics/General Practice posting (2 weeks posting) from 29th September-10th October, 2nd-13th February 2015, 1st-12th June 2015. During these 2 weeks the other ITU FY1 will not be allowed leave. (3)1 FY1 in vascular/breast surgery will be in community palliative care posting (2 weeks posting) from 29th September-10th October, 2nd-13th February 2015, 1st-12th June 2015. During these 2 weeks the other Fy1 in vascular surgery will not be allowed to take leave. (4)The second FY1 in vascular/breast surgery will be in Paediatrics/General Practice 17 posting (2 weeks posting) from 13th-24th October, 16th-27th February 2015, 15th-26th June 2015. Respectively the other FY1 cannot take leave during that time. In the last rotation April-August 2014, only one Vascular/breast FY1 will go to Community Palliative South Thames 14/KSS/RTP04/F1/029 ES29 Laura Crocker Prajapati Appendix 1: SASFTP Individual Foundation Programmes (IFPs) – FOUNDATION YEAR 2 Foundation School (Year 2) Foundation School rotation Num ber Given Nam e Surnam e Educational Supervisor South Thames 13/KSS/03/RTP04/01/F2/001 James Dusting Mr Veeramuthu South Thames 13/KSS/03/RTP04/01/F2/002 Kimmee Khan Mrs Gandhi South Thames 13/KSS/03/RTP04/01/F2/003 Chisom Emecheta Dr Dioszeghy South Thames 13/KSS/03/RTP04/01/F2/004 Gurveer Sagu Dr Pankhania South Thames 13/KSS/03/RTP04/02/F2/005 Amar Jessel Dr Nadjafi South Thames 13/KSS/03/RTP04/02/F2/006 Gregory Trilling Dr R Ahmed South Thames 13/KSS/03/RTP04/02/F2/007 Unmesh Bandyopadhyay Dr Katy Davies South Thames 13/KSS/03/RTP04/02/F2/008 Sanna-Noor Khan Dr Daneshmand South Thames 13/KSS/03/RTP04/02/F2/009 Thomas Koczlan Dr Prajapati South Thames South Thames 13/KSS/03/RTP04/02/F2/010 Charlotte Verrill Pettit 6/8/14-2/12/14 3/12/14-31/3/15 1/4/15 - 4/8//15 (Clinical Supervisor) (Clinical Supervisor) (Clinical Supervisor) Mr Veeramuthu Emergency Medicine Mrs Gandhi Obs & Gynae Dr Dioszeghy Emergency Medicine Dr Sercl Emergency Medicine Pramitkumar Patel General Practice Mr Selvan Trauma /Orthopaedics Chloe Miss Babar-Craig South Thames 13/KSS/03/RTP04/02/F2/012 Caroline Gosson Dr Makadsi South Thames 13/KSS/03/RTP04/02/F2/013 Josh King-Robson Dr Pankhania South Thames 13/KSS/03/RTP04/02/F2/014 Rachel Crane Dr Babu South Thames 13/KSS/03/RTP04/02/F2/015 Lucy Reeve Mrs Gandhi South Thames 13/KSS/03/RTP04/02/F2/016 Anna Duffy Dr Daneshmand South Thames 13KSS/03/RTP04/02/F2/017 Samantha Fernandes Dr Ali South Thames 13/KSS/03/RTP04/02/F2/018 Mohsin Asharia Dr Lew is South Thames 13/KSS/03/RTP04/02/F2/019 James Davis Dr Suleiman South Thames 13/KSS/03/RTP04/02/F2/020 Robert Adams Dr Dioszeghy South Thames 13/KSS/03/RTP04/02/F2/021 Christopher Peake Miss Babar-Craig South Thames 13/KSS/03/RTP04/02/F2/022 Rosalyn Haw kes Dr Niraula South Thames 13/KSS/03/RTP04/02/F2/023 Kate Markham Dr Webb South Thames 13KSS/03/RTP04/02/F2/024 Charlotte Young Dr Aggarw al South Thames 13/KSS/03/RTP04/02/F2/025 Rakesh Patel Dr Phongsathorn South Thames 13/KSS/03/RTP04/02/F2/026 Noel Murphy Dr Veerumuthu South Thames 13/KSS/03/RTP04/02/F2/027 Matthew Grant Dr Cow an South Thames 13/KSS/03/RTP04/02/F2/028 Holly Poppe Dr G Agarw al South Thames 13/KSS/03/RTP04/02/F2/029 Rathy Ramanathan Miss Wykes South Thames 13KSS/03/RTP04/02/F2/030 Andrew Badcock Dr Lew is 13KSS/03/RTP04/02/F2/031 Esha Aggarw al Miss Srivastrava South Thames 13KSS/03/RTP04/02/F2/032 Robert Gregory Dr Simon Parrington South Thames 13KSS/03/RTP04/02/F2/033 Richard Sennett Dr Katy Davies Mr Selvan Dr Daneshmand Trauma /Orthopaedics Emergency Medicine Dr Daneshmand Emergency Medicine Dr Prajapati G(I)M /Geriatrics Dr Prajapati G(I)M /Geriatrics Alan Clifford General Practice Rubey Dullo General Practice Dr Webb Emergency Medicine Dr Sercl Dr Makadsi Paul Spensley Emergency Medicine Elizabeth Moffett General Practice General Practice Dr Makadsi G(I)M - Rhemu Dr Makadsi G(I)M Dr Martin Emergency Medicine Nila Sathananthan G(I)M- Rhemu Mr Veeramuthu Emergency Medicine General Practice Mrs Gandhi Obs & Gynae Emergency Medicine Mr Bhat Trauma /Orthopaedics Dr Babu Psychiatry Dr Bucur Psychiatry Dr Daneshmand Emergency Medicine Rubey Dullo General Practice Dr Lew is Paediatrics Peter Morley Dr Dioszeghy Emergency Medicine Dr Daneshmand Emergency Medicine Dr Lew is Paediatrics Dr Sercl Emergency Medicine Gareth Bowen-Perkins General Practice Dr Sercl Miss Wykes Obs & Gynae Dr Lew is Paediatrics Michael Bosch General Practice Dr Lew is Paediatrics Dr Peter Martin Emergency Medicine Miss Waheed/Mr Ball South Thames 13KSS/03/RTP04/02/F2/034 Ayesha Memon Dr Fiona Lamb South Thames 13KSS/03/RTP04/02/F2/035 Gregory Horner Dr Simon Parrington South Thames 13KSS/03/RTP04/02/F2/036 Anna Coates Dr Laura Ferrigan Dr Dioszeghy General Practice Emergency Medicine Surgery Dr Dioszeghy Miss Waheed/Mr Ball Josie York Emergency Medicine Miss Waheed/Mr Ball Surgery Harminder Panesar General Practice Dr Sercl Surgery General Practice Emergency Medicine Gareth Bowen-Perkins Mr Veeramuthu B Mearns General Practice Emergency Medicine Acute Medicine (AMU) Dr Webb Dr Agarw al Asnita Drahaman Emergency Medicine Acute Medicine (MAU) General Practice Dr Agarw al / Asalieh Anny Gilani Dr Sercl Acute Medicine (AMU) General Practice Emergency Medicine Dr Phongsathorn Hana Patel Dr Peter Martin G(I)M /Geriatrics General Practice Emergency Medicine Mr Veeramuthu Dr Katy Davies Mr Selvan Emergency Medicine G(I)M /Geriatrics Trauma /Orthopaedics Hana Patel General Practice Mr Bhat Dr Daneshmand Emergency Medicine Dr Webb Dr Prajapati G(I)M /Geriatrics Mrs Gandhi Trauma/Orthopaedics Emergency Medicine 18 Obs & Gynae Miss Wykes Dr Babu Dr C Dioszeghy Obs & Gynae Psychiatry Emergency Medicine Dr Bucur Dr Daneshmand Paediatrics Psychiatry Emergency Medicine Miss Srivastrava Dr Katy Davies Dr Ranjan Obs & Gynae G(I)M /Geriatrics Dr Ravi Kumar Miss Srivastrava Dr Katy Davies ICU Obs & Gynae G(I)M /Geriatrics Dr Ranjan Miss Srivastrava Dr Katy Davies Wed AMU Wed- AMU G(I)M /Geriatrics Dr Katy Davies Dr Lew is South Thames Emergency Medicine Elizabeth Moffett General Practice Mr Veeramuthu Emergency Medicine Dr Babu Psychiatry Dr Bucur Psychiatry Dr Phongsathorn G(I)M /Geriatrics Dr Katy Davies G(I)M /Geriatrics Dr Niraula 13/KSS/03/RTP04/02/F2/011 Dr Phongsathorn G(I)M /Geriatrics Mr Selvan Trauma /Orthopaedics Miss Wykes Obs & Gynae Dr Lew is Paediatrics Dr Martin Emergency Medicine Dr Dioszeghy GPF2 trainee to w ork in ED/AMU 3 - 7 PM shift ICU G(I)M /Geriatrics ICU Obs & Gynae Miss Srivastrava Dr N Khan Dr Fiona Lamb Obs & Gynae G(I)M /Geriatrics Dr Ranjan Miss Srivastrava Dr N Khan ICU Obs & Gynae G(I)M /Geriatrics ICU Dr N Khan Dr Ravi Kumar Miss Srivastrava G(I)M /Geriatrics ICU Obs & Gynae Tues-ED Thurs-ED Thurs-AMU Tues-ED Wed-AMU Thurs-ED Thurs-ED Wed-ED Wed-ED Wed-ED Thurs-AMU Tues-AMU Tues-AMU Tues-ED Tues-AMU Thurs-AMU FOUNDATION YEAR 2 Appendix 2: Acute care scenarios and acute care skills for mini-CEX and DOPS assessments and sample assessment schedule for F1 and F2 years Acute Care Scenarios By the end of the F2 year, the foundation programme trainee should be able to recognise and demonstrate their understanding of the management of the following. Airway problems be able to recognise situations where the airway may be compromised o perform simple airway manoeuvres (with adjuncts) o know the indications for tracheal intubation be able to manage the core presentations of: o unconscious patient o anaphylaxis o stridor Breathing problems be able to assess breathing (rate, depth, symmetry, oxygen saturation) recognise that a high respiratory rate needs further evaluation be able to manage the core presentations of: o asthma o COPD o chest infection /pneumonia o pneumothorax o left ventricular failure o pulmonary embolism. Circulation problems be able to assess the circulation (heart rate, blood pressure, perfusion) know when a fluid challenge is required be able to manage the core presentations of : o bleeding o severe sepsis o tachyarrhythmias o bradyarrhythmias o volume and electrolyte depletion from diarrhoea/vomiting o hypotension in acute coronary syndromes o oliguria. Neurological problems in addition to the management of the unconscious patient (above), be able to manage the core presentations of: o collapse – ? cause o seizures o meningism o hypoglycaemia o acute onset of focal neurological signs. Continued over Psychiatric/behavioural problems demonstrate a basic understanding of the Mental Health Act 19 show awareness of situations where the safety of the patient, self or others may be at risk be able to manage the core presentations of: o overdose/other self harm o violence/aggression o substance abuse o delirium o acute confusional state or psychosis. Treating pain understand the analgesic ladder treat acute pain promptly, effectively and safely (using appropriate analgesia) understand that acute pain may present as a new event or in a setting of chronic pain e.g. palliative care patient be able to manage the core presentations of o chest pain o abdominal pain/acute abdomen o severe acute head injury o large joint pain o back pain o injuries. Acute Care Skills Procedures that F1 trainee should be competent and confident to perform: o venepuncture and IV cannulation o use of local anaesthetics o arterial puncture in an adult o blood cultures from peripheral and central sites o injection – subcutaneous, intradermal, intramuscular and intravenous o prepare and administer IV medications o intravenous infusions including the prescription of fluids, blood and blood products o perform and interpret an ECG o perform and interpret spirometry and peak flow o urethral catheterisation o airway care including simple adjuncts o nasogastric tube insertion. F2 Trainees During the F2 year, trainees are expected to maintain and improve their skills in the procedures listed above so that by the end of the F2 year they should be able to pass on their skills to others and assist others when procedures are difficult. There will also be opportunities for trainees to extend the range of practical procedures they can perform. Each specialty will specify a range of procedures relevant to that specialty in which the trainees will be expected to become proficient e.g., o aspiration of pleural fluid or air o skin suturing o lumbar puncture o insertion of a central venous pressure line o aspiration of joint effusion. 20 F1 4 8 8 CbD x 2 CbD x 2 CbD x 2 Mini – CEX X 2 Mini – CEX X 2 Mini – CEX X 2 DOPS X 4 MSF MSF (Option to repeat if concerns at the first MSF) F2 4 8 8 CbD x 2 CbD x 2 CbD x 2 Mini – CEX X 2 Mini – CEX X 2 Mini – CEX X 2 DOPS X 4 MSF MSF (Option to repeat if concerns at the first MSF) 21 Appendix 3: SASFTP Courses ORGANISATION Surrey and Sussex Healthcare NHS Trust* WEBPAGE http://web/hr/learningzone/default.htm Surrey and Borders Partnership NHS Trust Sussex Partnership Trust Surrey Primary Care Trust West Sussex Primary Care Trust Postgraduate Deanery for Kent, Surrey and Sussex http://www.sabp.nhs.uk/ COMMENTS Training courses available for all staff. List can be accessed from any SASH network computer http://nww.sussexpartnership.nhs.uk/ http://www.surreypct.nhs.uk/ http://www.westsussexpct.nhs.uk/ http://kssdeanery.ac.uk *Details of Statutory and Mandatory Training requirements for Medical and dental Staff at Surrey and Sussex Healthcare NHS Trust can be found on page 9 of the Trust Statutory and Mandatory Training Procedure available at: http://web/ed/staff/newstaff/Statutory%20and%20Mandatory%20Training%20Procedure.pdf 22 Appendix 4: Week Date Time Subject Speakers FY1 and FY2 Joint Teaching session 2014/2015 TUES TUES TUES TUES TUES TUES TUES TUES TUES TUES TUES TUES TUES 5th Aug 12th Aug 19th Aug 26th Aug 2nd Sept 9th Sept 16th Sept 23rd Sept 30th Sept 7th Oct 14th Oct 21st Oct 28th Oct 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm 1-2pm 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm e-portfolio and career planning How to Survive being an F1 IV Fluids Assessment & treatment of the breathless patient Appropriate use of antibiotics & Infection Control Initial assessment of patient on medical take Sepsis Pre-Operative Assessment Assessments of TIA'S Dr Pat Morgan Dr Fiona Lamb Dr Stuart Jones TUES TUES 4th Nov 11th Nov 1-2pm 12-1pm Leadership Arterial blood gas and non invasive ventilation TUES 18th Nov 12-1pm Pulmonary Embolism TUES 25th Nov 12-1pm COPD Assessment TUES 2nd Dec 12-1pm Suturing TUES TUES TUES TUES TUES 9th Dec 16th Dec 23rd Dec 30th Dec 6th Jan 1-2pm Miss Jean Dr Sushil Niraula Mr Muhammad Jawad Dr Cetti Mr Tim CampbellSmith Mr Alan James 12-1pm Post-operative fluid management TUES 13th Jan 1-2pm Assessment and Treatment of Shock TUES TUES 20th Jan 27th Jan 12-1pm 12-1pm TUES 3rd Feb 12-1pm Assessment and treatment of Diabetic Emergencies Acute Management of Status Epiepticus INTERIM ARCPs TUES 10th Feb 1-2pm Acute Renal Failure TUES TUES 17th Feb 24th Feb 12-1pm 12-1pm Stroke Prescribing - Pharmacy TUES 3th Mar 12-1pm GI bleeding assessment and management TUES TUES TUES TUES TUES TUES TUES 10th Mar 17th Mar 24th Mar 31st Mar 7th April 14th Apr 21st Apr 12-1pm 12-1pm 12-1pm 1-2pm 12-1pm 12-1pm 12-1pm Acute Eye Problems Assessment & treatment of acute chest pain Ethics as part of clinical practice X-Ray Dept Assessment and management of the painful/swollen limb Careers Session Blood transfusion/Approriate use of blood products TUES 28th Apr 12-1pm Stroke Thrombolysis TUES TUES TUES TUES TUES TUES TUES 5th May 12th May 19th May 26th May 2nd June 9th June 16th June 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm 12-1pm Cardiopulmonary resuscitation - a refresher Rheumatological emergencies ATLS-No Teaching TUES TUES TUES 23rd June 30th June 7th July 12-1pm 12-1pm 12-1pm Liverpool Care Pathway Joint Injections Skills of a GP & Professionalisam Insulin Types e-portfolio-WHO, WHAT & WHEN Mortality Review & Death Certification ATLS-No Teaching Assessment and management of the acute abdomen Christmas Meal Break Break Accident and Emergency: Assessment Painful, swollen joints Preparing for working in ED Endocrine emergencies 23 Mr Neil Smith Dr Natalie Powell TBC Dr Ed Cetti Dr Karen Knox Dr Asaleah Dr James Clark Dr Zachariah Dr Natalie Powell Dr Fiona Lamb Dr Gaurav Agarwal Dr Ben Field Dr Zhang Dr Zachariah Dr Caroline Ming(CMT) Dr Abousleiman Mead Ali Dr Gary Mackenzie Mr Umar Akbar Dr Ansuman Saha Naomi Collins Dr Sonia Biswas TBC Lisa Stone Simon Goodwin Dr Youssif Abousleiman Bernadette Lee Dr Makadsi Dr Julian Webb TBC Dr Webb Dr James Clark Dr Laura Kelly Dr Shattles GP Tutor TUES TUES 14th July 21st July 12-1pm Assessment and management of acute trauma 12-1pm Pain Control in Advanced Cancer **Please note that all dates and topics are subject to change** Mr Bhat Dr Laura Kelly Appendix 5: Week THUR Date 14/08 Time Subject 08.00-09.30 FY2 Teaching sessions August 2014 - January 2015 Welcome to Foundation Year 2 Planning your education and self directed learning and STFS Induction 09.30-10.30 SLASH course - PRACTICAL (Saving Lives Aseptic Skills for Healthcare) 10.30-11.30 ITU Management 11.30-13.00 Blood Competencies Using care pathways and care bundles: the sepsis care bundle 14.00-15.00 TUES THUR TUES THUR THUR 09/09 9/10 04/11 11/12 11/12 15.00-16.00 Safe prescribing and medication error, security issues in prescriptions, prescribing in special circumstances and adverse drug reactions 08.00-08.50 Leadership & Risk Management 08.50-09.40 Diabetes and Ketoacidosis Management 09.40-10.30 Evidenced based management of Ischaemic Heart Disease 10.30-11.20 Advanced ECG Interpretation Skills 11.20-12.10 Case Based Discussions - Respiratory 12.10-13.00 Infection Prevention Control and Antibiotic stewardship (IPCAS) LUNCH & CAREERS FAIR 13.50-14.40 Application Process 14.40-15.30 Careers Presentation BREAK 15.45-17.00 Mock Interviews 08.00-08.50 Use of CT 08.50-09.40 MRI Spiral Imaging 09.40-10.30 Advanced X-Ray interpretation 10.30-11.20 Ultrasound Techniques 11.30-12.30 Interpreting Blood Results & Arterial Blood Gases 13.50-14.40 TIA & Stroke 14.40-15.30 Making the best of the microbiology lab 15.30-16.20 Assessing the Psychiatric patient in Acute Medical setting(SABP) 16.20-17.10 Assessing the Psychiatric patient-Self Harming(SABP) 08.00-08.50 Basic Surgical Skills-PRACTICAL 08.50-09.40 CbD-General Surgery 09.40-10.30 Patient Safety: Oral anticoagulation and how to use it safely-Joint with FY1 10.30-11.20 ED-Assessment 11.20-12.10 Fluid and Electrolyte Management 13.00-13.50 Complaints Procedure 13.50-14.40 Communication and Professionalism 14.40-15.30 15.30-16.20 Ethics & Legal Issues Pain Control in Advanced Cancer 08.00-08.50 Management of Pleural Effusion 08.50-09.40 CbD-Orthopaedics 09.40-10.30 Post Mortem 10.30-11.20 Managing 3 way consultations with children and parents 11.20-12.10 CbD-Dermatology Quiz/Teaching 12.10-13.00 13.50-17.00 CbD-Cardiology Management of patients with disabilities 24 TUES 06/01 08.00-09.00 Central venous access & Inserting a central venous catheter-PRACTICAL 09.00-10.00 Chest Drains-PRACTICAL 10.15-11.15 CbD-Obs & Gynae 11.15-12.15 CbD-Rheumatology 12.15-13.15 14.15-15.15 Joint aspiration and injections-PRACTICAL CbD-CofE 15.15-16.15 Acute Oncology ***Please Note: All dates, timings and topics are subject to change. Subjects will be repeated Feb-July*** February 2015-July 2015 Thurs 5th Feb 2015 Tues 3rd March 2015 Thurs 14th April 2015 Tues 12th May 2015 Thurs 11th June 2015 Tues 7th July 2015 South Thames Foundation School Appendix 6: Requirements for satisfactory completion of F1 See UKFPO Reference Guide 2012, p 42-43, Section 10, Table 1 1 2 3 Requirement Notes Provisional registration and a licence to practise with the GMC Completion of 12 months of F1 training by August 2013 (taking account of allowable absence) The maximum permitted absence from training (other than annual leave) during the F1 year is 4-weeks. (See GMC guidance on sick leave for provisionally registered doctors). A satisfactory educational supervisor’s end of year report. Satisfactory educational supervisor’s end of placement reports. The report should draw upon all required evidence listed below. 5 Satisfactory clinical supervisor’s end of placement reports 6 atisfactory completion of the required number of assessments: If the F1 doctor has not satisfactorily completed one placement but has been making good progress in other respects, it may still be appropriate to confirm that the F1 doctor has met the requirements for satisfactory completion of F1. The last end of placement review must be satisfactory Continued over Team assessment of behaviour (TAB) 4 An educational supervisor’s end of placement report is not required for the last placement; the educational supervisor’s end of year report replaces this. (minimum of one per year). The minimum requirements are set out in the Curriculum. The Core procedures (all 15 GMC mandated procedures) 25 deanery/foundation school may set additional requirements. 7 8 9 A valid Immediate Life Support (ILS) or equivalent - certificate Evidence of participation in systems of quality assurance and quality improvement projects. Completion of the required number of Supervised Learning Events. The minimum requirements are set out in the Curriculum. The deanery/foundation school may set additional requirements If the certificate has expired, it may be appropriate to accept evidence that the doctor has booked to attend a refresher course. Foundation doctors should take part in systems of quality assurance and quality improvement in their clinical work and training. This includes completion of the national trainee survey and any end of placement surveys. Direct observation of doctor/patient interaction: • Mini CEX • DOPS (minimum of nine observations per year; at least six must be mini-CEX). Case-based discussion (CBD) (Minimum of six per year / two per placement) Developing the clinical teacher 10 An acceptable attendance record at generic foundation teaching sessions 11 Attendance at the appropriate level of Safeguarding Children training Attendance at an approved simulation course 12 (Minimum of one per year). It has been agreed that an acceptable attendance record should typically be 70%. However, if the F1 doctor has not attended 70% of teaching sessions for good reasons, it may still be appropriate to confirm that the F1 doctor has met the required standard e.g. making up missed sessions by completion of appropriate on-line learning modules. If there are concerns regarding engagement or if attendance is below 50%, the FTPD should discuss this with the STFS Director. STFS requirement STFS requirement 13 F1 – F2 Transfer of Information (TOI) form STFS requirement 14 Signed probity declarations This is in addition to the Declaration of Fitness to Practise required by the GMC when applying for full registration. 15 Leadership assessment and health All STFS F1 doctors are strongly encouraged to have completed a leadership assessment within the e-Portfolio (LEADER tool). Continued over 26 South Thames Foundation School Appendix 7: Requirements for satisfactory completion of F2 See UKFPO Reference Guide 2012, p 53-54, Section 11, Table 1 Requirement 1 2 3 Notes Full registration and a license to practice with the GMC Completion of 12 months of F2 training by August 2013 (taking account of allowable absence) A satisfactory educational supervisor’s end of year report. The maximum permitted absence from training (other than annual leave) during the F2 year is 4-weeks. The report should draw upon all required evidence listed below. 4 Satisfactory educational supervisor’s end of placement reports. An educational supervisor’s end of placement report is not required for the last placement; the educational supervisor’s end of year report replaces this. 5 Satisfactory clinical placement reports 6 Satisfactory completion of the required number of assessments: If the F2 doctor has not satisfactorily completed one placement but has been making good progress in other respects, it may still be appropriate to confirm that the F2 doctor has met the requirements for satisfactory completion of F2. The last end of placement review must be satisfactory. Team assessment of behavior (TAB) supervisor’s end of The minimum requirements are set out in the Curriculum. The deanery/foundation school may set additional requirements. 7 A valid Advanced Life Support (ALS) equivalent - certificate 8 Evidence of participation in systems of quality assurance and quality improvement projects. 9 Completion of the required Supervised Learning Events. number or of The minimum requirements are set out in the Curriculum. The deanery/foundation school may set additional requirements (minimum of one per year). Evidence that the foundation doctor can carry out the procedures required by the GMC. If the certificate has expired, it may be appropriate to accept evidence that the doctor has booked to attend a refresher course. Foundation doctors should take part in systems of quality assurance and quality improvement in their clinical work and training. The Curriculum requires that F2 doctors manage, analyse and present at least one quality improvement project (e.g. an audit) and use the results to improve patient care.F2 doctors are also required to complete the national trainee survey and any end of placement surveys. Direct observation of doctor/patient interaction: • Mini CEX • DOPS (minimum of nine observations per year; at least six must be mini-CEX). Case-based discussion (CBD) (Minimum of six per year / two per placement) Developing the clinical teacher(Minimum of one per year). Continued over 27 It has been agreed that an acceptable attendance record should typically be 70%. However, if the F1 doctor has not attended 70% of teaching sessions for good reasons, it may still be appropriate to confirm that the F1 doctor has met the required standard e.g. making up missed sessions by completion of appropriate on-line learning modules. If there are concerns regarding engagement or if attendance is below 50%, the FTPD should discuss this with the STFS Director. STFS requirement 10 An acceptable attendance record at generic foundation teaching sessions 11 Attendance at the appropriate Safeguarding Children training 12 F2 Destination Questionnaire Completion of the STFS questionnaire (separate guidance to follow) 13 Signed probity and health declarations A separate form should be signed for F2. 14 Leadership assessment All STFS F2 doctors are strongly encouraged to have completed a leadership assessment within the e-Portfolio (LEADER tool). level of 28