FDNS4500 Case Study: Stroke
advertisement

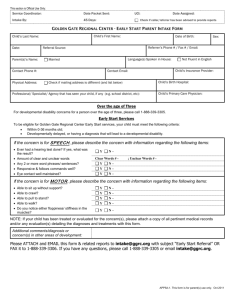
FDNS4500 Case Study #18: Stroke Emilie Koetter October 3, 2012 1. Define stroke. Describe the differences between ischemic and hemorrhagic stroke. A stroke occurs when blood supply to the brain is impeded or when a blood vessel in the brain bursts. Ischemic strokes are the most common type of stroke and are caused by the blockage of an artery to the brain, usually due to a blood clot or stenosis. This blockage causes a decrease or total stopping of blood flow to the brain which in turn leads to infarction (the death of brain cells due to lack of oxygen and nutrients). Hemorrhagic stroke occurs when an artery in the brain bursts and crosses the blood-brain barrier and disrupts the function of neurons. Hemorrhagic stroke can be caused by the bursting of an arterial wall or a weak spot within the wall of an artery (bleeding aneurysm). 3. What are the factors that place an individual at risk for stroke? Risk factors include age, gender, race/ethnicity, and stroke family history. • Risk for stroke increases with age • Men are more at risk for stroke than women, but more women die from stroke • African Americans are at higher risk for stroke The most significant risk factors are hypertension, heart disease, diabetes, and cigarette smoking. High total cholesterol as well as high LDL and low HDL cholesterol are also risk factors for stroke. High alcohol consumption will also increase risk. 4. What specific signs and symptoms that are noted with Mrs. Noland’s exam and history are consistent with her diagnosis? • hypertension and hyperlipidemia (high blood pressure, high total and LDL cholesterol, low HDL cholesterol) • heart problems • symptoms: dizziness, inability to talk, weakness of right side of body (arm and leg); • dysarthria with tongue deviation • motor function tone and strength diminished 6. Which symptoms that you identified in question 4 may place Mrs. Noland at nutritional risk? Explain your rationale. • dysarthria- causes dysphagia; may require enteral feeding route; can lead to inadequate intake • weakness- can lead to self-feeding difficulty and impaired ability to prepare foods/meals • diminished motor function- inability to access food and prepare meals; inability to feed self 7. Define dysphagia. Dysphagia: difficulty swallowing; can be caused by dysarthria (weakness or paralysis of the muscles of the mouth, tongue, larynx, or vocal cords as a result of a nerve, brain, or muscle disorder) One of the main causes of dysarthria is stroke. 15. Mrs. Noland’s usual body weight is approximately 165 lbs. Calculate and interpret her BMI. BMI= kg/m^2= 74.84 kg/ 2.48 m= 30.18; her BMI indicates that she is obese (class I) 16. Estimate Mrs. Noland’s energy and protein requirements. Should weight loss or weight gain be included in this estimation? What is your rationale? • EER for overweight and obese females 19+: • EER= TEE (kcal/day)= [448 - (7.95 x age) + PA x (11.4 x weight + 619 x height)] • TEE= 448- (7.95 x 77) + 1 x (11.4 x 74.84) + (619 x 2.48)= 2224.146= 2224 kcal/day • Weight loss is recommended for Mrs. Noland’s pre-existing conditions, as well as to prevent another stroke. Weight loss will help lower total serum cholesterol. To factor in weight loss, energy intake should be reduced by 500-1000 kcals per day as well as increasing energy expenditure. Mrs. Noland’s energy requirement for weight loss would be between 1224-1724 kcals/day. Increasing physical activity to increase energy expenditure is also recommended. Protein requirements: 1 FDNS4500 Case Study #18: Stroke • RDA= 0.8 g protein/ kg body weight= 0.8 x 74.84= 59.872= 60 g protein/day 17. Using Mrs. Noland’s usual dietary intake, calculate the total number of kilocalories she consumed as well as the energy distribution of kcals for protein, carbohydrate, and fat. • Total kcals= ~2,417 kcals • 99g protein= % kcals from protein= 16% • 360 g carbohydrate= % kcals from carbohydrate= 60% (too many refined grains, not enough whole grains) • % kcals from fat= 27% (25 g saturated fat) 18. Compare this to the recommended intake for an individual with hyperlipidemia and hypertension. Do these recommendations apply to Mrs. Noland at the present? When comparing Mrs. Noland’s usual intake to intakes recommended for individuals with hyperlipidemia and hypertension the most significant deviations are in sodium and fat intake. The DASH Diet for individuals with hypertension recommends an upper level intake of 2,300 mg sodium per day with 1,500 mg sodium per day being optimal for lowering blood pressure. Mrs. Noland’s current intake is approximately 3,900 mg of sodium per day. To lower serum cholesterol and triglycerides, Mrs. Noland should be consuming less fat, specifically saturated fat, less refined grains and more whole grains, and more fiber. Using her reported 24-hour dietary recall, her estimated average saturated fat intake is approximately 25 g per day. This value should optimally be less than 7% of her daily calories. Increasing her physical activity level would also promote weight loss, therefore helping to decrease blood pressure and blood lipid levels. In order to lose weight, Mrs. Noland must also reduce her overall energy intake by 500-1000 kcals per day below her recommended intake of 2,224 kcals/day. 19. Estimate Mrs. Noland’s fluid needs using the following methods: weight, age and weight; and energy needs. Slide on hydration status body weight: 1,500 + 20 mL/kg for each kg over 20 kg= 2596.8 mL fluid/day age and body weight: adult >65 yrs- 25 mL/kg= 1871 mL fluid/ day energy needs: 1 mL of fluid/ kcal= 2224 mL of fluid/ day 21. From the information gathered within the intake domain, list possible nutrition problems using the diagnostic term. • Excessive energy intake • Excessive fat intake • Less than optimal intake of types of fats • Excessive protein intake • Excessive carbohydrate intake • Excessive sodium intake 22. Review Mrs. Noland’s labs upon admission. Identify any that are abnormal. Using the following table, describe their clinical significance for Mrs. Noland. Chemistry Normal Value Mrs. Noland’s Value Reason for abnormality Transferrin 250-380 mg/dL 182 mg/dL May reflect illness or protein-energy malnutrition Inflammatory response Alkaline phosphatase 30-120 U/L 179 U/L diminished renal function special diet for treating liver function cholesterol 120-199 mg/dL 210 mg/dL high fat intake, genetic predisposition excessive fat intake, less than optimal intakes of types of fat 2 Nutritional Implications FDNS4500 Case Study #18: Stroke Chemistry Normal Value Mrs. Noland’s Value Reason for abnormality Nutritional Implications HDL-C >55 mg/dL 40 mg/dL low, below recommended level excessive fat intake, less than optimal intakes of types of fats LDL <130 mg/dL 155 mg/dL high, above recommended level excessive fat intake, especially saturated and trans fats TG 35-135 mg/dL 198 mg/dL high; above recommended level excessive fat intake, especially saturated and trans fats 23. From the information gathered within the clinical domain, list possible nutrition problems using the diagnostic term. • Swallowing difficulty • Obese Class I • Altered nutrition-related laboratory values (total serum cholesterol, HDL cholesterol, LDL cholesterol, triglycerides) 24. Select two high-priority nutrition problems and complete the PES statement for each. • on page 4 25. For each of the PES Statements that you have written, establish an ideal goal and an appropriate intervention. see attached pages 28. Describe Mrs. Noland’s potential nutritional problems upon discharge. What recommendations could you make to her husband to prevent each problem you identified? How would you monitor her progress? • Risks after discharge: • Weakness and fatigue may make cooking and food acquisition difficult. Mr. Noland may need to assist Mrs. Noland with feeding and food preparation. • Dysphagia may lead to inadequate energy intake. If Mr. Noland suspects inadequate intake or notices a change in Mrs. Noland’s diet, he must respond immediately to prevent malnutrition. • Because of the weakness and decrease in motor function, feeding may require addition time. Mr. Noland should ensure adequate time for Mrs. Noland to consume sufficient amounts of food and fluid. 3 FDNS4500 Case Study #18: Stroke Nutrition Assessment Nutrition Assessment Categories Food/Nutrition History Nutrition Assessment Data Diet about 2,400 kcal/day, good appetite Patient avoids fried foods, does not add salt at table High sodium intake, few whole grains, high fat and saturated fat intakes Multivitamin/mineral supplement daily, 500 mg calcium 3 x daily Meds: catopril 25 mg twice daily; levastatin 20 mg once daily Laboratory data Transferrin: 182 mg/dL Alk phos:179 U/L CHOL: 210 mg/dL HDL-C: 40 mg/dL LDL: 155 mg/dL TG: 198 mg/dL Anthropometric Measurements 5’2”, 165 #, BMI= 30.18 Physical Examination Client History Unable to speak or move right side; New-onset weakness of right side (arm and leg) Dysarthria with tongue deviation; cranial nerves III, V, VII, XII impaired Motor function tone and strength diminished BP: 138/88 mm Hg, HR: 91 bpm female, age 77 PMH: hypertension x 10 years; hyperlipidemia x 2 years; heart problems, arthritis, high blood pressure Family Hx: noncontributory Estimated energy and protein needs: ~2224 kcal/day, 60 g protein/day Nutrition Diagnosis (Note: this is not a medical diagnosis) Problem Obese Class I Etiology excessive energy intake (~200 kcal excess) Signs/Symptoms BMI of 30.18 as related to as evidenced by Problem Abnormal laboratory values as related to Etiology excessive fat intake as evidenced by Signs/Symptoms total serum cholesterol 210 mg/dL, HDL cholesterol 40 mg/dL, LDL cholesterol 155 mg/dL, triglycerides 198 mg/dL 4 FDNS4500 Case Study #18: Stroke Works Cited Nelms M, Sucher K, Lacey K, Roth S. Nutrition Therapy and Pathophysiology 2nd ed. California: Wadsworth, Cengage Learning, 2011. US Department of Agriculture. Food-A-Pedia. Version current 31 July 2012. Internet: https://www.supertracker.usda.gov/foodapedia.aspx (accessed 20 September 2012). US Department of Health and Human Services, National Institute of Health, National Heart, Lung, and Blood Institute. Your Guide to Lowering Your Blood Pressure With DASH. Version current April 2006. Internet: http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf (accessed 29 September 2012). 5