Dale Elleson

DALE ELLESON TEMPLATES – 6/14/06
D Elleson - H&P Exam & Impression
PHYSICAL EXAMINATION: This (age) -year-old (male/female) is
EYES:
EARS:
NOSE:
OROPHARYNX:
NECK:
LUNGS:
CARDIOVASCULAR:
ABDOMEN:
EXTREMITIES:
NEUROLOGIC:
IMPRESSION: well-nourished, well-developed, wellhydrated and in no acute distress.
The extraocular movements are intact.
Unremarkable.
Unremarkable.
Unremarkable.
No masses or adenopathy noted.
Clear to auscultation.
Normal sinus rhythm, without murmurs or extra heart sounds noted.
No masses, organomegaly or tenderness noted.
Full range of motion in all.
Grossly intact.
D Elleson – Past History
PAST HISTORY:
The patient's general health is described as excellent aside from the chief complaint. The patient takes no routine medications and has no known allergies to medications. There is no prior history of surgery. There is no history of bleeding disorders, diabetes, cardiac or pulmonary disease.
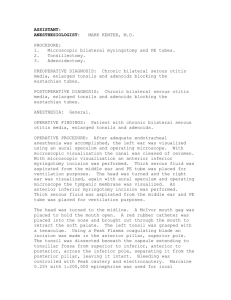
Elleson - Adenoidecomy
DETAILS OF PROCEDURE:
Under general anesthesia with orotracheal intubation, the nasopharynx was examined. A red rubber Robinson catheter was passed through the nose, exiting the mouth for gentle retraction of the soft palate. The nasopharynx could then be examined using the laryngeal mirror. The adenoids were noted to be markedly enlarged.
An adenoidectomy was performed using adenoid curets and a nasopharyngeal biopsy punch. A tonsil pack was placed in the nasopharynx for bleeding. Upon removal of the tonsillar pack, hemostasis was obtained with electrocautery. Having assured hemostasis, the procedure was terminated and the patient was taken to the recovery room in stable condition. There were no complications.
Elleson – Adenoidectomy & BMT
PREOPERATIVE DIAGNOSIS:
POSTOPERATIVE DIAGNOSIS:
PROCEDURE PERFORMED: Adenoidectomy with bilateral myringotomies and placement of ventilation tubes.
SURGEON: Dale A. Elleson, D.O.
ANESTHESIA:
ANESTHESIOLOGIST:
DETAILS OF PROCEDURE:
Under general anesthesia the right tympanic membrane was visualized under the operating microscope. A radial incision was made in the anterior inferior quadrant and a thin viscous middle ear effusion was aspirated. A ventilation tube was placed in the myringotomy incision. The same procedure was repeated on the opposite side, with a similar finding of thin serous middle ear effusion. After removal of the middle ear effusion and placement of ventilation tube, attention was turned to the oropharynx.
A McIvor mouthgag was placed for visualization. Using a laryngeal mirror the nasopharynx was identified. The adenoids were enlarged. An adenoidectomy was performed using an adenoid curet. Hemostasis was obtained with electrocautery. The nasopharynx was then irrigated through the nose while suctioning in the mouth. Hemostasis was again assured and the procedure was terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson – BMT Placement
DETAILS OF PROCEDURE:
Under general anesthesia, the right tympanic membrane was visualized under the operating microscope. A radial incision was made in the anterior inferior quadrant and a thin serous middle ear effusion was aspirated. A ventilation tube was placed in the myringotomy incision. The same procedure was repeated on the opposite side, with a similar finding of a thin serous middle ear effusion. Following placement of the second ventilation tube, the procedure was then terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson – BMT Removal
DETAILS OF PROCEDURE:
Under general anesthesia the right tympanic membrane was visualized under the operating microscope. The ventilation tube was localized in the anterior inferior quadrant and gently removed with an alligator forceps. The tympanostomy was then rimmed of squamous tissue using a cup forceps and a Barbara needle. The middle ear mucosa appeared normal. The same procedure was repeated on the opposite side. Following removal of the tubes and rimming of the squamous tissue, the procedure was terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson - Septoplasty
DETAILS OF PROCEDURE:
The patient was prepared and draped in the usual fashion. The nose was packed with cocaine-soaked Cottonoid pledgets. After waiting an appropriate period of time for the vasoconstrictive effect, the pledgets were removed. The nasal septum was injected with local anesthesia. The turbinates remained markedly enlarged after cocainization. The inferior edge of each inferior turbinate was injected with local anesthesia.
A left hemitransfixion incision was made and a mucoperichondrial flap was elevated. A 5 mm strip of cartilage was removed horizontally along the maxillary crest. A 3 mm strip of cartilage was removed vertically along the perpendicular plate.
This allowed the cartilaginous septum to swing free. Because of persistent bowing of the remaining cartilaginous septum, the cartilage was scored and morselized, which produced a cartilaginous septum which would lie in a midline position under no tension.
The right inferior turbinate remained markedly enlarged. It was fractured towards the midline. An incision was made along its free border and the soft tissue elevated from the lateral aspect of the undersurface of the turbinate. The turbinate bone was identified and excess turbinate bone was removed. Redundant soft tissue was also removed. The free edge of the turbinate was cauterized. The remaining turbinate was fractured laterally.
The same procedure was repeated on the opposite side. A good nasal airway was obtained on each side. The airway appeared clear. The nose was lightly packed with bacitracin impregnated
Telfa gauze.
The procedure was then terminated and the patient was taken to the recovery room in stable condition. There were no complications.
Elleson – T&A
DETAILS OF PROCEDURE:
Under general anesthesia a McIvor mouth gag was placed for visualization of the oropharynx. A red rubber Robinson catheter was passed through the nose, exiting the mouth for retraction of the soft palate. The adenoids were visualized and noted to be hypertrophied. An adenoidectomy was performed using an adenoid curet and nasopharyngeal biopsy punch. A nasopharyngeal pack was then placed in the nasopharynx for hemostasis. Attention was then turned to the tonsils.
The right tonsil was grasped with a tenaculum and retracted medially. The superior two-thirds of the tonsil was dissected free by both blunt and sharp dissection. The remainder of the tonsil was removed with a tonsillar snare. A tonsillar pack was placed in the tonsillar fossa. The same procedure was repeated on the opposite side. Upon removal of the tonsillar packs, hemostasis was obtained with electrocautery. Following the assurance of hemostasis, the tonsillar fossae were injected with local anesthesia. The nasopharyngeal pack was then removed and the nasopharynx irrigated through the nose while suctioning the mouth. All clots were removed and hemostasis was assured.
The procedure was then terminated and the patient was taken to the recovery room in stable condition. There were no complications.
Elleson – T&A BMT
PREOPERATIVE DIAGNOSIS:
POSTOPERATIVE DIAGNOSIS:
PROCEDURE PERFORMED: Tonsillectomy, adenoidectomy, bilateral myringotomies with placement of ventilation tubes.
SURGEON:
ANESTHESIA:
ANESTHESIOLOGIST:
DETAILS OF PROCEDURE:
Dale A. Elleson, D.O.
Under general anesthesia the right tympanic membrane was visualized under the operating microscope. A radial incision was made in the anterior inferior quadrant and a thin serous middle ear effusion was aspirated. A ventilation tube was placed in the myringotomy incision. The same procedure was repeated on the opposite side, with a similar finding of thin serous middle ear effusion. Following placement of the second ventilation tube, attention was turned to the oropharynx.
A McIvor mouthgag was placed for visualization. An adenoidectomy was performed using adenoid curets. A nasopharyngeal pack was placed in the nasopharynx. The right tonsil was then grasped with a tenaculum and retracted towards the midline. An incision was made in the mucous membrane of the anterior tonsillar pillar and supratonsillar fossa. The superior two-thirds of the tonsil was dissected free by both and sharp dissection. The remainder of the tonsil was removed with a tonsillar snare. Tonsillar packs were placed in the tonsillar fossa. The same procedure was repeated on the opposite side.
Upon removal of the tonsillar packs, hemostasis was obtained with electrocautery. The nasopharyngeal pack was then removed and hemostasis obtained with electrocautery, using the laryngeal mirror for visualization. The nasopharynx was then irrigated through the nose while suctioning in the mouth. Local anesthesia was injected into the tonsillar fossae and the procedure was terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson - Tonsillectomy
DETAILS OF PROCEDURE:
Under general anesthesia a McIvor mouth gag was placed for visualization of the oropharynx. The left tonsil was grasped with a tenaculum and retracted medially. The superior two-thirds of the tonsil was dissected free of the tonsillar fossa by both blunt and sharp dissection. The remainder of the tonsil was removed with a tonsillar snare. The tonsillar packs were placed in the tonsillar fossa. The same procedure was repeated on the opposite side. Upon removal of the tonsillar packs, hemostasis was obtained with electrocautery. Following the assurance of hemostasis, the tonsillar fossa was injected with local anesthesia. Hemostasis was again assured and the procedure was terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson - Tympanoplasty
DETAILS OF PROCEDURE:
Under general anesthesia, local anesthesia was injected into the external auditory canal and the soft tissue anterior to the tragus of the *(right/left) ear. An incision was made along the lateral aspect of the tragus and carried down to the tragal perichondrium. The soft tissue was elevated from the anterior surface of the tragal perichondrium. The perichondrium was incised and elevated. The perichondrium was then excised, pressed and dried, to be used as grafting material. The tragal incision was approximated with chromic suture. Attention was then turned to the tympanic membrane.
The perforation was rimmed of squamous tissue using a Barbara needle and cup forceps. Canal incisions were made at both 6 and
12 o'clock, extending from the annulus approximately 5 mm lateral. The lateral aspect of these incisions was connected posteriorly using a round knife. A posterior tympanomeatal flap was created and the middle ear entered inferiorly. The annulus was elevated and the tympanomeatal flap retracted anteriorly.
The mucous membranes appeared normal. The incudostapedial joint was intact. Gelfoam was then placed in the middle ear below the area of the perforation. The perichondrial graft was cut to size and placed lateral to the Gelfoam. Additional Gelfoam was added to ensure complete elevation and contact with the undersurface of the tympanic membrane. The tympanomeatal flap was retracted into its original position. Care was taken to ensure that the entire undersurface of the perforation was covered by graft.
Gelfoam was then placed lateral to the tympanic membrane and its underlying graft. Bacitracin Ointment was placed lateral to the
Gelfoam and a sterile cotton ball was placed in the ear. The procedure was then terminated, and the patient was taken to the recovery room in stable condition. There were no complications.
Elleson – UPPP & Tonsillectomy
PREOPERATIVE DIAGNOSIS:
Obstructive sleep apnea syndrome.
POSTOPERATIVE DIAGNOSIS:
Obstructive sleep apnea syndrome.
PROCEDURE PERFORMED:
1. Uvulopalatopharyngoplasty
2. Tonsillectomy.
SURGEON:
ANESTHESIA:
ANESTHESIOLOGIST:
ESTIMATED BLOOD LOSS:
Dale A. Elleson, D.O.
General.
DETAILS OF PROCEDURE:
Under general anesthesia, the patient was draped in the usual fashion. A McIvor mouthgag was placed for visualization. The left tonsil was grasped with a tenaculum and retracted towards the midline. An incision was made in the mucous membranes of the anterior tonsillar pillar extending through the supratonsillar fossa. The superior two-thirds of the tonsil was dissected free by both blunt and sharp dissection. The remainder of the tonsil was removed with a tonsillar snare.
Tonsillar packs were placed in the tonsillar fossa. The same procedure was repeated on the opposite side. After removal of the tonsillar packs, hemostasis was obtained with electrocautery.
Attention was then turned to the palate. A mucosal incision was made from the supratonsillar fossa on the right across the palate to the supratonsillar fossa on the left. Using a
Metzenbaum scissors, the palate was incised through to the nasal surface. Approximately 1 cm of soft palate, along with the uvula, was removed. Hemostasis was obtained with electrocautery. The mucous membrane of the nasal surface of the soft palate was then approximated with the lingual surface of the soft palate using interrupted chromic sutures. Local anesthesia was injected into the tonsillar bed and into the soft palate near the site of its free border. Hemostasis was again assured and the procedure was terminated.
The patient was taken to the recovery room in stable condition.
There were no complications.
Elleson – UPPP & tonsillectomy & glossectomy
PREOPERATIVE DIAGNOSIS:
Obstructive sleep apnea syndrome.
POSTOPERATIVE DIAGNOSIS:
Obstructive sleep apnea syndrome.
PROCEDURE PERFORMED:
1. Uvulopalatopharyngoplasty.
2. Tonsillectomy.
3. Radiofrequency partial glossectomy.
SURGEON:
ANESTHESIA:
ANESTHESIOLOGIST:
Dale A. Elleson, D.O.
General.
*
ESTIMATED BLOOD LOSS: * cc.
DETAILS OF PROCEDURE:
Under general anesthesia, a McIvor mouth gag was placed for visualization. Local anesthesia was injected around the supratonsillar and infratonsillar fossae on each side and also into the free edge of the soft palate. The left tonsil was grasped with a tenaculum and retracted towards the midline. The mucous membrane of the anterior tonsillar pillar and supratonsillar fossa was incised. The superior two-thirds of the tonsil was dissected free by blunt and sharp dissection.
The remainder of the tonsil was removed with a tonsil snare.
Tonsillar packs were placed in the tonsillar fossa. The same procedure was repeated on the opposite side. After removing the tonsillar packs, hemostasis was obtained with electrocautery.
Attention was then turned to the soft palate. A mucosal incision was made from the anterior tonsillar pillar on the right across the lingual surface of the soft palate to the anterior tonsillar pillar on the left. This incision was carried through to the lingual surface of the soft palate. This portion of the soft palate was then completely excised. The uvula was included in the excision. Hemostasis was obtained with electrocautery. The mucous membrane at the lingual surface of the soft palate was then approximated to the nasopharyngeal surface of the soft palate using interrupted chromic sutures.
Hemostasis was again assured. The McIvor mouth gag was then removed.
A bite block was then placed. The tongue was grasped with a 4x4 gauze and the base of tongue retracted with a retractor. The
Gyrus unit was set to rapid lesion mode and 550 joules. Using the dual needle probe, the needles were inserted in the midline of the tongue in the area of circumvallate papillae. Then
550 joules were delivered in the rapid lesion mode. The needles were removed and re-inserted approximately 1 cm anterior in the midline. A second treatment in the rapid lesion mode using
550 joules was delivered. The needles were then removed and the bite block removed. The procedure was terminated and the patient was taken to the recovery room in stable condition.
There were no complications.