Middle cerebral Artery
advertisement

1
Hemiplagia
Def
It is a paralysis of one side of the body due to pyramidal tract lesion
from the contralateral cortex to the ipsilateral upper cervical segment
N.B. Paralysis
=
loss of active movement.
Paresis
=
loss of active movement against resistance
The lesion must be above C5 in case of spinal cord lesion ?
Because U.L. nerve supply starts at C5 so lesion below 5th cx
segment may spare U.L. & may affect in L.L. only.
UMNL
ر
ر
ر
ر
ر
From cortex till AHCs
Clasp Knife spasticity
Slight wasting
Exaggerated deep reflexes
Extensor planter
LMNL
From AHCs & down wards
Hypotonia
Marked wasting
Lost
- ve
Motor pathway =
area 4
Internal
capsule
M. br.
Pons
M.O.
UMN
=corticospinal
tract
P.N.
muscle
AHCs
Motor root
LMN
2
î In neurological cases you must to answer about 2 questions
Where is the lesion ?
What is the lesion ?
î The tract carries the motor fibres of the opposite half of the body
so lesion at one side in the previous pathway
hemiplegia at
the opposite side
Localization of the lesion
(Where is the lesion)
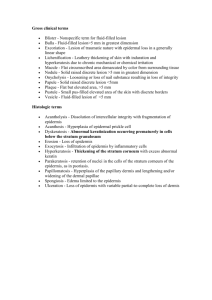
Cortical lesions
usually lead to monoplegia rather than hemiplegia
Q Why?
Due to 1) Wide distribution of Betz cells in area 4
2) The medial part of it supplied by bl. supply different
from the outer part.
Medial part = L.L. area supplied
by Ant. cerebral artery
outer part = face & U.L. area
supplied by
Middle cerebral Artery
ch. ch. of cortical lesion
starts as
monoplegia
cortical
other cortical
sensory loss in the
manifestations.
paralysed limb as
sensory cortex is nearby
motor area
aphasia
conjugate
Jacksonian
e.g. if LL is affected we find
Deviation fits
that there is loss of tactile
of the eye
Localization. & discrimination. L.L.
N.B.
Pt. with conjugate D. of the eye to one side
= ipsilateral cortical lesion or contralateral pontine lesion.
3
Capsular hemiplegia
(complete hemiplegia)
ch.ch.
UMNL
Hemiplegia in the opposite side
Hemihypothesia in the opposite side
Cr. Nr.
lower part of 7 opposite side
12 of opposite side
Tongue deviated to the side of paralysis
Homonymous hemiplegia
No cortical manifestations.
4
xx lesions
7th
Cr. N.
12th
Cr.N.
Here the lower part of
facial N. & 12th
Cr.N. are affected on the
same side of parlaysis
xx lesion
Ms of
Tongue x x
normal
side
of
paralysed
opposite
the side
of lesion
the tongue
so it is deviated
the side of
hemiplegia
N.B. Here Cr. Nr. lesion is UMNL lesion in tract = corticobulbar tract
lesion
4
Also Cr. Nr paralysis at the side of hemiplegia
5
Brain stem lesions
M.br.
Pons
(Crossed hemiplagia )
4
Lesion
3rd Cr. N.
4th Cr. N.
M.O.
N.B
midbrain lesion for example leads to :
1- Hemiplegia on the opposite side
2- Hemihypothesia on the opposite side
3- Cr. Nr. 3,4 LMNL on the same side of lesion = opposite
the side of hemiplegia = crossed hemiplegia
localization of brain stem lesions or crossed hemiplegia
a- general criteria of brain stem lesions : ( as above )
1- Hemiplagia & hemihypothesia on the opposite side of lesion.
2- Cr. Nr. (LMNL) on the same side of lesion opposite the
side of hemiplagia.
b- especial Criteria (according to the level)
1- Midbrain Cr. Nr. 3,4
Dilated pupil
Neurogenic hyperventilation
2- Pons
Cr. Nr. 5,6,7
pin point pupil
Apneustic breathing
3- M.O.
Cr. Nr. 9,10,11,12
Ataxic breathing
vital centers ( V.M.C. , Respiratory center
usually affected
6
Important Syndromes
= hemiplegia on the opposite side of
the
(Brain stem lesions)
lesion + Cr.Nr ( LMNL ) on
the same
side of the lesion
1- Weber’s $
midbrain lesion
Hemiplagia
2- Benedict’s $
hemihypothesia
midbrain lesion with
Cr. Nr. 3 lesion
only
3rd Cr. Nr.
Hemiplagia
Red nucleus
lesion
+ hemihypothesia
hemiatorxia
on the opposite
side of lesion
midibrain
mid brain
Red nucleus
3
rd
contralateral
cerebellum
Crebellum
cerebellum)
3- Millard $
Pontine lesion with
rd
3 Cr. nerve
(connected
to the
Cr.Nr.
Red nucleus
Hemiplagia + hemihyopthesia
Cr.Nr. 6,7
4- Foville’s
hemiplegia + affection of M.L.B.
conjD.of eye
5- M.O ( Avellis $ )
hemiplegia + Cr. Nrs 9 , 10
Spinal hemiplagia ( unilateral lesion above C5 )
post. Column tract
tract
spinothalamic
tract
(Brown sequard $)
post. c.
tract supply the
same side of the
body
post. column
supply the same
side of the body
spinoth. tract
supply opposite
side of the body
Spinal hemiplagia:
There is hemiplegia with deep sensory loss on the same side
of the lesion with dissociated superficial sensory loss on the
opposite side below the level of the lesion.
7
Causes of hemiplagia ?
= What is the lesion?
we
can
determine
the
causes
of
hemiplegia
by the followings :
# Onset
Course
duration
# Risk factors
D.M.
Hypertention
The
Heart(as
embolisation)
# age
# associated S. & S.
1-
Vascular hemiplegia
of
(cerebrovascular stroke)
Hemorrhage
Onset
Course
+ve risk factors
source
thrombus
embolus
acute
regressive !?
It is difficult clinically to differentiate the three
conditions but for example
Z- Pt. with MVD or prothetic valve
mostly embolic lesion
Z- Hypertensive Patient
lacunar infarction
Haemorrhage
due to lesion in penetrating arterioles
Z- Dramatic onset
=
mostly
Hage
embolic
Q
Vascular hemiplagia
Causes
in cases of embolism
or
what is the lesion?
Haemorrhage- embolus - thrombus
thrombosis
try to determine
the occluded artery
8
onset, course, risk F.
associated S & S
Where is the lesion?
( Cortical - caps. –Brain stem)
Causes of Vascular hemiplegia in young?
Renal hypertension ( 2 ry)
Heart as a source of embolism e.g M V D + AF
Vasculitis
young
young
S. L. E.
P Ar. N.
Angiomatous malformation.
2
Inflammatory :
( encephalitis)
acute onset
regressive course
Fever
signs of meningeal irritation
EEG
voltage !!
3Space occupying lesion :
gradual onset
progressive course
I. C. T.
4-
Congenital
The lesion is since birth.
5-
Traumatic
as sp. cord trauma (Br. sq. $)
6-
Degenerative disease
7-
Demyelinating : as D.S.
Q
Causes of transient or recurrent hemiplegia ?
gradual onset
remission & excerbation
1- Transient ischemic attack
2- Hypertensive encephalopathy
9
3456-
D. S.
Hysterical
Post. epileptic !? ( Todd’s paralysis )
Vasculitis.
Stages of hemiplegia
I
(In vascular cases)
Transient ischaemic attack
(specially in thrombotic lesions)
= Focal neurological deficit for < 24 hrs
e.g.
Heaviness, in UL or L L parathesia,
dysarthria
or deviation of mouth .
II
Stage of flaccid paralysis (flaccid stage )
Hypotonia
during this stage the pt. may be comatosed , How can
diagnose
i.e. looking for signs of lateralisation:
1- The paralysed side drops more passively.
2- Conj. D. of the eye
3- Cheek moves in & out with respiration on the
paralysed side
4- Normal limb moves with painful stimuli
5- Extensor planter
we
III
Hyporeflexia
Weakness
Spastic stage:
Weakness
Hypertonia (clasp knife)
Hyper reflexia
U.L. distal > proximal,
extensor > flexor
L.L. distal >proximal, flexor >extensor
Tone
U.L. position
L.L. position
flexion in elbow ,wrist ,
fingers & adduction
extension in hip, knee
& adduction
10
Hyper reflexia.
Extensor planter + loss of abdominal reflex.
Other sure signs of pyramidal lesions (see later)
* The condition is associated with hypothesia.
11
Sure signs of lesions
Extensor planter
Brisk reflex ( tendon jerk )
Lost abdominal reflex
Polyphasic reflex
Clonus
U.L.
Hoffman sign
Wartenburge sign
Finger jerk sign
Q
Investigation:
1- CT - Scan
value:
2- MRI
3- EEG
Space occupying lesion
haemorrhage
Subarach. & Subdural hage
Infarction ( appear within 48 - 72 hours )
lacunar infarction may be small < 5 mm
it may not appear
Brain oedema
Brain stem lesion
poor resolution
(Magnetic resonance Imaging)
It detects small infarction & brain stem lesions
diagnose epilepsy ( discharge from the site
of lesion )
4- CSF
encephalitis
proteins
subarachinoid hge
5- Risk Factors Fundus ex.
malignant H.
Bl. sugar & S. lipid - echocardiography
Bl. disease as polycythemia rubra vera
Complication of hemiplegia
1- Psychosis
3- Constipation
5- Osteoporosis
N.B.
( prolonged bed rest )
2- Bed sores
4- Wasting
6- D. V. T.
Sphincters usually are intact in hemiplegia as it is a unilateral
lesion.
12
ttt
Care of comatosed
a- Ryle tube
b- Mouth hygiene
c- bed sores
d- Physiotherapy
e- Prophylactic ABO to guard against infection.
Uncomatosed
a- good nursing
b- control Bl.pr.
c- ttt of risk factors
d- physiotherapy
Q
Role of anticoagulant, dehydrating measures and vasodilators ?
( See Strokes )
Case of hemiplagia
Key
Examine Cr. Nrs
Affected
Not affected
7,12 only toward
Other
Cortical
the side of hemiplegia Cr. Nr. opposite
( UMNL )
the side of hemiplegia
(LMNL)
usually
monoplegia
It is a Capsular
It is a Brainstem lesion
lesion
3,4 5,6,7 9,10,11,12
M.B.
Pons
Medulla
Complete hemiplegia from
the start
Spinal
Cord
Dissociated
sensory loss
on the
opposite side
below the
level of the
lesion
13
Paraplegia
Def
It is a paralysis of both L.L.
Spastic
paraplegia
Flaccid
Paraplegia.
due to shock stage of UMNL
or
due to UMNL
Opinion
A
due to LMNL !?
LMNL in L.L. is not considered as paraplegia
It can be discussed as separate subjects as
O AHCs lesion
poliomyelitis
O Root lesion
Qauda . E.
O PN lesion
P . neuropathy
Cortical paraplegia
Parasagittal meningioma
paralysis of both
L.L.
Occlusion of unpaired anterior cerebral artery
normal Ant.
cerebral Ar.
unpaired Ant. cerebral Ar.
Little disease = cerebral palsy
Congenital degeneration of nervous system
due to birth injury or hyopxia of newly
born.
It’s ch.ch. by
Bilat. lesion
Mental retardation
Involuntary movement
14
Cerebellar ataxia
Optic atrophy
Criteria of cortical paraplagia
Bilat
of both LL
B
Cortical
sensory loss of
both LL
No sensory or motor
level to be differentiated
from spinal cord lesion
Spinal
The most important group are the Focal spinal cord lesion
e.g
one segment is diseased ,
but above & below
which
the spinal cord is normal
lesion
a-
Causes of focal S.C. lesion (paraplegia with level)
Vascular
Ant. spinal Artery
occlusion
b-
Inflammatory
Transverse
myelitis
compression
paraplegia
Other causes of paraplegia( they are not focal lesions)
= paraplegia without level
due to lesion of tract in sp. cord from below upward
Causes
pellagra- subacute combined degeneration
Motor ataxia - Motor N.D.
D. S.
General manifestation of Focal S. C. lesion
i.e. paraplegia with level
above the level of
the lesion every
thing
is normal
below the level
15
Sensory level
e.g. T10
(Umbilicus)
loss
lesion
C / P. of paraplegia with level
I
at the level of lesion
of lesion there are
UMNL and sensory
(focal spinal cord lesion)
Sensory sensory loss due to
affection of the sensory root which
enters the affected segment
Motor
LMNL due to affection of motor root
Or AHC which a rise from the
affected segment
II Below the level of lesion
Motor give UMNL as the pyramidal tract is affected at this
level so, the pyramidal tract will not reach below that
level.
= manifest. in both L.L. (UMNL below the level of
lesion)
Hyperreflexia
Sensory
Hypertonia weakness extensor planter
clasp knife
Dist.> proximal
Flex.> extension
abd. > add
loss of sensation , due to affection of
spinothalamic or post column tract or both at the
level of the lesion, so these tracts will not carry
sensations from parts of the body below the level
of lesion
Sphincteric disturbance
acute
lesion
gradual
lesion
Retention
Hesitancy or Precepitancy
N.B. * Autonomic manifestation may occur ...
sympath. outflow from the cord is limited to segments from
T1
L2 so the lesion between.these segments give autonomic
16
disturb. below the level of lesion. Also lesion above T1 will give
autonomic manifestations below the level of the lesion
e.g.
V.D.
sweating
edema of the limb
* Paraplegia = bilateral lesion
sphincteric disturbances.
Transverse myelitis
The term myelopathy is more correct as the cause is not always infection
Aetiology :
1- viral
2- T.B.
3- pyogenic
4- $
C / P.
acute onset of fever then paraplagia
the course is usually regressive
At the level of the lesion ( as usual )
Sensory
Motor
loss of sensation
LMNL
e.g at the level of
in the ms Supplied by
Umbilicus if the level of the
the segment affected
lesion at T10
so, there are weakness, flaccidity,
and hyporeflexia in the muscles
supplied by the affected segment.
Below the level
0 Sensory
loss of all sensation due to affection
of
spinothalamic tract & post
column tract .
0 Motor
UMNL
acute stage
(shock stage or flaccid stage)
0
0
before)
after shock stage
Hypotonia
spasticity
Hyporeflexia
Hyper reflexia
Weakness
extensor planter
Sphincteric disturbance
early
retention with overflow
late
automatic bladder
Autonomic manifest.
below the lesion
(as
17
No gross abnormality
It aims to exclude compression by
C.T. scan
Myelography
MRI
D.V.T. - Psychosis - Bed sores - Constipation
Investigation
Complication
ttt
Steroids: e.g Prednisolone
20mg TDS at first then
gradual tappering with improvement
ACTH can be used.
Physiotherapy and general care
of paraplegic patients
Anterior spinal artery occlusion
this part
supplied by anterior
Sp.Ar.
It is a rare disease common in middle age & diabetics
C/P. acute onset of paraplagia as transverse myelitis
At the level there
is sensory loss +
LMNL
Below the level
UMNL(shock stage then spastic stage)
Sensory loss
with intact post column tract
dissociated sensory loss .
N.B.
In Ant. Sp. Ar. occlusion & T.V. myelitis
if ascending myelitis occur
this may affect cx segment
quadriplegia
Compression paraplegia
It is a focal S.C. lesion with gradual onset & progressive course due to cord
compression .
Causes I Extramedullary
18
Vertebral causes
Traumatic
pott’s disease
Tumors of spines
1ry
2ry
acute onset
Dural causes :
leukemic deposits (extradural)
meningioma (intradural)
pachy meningitis (dural)
tumours of S.C.(gliomas)
syringomyelia
II Intramedullary
N.B.
Disc prolapsed is the commonest extramedullary lesion
Diagnosis of intramedullary & extramedullary compression :
the Prognosis of extramedullary is much better than intramedullary
Surgical removal of extramedullary lesion is easier than
intramedullary So, It’s important to differentiate between
intramedullary & extramedullary compression according to the
following :
extramed. lesion
Intramed. lesion
Root pain
(Radicular pain)
Sphincters
Sensory loss
extramed.
+ ve early in the
course of disease
intramed.
usually not associated with
root pain or rare
early affected in intramedullary
Late in extramedullary
the fibres of spinoth. tract arranged that
sacral fibres are the outer one &
cx are the inner fibers so,
extramed lesion
early sacral
affection
Intramed lesion
late sacral
affection
19
there is special march for affection
especially if it is presented
Motor
with
quadriplegia
Why ?!
( i.e in cx lesion )
╥ affection of one U.L. then L.L. on the same
side
fibres !
C / P.
╥ then lower limb of the opposite side and
lastely upper limb .
of compression paraplagia ..
(Gradual onset, progressive course)
It’s a focal paraplagia as usual. So there are: حat the level
sensory loss
LMNL
حBelow
UMNL
the level
Sensory loss
Sphincteric manifestation
Stages of paraplegia :
Stage of neuronal shock
his occurs only with acute lesion & persists for wks.
there are
hypotonia
hypo reflexia
loss of all sensation
Paraplagia in extension
due to affection of fibers with preservation of extra
so, since the extensor muscles are more spastic
extension of L.L.
Late paraplagia in flexion
due to affection of extra fibers
the flexor muscles
are more rigid
flexion of L.L.
Investigation of compression paraplegia ..
1- plain x- ray
Secondaries
on spines
pott’s
disc
20
Soft tissue shadow
Narrowing of
of cold abscess.
Collapse of space disc space
between vertebrae
2- C.T. Scan
Limited C.T. Sca
3- Myelography
By
cisternal
puncture through
atlanto occipital membrane
The dye descent
down & arrested
at the site of the
lesion , it may be
used
to
differentiate
between extra &
intramedullary
lesions.
Or by lumbar
puncture.
21
dye
S.C.
extramed.
lesion lesion
subarachnoid
space.
dye
lesion
Unilateral tail
dye
Intramed.
lesion
lesion
N.B. Now the Dye is H2o soluble
No harm at all
4- C. S. F. ex.
a Colour Compression
venous congestion
escape of blood pigment into CSF
xanthochromia
b Protein Venous congestion
protein escape to
CSF
Spontaneous coagulation
c Cells i.e. Cytoalbuminous dissociation
Froin $
Xanthochromia
Spontaneous coagulation
Cytoalbuminous dissociation
= Compression on Spinal cord
N.B. Queckenstedt’s test
Normally CSF pr. = 5 - 15 cm H2o
We do lumbar puncture and measure the CSF Pr by manometer
and then we do pr. on jugular veins
a- Normally, with bilat. jugular. vein occlusion
CSF.Pr sharply
b- In partial extramedullary compassion
CSF pr. gradually
c- In complete compression no change in CSF pressure.
Complication
1 Bed rest
D.V.T.
Bed sores
constipation
2 neurog bladder
U.T.I.
CRF
Reflux
Back pressure on kidney
Nephropathy
22
ttt
1- ttt the cause
2- Care of bladder
3- Physiotherapy
4- symptomatic ttt for pain
Surgical
removal of space
5occupying lesions
N.B
The spinal cord is shorter than vertebral column so:
In cervical lesions, substract one from the segmental
level to detect the opposing vertebra.
In upper 6 thoracic
substract 2
In lower thoracic
substract 3
Syringomyelia
It is an intramedullary focal spinal cord lesion ccc by cavitation in the
center of the spinal cord and may be the brain stem (syringobulbia).
C/P
onset
gradual
Course
s. progressive
a- at the level
sensory loss
LMNL
b- Below level
sensory loss
as usual
UNNL
paraplegia
sphincteric disturbance
with level)
since it is an intramedullary lesion
Root pain late
N.B
early sphinctric disturbance
the Pattern of sensory loss
early : jacket hypothesia
late : sensory level
23
The Central lesion of
The s.c affects the
decussating
Fibres of sensory
roots of the
spinothalamic tract
near by the central
canal .
Late
this disease
usually affect
more than one
segment
early
Jacket hypothesia of dissociated sensory loss as
the P.C. is intact. ( as its fibres away from the
central canal )
Spinothalamic tract will be affected
level as any focal spinal cord lesion.
sensory
- Pathgenesis
blockage of the exit foramina of the fourth. V C.S.F
can’t escape into the subarachnoid space
pr in
the ventricle which communicating to central canal of
S.C
which expands
- Investig.
- ttt
compression of the S.C
Mylography, CT scan + MRI
decompression
24
Systemic diseases presented
with paraplagia
Q.
As S. C. D. & pellagra
Criteria of systemic diseases
جBilateral & symmetrical lesion
جgradual onset
جslowely progressive course
جselective ( i.e they affect certain systems )
tract lesion in systemic diseases ch.ch. by :all manifestation are present except
abd. reflex
sphincters
are
spared
SCD
= Subacute combined degeneration
It is a vit B12 ( see blood )
C/P
anaemia
neurological menifestation
bilateral lesion
bilateral P.C. lesions
in the spinal cord
sensory
from below upward , so :ataxia
early paraplegia
late Quadriplegia
see later
Invest. & ttt see anaemia
peripheral neuropathy
glove & stocke
Pellagra
It is one of vit B (nicotinamide )
C/P.
Bilat. & P. N. (as SCD but without P.C.)
other manifestations & TTT see vitamins .
see later
25
Disc prolapse and spondylosis
@
&
@
Intervertebral discs are kept in their position by ligaments anterior
posterior longitudinal
The disc composed of :
annulus
nucleus pulposus
jelly like
nucleus
annulus fibrosus
@
Types .. aetiology
1- Traumatic (acute disc prolapse)
acute onset, may occur due to lifting a heavy object usually occur
in
young age
usually lumbar L4 - L5 , L5 – S1
here there is tear in A.F. through which N. P. protrude
2- Degenerative (spondylosis)
It is mainly annular degeneration
N.P protrude
ch.ch : Old age - No trauma required, it may be due to wear and
tear, this can affect the cervical segments & lumbar segment
C/P.
Depend on the level of lesion & direction :Spine
post. prolapse
cord compression
Transverse
lateral root compression
sensory
process
motor
Spinal cord in vertebral canal
posterolateral
S.C. and root compression
So, C/P. may be
1- cx. level
cx.
Spondylosis quadriplegia
2- lumbar level
Siatica
Quada equina
3- thoracic segments
paraplegia
Lumbago is a low back pain due to abnormalities in :
1- Joints
3- Lumbar spines
2- Ligaments and muscle
4- Disc prolapse
Body of vertebrae
26
C /P. of cx Spondylosis
1- Lateral prolapse affects roots of U. L.
a- Sensory roots
e.g. C6 radicular pain or radicular sensory loss
along
lateral aspect of forearm
b- Motor C8 ,T1
Wasting of small ms of hands
N. B. Radiculopathy
= pathology within root
e.g.
motor LMNL
Sensory
Radicular pain
then radicular sensory loss
1- Cx Spondylosis
UL manifestations
2- Qauda equine
LL manifestations
3- Diabetic radiculopathy (not a compression)
mainly sensory manifestations
2- Posterior prolapse (Cord compression)
It is focal S.C.
(see before)
· .·
lesion may occurs in upper cx segment
Quadriplegia
= lesion in 4 limbs
3- Posterolateral prolapse (cord & root compression)
U.L.
signs of LMNL (root compression)
& UMNL (cord compression)
L.L.
UMNL
N.B.
C /P.
lesion which involves 5th segment inverted
supinator reflex i.e
lost or weak biceps C5,6 ( LMNL )
exaggerated triceps C5,6 ( UMNL )
= ( the Biceps reflex
flexion of fingers)
of Lumbar Spondylosis
- Qauda equina
- Sciatica
see later
27
28
Investig.
(Of cervical or lumbar spondylosis)
1- Plain X-ray
Narrowing of disc space
Osteophytes formation due to
calcification of the prolapsed disc
2- Myelography
3- C. T. Scan
4- MRI
ttt
1- Medical
NSAID
Glifarelax
Norflex
Coltramyl
Ms relaxant
2- Physiotherapy e.g short wave
3- Plastic collar for cervical lesions
for fixation but never > 3m. to avoid wasting of ms
or lumbar corset for lumbar lesions
4- Surgery ( Decompression )
Indication
of surgery
Cord compression
signs
Sphincteric disturbance
Severe resistant pain
N.B. other measures for TTT
1- Suction under CT Scan
2- Laser photocoagulation
29
Sciatica
It is a pain along the distribution of sciatic nerve
back of thigh, leg,
foot
Causes
1- acute disc prolapse (traumatic)
2- Lumbar Spondylosis
3- Malignant pelvic tumor
4- Sciatic nerve neuritis as in D.M.
( the commonest cause of sciatica is disc prolapse )
C/P
S. - pain along the course of sciatic nerve increase by cough ,
straining , stretching
S. - a. Sensory
hypothesia along sciatic nerve
+ ve signs of meningeal irritation as this
lead
to traction on roots of sciatic nerve, pt. can’t
elevate the leg up to 90 without pain
b. Motor LMNL in ms supply by the nerve
c. Back pain
Investig.
X- ray
ttt
as disc prolaspe
-
CT Scan
-
Myelography
> Lumbar canal stenosis
It is a congenital
narrowing of lumbar spinal canal,
exacerbated by degenerative changes which occur with age
there is pseudo claudication with normal peripheral pulsations
> Q
posterior
Acute disc prolapse = lumbar disc prolapse L 4 - L 5
L5-S
sciatica
Q. E
Spondylosis
cervical
cord comps
lateral
root comps
lumbar
sciatica
30
quda equina
26
Cauda equina
It is a radiculopathy (root disease ) affecting lumbo sacral roots, mostly
due to compression.
S.c
Causes
Meninges
Meningioma
leukaemic deposits
Spines tumours
disc prolapse
meninges
Prolapsed
disc
disc
C/P.
since Q. E. is lumbo sacral roots supplying the
L. L.
Motor
Sensory
1- Manifestation. of the cause (e.g disc)
2- Sensory
µ radicular sensory loss in L. L.
µ L. L. affected with asymmetry
3- Motor
asymmetrical LMNL in L. L.
wasting.
flaccidity
spines
hyporeflexia
4- Sphincteric disturbances ( according to the affected root )
Sensory root lesion
Motor root lesion
No desire +ve desire
but the patient
patient can’t
can micturate
micturate
Both roots lesions
Retention
Late
Retention
bladder
acts by its myogencity
(autonomic) bladder
ttt
ttt of the cause (compression)
Symptomatic ttt
27
Peripheral neuropathy
It is an inflammation or degeneration of the peripheral nerves with motor,
sensory and autonomic manifestations
Pathological classification ..
a.
Demyelinating neuropathy .
Rapid onset, CSF affected because of the root damage, + ve Cr.
Nr. Lesion there is degeneration of the myelin sheath due to
immunological or infectious insult .
e.g. Guillian - Barre $
Myelinopathy
b.
Axonal neuropathy :
Ch. ch. by degeneration of the distal ends of long axons
It starts with distal sensory manifestation & spread
proximally
Roots usually not involved so CSF is normal e.g. D. M.
c.
Neuronopathy : affection of the cell body
e.g.
Amytrophic Lateral Sclerosis
Paramalignant $
Classification of neuropathy
mono neuropathy: affection of a single nerve trunk in one limb
e.g. ulnar or median nerve
mono neuropathy multiplex: affection of more than one trunk in
one limb e.g. ulnar n. + median
nerve
poly neuropathy: systemic affection of peripheral nerves of all
limbs
Causes of polyneuropathy
Heridofamilial
Peroneal ms
atrophy
Symptomatic ( 2 ry )
Idiopathic
Paramalig. $
or immune mediated
bronchogenic carcinoma
Inflam. Viral
T.B. , D
G. Barre $
Drugs INH, vincristine
Toxic alcohol, lead
Vascular
P. Ar. N
28
Nutritional
SCD, pellagra, beri beri
Metabolic
D.M. , uremia
C.T disease SLE, Rh. D
Causes of mononeuropathy :
Trauma, D. M. , entrapment myopathy eg carpal tunnel $
Causes of mononeuritis multiplex :
D.M.
P.Ar.N
Sarcoidosis
Leprosy
amyloidosis
C / P. of polyneuropothy :a Motor
1- LMNL
2- Bilat, Symmetrical
3- L.L. > U.L.
4- D. > Pr. & extensor > flexor
5- Foot & Wrist drop
6- Ankle lost , Knee jerk is preserved
7- Cr. Nr. affection
8- Gait, high stoppage due to foot drop
b Sensory
1- Superficial sensory loss :
Glove & Stock (parathesia) then hypothesia
2- Deep sensory loss : ( sensory ataxia)
Vibration normal at ASIS & Decreased at malleoli .
c
Autonomic
hypotension
Coldness, cyanosis, loss of hair, orthostatic
Specific types of poly neuropathy
1- Peroneal ms atrophy ( Charcot - Marie tooth disease )
It is neuropathy mainly motor also there is glove and stocking
hypothesia
It is a herido familial ant. D in 1 st & 2nd decade, the wasting start
in
L.L. in peronii then ant. tibial group then
ascends to involve
the ms
of lower 1/3
of thigh inverted champagne bottle
appearance.
It is Ch. Ch. by
marked wasting
minimal weakness
2- Diabetic neuropathy :
Pathogenesis
a- micro angiopathy of vasa nervorum
b- Neutritional (hypovitaminosis)
c- Keton bodies
d- Glycosylation of
Protein
29
Lipoproteins
Collagen Fs thick basement membrane of
b
l
o
o
d
v
e
s
s
e
l
s
Five- Activation of sorbitol pathway which is a very toxic
substance to
peripheral nerves
C /P. (mainly sensory)
Sciatic Nr
a. early
mono neuropathy
Femoral Nr
ulnar, median Nr
b. Late
polyneuropathy
( as before )
superficial sensation
1st
parathesia which is an abnormal
sensation rather than
pain
Numbness
e.g.
late superficial sensory loss
Tingling
Deep sensory loss
sensory ataxia
Motor
LMNL - (D> P - loss of ankle jercke)
autonomic e.g impotence , diarrhea constipation,
gastroparesis postural hypotension
Cr. Nr.
Ocular 3,4,6
ttt
1- Control D.M.
2- Vit. B. complex
30
3- Severe parathesia
NB
tegretol (see epilepsy) 200-600mg/D
Diabetic amyotrophy
Painful weakness of thigh – Tenderness and marked wasting of
the thigh
Q
How can you test autonomic function ?
Postural hypotension
Carotid sinus massage
Valsalva (straining)
intra thoracic pr. V.R.
B.P. Reflex H. R.
Pupile
atropin (Dilatation)
Pilocarpine (Constriction)
Acute infective polyneuropathy
= Guillain Barre $
It is an inflammation of the peripheral nerve & roots due to
demyelination
due to immune or viral insult. (1-4 wks after viral
infection)
It is mainly motor
Cr.Nr. affected esp bilat.Facial nerves
Prognosis 85 %
recovery
C / P.
a.
b.
c.
Initial febrile illness
fever
malaise
Headache
Then laten period for days or wks
paralytic stags
all muscles of the limbs
proximal and distal muscles are involved
Start in L. L. & ascend to involve U. L.,
trunk, & ms of respiration
Sensory
glove & stock hypothesia
G. Nr.
3, 7, 10
C.S.F. cytoalbuminous dissociation due to root
31
affection (excess protein with either normal cell
count or a moderate increase in cells)
CSF examination
S. Lead - urinary porphyrin.
1 Rest
2 Care of ms of respiration
3 Steroids(20mg prednisolone TDS) 4 Plasmapharesis
4 Physiotherapy.
6 I.V immunoglobulins
Investig
ttt
N.B
you must to give the data below
In any type of neuropathy
1- Sensory or motor
2- autonomic manifestion
3- Cr. Nr. affected
e.g. D.M.
G.B.$
mainly sensory
mainly motor
autonomic + ve
+ ve
Cr. Nr. ocular
bilateral 7th cr.Nr
D. > P.
proximal and distal
Diphteritic neuropathy
aetiology
Exotoxin of diphteria
C/P.
1- Localized type
Cr.Nr.3
2- Generalized type
ttt
I.M
4
10 (bulbar symptoms)
peripheral nerves mainly motor
anti - D serum 100.000 unit
see diphtheria
Leprotic neuropathy
Organism
C/P.
mycobacterium leprae
mono multiplex or poly neuropathy
ulnar n.
5th
7th
Thickening of the affected nerves
Mainly sensory (maculo - anaesthetic patches)
32
ttt
Dapsone
-
Rifampicin
Mono neuropathy
Causes:
12345-
Trauma
injection (sciatic nr.)
Infection
H. Z. - leprosy
Vascular
P.Ar.N.
Compression
Intrapment neuropathy
D.M.
Q Metabolic neuropathies
D.M
Hypothyroidism
Acromegally
Uraemia
Chronic liver failure
Porphyria
Q
Intrapment neuropathies :
Compression of the N. where they pass through narrow channels.
Common sites :
1- Median N.
2- Ulnar N.
carpal T.
elbow
3- Radial N.
humeral groove
4- Brachial plexus
5- Sciatic
thoracic outlet
Buttock
6- Lat. cutaneous nerve of thigh
7- Cervical & Lumbar roots
inguinal ligament
intervertebral discs
Q Carpal tunnel $
Median nerve compression under flexor retinaculum.
Causes
pregnancy
Rh. Arthritis
myxodema
acromegally
33
determination
Amyloidosis
Tinel’s Sign - Phalen’s test –
Diagnosis
of nerve conduction velocity
cause - decompression
ttt
Q
Brachial plexus lesions
Q
Toxic neuropathies
Q
Hereditary Neuropathies
upper plexus C5,6
Erb - duchenne
Lower plexus C8, T1
(klumpke)
thoracic outlet $
C8 ,T1
INH
Ethambutol
Gold - vineristine
Peroneal muscle atrophy
Amyloid polyneuropathy
Porphyric Neuropathy
Mitochondrial Neuropathy
Myopathies
Diseases of the skeletal muscles without the central or peripheral nervous
system involvement.
N.B.
If this muscle disease is degenerative and genetically
determined, It is termed muscular dystrophy
C/P. of muscular dystrophy :
age
1st
- 2nd decade, +ve
family history.
onset
gradual
course
progressive
Sympt.
Clumsy gait
Inability to climb the stairs
Inability to pick up objects from the ground
weakness of certain ms of the body for example
because these ms are
{ Shoulder, pelvic girdles &}
developed early
34
{ trunk , why !?
}
during (intrauterine life)
Signs
1- Weakness like of LMNL
Hypotonia, hyporeflexia
Wasting
Bilat., Symmetrical,
UL and LL, Pr.>D.
2- Esp. mms weakness
esp. manifest,
a. Winging of scapula
due to weakness of serratus anterior
& trapezius
b. Waddling gait
due to weakness of gluteus medius
c. Characteristic manner in getting up from floor
Gower’s
sign
d. Exaggerated lumbar lordosis
due to weakness of the
ms of trunk
e. Pot-belly abdomen
due to weakness of abdominal ms
3 - Selectivity of the involved ms
atrophy of sternal head of pectoralis
preservation of its
clavicular head
4- The fascial ms are weak in certain types
(fascio - scapulo - humeral type)
5- Psudohypertrophy in Duchenns type affecting
calf ms in L.L. & deltoid ms in U.L.
6- Later on
fibrosis & contractures of the affected ms
Key of myopathy case
Case purely motor
Bilat., Symmetrical, Pr.>D.
Hypotonia & hyporeflexia
No
sensory
fasciculation (to excludes motor N. disease)
sphincteric manifestations
Q
DD of Quadriplegia or Qquadriparesis
1- Cx. spondylosis
4 limbs showing signs
2- SCD
, P.C., P.N.
3- Pellagra
, P.N.
4- Friedreich’s ataxia
(, P.C., P.N., cerebellum)
5- Maries ataxia
(, cerebellum)
6- Myopathy
purely motor
7- Neuropathy
weak. D. > Pr.
+ Glove & stocking hypothesia
8- Motor N.D.
purely motor
35
fasiculation
Investigation
Creatine & Creatinine in urine
normally creatine is absent & creatinine is present in urine,
In myopathy creatine`l and appears in urine & creatinine
because the diseased ms cannot metabolise creatine to creatinine
CPK (especially with Duchenne)
EMG
Ms biopsy
ttt
no specific ttt
vitamines , tonics
physiotherapy
family counseling , DNA analysis allow early diagnosis and Gene
therapy
muscle fibres transplantation . !
36
Classification of Ms disease
Aetiological classification of myopathy
1- muscular dystrophy
2- Myotonia
3- Inflammatory
polymyalgia Rheumatica
polymyositis
4- Endocrinal
e.g. grave’s disease
5- Periodic paralysis
6- Drug induced
Clinical types of progressive ms dystrophies
onset
1- Shoulder girdls type ( UL > LL )
late childhood
a- Scapulo humeral type ( Erb’s
)
Autosomal R
&early adulthood
b- Fascioscapulo humeral (Landouzy and
Dejerine)
2- Pelvic girdle (LL > UL )
a- Pseudo hypertrophic
serve
Duchenne
eary
mild
Becker
childhood
b- Atrophic type ( Leyden - Mobius )
3- Rare types
Distal myopathy of Gower
Ocular type of myopathy
Oculopharyngeal type
Duchenne
1 decads
progressive
+ ve ECG changes
(cardiomyopathy)
death early
st
Causes of death in ms dystrophy :
Paralysis of respiratory muscle
Cardiomyopathy (in Duchenne)
Pneumonia
Causes of pseudo hypertrophy of ms
Duchenne
Becker
Becker
2 or 3rd decades
Slowly progressive
No ECG
nd
Normal life span
Autosomal
D
X- linked
37
Acromegally
Myxoedema
Myotonia congenita
Dystrophin
It is a protein in the muscles, whose absence allows calcium and
complement components to enter and destroy muscle fibres, It is
absent in Duchenne & abnormal in Becher’s
Inflammatory myopathies
a. Polymyositis
- Collagen disease
- ESR - CPK
- Weakness , tender ms
- good response to steroid
b. Polymyalgia Rheumatica
- Old female
- idiopathic
- ESR
- Steroid sensitive
- Pain & stiffness in neck, & shoulder
K
K
Q Endocrine myopathy
thyrotoxicosis
hypothyroidism
Addison - cushing $
hypoparathyroidism.
Familial periodic paralysis
- attacks of flaccid weakness often associated with or
K , many cases are familial
- there are two types :
a. Hypokalemic type :
Sudden attack of flaccid paralysis after
CHO diet
ttt
K Supplements
Restrict C.H.O
b. Hyperkalemic type :
More frequent
Respond to Ca inject.
Toxic myopathy (drugs
mus disorders)
Carbenoxolone
Alcohol thiazides
penicillamine
Steroids Vineristine
Congenital myopath
glycogen storage disease
38
phosphofructokinase
mitochondrial myopathies