Lecture Notes
advertisement

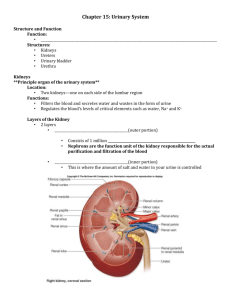
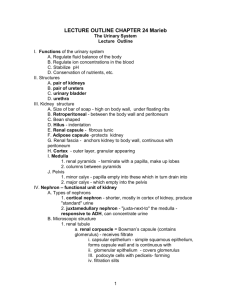
Chapter 23 The Urinary System Student Notes Urinary System Overview – details begin on page 2 Homeostatic functions Cleanse blood and maintain volume and blood pressure Maintain pH Stimulates calcitonin, renin and erythropoietin Components: Two kidneys, two ureters, one bladder, one urethra Kidneys: Location/surrounding structures Size and shape of kidneys Coverings of the kidneys Superficial Anatomy Sectional Anatomy Cortex, medulla, renal pyramids, remal papilla, renal columns, renal lobe, minor calyx and major calyx Histology of kidney Nephron – cortical and juxtamedullary Structural and functional unit of kidney approx. 1 million/kidney Glomerulus, tubules and collecting ducts Glomerulus – capsule which collects filtrate from capillary network Visceral and parietal layers. Visceral layer is made of podocytes which has slits for filtering Flow of filtrate – glomerulus – PCT – descending loop – loop of Henle – ascending loop- DCT – collecting duct – renal papilla – minor calyx – major calyx – ureter – bladder – urethra Flow of blood – renal artery – segmental a. – lobar a. – interlobar – arcuate – interlobular – afferent – glomerulus – efferent a. – peritubular cap and vasa recta – interlobular v. – arcuate v. – interlobar v. – renal v. – IVC Ureters Muscular, ~12 inches long, no valves, peristalsis, 3 layers, mucosa, muscularis, fibrous (outer connective t.) Urinary Bladder Hollow organ, held in place by peritoneum 4 layers: mucosa, middle, outer, serosa Micturation: voluntary and involuntary Capacity 700-800ml…at 400ml, stretch receptors tell your brain that it’s time Urethra Female 3 layers, mucous, with transitional epithelium near bladder then stratified squamous epithelium, intermediate layer containing veins, outer muscular layer continuous with urinary bladder Male 2 layers – inner mucous, outer mucosa 3 subdivisions – prosthetic urethra mucosa – 1. continuous with bladder, transitional epi 2. membranous urethra mucosa – pseudostratified columnar epithelium 3. Spongy urethra mucosa – mostly lined by pseudo, near external opening is stratified squamous I. Kidneys / functions: A. Kidneys cleanse the blood of many unnecessary or undesirable substances, such as __________________, while forming urine; purity and chemical constancy of the blood and other extracellular body fluids is maintained. They are the main homeostatic organ. The kidneys regulate blood _________________ and ____________________________ The kidneys help to regulate blood ____ The kidneys conserve _____________________ by preventing their ___________________ in the _____________ The kidneys stimulate the production of two hormones: __________________________- and _____________________________ B. Gross anatomy of the kidneys defines their location, external appearance, internal structure, and gross vasculature and nerve supply 1. Externally, kidneys appear red-brown and bean-shaped. 2. Kidneys lie retroperitoneally in the superior lumbar region between T12 and L3 The left kidney lies a bit lower than the right because it is crowded by the live. The kidneys are a paired organ but only one is necessary. They are approximately 5 inches high and 3 inches wide with a depth of less than 2 inches. The kidneys lie at an oblique angle to the frontal plane. 3. Internal gross anatomy of a kidney reveals two distinct regions, the cortex and the medulla 4. Gross vasculature of the kidneys involves the renal arteries, renal veins, and a complicated vascular pathway; the nerve supply of the kidney is supplied by the renal plexus. ( C. Microscopic anatomy reveals the uriniferous tubule as the main structural and functional unit of the kidney; the uriniferous tubule consists of a nephron and collecting tubule. 1. Mechanisms of urine production by the nephron involve three processes: filtration, reabsorption, and secretion. 2. The nephron is composed of the renal corpuscle and a tubular section consisting of the proximal convoluted tubule, loop of Henle, and distal convoluted tubule. i. The renal corpuscle (located in the cortex) is the site of filtration. ii. After forming in the renal corpuscle, the filtrate continues through the tubular section to join the collecting tubule; reabsorption and secretion occur along the way iii. There are two classes of nephrons: cortical nephrons and juxtamedullary nephrons. 3. Collecting tubules merge to form the papillae of the pyramids deep in the medulla, and now urine enters calices that merge to form the renal pelvis where urine enters the ureter. 4. Microscopic blood vessels associated with uriniferous tubules form two capillary beds: the glomeruli and the peritubular capillaries5. Vasa recta are capillary-like vessels around the loop of Henle. 6. The juxtaglomerular apparatus is a structure near the glomerulus that functions in the regulation of blood pressure. II. Ureters) A. Ureters are slender, retroperitoneal tubes of about 25 cm each. The ureters continue from the renal pelvis to enter the urinary bladder at an oblique angle. Microscopic anatomy of the ureter reveals walls composed of mucosa, muscularis, and adventitia. The epithelium of the mucosa is transitional epithelium. The muscularis of the ureter is unlike the digestive tract because the inner layer is longitudinal and the external layer is circular. The inferior one-third of the ureter contains an additional external layer of muscularis, which is longitudinal. III. Urinary Bladder A. The urinary bladder is a collapsible, muscular sac that stores and expels urine. It lies on the pelvic floor inferior to the peritoneal cavity. 1. An empty urinary bladder is shaped like an upside-down pyramid. At the anterior angle is a fibrous band called the urachus, which is the closed vestige of the allantois. 2. Arteries supplying the urinary bladder are branches of the internal iliac arteries. 3. The walls of the urinary bladder are composed of mucosa, a thick muscular layer, and adventitia. The epithelium of the mucosa is transitional epithelium. The muscular layer, called the detrusor muscle, is comprised of intermingled smooth muscle fibers arranged in inner and outer longitudinal layers and a middle circular layer. 4. A full adult urinary bladder can contain about 500 ml of urine. IV. Urethra (pp. 700–701, Fig. 23.16) A. The uretha is a thin-walled tube that drains urine from the urinary bladder and conveys it out of the body. B. In males, the smooth muscle layer of the urethra becomes very thin toward its distal end. The epithelium of the urethra in males changes from transitional epithelium to stratified and pseudostratified columnar, and finally stratified squamous epithelium at the urethra’s distal end. C. The internal urethral sphincter is a thickening of the detrusor muscle. This sphincter is an involuntary one, which prevents dribbling of urine between voiding. The external urethra sphincter is under voluntary control. D. The length and functions of the urethra differ in males and females. The female urethra is approximately 4 cm long, while in males the urethra is about 20 cm long. The male urethra has three named regions. From internal to external, the regions are prostatic urethra, membranous urethra, and spongy urethra E. Urinary Tract Infections Sexually transmitted, anal contamination Kidney stones (renal calculi) Cancer – may be caused by cigarette smoke, artificial sweeteners, industrial chemicals V. Micturition A. Micturition, also called urination or voiding, is the act of emptying the urinary bladder. VI. Disorders of the Urinary System A. Examples of disorders of the urinary tract are urinary tract infections, renal calculi, polycystic kidney disease, and cancer of urinary organs. B. Pyelonephritis – infection of kidney probably from fecal bacteria entering urethra and climbing upward, may also be blood-borne VII. Diagnostic radiology - pyelogram VIII. The Urinary System Throughout Life A. Three sets of kidneys develop in sequence in the embryo: pronephric, mesonephric, and metanephric. B. Kidneys of newborns cannot concentrate urine. (p. 706) C. Urinary infections are the most common problem through middle age; incontinence is a problem with the elderly.