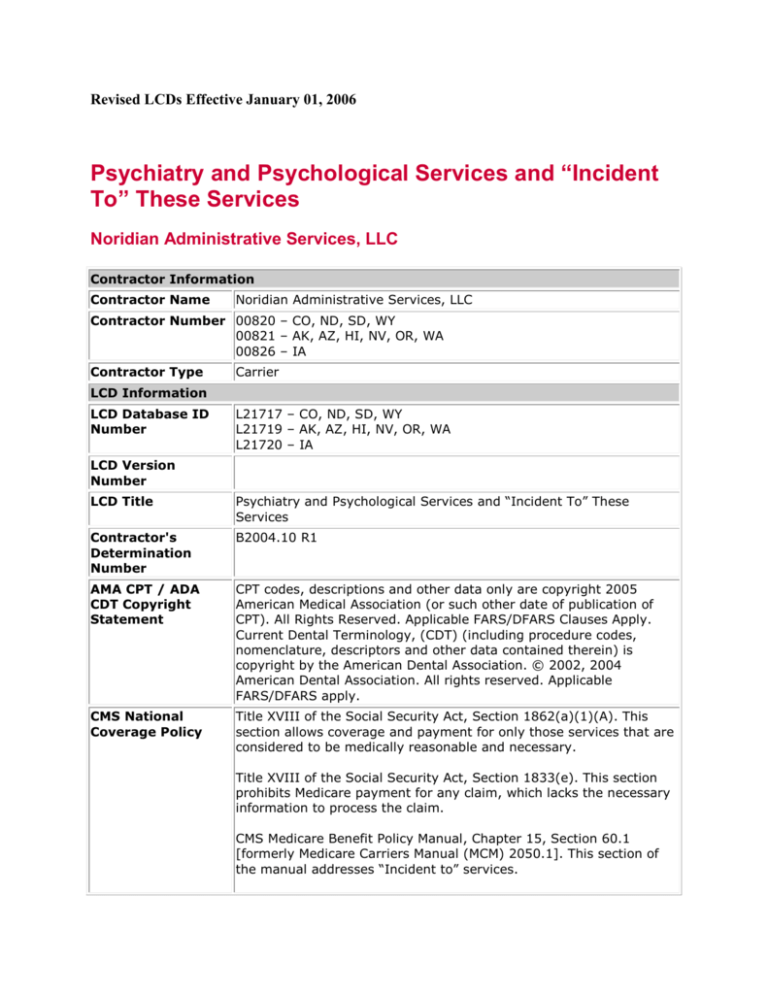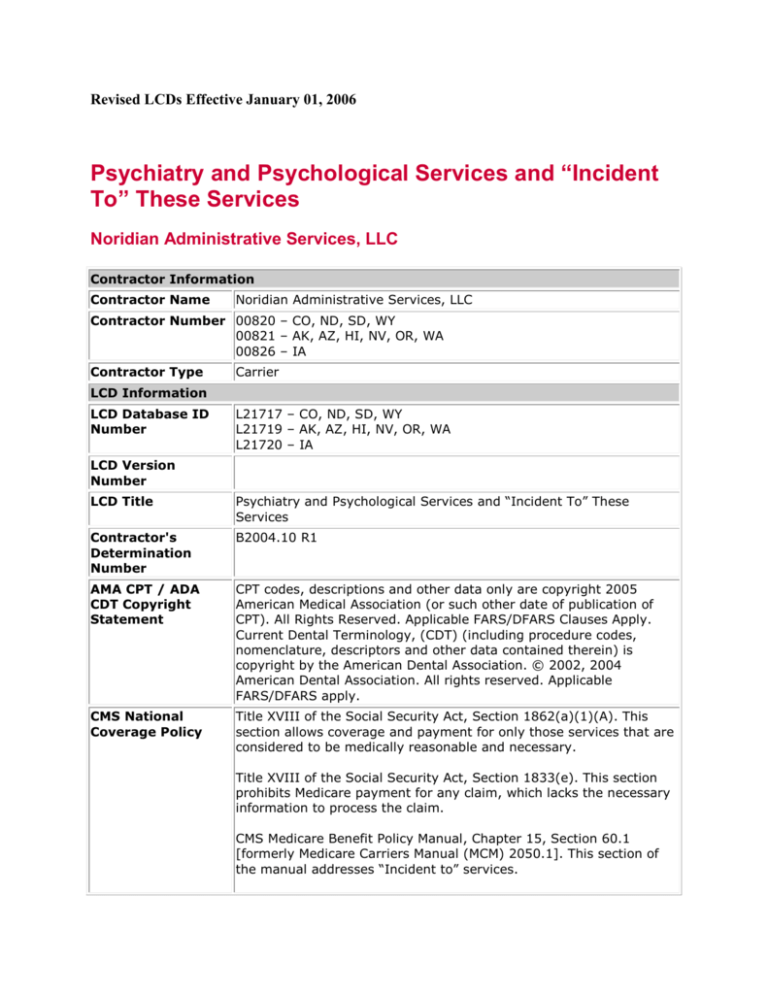
Revised LCDs Effective January 01, 2006
Psychiatry and Psychological Services and “Incident
To” These Services
Noridian Administrative Services, LLC
Contractor Information
Contractor Name
Noridian Administrative Services, LLC
Contractor Number 00820 – CO, ND, SD, WY
00821 – AK, AZ, HI, NV, OR, WA
00826 – IA
Contractor Type
Carrier
LCD Information
LCD Database ID
Number
L21717 – CO, ND, SD, WY
L21719 – AK, AZ, HI, NV, OR, WA
L21720 – IA
LCD Version
Number
LCD Title
Psychiatry and Psychological Services and “Incident To” These
Services
Contractor's
Determination
Number
B2004.10 R1
AMA CPT / ADA
CDT Copyright
Statement
CPT codes, descriptions and other data only are copyright 2005
American Medical Association (or such other date of publication of
CPT). All Rights Reserved. Applicable FARS/DFARS Clauses Apply.
Current Dental Terminology, (CDT) (including procedure codes,
nomenclature, descriptors and other data contained therein) is
copyright by the American Dental Association. © 2002, 2004
American Dental Association. All rights reserved. Applicable
FARS/DFARS apply.
CMS National
Coverage Policy
Title XVIII of the Social Security Act, Section 1862(a)(1)(A). This
section allows coverage and payment for only those services that are
considered to be medically reasonable and necessary.
Title XVIII of the Social Security Act, Section 1833(e). This section
prohibits Medicare payment for any claim, which lacks the necessary
information to process the claim.
CMS Medicare Benefit Policy Manual, Chapter 15, Section 60.1
[formerly Medicare Carriers Manual (MCM) 2050.1]. This section of
the manual addresses “Incident to” services.
CMS Medicare Benefit Policy Manual, Chapter 15, Section 80.2
[formerly Medicare Carriers Manual (MCM) 2070.2]. This section of
the manual addresses independent psychologists.
CMS Medicare National Coverage Determinations Manual, Chapter 1,
Part 1, Section 70.1 (formerly Medicare Coverage Issues Manual 3514).
Primary
Geographic
Jurisdiction
AK
AZ
CO
HI
IA
ND
NV
OR
SD
WA
WY
Oversight Region
Region X
CMS Consortium
Western
Original
Determination
Effective Date
For services performed on or after 12/31/2005
Original
Determination
Ending Date
Revision Effective
Date
For services performed on or after 01/01/2006
Revision Ending
Date
Indications and
Limitations of
Coverage and/or
Medical Necessity
Information in this part of the policy had been divided into six (6)
sections. These sections address each individual CPT/HCPCS
procedure code.
I. General Clinical Psychiatric Diagnostic or Evaluative Interview
Procedures
II. Special Clinical Psychiatric Diagnostic or Evaluative Procedures
III. Psychiatric Therapeutic Services
IV. Psychiatric Somatotherapy
V. Other Psychiatric Disorders
VI. Central Nervous System Assessments/Tests (e.g., NeuroCognitive, Mental Status, Speech Testing)
Section I: General Clinical Psychiatric Diagnostic or Evaluative
Interview Procedures:
Description: A psychiatric diagnostic interview examination
(90801) includes a history, mental status exam, and a disposition,
as well as ordering and medical interpretation of laboratory or other
medical diagnostic studies. The diagnostic interview may include
communication with family or other sources, and in certain
circumstances, other informants will be seen in lieu of the patient.
The psychiatrist obtains a complete medical and psychiatric history
from the patient and/or family and establishes a tentative diagnosis.
The patient's capacity to work psychotherapeutically is also evaluated
to determine how willing he or she is to work toward a positive
solution to the problem. The patient's condition determines the
extent of the mental status examination during the diagnostic
interview. The psychiatrist is looking for symptoms of
psychopathology in the patient's general appearance, attitude toward
the examiner, and overall behavior. In addition, the speech and
stream of talk, emotional reaction and mood, perception and thought
content, and cognition may be evaluated.
An evaluation and management (E/M) service may be substituted for
the initial interview procedure, including consultation codes
(CPT99241-99255), provided all required elements of the E/M service
billed are fulfilled. Consultation services require, in addition to the
interview and examination, providing a written opinion and/or advice.
They do not include psychiatric treatment, though such treatment
may be initiated on the same day as the consultation.
A psychiatric diagnostic interview examination is usually covered
once, when a provider first sees a patient for a suspected or
diagnosed psychiatric illness. It may be utilized again for the same
patient if a new episode of illness occurs or is thought to have
occurred, or on admission, or re-admission to inpatient status due to
complications of the underlying condition. If the provider is unable to
perform the psychiatric diagnostic interview examination at the initial
encounter because of the patient's mental or physical condition, a
code should be selected for the initial encounter based specifically on
what services/procedures the psychiatrist did perform or provide. If,
after completing an assessment it is concluded that no mental illness
is present, the visit may be coded with ICD-9-CM V71.09
(Observation for suspected mental condition - Other suspected
mental condition).
Section II: Special Clinical Psychiatric Diagnostic or
Evaluative interview examination.
Description: The interactive psychiatric diagnostic interview
examination (90802) is typically furnished to children. It involves
the use of physical aids and non-verbal communication to overcome
barriers to therapeutic interaction between the clinician and a patient
who has not yet developed, or has lost, either the expressive
language communication skills to explain his/her symptoms and
response to treatment, or the receptive communication skills to
understand the clinician if he/she were to use ordinary adult
language for communication. This code may also be used for the
initial evaluation of patients whose ability to communicate is impaired
by an expressive or receptive language impairment.
The Interactive Psychiatric Diagnostic Interview Examination
(90802) includes the same components as the Psychiatric Diagnosis
Interview Examination, which includes history, mental status,
disposition, and other components as indicated. However, in the
interactive examination, the physician uses inanimate objects, such
as toys and dolls for a child, physical aids and non-verbal
communication to overcome barriers to therapeutic interaction, or an
interpreter for a deaf person or one who does not speak English.
Documentation: The medial record must indicate that the person
being evaluated does not have the ability to interact through normal
verbal communicative channels. If the patient is incapable of
communication by any means this code may not be billed.
Section III: Psychiatric Therapeutic Procedures
Description: Procedure code 90865 (Narcosynthesis for
psychiatric diagnostic and therapeutic purposes [e.g., sodium
amobarbital {Amytal} interview]) is used for the administration of
sedative or tranquilizer drugs, usually intravenously, to relax the
patient and remove inhibitions for discussion of subjects difficult for
the patient to discuss freely in the fully conscious state.
Use of code 90865 is restricted to physicians.
Documentation: The medical record should document the medical
necessity of this procedure, i.e., the patient had difficulty verbalizing
about psychiatric problems without the aid of the drug. The record
should also document the specific pharmacological agent, dose and
route of administration, and whether the technique was effective or
non-effective.
Description: Procedures 90804 through 90829
Psychotherapy is defined in CPT as “the treatment for mental illness
and behavioral disturbances in which the physician establishes a
professional contract with the patient and, through definitive
therapeutic communication, attempts to alleviate the emotional
disturbances, reverse or change maladaptive patterns of behavior,
and encourage personality growth and development.”
Behavior modification is not a separate service specifically, but rather
an adjunctive measure in psychotherapy. It is not expected to be a
frequent or ongoing service, but may need to be repeated at
reasonable intervals to aid the individual, the family, and the staff in
managing the manifestations of the patient’s mental illness.
These covered services may be performed only by a person
authorized by the state to perform psychotherapy services. Medicare
coverage of procedure codes 90804-90829 does not include teaching
grooming skills, monitoring activities of daily living, recreational
therapy (dance, art, play) or social interaction, therefore, procedure
codes 90804-90829 should not be used to bill for ADL training and/or
social interaction skills.
Note: Procedure codes 90805, 90807, 90809, 90811, 90813,
90815, 90817, 90819, 90822, 90824, 90827, and 90829
include medical evaluation and management (E/M) services
which include continuing medical diagnostic evaluation as
well as pharmacologic management. Therefore,
pharmacologic management (90862) and E/M service codes
may not be billed separately on the same day as a
psychotherapy service by the same physician.
Guidelines For Procedure Codes 90804-90829:
1. Individual psychotherapy codes should be used only when the
focus of the treatment encounter involves psychotherapy.
Psychotherapy codes should not be used as generic psychiatric
service codes when another code, such as an E/M or pharmacologic
management code, would be more appropriate.
2. Prolonged treatment must be medically necessary and may be
subject to medical review. Documentation must be present in the
medical record indicating the necessity for an extended number of
treatment visits.
3. Procedure codes 90808, 90809, 90814, 90815, 90821, 90822,
90828, and 90829 (approximately 75-80 minutes) should not be
routinely used. They are reserved for exceptional circumstances. The
provider must document in the patient’s medical record the medical
necessity of these services and define the exceptional circumstances.
4. Medicare will not accept psychiatric therapy procedure codes
90804-90829 being billed on the same date of service as an
evaluation and management (E/M) service, by the same physician or
mental health profession group. The single exception is that a
consultation may be billed at the initial visit, and, in addition,
psychotherapy codes which do not include medical evaluation and
management services (90804, 90806, 90808, 90810, 90812, 90814,
90816, 90818, 90821, 90823, 90826, 90828) may be billed on the
same date of service, if such services are medically indicated and
performed.
5. Psychotherapy services are not covered when documentation
indicates that Dementia (ICD-9-CM codes 290.0, 290.20-290.9,
331.0-331.2) has produced a severe enough cognitive defect to
prevent psychotherapy to be effective. Severe and profound
mental retardation (ICD-9-CM codes 318.1 and 318.2) are
never covered for psychotherapy services. In such cases,
rehabilitative, evaluation and management (E/M) codes or
pharmacologic management codes should be reported.
6. For psychotherapy sessions lasting longer than 90 minutes, use
CPT code 90899 with a description in Item 19 of the CMS-1500 claim
form or electronic equivalent. When requested, please send Medicare
a copy of the patient’s medical record, documenting the face-to-face
time spent with the patient and the medical necessity for the
extended time.
7. These codes should not be used as generic psychiatric service
codes when other codes such as an Evaluation & Management
service or pharmacologic codes would be more appropriate.
8. When CPT codes 90804-90829 are performed by a physician, CPT
code 90862 is not a separate or additional benefit, but is included in
the psychotherapy codes
Description: Psychoanalysis (90845) refers to the use of
investigative techniques to gain insight into a person's unconscious
motivations, conflicts, and symbols to effect a change in maladaptive
behavior. This code refers to the practice of psychoanalysis and
should not be confused with or used for psychotherapy.
90845 is not time related, but is billed once for each necessary daily
session regardless of the time involved. In the rare circumstance
where psychoanalysis is used for a psychosis, the record must
document the necessity in terms of expected outcome in contrast
with other available therapeutic options.
Description: Procedure codes 90846, 90847, 90849 are used
for Family Therapy, a specialized therapeutic technique for treating
the identified patient’s mental illness by intervening in a family
system in such a way as to modify the family structure, dynamics
and interactions which exert influence on the patient’s emotions and
behavior. Family sessions are conducted face to face with family
members, with (90847) or without (90846) the patient present. Code
90849 is intended for group therapy sessions for multiple families
when similar dynamics are occurring due to a commonality of
problems in the family members under treatment.
Comments: The CMS Medicare National Coverage Determinations
Manual, Chapter 1, Part 1, Section 70.1 (formerly Medicare Coverage
Issues Manual 35-14), states that family psychotherapy services are
covered only where the primary purpose of such psychotherapy is
the treatment of the patient’s condition. Examples are as follows:
1. When there is a need to observe and correct, through
psychotherapeutic techniques, the patient’s interaction with family
members (CPT 90847).
2. Where there is a need to assess the conflicts or impediments
within the family, and assist through psychotherapy, the family
members in the management of the patient (90846 or 90847).
Procedure codes 90846-90847 represent psychotherapy services for
treatment of mental disorders. They should not be used to code
taking a family history or E/M counseling services. Further, 90846,
family psychotherapy without the patient present, should rarely be
billed and, when provided, must always be directed towards the
patient’s condition, not the family’s problems with the patient.
Code 90849 has restrictive coverage by Medicare and would
generally be non-covered. Such group therapy is directed to the
effects of the patients’ condition on the family, and does not meet
Medicare’s standards of being part of the physician’s personal
services to the patient. If such is not the case, individual
consideration may be given if documentation is submitted.
Description: Psychotherapy administered in a group setting
(90853) with a trained group leader in charge of several
patients. The psychotherapy process may be conducted with several
patients in a group setting. The personal dynamics of an individual
may be discussed by the group and the dynamics of the group may
be explored at the same time. Interpersonal interactions, support,
emotional catharsis, and reminiscing are other examples of the
processes explored in group settings.
Comments: Group therapy, since it involves psychotherapy, must
be led by a person who is authorized by state statute to perform this
service. This will usually mean a psychiatrist, psychologist, or clinical
social worker or, in some states, certified nurse practitioner, clinical
nurse practitioner, clinical nurse specialist, or qualified mental health
specialist. For Medicare Part B coverage, group therapy does not
include socialization, music therapy, recreational activities, art
classes, excursions, sensory stimulation or eating together, cognitive
stimulation, motion therapy, etc.
Description: Codes 90810-90815, 90823-90829 and 90857 are
used when the patient, or patients in the group setting, does not
have the ability to interact by ordinary verbal communication
therefore non-verbal communication skills are employed, or an
interpreter may be necessary. The guidelines in the Description,
Documentation, and Comments sections under CPT 90802 apply to
codes 90810-90815, 90823-90829, and 90857.
Comments: Codes 90810-90815 and 90823-90829 should not be
billed on the same dates of service as codes 90804-90809 or 9081690822. Code 90857 should not be billed on the same date of service
as 90853.
Section IV: Psychiatric Somatotherapy
Code 90862 is addressed in a separate LCD and will not be
discussed further in this policy.
Description: Code 90870 (Electroconvulsive therapy includes
necessary monitoring) is used for the application of electric current to
the brain, through scalp electrodes to produce a seizure.
When the psychiatrist administers the anesthesia for the
electroconvulsive seizure therapy, no separate payment may be
made for that service.
Section V: Other Psychiatric Therapy
Description: Codes 90875 and 90876 are used for individual
psychophysiological therapy incorporating biofeedback training by
any modality (face-to-face with the patient), with psychotherapy
(e.g., insight oriented, behavior modifying or supportive
psychotherapy); for approximately 20-30 minutes (90875) or
approximately 45-50 minutes (90876).
Medicare does not cover biofeedback for the treatment of psychiatric
disorders. Therefore, CPT codes 90875 and 90876 will always be
denied as NONCOVERED.
Description: Code 90880 (hypnotherapy) is a treatment that
makes use of an artificially induced alteration of consciousness
characterized by increased suggestibility and receptivity to direction.
It may be used for diagnostic purposes or for therapeutic purposes.
If hypnotherapy is provided with psychotherapy, only 90880 is
reported for that session.
When used therapeutically to enhance psychotherapy or provided in
conjunction with psychotherapy in the same session, only code
90880 or the psychotherapy code should be reported.
Note: Code 90882, environmental intervention for medical
management purposes on a psychiatric patient’s behalf with
agencies, employers, or institutions is NONCOVERED by Medicare.
Description: Code 90885 is used for evaluation of hospital records,
reports, tests and other data for medical diagnostic purposes. 90885
is considered to be a bundled service as a part of other codes and is
not separately payable by Medicare.
Description: Code 90887 is used when the treatment of the patient
may require explanations to the family, employers, or other involved
persons for their support in the therapy process. This may include
reporting of examinations, procedures and other accumulated data.
Code 90887 is considered to be a bundled service as a part of other
codes and is not separately payable by Medicare.
Description: Code 90889 involves preparation of reports for
insurance companies, agencies, courts, etc. Code 90889 is
considered to be a bundled service as a part of other codes and is
not separately payable by Medicare.
Section VI: Central Nervous System Assessments/Tests (e.g.,
Neuro-Cognitive, Mental Status, Speech Testing)
Codes 96101-96120 are used to report the services provided during
testing of the cognitive function of the central nervous system. The
testing of cognitive processes, visual motor responses, and
abstractive abilities is accomplished by the combination of several
types of testing procedures. It is expected that the administration of
these tests will generate material that will be formulated into a
report.
Developmental testing (96110 and 96111) is generally used for the
evaluation of children.
Central Nervous System Assessments/Tests are not
psychotherapeutic modalities, but rather diagnostic aids. Use of such
tests when mental illness is not suspected would be a screening
procedure and is not covered by Medicare. Each test performed must
be medically necessary and therefore standardized batteries of tests
are not acceptable. The Folstein Mini-Mental Exam and similar brief
mental status exams are not separately reimbursable by Medicare
and are included in the clinical interview or E/M service.
Changes in mental illness may require psychological testing to
determine new diagnoses or the need for changes in therapeutic
measure. Repeat testing not required for a diagnosis or continued
treatment would be considered medically unnecessary. Nonspecific
behaviors, which do not indicate the presence of, or change in, a
mental illness would not be an acceptable indication for testing.
Psychological or psychiatric evaluations that can be accomplished
through the clinical interview alone (e.g., response to medication)
would not require psychological testing, and such testing would be
considered medically unnecessary. Adjustment reactions or dysphoria
associated with moving to a nursing facility, do not constitute
medical necessity for psychological testing.
These codes should not be reported by the treating psychiatrist for
reading the report of the results of these tests. Reading of the report
is included in the office time, or floor time in the hospital, and would
be bundled into the payment for other services.
The independent psychologist (Specialty Code 62) is not a clinical
psychologist (Specialty Code 68), does not do psychotherapy and
practices independently of an institution, agency or physician’s
office….” [CMS Medicare Benefit Policy Manual, Chapter 15, Section
80.2 (formerly MCM 2070.2).] He or she performs the psychological
tests and interprets them.
Codes 96118-96120 are used for neuropsychological testing
intended to diagnose and characterize the neurocognitive effects of
medical disorders that impinge directly or indirectly on the brain.
Examples of problems which might lead to neuropsychological testing
are:
1. Detection of neurologic diseases that may result from mild head
injury, anoxic injuries, AIDS, and other diseases that may affect the
brain.
2. Differential diagnosis between psychogenic and neurogenic
syndromes;
3. Delineation of the neurocognitive effects of CNS disorders;
4. Neurocognitive monitoring of recovery or progression of CNS
disorders; and,
5. Assessment of neurocognitive functions for the formulation of
rehabilitation and/or management strategies among individuals with
neurologic disorders.
The content of neuropsychological testing procedures differs in a
large part from that of psychological testing (96101-96103) in that
neuropsychological testing consists primarily of individually
administered ability tests that comprehensively sample ability
domains that are known to be sensitive to the functional integrity of
the brain (e.g., abstraction, memory and learning, attention,
language, problem solving, sensorimotor functions, constructional
praxis, etc.). These procedures are objective and quantitative in
nature and require the patients to directly demonstrate their level of
competence in a particular cognitive domain. Neuropsychological
testing does not rely on self-report questionnaires such as the
Minnesota Multiphasic Personality Inventory 2 (MMPI-2), rating
scales such as the Hamilton Depression Rating Scale, or projective
techniques such as the Rorschach or Thematic Apperception Test
(TAT). These procedures are psychological tests. Brief screening
measures such as the Folstein Mini Mental Status Exam or use of
other mental status exams in isolation should not be reported
separately as neuropsychological Testing since they are typically part
of a more general clinical exam or interview.
Typically, the test battery will require from 5-7 hours to perform,
including administration, scoring and interpretation. If the testing is
done over several days, the testing time should be combined and
reported all on the last date of service. The medical record must
clearly evidence the clinical need for specific testing and (where
appropriate) its extent. For codes where the interpretation and report
preparation are time-dependent, the record must also evidence this
time and its necessity.
ALL Psychiatry and Psychological Services:
Medicare requires that all covered services and treatment are
expected to improve the health status or function of the patient. If
there is significant reason to doubt the patient’s ability to participate
in and to benefit from the service, then this issue must be explicitly
addressed in the medical record.
The medical record should also document the target symptoms, the
goals of therapy, methods of monitoring outcome, and estimated
duration of treatment in terms of number of sessions. It should
document why the chosen therapy is the appropriate treatment
modality either in lieu of or in addition to another form of psychiatric
treatment.
These codes should not be used as generic psychiatric service codes
when other codes such as an Evaluation & Management service or
pharmacologic codes would be more appropriate.
”Incident To” Services:
”Incident to a physician’s professional services means that the
services or supplies are furnished as an integral, although incidental,
part of the physician’s personal professional services in the course of
diagnosis or treatment of an injury or illness.” [CMS Medicare Benefit
Policy Manual, Chapter 15, Section 60.1 (MCM 2050.1).]
The “incident to” provision also applies to coverage for psychological
services furnished “incident to” the professional services of certain
non-physician practitioners (Clinical Psychologists, Clinical Nurse
Specialists, and Nurse Practitioners). The training requirements and
state licensure or authorization of individuals who perform
psychological services are intended to ensure an adequate level of
expertise in the cognitive skills required for the performance of
diagnostic and therapeutic psychological services. Therefore, only the
types of individuals listed below are considered qualified to perform
medically necessary psychological services as “incident to” services.
Delegation of diagnostic and therapeutic psychological services to
personnel not performing within the Scope of Practice as authorized
by state law, under the “incident to” provision, would bypass the
safeguards afforded by professional credentialing and state licensure
requirements. Such delegated services under the “incident to”
provision would be inappropriate, unreasonable and medically
unnecessary, and therefore, not covered by Medicare.
Only the following types of individuals, when they are performing
within their authorized scope of clinical practice under the state law
where the service is performed, are qualified to perform the indicated
diagnostic and/or therapeutic psychological services under the
“incident to” provision:
1. Doctorate level psychologists (Specialty Code 68): 90801, 90802,
90804, 90806, 90808, 90810, 90812, 90814, 90816, 90818, 90821,
90823, 90826, 90828, 90845, 90846, 90847, 90849, 90853, 90857,
90880, 90899
2. Doctorate or Masters level social workers (Specialty Code 80):
90801, 90802, 90804, 90806, 90808, 90810, 90812, 90814, 90816,
90818, 90821, 90823, 90826, 90828, 90846, 90847, 90849, 90853,
90857, 90899
3. Nurse Practitioners (NPs) (Specialty Code 50): 90801, 90802,
90804, 90806, 90808, 90810, 90812, 90814, 90816, 90818, 90821,
90823, 90826, 90828, 90846, 90847, 90849, 90853, 90857, 90880,
90899, (Also, if authorized by the state to prescribe medication:
90862, 90805, 90807, 90809, 90811, 90813, 90815, 90817, 90819,
90822, 90824, 90827, 90829)
4. Clinical Nurse Specialists (CNSs) (Specialty Code 89): 90801,
90802, 90804, 90806, 90808, 90810, 90812, 90814, 90816, 90818,
90821, 90823, 90826, 90828, 90846, 90847, 90849, 90853, 90857,
90880, 90899, (Also, if authorized by the state to prescribe
medication: 90862, 90805, 90807, 90809, 90811, 90813, 90815,
90817, 90819, 90822, 90824, 90827, 90829)
5. Other psychotherapists licensed by the state to perform
psychotherapy, e.g., licensed marriage and family therapists: 90804,
90806, 90808, 90810, 90812, 90814, 90846, 90847, 90849, 90857,
90880, 90899)
The psychological services referenced in the above CPT codes may be
delegated only to employees who qualify for one of the five
categories of individuals listed above. For example, a psychiatrist
may hire a social worker to perform services “incident to,” but the
services the social worker may perform must be limited to the
services designated by the CPT codes listed in number 2 above.
Individuals who are performing services “incident to” a qualified
Medicare practitioner are not required to be separately enrolled as an
independent practitioner in Medicare. Also, it is not appropriate for
the billing provider to hire and supervise a professional whose scope
of practice is outside the provider’s own scope of practice as
authorized under State law, or whose professional qualifications
exceed those of the “supervising” provider. For example, a certified
nurse midwife (CNMW) may not hire a psychologist and bill for that
psychologist’s services under the “incident to” provision, because a
psychologist’s services are not integral to a CNMW’s personal
professional services and are not regularly included in the CNMW’s
bill. Even though sections 1861(s)(2)(L) and 1861(gg) of the Social
Security Act authorize coverage for services furnished “incident to” a
CNMW’s services, psychological services are not commonly furnished
in CNMW’s offices nor within their scope of practice. Similarly, even
though section 1861(s)(2)(K)(iv) authorizes coverage for services
furnished “incident to” a physician assistant’s services, a physician
assistant would not be qualified to supervise psychological services
performed by the types of individuals listed above.
Note: In the “Medicare B News,” Issue 204, pages 17-19, Noridian
published in its entirety the CMS Program Memorandum Transmittal
AB-03-037. This document concerns payment for Part B mental
health services. Providers should consider this for the rule
concerning:
1) Qualifications for providers,
2) Definitions of “incident to,” “reasonable and necessary” and
“reasonable expectation of improvement” and
3) Documentation requirements.
Further, CMS subsequently published Medlearn Matters Number:
SE0441, “’Incident to’ Services”.
This LCD serves, accordingly, as an adjunct to these transmittals,
which are national CMS rules.
Coverage Topic
Doctor Office Visits
Mental Health Care (Inpatient)
Non-Physician Health Care Provider Services
Mental Health Care (Outpatient)
Mental Health Care (Partial Hospitalization)
Coding Information
Bill Type Codes
999x
Revenue Codes
99999
CPT/HCPCS Codes
Please note:
CPT codes 96101, 96102, 96103,96116, 96118, 96119, 96120 are
new codes for 2006 and are addressed in this policy.
Not Applicable
Not Applicable
90875, 90876 & 90882 are not a benefit under Medicare.
90885, 90887 & 90889 are each bundled services under Medicare
and not separately payable.
Note: Procedure codes 90862 and M0064 are addressed in the
Noridian Psychiatric Pharmacotherapy Policy (Number B2003.08)
located on the Noridian Medicare B Web site at
www.noridianmedicare.com
90801
Psy dx interview
90802
Intac psy dx interview
90804
Psytx, office, 20-30 min
90805
Psytx, off, 20-30 min w/e&m
90806
Psytx, off, 45-50 min
90807
Psytx, off, 45-50 min w/e&m
90808
Psytx, office, 75-80 min
90809
Psytx, off, 75-80, w/e&m
90810
Intac psytx, off, 20-30 min
90811
Intac psytx, 20-30, w/e&m
90812
Intac psytx, off, 45-50 min
90813
Intac psytx, 45-50 min w/e&m
90814
Intac psytx, off, 75-80 min
90815
Intac psytx, 75-80 w/e&m
90816
Psytx, hosp, 20-30 min
90817
Psytx, hosp, 20-30 min w/e&m
90818
Psytx, hosp, 45-50 min
90819
Psytx, hosp, 45-50 min w/e&m
90821
Psytx, hosp, 75-80 min
90822
Psytx, hosp, 75-80 min w/e&m
90823
Intac psytx, hosp, 20-30 min
90824
Intac psytx, hsp 20-30 w/e&m
90826
Intac psytx, hosp, 45-50 min
90827
Intac psytx, hsp 45-50 w/e&m
90828
Intac psytx, hosp, 75-80 min
90829
Intac psytx, hsp 75-80 w/e&m
90845
Psychoanalysis
90846
Family psytx w/o patient
90847
Family psytx w/patient
90849
Multiple family group psytx
90853
Group psychotherapy
90857
Intac group psytx
90865
Narcosynthesis
90870
Electroconvulsive therapy
90875
Psychophysiological therapy
90876
Psychophysiological therapy
90880
Hypnotherapy
90882
Environmental manipulation
90885
Psy evaluation of records
90887
Consultation with family
90889
Preparation of report
90899
Psychiatric service/therapy
96101
Psycho testing by psych/phys
96102
Psycho testing by technician
96103
Psycho testing admin by comp
Does the CPT 30%
Coding Rule
Apply?
ICD-9 Codes that
Support Medical
Necessity
96105
Assessment of aphasia
96110
Developmental test, lim
96111
Developmental test, extend
96116
Neurobehavioral status exam
96118
Neuropsych tst by psych/phys
96119
Neuropsych testing by tech
96120
Neuropsych tst admin w/comp
Yes
Note: Diagnosis codes are based on the current ICD-9-CM codes
that are effective at the time of LCD publication. Any updates to
ICD-9-CM codes will be reviewed by NAS; and coverage should not
be presumed until the results of such review have been
published/posted.
The following list of covered ICD-9 and DSM IV diagnosis codes
must be linked to the appropriate procedure before consideration
for Medicare payment may be made. These are the only covered
ICD-9-CM codes:
290.11 PRESENILE DEMENTIA WITH DELIRIUM
290.12 PRESENILE DEMENTIA WITH DELUSIONAL FEATURES
290.13 PRESENILE DEMENTIA WITH DEPRESSIVE FEATURES
290.20 SENILE DEMENTIA WITH DELUSIONAL FEATURES
290.21 SENILE DEMENTIA WITH DEPRESSIVE FEATURES
290.3
SENILE DEMENTIA WITH DELIRIUM
290.41 VASCULAR DEMENTIA, WITH DELIRIUM
290.42 VASCULAR DEMENTIA, WITH DELUSIONS
290.43 VASCULAR DEMENTIA, WITH DEPRESSED MOOD
291.0
ALCOHOL WITHDRAWAL DELIRIUM
291.1
ALCOHOL-INDUCED PERSISTING AMNESTIC DISORDER
291.2
ALCOHOL-INDUCED PERSISTING DEMENTIA
291.3
ALCOHOL-INDUCED PSYCHOTIC DISORDER WITH
HALLUCINATIONS
291.5
ALCOHOL-INDUCED PSYCHOTIC DISORDER WITH
DELUSIONS
291.81 ALCOHOL WITHDRAWAL
291.89 OTHER SPECIFIED ALCOHOL-INDUCED MENTAL
DISORDERS
291.9
UNSPECIFIED ALCOHOL-INDUCED MENTAL DISORDERS
292.0
DRUG WITHDRAWAL
292.11 DRUG-INDUCED PSYCHOTIC DISORDER WITH
DELUSIONS
292.12 DRUG-INDUCED PSYCHOTIC DISORDER WITH
HALLUCINATIONS
292.2
PATHOLOGICAL DRUG INTOXICATION
292.81 DRUG-INDUCED DELIRIUM
292.82 DRUG-INDUCED PERSISTING DEMENTIA
292.83 DRUG-INDUCED PERSISTING AMNESTIC DISORDER
292.84 DRUG-INDUCED MOOD DISORDER
292.85 DRUG INDUCED SLEEP DISORDERS
292.89 OTHER SPECIFIED DRUG-INDUCED MENTAL DISORDERS
292.9
UNSPECIFIED DRUG-INDUCED MENTAL DISORDER
293.0
DELIRIUM DUE TO CONDITIONS CLASSIFIED
ELSEWHERE
293.1
SUBACUTE DELIRIUM
293.81 PSYCHOTIC DISORDER WITH DELUSIONS IN
CONDITIONS CLASSIFIED ELSEWHERE
293.82 PSYCHOTIC DISORDER WITH HALLUCINATIONS IN
CONDITIONS CLASSIFIED ELSEWHERE
293.83 MOOD DISORDER IN CONDITIONS CLASSIFIED
ELSEWHERE
293.84 ANXIETY DISORDER IN CONDITIONS CLASSIFIED
ELSEWHERE
293.89 OTHER SPECIFIED TRANSIENT MENTAL DISORDERS DUE
TO CONDITIONS CLASSIFIED ELSEWHERE, OTHER
293.9
UNSPECIFIED TRANSIENT MENTAL DISORDER IN
CONDITIONS CLASSIFIED ELSEWHERE
294.0
AMNESTIC DISORDER IN CONDITIONS CLASSIFIED
ELSEWHERE
294.10 DEMENTIA IN CONDITIONS CLASSIFIED ELSEWHERE
WITHOUT BEHAVIORAL DISTURBANCE
294.11 DEMENTIA IN CONDITIONS CLASSIFIED ELSEWHERE
WITH BEHAVIORAL DISTURBANCE
294.8
OTHER PERSISTENT MENTAL DISORDERS DUE TO
CONDITIONS CLASSIFIED ELSEWHERE
294.9
UNSPECIFIED PERSISTENT MENTAL DISORDERS DUE TO
CONDITIONS CLASSIFIED ELSEWHERE
295.00 SIMPLE TYPE SCHIZOPHRENIA UNSPECIFIED STATE
295.01 SIMPLE TYPE SCHIZOPHRENIA SUBCHRONIC STATE
295.10 DISORGANIZED TYPE SCHIZOPHRENIA UNSPECIFIED
STATE
295.11 DISORGANIZED TYPE SCHIZOPHRENIA SUBCHRONIC
STATE
295.20 CATATONIC TYPE SCHIZOPHRENIA UNSPECIFIED STATE
295.21 CATATONIC TYPE SCHIZOPHRENIA SUBCHRONIC STATE
295.30 PARANOID TYPE SCHIZOPHRENIA UNSPECIFIED STATE
295.31 PARANOID TYPE SCHIZOPHRENIA SUBCHRONIC STATE
295.40 SCHIZOPHRENIFORM DISORDER, UNSPECIFIED
295.41 SCHIZOPHRENIFORM DISORDER, SUBCHRONIC
295.50 LATENT SCHIZOPHRENIA UNSPECIFIED STATE
295.51 LATENT SCHIZOPHRENIA SUBCHRONIC STATE
295.60 SCHIZOPHRENIC DISORDERS, RESIDUAL TYPE,
UNSPECIFIED
295.61 SCHIZOPHRENIC DISORDERS, RESIDUAL TYPE,
SUBCHRONIC
295.70 SCHIZOAFFECTIVE DISORDER, UNSPECIFIED
295.71 SCHIZOAFFECTIVE DISORDER, SUBCHRONIC
295.80 OTHER SPECIFIED TYPES OF SCHIZOPHRENIA
UNSPECIFIED STATE
295.81 OTHER SPECIFIED TYPES OF SCHIZOPHRENIA
SUBCHRONIC STATE
295.90 UNSPECIFIED TYPE SCHIZOPHRENIA UNSPECIFIED
STATE
295.91 UNSPECIFIED TYPE SCHIZOPHRENIA SUBCHRONIC
STATE
296.00 BIPOLAR I DISORDER, SINGLE MANIC EPISODE,
UNSPECIFIED
296.01 BIPOLAR I DISORDER, SINGLE MANIC EPISODE, MILD
296.02 BIPOLAR I DISORDER, SINGLE MANIC EPISODE,
MODERATE
296.03 BIPOLAR I DISORDER, SINGLE MANIC EPISODE, SEVERE,
WITHOUT MENTION OF PSYCHOTIC BEHAVIOR
296.04 BIPOLAR I DISORDER, SINGLE MANIC EPISODE, SEVERE,
SPECIFIED AS WITH PSYCHOTIC BEHAVIOR
296.05 BIPOLAR I DISORDER, SINGLE MANIC EPISODE, IN
PARTIAL OR UNSPECIFIED REMISSION
296.06 BIPOLAR I DISORDER, SINGLE MANIC EPISODE, IN FULL
REMISSION
296.10 MANIC AFFECTIVE DISORDER RECURRENT EPISODE
UNSPECIFIED DEGREE
296.11 MANIC AFFECTIVE DISORDER RECURRENT EPISODE
MILD DEGREE
296.12 MANIC AFFECTIVE DISORDER RECURRENT EPISODE
MODERATE DEGREE
296.13 MANIC AFFECTIVE DISORDER RECURRENT EPISODE
SEVERE DEGREE WITHOUT PSYCHOTIC BEHAVIOR
296.14 MANIC AFFECTIVE DISORDER RECURRENT EPISODE
SEVERE DEGREE SPECIFIED AS WITH PSYCHOTIC
BEHAVIOR
296.15 MANIC AFFECTIVE DISORDER RECURRENT EPISODE IN
PARTIAL OR UNSPECIFIED REMISSION
296.16 MANIC AFFECTIVE DISORDER RECURRENT EPISODE IN
FULL REMISSION
296.20 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE UNSPECIFIED DEGREE
296.21 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE MILD DEGREE
296.22 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE MODERATE DEGREE
296.23 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE SEVERE DEGREE WITHOUT PSYCHOTIC
BEHAVIOR
296.24 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE SEVERE DEGREE SPECIFIED AS WITH
PSYCHOTIC BEHAVIOR
296.25 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE IN PARTIAL OR UNSPECIFIED REMISSION
296.26 MAJOR DEPRESSIVE AFFECTIVE DISORDER SINGLE
EPISODE IN FULL REMISSION
296.30 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE UNSPECIFIED DEGREE
296.31 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE MILD DEGREE
296.32 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE MODERATE DEGREE
296.33 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE SEVERE DEGREE WITHOUT PSYCHOTIC
BEHAVIOR
296.34 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE SEVERE DEGREE SPECIFIED AS WITH
PSYCHOTIC BEHAVIOR
296.35 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE IN PARTIAL OR UNSPECIFIED REMISSION
296.36 MAJOR DEPRESSIVE AFFECTIVE DISORDER RECURRENT
EPISODE IN FULL REMISSION
296.40 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, UNSPECIFIED
296.41 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, MILD
296.42 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, MODERATE
296.43 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, SEVERE, WITHOUT MENTION OF
PSYCHOTIC BEHAVIOR
296.44 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, SEVERE, SPECIFIED AS WITH
PSYCHOTIC BEHAVIOR
296.45 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, IN PARTIAL OR UNSPECIFIED
REMISSION
296.46 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MANIC, IN FULL REMISSION
296.50 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, UNSPECIFIED
296.51 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, MILD
296.52 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, MODERATE
296.53 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, SEVERE, WITHOUT MENTION OF
PSYCHOTIC BEHAVIOR
296.54 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, SEVERE, SPECIFIED AS WITH
PSYCHOTIC BEHAVIOR
296.55 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, IN PARTIAL OR UNSPECIFIED
REMISSION
296.56 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) DEPRESSED, IN FULL REMISSION
296.60 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, UNSPECIFIED
296.61 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, MILD
296.62 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, MODERATE
296.63 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, SEVERE, WITHOUT MENTION OF
PSYCHOTIC BEHAVIOR
296.64 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, SEVERE, SPECIFIED AS WITH
PSYCHOTIC BEHAVIOR
296.65 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, IN PARTIAL OR UNSPECIFIED
REMISSION
296.66 BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) MIXED, IN FULL REMISSION
296.7
BIPOLAR I DISORDER, MOST RECENT EPISODE (OR
CURRENT) UNSPECIFIED
296.80 BIPOLAR DISORDER, UNSPECIFIED
296.81 ATYPICAL MANIC DISORDER
296.82 ATYPICAL DEPRESSIVE DISORDER
296.89 OTHER AND UNSPECIFIED BIPOLAR DISORDERS, OTHER
296.90 UNSPECIFIED EPISODIC MOOD DISORDER
296.99 OTHER SPECIFIED EPISODIC MOOD DISORDER
297.0
PARANOID STATE SIMPLE
297.1
DELUSIONAL DISORDER
297.2
PARAPHRENIA
297.3
SHARED PSYCHOTIC DISORDER
297.8
OTHER SPECIFIED PARANOID STATES
297.9
UNSPECIFIED PARANOID STATE
298.8
OTHER AND UNSPECIFIED REACTIVE PSYCHOSIS
298.9
UNSPECIFIED PSYCHOSIS
299.00 AUTISTIC DISORDER, CURRENT OR ACTIVE STATE
299.10 CHILDHOOD DISINTEGRATIVE DISORDER, CURRENT OR
ACTIVE STATE
299.80 OTHER SPECIFIED PERVASIVE DEVELOPMENTAL
DISORDERS, CURRENT OR ACTIVE STATE
300.01 PANIC DISORDER WITHOUT AGORAPHOBIA
300.02 GENERALIZED ANXIETY DISORDER
300.11 CONVERSION DISORDER
300.12 DISSOCIATIVE AMNESIA
300.13 DISSOCIATIVE FUGUE
300.14 DISSOCIATIVE IDENTITY DISORDER
300.15 DISSOCIATIVE DISORDER OR REACTION UNSPECIFIED
300.16 FACTITIOUS DISORDER WITH PREDOMINANTLY
PSYCHOLOGICAL SIGNS AND SYMPTOMS
300.19 OTHER AND UNSPECIFIED FACTITIOUS ILLNESS
300.21 AGORAPHOBIA WITH PANIC DISORDER
300.22 AGORAPHOBIA WITHOUT PANIC ATTACKS
300.23 SOCIAL PHOBIA
300.29 OTHER ISOLATED OR SPECIFIC PHOBIAS
300.3
OBSESSIVE-COMPULSIVE DISORDERS
300.4
DYSTHYMIC DISORDER
300.6
DEPERSONALIZATION DISORDER
300.7
HYPOCHONDRIASIS
300.82 UNDIFFERENTIATED SOMATOFORM DISORDER
302.70 PSYCHOSEXUAL DYSFUNCTION UNSPECIFIED
302.71 HYPOACTIVE SEXUAL DESIRE DISORDER
302.72 PSYCHOSEXUAL DYSFUNCTION WITH INHIBITED SEXUAL
EXCITEMENT
302.73 FEMALE ORGASMIC DISORDER
302.74 MALE ORGASMIC DISORDER
302.75 PREMATURE EJACULATION
302.76 DYSPAREUNIA, PSYCHOGENIC
302.79 PSYCHOSEXUAL DYSFUNCTION WITH OTHER SPECIFIED
PSYCHOSEXUAL DYSFUNCTIONS
303.90 OTHER AND UNSPECIFIED ALCOHOL DEPENDENCE
UNSPECIFIED DRINKING BEHAVIOR
303.91 OTHER AND UNSPECIFIED ALCOHOL DEPENDENCE
CONTINUOUS DRINKING BEHAVIOR
303.92 OTHER AND UNSPECIFIED ALCOHOL DEPENDENCE
EPISODIC DRINKING BEHAVIOR
303.93 OTHER AND UNSPECIFIED ALCOHOL DEPENDENCE IN
REMISSION
304.00 OPIOID TYPE DEPENDENCE UNSPECIFIED USE
304.01 OPIOID TYPE DEPENDENCE CONTINUOUS USE
304.02 OPIOID TYPE DEPENDENCE EPISODIC USE
304.03 OPIOID TYPE DEPENDENCE IN REMISSION
304.10 SEDATIVE, HYPNOTIC OR ANXIOLYTIC DEPENDENCE,
UNSPECIFIED
304.11 SEDATIVE, HYPNOTIC OR ANXIOLYTIC DEPENDENCE,
CONTINUOUS
304.12 SEDATIVE, HYPNOTIC OR ANXIOLYTIC DEPENDENCE,
EPISODIC
304.13 SEDATIVE, HYPNOTIC OR ANXIOLYTIC DEPENDENCE, IN
REMISSION
304.20 COCAINE DEPENDENCE UNSPECIFIED USE
304.21 COCAINE DEPENDENCE CONTINUOUS USE
304.22 COCAINE DEPENDENCE EPISODIC USE
304.23 COCAINE DEPENDENCE IN REMISSION
304.30 CANNABIS DEPENDENCE UNSPECIFIED USE
304.31 CANNABIS DEPENDENCE CONTINUOUS USE
304.32 CANNABIS DEPENDENCE EPISODIC USE
304.33 CANNABIS DEPENDENCE IN REMISSION
304.40 AMPHETAMINE AND OTHER PSYCHOSTIMULANT
DEPENDENCE UNSPECIFIED USE
304.41 AMPHETAMINE AND OTHER PSYCHOSTIMULANT
DEPENDENCE CONTINUOUS USE
304.42 AMPHETAMINE AND OTHER PSYCHOSTIMULANT
DEPENDENCE EPISODIC USE
304.43 AMPHETAMINE AND OTHER PSYCHOSTIMULANT
DEPENDENCE IN REMISSION
304.50 HALLUCINOGEN DEPENDENCE UNSPECIFIED USE
304.51 HALLUCINOGEN DEPENDENCE CONTINUOUS USE
304.52 HALLUCINOGEN DEPENDENCE EPISODIC USE
304.53 HALLUCINOGEN DEPENDENCE IN REMISSION
304.60 OTHER SPECIFIED DRUG DEPENDENCE UNSPECIFIED
USE
304.61 OTHER SPECIFIED DRUG DEPENDENCE CONTINUOUS
USE
304.62 OTHER SPECIFIED DRUG DEPENDENCE EPISODIC USE
304.63 OTHER SPECIFIED DRUG DEPENDENCE IN REMISSION
304.70 COMBINATIONS OF OPIOID TYPE DRUG WITH ANY
OTHER DRUG DEPENDENCE UNSPECIFIED USE
304.71 COMBINATIONS OF OPIOID TYPE DRUG WITH ANY
OTHER DRUG DEPENDENCE CONTINUOUS USE
304.72 COMBINATIONS OF OPIOID TYPE DRUG WITH ANY
OTHER DRUG DEPENDENCE EPISODIC USE
304.73 COMBINATIONS OF OPIOID TYPE DRUG WITH ANY
OTHER DRUG DEPENDENCE IN REMISSION
304.80 COMBINATIONS OF DRUG DEPENDENCE EXCLUDING
OPIOID TYPE DRUG UNSPECIFIED USE
305.20 NONDEPENDENT CANNABIS ABUSE UNSPECIFIED USE
305.21 NONDEPENDENT CANNABIS ABUSE CONTINUOUS USE
305.22 NONDEPENDENT CANNABIS ABUSE EPISODIC USE
305.23 NONDEPENDENT CANNABIS ABUSE IN REMISSION
305.30 NONDEPENDENT HALLUCINOGEN ABUSE UNSPECIFIED
USE
305.31 NONDEPENDENT HALLUCINOGEN ABUSE CONTINUOUS
USE
305.32 NONDEPENDENT HALLUCINOGEN ABUSE EPISODIC USE
305.33 NONDEPENDENT HALLUCINOGEN ABUSE IN REMISSION
305.40 SEDATIVE, HYPNOTIC OR ANXIOLYTIC ABUSE,
UNSPECIFIED
305.41 SEDATIVE, HYPNOTIC OR ANXIOLYTIC ABUSE,
CONTINUOUS
305.42 SEDATIVE, HYPNOTIC OR ANXIOLYTIC ABUSE, EPISODIC
305.43 SEDATIVE, HYPNOTIC OR ANXIOLYTIC ABUSE, IN
REMISSION
305.50 NONDEPENDENT OPIOID ABUSE UNSPECIFIED USE
305.51 NONDEPENDENT OPIOID ABUSE CONTINUOUS USE
305.52 NONDEPENDENT OPIOID ABUSE EPISODIC USE
305.53 NONDEPENDENT OPIOID ABUSE IN REMISSION
305.60 NONDEPENDENT COCAINE ABUSE UNSPECIFIED USE
305.61 NONDEPENDENT COCAINE ABUSE CONTINUOUS USE
305.62 NONDEPENDENT COCAINE ABUSE EPISODIC USE
305.63 NONDEPENDENT COCAINE ABUSE IN REMISSION
305.70 NONDEPENDENT AMPHETAMINE OR RELATED ACTING
SYMPATHOMIMETIC ABUSE UNSPECIFIED USE
305.71 NONDEPENDENT AMPHETAMINE OR RELATED ACTING
SYMPATHOMIMETIC ABUSE CONTINUOUS USE
305.72 NONDEPENDENT AMPHETAMINE OR RELATED ACTING
SYMPATHOMIMETIC ABUSE EPISODIC USE
305.73 NONDEPENDENT AMPHETAMINE OR RELATED ACTING
SYMPATHOMIMETIC ABUSE IN REMISSION
305.80 NONDEPENDENT ANTIDEPRESSANT TYPE ABUSE
UNSPECIFIED USE
305.81 NONDEPENDENT ANTIDEPRESSANT TYPE ABUSE
CONTINUOUS USE
305.82 NONDEPENDENT ANTIDEPRESSANT TYPE ABUSE
EPISODIC USE
305.83 NONDEPENDENT ANTIDEPRESSANT TYPE ABUSE IN
REMISSION
305.90 OTHER MIXED OR UNSPECIFIED DRUG ABUSE
UNSPECIFIED USE
305.91 NONDEPENDENT OTHER MIXED OR UNSPECIFIED DRUG
ABUSE CONTINUOUS USE
305.92 NONDEPENDENT OTHER MIXED OR UNSPECIFIED DRUG
ABUSE EPISODIC USE
306.51 PSYCHOGENIC VAGINISMUS
307.1
ANOREXIA NERVOSA
307.20 TIC DISORDER UNSPECIFIED
307.21 TRANSIENT TIC DISORDER
307.22 CHRONIC MOTOR OR VOCAL TIC DISORDER
307.23 TOURETTE'S DISORDER
307.3
STEREOTYPIC MOVEMENT DISORDER
307.42 PERSISTENT DISORDER OF INITIATING OR MAINTAINING
SLEEP
307.44 PERSISTENT DISORDER OF INITIATING OR MAINTAINING
WAKEFULNESS
307.46 SLEEP AROUSAL DISORDER
307.50 EATING DISORDER UNSPECIFIED
307.51 BULIMIA NERVOSA
307.52 PICA
307.53 RUMINATION DISORDER
307.54 PSYCHOGENIC VOMITING
307.59 OTHER DISORDERS OF EATING
307.80 PSYCHOGENIC PAIN SITE UNSPECIFIED
307.89 OTHER, PAIN DISORDER RELATED TO PSYCHOLOGICAL
FACTORS
308.3
OTHER ACUTE REACTIONS TO STRESS
309.0
ADJUSTMENT DISORDER WITH DEPRESSED MOOD
309.1
ADJUSTMENT REACTION WITH PROLONGED DEPRESSIVE
REACTION
309.21 SEPARATION ANXIETY DISORDER
309.23 SPECIFIC ACADEMIC OR WORK INHIBITION
309.24 ADJUSTMENT DISORDER WITH ANXIETY
309.28 ADJUSTMENT DISORDER WITH MIXED ANXIETY AND
DEPRESSED MOOD
309.3
ADJUSTMENT DISORDER WITH DISTURBANCE OF
CONDUCT
309.4
ADJUSTMENT DISORDER WITH MIXED DISBURBANCE OF
EMOTIONS AND CONDUCT
309.81 POSTTRAUMATIC STRESS DISORDER
310.1
PERSONALITY CHANGE DUE TO CONDITIONS
CLASSIFIED ELSEWHERE
311
DEPRESSIVE DISORDER NOT ELSEWHERE CLASSIFIED
312.81 CONDUCT DISORDER CHILDHOOD ONSET TYPE
312.82 CONDUCT DISORDER ADOLESCENT ONSET TYPE
312.89 OTHER SPECIFIED CONDUCT DISORDER NOT
ELSEWHERE CLASSIFIED
313.23 SELECTIVE MUTISM
313.81 OPPOSITIONAL DEFIANT DISORDER
313.82 IDENTITY DISORDER OF CHILDHOOD OR ADOLESCENCE
314.00 ATTENTION DEFICIT DISORDER OF CHILDHOOD
WITHOUT HYPERACTIVITY
314.01 ATTENTION DEFICIT DISORDER OF CHILDHOOD WITH
HYPERACTIVITY
314.1
HYPERKINESIS OF CHILDHOOD WITH DEVELOPMENTAL
DELAY
314.2
HYPERKINETIC CONDUCT DISORDER OF CHILDHOOD
314.8
OTHER SPECIFIED MANIFESTATIONS OF HYPERKINETIC
SYNDROME OF CHILDHOOD
314.9
UNSPECIFIED HYPERKINETIC SYNDROME OF CHILDHOOD
315.00 DEVELOPMENTAL READING DISORDER UNSPECIFIED
315.01 ALEXIA
315.02 DEVELOPMENTAL DYSLEXIA
315.09 OTHER SPECIFIC DEVELOPMENTAL READING DISORDER
315.1
MATHEMATICS DISORDER
315.2
OTHER SPECIFIC DEVELOPMENTAL LEARNING
DIFFICULTIES
315.31 EXPRESSIVE LANGUAGE DISORDER
315.32 MIXED RECEPTIVE-EXPRESSIVE LANGUAGE DISORDER
315.39 OTHER DEVELOPMENTAL SPEECH DISORDER
315.4
DEVELOPMENTAL COORDINATION DISORDER
315.5
MIXED DEVELOPMENT DISORDER
315.8
OTHER SPECIFIED DELAYS IN DEVELOPMENT
315.9
UNSPECIFIED DELAY IN DEVELOPMENT
317
MILD MENTAL RETARDATION
318.0
MODERATE MENTAL RETARDATION
318.1
SEVERE MENTAL RETARDATION
318.2
PROFOUND MENTAL RETARDATION
332.1
SECONDARY PARKINSONISM
333.92 NEUROLEPTIC MALIGNANT SYNDROME
333.99 OTHER EXTRAPYRAMIDAL DISEASES AND ABNORMAL
MOVEMENT DISORDERS
347.00 NARCOLEPSY, WITHOUT CATAPLEXY
347.01 NARCOLEPSY, WITH CATAPLEXY
347.10 NARCOLEPSY IN CONDITIONS CLASSIFIED ELSEWHERE,
WITHOUT CATAPLEXY
347.11 NARCOLEPSY IN CONDITIONS CLASSIFIED ELSEWHERE,
WITH CATAPLEXY
389.00 CONDUCTIVE HEARING LOSS UNSPECIFIED
389.01 CONDUCTIVE HEARING LOSS EXTERNAL EAR
389.02 CONDUCTIVE HEARING LOSS TYMPANIC MEMBRANE
389.03 CONDUCTIVE HEARING LOSS MIDDLE EAR
389.04 CONDUCTIVE HEARING LOSS INNER EAR
389.08 CONDUCTIVE HEARING LOSS OF COMBINED TYPES
389.10 SENSORINEURAL HEARING LOSS UNSPECIFIED
389.11 SENSORY HEARING LOSS
389.12 NEURAL HEARING LOSS
389.14 CENTRAL HEARING LOSS
389.18 SENSORINEURAL HEARING LOSS OF COMBINED TYPES
389.2
MIXED CONDUCTIVE AND SENSORINEURAL HEARING
LOSS
389.7
DEAF MUTISM NOT ELSEWHERE CLASSIFIABLE
780.09 ALTERATION OF CONSCIOUSNESS OTHER
780.52 INSOMNIA, UNSPECIFIED
784.3
APHASIA
784.41 APHONIA
784.5
OTHER SPEECH DISTURBANCE
995.2
UNSPECIFIED ADVERSE EFFECT OF DRUG MEDICINAL
AND BIOLOGICAL SUBSTANCE NOT ELSEWHERE
CLASSIFIED
995.50 UNSPECIFIED CHILD ABUSE
995.51 CHILD EMOTIONAL/PSYCHOLOGICAL ABUSE
995.52 CHILD NEGLECT (NUTRITIONAL)
995.53 CHILD SEXUAL ABUSE
995.54 CHILD PHYSICAL ABUSE
995.55 SHAKEN BABY SYNDROME
995.59 OTHER CHILD ABUSE AND NEGLECT
995.80 UNSPECIFIED ADULT MALTREATMENT
995.81 ADULT PHYSICAL ABUSE
995.82 ADULT EMOTIONAL/PSYCHOLOGICAL ABUSE
995.83 ADULT SEXUAL ABUSE
995.84 ADULT NEGLECT (NUTRITIONAL)
995.85 OTHER ADULT ABUSE AND NEGLECT
V71.09 OBSERVATION OF OTHER SUSPECTED MENTAL
CONDITION
Diagnoses that
Support Medical
Necessity
All diagnoses listed in “ICD-9-CM Codes that Support Medical
Necessity” above.
ICD-9 Codes that
DO NOT Support
Medical Necessity
All diagnoses not listed in “ICD-9-CM Codes that Support Medical
Necessity” above.
Non-Medical
Necessity ICD-9
Codes Asterisk
Explanation
Diagnoses that DO
NOT Support
Medical Necessity
c
All diagnoses not listed in “ICD-9-CM Codes that Support Medical
Necessity” above.