Complex_trauma_papers
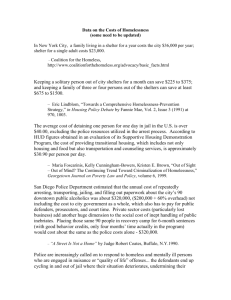
advertisement

Literature Search Complex trauma and PTSD Literature reviews (Bassuk, Melnick et al. 1998) US (Kim and Ford 2006) US (Tischler, Edwards et al. 2009) UK Americans have started to recognize interpersonal violence as a major health care issue. Increasingly, clinicians are beginning to recognize both the high rate of victimization among extremely poor women and its health consequences. However, most clinical responses focus on the immediate effects of child abuse, partner abuse, and rape. The long-term medical and mental health consequences and the relationship between early victimization and adult problems are still largely ignored. This article focuses on medical and mental health needs of extremely poor women survivors of interpersonal violence. It begins by documenting the extent and nature of violence against low-income women. Special attention is focused on the long-term sequelae of childhood abuse and on identifying and managing complex trauma responses in these women. The article concludes by discussing obstacles to care and the necessity of advocating for increased resources to respond to women living in extreme poverty. As the prevalence of homelessness among men increases, the impact of trauma and posttraumatic stress disorder in the lives of homeless men warrants attention. We will review research and clinical reports on the impact of traumatic event exposure, the antecedents and consequences of traumatic events, and homelessness among males in order to begin to develop scientific, public health, and social policy answers to several questions. The nascent clinical and scientific literature provides evidence of the need for prospective studies of the etiology, epidemiology, course, and prevention of post-traumatic stress disorder among males who are at risk for or in the early stages of homelessness. We attempt to summarize, categorize, and suggest important variables and causal relationships that can inform future research studies and interventions in order to contribute to the growth of this underdeveloped and important knowledge base Homelessness is recognised to be a traumatic event in itself and is often preceded by the experience of violence. More recent research has indicated that homelessness can function to enact growth and resilience in women with dependent children. This review paper draws together findings from a series of studies involving women with dependent children who experience homelessness. It identifies key psychosocial and health priorities in this population and how findings related to resilience and growth can be harnessed in therapeutic 1 (Thompson and Carll 2007) -youth homelessness including why youth become homeless and trauma and homeless youth US work. Pragmatic service developments and examples of good practice in therapeutic and multi-agency interventions from the domestic violence and homelessness literature are described and recommendations are made for developing services and working therapeutically with marginalised and transient populations. Therapists need to work in a flexible and integrated way with other key services, so that the crisis and long term needs of this population are met Homeless adolescents are some of this nation's most vulnerable and underserved youth and comprise approximately one-quarter of all people who are homeless (Cauce et al., 2000). Homelessness among youth populations has serious consequences for public health. Topics discussed in this chapter include why youth become homeless; homeless youth victimization; trauma and homeless youth; homeless youth case vignettes; intervention options and recommendations; and social policy implications. Research Articles suggesting link between complex trauma/ PTSD and homelessness Reference n Country Population Method/measures type (AndresLemay, Jamieson et al. 2005) 3760 Canada adolescent Survey Age of homelessness correlated with child trauma (Bassuk, Dawson et al. 2001) 425 US Women Longitudinal study Homeless vs poor Shelter Outcome Respondents who reported physical abuse only, sexual abuse only, and physical abuse with sexual abuse were 2 to 4 times more likely to report running away from home before age 16 years. Parental psychiatric disorder, respondent psychiatric disorder, respondent age, and income were also significant correlates of running away. We found that extremely poor women with lifetime PTSD were more likely to have grown up in family environments of violence, threat, and anger than those without PTSD. The strongest risk factor for PTSD was childhood sexual abuse with threat. Many low-income women have difficulty using medical care appropriately because of childhood histories of physical and sexual abuse, the subsequent development of post-trauma responses, and structural barriers to care. Given these factors, it is critical that 2 (BearsleySmith, Bond et al. 2008) H- 137 a-r 766 n-r 4844 Australia adolescent Chamberlain and Mackenzies selfreport scale Homeless (H) vs at-risk(a-r) vs students (nr) (Belcher, Greene et al. 2001) (Blankertz, Cnaan et al. 1993) US US Adults, dual diagnosis Risk factors (Browne 1993) US women prevalence health care clinicians routinely screen for histories of violence and PTSD and develop treatment plans that ensure safety, link current symptoms with prior experiences, and provide support as necessary. A team approach coordinated by a case manager may be the best strategy. Without routine screening for PTSD and sensitive treatment, many extremely poor women will receive compromised health care and may even be retraumatized. In multivariate analyses, homeless and at risk adolescents reported equivalent levels of family conflict, early problem behaviour and low opportunities and rewards for family involvement. Compared to adolescents not at risk, at risk adolescents were more likely to be female and to show poorer social skills/assertiveness and depressive symptoms. Compared to at risk adolescents, homeless adolescents showed additional family, school, peer and individual risks, but lower depressive symptomatology. No abstract This article examines the prevalence of these five childhood risk factors among dually diagnosed (mentally ill and substance abusing) homeless adults in rehabilitation programs. It further assesses the impact of each risk factor individually and in combinations of two on the social functioning skills and rehabilitation progress of these multiply disadvantaged clients. Higher lifetime rates of childhood physical and sexual abuse. This can increase vulnerability to homelessness Some of the manifestations of traumatic 3 (Browne and Bassuk 1997) h-220 p-216 US Women (Buhrich, Hodder et al. 2000) 157 Australia (Cauce, Paradise et al. 2000) 364 US adolescents (Craig and 268 UK Young people Prevalence abuse homeless (h) vs poor Composite International Diagnostic interview prevalence Diagnostic interview and selfreport measures reasons Homeless vs. victimization can be systematized in terms of posttraumatic stress disorder (PTSD). nearly two-thirds reported severe physical violence by a childhood caretaker, 42% reported childhood sexual molestation, and 61% reported severe violence by a male partner. Comparisons of homeless and housed women are presented, and implications for prevention and intervention are discussed in light of recent welfare reform legislation All women and over 90% of men reported at least one event of trauma in their life. Fifty-eight per cent suffered serious physical assault and 55% witnessed someone being badly injured or killed. Half the women and 10% of men reported that they had been raped. CONCLUSION: The experience of at least one lifetime event of trauma is almost universal among homeless people in Sydney and is considerably higher than for the USA general population. Reasons for such high prevalence rates are discussed. Depression and posttraumatic stress disorder are associated with a history of trauma. Health professionals need to be aware of past events of trauma among individuals who are homeless. Results of analyses suggest that homeless youth come from generally troubled backgrounds and have elevated rates of psychiatric disorders. For boys, their histories typically include physical abuse during childhood, physical assault on the street, and elevated rates of externalizing disorders. For girls, histories are more often marked by sexual abuse during childhood, sexual victimization on the streets, and elevated rates of internalizing disorders. Implications of these results for service delivery are discussed. The evidence presented in this paper supports the 4 Hodson 1998) (under 22 years) domiciled Women, severe mental illness prevalence (DaviesNetzley, Hurlburt et al. 1996) 120 US (Goodman, Saxe et al. 1991) (Goodman 1991) n/a US 50 each US mothers (Gwadz, Nish et al. 2007) 85 US Youth Risk factors Drop-in Centre Homeless vs housed Structured interview prevalence hypotheses that characterize the young homeless population as experiencing higher rates of childhood adversity and psychiatric disorder than their domiciled contemporaries. A tentative model is suggested whereby childhood experiences, educational attainment and the prior presence of psychiatric disorder all independently increase the likelihood of homelessness in a youthful population The prevalence of childhood abuse in this sample of women was substantially higher than among homeless women in general. The experience of childhood abuse was related to increased suicidality, and resulted in symptoms of posttraumatic stress disorder for some women. Women who had suffered abuse were also much more likely to become homeless during childhood and it is suggested that this is an important precursor to homelessness for many homeless women with chronic and severe mental illness. Homelessness is a risk factor for psychological trauma, including implications of trauma theory improving psychosocial conditions of homelessness. The only between-group difference was that a significantly higher proportion of housed mothers had experienced sexual abuse in adulthood. However, both groups had high lifetime prevalence rates for all forms of abuse. Data suggest that mental health services are urgently needed for both populations because of the traumatic psychological effects produced by homelessness and abuse. Rates of childhood maltreatment were substantial. Further, almost all youth experienced at least one traumatic event, with most experiencing multiple types of trauma. Gender differences were found in the types, but not prevalence or magnitude, of childhood 5 (Feitel, Margetson et al. 1992) 150 Youth Interview DSM-IIIR prevalence Shelter (Heffron, Skipper et al. 1995) (Herman, Susser et al. 1997) US US Homeless vs 2 other groups Health clinic h-92 nh395 US adult Structured interview including scale for lack of care from parents Risk factors Homeless(h) vs non- maltreatment and traumatic events experienced. Partial symptomatology of PTSD was common for females but not males. Symptoms of depression and anxiety were found to co-occur with PTSD for females, which may complicate treatment efforts. Most of the respondents came from backgrounds characterized by severe emotional deprivation and physical or sexual abuse. Of the 140 who completed the full interview, 90 percent fulfilled DSM-III-R criteria for an emotional or behavioral disorder. Fiftynine percent had conduct disorder, three-quarters were depressed, 41 percent had considered suicide, and more than one-quarter had attempted suicide Significant differences in families of origin among these three groups were identified. On univariate analysis, homeless persons were found to have an increased prevalence of alcoholism in the family of origin, earlier departure from the home, minority status, a self-described negative childhood, experiences of abuse as a child, high birth order in large families, less parental education, less-skilled parental occupations, less feeling of love in the childhood family, less likelihood of the father being in the home, more risk of the father having been in jail, and less identification with a religious group. Multivariate analysis revealed that compared to the study groups, the following family of origin factors were associated with homelessness: ethnic group, alcoholism, feeling loved as a child, and having one's father in jail. Lack of care from a parent during childhood sharply increased the likelihood of subsequent homelessness (odds ratio [OR] = 13), as did physical abuse (OR = 16). Sexual abuse during childhood was associated 6 (Hyde 2005) (Jainchill, Hawke et al. 2000) 50 US Young people US Adult Shelter-based therapeutic community and single items for abuse Validated scale homeless(nh) with a nonsignificant trend toward homelessness (OR = 1.7). The risk of subsequent homelessness among individuals who experienced both lack of care and either type of abuse was dramatically increased compared with subjects reporting neither of these adversities (OR = 26). CONCLUSIONS: Adverse childhood experiences are powerful risk factors for adult homelessness. Effectively reducing child abuse and neglect may ultimately help prevent critical social problems including homelessness. Life history interviews Why became homeless In professional discourses, homeless young people are often portrayed as victims of physical abuse and emotional neglect. Although participants' narratives reveal that abuse and neglect play a central role in their decisions to leave home, many maintain a sense of agency in the recounting of how they became homeless. The sample presents with extensive psychopathology and a history of physical and sexual abuse. Gender differences indicate that, except for antisocial personality, females yield higher rates on measures of both psychiatric disturbance and abuse. The relationship between psychopathology and abuse also appears to be much stronger for females than for males. However, the relationship between abuse and adult homelessness appears to be similar for men and women. The gender differences in the relationship between histories of abuse and manifestations of psychiatric disturbance support a hypothesis that has been proposed elsewhere: Females internalize the trauma associated with abusive experience, while males externalize it. The findings suggest that, although there may be a need for gender-specific prevalence 7 (Janus, Archambault et al. 1995) 195 Canada (Kaufman and Widom 1999) 1196 each US (Khurana, Sharma et al. 2004) adolescents Documented cases of abuse India Children Child observation home Descriptive investigation prevalence Interview + followup Cases of neglect vs matched controls hopelessness scale for children by Kazdin, Beck depression inventory, Psychological prevalence targeted interventions, treatment providers must also recognize that the impact of abuse seems to transcend gender within this population. In this sample, 86% of the population (74% of the males and 90% of the females) reported at least one physically abusive experience. The data reported suggest that this population of adolescents have been the victims of chronic, extreme abuse, experienced at a young age, often perpetrated by the biological parent (most often the mother), and was initiated prior to the first runaway episode. Female runaways were at greater risk than males for all types of abuse experience. Once youths left home, the physical abuse experiences decreased in frequency, but grew in severity, particularly for males Results indicate that: (1) being abused or neglected in childhood increases the likelihood of running away from home; (2) both childhood victimization and running away increase the risk of juvenile arrest; and (3) chronic runaway youths are at greater risk of arrest. Running away increases the risk of juvenile arrest for both childhood victims and nonvictims, and therefore does not mediate the relationship between childhood victimization and delinquency. The effect of running away is stronger for non-abused and nonneglected youths. This unexpected finding suggests that all runaways are at risk for delinquency regardless of childhood victimization 20.7% of children were found to have high hopelessness and 8% of children had depression. 2% of children revealed that they had attempted suicide at any point of time in life. Among children with high hopelessness, 3.2% had ever attempted suicide. 8.3% of the depressed children gave history of suicidal 8 (Kim and Arnold 2004) 99 (Martijn and Sharpe 2006) 35 (McManus and Thompson 2008) n/a (MorrellBellai, Goering 29 US Men 5 substance abuse agencies Australia Age 14-25 survey questionnaire and RUTTER-B2 scale were used to assess various mental health problems. Stressful Life Events Screening Questionnaire, Trauma Symptoms Checlist-40 Quasi-qualitative adolescents Canada Chronically homeless prevalence Pathways to homelessness Abuse-skills and homelessnes Multimethod – qualitative Reasons for homelessness attempts. 38% of children gave history of physical abuse, 14.6% of sexual abuse and a large number reported substance abuse. 69.33% were found to have behavioral problems (i.e. scored above the recommended cut off score of 9). 81% of children had antisocial behavior, 7.8% were neurotic and 10.5% remained undifferentiated. Analyses revealed that the number of stressful life events and the presence of a co-occurring mental health disorder were both significant predictors of the severity of trauma symptoms. Findings suggest that treatment professionals working with this population should assess for stressful life events and trauma symptoms as part of a comprehensive approach to substance abuse treatment for homeless men. Discuss 5 trajectories into homelessness. More psychological disorders than average, trauma is common prior to homelessness The detrimental effects of traumatic experiences often inhibit homeless youths' ability to employ the psychosocial skills necessary to a transition out of homelessness. Consequently, interventions targeting the mitigation of post-traumatic stress symptoms among this population are crucial. This article aims to address the symptoms and needs of unaccompanied homeless youth who experience post-traumatic stress disorder symptomatology and offers a strength-based intervention framework for understanding, identifying, and beginning to address trauma-related mental health needs within the cultural context and experience of youth homelessness The findings suggest that people both become and remain homeless due to a combination of macro level 9 et al. 2000) (adults) component (Mounier and Andujo 2003) 25 US youth Interview, Defense Mechanism Rating Scale Relationship between homelessness, coping strategies and victimization (North and Smith 1992) 900 US adult Diagnostic Interview ScheduleHomeless Supplement (PTSD) prevalence factors (poverty, lack of employment, low welfare wages, lack of affordable housing) and personal vulnerability (childhood abuse or neglect, mental health symptoms, impoverished support networks, substance abuse). Chronically homeless individuals often reported experiences of severe childhood trauma and tended to attribute their continued homelessness to a substance abuse problem. It is concluded that both macro anal individual level factors must be considered in planning programs and services to address the issue of homelessness in Canada. Relationships were demonstrated between use of defenses and specific as well as cumulative victimization experiences. All levels of defenses became more pervasive in response to victimization, but this was not a predictor of overall immature defensive functioning. CONCLUSIONS: Clinical and program interventions to engage homeless youth need to incorporate an understanding of the relationship between defenses and victimization in order to be effective in maximizing upon the strengths of this population. Most subjects with PTSD had an additional lifetime psychiatric diagnosis. No consistent pattern of association was apparent, however, between individual diagnoses and either traumatic events or PTSD. In almost three-fourths of both men and women, the onset of PTSD had preceded the onset of homelessness. Childhood histories of abuse and family fighting were predictive of both traumatic events and PTSD. The results suggest that factors leading to PTSD in the study sample began long before the onset of homelessness and may overlap with factors operative in the genesis of homelessness. 10 (North, Smith et al. 1994) 900 US (Nyamathi, Wenzel et al. 2001) 507+ partners US women History of adult victimization yes/no response format,. revised version of the Coopersmith SelfEsteem Inventory (SEI). Brief Symptom Inventory (BSI), Drug History Form. prevalence US Youth (13-17 years) Questionnaires, behavioural indicators prevalence (Powers, Jaklitsch et al. 1989) Abuse and other illness Sought services Many subjects had experienced a traumatic event, and post-traumatic stress disorder was very common. Substance abuse and other Axis I disorders were associated with a history of a traumatic event. The majority of men and a substantial proportion of women also had a history of physically aggressive behaviors, often beginning in childhood. Aggressive adult behavior was associated with substance abuse and major depression. The aggressive behaviors usually predated homelessness, and about half continued after the individual had become homeless. Thirty-nine percent of the women reported being physically and/or sexually assaulted as adults. Controlling for potential confounders, victimized women were more likely than others to have a history of childhood sexual and physical abuse, lifetime substance use, greater mental health symptomatology, and current risky sexual activity. Thus, homeless women with mental health and substance abuse problems ought to be screened for violent experiences and encouraged to obtain treatment appropriate to their problems to reduce their ongoing risk of victimization. Results indicate that clear behavioral indicators of maltreatment can be observed among runaway and homeless youth, which varied as a function of gender, type of maltreatment, and the reason the youth sought services from the program. One of the most common behavioral indicators of maltreatment observed had to do with school failure. Data showed several gender differences including the fact that girls tended to engage in victim type behaviors while boys tended to be more anti-social. All of the behavioral 11 (Rayburn, Wenzel et al. 2005) US Women Shelter (Rew 2002) s-96, f-32, i-10 US youth (Rew, TaylorSeehafer et al. 2001) 96 US adolescents Longitudinal analysis Homeless vs low-income Survey, focus groups and interviews prevalence prevalence indicators pointed to a high degree of psychological pathology and dysfunction. Results highlight the diversity of trauma. In a longitudinal analysis, women who lived in shelters or experienced major violence had a twofold increase in their risk of depression over the 6-month follow-up. In a cross-sectional analysis, childhood sexual abuse, living in a shelter, physical violence, childhood physical abuse, and death or injury of a friend or relative predicted avoidant coping and symptoms of depression. Active coping and depression predicted mental health service seeking among traumatized women. Modifying coping strategies may ameliorate some of the negative impact of trauma and potentially enhance mental health service use among at-risk women. Sixty percent of the sample reported sexual abuse, which was significantly related to loneliness and inversely related to connectedness and perceived wellbeing. Subjects felt lonely and disconnected. They perceived their well-being in terms of current health status. Over 60% of the sample reported a history of sexual abuse; the majority were under the age of 12 years when they first tried alcohol, marijuana, and cocaine; 56.3% had injected drugs, and 46.9% had tried inhalants. A disproportionate number of Hispanics (95% of the sample) reported a history of sexual abuse. Participants with a history of sexual abuse were significantly more likely than those who did not have a history of sexual abuse to have used alcohol and/or marijuana (chi square = 9.93, p < .01) and to have considered suicide in the past 12 months (F = 14.93, p < .001). We found that sexual abuse history 12 (Rosenheck and Fontana 1994) 1460 US (Rosenthal, Mallett et al. 2006) 692 (Ryan, Kilmer et al. 2000) 329 US Adolescents (Shelton, 14,888 UK Young adults is greater in this sample than in the general population and is particularly prevalent among Hispanic/Latino subjects. As in other studies, sexual abuse was more common among females than among males. Postmilitary social isolation, psychiatric disorder, and substance abuse had the strongest direct effects on HML, although substantial indirect effects from stressors related to being in the war zone and from premilitary conduct disorder were observed. Several premilitary factors (e.g., year of birth, childhood physical or sexual abuse, placement in foster care during childhood) also had direct effects on HML. Conflict with parents was the only reason reported as important by at least two-thirds of respondents. Desire for independence and/or adventure was rated as important by nearly one-half of young men and women. veterans Structural Equation modelling Causes of homelessness Young people (12-20yrs) trained interviewers using Questionnaire Delivery System, importance of each of 22 reasons for leaving home on a four-point scale interviewed over a year-long period. Ss also completed standardized clinical interviews and symptom checklists to assess mental health status. Psychosocial status was assessed using standardized, selfreport scales. Causes of homelessness Prevalence and abuse and internalizing Results show significant differences across groups for rates of assault, rape, depression/dysthymia, and attempted suicide; and significant differences in severity of internalizing problems and cognitive problems. Without exception, the group with histories of both physical and sexual abuse exhibited the most severe symptomatology and was at greatest risk for revictimization. Multiple regression analyses suggested that abuse histories were predictive of internalizing problems while family characteristics were more predictive of externalizing problems. survey Causes of Several factors related to childhood experiences of 13 Taylor et al. 2009) (Spence, Lee et al. 2006) (Stein, Leslie et al. 2002) (682 had been homeless) 581 US Surveyed population homelessness poor family functioning, socioeconomic disadvantage, and separation from parents or caregivers were independently associated with ever being homeless. Other significant independent factors included current socioeconomic difficulty, mental health problems, and addiction problems. involvement in crime and addiction problems with gambling and alcohol were not independently associated with homelessness. The findings underscore the relationship between specific indicators of adversity in childhood and risk of homelessness and point to the importance of early intervention efforts. mental health problems also appear to be associated with homelessness, highlighting the potentially complex service needs of this population No abstract Women Trauma and homeless, substance abuse Childhood abuse directly predicted later physical abuse, chronic homelessness, depression, and less self-esteem. Parent substance use directly predicted later substance use problems among the women. Recent physical abuse predicted chronic homelessness, depression, and substance use problems. Greater self-esteem predicted less depression and fewer substance use problems. Childhood abuse also had significant indirect effects on depression, chronic homelessness, and drug and alcohol problems mediated through later physical abuse and self-esteem.CONCLUSIONS: Although there was a strong relationship between childhood abuse and parent drug use, childhood abuse was the more pervasive and devastating predictor of dysfunctional outcomes. Childhood abuse predicted a wider range of problems including lower self-esteem, more Shelters or sober living centers 14 (Sumerlin 1999) (TaylorSeehafer, Jacobvitz et al. 2008) 146 US Men, chronicity US adolescents Placement abuse and homeless Adult attachment interview victimization, more depression, and chronic homelessness, and indirectly predicted drug and alcohol problems. The mediating roles of recent physical abuse and self-esteem suggest salient leverage points for change through empowerment training and self-esteem enhancement in homeless women. significant with longer periods of time since first homeless and greater lengths of a current episode of homelessness associated with childhood out-of-home placement. Homeless men who had experienced abuse as a child had more episodes of homelessness than those who had not experienced abuse. Mean Brief Index of Self-actualization scores were not different for those with out-of-home placement or abuse; however, self-actualization scores were minimally lower with greater number of homeless episodes but not with total time homeless. Case histories supported the quantitative findings that loss of feelings of belonging in childhood were preparatory for chronic homelessness While it has been established that attachment is a salient factor with regard to childhood maltreatment and later psychosocial problems, there is a dearth of information on how homeless youths' thoughts and feelings about attachment may also be linked to behavioral risks including alcohol and substance use. This exploratory study examines older homeless adolescent's perspectives on attachment, trauma, and substance use via the semistructured Adult Attachment Interview and survey data. The findings illuminate the relationship between these factors and implications for future research and work with this population. 15 (Taylor and Sharpe 2008) 70 (Thompson 2005) 400 Australia Age 18-73 Randomly sampled through 8 homeless services US Composite International Diagnostic Interview Adolescents Prevalence The majority of the sample had experienced at least one traumatic event in their lifetime (98%). Indeed, the mean number of traumas per person was six. The 12 month prevalence of post-traumatic stress disorder was higher among homeless adults in Sydney in comparison to the Australian general population (41% vs 1.5%). But 79% of the sample had a lifetime prevalence of post-traumatic stress. In 59% of cases, the onset of post-traumatic stress disorder preceded the age of the first reported homeless episode. CONCLUSIONS: Homeless adults in Sydney frequently experience trauma and posttraumatic stress disorder. The study found that trauma and post traumatic stress disorder more often precede homelessness, but re victimization is common. These findings highlight the high mental health needs among homeless people and have implications for services for homeless people. Prevalence Ninety-eight percent of participants had elevated PTSD symptom scores. Although use of inhalants and LSD was associated with PTSD symptoms, only depression, anxiety, and dissociation, mother's ecstasy or LSD use, youth's worry about family relationships, and poor family communication predicted higher PTSD scores. Runaway/homeless youth entering emergency shelters services must be evaluated concerning trauma and associated comorbid symptoms Findings indicate that adolescents exposed to neglect (beta=-.20) and sexual abuse (beta=-.16) ran away sooner and were more likely to be victimized on the street. Rural adolescents who experienced higher levels of physical abuse relied more heavily on deviant subsistence strategies (beta=.15) and remained in Youth emergency shelters (Thrane, Hoyt et al. 2006) 602 US Adolescents Convenience sample Interviews, multiple regression Abuse and ran away sooner, rural vs urban 16 (Tiwari, Gulati et al. 2002) 40 India Boys Characteristics of runaways (Tyler 2006) 372 US youth Qualitative interview pathways (Tyler and Cauce 2002) 372 US Adolescents interviews Prevalence and perpetrators of abuse Child observation home Systematic sampling Streets and shelter abusive homes longer (beta=.15) than their similarly situated urban counterparts. The most common reason for running away was; beating by parents/relatives, followed by a desire for economic independence (28.5%). Other reasons were maltreatment by step parent/s, being both parents dead argument with parent etc. The factors emerging can be useful for identifying high-risk families with children in pre adolescent age and hence for prevention and rehabilitation Multiple forms of child maltreatment, family alcoholism, drug use, and criminal activity characterized early family histories of many youth. Leaving home because of either running away or being removed by child protective services often resulted in multiple transitions, which regularly included moving from foster care homes to a group home, back to their parents, and then again returning to the streets Approximately one-half of these young people reported being physically abused and almost one-third experienced sexual abuse. Females experienced significantly higher rates of sexual abuse compared to males, and sexual minority youth experienced significantly higher rates of physical and sexual abuse compared to heterosexual youth. Average duration of physical and sexual abuse was 5 and 2 years, respectively. Both types of abuse were rated as extremely violent by more than half of those who were abused. The average number of different perpetrators of physical and sexual abuse was four and three, respectively. Biological parents were the majority of perpetrators for physical abuse whereas non-family members most often perpetrated sexual 17 abuse. Average age of perpetrators was late 20s to early 30s and the majority of perpetrators were male for both types of abuse. CONCLUSIONS: The pattern of exploitation and victimization within the family may have serious and cumulative developmental consequences for these youth as they enter the street environment. Early intervention programs are needed to break the cycle of exploitation and abuse that adolescents experience within the family. Without intervention, many of these youth may be at risk of future exploitation and re-victimization out on the street. (Warren, Gary et al. 1994) (Weinreb, Buckner et al. 2006) (Whitbeck, Hoyt et al. 1997) 120 + parents US mothers Prevalence in 1993 vs 2003 US adolescents Parent vs runaway The authors provide data in this descriptive study to suggest that physical and sexual abuse within the family system frequently expedites youths' decisions to leave home. The role that drugs and alcohol play in runaway youths' lifestyles is also explained Homeless families taking part in the 2003 study were poorer than those taking part in the 1993 study, and female heads of household in that study reported more physical health limitations, major depressive illness, and posttraumatic stress disorder. Both the parents/caretakers and their runaway adolescents reported lower levels of parental monitoring and warmth and supportiveness and higher levels of parental rejection than comparison groups of nonrunaway families. Parents/caretakers and runaway adolescents reported high levels of family violence and sexual abuse. Similarly, they concur regarding conduct problems for the adolescents. The findings suggest that runaway and homeless adolescents accurately depict the troubled family situations that they choose 18 (Zozus and Zax 1991) to leave. The policy implications for recent debates involving criminalization and mandatory return to parental custody of homeless and runaway youth are discussed. No abstract US PTSD/complex trauma in relation to other factors (Goodman, Rosenberg et al. 1997) References (Bassuk, Buckner et al. 1998) n h-220 p-216 Country US Population mothers Measure/Method aim Homeless (h) vs poor(p) (Bebbington, Bhugra et al. 2004) 8580 UK adults structured assessment, Respondents were asked whether they had experienced selected events displayed on cards.(n=8540) Trauma and later disorders (Bebout, Harris et al. 2001) US (Carroll and Trull 1999) US Trauma and others African American Phenomenological procedures Abuse and substance Outcome Homeless and housed mothers had similar rates of psychiatric and substance use disorders. Both groups had higher lifetime and current rates of major depression and substance abuse than did all women in the National Comorbidity Survey. Both groups also had high rates of posttraumatic stress disorder and two or more lifetime conditions In people with psychosis, there is a marked excess of victimising experiences, many of which will have occurred during childhood. This is suggestive of a social contribution to aetiology. Describes the measures that residential programs might want to consider in order to respect the needs and vulnerabilities of survivors of physical and sexual abuse. This study examined how homeless African American women who have been professionally 19 Women (Goodman, Dutton et al. 1995) 99 US Women, serious mental illness (Johnson, Rew et al. 2006) 371 US Adolescents (16-23 years) Street outreach centre Professionally assessed use Abuse and victimisation Computer assisted self interview (A-CASI) Abuse and sexual risktaking, support and future time perspective assessed and who self-report to be dependent on alcohol and other drugs make sense of their becoming chemically dependent. The data were analyzed using phenomenological analysis procedures. The results show that interviewees perceived childhood physical, sexual, and psychological abuse and neglect to be among the biopsychosocial antecedents to their becoming chemically dependent. Three aspects of physical and sexual assault were assessed: lifetime prevalence; severity, cooccurrence, and recency; and associations between levels of this victimization and specific characteristics of the women. Results indicate that the life-time risk for violent victimization was so high (97%) as to amount to normative experiences for this population Sexually abused participants had significantly less future time perspective (p = .05), fewer sexual selfcare behaviors (p = .04), and less social support than non-abused participants (p = .01) and almost significantly more sexual risk-taking (p = .08). However, no significant differences were found between abused and non-abused participants on sexual self-concept, self-efficacy or intention to use condoms, safe sex behaviors, AIDS knowledge, assertive communication, or self-efficacy to perform testicular/ breast self-exams. Overall, participants who did not report a history of sexual abuse had significantly more sexual health resources and engaged in fewer sex-risk behaviors than those who reported having been abused. These differences have notable implications for screening adolescents for a history of sexual abuse. Adolescents who 20 (Johnson, Rew et al. 2006) US adolescents (Kim and Ford 2006) US Men Trauma Symptom Checklist-40, Stressful Life Event Screening Questionnaire Trauma and mental health (Kim and Ford 2006) US Men Qualitative interview Trauma and mental healt US women qualitative Substance abuse and trauma (Nyamathi, Bayley et al. 1999) 414 239 gender report sexual abuse should receive risk counseling and be screened regularly for the development of sexual risk behaviors We found that male and female abuse victims differ in terms of their cognitive-perceptual and behavioral factors associated with sexual health practices. Early identification of those who have been abused is critical so that interventions can be developed. Effective short-term interventions are needed for the adolescent victims of Child Sexual Abuse (CSA), particularly those who are homeless and prone to further sexual victimization. Analyses revealed that the number of stressful life events and the presence of a co-occurring mental health disorder were both significant predictors of the severity of trauma symptoms. Findings suggest that treatment professionals working with this population should assess for stressful life events and trauma symptoms as part of a comprehensive approach to substance abuse treatment for homeless men reported a high prevalence of depression, family dysfunction, trauma, and a pattern of several previous treatment experiences for substance abuse and/or mental health. Findings imply that in order to promote long-lasting positive outcomes in substance abuse recovery, mental health stability, and quality of life, treatment professionals need to address complex and interrelated issues that often surround this underserved population homeless women who currently used drugs and alcohol, homeless women who currently used drugs only, and to a lesser extent current alcohol users only, had suffered traumatic childhood events and 21 (Nyamathi, Longshore et al. 2001) 223 US women Abuse and substance abuse (Robert, Fournier et al. 2004) 130 Canada Adolescents (12-17yrs) Behavioural problems family dysfunction and had to cope with low selfesteem, emotional distress, and poor physical health. The initiation of drug and/or alcohol use was strongly affected by the social influence of other users. In comparison, homeless women who did not use drugs or alcohol reported a positive self-image, few traumatic events, and chose partners who did not use drugs or alcohol. Common among current drug and/or alcohol users were the reported social benefits of drug use. Quantitative analyses revealed homeless women who were current drug users were significantly more likely to have experienced childhood and adult victimization as compared with women in the other groups Physical abuse and parental drug abuse predicted daily drug use in the whole sample and selected subgroups, whereas parental alcohol abuse predicted daily alcohol use in the whole sample. Teen self-esteem was also found to have a protective effect on daily alcohol use for the sample and for African American women. Negative peer influence in adolescence predicted daily drug use among high-acculturated Latinas. In summary, childhood abuse, parental substance use, and negative peer influence affect important roles in homeless women’s daily substance use. Therefore, the members of Group B have a higher probability of being diagnosed as having a conduct disorder, being male, and associating with delinquent peers. This group had not experienced a higher level of parental violence. The opposite is true for the members of Group A. Conclusion: Our study demonstrates that parental violence and behavioral problems are variables that are 22 (Stump and Smith 2008) 50 US women (Tam, Zlotnick et al. 2003) 397 US Adults (Tyler, Hoyt et al. 2001) 372 County-wide probability sampling US Youth (1220yrs) Streets + Substance use and PTG Interviewed 3 times over 15 months Trauma and substance use/labour participation Abuse and street sexual victimization independently related to the defined categories of runaways. Therefore, these variables do not constitute, as some thinkers have claimed, the components of a unique dynamic able to explain the phenomenon of the runaway. Our results vitiate the doubts sometimes expressed by researchers about the importance of parental violence to the phenomenon of adolescent runaways. In line with predictions, more current substance use was related to less PTG, more reliance on avoidant coping once approach coping was accounted for, and greater PTSD symptomatology. Levels of growth were comparable to those found in samples with less trauma exposure. Adverse childhood events were precursors to adulthood alcohol and drug use. Consistent substance use was negatively associated with longterm labor force participation and with social service utilization among homeless adults. Adverse events at childhood, however, were positively associated with service use. Conclusions: Adverse childhood events may contribute to negative adulthood consequences, including consistent substance use and reduced labor force participation. Agencies that are involved in halting the abuse or neglect also should participate in more preventive interventions. Job-related assistance is particularly important to facilitate employment and labor force participation among homeless adults. Results show that high rates of both childhood sexual abuse and street sexual victimization were reported, with females experiencing much greater rates vs their male counterparts. Early sexual abuse 23 shelters (Tyler, Hoyt et al. 2000) 361 US Female adolescents Risk amplification model Abuse and victimisation (Whitbeck, Hoyt et al. 1997) 120 + parent Us adolescent interviews Abuse and victimization (Whitbeck and 1-156 US Adolescents(1) interviews Age and in the home increased the likelihood of later sexual victimization on the streets indirectly by increasing the amount of time at risk, deviant peer affiliations, participating in deviant subsistence strategies, and engaging in survival sex. These findings suggest that exposure to dysfunctional and disorganized homes place youth on trajectories for early independence. early sexual abuse in the home had a positive direct effect on sexual victimization of adolescents on the streets. Early sexual abuse also increased the likelihood of later sexual victimization indirectly by increasing the amount of time at risk, deviant peer associations, and incidents of survival sex. Young women who leave dysfunctional and disorganized homes often characterized by abuse continue on negative developmental trajectories once they reach the streets. The social context of street life puts these adolescents in close proximity to potential offenders and exposes them to crime and criminals. The combination of a negative developmental trajectory and the high-risk street environment increases these young women's chances of being sexually victimized Data on levels of physical and sexual abuse within family of origin, participation in deviant subsistence strategies, and levels of victimization while on the streets were collected. Path analysis indicated that abusive family backgrounds had a positive direct effect on victimization of adolescents on the streets, and indirectly increased the likelihood of victimization by increasing the amount of time at risk, deviant peer associations, and risky behaviors Homeless adolescents were more likely to be from 24 Simons 1993) 2-319 and adults(2) Streets + shelters trauma abusive family backgrounds, more likely to rely on deviant survival strategies, and more likely to be criminally victimized. A social learning model of adaptation and victimization on the streets was hypothesized Research looking at Mental Health Reviews/chapter reference (Buckner, Bassuk et al. 1993) country US (Minkoff, Drake et al. 1992) US (Driessen and Dilling 1997) German? (Eagle, Caton et al. 1990) US (Fazel, Khosla et al. 2008) UK outcome A review of the relevant literature is followed by an exploration of the complex relationship, especially for women, between homelessness and mental health. Various mental health and gender-related concerns that have implications for the design of interventions for homeless women are explored psychiatry's awareness of the problem of substance use disorder among people with severe mental illness-often referred to as dual diagnosis--has grown rapidly over the past 10 years / individuals with HDD [homelessness and dual diagnosis] constitute a subgroup defined by three major problems--homelessness, severe psychiatric disorder, and substance use disorder / for this particular subgroup, homelessness operates metaphorically as a third diagnosis; all of the difficulties that attend dual diagnosis are amplified by a third set of complicating factors related to homelessness / review current thinking regarding HDD in several domains: epidemiology, barriers to care, philosophical issues related to treatment, emerging clinical models, phases of treatment, and research issues The state of Anglo-American research on psychiatric disorders among homeless persons is summarised. Several authors reported on life-time prevalence (50-75%) and present prevalence rates (30-50%) of psychiatric disorders in this population. Alcohol-related and drug-related disorders were most frequent. Most studies, however, only included single and male subjects, while there is little information on homeless persons living with a partner or in a family. Up to now, no representative studies exist. Some recent investigations evaluated classic single case models versus case management approaches. Short-term programmes only yielded shortterm effects, but linking psychiatric and social services seems to improve health service utilization by the homeless focus on a subpopulation of the homeless, those who are mentally ill (from the chapter) explore who they are and how they came to be homeless We undertook a systematic review of surveys of such disorders in homeless people. The most common mental 25 (Folsom and Jeste 2002) (Fischer and Breakey 1991) US US (Kamieniecki 2001) Australia (McQuiston, Gillig et al. 2006) US (Philippot, Lecocq et al. 2007) Belguim – review focused on Europe (Scott 1993) UK disorders were alcohol dependence, which ranged from 8.1% to 58.5%, and drug dependence, which ranged from 4.5% to 54.2%. For psychotic illness, the prevalence ranged from 2.8% to 42.3%, with similar findings for major depression. CONCLUSIONS: Homeless people in Western countries are substantially more likely to have alcohol and drug dependence than the age-matched general population in those countries, and the prevalences of psychotic illnesses and personality disorders are higher. Models of psychiatric and social care that can best meet these mental health needs requires further investigation This article systematically reviews studies of prevalence of schizophrenia in homeless persons. Describes recent research on the prevalence of alcohol, drug, and mental (ADM) disorders and the characteristics of homeless substance abusers and persons with mental illnesses. Methodological problems in homelessness research are reviewed, particularly in relation to definitions of homelessness and sampling- and case-ascertainment methods. Prevalence rates of ADM disorders are much higher in homeless groups than in the general population. Reviewed literature on psychological distress and psychiatric disorders among homeless youth in Australia, and compared these rates with Australian youth as a whole. 14 separate studies were located. Homeless youth in Australia have extremely high rates of psychological distress and psychiatric disorders. As homeless youth are at risk of developing psychiatric disorders and possibly self-injurious behavior the longer they are homeless, early intervention in relevant health facilities is required We have set out to assemble a practical clinical guide for work with homeless people who have mental illness, written by clinicians, for clinicians. It approaches treatment and rehabilitation from the vantage point of the treatment environment, from street to housing--and, we hope, almost everything in between. The ideas in this book reflect what we believe is the evolution of consensus on a clinical approach to the homeless mentally ill person, developed over more than two decades by many experts but until now not assembled in a detailed, practical format. The rapidly growing, but still small, research literature on homelessness in Europe has often been provided by non-academics, using qualitative methods, and has been published in sources that are not widely available. This article summarizes definitions employed, observed prevalence, the socio-demographic characteristics, and the physical and mental health status of the homeless in Western Europe. Research pertaining to the causes of homelessness and the societal response to the problem are also reviewed, and the ethical and methodological questions raised by European researchers are debated. A critical analysis of the largely descriptive European research is provided, and some noteworthy exceptions are described. We also discuss a number of promising theoretical models, including those that focus on learned helplessness, social strain, and social stress Significant mental illness is present in 30-50% of the homeless: functional psychoses predominate; acute distress and personality dysfunction are also prevalent. Co-morbidity of mental illness and substance abuse occurs in 20%, and physical morbidity rates exceed those of domiciled populations. The homeless mentally ill 26 also have many social needs. Pathways to homelessness are complex; deinstitutionalization may be only one possible cause of the increase in the number of homeless people. This review outlines the research, highlights current views on the definition and classification of homeless populations, and offers some guidelines on avenues which need to be explored This paper reviews 18 surveys of mental health problems among homeless adolescents and reports on a pilot study of the same topic conducted in Amsterdam. Sampling methods and measures of mental health are discussed. The reported estimates of mental health problems vary greatly, very probably because of methodological differences. Despite the different methods used, there seems to be considerable research evidence to support a high prevalence of mental disorders among homeless adolescents. The results of the pilot study of 50 homeless adolescents in Amsterdam are consistent with the surveys reviewed. A highly structured interview was conducted at all four services sites for homeless adolescents in Amsterdam. Of the homeless adolescents interviewed, 78% had at least one lifetime DIS/DSM-III-R diagnosis, and 64% had at least one 1-month diagnosis Research on the mental health and service needs of homeless seniors has been scant. This paper reviews the available literature and presents findings of a Toronto survey in an effort to describe the demographics of homeless seniors, their level of impairment, and their mental and physical health needs. Although seniors represent a small percentage of the homeless population, their numbers are growing. The available literature suggests a high prevalence of psychiatric disorders and cognitive impairment in this population, with a greater proportion of older women than men having severe mental illness. (Sleegers, Spijker et al. 1998) Netherlands (Stergiopoulos and Herrmann 2003 Canada (Vázquez and Muñoz 2001) Vázquez and Muñoz- Spain In the present article, the authors synthesize the main data on this topic available in Spain, first, by presenting preliminary results of a project investigating the sociodemographic characteristics of the homeless in Madrid and, second, by examining the complex relationships among homelessness, mental health, and stressful life events. (Wallace, Struening et al. 1993) US what are the causal relationships between the recent environmental blight of urban homelessness and psychopathological symptoms / the complex feedback loops involved in these processes are discussed / stress the importance of social networks for the development of coping strategies of individuals threatened by the loss of their regular domiciles, a loss that is viewed by the authors as a "slow disaster" (from the introduction) the rigorous experience of IFD [irregular forms of domicile] itself may exacerbate, or even trigger, behavioral and other symptomatology / argue that the often observed relationship between psychopathology and homelessness has led to a misidentification of the causal process, and that a larger perspective is required if proper interventions are to be designed and effectively implemented 27 Research articles(mental health) Reference (Aichhorn, Santeler et al. 2008) n 40 Country Austria Population Young people (14-23 years) Shelter/counselling centre Method/measures Structured Clinical Interview for DSMIV (SKID-I) longitudinal type prevalence (Barak and Cohen 2003) 2567 Israel elderly Structured Clinical Interview for DSMIV Prevalence (Bassuk, Rubin et al. 1984) 78 US All ages interviews Prevalence Emergency shelter Outcome The results show that 58% of the homeless adolescents were exposed to continuous violence in their families and that violence was a major reason for them to leave home. The overall prevalence of diagnosed psychiatric disorders was 80% in the whole sample; the leading disorder was substance abuse/dependence (65%), followed by mood disorders (42.5%), anxiety disorders (17.5%) and eating disorders (17.5%). Duration of homelessness had the greatest influence on the prevalence of mental disorders. Longer duration of homelessness was associated with a higher risk of psychiatric disorder or self-harm. These results demonstrate the urgent need for early psychosocial and psychiatric help for homeless adolescents In 44/98 (44.9%), a formal DSM-IV axis I psychiatric disorder was diagnosed, most common being dementia (15/44) and schizophrenia (15/44). A significant minority of 13/44 (29.5%) were diagnosed and treated prior to becoming homeless. Physical co-morbidity was found in nearly 2/3 subjects. Following intensive case-management by social workers, 35/44 (79.5%) subjects were successfully placed in permanent housing. The vast majority were found to have severe psychological illnesses that largely remained untreated. Approximately 91% were given primary psychiatric diagnoses: About 40% had psychoses, 29% were chronic alcoholics, and 21% had personality disorders. Approximately one-third had been hospitalized for psychiatric care. The authors 28 (Booth and Zhang 1996) 219 US Adolescents and children (Breakey, Fischer et al. 1989) 298 men and 230 women then subsample of 203 subjects was randomly selected US (Caton, Shrout et al. 1995) 100 each US Women with/without schizophrenia (Chen, Tyler et al. 2004) 361 US Adolescent female missions, shelters, and jail Diagnostic Interview Schedule for Children baseline interview that provided extensive sociodemographic and health-related data In the second stage, systematic psychiatric and physical examinations. Standardized research instruments Prevalence and relationships Schizophrenia and other diagnoses Abuse and substance use discuss the relationship of mental health policy to the homeless and suggest that shelters have become alternative institutions to meet the needs of mentally ill people who are no longer cared for by departments of mental health Although these constructs were related to each other, a third of the subjects met criteria for only one. Childhood sexual abuse was associated with conduct disorder, while living in a home where drugs were used was associated with aggression. Severe aggressive behavior was associated with other problem behaviors, including attempted suicide, behavior that precipitated residential psychiatric treatment, pregnancy, arrests, and convictions. Data from the clinical examinations demonstrate the high prevalence of mental illnesses and other psychiatric disorders and of a wide range of physical disorders and confirm the high prevalence of alcohol abuse disorders. The high rates of comorbidity of these conditions is demonstrated and data are provided on the subjects' needs for mental health and substance abuse services Findings adjusted for ethnicity revealed that homeless women had higher rates of a concurrent diagnosis of alcohol abuse, drug abuse, and antisocial personality disorder. Homeless women also had less adequate family support. the current study revealed a high prevalence of drug use, especially use of cocaine among youths with sexual abuse histories. Path analyses showed that early sexual abuse indirectly affected drug use on the streets via running away at an earlier age, 29 (Chen, Thrane et al. 2007) US Adolescent (conduct disorder) Interview Conduct disorder and other (Commander, Davis et al. 2002) UK Young people Survey Homeless vs non-homeless (Commander and Odell 2001) UK Psyhiactiric disorders – compares needs of homeless vs nonhomeless Matched controls Homeless vs non-homeless spending more time on the street, and use of deviant strategies to survive compared with those who exhibit adolescent-onset conduct disorder, youth with childhood onset are more likely to engage in a series of antisocial behaviors such as use of sexual and nonsexual survival strategies. Second, youth with childhoodonset conduct disorder are more likely to experience violent victimization; this association, however, is mostly through an intervening process such as engagement in deviant survival strategies. The homeless sample were younger and more likely to be male than their domiciled counterparts. They had more often spent time in institutional child care and had worse educational records and lower levels of employment. Young people who were homeless had greater involvement with the police, more frequently used illicit drugs and reported worse physical and mental health than those in private households. They were equally likely to see a general practitioner and more often consulted for 'nerves' as well as having a higher rate of contact with mental health professionals Homeless patients were more symptomatic and behaviorally disturbed than controls. They were significantly more likely to have a criminal history and to be identified by key workers as having problems related to substance use. Homeless patients were less likely to have been born in Birmingham and to have ongoing contact with childhood carers but despite being less aware of the need for treatment, uptake of psychiatric care was comparable with that of controls. The implications for the development of dedicated mental health 30 (Connolly, CobbRichardson et al. 2008) 60 US (Cougnard, Grolleau et al. 2006) 104 France (Crane 1998) 255 UK (DeMallie, North et al. 900 US Structured Clinical interview (DSM IV axis I &II disorders), Positive and Negative syndrome Scale Personality disorder prevalence ICD-10 diagnosis Prevalence and comorbidity Older adult Semi-structured interviews Cause of homelessness Older vs younger National Instiutue of Mental Health Prevalence Drop-in clinic Emergency psychiatric serivces services for this population are discussed. Very high rates of all personality disorders were found for Cluster A (73% paranoid, 65% schizoid, 43% schizotypal), B (57% antisocial, 62% borderline, 20% histrionic, 57% narcissistic) and C (50% avoidant, 25% dependent, 57% obsessive compulsive). Axis I mood, anxiety, and substance use disorders were each diagnosed in over half the sample. At least one Cluster A disorder was diagnosed in 92% of the sample, and these disorders were distinguished from Axis I psychotic disorders (20%) with regard to prevalence, patterns of association, and constellation of symptoms. Cluster A disorders were not associated with any Axis I disorder, suggesting diagnostic independence in this sample. Nearly one out of three homeless subjects (32.7%) presented with a psychotic disorder, a higher proportion than that found in non-homeless subjects (15.7%). Compared to non-homeless subjects with psychosis, homeless subjects with psychosis were more likely to be male and to present with drug use disorder. There was a high prevalence of mental illness among the Ss and this was a factor in the entry to homelessness in many cases. There were indications that some Ss with mental health problems became homeless because their needs had been neglected or undetected. Mental health problems also had an impact on the circumstances of older homeless people and affected their ability to seek and accept help. Compared with their younger counterparts, older subjects were more likely to be male and white, to 31 1997) Diagnostic Interview Schedule (Fichter, Koniarczyk et al. 1996) 271 Germany men . The Diagnostic Interview Schedule (DIS) was used for diagnostic classification according to DSMIII in the main interview Prevalence (Fichter and Quadflieg 2005) 265 Germany men Interview Differences over 3 years (Fischer, 51 US Survey, diagnostic Prevalence report lower incomes and poorer health, and to meet criteria for lifetime alcohol-use disorder. Fewer older than younger subjects met criteria for lifetime drug use disorder and post-traumatic stress disorder. These findings suggest that older and younger individuals have different vulnerabilities to homelessness. the following lifetime prevalence rates were obtained: 91.8% for substance use disorder (82.9% alcohol dependence), 41.8% for affective disorders, 22.6% for anxiety disorders and 12.4% for schizophrenia. Of the homeless males in Munich, 94.5% had at least one DIS/DSM-III axis I diagnosis. Six-month prevalence data is also presented. Results are compared with those of a very similar study on homeless individuals in Los Angeles, which also used DIS/DSM-III diagnoses. In comparison with representative community samples in the United States and in Germany, mental illness was much more frequent among homeless individuals in Munich as well as in Los Angeles. Implications for health care planning are discussed. Rates of mental illness decreased from 79 % to 66% over 3 years possibly due to an improved housing situation and increased medical/psychiatric attention and service. The prevalence of mood disorders, substance use disorders and anxiety disorders was significantly lower at 3-year follow-up while psychotic disorders showed a slight increase over time. A high rate of use of general medical inpatient services was found. Considering the very high prevalence of mental illness, the use of psychiatric services was very low with some increase over time. bout one-third of the homeless scored high on the 32 Shapiro et al. 1986) interview schedule Mission usrs (Greifenhagen and Fichter 1997) 32 Germany women Diagnostic Interview Schedule for DSM-III (Haugland, Siegel et al. 1997) 201 US Have mental illness intake assessment semistructured interview (Koegel, Burnam et al. 1988) 379 (Kovess and Mangin Lazarus 1999) 838 France (McGilloway and Donnelly 401 UK (Northern shelter US Sheltered + unsheltered Single people Prevalence Diagnostic Interview Schedule Prevalence Composite International Diagnostic Interview Prevalence Institutional history Prevalence General Health Questionnaire which measures distress. A similar proportion had a current psychiatric disorder as ascertained by the Diagnostic Interview Schedule (DIS), with the homeless exhibiting higher prevalence rates in every DIS/DSM III diagnostic category compared to domiciled men Results point to very high prevalence rates of mental disorders among homeless women. The most frequent diagnostic groups were alcohol and drug abuse (lifetime prevalence rate 90.6%), affective disorders (50.0%), anxiety disorders (43.8%) and schizophrenia (21.9%). Twenty-one percent of the cohort was classified as having mental illness. Seventy-two percent had a diagnosis of drug abuse or dependence, and 51 percent had alcohol abuse or dependence. Persons with mental illness also experienced homelessness of some kind over a significantly longer period Analyses indicated that Ss' lifetime and current rates of major mental illnesses were disproportionately high when compared with a household sample for the city. 12% of the Ss had dual diagnoses of chronic major mental illness and chronic substance abuse. The lifetime prevalence of psychiatric disorders was 57.9%, while the 1-year prevalence was 29.1%. For definite psychotic disorders, prevalence was 16% (lifetime) and 6% (1 year). Generally, this Parisian homeless population had some access to care: in the preceding 6 months 57.7% of them had been medically attended and 14.2% of these had been hospitalised. 41% were identified as having a mental health problem. 59% of Ss in this target' group had an 33 2001) Ireland) (Mundy, Robertson et al. 1990) (North, Thompson et al. 1997) 96 US h-166 nh-107 + h-900 US (North, Smith et al. 1993) 900 each US adoloescents Prevalence DSM IIIR Homeless (h) vs non-homeless (nh) National Institute of Mental Health Diagnostic Interview Schedule. Homeless vs non-homeless Outpatient clinic (n=900 from survey) institutional history. Almost 25% of residents had high deviant behavior scores. Mean general behavior scores indicated that, overall, the group was comparable with the worst 15% of patients in an average day hospital, although half were rated as having sufficient skills to "survive" in the community with minimal or no formal support. No abstract Rates of schizophrenia, bipolar disorder, and somatization disorder were not significantly different between homeless and non-homeless groups. Major depression was about four times as prevalent in nonhomeless men as in homeless men. Homeless men were significantly more likely than non-homeless men to qualify for a diagnosis of alcohol use disorder, and homeless women were more likely than other women to qualify for a diagnosis of drug use disorder. Both homeless men and women were significantly more likely than their domiciled counterparts to meet criteria for antisocial personality disorder. Personality disorder other than antisocial was more prevalent in nonhomeless men than in homeless men. Combined rates of personality disorder were significantly higher among homeless than non-homeless women, but not men. In this sample of homeless men and women, most, but not all, adult symptoms of antisocial personality disorder were significantly associated with number of childhood conduct disorder symptoms. The onset of symptoms of antisocial personality disorder usually preceded the onset of homelessness. The rates of antisocial personality disorder were not significantly 34 (O'Reilly, Taylor et al. 2009) 25 homeless young people, 5 Mental Health Coordinators and 12 homeless shelter staff. UK young people (Pollio, North et al. 1997) 60 each US Mental illness (Reinking, Wolf et al. 2001) 150 Netherlands Adult living in homeless shelters in 5 large geographical areas ( 6 centres for homeless discourse analysis of semi-structured interviews, Perceptions of mental health Housed vs not housed the depression screener from Schrijvers et al., the schizophrenia section from the Composite International Diagnostic Interview (CIDI) a Prevalence affected by discounting the antisocial disorder symptoms thought to be confounded with homelessness. CONCLUSIONS: Overall, the data support the appropriateness of the diagnosis of antisocial personality disorder among homeless populations. It cannot be said from these data that homelessness often leads to antisocial behaviors They report negative and stigmatising descriptions of mental health despite their involvement with a mental health service. Four key interpretative repertoires are identified; denial of problems, mental health as negative, the need to talk, and challenging prejudice. It is concluded that the term 'mental health', which appears in the title of the service (of which they are clients), presents barriers for usage but works to challenge prejudice and educate young people. Use of eight types of services over a 26-month period was examined. Individuals whose primary presenting problem was subsistence needs were more likely to be housed than those whose primary problem was mental, illness or substance abuse. Those with a diagnosis of personality disorder used fewer services. Housed individuals were more likely to use services than those who were homeless 32% had a more narrowly defined form of depression, 15% a schizophrenic disorder (DSM-IIIR-codes 295.00-295.70) and 52% an antisocial personality disorder. In the case of depression and schizophrenia it concerned a 6-month prevalence and in the case of antisocial personality disorders it concerned the lifetime prevalence. 35 (Slesnick and Prestopnik 2005) 226 Us Youth (13-17 years) Runaway shelters (Smith, North et al. 1993) 300 US Women modified questionnaire from Schrijvers, related to the DSM-III-R, about aggressive behaviour and the Addiction severity index, European variant, version III. DSM-IV based computerized diagnostic interview schedule for children Diagnostic Interview schedule Prevalence Prevalence shelters (Taylor, Stuttaford et al. 2006) 150 UK Young people 18 foyers in 5 regions history The majority of the youth in our sample met criteria for dual or multiple diagnosis (60%) with many having more than one substance-use diagnosis (56%). The severity of mental-health and substance-use problems in this sample of substanceabusing runaways suggests the need for continued development of comprehensive services. The range and intensity of diagnoses seen indicates a need for greater focus on treatment development and strategies to address their multiple areas of risk. Schizophrenia and bipolar affective disorder account for only a small portion of the mental illness in these women. Nearly one in three has a history of substance abuse, with drug abuse being more prevalent than alcoholism. One third of the sample met lifetime criteria for posttraumatic stress disorder. One fourth of the women have received inpatient psychiatric care, and the majority with a nonsubstance Axis I diagnosis have received some mental health treatment. Young people reported multiple needs such as use of illicit drugs, experience of physical or sexual abuse, and self-harm. lengthy and recurrent mental health problems from childhood, with intermittent and usually fragmented contact with services. There was 36 (Timms and Fry 1989) UK Men interviewed prevalence The Family Crisis Oriented Personal Evaluation Scales (F-COPES) the General Health Questionnaire (GHQ) a semistructured questionnaire identified their goals. Coping strategies and mental health Salvation Army hostel (Tischler and Vostanis 2007) 72, 44 at follow-up (Tolomiczenko, 112 mothers a subset of the a range of mental complaints, predominantly depressive, anxiety and post-traumatic stress symptoms Conclusions: The young homeless people referred to the mental health service reported a range of complex mental health needs, the majority of which could not be met by statutory specialist services. Young people's lower to medium level mental health needs could be met by services operating on the interface with specialist services, if these are jointly planned and co-coordinated. Thirty-one per cent fulfilled the diagnostic and statistical manual (DSM: 111R) criteria for a diagnosis of schizophrenia and more than half were not in contact with psychiatric services. This suggests that a significant number of male schizophrenics are lost to follow-up and become homeless. Lower use of problem-focussed coping was associated with poorer mental health at the time of homelessness. Mental health problems improved over time, but levels of psychopathology remained high at follow-up. Most women had achieved their primary goal of resettlement, and this was associated with use of problem-focussed coping. Lower use of problem-focussed coping, in particular, acquiring social support, was associated with continuation of mental health problems at follow-up, however the greatest predictor of mental health at follow-up was mental health status whilst homeless. Despite exposure to major stressors and poor mental health, mothers experiencing homelessness can maintain their ability to cope effectively, in order to achieve their goals. The psychiatric status of homeless adults has been 37 Sota et al. 2000) Personality Assessment Inventory, this study tests the feasibility and usefulness of a brief, selfadministered questionnaire (Torchalla, Albrecht et al. 2004) 17 Germany women Structured Clinical Interview for DSMIV (SKID-I). Prevalence (Whitbeck, Hoyt et al. 2007) 428 US 16-19years Interviews Prevalence described primarily in terms of Axis I disorders. By adding Two of these were characterized by extreme scores on pathological dimensions of personality (borderline features, antisocial traits, and aggressivity) and differed primarily on the dimension of suicidality. The third reflected moderate levels of personality dysfunction and the fourth did not deviate from adult nonclinical norms. Brief personality assessment can be a cost-effective approach to matching services with clinical needs of homeless adults by attending to interpersonal dimensions that will likely affect service provision The prevalence of diagnosed psychiatric disorders was 71 %; the leading disorder was substance abuse/dependence (43 %), followed by anxiety disorders (35 %) and schizophrenia (12 %). Multiple diagnoses were made in 35 % of the women. DISCUSSION: Striking features were the often early onset of homelessness and the reticence in seeking help. The flight from violence was a crucial precipitant of the loss of the home and should also be discussed in the context of the development of the psychiatric disorders. About one-third (35.5%) of the runaways met lifetime criteria for PTSD and 16.1% met 12-month criteria for the disorder. More than 90% of the adolescents who met criteria for PTSD met criteria for at least one of the other four diagnoses. Multivariate analyses indicated that correlates of PTSD were age of adolescent, being female, having experienced serious physical abuse and/or sexual abuse from an adult caretaker, and having been assaulted or injured by weapon when on the street. The multiplicative interaction between sexual abuse 38 (Whitbeck, Johnson et al. 2004) 428 US Adolescents (1619years) Streets and shelter UM-CIDI and DISC-R structured interviews Prevalence and comorbidity (Winkleby, Rockhill et al. 1992) 1437 US adult Survey Prevalence (Yoder, Longley et al. 2008) 428 US adolescents Factor Analysis Suicidality and psychopathology by caretaker and sexual assault when the adolescents were on their own was statistically significant, indicating that rape victims were highly likely to meet criteria for PTSD regardless of early sexual abuse. At very high levels of early sexual abuse, the probability of meeting criteria for PTSD converges with that for sexual assault victims Homeless and runaway adolescents in small and mid-sized Midwestern cities report significant levels of mental disorder and comorbidity that are comparable and often exceed that reported in studies of larger magnet cities. The largest differences between the homeless and a comparison group of 3122 nonhomeless adults were for psychiatric hospitalization (odds ratios [ORs] of 4.6 for men and 5.9 for women) and alcohol abuse (ORs of 2.3 for men and 4.0 for women). However, when pre-homeless prevalences of addictive and psychiatric disorders were compared with prevalences among the non-homeless, absolute differences were no greater than 12%. support for a three-factor model in which suicidality (measured with lifetime suicidal ideation and suicide attempts), internalizing disorders (assessed with lifetime diagnoses of major depressive episode and post-traumatic stress disorder), and externalizing disorders (indicated by lifetime diagnoses of conduct disorder, alcohol abuse, and drug abuse) were positively intercorrelated. The findings illustrate the utility of a dimensional approach that integrates suicidality and psychopathology into one model. 39 Research looking at interventions Literature reviews (Bhui, Shanahan et al. 2006) UK (Dickey 2000) US A literature review of homeless service users' perceptions of services for homeless mentally ill people was supplemented by a qualitative in-depth survey of 10 homeless people. This article reports on their views about the services they receive. Mismatch between expectations and provision, disputes with healthcare providers, dissatisfaction with the degree to which they have choice in their care, and suspicions about the intentions of health professionals demonstrate the extent to which powerlessness and social exclusion are replicated in healthcare economies. Despite recent prosperity in the U.S., homelessness is still a widespread social problem. It is estimated that 25% of homeless persons have a serious mental illness. This article will review the literature evaluating prevention services and specialized outreach, treatment, and housing programs designed to reduce homelessness for individuals who are mentally ill. Although these interventions have been helpful in addressing the complex needs of the homeless mentally ill, it is difficult to measure how they have improved outcomes. It is even more challenging to determine whether the programs are cost-effective. Research Articles Reference (Ball, CobbRichardson et al. 2005) (Christensen, Hodgkins et al. 2005) n Country US Population adolescents 78 US Comorbid serious mental illness and substance abuse Method/measures intervention Dual focus schema therapy vs substance abuse counselling STAR, description of trauma intervention and prevalence Outcome Overall better use of DFST,but severe personality disorders used SAC better (n=78) were analyzed for a history of trauma events. Of those individuals evaluated, 79.5% (62/78) acknowledged a history of either physical and/or sexual abuse at some time in their lifetimes. Of this population, 100% of the homeless women (27/27) with co-occurring disorders had experienced a life-altering traumatic event while 68.6% (35/51) of the homeless men also reported trauma histories. We describe the trauma-based interventions made in the STAR Program that have the potential for replication in other initiatives 40 Commander (Desai, HarpazRotem et al. 2008) (Gonzalez and Rosenheck 2002) 359 UK US 5432 US Women, veterans Seeking safety, CBT manual Serious mental illness and substance abuse ACCESS centre for mental health services (Access to Community ~Care and Effective Services) Dual diagnosis vs other (Karim, Tischler et al. 2006) 35 UK Families following mental health (Hospital Anxiety and Depression Scale, following admission to two homeless hostels committed to serving homeless individuals with co-occurring disorders. No abstract CBT manual group reported significantly better outcomes over one year in employment, social support, general symptoms of psychiatric distress, and symptoms of posttraumatic stress disorder, particularly in the avoidance and arousal clusters. However, the Seeking Safety cohort was significantly more likely to have used drugs in the past 30 days. At baseline, clients with dual diagnoses were worse off than those without dual diagnoses on most clinical and social adjustment measures. Clients with dual diagnoses also had poorer outcomes at follow-up on 15 (62 percent) of 24 outcome measures. However, among clients with dual diagnoses, those who reported extensive participation in substance abuse treatment showed clinical improvement comparable to or better than that of clients without dual diagnoses. On measures of alcohol problems, clients with dual diagnoses who had a high rate of participation in selfhelp groups had outcomes superior to those of other clients with dual diagnoses. Clients with dual diagnoses who received high levels of professional services also had superior outcomes in terms of social support and involvement in the criminal justice system. Children and their mothers continued to experience high rates of mental health problems whilst resident in the hostels and 41 admission to two homeless hostels (Lester, Milby et al. 2007) 118 US Dual diagnosis, cocaine dependant (Maguire 2006) 4 UK referral criteria : 1) had alcohol and/or substance misuse problems, Eyberg Child Behaviour Inventory Scale, Health of the Nation Outcome Scales for Children and Adolescents), parenting problems (Parenting Daily Hassles Scale), and service satisfaction (semi-structured interview) .A number of measures including mental health and social functioning constructs were used to evaluate the CBT and homelessness after rehousing. However, a proportion of parents expressed a subjective improvement, which was often associated with their housing and social circumstances. A diverse range of further needs was described. CONCLUSIONS: There is a need to address the complex problems experienced by these families, with housing only forming one aspect of this provision. Interagency strategy, commissioning and services are required to meet the needs of this vulnerable group of parents and children Among those with trauma exposure and PTSD symptoms, the group receiving more behaviorally intensive, contingency management treatment had significantly greater reductions in PTSD symptomatology than did the group receiving less-intensive treatment. Regression analyses revealed that greater positive distraction coping and lower negative avoidance coping at baseline, in addition to changes in avoidance coping over the 6-month study period, were significantly related to greater symptom and severity reductions. The study provides some initial evidence of important treatment outcomes other than abstinence in addiction-related interventions. All residents reduced incidents of theft, violence and alcohol consumption. Risk to self and others was also reduced for all residents. Perceived self-efficacy increased slightly for all residents, and staff perceived that they could be more effective, less hopeless, and 42 2)were roofless 3) difficulty accessing hostel places (Morrissey, Calloway et al. 2002) project, in addition to some qualitative data. therefore possibly less stressed as a result of training. US ACCESS START, referral to a specialist team (Power and Attenborough 2003) 100 UK (Rosenheck, Kasprow et al. 2003) 182 US veterans Supported housing integrating clinical and housing services Contrary to expectations, the nine experimental sites did not demonstrate significantly greater overall systems integration than the nine comparison sites. However, the experimental sites demonstrated better project-centered integration than the comparison sites. Moreover, more extensive implementation of strategies for system change was associated with higher levels of overall systems integration as well as projectcentered integration at both the experimental sites and the comparison sites. Clients referred to the team on more than one occasion were marginally more likely to remain in contact with services. 10% of the sample had returned to the homeless circuit; 49% were resettled to more permanent accommodation. 43% were not in contact with services while 55% were still in contact 4 years later. This study supports the suggestion that with specialist intervention and support people with mental health problems who are homeless can live a more settled existence During a 3-year follow-up, HUD-VASH veterans had 16% more days housed than the case management-only group and 25% more days housed than the standard care group (P<.001 for both). The case managementonly group had only 7% more days housed 43 (Slesnick, Kang et al. 2008) 133 US youth Stepwise regression (Slesnick and Prestopnik 2005) 124 US adolescents Self-report Ecologically-based family therapy vs service as usual through a shelter than the standard care group (P =.29). The HUD-VASH group also experienced 35% and 36% fewer days homeless than each of the control groups (P<.005 for both). There were no significant differences on any measures of psychiatric or substance abuse status or community adjustment, although HUD-VASH clients had larger social networks. From the societal perspective, HUD-VASH was 6200 US dollars (15%) more costly than standard care. Incremental cost-effectiveness ratios suggest that HUD-VASH cost 45 US dollars more than standard care for each additional day housed (95% confidence interval, -19 US dollars to 108 US dollars). CONCLUSIONS: Supported housing for homeless people with mental illness results in superior housing outcomes than intensive case management alone or standard care and modestly increases societal costs. Stepwise regression results indicated that a history of sexual abuse and suicide attempts were the two strongest predictors of the treatment attendance rate, higher attendance among those with these histories. Youths who attended greater than 6 treatment sessions showed a significant reduction in alcohol use at post-treatment, but attendance rates did not impact other substance use. Youth assigned to EBFT reported greater reductions in overall substance abuse compared to youth assigned to SAU while other problem areas improved in both conditions. Findings suggest that EBFT is an 44 efficacious intervention for this relatively severe population of youth. (Stergiopoulos, Dewa et al. 2008) 73 Canada (Taylor, Stuttaford et al. 2007) 150 UK Shelter-based collaborative MH team Young people1625 years. Health of the Nation Outcome Scales (HoNOS), a risk assessment, and a service checklist at referral and final service contact. short-term clinical outcome of young homeless people in contact with a designated mental health service, Among the referred clients, the prevalence of severe and persistent mental illness and substance use disorders was 76.5% and 48.5%, respectively. At 6 months, 24 clients (35.3%) had improved clinically, and 33 (48.5%) were housed. Logistic regression identified 2 factors associated with clinical improvement: the number of visits with a psychiatrist and treatment adherence. The same 2 factors were associated with higher odds of housing, and presence of substance use disorder was associated with lower odds of housing at 6-month follow-up. Young homeless people have high rates of psychiatric disorders and related complex needs. However, they often find it difficult to access mainstream mental health services. The aim of this study was to establish the and whether this is predicted by variables in young people's profiles. Young people reported a range of previous adversities and service contacts, and high HoNOS and risk scores. There was significant improvement on most HoNOS items for those who attended more than one session, but only one risk behaviour (self-harm) significantly decreased. Previous experience of mental health problems and agreed completion of treatment predicted better clinical outcome. Despite their multiple and complex mental health needs, at least a proportion of young homeless people, can 45 engage and benefit from their contact with a designated mental health service. Methodological considerations References (Cwikel 1994) Country Israel Population Measure/Method Outcome The epidemiological triangle of host, agent, and environmental risk factors is presented as a method of organizing available research on homelessness and conceptualizing methods of treatment and prevention. Diagnostic Interview Schedule (DIS) administered by a clinical social worker + a full clinical psychiatric social work assessment + a thorough and systematic clinical psychiatric evaluation by a psychiatrist or psychologist Homeless Supplement to the Diagnostic Interview Schedule Compared to clinician assessment, structured interviews underdiagnosed antisocial personality disorder (ASPD) and overdiagnosed major depression. Alcohol use disorder and schizophrenia showed only small discrepancies by assessment method. Drug use disorder revealed no bias according to method of ascertainment, but showed very discrepant kappa levels comparing DIS to clinician assessment in the two different comparison contexts. (Koegel, Burnham et al. 1992) (North, Pollio et al. 1997) US (North, Eyrich et al. 2004) US Test-rest analysis Subtance Abuse-no direct link with homelessness – (Vangeest and Johnson 2002) US To investigate whether substance abuse is a direct factor in the explanation of homelessness or one that operates indirectly through disaffiliation and human capital processes to place individuals at greater risk of the condition. Analysis of several 46 nested models of homelessness links substance abuse only indirectly to loss of domicile, primarily through its impact on social and institutional affiliations. Contrary to expectations, substance abuse did not impact homelessness indirectly by diminishing the accumulation of human capital. CONCLUSIONS: The role of disaffiliation as a proximate cause of homelessness was confirmed. This locates the phenomenon within the context of society itself, as a direct result of a breakdown in the social bonds necessary for human community. Substance abuse plays a critical role in this breakdown, negatively influencing social as well as institutional relationships Policy (Becker and Kunstmann 2001) Germany (Gupta 1995) US (Staller 2004) US (Velleman, Baker et al. 2007) UK Provides: (1) brief information on the social and economic background of homelessness in Germany; (2) a summary of existing research on homelessness and mental health; and (3) a discussion of health-care approaches and further development of health services for mentally ill homeless people. The authors note that there is no evidence that deinstitutionalization was a major factor leading to the increase in homelessness in Germany, but the extent to which established psychiatric outpatient services are providing sufficient support for their clientele is debated. It is argued that the problems of homeless people can be overcome only be a functional network of different, responsible, and accountable services. Reviews factors associated with homelessness. The loss of employment and income are significant variables involved in homelessness. During the early decades, most of the homeless were single men with little education and skills who were unemployed. However, recent reports indicate an increasing number of families in the homeless population. Estimates of the number of homeless people range between 300,000 and 3,000,000. Inconsistencies are observed in the public policies, most policymakers dealing with homelessness as a local concern. Homelessness is found to be associated with mental health and unemployment. It can be interpreted as a generalizational problem, an extreme end of poverty syndrome, fueled by poor planning and the lack of incentives to find a job System dynamics models help explain why intuitive, well-intentioned solutions to social problems go awry when introduced into complicated social systems. In this article, the author develops a dynamic model, applying it to runaway and homeless youth behavior and shelter usage. Together, the model and supporting evidence imply that simple linear thinking may guide policy expansion to the detriment of homeless youth. Shelters provide incentives for other service systems to neglect difficult cases, which raises serious questions about the efficacy of the shelter system. This model provides common ground upon which practitioners, administrators, policymakers, and research communities can consider the impact and effectiveness of policy and service. Furthermore, the model challenges these communities to bring dynamic system considerations to their work Notes that there is convincing evidence that homeless people have higher rates of both mental health and substance misuse problems than the general population, in addition to lowered access to services and other helping resources. It is proposed that a model of care which includes designated, well-trained, and well-supervised workers who can work effectively across 47 the various domains of mental health, substance misuse, and housing will be the main future direction. The author argues that it is important to adopt a holistic (and pragmatic) view as to what the targets of treatment should be, and that therapists need very high levels of skill in engagement. In addition, the assessment of co-existing mental health and alcohol/other drug use problems in people who are also homeless should follow a similar process as for other clients. However, there are important individual barriers and organizational issues that need to be addressed. The author concludes by suggesting that there are four areas from which treatment ideas can be drawn: substance misuse, mental health generally, assertive outreach in particular, and housing. 48 References Aichhorn, W., S. Santeler, et al. (2008). "[Prevalence of psychiatric disorders among homeless adolescents]." Neuropsychiatrie: Klinik, Diagnostik, Therapie Und Rehabilitation: Organ Der Gesellschaft Österreichischer Nervenärzte Und Psychiater 22(3): 180-188. Andres-Lemay, V. J., E. Jamieson, et al. (2005). "Child abuse, psychiatric disorder, and running away in a community sample of women." Canadian Journal Of Psychiatry. Revue Canadienne De Psychiatrie 50(11): 684-689. Ball, S. A., P. Cobb-Richardson, et al. (2005). "Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trial." Comprehensive Psychiatry 46(5): 371-379. Barak, Y. and A. Cohen (2003). "Characterizing the elderly homeless: a 10-year study in Israel." Archives Of Gerontology And Geriatrics 37(2): 147-155. Bassuk, E. L., J. C. Buckner, et al. (1998). "Prevalence of mental health and substance use disorders among homeless and lowincome housed mothers." The American Journal Of Psychiatry 155(11): 1561-1564. Bassuk, E. L., R. Dawson, et al. (2001). "Post-traumatic stress disorder in extremely poor women: implications for health care clinicians." Journal Of The American Medical Women's Association (1972) 56(2): 79-85. Bassuk, E. L., S. Melnick, et al. (1998). "Responding to the needs of low-income and homeless women who are survivors of family violence." Journal Of The American Medical Women's Association (1972) 53(2): 57-64. Bassuk, E. L., L. Rubin, et al. (1984). "Is homelessness a mental health problem?" The American Journal Of Psychiatry 141(12): 1546-1550. Bearsley-Smith, C., L. Bond, et al. (2008). "The psychosocial profile of adolescent risk of homelessness." European Child & Adolescent Psychiatry 17(4): 226-234. Bebbington, P. E., D. Bhugra, et al. (2004). "Psychosis, victimisation and childhood disadvantage: Evidence from the second British National Survey of Psychiatric Morbidity." British Journal of Psychiatry 185(3): 220-226. Bebout, R. R., M. Harris, et al. (2001). Trauma-informed approaches to housing. Using trauma theory to design service systems. San Francisco, CA US, Jossey-Bass: 47-55. Becker, H. and W. Kunstmann (2001). "The homeless mentally ill in Germany." International Journal of Mental Health 30(3): 57-73. Belcher, J. R., J. A. Greene, et al. (2001). "Considering pathways into homelessness: mothers, addictions, and trauma." Journal of Addictions Nursing 13(3/4): 199-208. 49 Bhui, K., L. Shanahan, et al. (2006). "Homelessness and mental illness: a literature review and a qualitative study of perceptions of the adequacy of care." The International Journal Of Social Psychiatry 52(2): 152-165. Blankertz, L. E., R. A. Cnaan, et al. (1993). "Childhood risk factors in dually diagnosed homeless adults." Social Work 38(5): 587596. Booth, R. E. and Y. Zhang (1996). "Severe aggression and related conduct problems among runaway and homeless adolescents." Psychiatric Services 47(1): 75-80. Breakey, W. R., P. J. Fischer, et al. (1989). "Health and mental health problems of homeless men and women in Baltimore." JAMA: The Journal Of The American Medical Association 262(10): 1352-1357. Browne, A. (1993). "Family violence and homelessness: The relevance of trauma histories in the lives of homeless women." American Journal of Orthopsychiatry 63(3): 370-384. Browne, A. and S. S. Bassuk (1997). "Intimate violence in the lives of homeless and poor housed women: Prevalence and patterns in an ethnically diverse sample." American Journal of Orthopsychiatry 67(2): 261-278. Buckner, J. C., E. L. Bassuk, et al. (1993). "Mental health issues affecting homeless women: implications for intervention." The American Journal Of Orthopsychiatry 63(3): 385-399. Buhrich, N., T. Hodder, et al. (2000). "Lifetime prevalence of trauma among homeless people in Sydney." The Australian And New Zealand Journal Of Psychiatry 34(6): 963-966. Carroll, J. J. and L. A. Trull (1999). "Homeless African American women's interpretations of child abuse as an antecedent of chemical dependence." Early Child Development and Care 155: 1-16. Caton, C. L. M., P. E. Shrout, et al. (1995). "Risk factors for homelessness among women with schizophrenia." American Journal of Public Health 85(8 part 1): 1153-1156. Cauce, A. M., M. Paradise, et al. (2000). "The characteristics and mental health of homeless adolescents: Age and gender differences." Journal of Emotional and Behavioral Disorders 8(4): 230-239. Chen, X., L. Thrane, et al. (2007). "Onset of conduct disorder, use of delinquent subsistence strategies, and street victimization among homeless and runaway adolescents in the Midwest." Journal Of Interpersonal Violence 22(9): 1156-1183. Chen, X., K. A. Tyler, et al. (2004). "Early Sexual Abuse, Street Adversity, and Drug Use Among Female Homeless and Runaway Adolescents in the Midwest." Journal of Drug Issues 34(1): 1-21. Christensen, R. C., C. C. Hodgkins, et al. (2005). "Homeless, mentally ill and addicted: the need for abuse and trauma services." Journal of Health Care for the Poor & Underserved 16(4): 615-621. 50 Commander, M., A. Davis, et al. (2002). "A comparison of homeless and domiciled young people." Journal of Mental Health 11(5): 557-564. Commander, M. J. and S. M. Odell (2001). "A comparison of the needs of homeless and never homeless patients with psychotic disorders." Journal of Mental Health 10(4): 449-456. Connolly, A. J., P. Cobb-Richardson, et al. (2008). "Personality disorders in homeless drop-in center clients." Journal of Personality Disorders 22(6): 573-588. Cougnard, A., S. Grolleau, et al. (2006). "Psychotic disorders among homeless subjects attending a psychiatric emergency service." Social Psychiatry And Psychiatric Epidemiology 41(11): 904-910. Craig, T. K. and S. Hodson (1998). "Homeless youth in London: I. Childhood antecedents and psychiatric disorder." Psychological Medicine 28(6): 1379-1388. Crane, M. (1998). "The associations between mental illness and homelessness among older people: an exploratory study." Aging & Mental Health 2(3): 171-180. Cwikel, J. (1994). "Social epidemiology: An integrative research and practice strategy applied to homelessness." Journal of Social Service Research 19(1): 23-47. Davies-Netzley, S., M. S. Hurlburt, et al. (1996). "Childhood abuse as a precursor to homelessness for homeless women with severe mental illness." Violence And Victims 11(2): 129-142. DeMallie, D. A., C. S. North, et al. (1997). "Psychiatric disorders among the homeless: a comparison of older and younger groups." The Gerontologist 37(1): 61-66. Desai, R. A., I. Harpaz-Rotem, et al. (2008). "Impact of the seeking safety program on clinical outcomes among homeless female veterans with psychiatric disorders." Psychiatric Services (Washington, D.C.) 59(9): 996-1003. Dickey, B. (2000). "Review of programs for persons who are homeless and mentally ill." Harvard Review Of Psychiatry 8(5): 242250. Driessen, M. and H. Dilling (1997). "[Psychiatric disorders in homeless persons--Anglo-American studies of epidemiology and management]." Psychiatrische Praxis 24(4): 162-166. Eagle, P. F., C. L. M. Caton, et al. (1990). Homelessness and mental illness. Homeless in America. New York, NY US, Oxford University Press: 59-75. Fazel, S., V. Khosla, et al. (2008). "The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis." Plos Medicine 5(12): e225-e225. 51 Feitel, B., N. Margetson, et al. (1992). "Psychosocial background and behavioral and emotional disorders of homeless and runaway youth." Hospital & Community Psychiatry 43(2): 155-159. Fichter, M. M., M. Koniarczyk, et al. (1996). "Mental illness in a representative sample of homeless men in Munich, Germany." European Archives of Psychiatry and Clinical Neuroscience 246(4): 185-196. Fichter, M. M. and N. Quadflieg (2005). "Three year course and outcome of mental illness in homeless men: a prospective longitudinal study based on a representative sample." European Archives Of Psychiatry And Clinical Neuroscience 255(2): 111-120. Fischer, P. J. and W. R. Breakey (1991). "The epidemiology of alcohol, drug, and mental disorders among homeless persons." American Psychologist 46(11): 1115-1128. Fischer, P. J., S. Shapiro, et al. (1986). "Mental health and social characteristics of the homeless: a survey of mission users." American Journal Of Public Health 76(5): 519-524. Folsom, D. and D. V. Jeste (2002). "Schizophrenia in homeless persons: a systematic review of the literature." Acta Psychiatrica Scandinavica 105(6): 404-413. Gonzalez, G. and R. A. Rosenheck (2002). "Outcomes and service use among homeless persons with serious mental illness and substance abuse." Psychiatric Services (Washington, D.C.) 53(4): 437-446. Goodman, L. A. (1991). "The prevalence of abuse among homeless and housed poor mothers: a comparison study." The American Journal Of Orthopsychiatry 61(4): 489-500. Goodman, L. A., M. A. Dutton, et al. (1995). "Episodically homeless women with serious mental illness: prevalence of physical and sexual assault." The American Journal Of Orthopsychiatry 65(4): 468-478. Goodman, L. A., S. D. Rosenberg, et al. (1997). "Physical and sexual assault history in women with serious mental illness: prevalence, correlates, treatment, and future research directions." Schizophrenia Bulletin 23(4): 685-696. Goodman, L. A., L. Saxe, et al. (1991). "Homelessness as psychological trauma: Broadening perspectives." American Psychologist 46(11): 1219-1225. Greifenhagen, A. and M. Fichter (1997). "Mental illness in homeless women: An epidemiological study in Munich, Germany." European Archives of Psychiatry and Clinical Neuroscience 247(3): 162-172. Gupta, G. R. (1995). "Homelessness and mental disorder: Policy considerations." Journal of Social Distress & the Homeless 4(1): 33-42. 52 Gwadz, M. V., D. Nish, et al. (2007). "Gender differences in traumatic events and rates of post-traumatic stress disorder among homeless youth." Journal Of Adolescence 30(1): 117-129. Haugland, G., C. Siegel, et al. (1997). "Mental illness among homeless individuals in a suburban county." Psychiatric Services (Washington, D.C.) 48(4): 504-509. Heffron, W. A., B. J. Skipper, et al. (1995). "Risk factors for homelessness: a study of families of origin." Family Medicine 27(9): 586-591. Herman, D. B., E. S. Susser, et al. (1997). "Adverse childhood experiences: are they risk factors for adult homelessness?" American Journal Of Public Health 87(2): 249-255. Hyde, J. (2005). "From home to street: Understanding young people's transitions into homelessness." Journal of Adolescence 28(2): 171-183. Jainchill, N., J. Hawke, et al. (2000). "Gender, psychopathology, and patterns of homelessness among clients in shelter-based TCs." The American Journal Of Drug And Alcohol Abuse 26(4): 553-567. Janus, M. D., F. X. Archambault, et al. (1995). "Physical abuse in Canadian runaway adolescents." Child Abuse & Neglect 19(4): 433-447. Johnson, R. J., L. Rew, et al. (2006). "Gender differences in victimized homeless adolescents." Adolescence 41(161): 39-53. Johnson, R. J., L. Rew, et al. (2006). "The relationship between childhood sexual abuse and sexual health practices of homeless adolescents." Adolescence 41(162): 221-234. Kamieniecki, G. W. (2001). "Prevalence of psychological distress and psychiatric disorders among homeless youth in Australia: A comparative review." Australian and New Zealand Journal of Psychiatry 35(3): 352-358. Karim, K., V. Tischler, et al. (2006). "Homeless children and parents: short-term mental health outcome." International Journal of Social Psychiatry 52(5): 447-458. Kaufman, J. G. and C. S. Widom (1999). "Childhood victimization, running away, and delinquency." Journal of Research in Crime and Delinquency 36(4): 347-370. Khurana, S., N. Sharma, et al. (2004). "Mental health status of runaway adolescents." Indian Journal Of Pediatrics 71(5): 405-409. Kim, M. M. and E. M. Arnold (2004). "Stressful life events and trauma among substance-abusing homeless men." Journal of Social Work Practice in the Addictions 4(2): 3-19. Kim, M. M. and J. D. Ford (2006). "Trauma and post-traumatic stress among homeless men: a review of current research." Journal of Aggression, Maltreatment & Trauma 13(2): 1-22. 53 Koegel, P., M. A. Burnam, et al. (1988). "The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles." Archives of General Psychiatry 45(12): 1085-1092. Koegel, P., M. A. Burnham, et al. (1992). Problems in the assessment of mental illness among the homeless: An empirical approach. Homelessness: A national perspective. New York, NY US, Plenum Press: 77-99. Kovess, V. and C. Mangin Lazarus (1999). "The prevalence of psychiatric disorders and use of care by homeless people in Paris." Social Psychiatry And Psychiatric Epidemiology 34(11): 580-587. Lester, K. M., J. B. Milby, et al. (2007). "Impact of behavioral contingency management intervention on coping behaviors and PTSD symptom reduction in cocaine-addicted homeless." Journal Of Traumatic Stress 20(4): 565-575. Maguire, N. (2006). "Cognitive behavioural therapy and homelessness: A case series pilot study." Behavioural and Cognitive Psychotherapy 34(1): 107-111. Martijn, C. and L. Sharpe (2006). "Pathways to youth homelessness." Social Science & Medicine 62(1): 1-12. McGilloway, S. a. and M. Donnelly (2001). "Prevalence and nature of mental health problems among single, homeless people in Belfast, Northern Ireland." International Journal of Mental Health 30(3): 40-49. McManus, H. H. and S. J. Thompson (2008). "Trauma among unaccompanied homeless youth: the integration of street culture into a model of intervention." Journal of Aggression, Maltreatment & Trauma 16(1): 92-109. McQuiston, H. L., P. M. Gillig, et al. (2006). Mental Illness and Homelessness: An Introduction. Clinical guide to the treatment of the mentally ill homeless person. Arlington, VA US, American Psychiatric Publishing, Inc.: 1-8. Minkoff, K., R. E. Drake, et al. (1992). Homelessness and dual diagnosis. Treating the homeless mentally ill: A report of the Task Force on the Homeless Mentally Ill. Arlington, VA US, American Psychiatric Publishing, Inc.: 221-247. Morrell-Bellai, T., P. N. Goering, et al. (2000). "Becoming and remaining homeless: a qualitative investigation." Issues in Mental Health Nursing 21(6): 581-604. Morrissey, J. P., M. O. Calloway, et al. (2002). "Integration of service systems for homeless persons with serious mental illness through the ACCESS program. Access to Community Care and Effective Services and Supports." Psychiatric Services (Washington, D.C.) 53(8): 949-957. Mounier, C. and E. Andujo (2003). "Defensive functioning of homeless youth in relation to experiences of child maltreatment and cumulative victimization." Child Abuse & Neglect 27(10): 1187-1204. Mundy, P., M. Robertson, et al. (1990). "The prevalence of psychotic symptoms in homeless adolescents." Journal Of The American Academy Of Child And Adolescent Psychiatry 29(5): 724-731. 54 North, C. S., K. M. Eyrich, et al. (2004). "The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses." International Journal of Methods in Psychiatric Research 13(3): 184-191. North, C. S., D. E. Pollio, et al. (1997). "A comparison of clinical and structured interview diagnoses in a homeless mental health clinic." Community Mental Health Journal 33(6): 531-543. North, C. S. and E. M. Smith (1992). "Posttraumatic stress disorder among homeless men and women." Hospital & Community Psychiatry: A Journal of the American Psychiatric Association 43(10): 1010-1016. North, C. S., E. M. Smith, et al. (1993). "Is antisocial personality a valid diagnosis among the homeless?" The American Journal Of Psychiatry 150(4): 578-583. North, C. S., E. M. Smith, et al. (1994). "Violence and the homeless: an epidemiologic study of victimization and aggression." Journal Of Traumatic Stress 7(1): 95-110. North, C. S., S. J. Thompson, et al. (1997). "A diagnostic comparison of homeless and nonhomeless patients in an urban mental health clinic." Social Psychiatry And Psychiatric Epidemiology 32(4): 236-240. Nyamathi, A., L. Bayley, et al. (1999). "Perceived factors influencing the initiation of drug and alcohol use among homeless women and reported consequences of use." Women & Health 29(2): 99-114. Nyamathi, A., S. L. Wenzel, et al. (2001). "Comparison of psychosocial and behavioral profiles of victimized and nonvictimized homeless women and their intimate partners." Research In Nursing & Health 24(4): 324-335. Nyamathi, A. M., D. Longshore, et al. (2001). "Childhood predictors of daily substance use among homeless women of different ethnicities." American Behavioral Scientist 45(1): 35-50. O'Reilly, M., H. C. Taylor, et al. (2009). ""Nuts, schiz, psycho": An exploration of young homeless people's perceptions and dilemmas of defining mental health." Social Science & Medicine (1982) 68(9): 1737-1744. Philippot, P., C. Lecocq, et al. (2007). "Psychological research on homelessness in Western Europe: A review from 1970 to 2001." Journal of Social Issues 63(3): 483-504. Pollio, D. E., C. S. North, et al. (1997). "Predictors of achieving stable housing in a mentally ill homeless population." Psychiatric Services (Washington, D.C.) 48(4): 528-530. Power, C. and J. Attenborough (2003). "Up from the streets: A follow-up study of people referred to a specialist team for the homeless mentally ill." Journal of Mental Health 12(1): 41-49. Powers, J. L., B. Jaklitsch, et al. (1989). "Behavioral characteristics of maltreatment among runaway and homeless youth." Early Child Development and Care 42: 127-139. 55 Rayburn, N. R., S. L. Wenzel, et al. (2005). "Trauma, Depression, Coping, and Mental Health Service Seeking Among Impoverished Women." Journal of Consulting and Clinical Psychology 73(4): 667-677. Rees, S. (2009) “Mental Ill Health in the Adult Single Homeless Population: a review of the literature". Crisis/PHRU Reinking, D. P., J. R. Wolf, et al. (2001). "[High prevalence of mental disorders and addiction problems among the homeless in Utrecht]." Nederlands Tijdschrift Voor Geneeskunde 145(24): 1161-1166. Rew, L. (2002). "Relationships of sexual abuse, connectedness, and loneliness to perceived well-being in homeless youth." Journal for Specialists in Pediatric Nursing 7(2): 51-63. Rew, L., M. Taylor-Seehafer, et al. (2001). "Sexual abuse, alcohol and other drug use, and suicidal behaviors in homeless adolescents." Issues in Comprehensive Pediatric Nursing 24(4): 225-240. Robert, M., L. Fournier, et al. (2004). "La victimisation et les problèmes de comportement. Deux composantes de profils types de fugueurs adolescents." Child Abuse & Neglect 28(2): 193-208. Rosenheck, R. and A. Fontana (1994). "A model of homelessness among male veterans of the Vietnam War generation." American Journal of Psychiatry 151(3): 421-427. Rosenheck, R., W. Kasprow, et al. (2003). "Cost-effectiveness of supported housing for homeless persons with mental illness." Archives Of General Psychiatry 60(9): 940-951. Rosenthal, D., S. Mallett, et al. (2006). "Why do homeless young people leave home?" Australian & New Zealand Journal of Public Health 30(3): 281-285. Ryan, K. D., R. P. Kilmer, et al. (2000). "Psychological consequences of child maltreatment in homeless adolescents: untangling the unique effects of maltreatment and family environment." Child Abuse & Neglect 24(3): 333-352. Scott, J. (1993). "Homelessness and mental illness." The British Journal Of Psychiatry: The Journal Of Mental Science 162: 314324. Shelton, K. H., P. J. Taylor, et al. (2009). "Risk factors for homelessness: evidence from a population-based study." Psychiatric Services (Washington, D.C.) 60(4): 465-472. Sleegers, J., J. Spijker, et al. (1998). "Mental health problems among homeless adolescents." Acta Psychiatrica Scandinavica 97(4): 253-259. Slesnick, N., M. J. Kang, et al. (2008). "Treatment attendance among homeless youth: the impact of childhood abuse and prior suicide attempts." Substance Abuse 29(2): 43-52. 56 Slesnick, N. and J. Prestopnik (2005). "Dual and multiple diagnosis among substance using runaway youth." The American Journal Of Drug And Alcohol Abuse 31(1): 179-201. Slesnick, N. and J. L. Prestopnik (2005). "Ecologically based family therapy outcome with substance abusing runaway adolescents." Journal Of Adolescence 28(2): 277-298. Smith, E. M., C. S. North, et al. (1993). "Alcohol, drugs, and psychiatric comorbidity among homeless women: an epidemiologic study." The Journal Of Clinical Psychiatry 54(3): 82-87. Spence, S. A., K. H. Lee, et al. (2006). "Childhood abuse and adult violence in homeless people." Psychiatry And Clinical Neurosciences 60(2): 259-259. Staller, K. M. (2004). "Runaway Youth System Dynamics: A Theoretical Framework for Analyzing Runaway and Homeless Youth Policy." Families in Society 85(3): 379-390. Stein, J. A., M. B. Leslie, et al. (2002). "Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: mediating roles of self-esteem and abuse in adulthood." Child Abuse & Neglect 26(10): 1011-1027. Stergiopoulos, V., C. S. Dewa, et al. (2008). "Collaborative mental health care for the homeless: the role of psychiatry in positive housing and mental health outcomes." Canadian Journal Of Psychiatry. Revue Canadienne De Psychiatrie 53(1): 61-67. Stump, M. J. and J. E. Smith (2008). "The relationship between posttraumatic growth and substance use in homeless women with histories of traumatic experience." The American Journal On Addictions / American Academy Of Psychiatrists In Alcoholism And Addictions 17(6): 478-487. Sumerlin, J. R. (1999). "Cognitive-affective preparation for homelessness: quantitative and qualitative analyses of childhood out-ofhome placement and child abuse in a sample of homeless men." Psychological Reports 85(2): 553-573. Tam, T. W., C. Zlotnick, et al. (2003). "Longitudinal perspective: Adverse childhood events, substance use, and labor force participation among homeless adults." American Journal of Drug and Alcohol Abuse 29(4): 829-846. Taylor-Seehafer, M., D. Jacobvitz, et al. (2008). "Patterns of attachment organization, social connectedness, and substance use in a sample of older homeless adolescents: preliminary findings." Family & Community Health 31(1S): S81-8. Taylor, H., M. Stuttaford, et al. (2006). "Why a 'roof' is not enough: the characteristics of young homeless people referred to a designated mental health service." Journal of Mental Health 15(4): 491-501. Taylor, H., M. Stuttaford, et al. (2007). "Short-term outcome of young homeless people in contact with a designated mental health service." European Journal of Psychiatry 21(4): 268-278. 57 Taylor, K. M. and L. Sharpe (2008). "Trauma and post-traumatic stress disorder among homeless adults in Sydney." The Australian And New Zealand Journal Of Psychiatry 42(3): 206-213. Thompson, S. J. (2005). "Factors Associated with Trauma Symptoms Among Runaway/Homeless Adolescents." Stress, Trauma and Crisis: An International Journal 8(2): 143-156. Thompson, S. J. and E. K. Carll (2007). Youth homelessness and trauma. Trauma psychology: Issues in violence, disaster, health, and illness, Vol 2: Health and illness. Westport, CT US, Praeger Publishers/Greenwood Publishing Group: 203-229. Thrane, L. E., D. R. Hoyt, et al. (2006). "Impact of family abuse on running away, deviance, and street victimization among homeless rural and urban youth." Child Abuse & Neglect 30(10): 1117-1128. Timms, P. W. and A. H. Fry (1989). "Homelessness and mental illness." Health Trends 21(3): 70-71. Tischler, V., V. Edwards, et al. (2009). "Working therapeutically with mothers who experience the trauma of homelessness: an opportunity for growth." Counselling & Psychotherapy Research 9(1): 42-46. Tischler, V. A. and P. Vostanis (2007). "Homeless mothers: Is there a relationship between coping strategies, mental health and goal achievement?" Journal of Community & Applied Social Psychology 17(2): 85-102. Tiwari, P. A., N. Gulati, et al. (2002). "Why do some boys run away from home?" Indian Journal Of Pediatrics 69(5): 397-399. Tolomiczenko, G. S., T. Sota, et al. (2000). "Personality assessment of homeless adults as a tool for service planning." Journal of Personality Disorders 14(2): 152-161. Tyler, K. A. (2006). "A qualitative study of early family histories and transitions of homeless youth." Journal of Interpersonal Violence 21(10): 1385-1393. Tyler, K. A. and A. M. Cauce (2002). "Perpetrators of early physical and sexual abuse among homeless and runaway adolescents." Child Abuse & Neglect 26(12): 1261-1274. Tyler, K. A., D. R. Hoyt, et al. (2000). "The effects of early sexual abuse on later sexual victimization among female homeless and runaway adolescents." Journal Of Interpersonal Violence 15(3): 235-250. Tyler, K. A., D. R. Hoyt, et al. (2001). "The impact of childhood sexual abuse on later sexual victimization among runaway youth." Journal of Research on Adolescence 11(2): 151-176. Vázquez, C. and M. Muñoz (2001). "Homelessness, mental health, and stressful life events: The Madrid experience." International Journal of Mental Health 30(3): 6-25. Vangeest, J. B. and T. P. Johnson (2002). "Substance abuse and homelessness: direct or indirect effects?" Annals of Epidemiology 12(7): 455-461. 58 Velleman, R., A. Baker, et al. (2007). Homelessness alongside co-existing mental health and drug and alcohol problems. Clinical handbook of co-existing mental health and drug and alcohol problems. New York, NY US, Routledge/Taylor & Francis Group: 177-196. Wallace, R., E. Struening, et al. (1993). Homelessness and psychopathology. Environment and psychopathology. New York, NY US, Springer Publishing Co: 87-101. Warren, J. K., F. Gary, et al. (1994). "Self-reported experiences of physical and sexual abuse among runaway youths." Perspectives in Psychiatric Care 30(1): 23-28. Whitbeck, L. B., D. R. Hoyt, et al. (1997). "Abusive family backgrounds and later victimization among runaway and homeless adolescents." Journal of Research on Adolescence 7(4): 375-392. Whitbeck, L. B., D. R. Hoyt, et al. (1997). "Families of homeless and runaway adolescents: a comparison of parent/caretaker and adolescent perspectives on parenting, family violence, and adolescent conduct." Child Abuse & Neglect 21(6): 517-528. Whitbeck, L. B., D. R. Hoyt, et al. (2007). "Victimization and posttraumatic stress disorder among runaway and homeless adolescents." Violence And Victims 22(6): 721-734. Whitbeck, L. B., K. D. Johnson, et al. (2004). "Mental disorder and comorbidity among runaway and homeless adolescents." Journal of Adolescent Health 35(2): 132-140. Whitbeck, L. B. and R. L. Simons (1993). "A comparison of adaptive strategies and patterns of victimization among homeless adolescents and adults." Violence and Victims 8(2): 135-152. Winkleby, M. A., B. Rockhill, et al. (1992). "The medical origins of homelessness." American Journal of Public Health 82(10): 13941398. Yoder, K. A., S. L. Longley, et al. (2008). "A dimensional model of psychopathology among homeless adolescents: suicidality, internalizing, and externalizing disorders." Journal Of Abnormal Child Psychology 36(1): 95-104. Zozus, R. T., Jr. and M. Zax (1991). "Perceptions of childhood: exploring possible etiological factors in homelessness." Hospital & Community Psychiatry 42(5): 535-537. 59