CVS I: Chest Pain, IHD, CCF
advertisement

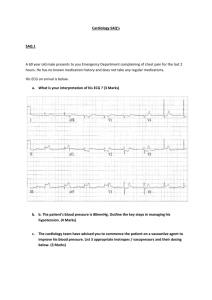
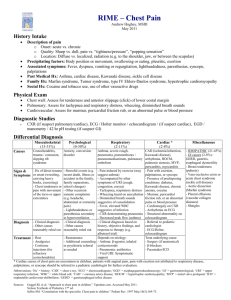
SAQ CVS 1 A 55 year old man is brought to hospital by ambulance complaining of severe headache, vomiting and blurred vision. On initial examination his BP is 260 / 145, similar in both arms. His Glasgow Coma Score is 14. CT scan reveals no abnormality. Question Discuss the pharmacological treatment options for the treatment of his hypertension. Answer Answer and Interpretation FACEM SAQ Exam 2009.1 – Question 4 The overall pass rate for this question was 63/81 (78%). Pass Criteria The examiner pair felt that this was an excellent question on a core EM presentation. Pass criteria included nominating an appropriate range of medications with appropriate dosages and routes of administration within the context of close physiological monitoring and safe BP reductions. Features of unsuccessful answers Inadequate answers suggested oral administration or inappropriate dosages. An 82 year old man is brought to the emergency department following a brief collapse at home. He has a history of chronic renal failure and hypertension. His medications include an angiotensin converting enzyme inhibiting agent (ACEI), frusemide and metoprolol. He has no traumatic injuries from this episode. Examination reveals: His ECG demonstrates third degree atrioventricular block. Question Describe your management Answer Answer and Interpretation FACEM SAQ Exam 2010.1 – Question 6 The overall pass rate for this question was 45/70 (64.3%) Pass Criteria Recognition of shock Consideration of all of: IV Fluids Atropine Pacing (transcutaneous or transvenous) Use of inotropes/chronotropes Discussion of disposition to appropriately monitored bed. Better answers described above in context of possible causes of collapse in this patient – Bblocker toxicity, ACS, electrolyte imbalance, head injury, hypothermia. Features of unsuccessful answers Failure to recognise shock Failure to take steps to correct rate A 47 year old man with a history of hypertension and depression has presented to your emergency department following deliberate self poisoning approximately 3hrs ago with 20 x 240mg slow release verapamil tablets. Question Describe your management of this patient. Answer Answer and Interpretation FACEM SAQ Exam 2009.1 – Question 3 The overall pass rate for this question was 62/81 (76.5%). Pass Criteria The examiners felt that this was a good toxicology question. Comprehensive answers took into context the time of presentation and utilized whole bowel irrigation as the decontamination method of choice plus discussed the evidence for other therapies such as activated charcoal, glucose/insulin and glucagon. Appropriate disposition, including psychiatric assessment, was deemed mandatory also. Features of unsuccessful answers Poor answers failed to address the critical nature of this presentation and the indication for whole bowel irrigation. Discuss the investigations for a suspected pulmonary embolus in a 24 year old woman who is 10 weeks pregnant. Answer Answer and Interpretation FACEM SAQ Exam 2010.1 – Question 4 The overall pass rate for this question was 47/70 (67.1%) Pass Criteria Discussion of supportive tests, definitive tests, risk benefit analysis Rational approach to reducing radiation risk (when discussing the definitive tests) Features of unsuccessful answers Clear statement showing lack of understanding of radiation risk (CTPA and V/Q) Algorithm using both VQ and CTPA Stating that CTPA was not indicated in pregnancy Not “discussing” question A 67 year old male presents to your urban district emergency department 1 hour post onset of chest pain. His ECG reveals acute ST segment elevation of 3mm in leads V3, V4 and V5. He is treated with aspirin (300mg), reteplase (two 10 unit boluses 30 minutes apart), and unfractionated heparin (5000 unit bolus and 1000 units/hr infusion). Sixty minutes after the thrombolysis is administered the patient complains of increasing left sided chest discomfort and shortness of breath. A repeat CXR reveals a new large left-sided collection in the pleural space. His vital signs are currently heart rate 100, BP 85/55, RR 26 and O2 sat 92% on 6L per minute via Hudson mask.. Question a. Outline your management of this situation. Answer Answer and Interpretation Facem Vaq Exam 2003.1 – Question 8 The overall pass rate for this question was 56 / 83 (67.5%). Examiners considered this a good question that covered a relevant scenario but included many issues other than just basic resuscitation to cover. These included an appreciation of alternate diagnoses to AM1 (such as aortic dissection), reversal of anticoagulation (prior to), insertion of an ICC, likely need for transfer. Failures tended not to cover these and ‘consider’ rather than say what they would do. A 53 year old previously well man presents with a 6 hour history of palpitations. He is otherwise asymptomatic. His vitals signs are: ECG reveals atrial fibrillation with a rate of 130 /minute. His assessment does not reveal a cause for his arrhythmia. Question Discuss the management options for this patient. Answer (100 %) Answer and Interpretation FACEM SAQ Exam 2009.1 – Question 7 The overall pass rate for this question was 60/81 (74.1%). Pass Criteria Pass criteria were addressing the options of no treatment, rate control, cardioversion (chemical/electrical) and anticoagulation. Features of unsuccessful answers Poor answers failed to discuss these issues in the context of this presentation or missed a major criterion altogether. 5. An elite athlete has presented with chest discomfort after training. He has a family history of HOCM and is concerned that he may also have it. Your findings on physical examination include: BP 110/70, pulse rate 40/min, displaced apex beat, prominent 4 th heart sound, systolic ejection murmur, otherwise unremarkable. His ECG shows Mobitz Type 1 block, incomplete RBBB, LVH and ST elevation in the chest leads. CXR shows CT ratio of 0.6 and prominent upper lobe veins. Discuss these findings. Are any other investigations justifiable? HOCM – asymmetrical LV/RVOT hypertrophy and mitral valve problems SOB, angina, syncope, sudden death, a wave, double apex beat S4, pansystollic murmur if MR, louder with valsalva, last 2 important differentiating features LVH, LAH, septal Q waves CXR usually normal, can have venous congestion Athlete – benign ’s reverse on cessation training, 40% male elite athletes must rule out IHD, HOCM, pericarditis Signs – bradycardia, displaced apex beat, ejection systolic murmur, no failure ECG – sinus brady, incomplete RBBB, 1O or Mobitz I common, LVH and ST repolarisation ’s common CXR – can have prominent pulmonary vasculature due to CO Echo – uniform hypertrophy and normal mitral valve This fellow has features mainly suggestive of benign cardiac hypertrophy of the elite athlete, BUT need to investigate further if : family history HOCM/sudden death at young age (30’s and 40’s) hypertension or heart failure murmur accentuates with valsalva develops Mobitz II, 3O block or long QT This fellow 1. Rule out acute event now (IHD, pericarditis) troponins and ECG, CXR 2. Confirm family history HOCM 3. Echo indicated semi-urgently – avoid strenuous exercise until done 4. Cardiologist review 5. Consider other causes of his pain SAQ 336 A 65 year old female presents 10 days following coronary artery bypass surgery at your regional referral hospital. She is complaining of lightheadedness and sharp chest pain. On examination, she has a clean median sternotomy wound, pulse rate 105/min, blood pressure 145/90, respiratory rate 24/min, SaO2 94% (room air). There is dullness to percussion and reduced breath sounds at the left lung base. ECG shows sinus tachycardia with ST-T changes present on her pre-discharge ECG. Chrst xray shows a moderate left pleural effusion. a) Outline your assessment of this patient (50%) b) Outline your management of this patient (50%) ISSUES Left pleural effusion 10d post-CABG, mild tachycardia and hypoxia with tachypnoea. DDx pleural effusion Transudate - cardiac failure - other: hepatic/renal failure/hypoalbunimea (unlikely) Exudate - infection eg community acquired pneumonia - inflammatory eg pleuritis secondary to pleural irritation - PE - other: autoimmune (SLE), pancreatitis, malignancy (less likely) Empyema Hemothorax - ?2 Chylothorax – a) ASSESSMENT Aims: - look for cause - assess severity/complications 1. History HPC - duration of symptoms – CP, lightheadedness gradual – slow accumulation of fluid sudden – hemothorax - associated symptoms – infective: fever, productive cough, malaise PE: pleuritic CP, SOB, palpitation, presyncope CCF: SOB/orthopnoea/PND, peripheral edema PMHx RF for DVT/PE: recent OT, immobilisation, ?DVT prophylaxis, PHx/FHx DVT, hormonal Rx, smoking Underlying malignancy, autoimmune d/o Cardiorespiratory reserve Meds Antiplatelets Anticoagulants Immunosuppressants Allergies, Alcohol SHx ADLs, supports 2. Examination Immediate life threats: A,B airway patency and protection wrt GCS RR, sats ?hypoxia ?respiratory mm. fatigue C monitor for tachycardia, hypotension (postural) , cap refil ?mediastinal (tracheal) shift 2 D GCS E BSL, temp. Systems examination: Lungs AE, creps ?pulmonary edema ?consolidation Cardiac HS, added sounds, murmur (new or old) ?pericardial effusion signs of failure – pulmonary edema, elevated JVP, peripheral edema Abdo congested liver, ascites Neuro GCS, ?focal neurology (thromboembolism) Skin ?bruising 2 3. Investigations Bedside: - ECG no new changes - ABG PaO2 ?hypoxemia pH ?acidosis (resp or metabolic) Laboratory: - FBE ?anemia ?raised WCC in infection ?low platelets (?HITS) - U&E renal function, hypoalbuminemia - LFT ?hepatitis 2 - TnI compare to discharge Tn - coags ?warfarin/heparin - G&H may need BTF - ?sternotomy wound swab - Pleural fluid tap: m/c/s WCC, RCC protein glucose LDH - BC if febrile > 38.5 Imaging: Repeat CXR CT chest/CTPA ?PE Echo cardiac contractility, RWMA, pericardial collection, valves b) MANAGEMENT Acute area, full non-invasive monitoring Treatment 1. Stabilisation A,B consider NIPPV/IPPV if: Hypoxic Respiratory mm. fatigue GCS < 9 Otherwise high flow O2 via NRB C 18g canula Tachycardic – 500ml n/saline, assess response Aim – PR < 100, SBP > 100, CR < 3 sec Watch for pulmonary edema Packed cells if Hb < 110 (transfusion guidelines) If collection is causing hemodynamic compromise via mediastinal shift – ICC, 30F, light sedation, underwater seal drain D monitor GCS, pupils 2. Specific treatment Optimise hemodynamics Drain pleural effusion as above Watch for reflex pulmonary edema Infective IV antibiotics: empiric – iv ceftriaxone + erythromycin – modify according to micro Cardiac failure Diuretics, ACE-inhibitors, +/- inotropes Hemothorax 30F ICC If unstable (>1.5L stat or > 500ml/h) urgent thoracic surgery 3. Treat complications Acute lung injury – supportive Sepsis – iv antibiotics, +/- inotropes Coagulopathy – FFP, platelets, cryoprecipitate as per guidelines Renal failure – fluid balance, +/- dialysis Supportive care Sit up Analgesia - iv morphine 2.5mg doses – titrate Antiemetic – iv metoclopramide 10mg Educate and support patient and family Disposal Unstable HDU/ICU Consider OT for formal drainage Stable CCU Telemetry bed Monitor gas exchange, hemodynamics, fluid balance Involve cardiologist, cardiothoracic surgeon +/- intensivist 1 A 76 year old man presents to the ED after becoming light-headed at church that morning. He has not experienced any chest pain, and his ECG reveals 3 rd degree heart block at a rate of 24 /min. (a) Outline the investigations you would perform (b) Discuss the options for increasing his heart rate. 2 (30%) (70%) The hospital executive in your large urban district hospital has asked you to introduce a chest pain unit, to reduce the work of the frequently full coronary care unit. It is willing to provide you with appropriate resources. (a) Outline the steps you would take in planning this unit. (b) Outline a protocol for a patient referred to this unit (50%) (50%) 3 Describe the role of anti-platelet drugs in the treatment of acute coronary syndromes in the ED. 4. Discuss the pharmacological options that you would consider for the treatment of a hypertensive emergency in the ED. 1. A 72 yo woman presents with a 24 hour history of palpitations. It is her first episode. She reports no other symptoms. Her only past history is hypertension, treated with irbesartan. Examination reveals an alert lady with a BP of 135 /80; ECG shows atrial fibrillation with a rate of 145. Discuss the management options. 7. A 35 year old man complains of calf pain after exercise. He is asymptomatic when you see him. You note that he is hypertensive (160/70 in both arms). He has an ejection systolic murmur plus clinical and ECG signs of moderate LVH. The pulses in his legs are weak. What is the differential diagnosis? What further investigations and treatment does he need? Story suggests vascular insufficiency to legs. Could just be musculo-skeletal strain Differential diagnosis Most likely given story is coarctation aorta Others: Central vascular occlusion eg abdo mass Embolism Peripheral vascular disease – atheroma, Raynaud’s, arteritis Examination Radio-femoral delay, ankle/brachial index Upper and lower limb hypertension Document all peripheral pulses Assoc with bicuspid aortic valve - ?opening snap or ESM? Flow murmur heard over back Exclude AAA Investigations ECG – hypertrophy CXR – notching of ribs by collateral intercostals Echo – TOE only likely to be sensitive enough Peripheral vascular Doppler studies Subtraction angiography of iliacs and lower limbs Arch aortogram Pressure gradient across coarctation Complications if untreated Of peripheral vascular disease limb ischaemia, ulcers and loss Of coarctation Dissection, IHD/CAD, LVF, CVA, endocarditis Treatment choices Balloon dilatation – risk dissection/recurrence Surgical correction if pressure gradient >30mmHg 8. A patient with a prosthetic heart valve has collapsed. Outline how you would assess the patient to determine if the collapse was the result of a complication of the prosthetic valve. History Of collapse event – CVS/neuro symptoms, ?LOC etc, ?previous collapses Of prosthetic valve – when/why/which/where placed? On Warfarin? IVDU? Any previous valve complications? – endocarditis? valve/heart failure?, AMI, CVA, Other co-morbidities? Generic collapse FI questions Examination Vital signs, ABC, GCS, temperature signs SBE thorough neuro and CVS exam other exam Investigations General collapse invx – usual bloods, INR, blood cultures ECG, CXR, infection screen, CT brain if suspect SOL, ICH, trauma, abscess, cerebral event Specific to valve Multiple blood cultures (3+) if SBE suspected Echo – TTE easier but TOE better Bottom line – Echo will give best info on functional status of valve, but other causes collapse need to be ruled out 1.) A 75 year old man is brought into your tertiary level emergency department by ambulance. The ambulance officers tell you he had a sudden onset of severe, sharp chest and back pain 2/24 ago followed by a syncopal episode. When they arrived he was sweaty and agitated and had a paraplegia which resolved 20 minutes later. He has a past history of hypertension but is non compliant with medications. His BP is 180/85 in the right arm and 140/65 in the left arm pulse 80. He remains agitated. , a.) Outline your management. (30%) b.) Discuss investigations that may of benefit in the assessment of this man (70%) 2.) You are asked to improve time taken to thrombolysis for patients with acute myocardial infarction in your hospital. Outline the way that you would do this 2.) An 80 year old woman is brought to your ED after collapsing while on an organi~ThToui.On~iva1, she is confused and dyspnoeic, with PR 50, BP 85/40, s~O29O%(r~~gen). ECG shows a narrow complex bradycardia with no ~ ischaemic changes. a.) outline your investigations b.) describe your treatment options A 52 year old man presents to the ED via ambulance. His wife reports that he has had severe central chest pain for 6 hours. His EGG shows a large anterolateral AMI and a sinus rhythm of 110. He is agitated, with ~PO2 88% on 15 I/rn in 02 and a BP of 80/45. Examination reveals severe LVF. Outline your management. 3.) Discuss the radiological investigations available for the assessment of a patient with suspected pulmonary embolism. The expectation of examiners was that answers to this question would include a clinical risk stratification to guide test selection, acknowledgement of the limited utility of tests such as ABG/ECG/CXR & troponin and a more detailed discussion of the important tests such as D-dimer, V/Q scan, CTPA, echo, Doppler ultrasound and angiography. The better answers concentrated on the more controversial areas with risk stratification as a prominent part of their preferred approach. Failing candidates tended to neglect the importance of pretest risk stratification when deciding on the value or otherwise of tests, did not provide sufficient detail in the important areas or simply failed to “discuss” (and so did not answer the question). 2.) A SQyear-oliLmDn_with a history of rheumatic heart disease dies of bacterial endocarditis after an indwelling catheter insertion in your rgedi5ydbpartrnent. -~ How would you reduce the risks of endocarditis after ED procedures in your department? 2008.2 SAQ 1 A 52 year old woman presents with atypical chest pain and a normal ECG. What features on assessment would influence the disposition of this patient? (100%) The overall pass rate for this question was 51/81 (63%). Pass Criteria The examiners felt that this was a good question in that it tested a topical and common area in Emergency Medicine. Good answers suggested a structure for ACS stratification and recognised the wide differential of chest pain. The best answers demonstrated knowledge of recently published guidelines ( Cardiac Society, TIMI). Features of unsuccessful answers Poor answers either failed to answer the question or did not mention serial ECG/Cardiac Enzymes as part of the risk stratification Describe the use of amiodarone in the emergency department, including its indications and limitations. Answer Answer and Interpretation FACEM SAQ Exam 2006.2 – Question 3 The overall pass rate for this question was 37/57 (64.9%). Pass Criteria Examiners considered that this question worked well as it tested a widely used Emergency Department drug. Candidates were expected to show good knowledge of currently accepted indications and acute toxicity. Extra marks were allocated for those showing knowledge of recent clinical trials and for discussing areas of clinical controversy. Features of unsuccessful answers Candidates who failed the question did not address all the standard indications, showed poor knowledge of common problems with acute use and did not state appropriate dosing schedules. SAQ 165 A 65 year old woman presents to your ED with sudden onset of a painful, cold, pulseless right leg. Outline your management. ISSUES Ischemic right lower limb Sudden = probable embolus rather than thrombus ?source ?AF (90% cardiac, other – AAA) Limb-threatening illness – needs urgent care and vascular referral MANAGEMENT Acute area. Full non-invasive monitoring Call vascular surgeon and interventional radiologist early Treatment 1. Stabilisation High flow O2 to maximise O2 delivery to limb (15L via NRB) Optimise hemodynamics with gentle fluid loading 250ml n/saline titrated to endpoint of PR < 100, SBP > 100 Monitor GCS, BSL, temp Check other limbs 2. Specific treatment mild elevation of limb to prevent venous congestion, relieve pain Anticoagulate: unfractionated heparin iv 60mg/kg load, then 12u/kg/hr infusion, monitor aPTT Definitive treatment: remove clot and reperfuse leg a. Angiography intra-arterial thrombolysis with urokinase embolectomy b. Vascular surgery end-arterectomy fem-pop bypass 3. Treatment of complications (monitor for:) Compartment syndrome Rhabdomyolysis Emboli to other regions/trashing Reperfusion injury eg hyperkalemia Supportive Care Prepare for sedation/GA: ECG, CXR, coags (?spinal anaesthetic), G&H Optimise lung and cardiac function within time limits Analgesia – iv morphine 2.5mg doses – titrate Antiemetic – iv metoclopramide 10mg Pressure area care Inform and support patient and family Disposal OT/Angiography suite for definitive care Ix to find source of embolus: Echo, CT abdomen Input from vascular surgeons, interventional radiologist, +/- anaesthetist SAQ 319 (a) List the clinical signs that may be seen in thoracic aortic dissection (30%) (b) List the diagnostic modalities that may be used in suspected thoracic aortic dissection and comment on the advantages and disadvantages of each (70%) (a) Clinical signs: General signs: • Distressed • Diaphoretic • Tachycardia • Hypertensive / hypotensive (pre-terminal sign) • Hypoxia Specific signs associated with potential complications: • Acute aortic incompetence – new murmur, LVF (pulmonary crepitations). • Pericardial blood – tamponade – raised JVP, muffled heart sounds, hypotension. • Extravascular free rupture – pre-terminal – signs of massive haemothorax. • Aortic branch occlusions: o Carotids – altered level of consciousness, hemiplegia, pulse deficits. o Subclavian – pulse deficits, BP discrepancies. o Renal – renal bruits. o Lumbar / spinal – paraplegia, sensory changes. o Femoral – pulse deficits, ischaemic lower limb. • Pressure effects – Horner’s syndrome, superior vena caval syndrome. (b) Diagnostic modalities: CXR: Advantages: • Simple, rapid, readily available. • Non-invasive. • 85% sensitivity Disadvantages: • Non-specific, not diagnostic. • Cannot be used to exclude dissection – as only 85% sensitivity. CTA Chest: Advantages: • Relatively quick and available. • Non-invasive. • Sensitivity 80-90% • Specificity 87-100% • Identifies other causes of widened mediastinum or causes for the chest pain. Disadvantages: • Only for haemodynamically stable patients. • Requires use of contrast – allergies, renal implications. • Unable to demonstrate aortic valve involvement. • May not be able to demonstrate site of intimal tear, or branch vessel involvement. • Negative predictive value only 86% - potentially have to investigate further. MRI: Advantages: • Non-invasive. • No contrast or radiation • Sensitivity 95-100% • Specificity 94-100% Disadvantages: • Limited availability • Long acquisition time • Requires a haemodynamically stable patient. • No information on coronary artery involvement. Echocardiography: Transthoracic: • Advantages: o Rapid, non-invasive, perform at bedside. o Able to demonstrate aortic incompetence, myocardial function, pericardial blood / tamponade. o Sensitivity 60-85% / Specificity 63-96%. • Disadvantages: o Sensitivity only 60-85% o Poor sensitivity for Type B dissections – difficulty imaging arch and descending aorta. Transoesophageal: • Advantages: o Perform at bedside. o Sensitivity 98-99%. o Demonstrates aortic valve involvement, pericardial blood / tamponade, coronary artery involvement. • Disadvantages: o Invasive. o Requires patient to be sedated or intubated and ventilated. o Not as sensitive for distal dissections. Aortography: Advantages: • Sensitivity – 81-91% / Specificity 90-95%. • Demonstrates aortic valve involvement, coronary artery and branch vessel involvement. Disadvantages: • Invasive. • Use of contrast – allergic and renal implications. • Time-intensive. • Negative predictive value – 84% (may fail to demonstrate false lumen or intimal flap.